Abstract
The substantial decline in skeletal muscle mass, strength, and gait speed is a sign of severe sarcopenia, which may partly depend on genetic risk factors. So far, hundreds of genome-wide significant single nucleotide polymorphisms (SNPs) associated with handgrip strength, lean mass and walking pace have been identified in the UK Biobank cohort; however, their pleiotropic effects on all three phenotypes have not been investigated. By combining summary statistics of genome-wide association studies (GWAS) of handgrip strength, lean mass and walking pace, we have identified 78 independent SNPs (from 73 loci) associated with all three traits with consistent effect directions. Of the 78 SNPs, 55 polymorphisms were also associated with body fat percentage and 25 polymorphisms with type 2 diabetes (T2D), indicating that sarcopenia, obesity and T2D share many common risk alleles. Follow-up bioinformatic analysis revealed that sarcopenia risk alleles were associated with tiredness, falls in the last year, neuroticism, alcohol intake frequency, smoking, time spent watching television, higher salt, white bread, and processed meat intake; whereas protective alleles were positively associated with bone mineral density, serum testosterone, IGF1, and 25-hydroxyvitamin D levels, height, intelligence, cognitive performance, educational attainment, income, physical activity, ground coffee drinking and healthier diet (muesli, cereal, wholemeal or wholegrain bread, potassium, magnesium, cheese, oily fish, protein, water, fruit, and vegetable intake). Furthermore, the literature data suggest that single-bout resistance exercise may induce significant changes in the expression of 26 of the 73 implicated genes in m. vastus lateralis, which may partly explain beneficial effects of strength training in the prevention and treatment of sarcopenia. In conclusion, we have identified and characterized 78 SNPs associated with sarcopenia and 55 SNPs with sarcopenic obesity in European-ancestry individuals from the UK Biobank.
Keywords: sarcopenia, sarcopenic obesity, genetics, DNA, nutrition, physical activity, testosterone, height, fat-free mass, weakness
1. Introduction
Sarcopenia is an age-associated condition characterized by the loss of skeletal muscle strength and muscle mass, and in severe cases, followed by reduced physical performance (e.g., slower gait speed) [1]. In most cases (53–84%), sarcopenia co-exists with obesity [2,3]. Older adults are usually identified as having sarcopenic obesity if low muscle mass and strength, as well as increased adiposity are present [4,5,6]. Furthermore, individuals with sarcopenic obesity can be stratified into stage I (absence of clinical complications) or stage II (presence of clinical complications) [7].
The prevalence of sarcopenia and sarcopenic obesity depends on the diagnostic criteria used to describe these conditions, with the range from 10–27% for sarcopenia [6], and from 10–23% for sarcopenic obesity [8]. Both sarcopenia and sarcopenic obesity are related to negative health-related outcomes, such as increased risk of falls, disability, frailty, osteoporosis, type 2 diabetes (T2D), metabolic syndrome, poor glycaemic profiles (i.e., hyperglycaemia, high HbA1c, insulin resistance, etc.) cardiovascular diseases, dyslipidaemia, poor neurocognitive functioning and quality of life, decreased health span and mortality [9,10,11,12,13,14]. Importantly, while declines in lean mass could contribute to further gains in fat mass, high fat mass may also lead to accelerated loss of lean mass [10].
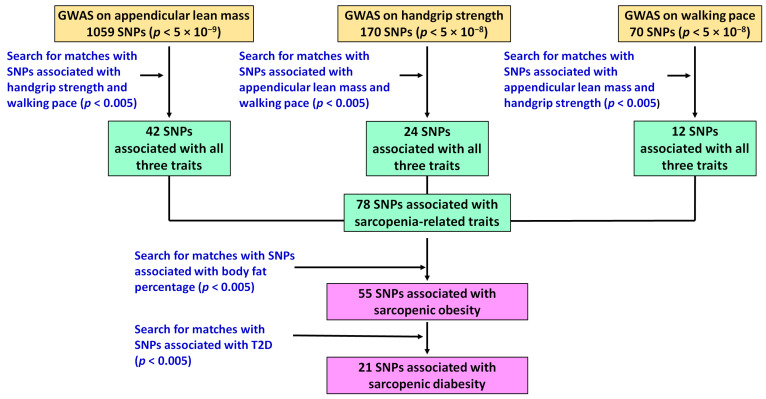
There is a wide range of individual variability in skeletal muscle quantity and quality even under the same biological (age, sex) and environmental (level and type of physical activity, macro and micronutrient intake, etc.) conditions. This variability partly depends on genetic factors, with high heritability for muscle strength (49–56%) [15] and fat-free mass (45–76%) [16]. So far, hundreds of genome-wide significant (p < 5 × 10−8) single nucleotide polymorphisms (SNPs) associated with sarcopenia-related traits, such as handgrip strength (170 SNPs) [17,18,19], appendicular lean mass (1059 SNPs) [20] and walking pace (70 SNPs) [21] have been individually identified in the UK Biobank cohort. However, their pleiotropic effects on all three traits have not been investigated on a systemic level.
Since muscle strength has been shown to be positively correlated with muscle mass and walking speed [22,23], we hypothesized that these phenotypes might be positively associated at a genetic level as well. One might also suggest that alleles associated with all three sarcopenia-related traits (i.e., low muscle strength, low lean mass and slow walking pace) can be considered as the most robust predictors of sarcopenia. On the other hand, risk alleles for both sarcopenia and increased adiposity can be considered as genomic predictors of sarcopenic obesity.
The aims of the present study were threefold: (1) to identify SNPs with pleiotropic effects on handgrip strength, appendicular lean mass, usual walking pace and fat percentage using summary statistics from the UK Biobank cohort; (2) to identify the potential mechanism of action of each SNP on sarcopenia-related traits by searching for intermediate phenotypes and using mice knockout models; and (3) to investigate the effect of resistance exercise on the expression of sarcopenia-related genes using bioinformatic tools.
2. Materials and Methods
2.1. UK Biobank Study
The UK Biobank is an open-access large prospective study with phenotypic and genotypic data from more than 500,000 participants (>90% of participants are of white ethnicity) with an age range for inclusion of 40–69 years when recruited in 2006–2010 [24]. UK Biobank has approval from the North West Multi-centre Research Ethics Committee (MREC) as a Research Tissue Bank (RTB) approval (reference 11/NW/0382). Full written informed consent was obtained from all participants prior to the study.
2.2. Identification of Genomic Predictors of Sarcopenia and Sarcopenic Obesity Using UK Biobank Data
In the first stage, we used publicly available summary statistics from five published genome-wide association studies (GWASes) on handgrip strength [17,18,19], appendicular lean mass [20] and walking speed [21], making an initial list of 1299 genome-wide significant (p < 5 × 10−8) SNPs (Table 1). To identify correspondences between phenotypes (for example, to find if a specific SNP associated with handgrip strength is also associated with appendicular lean mass and walking pace), we used publicly available summary statistics from GWASes on appendicular lean mass [20], appendicular lean mass in older adults [25], handgrip strength (left) [26], handgrip strength (right) [26], handgrip strength in older adults (weakness) [19] and usual walking pace [26] with less stringent p value threshold (p < 0.005) (Table 1). SNPs associated with all three phenotypes (i.e., with appendicular lean mass, handgrip strength and walking pace) with consistent effect directions were considered as potential genomic predictors of sarcopenia.
Table 1.
The list of phenotypes used from the studies involving UK Biobank cohorts.
