Abstract
Purpose
Infection at the pin site remains the most common complication of external fixators (EFs). It is known that hydroxyapatite (HA)-coated pins increase bone adhesion and may lead to reduced rates of reported infections. The present study compares the rates of pin track infection associated with stainless steel and HA-coated pins.
Methods
This is a prospective, multicenter, nonrandomized, comparative intervention study among patients undergoing surgical treatment with EFs of any type between April 2018 and October 2021. Patients were followed up until the removal of the EF, or the end of the study period (ranging from 1 to 27.6 months). The definition of pin track infection was based upon the Maz-Oxford-Nuffield (MON) pin infection grading system.
Results
Overall, 132 patients undergoing external fixation surgery were included. Of these, 94 (71.2%) were male, with a mean age of 36.9 years (SD ± 18.9). Infection of any type (score > 1) was observed in 63 (47.7%) patients. Coated and uncoated-pin track-infection occurred in 45.7% and 48.5% of patients, respectively (P= 0.0887). The probability of developing infection (defined as a score ≥ 2) adjusted for comorbidities and follow-up time was not statistically higher among those who received uncoated pins compared to those who received pins coated with HA (odds ratio (OR) = 1.56, 95% confidence interval (95% CI): 0.67–3.67, p <0.05).
Conclusion
In the present study, the external fixator pin infection rates were similar when using HA coating and standard steel pins.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00264-023-05717-w.
Keywords: External fixator, Pin insertion site infection, Stainless steel pin, Coated pin, Hydroxyapatite
Introduction
External fixators (EFs) that maintain a means of communication between the bone and the external environment, have been successfully used for bone stabilization in the treatment of fractures, correction of deformities, pseudoarthrosis, and osteomyelitis [1–3]. Among the complications related to EFs, the most common is infection at the pin insertion site, especially in fixators kept in place for a long time, with a reported incidence ranging from 11.3 to 100% of cases [4–6].
The clinical manifestations of infection can range from local erythaema with or without the presence of secretion to loosening of the pin with the possibility of deep tissues and systemic complications, such as necrotizing fasciitis and sepsis. However, in the early stages, the clinical diagnosis of infection may be difficult to conclude [7, 8]. To overcome this challenge the Maz-Oxford-Nuffield pin infection grading system has been validated and seems to be a reliable and reproductive methods to assist clinicians at the bed site to define pin-track infection [9, 10].
Different strategies, such as the technique of inserting pins during surgery, local daily care at the site around the pins, and antibiotic prophylaxis, have been attempted to control these infections [11–13]. Additionally, coating technologies and different material compositions of the pins have been tested. Among the types of pin materials and coatings that have been assessed in published clinical studies, there are bioceramics and different metals (stainless steel and titanium), as well as coatings such as hydroxyapatite (HA), HA plus FGF-2 (factor of fibroblast growth 2), silver coating, and iodine coated systems [13–15]. Although HA coating is one of the most studied systems, the real impact towards the reduction of superficial and deep infectious complications still needs to be evaluated [16, 17]. In fact, over the last 20 years, few comparative prospective clinical studies and only two systematic reviews have addressed the role of coated pins in the infection rate of the pin site in human clinical studies. Notwithstanding, due to their osteoconductive properties and likelihood of improvement in pin-to-bone fixation, pins coated with hydroxyapatite (HA) have been regarded as an efficient material to overcome this complication, but the real impact in reducing the rates of superficial and deep pin-track infectious have yet to be proved [14–16].
Few previous studies assessed the clinical impact of the anti-infective HA properties, suggesting that HA-coated pins would likely reduce the incidence of pin-track complications including infections [14, 18]. Given the scarcity of data related to HA and its likely anti-infective properties, in the present study, we evaluate whether its use can lead to a decrease in pin-track infection rates. Potential risk factors associated to pin-track infection were also assessed.
Materials and methods
This is a prospective, multicenter, nonrandomized comparative clinical study in patients undergoing surgical treatment with insertion of EFs of HA-coating or stainless-steel pins between April 2018 and October 2021 in Brazilian tertiary teaching hospitals. Patients were divided into two groups, one group with patients using only stainless steel EFs pins, and the other with patients using only HA-coated EFs pins. The primary objective is to compare the superficial and deep infection rates associated with EFs with HA-coated pins or uncoated steel pins. All human rights norms during patient follow-up, and data collection were strictly followed. The study was approved by the local Research Ethics Committee under protocol number 2,572,550.
