Abstract
Characterization of the oropharynx, a subdivision of the pharynx between the soft palate and the epiglottis, is limited to simple measurements. Structural changes in the oropharynx in whiplash‐associated disorder (WAD) cohorts have been quantified using two‐dimensional (2D) and three‐dimensional (3D) measures but the results are inconsistent. Statistical shape modelling (SSM) may be a more useful tool for systematically comparing morphometric features between cohorts. This technique has been used to quantify the variability in boney and soft tissue structures, but has not been used to examine a hollow cavity such as the oropharynx. The primary aim of this project was to examine the utility of SSM for comparing the oropharynx between WAD cohorts and control; and WAD severity cohorts. The secondary aim was to determine whether shape is associated with sex, height, weight and neck length. Magnetic resonance (MR) T1‐weighted images were obtained from healthy control (n = 20), acute WAD (n = 14) and chronic WAD (n = 14) participants aged 18–39 years. Demographic, WAD severity (neck disability index) and body morphometry data were collected from each participant. Manual segmentation of the oropharynx was undertaken by blinded researchers between the top of the soft palate and tip of the epiglottis. Digital 3D oropharynx models were constructed from the segmented images and principal component (PC) analysis was performed with the PC weights normalized to z‐scores for consistency. Statistical analyses were undertaken using multivariate linear models. In the first statistical model the independent variable was group (acute WAD, chronic WAD, control); and in the second model the independent variable was WAD severity (recovered/mild, moderate/severe). The covariates for both models included height, weight, average neck length and sex. Shape models were constructed to visualize the effect of perturbing these covariates for each relevant mode. The shape model revealed five modes which explained 90% of the variance: mode 1 explained 59% of the variance and primarily described differences in isometric size of the oropharynx, including elongation; mode 2 (13%) primarily described lateral (width) and AP (depth) dimensions; mode 3 (8%) described retroglossal AP dimension; mode 4 (6%) described lateral dimensions at the retropalatal‐retroglossal junction and mode 5 (4%) described the lateral dimension at the inferior retroglossal region. There was no difference in shape (mode 1 p = 0.52; mode 2 p = 0.96; mode 3 p = 0.07; mode 4 p = 0.54; mode 5 p = 0.74) between control, acute WAD and chronic WAD groups. There were no statistical differences for any mode (mode 1 p = 0.12; mode 2 p = 0.29; mode 3 p = 0.56; mode 4 p = 0.99; mode 5 p = 0.96) between recovered/mild and moderate/severe WAD. Sex was not significant in any of the models but for mode 1 there was a significant association with height (p = 0.007), mode 2 neck length (p = 0.044) and in mode 3 weight (p = 0.027). Although SSM did not detect differences between WAD cohorts, it did detect associations with body morphology indicating that it may be a useful tool for examining differences in the oropharynx.
Keywords: Human, oropharynx, statistical shape modelling, whiplash‐associated disorder
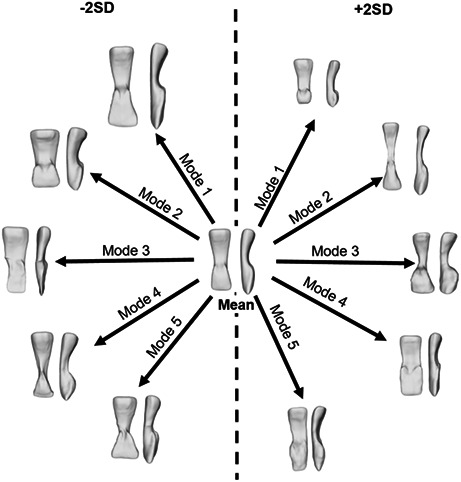
Visual summary of the shape variation described by each of the modes of the oropharynx model: Mode 1 described variance in isometric size including elongation; mode 2 width and depth; mode 3 retroglossal antero‐posterior dimension; mode 4 lateral dimensions at the retropalatal and retroglossal junction and mode 5 the lateral dimension at the inferior retroglossal region. Each mode is shown at the limits of ‐2SD and + 2SD from the mean shape.
1. INTRODUCTION
The oropharynx is a subdivision of the pharynx between the soft palate and the epiglottis. It is bounded by the soft palate and tongue anteriorly and the muscles of the pharyngeal wall posteriorly. The oropharyngeal cavity is a common pathway for food to the oesophagus and air to the lungs. The function of the oropharynx can be affected by structural changes including narrowing antero‐posteriorly and laterally as well as elongation resulting in decreased volume (Passos et al., 2019; Whyte & Gibson, 2020). However, thus far characterization of the oropharynx has been limited to simple measurements and not the analysis of shape.
In whiplash‐associated disorder (WAD), it has been suggested that oropharyngeal size is reduced and these morphometric changes may be responsible for swallowing‐related problems (Elliott et al., 2008; Elliott et al., 2012; Stone et al., 2021b). Further, one study has determined that the severity of symptoms following whiplash are related to oropharyngeal size (Elliott et al., 2012). These findings have been made using 2D MRI measurements at nominal vertebral sites, or 3D measurements of volume which were not replicated in a follow‐up study (Stone et al., 2020; Stone et al., 2021a).