| Phenotype | p Value | Number of Participants | Reference |
|---|---|---|---|
| Formation of initial list of SNPs associated with sarcopenia-related traits | |||
| Appendicular lean mass (1059 SNPs) | <5 × 10−9 | 450,243 | [20] |
| Maximal handgrip strength (16 SNPs) | <5 × 10−8 | 195,180 | [17] |
| Relative handgrip strength (139 SNPs) | <5 × 10−8 | 334,925 | [18] |
| Handgrip strength in older adults (15 SNPs) | <5 × 10−8 | 256,523 | [19] |
| Self-reported walking pace (70 SNPs) | <5 × 10−8 | 450,967 | [21] |
| Matching phenotypes to identify SNPs with pleiotropic effects | |||
| Appendicular lean mass | <0.005 | 450,243 | [20] |
| Appendicular lean mass in older adults | <5 × 10−8 | 181,862 | [25] |
| Handgrip strength (left) | <0.005 | 359,704 | [26] |
| Handgrip strength (right) | <0.005 | 359,729 | [26] |
| Handgrip strength in older adults | <0.005 | 256,523 | [19] |
| Usual walking pace | <0.005 | 358,974 | [26] |
| Traits analysed for associations with the selected SNPs | |||
| Body fat percentage | <0.005 | 354,628 | [26] |
| Type 2 diabetes | <0.005 | 408,959 | [26] |
| Heel bone mineral density | <0.005 | 426,824 | [27] |
| Frequency of tiredness | <0.005 | 350,580 | [26] |
| Self-reported tiredness | <0.005 | 108,976 | [26] |
| Recent feelings of tiredness or low energy | <0.005 | 117,828 | [26] |
| Falls in the last year | <0.005 | 360,344 | [26] |
| Testosterone levels | <0.005 | 425,097 | [28] |
| Insulin-like growth factor 1 (IGF1) levels | <0.005 | 435,516 | [29] |
| 25-hydroxyvitamin D levels | <0.005 | 417,580 | [30] |
| Time spent watching television | <0.005 | 341,859 | [26] |
| Vigorous physical activity | <0.005 | 261,055 | [31] |
| Participation in strenuous sports | <0.005 | 359,263 | [26] |
| Participation in other exercises | <0.005 | 359,263 | [26] |
| Duration of moderate activity | <0.005 | 268,826 | [26] |
| Duration of other exercises | <0.005 | 172,650 | [26] |
| Moderate to vigorous physical activity levels | <0.005 | 377,234 | [31] |
| Number of days/week of vigorous PA 10+ min | <0.005 | 344,084 | [26] |
| Number of days/week of moderate PA 10+ min | <0.005 | 343,943 | [26] |
| Alcohol intake frequency | <0.005 | 360,726 | [26] |
| Current smoking/ever smoked | <0.005 | 360,797 | [26] |
| Cheese intake | <0.005 | 352,458 | [26] |
| Processed meat intake | <0.005 | 360,468 | [26] |
| Oily fish intake | <0.005 | 359,340 | [26] |
| Water intake | <0.005 | 333,363 | [26] |
| Fruit (fresh or dried) intake | <0.005 | 329,134 | [26] |
| Vegetable (cooked/salad/raw) intake | <0.005 | 350,404 | [26] |
| Muesli intake | <0.005 | 299,898 | [26] |
| Cereal intake | <0.005 | 345,019 | [26] |
| Wholemeal or wholegrain bread intake | <0.005 | 348,424 | [26] |
| White bread intake | <0.005 | 348,424 | [26] |
| Ground (espresso, filter etc.) coffee intake | <0.005 | 283,449 | [26] |
| Salt added to food | <0.005 | 360,954 | [26] |
| Protein intake | <0.005 | 51,453 | [26] |
| Potassium intake | <0.005 | 51,453 | [26] |
| Magnesium intake | <0.005 | 51,453 | [26] |
| Height | <0.005 | 458,235 | [29] |
| Cognitive performance | <0.005 | 257,841 | [32] |
| Intelligence | <0.005 | 269,867 | [33] |
| Educational attainment | <0.005 | 357,549 | [26] |
| Average total household income before tax | <0.005 | 311,028 | [26] |
| Neuroticism | <0.005 | 380,506 | [34] |
SNPs, single nucleotide polymorphisms; PA, physical activity.
In the second stage, to test the hypothesis that sarcopenia-related SNPs are also associated with other health-related traits, we used summary statistics from GWASes on body fat percentage [26], type 2 diabetes [26], heel bone mineral density [27], frequency of tiredness [26], self-reported tiredness [26], recent feelings of tiredness or low energy [26], and falls in the last year [26] (Table 1). Risk alleles for both sarcopenia and increased body fat percentage were considered as genomic predictors of sarcopenic obesity. Furthermore, risk alleles for both sarcopenic obesity and type 2 diabetes were considered as genomic predictors of sarcopenic diabesity. We also used other traits (biochemical, anthropometric, physiological, behavioral) to identify shared genetic architecture between sarcopenia-related traits and lifestyle exposures (Table 1).
2.3. Analysis of Sarcopenia-Related Polygenic Profiles in European Populations
Raw genetic data of sarcopenia-related SNPs of 503 anonymized individuals of European origin from the 1000 Genomes project (Phase 3) [35] were used to calculate a genetic sum score of risk alleles for each individual. This cohort was composed of five subgroups (British from England and Scotland (n = 91), Finnish in Finland (n = 99), Toscani in Italia (n = 107), Iberian populations in Spain (n = 107), Utah residents (CEPH) with Northern and Western European ancestry (n = 99). Unweighted polygenic risk scores (coded as 0, 1 and 2 for homozygous non-risk genotype, heterozygous genotype and homozygous risk genotype, respectively) were developed for the prediction of sarcopenia, sarcopenic obesity and sarcopenic diabesity in European populations. Individuals were evenly divided into 5 groups (20% each) with high (high number of risk alleles), above average, average, below average and low (low number of risk alleles) risks for sarcopenia, sarcopenic obesity and sarcopenic diabesity.
2.4. Analysis of Association of Sarcopenia-Related SNPs with Gene Expression
The Genotype-Tissue Expression (GTEx) portal [36] was used to analyze the association between sarcopenia-related SNPs and expression of genes in different tissues with the focus on skeletal muscle tissue and nervous system (p < 0.05). The GTEx project is an ongoing effort to build a comprehensive public resource to study tissue-specific gene expression and regulation. Samples were collected from 49 tissue sites across >800 individuals, primarily for molecular assays including whole genome sequencing (WGS), whole exome sequencing (WES), and RNA-Seq [37]. SNPs that were significantly (p < 0.05) correlated with expression of genes (levels of mRNAs) were considered as expression quantitative trait loci (eQTLs).
2.5. Analysis of Effects of Knockouts of Implicated Genes on Sarcopenia-Related Traits in Mice
Data from the International Mouse Phenotyping Consortium (IMPC) database [38] were used to assess the effects (p < 0.05) of genes knockout on lean mass, fat mass and grip strength in mice. The IMPC web portal makes available curated, integrated and analyzed knockout mouse phenotyping data from 9000 mouse lines [39].
2.6. Analysis of Effects of Strength Training on the Expression of Sarcopenia-Related Genes
Publicly available human skeletal muscle transcriptome dataset was used to check the significant effect (p < 0.05) of a single-bout resistance exercise on the mRNA of the sarcopenia-related genes in m. vastus lateralis of seven young men (age 23.3 ± 0.6 years) at 2.5 h and 5 h timepoints compared to baseline [40].
3. Results
3.1. Potential Genomic Predictors of Sarcopenia and Sarcopenic Obesity
A flow diagram displaying the study design and the main findings is shown in Figure 1. First, by combining data from five published GWASes on handgrip strength [17,18,19], appendicular lean mass [20] and walking speed [21], we made a list of 1299 genome-wide significant SNPs. The 78 out of those SNPs (from 73 loci) were independently (i.e., all SNP with linkage disequilibrium (LD) threshold r2 > 0.2 were excluded) associated (p < 0.005) with all three traits—appendicular lean mass, handgrip strength and walking pace—with consistent effect directions (Table 2). These 78 SNPs can be considered as potential genomic predictors of sarcopenia and can be used as instruments for Mendelian randomization analysis to study and uncover causal relationships between sarcopenia and other traits.
Figure 1.
A schematic overview of the study design and the main findings.
Table 2.
DNA polymorphisms associated with sarcopenia-related traits, fat percentage and type 2 diabetes.