Inclusion and exclusion criteria
Patients who underwent surgical treatment with an external fixator of any type for open and closed fractures, correction of deformities, treatment of osteomyelitis and/or pseudoarthrosis, and expecting to maintain EF for a minimum period of one month were included, and followed until EF removal, or the end of study period. Those agreed to participate, signed the informed consent.
Definition of pin-track infection
The definition of superficial and deep infection associated with EF pins was based on the validated Maz-Oxford-Nuffield pin infection grading system (Table S1). Grade 2 infection was considered and beyond, with the presence of skin erythaema, serous or purulent secretion, pain, and tenderness in the soft tissues [10].
Variables studied
The patients included in the study were evaluated at the outpatient setting monthly or according to the clinical need. The data was collected by the principal investigator and by two other orthopaedic surgeons in the outpatient setting. The variables evaluated in the two study groups included demographic data, comorbidities (systemic arterial hypertension, diabetes mellitus, smoking), and underlying medical disease, reasons for external fixator insertion (fracture, pseudoarthrosis, osteomyelitis), and length of time from surgery to the diagnosis of infection.
Insertion methods for external fixation bolts
Pin insertion was performed through an irrigated pre-perforation to reduce the chances of thermal necrosis and consequent loosening or infection. Steel Shanz pins coated with or without hydroxyapatite between 5 and 6 mm in diameter were used.
Statistical analysis
The sample size was based on the total number of patients with infectious complications related to external fixation pins according to previous study [19]. In this study, among all patients involved, who received pins with HA coating or without any coating, 23.7% had complications related to pins. By assuming a significance level of 95% and a power of 80%, a sample size of 119 patients was calculated. By adding an attrition rate of 10% and 5% of lost follow-up, 136 patients were needed in the present study. However, we obtained a final sample of 132 patients. The data table was constructed using Microsoft Excel, and the statistical analysis was conducted using IBM SPSS Statistics version 27 for Windows. The continuous variables are expressed as the mean ± standard deviation or median (25th percentile–75th percentile), and the categorical variables are expressed as absolute and relative frequencies. The associations between the presence of HA coating, categorical and quantitative variables were tested using Pearson’s chi-squared test or Fisher’s exact test when necessary, and analysis of variance with a classification criterion or Mann–Whitney U test. The associations between the chance of developing infection in the follow-up and the presence of HA coating, adjusted for the follow-up time and underlying medical conditions were evaluated using logistic regression models that was used to select significant variables from those identified as significant in univariate analyses. Only variables with significance less than 0.20 (p < 0.20) were included in the logistic regression. Variables with significance less than 0.05 (p < 0.05) in the multiple regression were included in the final model. Infection-free survival grade 2 or 3 was estimated using the Kaplan–Meier method and compared between groups using the log-rank test.
Results
Study population
Overall, 132 patients undergoing external fixation surgery were included and followed up. Of these, 94 (71.2%) were male, with a mean age of 36.9 years (±18.9). Smoking, hypertension, and diabetes mellitus were identified in 12.9%, 9.8%, and 7.6% of patients, respectively. No statistically significant difference between the groups with HA-coated pins and uncoated pins were observed regarding morbidities (Table 1). The main indications for the use of EF were the treatment of tibial/fibular fracture in 28% of cases, tibial pseudoarthrosis in 24.2% of cases, osteomyelitis of the tibia in 15.9% of cases, malunion of the tibia/fibula in 10.6% of cases and pseudoarthrosis of the femur in 9.1% of cases (Table 1). Higher rates of HA-coated pins use were observed among patients with pseudoarthrosis of the femur compared to steel surface pins (28.6% vs. 2.1 %, p <0.001). Table 1 describes the characteristics of the study population.
Table 1.