Structural changes in the oropharynx in WAD have been quantified using 2D and 3D magnetic resonance image (MRI) measurements of cross‐sectional area, anteroposterior (AP) and lateral dimensions and volume (Elliott et al., 2008, 2012; Stone et al., 2020). 2D measures are intrinsically limited resulting in a wide variation of reported single‐level CSA measures (Welch et al., 2002). 2D measures are affected by the alignment of the oropharynx within the axial plane (Aboudara et al., 2009; Guijarro‐Martinez & Swennen, 2011; Welch et al., 2002) and the cervical spine or soft tissue level used as the reference point (Guijarro‐Martinez & Swennen, 2011). 3D measurements of the oropharynx identify volumetric status but do not enable the identification of where the underlying changes or differences have occurred. For example, the location of any narrowing and whether it is consistent within a cohort compared to another. 3D models of the oropharynx have been constructed in control and patient groups (Chen et al., 2018; Garcia‐Usó et al., 2021; Zheng et al., 2014), but shape has not been used to describe the oropharynx or identify differences between cohorts.
Statistical shape modelling (SSM) is emerging as a useful tool for systematically comparing morphometric features and determining whether there are systematic differences between cohorts. Shapes are decomposed into modes which describe the main ways in which the shape varies across the population (Cootes et al., 1992; Dryden & Mardia, 1998). By understanding the way shapes vary and whether separate cohorts vary differently, subtle changes can be uncovered. This technique has been used to quantify the variability in boney and soft tissue structures such as the lumbar spine, hip, knee, ankle, orbit, ossicles and levator ani (Bartling et al., 2021; Gass et al., 2022; Pavlova et al., 2017; Vafaeian et al., 2022; Vrancken et al., 2014). However, SSM has not been used to examine a hollow cavity such as the oropharynx in vivo.
Because SSM can be used to differentiate between cohorts, it may prove to be a useful tool for examining the oropharynx after whiplash and other pathologies such as obstructive sleep apnoea (OSA) (Rodrigues et al., 2017). The primary aim of this study was to examine the utility of SSM for comparing the oropharynx between cohorts. Specifically, whether SSMs can differentiate between acute and chronic WAD and control cohorts; and WAD severity based on neck disability index (NDI) score. The secondary aim was to determine whether shape is associated with sex or body morphometry, specifically height, weight and neck length.
2. METHODS
The institutional human research ethics (HREC) committees (ACT Health HREC protocol number ETH.11.12.285; ANU HREC protocol number 2013/015) approved the study. All participants provided written informed consent. The data analysed in this study come from a larger WAD imaging study.
2.1. Participants
Participants aged 18–39 years were prospectively recruited to the study during 2014–19. The inclusion criteria included no known cervical spine disease or surgery and no contraindications for MR scanning. These data were achieved using a participant screening form which included questions about their medical history. Non‐WAD control participants, without history of neck pain or previous MVT, were recruited from the community via flyers and word of mouth. Acute WAD participants (<3 weeks since MVT) were recruited from the admissions database of an Australian tertiary hospital's Emergency Department; and chronic WAD participants (12 weeks–3 years since MVT) (Sterling, 2014) were recruited from the community. All were classified as Quebec Task Force classification WAD II (defined as having neck pain and neck stiffness, reduced neck movement or tenderness in the neck region) (Spitzer et al., 1995) after motor vehicle trauma (MVT) (Sterling, 2014).
2.2. Data collection
Demographic, MVT history and health data were collected from each participant using a questionnaire administered by the research team (AW, DP). WAD severity was measured using the NDI (Vernon & Mior, 1991) and previously published thresholds were used to group the WAD participants as either recovered/mild (0–28% NDI) or moderate/severe (>28% NDI) (Elliott et al., 2012). Standing height was measured using a stadiometer and body mass using a mechanical scale to calculate BMI (body mass [kg]/height squared [m2]). Neck length was measured with the subject seated, using a flexible non‐stretch measurement tape (Webb et al., 2011). Neck length was calculated from the average of the anterior (gnathion to the suprasternal notch) and posterior (inion to the tip of the C7 spinous process) neck lengths. All measurements were repeated three times and an average value calculated.
2.3. MRI protocol
Participants were positioned supine in a 3‐Tesla Skyra scanner (Siemens, Erlangen, Germany) with a head and neck coil and the head positioned on a rest with foam pads laterally to minimize motion during scanning. Each participant was instructed to remain awake and alert with regular breathing. MR images, from the occiput to T1 level, were attained using an axial T1‐weighted spin echo (15 ms echo time, 827 ms repetition time, 45 slices, 4 mm slice thickness, no inter‐slice gap) sequence. The axial slices were positioned parallel to the C2/3 intervertebral disc. Phase oversampling was employed to reduce the wrap‐around effect. All imaging was conducted at the same facility on the same machine by qualified radiographers.
2.4. Oropharynx segmentation and morphometry measurements
The border of the oropharynx lumen was manually segmented on each axial MR image using a Matlab (Mathworks VR) graphical user interface (Al Suman et al., 2019) specifically designed for this purpose. Anteriorly, the soft palate and tongue and posteriorly the pharyngeal muscles were used to define the borders of the oropharynx. The segmentations were performed from the top of the soft palate superiorly to the tip of the epiglottis inferiorly (Welch et al., 2002, Alves Jr. et al., 2012, Ma et al., 2016, Standring, 2016, Martins et al., 2018, Alkhader & Geijer, 2019). Digital 3D models were constructed from the segmented images. The researcher (AW) undertaking the segmentation was blind to the clinical presentation of each participant.
Ten subjects were randomly selected for the determination of intra‐observer reliability (measurements made on two different occasions 2 weeks apart by the same observer) and inter‐observer reliability (measurements made on the same day by a second observer) trained and blinded to the results of the first observer. Based on 89 axial segmentations, the reliability of this method was determined to be excellent (intra‐rater ICC = 0.98; inter‐rater ICC2,1 = 0.90).