| Gene/Near Gene | SNP | Protective Allele |
Risk Allele |
p Value | ||||
|---|---|---|---|---|---|---|---|---|
| Handgrip Strength | Appendicular Lean Mass | Usual Walking Pace | Body Fat Percentage | Type 2 Diabetes | ||||
| GDF5 | rs143384 | G | A | 5.5 × 10−46 | 7.0 × 10−319 | 4.0 × 10−8 | NS | NS |
| POLD3 | rs72977282 | T | A | 7.4 × 10−28 | 9.3 × 10−8 | 3.6 × 10−3 | NS | NS |
| LCORL | rs1472852 | C | A | 4.0 × 10−24 | 8.2 × 10−135 | 3.7 × 10−4 | 3.0 × 10−5 | NS |
| ADCY3 | rs10203386 | T | A | 1.6 × 10−23 | 1.7 × 10−36 | 3.3 × 10−3 | 2.4 × 10−38 | NS |
| DLEU1 | rs3116602 | T | G | 1.4 × 10−21 | 9.5 × 10−155 | 8.7 × 10−4 | NS | NS |
| AOC1 | rs6977416 | A | G | 6.7 × 10−19 | 1.4 × 10−113 | 7.7 × 10−4 | 5.6 × 10−10 | NS |
| SLC39A8 | rs13107325 | C | T | 2.0 × 10−17 | 3.9 × 10−3 | 1.8 × 10−21 | 5.0 × 10−23 | 1.1 × 10−4 |
| HLA-DRB1 | rs34415150 | A | G | 3.4 × 10−17 | 2.5 × 10−17 | 2.3 × 10−5 | 6.6 × 10−4 | 6.0 × 10−17 |
| HLA-DRB1 | rs2760975 | G | A | 4.6 × 10−17 | 1.7 × 10−17 | 1.6 × 10−5 | 8.4 × 10−6 | 6.9 × 10−10 |
| MLLT10 | rs1243182 | C | T | 3.5 × 10−16 | 2.6 × 10−3 | 3.9 × 10−7 | 6.5 × 10−14 | NS |
| PRRC2A | rs2260051 | A | T | 1.0 × 10−15 | 5.2 × 10−6 | 2.6 × 10−5 | 3.3 × 10−17 | 1.7 × 10−13 |
| BTNL2 | rs2213581 | T | C | 1.1 × 10−15 | 4.3 × 10−20 | 6.3 × 10−4 | 3.3 × 10−6 | 3.2 × 10−11 |
| FKBPL | rs41268905 | G | A | 2.4 × 10−15 | 8.9 × 10−17 | 4.0 × 10−4 | 1.3 × 10−5 | NS |
| ZBTB38 | rs2871960 | C | A | 4.0 × 10−15 | 2.2 × 10−135 | 1.0 × 10−3 | NS | 9.5 × 10−5 |
| ADCY3 | rs1056074 | T | C | 7.6 × 10−15 | 1.2 × 10−11 | 1.3 × 10−3 | 1.8 × 10−17 | NS |
| PML | rs5742915 | C | T | 1.8 × 10−14 | 9.3 × 10−39 | 4.0 × 10−5 | 4.1 × 10−8 | 1.6 × 10−3 |
| POU6F2 | rs4549685 | T | C | 4.5 × 10−14 | 4.0 × 10−7 | 7.3 × 10−5 | 2.1 × 10−12 | 1.5 × 10−4 |
| HMGA2 | rs4338565 | C | T | 8.0 × 10−14 | 4.9 × 10−151 | 2.3 × 10−4 | NS | 1.4 × 10−3 |
| HLA-DRB1 | rs113315602 | A | C | 1.4 × 10−12 | 1.0 × 10−5 | 5.4 × 10−4 | 3.5 × 10−6 | NS |
| WWP2 | rs4985445 | A | G | 1.4 × 10−12 | 3.3 × 10−20 | 1.2 × 10−5 | 4.6 × 10−18 | 1.7 × 10−5 |
| MTCH2 | rs11039324 | G | A | 3.5 × 10−12 | 7.3 × 10−26 | 3.9 × 10−15 | 9.0 × 10−38 | 3.2 × 10−6 |
| HLA-DRB5 | rs117108573 | C | T | 3.6 × 10−11 | 1.1 × 10−4 | 7.4 × 10−4 | 3.4 × 10−4 | NS |
| GBF1 | rs2273555 | G | A | 4.1 × 10−11 | 8.1 × 10−5 | 8.2 × 10−5 | NS | NS |
| SFMBT1 | rs62253653 | G | A | 9.5 × 10−11 | 3.0 × 10−3 | 1.0 × 10−7 | 4.0 × 10−3 | 1.2 × 10−3 |
| JARID2 | rs2237149 | A | C | 7.5 × 10−10 | 4.5 × 10−5 | 1.8 × 10−4 | 6.4 × 10−6 | NS |
| ADPGK | rs4776614 | C | G | 1.9 × 10−9 | 8.4 × 10−6 | 1.4 × 10−4 | 5.6 × 10−13 | NS |
| JUND | rs7249 | T | C | 2.0 × 10−9 | 1.2 × 10−6 | 2.6 × 10−4 | 5.8 × 10−13 | NS |
| KIF1B | rs3903151 | G | A | 2.6 × 10−9 | 1.3 × 10−16 | 3.0 × 10−4 | 1.2 × 10−4 | 2.9 × 10−3 |
| SWT1 | rs10797999 | T | C | 3.0 × 10−9 | 1.4 × 10−5 | 1.4 × 10−8 | 2.5 × 10−4 | NS |
| FOXP1 | rs4677611 | T | C | 3.2 × 10−9 | 2.4 × 10−4 | 2.2 × 10−3 | 2.3 × 10−5 | NS |
| SOX5 | rs11047225 | C | T | 8.5 × 10−9 | 4.3 × 10−10 | 2.2 × 10−3 | NS | NS |
| NCOA1 | rs77012907 | A | G | 1.2 × 10−8 | 1.2 × 10−13 | 5.8 × 10−4 | 2.9 × 10−15 | NS |
| MMS22L | rs9320823 | T | C | 1.4 × 10−8 | 7.9 × 10−10 | 1.1 × 10−6 | 3.9 × 10−22 | 1.5 × 10−4 |
| ZKSCAN5 | rs3843540 | C | T | 2.3 × 10−8 | 5.8 × 10−6 | 1.1 × 10−4 | 4.0 × 10−9 | NS |
| MLN | rs12055409 | G | A | 3.5 × 10−8 | 3.6 × 10−3 | 1.8 × 10−3 | 3.2 × 10−7 | 4.4 × 10−4 |
| FOXP1 | rs830643 | A | G | 4.0 × 10−8 | 9.7 × 10−7 | 2.9 × 10−7 | 5.7 × 10−8 | 9.3 × 10−6 |
| GADD45G | rs1329733 | A | G | 4.3 × 10−8 | 2.2 × 10−4 | 6.4 × 10−5 | 9.0 × 10−13 | NS |
| IL11 | rs4252548 | C | T | 6.2 × 10−8 | 4.8 × 10−35 | 2.6 × 10−3 | NS | NS |
| COMMD4 | rs11636600 | G | A | 6.8 × 10−8 | 5.0 × 10−13 | 9.7 × 10−11 | NS | NS |
| HABP4 | rs6477489 | C | A | 7.2 × 10−8 | 5.2 × 10−59 | 3.7 × 10−3 | 1.1 × 10−3 | NS |
| GLCCI1 | rs12702693 | T | C | 1.8 × 10−7 | 6.6 × 10−20 | 1.4 × 10−3 | NS | NS |
| H1FX | rs4073154 | G | A | 2.5 × 10−7 | 1.9 × 10−33 | 3.3 × 10−8 | NS | NS |
| CEP192 | rs1786263 | G | T | 3.1 × 10−7 | 1.0 × 10−22 | 2.3 × 10−3 | 5.5 × 10−7 | NS |
| PPARD | rs3734254 | T | C | 5.2 × 10−7 | 2.3 × 10−33 | 5.6 × 10−6 | NS | NS |
| ZNF568 | rs1667369 | A | C | 1.3 × 10−6 | 1.5 × 10−10 | 2.7 × 10−8 | 1.7 × 10−3 | NS |
| SERPINA1 | rs28929474 | T | C | 3.5 × 10−6 | 1.1 × 10−14 | 3.4 × 10−4 | NS | 2.6 × 10−3 |
| NMT1 | rs2301597 | C | T | 4.6 × 10−6 | 4.8 × 10−33 | 2.7 × 10−9 | 1.3 × 10−8 | NS |
| PIEZO1 | rs2968478 | T | G | 5.1 × 10−6 | 5.6 × 10−14 | 2.8 × 10−3 | NS | NS |
| CELF4 | rs12962050 | A | G | 6.8 × 10−6 | 1.5 × 10−14 | 4.8 × 10−4 | 2.1 × 10−3 | NS |
| BCKDHB | rs9350850 | C | T | 7.5 × 10−6 | 2.9 × 10−24 | 1.3 × 10−3 | NS | NS |
| E2F3 | rs4134943 | T | C | 9.9 × 10−6 | 2.0 × 10−8 | 4.9 × 10−9 | 6.7 × 10−5 | 1.2 × 10−5 |
| BTRC | rs10883618 | A | G | 2.6 × 10−5 | 1.8 × 10−4 | 4.1 × 10−9 | 1.5 × 10−6 | 4.6 × 10−3 |
| LIN28A | rs4274112 | A | G | 2.8 × 10−5 | 2.5 × 10−28 | 8.5 × 10−4 | 6.8 × 10−4 | 3.3 × 10−4 |
| ZNF420 | rs62108897 | C | A | 6.3 × 10−5 | 7.7 × 10−19 | 4.7 × 10−3 | 7.1 × 10−4 | NS |
| JUND | rs10686842 | TAAA | T | 6.4 × 10−5 | 7.4 × 10−24 | 3.7 × 10−4 | 1.6 × 10−19 | NS |
| DIPK1A | rs12733767 | C | T | 6.8 × 10−5 | 9.4 × 10−14 | 9.0 × 10−5 | 3.2 × 10−3 | NS |
| IGF2BP3 | rs34776209 | C | T | 6.9 × 10−5 | 1.8 × 10−47 | 8.4 × 10−4 | NS | NS |
| XPO4 | rs7321635 | A | C | 9.0 × 10−5 | 2.6 × 10−11 | 4.5 × 10−4 | NS | NS |
| FHL2 | rs55680124 | C | T | 1.1 × 10−4 | 4.2 × 10−4 | 2.6 × 10−9 | 6.0 × 10−8 | 2.3 × 10−7 |
| VCAN | rs115912456 | G | A | 1.8 × 10−4 | 3.7 × 10−34 | 1.8 × 10−3 | 3.5 × 10−14 | NS |
| RBL2 | rs72801843 | A | T | 1.9 × 10−4 | 8.8 × 10−52 | 8.9 × 10−6 | NS | 4.5 × 10−5 |
| NPPC | rs73000823 | C | T | 2.3 × 10−4 | 1.7 × 10−15 | 3.7 × 10−4 | 1.4 × 10−5 | NS |
| MYO1C | rs9905106 | T | C | 3.5 × 10−4 | 7.5 × 10−14 | 3.9 × 10−3 | 4.4 × 10−5 | NS |
| CDKAL1 | rs745771286 | G | GA | 3.9 × 10−4 | 2.7 × 10−11 | 4.8 × 10−5 | 4.7 × 10−5 | NS |
| GIP | rs4794005 | A | G | 4.3 × 10−4 | 8.8 × 10−15 | 1.1 × 10−3 | 4.9 × 10−4 | 3.6 × 10−4 |
| NCL | rs10202701 | T | C | 4.3 × 10−4 | 3.1 × 10−33 | 2.0 × 10−3 | 2.3 × 10−5 | NS |