Characteristics of the study population
| Coating | ||||
|---|---|---|---|---|
| Variable | Global (n=132) | Yes (n=35) | No (n=97) | p |
| Demography | ||||
| Age | 36.9 ± 18.9 | 40.2 ± 14.3 | 35.7 ± 20.3 | 0.165 |
| Male sex | 94 (71.2%) | 25 (71.4%) | 69 (71.1%) | 0.974 |
| Comorbidities | ||||
| Smoking habits | 17(12.9%) | 4 (11.4%) | 13 (13.4%) | 1.000 |
| SAH | 13 (9.8%) | 4 (11.4%) | 9 (9.3%) | 0.744 |
| DM | 10 (7.6%) | 1 (2.9%) | 9 (9.3%) | 0.289 |
| Underlying medical conditions* | ||||
| Pseudoarthrosis of the femur | 12 (9.1%) | 10 (28.6%) | 2 (2.1%) | < 0.001 |
| Pseudoarthrosis of the tibia | 32 (24.2%) | 10 (28.6%) | 22 (22.7%) | 0.486 |
| Pseudoarthrosis of the humerus | 2 (1.5%) | - - | 2 (2.1%) | 1.000 |
| Femur fracture | 5 (3.8%) | - - | 5 (5.2%) | 0.324 |
| Tibia/fibula fracture | 37 (28.0%) | 4 (11.4%) | 33 (34.0%) | 0.011 |
| Femural malunion | 4 (3.0%) | 2 (5.7%) | 2 (2.1%) | 0.286 |
| Tibial/fibular malunion | 14 (10.6%) | 6 (17.1%) | 8 (8.2%) | 0.197 |
| Osteomyelitis of the femur | 8 (6.1%) | 3 (8.6%) | 5 (5.2%) | 0.437 |
| Osteomyelitis of the tibia | 21 (15.9%) | 9 (25.7%) | 12 (12.4%) | 0.064 |
| Congenital deformity of the femur | 8 (6.1%) | 1 (2.9%) | 7 (7.2%) | 0.681 |
| Congenital tibial deformity | 10 (7.6%) | 1 (2.9%) | 9 (9.3%) | 0.218 |
| Arthrodesis of the knee | 1 (0.8%) | 1 (2.9%) | - - | 0.265 |
| Ankle arthrodesis | 4 (3.0%) | 2 (5.7%) | 2 (2.1%) | 0.280 |
p probability value; SAH systemic arterial hypertension; DM diabetes mellitus
Values are expressed as the mean ± standard deviation or absolute or relative frequency. *Underline medical condition: some patients had more than one underlying disease undergoing treatment with the same external fixator. Therefore, the total number of underlying diseases does not reflect the total number of patients followed up
Infection rates associated with EF pins
The median follow-up time between groups was not statistically significant. Overall infection (score> 1) was observed in 47.7% of patients. In general, in the present study EFs infection rates were higher among patients using stainless steel pins (Table S2). Nevertheless, no statistically significant difference was observed in the development of infection between the two groups. Coated and uncoated-pin track-infection occurred 45.7% and 48.5%, respectively (P= 0.0887). Table 2 describes the degree of infection associated with the EF pins according to the Maz-Oxford-Nuffield classification. The probability of developing infection (defined as a score ≥ 2) adjusted for follow-up time was not statistically higher among those who received uncoated pins compared to those who received pins coated with HA (odds ratio (OR) = 1.56, 95% confidence interval (95% CI): 0.67–3.67, p <0.05).
Table 2.
Maximum degree of infection during follow-up, according to the Maz Oxford Nuffield classification
| Variable | Global (n=132) | Coating | p | |
|---|---|---|---|---|
| Yes (n=35) | No (n=97) | |||
| Follow-up time& (days) | 187 (91–317) | 207 (154–379) | 174 (90–290) | 0.054 |
| Maz-Oxford-Nuffield infection score | 0.887 | |||
| 1 | 69 (52.3%) | 19 (54.3%) | 50 (51.5%) | |
| 2 | 42 (31.8%) | 10 (28.6%) | 32 (33.0%) | |
| 3 | 21 (15.9%) | 6 (17.1%) | 15 (15.5%) | |
Values are expressed as medians (25th percentile–75th percentile) or the absolute and relative frequency. &Follow-up time: time frame between the first patient`s medical examination and EF removal or end of the study
Risk factors for developing superficial and deep infection associated with EF pins