Statistical shape modelling (SSM) was used to characterize the oropharynx shape. SSM is a machine learning technique which uses principal component analysis (PCA) to investigate and compare the variations within geometries of very complex structures. The technique used for this analysis was based on a previously developed technique (Zhang et al., 2014). First, a template mesh, based on a single mesh from one oropharynx in the dataset, was created using a series of radial basis functions to parameterize each oropharynx (Zhang et al., 2018). This template was iteratively fit with a series of coarse to fine fits to all meshes in the dataset, which resulted in maximum correspondence between meshes. Next, corresponding meshes were rigidly aligned, using a Procrustes analysis, allowing for both the shape and size variability to be included in the model (Zhang et al., 2014). Finally, a PCA was run on the nodal coordinates of the aligned meshes to create a shape model. PCA allows for any shape in the dataset to be approximated as the sum of the mean shape plus the weighted sum of the principal components (PC) (Heimann & Meinzer, 2009).
The fitting process was then repeated using the mean shape as the template. Following this, the fitting process was further refined for individual shape differences by incorporating PCA fitting using the previous SSM generated from the dataset. A final PCA was performed on the nodal coordinates to generate an SSM which determined the principal component weights used in the subsequent analysis. One model was created which contained acute, chronic and control oropharynx shapes. The principal components, or modes, which accounted for 90% of accumulated variance were retained. The PCA was performed to create shape models which generated PCs accounting for 90% of the cumulative variance and their subsequent weights. All PC weights were then normalized to z‐scores for consistency and used in further analyses (Lynch et al., 2019). The z‐scores were developed post‐hoc using SPSS statistical package, version 25 (IBM Inc.).
2.5. Statistical analysis
Multivariate linear models were performed for analyses. The dependent variables were z‐scores for each mode (principal components 1–5). In the first model, the independent variable was WAD group (acute, chronic) and control. The covariates included height (cm), weight (kg), average neck length (cm) and sex. In the second model, the independent variable was WAD severity group determined by NDI score of the acute and chronic WAD participants (recovered/mild, moderate/severe). The covariates were the same as the first model. Shape models were constructed to visualize the effect of perturbing these variables for each relevant mode. All models were assessed for linearity using Q‐Q plots of the residuals. All statistical analyses were performed using SPSS statistical package, version 25 (IBM Inc.).
3. RESULTS
Demographic and clinical characteristics for the 48 participants, by control and WAD groups, are shown in Table 1.
TABLE 1.
Demographics presented as counts or mean (SD) for control, acute WAD (<3 weeks since MVT) and chronic WAD (12 weeks‐3 years since MVT); and recovered/mild (0–28% NDI) and moderate/severe (>28% NDI) for WAD participants
| WAD Groups | NDI Groups (no control) | ||||
|---|---|---|---|---|---|
| Control (n = 20) | Chronic WAD (n = 14) | Acute WAD (n = 14) | Recovered/mild WAD (n = 12) | Moderate/severe WAD (n = 16) | |
| Age (years) | 27 (3) | 27 (4) | 26 (7) | 27 (6) | 27 (5) |
| Sex (M/F) | 9:11 | 3:11 | 3:11 | 4:8 | 2:14 |
| Height (cm) | 175 (11) | 171 (11) | 167 (8) | 171 (13) | 167 (7) |
| Mass (kg) | 69 (14) | 77 (19) | 68 (14) | 74 (22) | 71 (12) |
| BMI (kg/m2) | 23 (3) | 27 (5) | 24 (5) | 25 (6) | 25 (5) |
| Neck length (cm) | 15 (2) | 15 (2) | 14 (1) | 15 (2) | 14 (2) |
| Days since MVT | NA | 334 (284) | 8 (5) | 33 (40) | 19 (28) |
| Acute:Chronic | NA | NA | NA | 6:6 | 8:8 |
| NDI (%) | 2 (3) | 33 (17) | 29 (16) | 16 (8) | 45 (10) |
Abbreviations: BMI, body mass index; MVT, motor vehicle trauma; NDI, neck disability index; WAD, whiplash‐associated disorder.
The 3D models of the air‐filled space of the oropharynx demonstrated an ‘hourglass’ shape in the anterior view and a ‘telephone handset’ shape in the lateral view concave anteriorly in the midsection (Figures 1 and 2). The surrounding structures describing this shape are shown in Figure 3.
FIGURE 1.
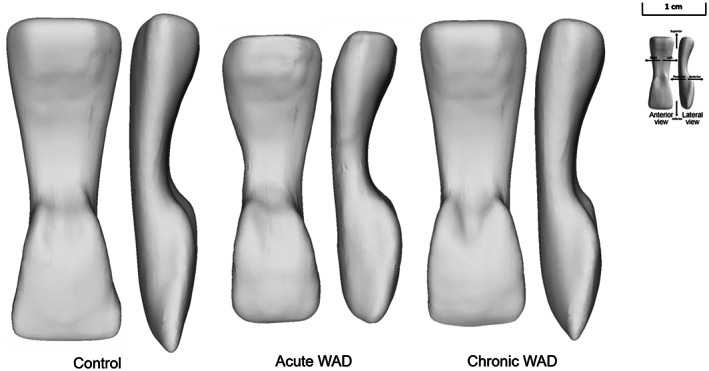
Mean oropharynx shape models (anterior view [left model] and lateral view [right model]) for the healthy control (n = 20) and the acute (n = 14) and chronic (n = 14) whiplash‐associated disorder (WAD) groups
FIGURE 2.