| SOCS5 | rs62136933 | A | G | 5.7 × 10−4 | 9.0 × 10−32 | 2.1 × 10−4 | 3.8 × 10−11 | NS |
| CAMKMT | rs11893991 | A | G | 6.0 × 10−4 | 2.3 × 10−9 | 2.4 × 10−3 | NS | NS |
| RIN3 | rs117068593 | T | C | 6.0 × 10−4 | 8.8 × 10−62 | 3.9 × 10−3 | 3.8 × 10−10 | NS |
| JMJD1C | rs7924036 | T | G | 8.9 × 10−4 | 1.2 × 10−5 | 1.2 × 10−13 | NS | NS |
| TRIB1 | rs4870941 | G | C | 1.3 × 10−3 | 1.1 × 10−39 | 2.1 × 10−3 | NS | NS |
| SDCCAG8 | rs2994330 | T | G | 2.4 × 10−3 | 6.6 × 10−12 | 9.6 × 10−5 | 3.0 × 10−4 | NS |
| NYAP2 | rs2054079 | T | C | 3.0 × 10−3 | 3.9 × 10−4 | 4.3 × 10−9 | NS | NS |
| MAML3 | rs57800857 | C | A | 3.5 × 10−3 | 4.0 × 10−7 | 6.4 × 10−11 | 1.4 × 10−13 | 2.7 × 10−4 |
| PITX1 | rs4976261 | G | C | 3.6 × 10−3 | 8.7 × 10−43 | 1.7 × 10−3 | NS | NS |
| PKDCC | rs3035165 | T | TTA | 3.7 × 10−3 | 6.9 × 10−14 | 1.0 × 10−3 | 3.0 × 10−8 | NS |
| HTT | rs362307 | C | T | 3.9 × 10−3 | 2.5 × 10−7 | 1.1 × 10−9 | 2.8 × 10−9 | 1.3 × 10−6 |
| ZNF462 | rs902144 | C | G | 4.0 × 10−3 | 7.2 × 10−13 | 4.0 × 10−4 | 1.7 × 10−3 | NS |
NS, not significant (p > 0.005). SNP, single nucleotide polymorphism. Handgrip strength: any type of handgrip strength (maximal or relative handgrip strength, left or right handgrip strength, handgrip strength in older adults) with the lowest p value. Protective allele: allele associated with greater strength, lean mass, and walking speed and low risk of obesity and T2D. Risk allele: allele associated with lower strength, lean mass, walking speed and high risk of obesity and T2D.
Next, by using summary statistics from GWASs on other health-related traits we found that 55 of the 78 SNPs were associated with body fat percentage with consistent effect directions (i.e., the same allele is a risk variant for both sarcopenia and adiposity) and can be regarded as potential genomic predictors of sarcopenic obesity. Of these 55 SNPs, the 21 SNPs were also associated with the risk of T2D with consistent effect directions (potential genomic predictors of sarcopenic diabesity) (Table 2).
Follow-up bioinformatic analysis revealed that sarcopenia risk alleles were associated with tiredness (16 SNPs), falls in the last year (8 SNPs), neuroticism (12 SNPs), alcohol intake frequency (24 SNPs), smoking (14 SNPs), time spent watching television (22 SNPs), higher salt (8 SNPs), white bread (14 SNPs), and processed meat (6 SNPs) intake. In contrast, the protective alleles were positively associated with bone mineral density (10 SNPs), serum testosterone (23 SNPs), IGF1 (3 SNPs), and 25-hydroxyvitamin D (9 SNPs) levels, height (69 SNPs), intelligence (25 SNPs), cognitive performance (20 SNPs), educational attainment (45 SNPs), income (26 SNPs), physical activity (26 SNPs), ground coffee drinking (12 SNPs) and healthier diet (muesli (17 SNPs), cereal (7 SNPs), wholemeal or wholegrain bread (12 SNPs), potassium (4 SNPs), magnesium (4 SNPs), cheese (18 SNPs), oily fish (11 SNPs), protein (3 SNPs), water (4 SNPs), fruit (16 SNPs), and vegetable (7 SNPs) intake) (Supplementary Table S1).
3.2. Polygenic Analysis of Sarcopenia, Sarcopenic Obesity and Sarcopenic Diabesity
A genetic sum score of sarcopenia risk alleles composed of 78 SNPs was calculated for each of 503 individuals of European origin from the 1000 Genomes project. Individuals were then evenly (by ~20%) divided into five groups. Carriers of 58–68 risk alleles had the lowest risk of sarcopenia, whereas carriers of 81–95 risk alleles had the highest risk. The distribution of risk alleles in each subgroup for sarcopenia, sarcopenic obesity and sarcopenic diabesity is shown in Table 3 and may be used to improve prediction of these disease states when incorporated into existing clinical risk tools in individuals of European origin.
Table 3.
Stratification of European individuals by the number of risk alleles.
| Trait | Disease Risk and Number of Risk Alleles | ||||
|---|---|---|---|---|---|
| Low | Below Average | Average | Above Average | High | |
| Sarcopenia (78 SNPs) | 58–68 | 69–72 | 73–76 | 77–80 | 81–95 |
| Sarcopenic obesity (55 SNPs) | 37–47 | 48–50 | 51–53 | 54–57 | 58–70 |
| Sarcopenic diabesity (21 SNPs) | 10–16 | 17–18 | 19–20 | 21–22 | 23–30 |
SNPs, single nucleotide polymorphisms. The ranges of the number of risk alleles in European individuals with different degrees of the diseases risks is shown.
3.3. Association of Sarcopenia-Related SNPs with Expression of Genes
Of the 78 SNPs, the 58 were identified as eQTL SNPs in the GTEx database that correlated with expression of genes in various tissues including skeletal muscle (32 SNPs), nervous system (13 SNPs), testis (3 SNPs), thyroid (3 SNPs), adipose (1 SNP), left ventricle (3 SNPs), digestive system (2 SNPs), and artery (1 SNP) (Supplementary Table S1).
3.4. Effects of Gene Knockouts of Implicated Genes on Sarcopenia-Related Traits in Mice
As mentioned above, the discovered 78 SNPs are located in or near 73 genes. Using IMPC database we assessed the effects of genes knockout on lean mass, fat mass and grip strength in mice. Data for the knockout effects of 35 genes (of the 73 genes) were available in the database, of which 27 were significant (p < 0.05). Knockouts in 12 genes (Adcy3, Aoc1, Bckdhb, Btnl2, Cdkal1, Cep192, Gdf5, H1fx, Pold3, Rbl2, Swt1, Znf462) led to the decrease in lean mass and strength (with increase in fat mass), whereas knockouts in 15 genes (Adpgk, Btrc, Camkmt, Dipk1a, E2f3, Foxp1, Htt, Igf2bp3, Jmjd1c, Lcorl, Mllt10, Mtch2, Ncoa1, Piezo1, Trib1) had positive effects on lean mass and strength, but negative on fat mass (Supplementary Table S1).
By comparing human (GWAS, GTEx) and mice genes knockout data, we identified eight genes with the same direction of association. More specifically, while protective alleles in ADCY3 (rs10203386 T), BCKDHB (rs9350850 C), CEP192 (rs1786263 G), H1FX (rs4073154 G), and POLD3 (rs72977282 T) genes were associated with the increased expression of these genes in human tissues, the knockout of the corresponding genes in mice (Adcy3, Bckdhb, Cep192, H1fx, and Pold3) led to the decrease in lean mass and strength (with increase in fat mass).