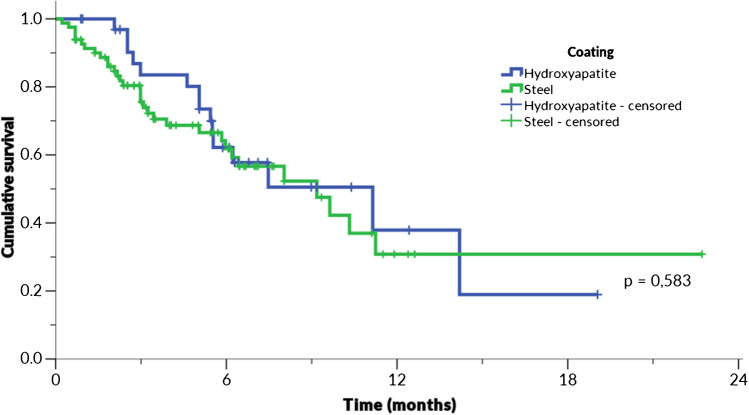
In the bivariate analysis, tibial pseudoarthrosis and femur osteomyelitis were statistically associated with higher rates of pin-track infection in the study patients. On the other hand, treatment of tibial and/or fibular fractures with any type of EF pins resulted in fewer rates of infection (36.2% vs. 19%, p = 0.028) (Table 3). Furthermore, no statistically significant association between the presence or absence of HA coating and the occurrence of infection was observed in the follow-up period (OR 1.70 [95% CI 0.71–4.01]), even when adjusted for the follow-up time (OR 1.71 [95% CI 0.70–4.22]) and for the presence of the underlying medical conditions (OR 1.79 [95% CI 0.75–4.29]). As shown in Fig. 1, there was no statistically significant difference between grade 2 or 3 infection-free survival between patients who received HA-coated or non-coated pins, with a median infection-free survival of 340 vs. 280 days, respectively (p = 0.583).
Table 3.
Variables potentially associated with the incidence of pin-track infection in the bivariate analysis (n = 132)
| Variable | Infection* | p | |
|---|---|---|---|
| No (n=69) | Yes (n=63) | ||
| Demography | |||
| Age (years) | 36.5 ± 18.7 | 37.4 ± 19.3 | 0.775 |
| Male sex | 49 (71.0%) | 45 (71.4%) | 0.958 |
| Comorbidities | |||
| Smoking | 9 (13.0%) | 8 (12.7%) | 0.953 |
| SAH | 7 (10.1%) | 6 (9.5%) | 0.905 |
| DM | 4 (5.8%) | 6 (9.5%) | 0.518 |
| Underlying medical condition | |||
| Pseudoarthrosis of the femur | 8 (11.6%) | 4 (6.3%) | 0.295 |
| Pseudoarthrosis of the tibia | 11 (15.9%) | 21 (33.3%) | 0.020 |
| Pseudoarthrosis of the humerus | 1 (1.4%) | 1 (1.6%) | 1.000 |
| Femur fracture | 2 (2.9%) | 3 (4.8%) | 0.669 |
| Tibia/fibula fracture | 25 (36.2%) | 12 (19.0%) | 0.028 |
| Femoral malunion | 2 (2.9%) | 2 (3.2%) | 1.000 |
| Tibial/fibular malunion | 8 (11.6%) | 6 (9.5%) | 0.700 |
| Osteomyelitis of the femur | - - | 8 (12.7%) | 0.002 |
| Osteomyelitis of the tibia | 9 (13.0%) | 12 (19.0%) | 0.346 |
| Congenital deformity of the femur | 3 (4.3%) | 5 (7.9%) | 0.478 |
| Congenital tibial deformity | 8 (11.6%) | 2 (3.2%) | 0.100 |
| Arthrodesis of the knee | - - | 1 (1.6%) | 0.477 |
| Ankle arthrodesis | 4 (5.8%) | - - | 0.121 |
| Coating by hydroxyapatite | 19 (27.5%) | 16 (25.4%) | 0.781 |
*Score ≥ 2 in any evaluation during follow-up. SAH systemic arterial hypertension; DM diabetes mellitus
Values are expressed the mean ± standard deviation or absolute or relative frequency
Fig. 1.
Infection-free survival grade 2 or 3 (n = 116). p: probability value (log-rank). The censored patients were cases in which they already had EF infection in the first evaluation, or who ended the follow-up without infection
Discussion
As far as we are aware of, few prospective studies assessed the role of HA coating on pin-track infection rates of EF. Most of previous studies included a small sample size with a limited follow-up period [19–21]. Conversely, the present prospective study included a largest sample size, exposing patients with a wide variability of underlying medical conditions treated with EFs. Besides, the overall mean period of follow-up time was 187 days, and the definition of pin-track infection was based upon the validated Maz-Oxford-Nuffield pin infection grading system. Compared to uncoated stainless-steel pins, the HA-coating pins did not increased protection from infection, and infection-free survival was also not statistically significant between the two groups.