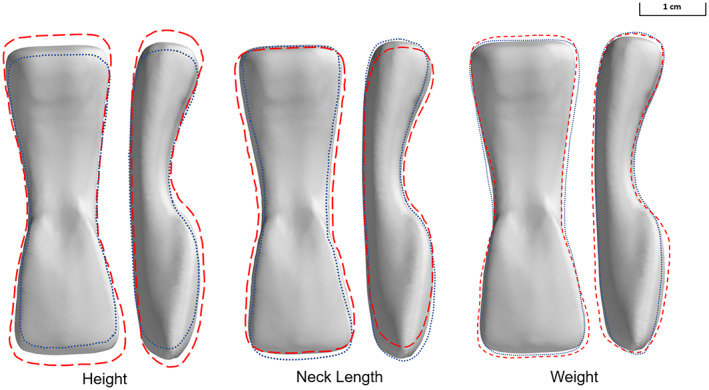
Representation of mean oropharyngeal shape variation (anterior view [left model] and lateral view [right model]) as a function of height (−10 cm represented by the dotted blue line and +10 cm by the dashed red line), neck length (−2 cm represented by the dotted blue line and +2 cm by the dashed red line) and weight (−20 kg represented by the dotted blue line and +20 kg by the dashed red line)
FIGURE 3.
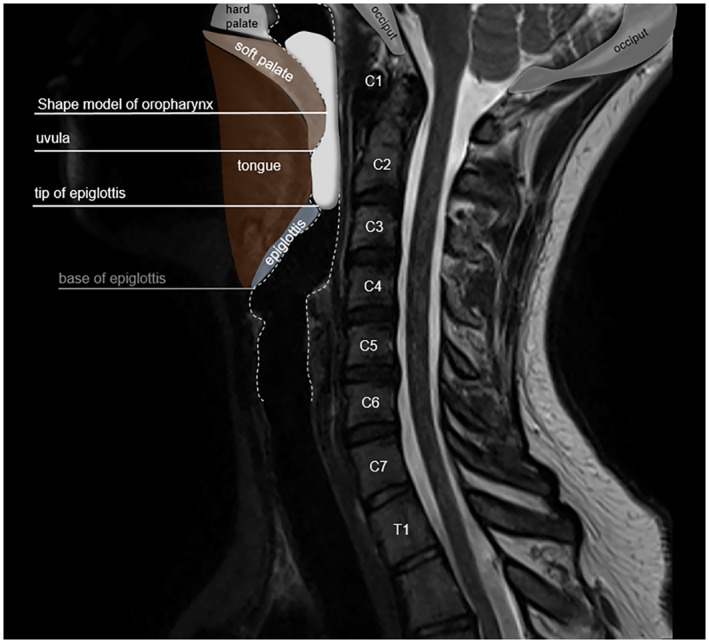
Oropharynx shape model in the context of a T2‐weighted sagittal MRI image. The oropharynx is defined superiorly by the top of the soft palate and inferiorly by the tip of the epiglottis and subdivided into the retropalatal and retroglossal regions posterior to the soft palate and tongue, respectively
The shape model revealed five modes which explained 90% of the variance (Figure 4). Mode 1 explained most of the variance (59%). Mode 1 represented the isometric size component, however, it also demonstrated variance in elongation of the oropharynx (Figure 5) notably retroglossally, with greater elongation at −2SD compared to +2SD. Mode 2 explained 13% of the variance. Mode 2 primarily described the relative lateral (width) and AP (depth) dimensions (Figure 5) with the dimensions at +2SD being much narrower, most notably retropalatally. Mode 3 explained 8% of the variance. Mode 3 primarily described the relative AP dimension of the retroglossal region with −2SD being much narrower (Figure 5). Mode 4 explained 6% of the variance. Mode 4 primarily described the relative lateral dimensions at the junction between the retropalatal and retroglossal regions (Figure 5) with the dimensions at −2SD being much narrower compared to +2SD. Mode 5 explained 4% of the variance. Mode 5 described the relatively larger lateral dimension at the inferior retroglossal region where it borders the epiglottis (Figure 5).
FIGURE 4.
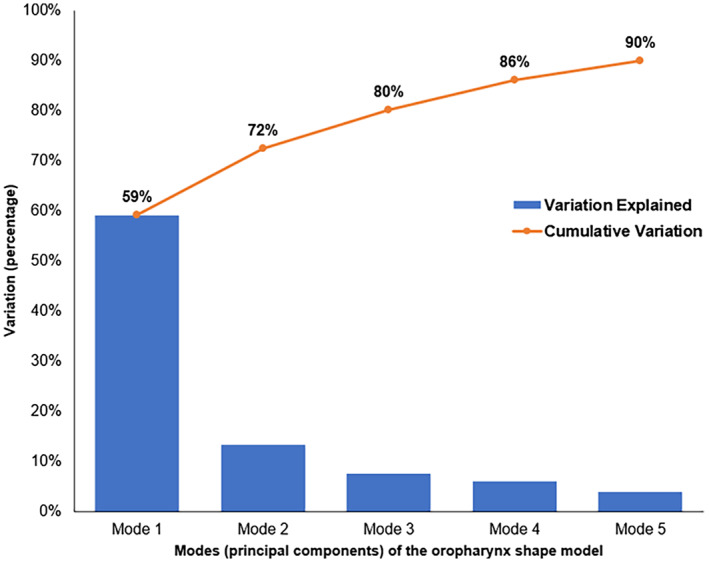
The contributions of modes 1 to 5 that accounted for 90% of the variance of the oropharynx shape model
FIGURE 5.