On the other hand, while protective alleles in BTRC (rs10883618 A), LCORL (rs1472852 C), MTCH2 (rs11039324 G) genes were associated with a decreased expression of these genes in human tissues, the knockout of the corresponding genes in mice (Btrc, Lcorl, and Mtch2) led to the increase in lean mass and strength (with decrease in fat mass) (Supplementary Table S1).
3.5. Effects of Strength Training on the Expression of Sarcopenia-Related Genes
Publicly available human skeletal muscle transcriptome dataset [40] provides evidence on the effects of a single-bout resistance (n = 7) exercise on the mRNA expression in 73 implicated genes. Using this data, we found that strength training induces significant changes in the expression of 26 genes (10 upregulated: ADCY3, E2F3, JMJD1C, JUND, MLN, MYO1C, PIEZO1, PPARD, SFMBT1, ZNF462; 16 downregulated: CDKAL1, CEP192, DLEU1, GADD45G, GBF1, GLCCI1, MAML3, MMS22L, NYAP2, SDCCAG8, SWT1, TRIB1 WWP2, XPO4, ZBTB38, ZNF420) (Supplementary Table S1), which may partly explain beneficial effects of strength training in the prevention and treatment of sarcopenia.
4. Discussion
In this study, we identified and characterized 78 pleiotropic genomic predictors of sarcopenia based on previously discovered genome-wide significant SNPs associated with handgrip strength, appendicular lean mass and walking pace. Of the 78 SNPs, 55 polymorphisms were also associated with body fat percentage and 25 polymorphisms with type 2 diabetes (T2D), indicating that sarcopenia, obesity and T2D share many common risk alleles. It is, therefore, unsurprising that according to the Data from Health and Nutrition Examination Survey (NHANES), 83.6% of women and 79.3% of men (aged 60 and older) with sarcopenia also have obesity (i.e., sarcopenic obesity) [2].
The identified 78 SNPs are located in or near 73 genes that have multiple functions including apoptosis (GLCCI1, JUND), calcium signaling (CAMKMT), carbohydrate metabolism (ADPGK, CDKAL1, GIP, PRRC2A), DNA repair (MMS22L, POLD3), growth and development (AOC1, CEP192, DLEU1, FHL2, FKBPL, GADD45G, GDF5, IGF2BP3, IL11, JARID2, LCORL, LIN28A, NPPC, PIEZO1, PITX1, PKDCC, POU6F2, SDCCAG8, TRIB1, VCAN), immune surveillance (BTNL2, HLA-DRB1, HLA-DRB5), intracellular transport (GBF1, KIF1B, RIN3, SLC39A8, XPO4), lipid metabolism (ADCY3, E2F3, HMGA2, MTCH2, NCOA1, NMT1, PPARD), myogenesis (SFMBT1), neurogenesis (DIPK1A, FOXP1, HTT, NYAP2, ZBTB38, ZNF568), protein metabolism (BCKDHB, BTRC, COMMD4, SERPINA1, WWP2), regulation of translation (CELF4), signal transduction (SOCS5), smooth muscle contraction (MLN), and transcriptional regulation (H1FX, HABP4, JMJD1C, MAML3, MLLT10, MYO1C, NCL, PML, RBL2, SOX5, SWT1, ZKSCAN5, ZNF420, ZNF462) (Supplementary Table S1). Interestingly, of the 73 genes, knockouts of 27 genes in mouse models led to functional consequences such as changes in the lean mass, fat mass and grip strength.
Of the 78 SNPs, 58 were identified as eQTL SNPs that correlated with expression of genes in various tissues including skeletal muscle and nervous system, indicating that they are likely to be functional and may influence multiple traits. Indeed, we found that risk alleles were also associated with other intermediate phenotypes of sarcopenia, namely tiredness, falls in the last year, low physical activity, and low bone mineral density. Furthermore, risk alleles were associated with neuroticism, time spent watching television, alcohol intake, smoking and poor diet (higher salt, white bread, and processed meat intake), whereas protective alleles were positively associated with serum testosterone, IGF1, and 25-hydroxyvitamin D levels, height, intelligence, cognitive performance, educational attainment, income, ground coffee drinking and healthier diet (muesli, cereal, wholemeal or wholegrain bread, potassium, magnesium, cheese, oily fish, protein, water, fruit, and vegetable intake).
This is in line with the previous studies stating that low educational attainment [41], neuroticism [42], low testosterone levels [43], short stature [44], high alcohol [45], processed meat [46] and salt [47] intake, sedentary behavior (such as watching television) [48], smoking and physical inactivity [49] are associated with an increased risk of sarcopenia or low muscle strength, whereas coffee, magnesium, potassium, protein, vitamin D, water, oil fish, fruits and vegetables intake [46,50,51,52,53,54] have protective effects against sarcopenia.
Future research is needed to test interventional strategies focusing on all these factors to evaluate improvement in muscle quality and quantity. Given that resistance exercise induces significant changes in the expression of 26 genes (out of 73 implicated genes) in human skeletal muscle compared to the pre-training state, our findings also partly explain beneficial effects of strength training in the prevention and treatment of sarcopenia [55].
The link of 78 SNPs with muscle strength and lean mass indicates that these markers may be important not only in the general population, but also in athletes. Indeed, of this panel of markers, some of protective alleles have been reported to be over-represented in elite sprinters (E2F3 rs4134943 T, FHL2 rs55680124 C, GDF5 rs143384 G, SLC39A8 rs13107325 C, and ZNF568 rs1667369 A) [56] and elite strength athletes (ADCY3 rs10203386 T, ADPGK rs4776614 C, MMS22L rs9320823 T and ZKSCAN5 rs3843540 C) [57] compared to controls. Furthermore, GBF1 rs2273555 G, MLN rs12055409 G, and MMS22L rs9320823 T alleles (all protective) were found to be positively associated with weightlifting performance [58,59]. One of markers (rs3734254) is located in the PPARD gene which is in high linkage disequilibrium (LD) with the PPARD rs2016520 SNP, which has been previously associated with endurance athlete status [60].
Several studies have investigated the association between the DNA polymorphisms and sarcopenia-related traits outside of the UK Biobank project using GWAS [61,62,63,64,65,66,67,68,69,70] or a candidate gene [71,72,73,74,75,76,77,78,79,80,81] approaches. Apart from the classical skeletal muscle traits (lean mass, absolute and relative skeletal muscle mass, skeletal muscle mass index, muscle thickness, anatomical cross-sectional area of muscle groups, etc.), genomic predictors of muscle fiber size (one of surrogate indicators of muscle mass) have been also studied [58,82,83,84,85].
Our study presents novel data of sarcopenia-related genetic markers. However, there are also limitations. Firstly, our findings were based on summary statistics of three different phenotypes which were discovered in the whole sample of the UK Biobank. To confirm the association between identified SNPs, sarcopenia and sarcopenic obesity, a case-control study (individuals with confirmed sarcopenia vs. individuals with normal muscle quality and quantity) is needed in independent studies. Second, our results were obtained using genomic data of European-ancestry individuals from the UK Biobank. Therefore, the set of 78 SNPs should be analyzed for association with sarcopenia in other populations as well before implementation in practice. We also recognise small sample size (n = 7) in the study of transcriptomic responses to a single-bout resistance exercise and encourage independent replication in larger cohorts.
5. Conclusions
In conclusion, we have identified and characterized 78 SNPs associated with sarcopenia and 55 SNPs with sarcopenic obesity that highlight shared genetic architecture between sarcopenia-related traits and lifestyle exposures.
We strongly suspect that many additional common polymorphisms, and probably rare mutations as well, will be shown to be associated with sarcopenia-related traits in due course. Thus, we suspect that the 78 polymorphisms we have identified constitute only a small fraction of the genetic factors that influence muscle strength, muscle mass and walking pace. However, looking to the future, when thousands of polymorphisms will be discovered that contribute to the variability in sarcopenia-related traits, the power of such information (in conjunction with standard measurement data) as a practical tool for clinicians will emerge.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15030758/s1, Table S1: Association of top sarcopenia-related SNPs and implicated genes with health-related traits, gene expression and responses to resistance training.
Author Contributions
Conceptualization, I.I.A.; methodology, I.I.A.; formal analysis, E.A.S., E.P., L.J.G. and I.I.A.; writing—original draft preparation, I.I.A.; writing—review and editing, E.A.S., E.P. and E.A.B.; project administration, I.I.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
UK Biobank has approval from the North West Multi-centre Research Ethics Committee (MREC) as a Research Tissue Bank (RTB) approval (reference no. 11/NW/0382).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the UK Biobank study.