The concept of manipulating the interface pin-soft tissue-bone by coating of EF pins towards the improvement of fixation and reduction of infection is not new. Attempts to apply silver as a coating material due to its antimicrobial and bacteriostatic activity proved unsuccessful regarding infection control and authors observed an increase in serum silver levels in some patients who received silver pins [22]. Due to its well-proved osteoconductive and osteointegration properties and increased extraction torques, HA-coated pin has also been thought to indirect decrease soft tissue and bone infection and loosening pin rates. Likewise, HA has also been proved by in vitro studies to prevent biofilm formation mainly through an anti-adhesive property [23]. Extrapolation of HA anti-infective properties identified in pre-clinical study results to clinical studies have not proved successful.
The studies by Pieske published in 2010 and 2011 compare the infection rates between HA-coated pins with steel pins and titanium pins in wrist fractures. None showed a statistically significant difference in infection rates between the different groups [19, 20]. There have been few other older studies that compared infection rates between HA-coated and steel pins. In 2004, Pizá et al. conducted a randomized prospective clinical study comparing infection rates between HA-coated pins and steel pins. In total, 23 patients were evaluated in which 56 EFs were used, with a follow-up of 530 days. The infection rates between pins were evaluated using the Checketts–Otterburn classification and were similar, with 30.4% for HA pins and 30.7% for steel pins [15]. A systematic review published in 2010 with four included articles comparing infection rates between with HA-coated and uncoated pins found no evidence of protection against HA infection, suggesting the need for larger studies to draw better conclusions [14].
Other aspects that are likely to influence the higher rates of pin site infection are demographic and underlying chronic medical conditions that affects the skin and soft tissue immune system and wound healing capacity, such as age, diabetes (DM) and hypertension (SAH), vascular chronic insufficiency, and smoking habits. Notwithstanding, the correlation of age, DM, SAH, and smoking with pin-site infection rates were analyzed in this study, and none of them were significantly associated with higher rates of infection into the multiple regression analysis. On the other hand, a recently published systematic review investigated the likelihood of several host factors increasing pin site infection rates, and DM increased the risk for pin site infection [24]. In addition, the length of the treatment using the external fixator can lead to increased rates of pin site infection in previous publications, including the results of the present study [24, 25]. This might explain the higher rates of pin site infection among patients treated with EF for pseudoarthrosis. Indeed, compared to uncoated pins, HA-coated pins remained in place for a longer period of time (207 vs. 174 days). We also emphasize that pins in the proximal femur, where the soft tissue is larger and constantly damaged by pins movements, often get infected.
An in vitro study compared biofilm formation on the surface of HA-coated titanium, stainless steel and Kirschner wires, in which the HA implant was more resistance to biofilm attachment [23, 26]. This study was not clinically assessed according to a recently published meta-analysis. Indeed, our group carried out a systematic review with meta-analysis of studies over the past 20 years evaluating the clinical benefits of pins manufactured from varied materials and coating systems and their possible role in pin track infection reduction rates. Seven studies were included which compared HA-coated and uncoated stainless-steel, titanium, and silver pins. The definition applied for pin track infection was arbitrary and not standardized among studies. Meta-analyses were carried out, comparing stainless steel vs. silver pins, stainless steel vs. HA-coated pins, and titanium vs. HA-coated pins. None of this analysis resulted in statistically significant differences in pin track infection rates [27].
The present study has limitations to be addressed. First, this is a prospective multicenter design study, but it was carried out without randomization due to technical issues that we had to deal with during the COVID-19 lockdown period. The study took place at two different teaching hospitals located in a medium-size city in the south of Brazil offering specialized orthopedic care. Consequently, the results obtained at our hospitals may not apply to others. Second, even though a sample size calculation was previously performed, and the rate of pin track infection was almost 50% for both groups, larger number of patients would have added supplementary information among the subgroup of patients that needed longer than six months of EF. Third, we did not take the number of individual infected pins into account. Pin track infection was considered irrespective of the number of affected pin sites, and differentiation between a single or multiple pin infected sites was not carried out. Comparing the rates of infection per patient rather than per pin site may have biased our results, as pin site more accurately depicts the total number of infections. On the other hand, EF infection rates are also considered a strength as each time a pin in a patient become infected the patient’s other pins have to be censored as the patient is treated with local or systemic antibiotic.