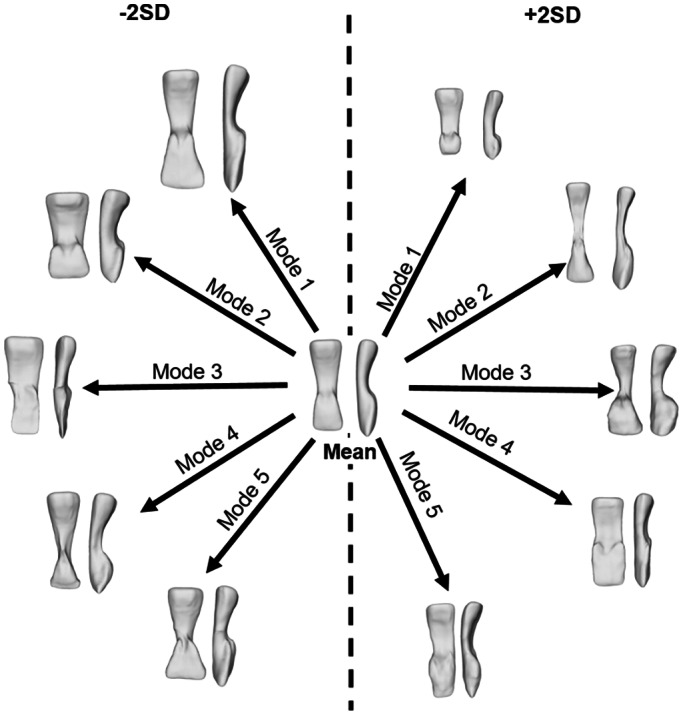
Visual summary of the shape variation described by each of the modes of the oropharynx model (anterior view [left model] and lateral view [right model]) for all participants (n = 48). Each mode is shown at the limits of minus 2 standard deviations (−2SD) from the mean shape and plus 2 standard deviations (+2SD). Mode 1 described variance in isometric size including elongation; mode 2 width and depth; mode 3 retroglossal antero‐posterior dimension; mode 4 lateral dimensions at the retropalatal and retroglossal junction and mode 5 the lateral dimension at the inferior retroglossal region
There was no difference in shape between control, acute WAD and chronic WAD groups (mode 1 p = 0.52; mode 2 p = 0.96; mode 3 p = 0.07; mode 4 p = 0.54; mode 5 p = 0.74) (Figure 1). When the acute and chronic WAD participants were grouped according to their NDI score (recovered/mild = 0–28% NDI; moderate/severe = >28% NDI) there were no statistical differences between groups for any mode (mode 1 p = 0.12; mode 2 p = 0.29; mode 3 p = 0.56; mode 4 p = 0.99; mode 5 p = 0.96).
Body morphometry and sex were interrogated in the first model only (n = 48). Sex was not significant in any of the modes. In mode 1, height (mean 170.5 cm) was significant (p = 0.007); for every increase of 1 cm in height the z‐score decreased by 0.042. This is illustrated in Figure 2 which shows the mode 1 shape differences for ±10 cm in height. For mode 2, neck length (mean 14.5 cm) was significant (p = 0.044); for every increase of 1 cm in neck length the z‐score decreased by 0.173. This is illustrated in Figure 2 which shows the mode 2 shape differences for ±2 cm in neck length. In mode 3 weight, was the most important variable in the model. Weight (mean 70.5 kg) was significant (p = 0.027) for every increase of 1 kg in weight the z‐score increased by 0.023. This is illustrated in Figure 2 which shows the mode 3 shape differences for ±20 kg. Morphological variables were not important in modes 4 and 5.
4. DISCUSSION
This study examined the utility of SSM for comparing the shape of the oropharynx between cohorts. There were no differences in shape between acute WAD, chronic WAD and control groups. Similarly, there was no difference between WAD participants grouped by NDI severity. However, there were associations between oropharynx shape and morphological factors including height, neck length and weight.
In this study, we found no association between oropharynx shape and WAD. Previous studies have observed differences in oropharynx CSA at the C1‐2 level between cohorts of chronic WAD and control (Elliott et al., 2008), and also differences between recovered and non‐recovered WAD based on NDI (Elliott et al., 2012). This evidence was used to postulate that swallowing difficulties after whiplash may be due to changes in the shape of the oropharynx. However, more recent studies which have compared volume between cohorts have not detected the same differences (Stone et al., 2020; Stone et al., 2021a). In this study, we specifically examined shape parameters as opposed to simple dimensional data, and found no association between oropharynx shape and WAD. Nor was there any impact of WAD severity status based on NDI score.