Data Availability Statement
The data presented in this study are publicly available online at https://genetics.opentargets.org (accessed on 27 December 2022).
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
I.I.A. and E.A.B. have been supported by a grant from the Russian Science Foundation (grant no. 22-75-10122: “Evaluation of the influence of endogenous and exogenous factors for the development of various types of obesity”). E.A.S., E.P. and L.J.G. have not received any funding to conduct this study.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cruz-Jentoft A.J., Bahat G., Bauer J., Boirie Y., Bruyère O., Cederholm T., Cooper C., Landi F., Rolland Y., Sayer A.A., et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Batsis J.A., Mackenzie T.A., Emeny R.T., Lopez-Jimenez F., Bartels S.J. Low lean mass with and without obesity, and mortality: Results from the 1999–2004 national health and nutrition examination survey. J. Gerontol. A Biol. Sci. Med. Sci. 2017;72:1445–1451. doi: 10.1093/gerona/glx002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han T., Yuan T., Liang X., Chen N., Song J., Zhao X., Weng Y., Hu Y. Sarcopenic obesity with normal body size may have higher insulin resistance in elderly patients with type 2 diabetes mellitus. Diabetes Metab. Syndr. Obes. 2022;15:1197–1206. doi: 10.2147/DMSO.S360942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott D., Sanders K.M., Aitken D., Hayes A., Ebeling P.R., Jones G. Sarcopenic obesity and dynapenic obesity: 5-year associations with falls risk in middle-aged and older adults. Obesity. 2014;22:1568–1574. doi: 10.1002/oby.20734. [DOI] [PubMed] [Google Scholar]
- 5.Nezameddin R., Itani L., Kreidieh D., El Masri D., Tannir H., El Ghoch M. Understanding sarcopenic obesity in terms of definition and health consequences: A clinical review. Curr. Diabetes Rev. 2020;16:957–961. doi: 10.2174/1573399816666200109091449. [DOI] [PubMed] [Google Scholar]
- 6.Petermann-Rocha F., Balntzi V., Gray S.R., Lara J., Ho F.K., Pell J.P., Celis-Morales C. Global prevalence of sarcopenia and severe sarcopenia: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle. 2022;13:86–99. doi: 10.1002/jcsm.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donini L.M., Busetto L., Bischoff S.C., Cederholm T., Ballesteros-Pomar M.D., Batsis J.A., Bauer J.M., Boirie Y., Cruz-Jentoft A.J., Dicker D., et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Obes. Facts. 2022;15:321–335. doi: 10.1159/000521241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao Q., Mei F., Shang Y., Hu K., Chen F., Zhao L., Ma B. Global prevalence of sarcopenic obesity in older adults: A systematic review and meta-analysis. Clin. Nutr. 2021;40:4633–4641. doi: 10.1016/j.clnu.2021.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Yu F., Hedström M., Cristea A., Dalén N., Larsson L. Effects of ageing and gender on contractile properties in human skeletal muscle and single fibres. Acta Physiol. 2007;190:229–241. doi: 10.1111/j.1748-1716.2007.01699.x. [DOI] [PubMed] [Google Scholar]
- 10.Hirani V., Naganathan V., Blyth F., Le Couteur D.G., Seibel M.J., Waite L.M., Handelsman D.J., Cumming R.G. Longitudinal associations between body composition, sarcopenic obesity and outcomes of frailty, disability, institutionalisation and mortality in community-dwelling older men: The Concord Health and Ageing in Men Project. Age Ageing. 2017;46:413–420. doi: 10.1093/ageing/afw214. [DOI] [PubMed] [Google Scholar]
- 11.Khadra D., Itani L., Tannir H., Kreidieh D., El Masri D., El Ghoch M. Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: A systematic review and meta-analysis. World J. Diabetes. 2019;10:311–323. doi: 10.4239/wjd.v10.i5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasmussen L.J.H., Caspi A., Ambler A., Broadbent J.M., Cohen H.J., d’Arbeloff T., Elliott M., Hancox R.J., Harrington H., Hogan S., et al. Association of neurocognitive and physical function with gait speed in midlife. JAMA Netw. Open. 2019;2:e1913123. doi: 10.1001/jamanetworkopen.2019.13123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Veronese N., Demurtas J., Soysal P., Smith L., Torbahn G., Schoene D., Schwingshackl L., Sieber C., Bauer J., Cesari M., et al. Sarcopenia and health-related outcomes: An umbrella review of observational studies. Eur. Geriatr. Med. 2019;10:853–862. doi: 10.1007/s41999-019-00233-w. [DOI] [PubMed] [Google Scholar]
- 14.Liu C., Liu N., Xia Y., Zhao Z., Xiao T., Li H. Osteoporosis and sarcopenia-related traits: A bi-directional Mendelian randomization study. Front. Endocrinol. 2022;13:975647. doi: 10.3389/fendo.2022.975647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zempo H., Miyamoto-Mikami E., Kikuchi N., Fuku N., Miyachi M., Murakami H. Heritability estimates of muscle strength-related phenotypes: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports. 2017;27:1537–1546. doi: 10.1111/sms.12804. [DOI] [PubMed] [Google Scholar]
- 16.Abney M., McPeek M.S., Ober C. Broad and narrow heritabilities of quantitative traits in a founder population. Am. J. Hum. Genet. 2001;68:1302–1307. doi: 10.1086/320112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willems S.M., Wright D.J., Day F.R., Trajanoska K., Joshi P.K., Morris J.A., Matteini A.M., Garton F.C., Grarup N., Oskolkov N., et al. Large-scale GWAS identifies multiple loci for hand grip strength providing biological insights into muscular fitness. Nat. Commun. 2017;8:16015. doi: 10.1038/ncomms16015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tikkanen E., Gustafsson S., Amar D., Shcherbina A., Waggott D., Ashley E.A., Ingelsson E. Biological insights into muscular strength: Genetic findings in the UK Biobank. Sci. Rep. 2018;8:6451. doi: 10.1038/s41598-018-24735-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones G., Trajanoska K., Santanasto A.J., Stringa N., Kuo C.L., Atkins J.L., Lewis J.R., Duong T., Hong S., Biggs M.L., et al. Genome-wide meta-analysis of muscle weakness identifies 15 susceptibility loci in older men and women. Nat. Commun. 2021;12:654. doi: 10.1038/s41467-021-20918-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pei Y.F., Liu Y.Z., Yang X.L., Zhang H., Feng G.J., Wei X.T., Zhang L. The genetic architecture of appendicular lean mass characterized by association analysis in the UK Biobank study. Commun. Biol. 2020;3:608. doi: 10.1038/s42003-020-01334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Timmins I.R., Zaccardi F., Nelson C.P., Franks P.W., Yates T., Dudbridge F. Genome-wide association study of self-reported walking pace suggests beneficial effects of brisk walking on health and survival. Commun. Biol. 2020;3:634. doi: 10.1038/s42003-020-01357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hayashida I., Tanimoto Y., Takahashi Y., Kusabiraki T., Tamaki J. Correlation between muscle strength and muscle mass, and their association with walking speed, in community-dwelling elderly Japanese individuals. PLoS ONE. 2014;9:e111810. doi: 10.1371/journal.pone.0111810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin Y.H., Chen H.C., Hsu N.W., Chou P. Using hand grip strength to detect slow walking speed in older adults: The Yilan study. BMC Geriatr. 2021;21:428. doi: 10.1186/s12877-021-02361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sudlow C., Gallacher J., Allen N., Beral V., Burton P., Danesh J., Downey P., Elliott P., Green J., Landray M., et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779. doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hernandez Cordero A.I., Gonzales N.M., Parker C.C., Sokolof G., Vandenbergh D.J., Cheng R., Abney M., Sko A., Douglas A., Palmer A.A., et al. Genome-wide associations reveal human-mouse genetic convergence and modifiers of myogenesis, CPNE1 and STC2. Am. J. Hum. Genet. 2019;105:1222–1236. doi: 10.1016/j.ajhg.2019.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Open Targets Genetics. [(accessed on 27 December 2022)]. Available online: https://genetics.opentargets.org.