Conclusion
In summary, we identify higher rates of mild to moderate (lower grades) pin track infection in the present study. Infection rates in stainless steel pin track did not statistically differed from the rates in HA-coated pins. This applies regardless of the medical condition being treated with the EF, the presence of comorbidities, or by length of EF time. Pseudoarthrosis of the tibia and osteomyelitis of the femur are associated with a higher probability of pin track infection during follow-up. Therefore, the results of the present study showed that HA coating may not affect the EF pin infection rates compared to standard steel pins, but larger, multicenter randomized clinical studies are still needed.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Stoffel C: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.; de Lima E: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; Salles MJ: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have read and approved the final manuscript.
Funding
This study is financed with resources from researchers and the public health system.
Data Availability
The datasets generated during and/or analysed the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Research Ethics Committee under protocol number 2,572,550 and registered at ClinicalTrials.gov with ID number 84939418.6.0000.5342 in 08/27/2018.
Consent to participate
The patients participated in the research voluntarily and signed an informed consent.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bliven EK, Greinwald M, Hackl S, Augat P. External fixation of the lower extremities: Biomechanical perspective and recent innovations. Injury. 2019;50(Suppl 1):S10–S17. doi: 10.1016/j.injury.2019.03.0412. [DOI] [PubMed] [Google Scholar]
- 2.Behrens F, Johnson WD, Koch TW, Kovacevic N. Bending stiffness of unilateral and bilateral fixator frames. Clin Orthop Relat Res. 1983;178:103–110. doi: 10.1097/00003086-198309000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Huiskes R, Chao EY, Crippen TE. Parametric analyses of pin-bone stresses in external fracture fixation devices. J Orthop Res. 1985;3(3):341–3494. doi: 10.1002/jor.1100030311. [DOI] [PubMed] [Google Scholar]
- 4.Moroni A, Vannini F, Mosca M, Giannini S. State of the art review: techniques to avoid pin loosening and infection in external fixation. J Orthop Trauma. 2002;16(3):189–195. doi: 10.1097/00005131-200203000-000095. [DOI] [PubMed] [Google Scholar]
- 5.Shirai T, Watanabe K, Matsubara H, Nomura I, Fujiwara H, Arai Y, et al. Prevention of pin track infection with iodine-supported titanium pins. J Orthop Sc. 2014;19:598–602. doi: 10.1007/s00776-014-0561-z. [DOI] [PubMed] [Google Scholar]
- 6.Yin P, Ji Q, Li T, Li J, Li Z, Liu J, et al. (2015) A systematic review and meta-analysis of Ilizarov methods in the treatment of infected nonunion of tibia and femur. PLoS ONE 10(11). 10.1371/journal.pone.0141973 [DOI] [PMC free article] [PubMed]
- 7.Ring D, Bruinsma WE, Jupiter JB. Complications of hinged external fixation compared with cross-pinning of the elbow for acute and subacute instability. Clin Orthop Relat Res. 2014;472:2044–2048. doi: 10.1007/s11999-014-3510-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jauregui JJ, Bor N, Thakral R, Standard SC, Paley D, Herzenberg JE. Life and limb-threatening infections following the use of an external fixator. Bone Joint J. 2015;97:1296–1300. doi: 10.1302/0301-620X.97B9.35626. [DOI] [PubMed] [Google Scholar]
- 9.Checketts RG, MacEachern AG, Otterburn M (2000) Pin track infection and the principles of pin site care. In: Orthofix external fixation in trauma and orthopedics. London: Springer 97–102.
- 10.MON (Maz Oxford Nuffield) Pin Infection Grading System © [internet]. Available from: https://www.ouh.nhs.uk/limbreconstruction/information/documents/pin-infection-grading-system.pdf. Acessed July 25, 2022.