Our models revealed an association between body morphometry and oropharyngeal shape. Increased height was associated with an elongated oropharynx. Increased neck length was associated with a narrower oropharynx. Increased weight was associated with an increased A‐P diameter, especially in the retroglossal region (Figures 3 and 5). There have been no previous reports of height being associated with oropharynx elongation, nor of increased neck length being associated with a narrower oropharynx. However, there have been reports of weight being associated with tongue size and diminished oropharynx airway dimensions. A previous laryngoscopy study detected that reduced oropharyngeal size, especially at the base of the tongue, was related to obesity (Voyagis et al., 1998). This relationship between the size of the tongue and obesity was verified by Kim et al. (2014) who reported enlarged tongue volume and increased fat within the tongue of obese apneics; and more recently by Wang et al. (2020) who demonstrated that weight loss decreases tongue fat in patients with sleep apnoea. In contrast, we found that increased weight was associated with an increase in AP dimension, especially in the retroglossal region. This is not consistent with either Wang et al. (2020) or Kim et al. (2014) possibly because our cohorts were less obese (mean BMI 23–27 (SD 3–5); Wang et al., 2020 42.6 (8.5); Kim et al., 2014 39 (8.3)). This finding is interesting and requires more investigation. In this study, we modelled height and weight separately rather than BMI which may explain the difference, but it is possible that the relationship between obesity and oropharynx size is not linear.
The literature indicates that males generally have a larger oropharynx than females (Brooks & Strohl, 1992; Inamoto et al., 2015; Mohsenin, 2001; Shigeta et al., 2008), however, some studies report no difference (Daniel et al., 2007). In agreement with Daniel et al. (2007), none of our models detected any difference in shape due to sex unlike Shigeta et al. (2008), who found that sex predicted oropharynx length after normalizing for body height. However, their male‐to‐female ratio was equal, whereas our WAD cohort had twice as many females than males. The strongest predictor of oropharynx elongation in our participants was height, indicating that previous findings of sex differences may have been due to the height of the participants.
This study needs to be considered in the light of the methodological limitations. First, although all participants were imaged awake in supine with their heads resting on a standard neck rest and an instruction to breathe normally, we did not control factors such as tongue position and nasal/oral breathing. Because the oropharynx is a dynamic space, the shape could have been systematically affected by these factors (Hsu et al., 2021; Inamoto et al., 2015; Passos et al., 2019; Stone et al., 2020). Therefore, further research should attempt to use detailed standardized protocols. The sample size was not large and therefore may have failed to detect differences in our cohorts where differences did exist. Power analyses for CSA in a previous study (Webb, A.L., Lo, L., Pickering, M., & Perriman, D.M., unpublished data) determined that 11 participants in each group were required to detect a difference and so the numbers presented here should theoretically be sufficient. However, in this case, shape was the outcome and we did not have data to determine an a priori sample size. Therefore, it is recommended that further studies using the same methodology be undertaken with larger samples, as well as patient groups with different oropharyngeal disorders such as obstructive sleep apnoea, to further explore the utility of SSM in differentiating between cohorts.
5. CONCLUSIONS
Although SSM did not detect differences between our WAD or NDI‐based severity groups, it did detect associations between shape and morphological differences. This finding supports the use of SSM for the oropharynx but issues such as standardization of imaging protocols need to be established.
AUTHOR CONTRIBUTIONS
The study was conceived by DP and AW. All authors contributed in part to data collection and analysis: participant recruitment and data collection (DP, AW); oropharynx segmentation (AW); model development (JL, MP); data analysis (DP, JL); data interpretation (DP, JL, AW). DP and AW drafted the manuscript and all authors contributed critical input and feedback on multiple versions of the manuscript.
ACKNOWLEDGMENTS
This research was supported by the Royal Australian and New Zealand College of Radiologists Research Grant and Canberra Health Services Private Practice Trust Fund Grant. Open access publishing facilitated by Australian National University, as part of the Wiley ‐ Australian National University agreement via the Council of Australian University Librarians.
[Correction added on 28 November 2022, after first online publication: CAUL funding statement has been added.]
Webb, A.L. , Lynch, J.T. , Pickering, M.R. & Perriman, D.M. (2023) Shape modelling of the oropharynx distinguishes associations with body morphology but not whiplash‐associated disorder. Journal of Anatomy, 242, 535–543. Available from: 10.1111/joa.13783
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Aboudara, C. , Nielsen, I. , Huang, J.C. , Maki, K. , Miller, A.J. & Hatcher, D. (2009) Comparison of airway space with conventional lateral headfilms and 3‐dimensional reconstruction from cone‐beam computed tomography. American Journal of Orthodontics and Dentofacial Orthopedics, 135, 468–479. [DOI] [PubMed] [Google Scholar]