- 27.Morris J.A., Kemp J.P., Youlten S.E., Laurent L., Logan J.G., Chai R.C., Vulpescu N.A., Forgetta V., Kleinman A., Mohanty S.T., et al. An atlas of genetic influences on osteoporosis in humans and mice. Nat. Genet. 2019;51:258–266. doi: 10.1038/s41588-018-0302-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruth K.S., Day F.R., Tyrrell J., Thompson D.J., Wood A.R., Mahajan A., Beaumont R.N., Wittemans L., Martin S., Busch A.S., et al. Using human genetics to understand the disease impacts of testosterone in men and women. Nat. Med. 2020;26:252–258. doi: 10.1038/s41591-020-0751-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barton A.R., Sherman M.A., Mukamel R.E., Loh P.R. Whole-exome imputation within UK Biobank powers rare coding variant association and fine-mapping analyses. Nat. Genet. 2021;53:1260–1269. doi: 10.1038/s41588-021-00892-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Revez J.A., Lin T., Qiao Z., Xue A., Holtz Y., Zhu Z., Zeng J., Wang H., Sidorenko J., Kemper K.E., et al. Genome-wide association study identifies 143 loci associated with 25 hydroxyvitamin D concentration. Nat. Commun. 2020;11:1647. doi: 10.1038/s41467-020-15421-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klimentidis Y.C., Raichlen D.A., Bea J., Garcia D.O., Wineinger N.E., Mandarino L.J., Alexander G.E., Chen Z., Going S.B. Genome-wide association study of habitual physical activity in over 377,000 UK Biobank participants identifies multiple variants including CADM2 and APOE. Int. J. Obes. 2018;42:1161–1176. doi: 10.1038/s41366-018-0120-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee J.J., Wedow R., Okbay A., Kong E., Maghzian O., Zacher M., Nguyen-Viet T.A., Bowers P., Sidorenko J., Linnér R.K., et al. Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nat. Genet. 2018;50:1112–1121. doi: 10.1038/s41588-018-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Savage J.E., Jansen P.R., Stringer S., Watanabe K., Bryois J., de Leeuw C.A., Nagel M., Awasthi S., Barr P.B., Coleman J.R.I., et al. Genome-wide association meta-analysis in 269,867 individuals identifies new genetic and functional links to intelligence. Nat. Genet. 2018;50:912–919. doi: 10.1038/s41588-018-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagel M., Watanabe K., Stringer S., Posthuma D., van der Sluis S. Item-level analyses reveal genetic heterogeneity in neuroticism. Nat. Commun. 2018;9:905. doi: 10.1038/s41467-018-03242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Ensembl Project Portal. [(accessed on 27 December 2022)]. Available online: http://www.ensembl.org/Homo_sapiens/Info/Index.
- 36.GTEx Portal. [(accessed on 27 December 2022)]. Available online: https://gtexportal.org/home/index.html.
- 37.GTEx Consortium The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science. 2020;369:1318–1330. doi: 10.1126/science.aaz1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The International Mouse Phenotyping Consortium (IMPC) Database. [(accessed on 27 December 2022)]. Available online: https://www.mousephenotype.org/data/search.
- 39.Groza T., Gomez F.L., Mashhadi H.H., Muñoz-Fuentes V., Gunes O., Wilson R., Cacheiro P., Frost A., Keskivali-Bond P., Vardal B., et al. The International Mouse Phenotyping Consortium: Comprehensive knockout phenotyping underpinning the study of human disease. Nucleic Acids Res. 2023;51:D1038–D1045. doi: 10.1093/nar/gkac972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vissing K., Schjerling P. Simplified data access on human skeletal muscle transcriptome responses to differentiated exercise. Sci. Data. 2014;1:140041. doi: 10.1038/sdata.2014.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swan L., Warters A., O’Sullivan M. Socioeconomic disadvantage is associated with probable sarcopenia in community-dwelling older adults: Findings from the English Longitudinal Study of Ageing. J. Frailty Aging. 2022;11:398–406. doi: 10.14283/jfa.2022.32. [DOI] [PubMed] [Google Scholar]
- 42.Tolea M.I., Terracciano A., Simonsick E.M., Metter E.J., Costa P.T., Jr., Ferrucci L. Associations between personality traits, physical activity level, and muscle strength. J. Res. Pers. 2012;46:264–270. doi: 10.1016/j.jrp.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moctezuma-Velázquez C., Low G., Mourtzakis M., Ma M., Burak K.W., Tandon P., Montano-Loza A.J. Association between low testosterone levels and sarcopenia in cirrhosis: A cross-sectional study. Ann. Hepatol. 2018;17:615–623. doi: 10.5604/01.3001.0012.0930. [DOI] [PubMed] [Google Scholar]
- 44.Rossini-Venturini A.C., Abdalla P.P., Fassini P.G., Dos Santos A.P., Tasinafo Junior M.F., Alves T.C., Gomide E.B.G., de Pontes T.L., Pfrimer K., Ferriolli E., et al. Association between classic and specific bioimpedance vector analysis and sarcopenia in older adults: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 2022;14:170. doi: 10.1186/s13102-022-00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hong S.H., Bae Y.J. Association between alcohol consumption and the risk of sarcopenia: A systematic review and meta-analysis. Nutrients. 2022;14:3266. doi: 10.3390/nu14163266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gedmantaite A., Celis-Morales C.A., Ho F., Pell J.P., Ratkevicius A., Gray S.R. Associations between diet and handgrip strength: A cross-sectional study from UK Biobank. Mech. Ageing Dev. 2020;189:111269. doi: 10.1016/j.mad.2020.111269. [DOI] [PubMed] [Google Scholar]
- 47.Yoshida Y., Kosaki K., Sugasawa T., Matsui M., Yoshioka M., Aoki K., Kuji T., Mizuno R., Kuro-O M., Yamagata K., et al. High salt diet impacts the risk of sarcopenia associated with reduction of skeletal muscle performance in the Japanese population. Nutrients. 2020;12:3474. doi: 10.3390/nu12113474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Souza L.F., Danielewicz A.L., Rech C.R., d’Orsi E., Mendonça V.A., Lacerda A.C.R., de Avelar N.C.P. How much time in sedentary behavior is associated with probable sarcopenia in older adults? Geriatr. Nurs. 2022;48:127–131. doi: 10.1016/j.gerinurse.2022.09.007. [DOI] [PubMed] [Google Scholar]
- 49.Gao Q., Hu K., Yan C., Zhao B., Mei F., Chen F., Zhao L., Shang Y., Ma Y., Ma B. Associated factors of sarcopenia in community-dwelling older adults: A systematic review and meta-analysis. Nutrients. 2021;13:4291. doi: 10.3390/nu13124291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dirks-Naylor A.J. The benefits of coffee on skeletal muscle. Life Sci. 2015;143:182–186. doi: 10.1016/j.lfs.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Welch A.A., Skinner J., Hickson M. Dietary magnesium may be protective for aging of bone and skeletal muscle in middle and younger older age men and women: Cross-sectional findings from the UK biobank cohort. Nutrients. 2017;9:1189. doi: 10.3390/nu9111189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Remelli F., Vitali A., Zurlo A., Volpato S. Vitamin D deficiency and sarcopenia in older persons. Nutrients. 2019;11:2861. doi: 10.3390/nu11122861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petermann-Rocha F., Chen M., Gray S.R., Ho F.K., Pell J.P., Celis-Morales C. Factors associated with sarcopenia: A cross-sectional analysis using UK Biobank. Maturitas. 2020;133:60–67. doi: 10.1016/j.maturitas.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Kuo Y.W., Chen C.W., Zhang J.Y., Lee J.D. Association of eating behavior, nutritional risk, and frailty with sarcopenia in taiwanese rural community-dwelling elders: A cross-sectional study. Nutrients. 2022;14:3254. doi: 10.3390/nu14163254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhao H., Cheng R., Song G., Teng J., Shen S., Fu X., Yan Y., Liu C. The effect of resistance training on the rehabilitation of elderly patients with sarcopenia: A meta-analysis. Int. J. Environ. Res. Public Health. 2022;19:15491. doi: 10.3390/ijerph192315491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guilherme J.P.L.F., Semenova E.A., Larin A.K., Yusupov R.A., Generozov E.V., Ahmetov I.I. Genomic predictors of brisk walking are associated with elite sprinter status. Genes. 2022;13:1710. doi: 10.3390/genes13101710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moreland E., Borisov O.V., Semenova E.A., Larin A.K., Andryushchenko O.N., Andryushchenko L.B., Generozov E.V., Williams A.G., Ahmetov I.I. Polygenic profile of elite strength athletes. J. Strength Cond. Res. 2022;36:2509–2514. doi: 10.1519/JSC.0000000000003901. [DOI] [PubMed] [Google Scholar]