- 11.Parameswaran AD, Roberts CS, Seligson D, Voor M. Pin track infection with contemporary external fixation: how much of a problem? J Orthop Trauma. 2003;17:503–507. doi: 10.1097/00005131-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Jennison T, McNally M, Pandit H. Prevention of infection in external fixator pin sites. Acta Biomater. 2014;10:595–603. doi: 10.1016/j.actbio.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Britten S, Ghoz A, Duffield B, Giannoudis PV. Ilizarov fixator pin site care: the role of crusts in the prevention of infection. Injury. 2013;44(10):1275–1278. doi: 10.1016/j.injury.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Saithna A. The influence of hydroxyapatite coating of external fixator pins on pin loosening and pin track infection: a systematic review. Injury. 2010;41(2):128–132. doi: 10.1016/j.injury.2009.01.00115. [DOI] [PubMed] [Google Scholar]
- 15.Pizà G, Caja VL, Gonzáles-Viejo MA, Navarro A. Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-track infection in leg lengthening for short stature. J Bone Joint Surg Br. 2004;86:892–7. doi: 10.1302/0301-620x.86b6.13875. [DOI] [PubMed] [Google Scholar]
- 16.Toksvig-Larsen S, Aspenberg P. Bisphosphonate-coated external fixation pins appear similar to hydroxyapatite-coated pins in the tibial metaphysis and to uncoated pins in the shaft. Acta Orthop. 2013;84:314–8. doi: 10.3109/17453674.2013.797315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakamura H, Matsuno T, Hashimoto Y, Nakamura T, Mataga I. Comparison of a hydroxyapatite-coated and an anodic oxidized titanium implant for experimentally induced peri-implantitis: macroscopic and novel radiographic evaluations in a canine model. J Hard Tissue Biol. 2015;24:347–55. doi: 10.2485/jhtb.24.347. [DOI] [Google Scholar]
- 18.LeGeros RZ. Properties of osteoconductive biomaterials: calcium phosphates. Clin Orthop Relat Res. 2002;395:81–98. doi: 10.1097/00003086-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Pieske O, Kaltenhauser F, Pichlmaier L, Schramm N, Trentzsch H, Löffler T, et al. Clinical benefit of hydroxyapatite-coated pins compared with stainless steel in external fixation at the wrist: a randomized prospective study. Injury. 2010;41:1031–1036. doi: 10.1016/j.injury.2010.03.030. [DOI] [PubMed] [Google Scholar]
- 20.Pieske O, Pichlmaier L, Kaltenhauser F, Schramm N, Rubenbauer B, Greiner A, et al. Hydroxyapatite-coated pins vs titanium alloy pins in external fixation at the wrist: a controlled cohort study. J Trauma. 2011;70:845–851. doi: 10.1097/TA.0b013e3181e97761. [DOI] [PubMed] [Google Scholar]
- 21.Pommer A, Muhr G, Dávid A. Hydroxyapatite-coated Schanz pins in external fixators used for distraction osteogenesis: a randomized, controlled trial. J Bone Joint Surg Am. 2002;84:1162–1166. doi: 10.2106/00004623-200207000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Massè A, Bruno A, Bosetti M, Biasibetti A, Cannas M, Gallinaro P. Prevention of pin track infection in external fixation with silver coated pins: clinical and microbiological results. J Biomed Mater Res. 2000;53:600–604. doi: 10.1002/1097-4636(200009)53:5<600::aid-jbm21>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 23.Meyer F, Enax J. Hydroxyapatite in oral biofilm management. Eur. J. Dent. 2019;13:287. doi: 10.1055/s-0039-1695657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iobst CA, Liu RW. A systematic review of incidence of pin track infections associated with external fixation. J Limb Lengthen Reconstr. 2016;2:6–16. doi: 10.4103/2455-3719.182570. [DOI] [Google Scholar]
- 25.Fridberg M, Bue M, Rölfing JD. Kold S (2022) Host factors and risk of pin site infection in external fixation: a systematic review examining age, body mass index, smoking, and comorbidities including diabetes. J Limb Lengthen Reconstr. 2022;8:S3–15. doi: 10.4103/jllr.jllr_32_21. [DOI] [Google Scholar]
- 26.Goodman SB, Yao Z, Keeney M, Yang F. The future of biologic coatings for orthopedic implants. Biomaterial. 2013;34(13):3174–3183. doi: 10.1016/j.biomaterials.2013.01.07425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stoffel C, Eltz B, Salles MJ. Role of coatings and materials of external fixation pins on the rates of pin track infection: a systematic review and meta-analysis. World J Orthop. 2021;12(11):920–930. doi: 10.5312/wjo.v12.i11.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed the current study are available from the corresponding author on reasonable request.