- Al Suman, A. , Aktar, N. , Asikuzzaman, M. , Webb, A.L. , Perriman, D.M. & Pickering, M.R. (2019) Segmentation and reconstruction of cervical muscles using knowledge‐based grouping adaptation and new step‐wise registration with discrete cosines. Computer Methods in Biomechanics and Biomedical Engineering: Imaging & Visualization, 7, 12–25. [Google Scholar]
- Alkhader, M. & Geijer, M. (2019) Comparative analysis of the oropharyngeal airway in patients aged over 40 years: A cone beam computed tomography study. European Journal of General Dentistry, 8, 76–79. [Google Scholar]
- Alves, M., Jr. , Baratieri, C. , Mattos, C.T. , Brunetto, D. , Fontes, R.C. , Santos, J.R.L. et al. (2012) Is the airway volume being correctly analyzed? American Journal of Orthodontics and Dentofacial Orthopedics, 141, 657–661. [DOI] [PubMed] [Google Scholar]
- Bartling, M.L. , Rohani, S.A. , Ladak, H.M. & Agrawal, S.K. (2021) Micro‐CT of the human ossicular chain: Statistical shape modeling and implications for otologic surgery. Journal of Anatomy, 239, 771–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, L.J. & Strohl, K.P. (1992) Size and mechanical properties of the pharynx in healthy men and women. The American Review of Respiratory Disease, 146, 1394–1397. [DOI] [PubMed] [Google Scholar]
- Chen, H. , van Eijnatten, M. , Aarab, G. , Forouzanfar, T. , de Lange, J. , van der Stelt, P. et al. (2018) Accuracy of MDCT and CBCT in three‐dimensional evaluation of the oropharynx morphology. European Journal of Orthodontics, 40, 58–64. [DOI] [PubMed] [Google Scholar]
- Cootes, T.F. , Taylor, C.J. , Cooper, D.H. & Graham, J. (1992) Training models of shape from sets of examples. In: Hogg, D. , Boyle, R. (Eds.) BMVC. London: Springer, pp. 9–18. [Google Scholar]
- Daniel, M.M. , Lorenzi, M.C. , da Costa, L.C. & Lorenzi‐Filho, G. (2007) Pharyngeal dimensions in healthy men and women. Clinics (São Paulo, Brazil), 62, 5–10. [DOI] [PubMed] [Google Scholar]
- Dryden, I.L. & Mardia, K.V. (1998) Statistical Shape Analysis. New York: John Wiley & Sons. [Google Scholar]
- Elliott, J. , Cannata, E. , Christensen, E. , DeMaris, J. , Kummrow, J. , Manning, E. et al. (2008) MRI analysis of the size and shape of the oropharynx in chronic whiplash. Otolaryngology and Head and Neck Surgery, 138, 747–751. [DOI] [PubMed] [Google Scholar]
- Elliott, J.M. , Pedler, A.R. , Theodoros, D. & Jull, G.A. (2012) Magnetic resonance imaging changes in the size and shape of the oropharynx following acute whiplash injury. The Journal of Orthopaedic and Sports Physical Therapy, 42, 912–918. [DOI] [PubMed] [Google Scholar]
- Garcia‐Usó, M. , Lima, T.F. , Trindade, I.E.K. , Pimenta, L.A.F. & Trindade‐Suedam, I.K. (2021) Three‐dimensional tomographic assessment of the upper airway using 2 different imaging software programs: A comparison study. American Journal of Orthodontics and Dentofacial Orthopedics, 159, 217–223. [DOI] [PubMed] [Google Scholar]
- Gass, M. , Fussinger, M.A. , Metzger, M.C. , Schwarz, S. , Bähr, J.D. , Brandenburg, L.S. et al. (2022) Virtual reconstruction of orbital floor defects using a statistical shape model. Journal of Anatomy, 240, 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guijarro‐Martinez, R. & Swennen, G.R. (2011) Cone‐beam computerized tomography imaging and analysis of the upper airway: A systematic review of the literature. International Journal of Oral and Maxillofacial Surgery, 40, 1227–1237. [DOI] [PubMed] [Google Scholar]
- Heimann, T. & Meinzer, H.P. (2009) Statistical shape models for 3D medical image segmentation: A review. Medical Image Analysis, 13, 543–563. [DOI] [PubMed] [Google Scholar]
- Hsu, Y.B. , Lan, M.Y. , Huang, Y.C. , Kao, M.C. & Lan, M.C. (2021) Association between breathing route, oxygen desaturation, and upper airway morphology. Laryngoscope, 131, E659–E664. [DOI] [PubMed] [Google Scholar]
- Inamoto, Y. , Saitoh, E. , Okada, S. , Kagaya, H. , Shibata, S. , Baba, M. et al. (2015) Anatomy of the larynx and pharynx: Effects of age, gender and height revealed by multidetector computed tomography. Journal of Oral Rehabilitation, 42, 670–677. [DOI] [PubMed] [Google Scholar]
- Kim, A.M. , Keenan, B.T. , Jackson, N. , Chan, E.L. , Staley, B. , Poptani, H. et al. (2014) Tongue fat and its relationship to obstructive sleep apnea. Sleep, 37, 1639–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, H. , Wang, C. , Zhang, H. , Xiong, H. , Li, Z. , Huang, X. et al. (2019) Threshold of the upper airway cross‐section for hypopnea onset during sleep and its identification under waking condition. Respiratory Research, 20, 280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch, J.T. , Schneider, M.T.Y. , Perriman, D.M. , Scarvell, J.M. , Pickering, M.R. , Asikuzzaman, M. et al. (2019) Statistical shape modelling reveals large and distinct subchondral bony differences in osteoarthritic knees. Journal of Biomechanics, 93, 177–184. [DOI] [PubMed] [Google Scholar]
- Ma, M.A. , Kumar, R. , Macey, P.M. , Yan‐Go, F.L. & Harper, R.M. (2016) Epiglottis cross‐sectional area and oropharyngeal airway length in male and female obstructive sleep apnea patients. Nature and Science of Sleep, 8, 297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins, L.S. , Liedke, G.S. , Heraldo, L. , Da Silveira, P.F. , Arus, N.A. , Ongkosuwito, E.M. et al. (2018) Airway volume analysis: Is there a correlation between two and three‐dimensions? European Journal of Orthodontics, 40, 262–267. [DOI] [PubMed] [Google Scholar]