- 58.Grishina E.E., Zmijewski P., Semenova E.A., Cięszczyk P., Humińska-Lisowska K., Michałowska-Sawczyn M., Maculewicz E., Crewther B., Orysiak J., Kostryukova E.S., et al. Three DNA polymorphisms previously identified as markers for handgrip strength are associated with strength in weightlifters and muscle fiber hypertrophy. J. Strength Cond. Res. 2019;33:2602–2607. doi: 10.1519/JSC.0000000000003304. [DOI] [PubMed] [Google Scholar]
- 59.Kikuchi N., Moreland E., Homma H., Semenova E.A., Saito M., Larin A.K., Kobatake N., Yusupov R.A., Okamoto T., Nakazato K., et al. Genes and weightlifting performance. Genes. 2022;13:25. doi: 10.3390/genes13010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Akhmetov I.I., Astranenkova I.V., Rogozkin V.A. Association of PPARD gene polymorphism with human physical performance. Mol. Biol. 2007;41:852–857. [PubMed] [Google Scholar]
- 61.Liu X.G., Tan L.J., Lei S.F., Liu Y.J., Shen H., Wang L., Yan H., Guo Y.F., Xiong D.H., Chen X.D., et al. Genome-wide association and replication studies identified TRHR as an important gene for lean body mass. Am. J. Hum. Genet. 2009;84:418–423. doi: 10.1016/j.ajhg.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guo Y.F., Zhang L.S., Liu Y.J., Hu H.G., Li J., Tian Q., Yu P., Zhang F., Yang T.L., Guo Y., et al. Suggestion of GLYAT gene underlying variation of bone size and body lean mass as revealed by a bivariate genome-wide association study. Hum. Genet. 2013;132:189–199. doi: 10.1007/s00439-012-1236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pei Y.F., Hu W.Z., Yang X.L., Wei X.T., Feng G.J., Zhang H., Shen H., Tian Q., Deng H.W., Zhang L. Two functional variants at 6p21.1 were associated with lean mass. Skelet. Muscle. 2019;9:28. doi: 10.1186/s13395-019-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ran S., Zhang Y.X., Liu L., Jiang Z.X., He X., Liu Y., Shen H., Tian Q., Pei Y.F., Deng H.W., et al. Association of 3p27.1 variants with whole body lean mass identified by a genome-wide association study. Sci. Rep. 2020;10:4293. doi: 10.1038/s41598-020-61272-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ran S., He X., Jiang Z.X., Liu Y., Zhang Y.X., Zhang L., Gu G.S., Pei Y., Liu B.L., Tian Q., et al. Whole-exome sequencing and genome-wide association studies identify novel sarcopenia risk genes in Han Chinese. Mol. Genet. Genom. Med. 2020;8:e1267. doi: 10.1002/mgg3.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu S.E., Chen W.L. A Genome-wide association study identifies novel risk loci for sarcopenia in a taiwanese population. J. Inflamm. Res. 2021;14:5969–5980. doi: 10.2147/JIR.S338724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoon K.J., Yi Y., Do J.G., Kim H.L., Lee Y.T., Kim H.N. Variants in NEB and RIF1 genes on chr2q23 are associated with skeletal muscle index in Koreans: Genome-wide association study. Sci. Rep. 2021;11:2333. doi: 10.1038/s41598-021-82003-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Luo J., Zhang T., Wang W., Zhang D. Genome-wide association study of handgrip strength in the Northern Chinese adult twins. Connect. Tissue Res. 2022:1–9. doi: 10.1080/03008207.2022.2104160. [DOI] [PubMed] [Google Scholar]
- 69.Jin H., Yoo H.J., Kim Y.A., Lee J.H., Lee Y., Kwon S.H., Seo Y.J., Lee S.H., Koh J.M., Ji Y., et al. Unveiling genetic variants for age-related sarcopenia by conducting a genome-wide association study on Korean cohorts. Sci. Rep. 2022;12:3501. doi: 10.1038/s41598-022-07567-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gim J.A., Lee S., Kim S.C., Baek K.W., Yoo J.I. Demographic and genome wide association analyses according to muscle mass using data of the korean genome and epidemiology study. J. Korean Med. Sci. 2022;37:e346. doi: 10.3346/jkms.2022.37.e346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roth S.M., Zmuda J.M., Cauley J.A., Shea P.R., Ferrell R.E. Vitamin D receptor genotype is associated with fat-free mass and sarcopenia in elderly men. J. Gerontol. A Biol. Sci. Med. Sci. 2004;59:10–15. doi: 10.1093/gerona/59.1.B10. [DOI] [PubMed] [Google Scholar]
- 72.Fuku N., Mori S., Murakami H., Gando Y., Zhou H., Ito H., Tanaka M., Miyachi M. Association of 29C>T polymorphism in the transforming growth factor-β1 gene with lean body mass in community-dwelling Japanese population. Geriatr. Gerontol. Int. 2012;12:292–297. doi: 10.1111/j.1447-0594.2011.00768.x. [DOI] [PubMed] [Google Scholar]
- 73.Walsh S., Ludlow A.T., Metter E.J., Ferrucci L., Roth S.M. Replication study of the vitamin D receptor (VDR) genotype association with skeletal muscle traits and sarcopenia. Aging Clin. Exp. Res. 2016;28:435–442. doi: 10.1007/s40520-015-0447-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Johns N., Stretch C., Tan B.H., Solheim T.S., Sørhaug S., Stephens N.A., Gioulbasanis I., Skipworth R.J., Deans D.A., Vigano A., et al. New genetic signatures associated with cancer cachexia as defined by low skeletal muscle index and weight loss. J. Cachexia Sarcopenia Muscle. 2017;8:122–130. doi: 10.1002/jcsm.12138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pratt J., Boreham C., Ennis S., Ryan A.W., De Vito G. Genetic associations with aging muscle: A systematic review. Cells. 2019;9:12. doi: 10.3390/cells9010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yao X., Yang L., Li M., Xiao H. Relationship of vitamin D receptor gene polymorphism with sarcopenia and muscle traits based on propensity score matching. J. Clin. Lab. Anal. 2020;34:e23485. doi: 10.1002/jcla.23485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Khanal P., He L., Herbert A.J., Stebbings G.K., Onambele-Pearson G.L., Degens H., Morse C.I., Thomis M., Williams A.G. The Association of multiple gene variants with ageing skeletal muscle phenotypes in elderly women. Genes. 2020;11:1459. doi: 10.3390/genes11121459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.He L., Khanal P., Morse C.I., Williams A., Thomis M. Associations of combined genetic and epigenetic scores with muscle size and muscle strength: A pilot study in older women. J. Cachexia Sarcopenia Muscle. 2020;11:1548–1561. doi: 10.1002/jcsm.12585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guilherme J.P.L., Shikhova Y.V., Dondukovskaya R.R., Topanova A.A., Semenova E.A., Astratenkova I.V., Ahmetov I.I. Androgen receptor gene microsatellite polymorphism is associated with muscle mass and strength in bodybuilders and power athlete status. Ann. Hum. Biol. 2021;48:142–149. doi: 10.1080/03014460.2021.1919204. [DOI] [PubMed] [Google Scholar]
- 80.Guilherme J.P.L.F., Semenova E.A., Borisov O.V., Kostryukova E.S., Vepkhvadze T.F., Lysenko E.A., Andryushchenko O.N., Andryushchenko L.B., Lednev E.M., Larin A.K., et al. The BDNF-increasing allele is associated with increased proportion of fast-twitch muscle fibers, handgrip strength, and power athlete status. J. Strength Cond. Res. 2022;36:1884–1889. doi: 10.1519/JSC.0000000000003756. [DOI] [PubMed] [Google Scholar]
- 81.Khanal P., Morse C.I., He L., Herbert A.J., Onambélé-Pearson G.L., Degens H., Thomis M., Williams A.G., Stebbings G.K. Polygenic models partially predict muscle size and strength but not low muscle mass in older women. Genes. 2022;13:982. doi: 10.3390/genes13060982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ahmetov I.I., Mozhayskaya I.A., Lyubaeva E.V., Vinogradova O.L., Rogozkin V.A. PPARG Gene polymorphism and locomotor activity in humans. Bull. Exp. Biol. Med. 2008;146:630–632. doi: 10.1007/s10517-009-0364-y. [DOI] [PubMed] [Google Scholar]
- 83.Seaborne R.A., Hughes D.C., Turner D.C., Owens D.J., Baehr L.M., Gorski P., Semenova E.A., Borisov O.V., Larin A.K., Popov D.V., et al. UBR5 is a novel E3 ubiquitin ligase involved in skeletal muscle hypertrophy and recovery from atrophy. J. Physiol. 2019;597:3727–3749. doi: 10.1113/JP278073. [DOI] [PubMed] [Google Scholar]
- 84.Guilherme J.P.L., Semenova E.A., Borisov O.V., Larin A.K., Moreland E., Generozov E.V., Ahmetov I.I. Genomic predictors of testosterone levels are associated with muscle fiber size and strength. Eur. J. Appl. Physiol. 2022;122:415–423. doi: 10.1007/s00421-021-04851-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hall E.C.R., Semenova E.A., Bondareva E.A., Andryushchenko L.B., Larin A.K., Cięszczyk P., Generozov E.V., Ahmetov I.I. Association of genetically predicted bcaa levels with muscle fiber size in athletes consuming protein. Genes. 2022;13:397. doi: 10.3390/genes13030397. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are publicly available online at https://genetics.opentargets.org (accessed on 27 December 2022).