- Mohsenin, V. (2001) Gender differences in the expression of sleep‐disordered breathing: Role of upper airway dimensions. Chest, 120, 1442–1447. [DOI] [PubMed] [Google Scholar]
- Passos, U.L. , Genta, P.R. , Marcondes, B.F. , Lorenzi‐Filho, G. & Gebrim, E. (2019) State‐dependent changes in the upper airway assessed by multidetector CT in healthy individuals and during obstructive events in patients with sleep apnea. Jornal Brasileiro de Pneumologia, 45, e20180264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlova, A.V. , Saunders, F.R. , Muthuri, S.G. , Gregory, J.S. , Barr, R.J. , Martin, K.R. et al. (2017) Statistical shape modelling of hip and lumbar spine morphology and their relationship in the MRC National Survey of Health and Development. Journal of Anatomy, 231, 248–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues, M.M. , Pereira Filho, V.A. , Gabrielli, M.F.R. , Oliveira, T.F.M. , Batatinha, J.A.P. & Passeri, L.A. (2017) Volumetric evaluation of pharyngeal segments in obstructive sleep apnea patients. Brazilian Journal of Otorhinolaryngology, 84, 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigeta, Y. , Ogawa, T. , Venturin, J. , Nguyen, M. , Clark, G.T. & Enciso, R. (2008) Gender‐ and age‐based differences in computerized tomographic measurements of the orophaynx. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 106, 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, W.O. , Skovron, M.L. , Salmi, L.R. , Cassidy, J.D. , Duranceau, J. , Suissa, S. et al. (1995) Scientific monograph of the quebec task force on whiplash‐associated disorders: Redefining “whiplash” and its management. Spine (Phila Pa 1976), 20, 1 S–73 S. [PubMed] [Google Scholar]
- Standring, S. (2016) Gray's Anatomy. The Anatomical Basis of Clinical Practice. Philadelphia, USA: Elsevier. [Google Scholar]
- Sterling, M. (2014) Physiotherapy management of whiplash‐associated disorders (WAD). Journal of Physiotherapy, 60, 5–12. [DOI] [PubMed] [Google Scholar]
- Stone, D. , Bogaardt, H. , Linnstaedt, S.D. , Martin‐Harris, B. , Smith, A.C. , Walton, D.M. et al. (2020) Whiplash‐Associated Dysphagia: Considerations of Potential Incidence and Mechanisms. Dysphagia, 35, 403–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone, D. , Ward, E.C. , Bogaardt, H. , Heard, R. , Martin‐Harris, B. , Smith, A.C. et al. (2021a) Self‐reported dysphagia and pharyngeal volume following whiplash injury. Dysphagia, 36, 1019–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone, D.B. , Ward, E.C. , Knijnik, S.R. , Bogaardt, H. & Elliott, J.M. (2021b) Whiplash‐associated dysphagia and dysphonia: A scoping review. Dysphagia, 36, 303–315. [DOI] [PubMed] [Google Scholar]
- Vafaeian, B. , Riahi, H.T. , Amoushahi, H. , Jomha, N.M. & Adeeb, S. (2022) A feature‐based statistical shape model for geometric analysis of the human talus and development of universal talar prostheses. Journal of Anatomy, 240, 305–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon, H. & Mior, S. (1991) The Neck Disability Index: A study of reliability and validity. Journal of Manipulative and Physiological Therapeutics, 14, 409–415. [PubMed] [Google Scholar]
- Voyagis, G.S. , Kyriakis, K.P. , Dimitriou, V. & Vrettou, I. (1998) Value of oropharyngeal Mallampati classification in predicting difficult laryngoscopy among obese patients. European Journal of Anaesthesiology, 15, 330–334. [DOI] [PubMed] [Google Scholar]
- Vrancken, A.C. , Crijns, S.P. , Ploegmakers, M.J. , O'kane, C. , van Tienen, T.G. , Janssen, D. et al. (2014) 3D geometry analysis of the medial meniscus–A statistical shape modeling approach. Journal of Anatomy, 225, 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, S.H. , Keenan, B.T. , Wiemken, A. , Zang, Y. , Staley, B. , Sarwer, D.B. et al. (2020) Effect of weight loss on upper airway anatomy and the apnea‐hypopnea index. The importance of tongue fat. American Journal of Respiratory and Critical Care Medicine, 201, 718–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb, A. , Darekar, A. & Rassoulian, H. (2011) The influence of age, anthropometrics and range of motion on the morphometry of the synovial folds of the lateral atlanto‐axial joints: A pilot study. European Spine Journal, 20, 542–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch, K.C. , Foster, G.D. , Ritter, C.T. , Wadden, T.A. , Arens, R. , Maislin, G. et al. (2002) A novel volumetric magnetic resonance imaging paradigm to study upper airway anatomy. Sleep, 25, 532–542. [PubMed] [Google Scholar]
- Whyte, A. & Gibson, D. (2020) Adult obstructive sleep apnoea: Pathogenesis, importance, diagnosis and imaging. Journal of Medical Imaging and Radiation Oncology, 64, 52–66. [DOI] [PubMed] [Google Scholar]
- Zhang, J. , Ackland, D. & Fernandez, J. (2018) Point‐cloud registration using adaptive radial basis functions. Computer Methods in Biomechanics and Biomedical Engineering, 21, 498–502. [DOI] [PubMed] [Google Scholar]
- Zhang, J. , Malcolm, D. , Hislop‐Jambrich, J. , Thomas, C.D.L. & Nielsen, P.M.F. (2014) An anatomical region‐based statistical shape model of the human femur. Computer Methods in Biomechanics and Biomedical Engineering: Imaging & Visualization, 2, 176–185. [Google Scholar]
- Zheng, Z.H. , Yamaguchi, T. , Kurihara, A. , Li, H.F. & Maki, K. (2014) Three‐dimensional evaluation of upper airway in patients with different anteroposterior skeletal patterns. Orthodontics & Craniofacial Research, 17, 38–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


