Abstract
Current evidence and professional guidance recommend sleeping between 7 and 9 h in a 24-h period for optimal health. The present study examines the association between sleep duration and mortality and assesses whether this association varies by racial/ethnic identity for a large and diverse sample of United States adults. We use data on 274,836 adults, aged 25 and older, from the 2004–2014 waves of the National Health Interview Survey (NHIS) linked to prospective mortality through 2015 (23,382 deaths). Cox proportional hazards models were used in multi-variable regressions to estimate hazard ratios for mortality by sleep duration and racial/ethnic identity, controlling for sociodemographic, socioeconomic, and psychological distress variables. We find elevated risks of mortality from any cause for adults who sleep less than 5 h or more than 9 h in a 24-h period after all adjustments. Further, we find evidence that these elevated risks for mortality are more pronounced for some racial/ethnic groups and less pronounced for others. Improved understanding of differences in sleep duration and sleep health can facilitate more effective and culturally-tailored interventions around sleep health, improving overall well-being and enhancing longevity.
Keywords: Sleep duration, Mortality, Race, Ethnicity, Health disparities
Highlights
-
•
Sleeping less than 5 h associates with higher mortality than sleeping 5–7 h.
-
•
Sleeping more than 9 h associates with higher mortality than sleeping less than 7 h.
-
•
Mortality risks associated with inadequate and excessive sleep are race/ethnic specific.
1. Introduction
The American Academy of Sleep Medicine, the Sleep Research Society, and the National Sleep Foundation recommend sleeping between 7 and 9 h in a 24-h period for optimal health (Ramar et al., 2021). Sleeping either less than 7 or more than 9 h has been associated with an increased risk of cardiovascular disease, cancer, and all-cause mortality (Tao et al., 2021). Previous studies focusing on the link between sleep duration and mortality have examined and reported important differences by age and sex (Liu et al., 2017; Shan et al., 2015). Namely, the association between sleep duration and mortality is stronger among individuals below 65 years of age, compared to those 65 and older (Akerstedt et al., 2017). Men tend to experience a higher rate of mortality from sleep issues than women, although women have higher rates of sleep issues and overall shorter sleep duration than men (Grandner, 2017). Much less is known about the extent to which the association between sleep duration and mortality might also vary by racial/ethnic identity in the United States (U.S.).
2. Race/ethnicity, sleep, and mortality
Racial and ethnic disparities in health and mortality have been well documented for over 100 years (Williams, 2012). Some racial and ethnic groups in the U.S., particularly non-Hispanic Black and American Indian and Alaska Native (AIAN) people, suffer disproportionately from a variety of chronic health conditions and mortality (Breathett et al., 2020; McGrath et al., 2019). This leads to wide differences in, for example, life expectancy across racial and ethnic groups (Olshansky et al., 2012). In this study, we approach racial and ethnic health disparities in sleep health, chronic health conditions, and mortality as a product of the social determinants of health and the disproportionate inequities that racial minorities face in their lifetime, compared to non-Hispanic Whites (Braveman et al., 2011).
Our examination of sleep duration and mortality across racial and ethnic groups is informed by evidence that indicates the presence of racial and ethnic disparities in risk factors for mortality (see Williams, 2012). For example, previous research has found that mortality risks associated with similar levels of cigarette smoking and alcohol consumption are greater for racial and ethnic minorities than for non-Hispanic Whites. Reasons for the added burden for racial minorities are likely multifaceted and include some combination of social, economic, cultural, and even biological adaptation, including gene expression changes in response to risk factor exposure (Williams et al., 2010). Thus, if short and long sleep duration are associated with increased mortality risk, might those risks be exacerbated for racial and ethnic minorities?
Previous studies have described differences in sleep duration by race/ethnicity (Grandner, 2017; Whinnery et al., 2014) and showed that non-Hispanic Blacks, non-Hispanic Asians, and non-Mexican Hispanics/Latinos were more likely to report very short sleep duration (less than 5 h) than non-Hispanic Whites (Whinnery et al., 2014). Other studies have linked racial/ethnic differences in sleep duration to health disparities in disease prevalence (Chattu et al., 2019; Grandner et al., 2014, 2016). A recent study reporting differences in sleep duration between non-Hispanic Whites and non-Hispanic Blacks argued that this disparity explains an increased risk in cardiovascular disease among non-Hispanic Blacks (Butler et al., 2020).
Research studies using nationally representative samples have reported racial differences in the associations between sleep health and chronic health outcomes (Grandner et al., 2014; Sands-Lincoln et al., 2013; Zizi et al., 2012). Another study comparing non-Hispanic Whites, non-Hispanic Blacks, Mexican Americans, other Hispanic/Latinos, and Asians, reported that the association between short sleep duration and obesity is strongest among non-Hispanic Blacks, while the association between short sleep duration and hypertension is strongest in non-Hispanic Whites, non-Hispanic Blacks, and other Hispanic/Latinos, than in Mexican Americans and Asians (Whinnery et al., 2014). A study using the National Health and Nutrition Examination Survey reported that symptoms of obstructive sleep apnea had a stronger association with hypertension in non-Hispanic Blacks, compared to non-Hispanic Whites and Hispanics (Sands-Lincoln et al., 2013). Finally, a study using the National Health Interview Survey showed that the associations between short and long sleep duration and type 2 diabetes was stronger for non-Hispanic Blacks, compared to non-Hispanic Whites (Zizi et al., 2012).
Despite the longstanding interest in understanding sleep health disparities by race/ethnicity and their impact on health outcomes, no study to date has examined whether disparities in sleep duration might be associated with differences in all-cause mortality risk. Because previous studies have showed that both short and long sleep durations are associated with multiple chronic health conditions, we expect that short and long sleep duration will increase all-cause mortality risk. Previous studies have also reported significant racial differences in the associations between sleep duration and chronic health conditions. Thus, we expect that the link between sleep duration and all-cause mortality risk will vary by race/ethnicity.
3. Objectives
The current study fills a gap in the sleep health disparities literature by leveraging a large national dataset to examine the association between sleep duration and mortality in 5 racial/ethnic groups: non-Hispanic (NH) Whites, NH Blacks, NH American Indian and Alaska Native people, NH Asians, and Hispanics. The objectives of the present study are to measure the association between sleep duration and all-cause mortality risk and to assess whether the association between sleep duration and all-cause mortality varies by race/ethnicity.
4. Data and methods
4.1. Data
Data come from the 2004–2014 waves of the National Health Interview Survey (NHIS), a cross-sectional, nationally representative survey, linked to prospective mortality status through 2015. For prospective mortality linkage to the NHIS, the National Center for Health Statistics (NCHS) uses a probabilistic mortality matching scheme described elsewhere (Mirel et al., 2020, pp. 1–32) to create the Linked Mortality File (LMF). The IPUMS NHIS provided by the Institute for Social Research and Data Innovation at the University of Minnesota includes the complete mortality linked data set used for our analysis (Blewett et al., 2021).
4.2. Measures
The dependent variable in our primary analysis is a binary variable representing death from any cause (coded 1) or survival during the follow-up period (coded 0). In multivariable analyses, described below, we include a core set of individual-level sociodemographic and socioeconomic control measures including age and age squared (to account for the non-linear association between age and mortality), sex, region of residence, marital status, educational attainment, household poverty status, and employment status. We also include a mental health indicator, the Kessler 6-item (K6) scale for psychological distress (Kessler et al., 2003, 2010). Psychological distress ranges from 0 (no distress) to 24 (extreme distress). Based on previous research (Kessler et al., 2003, 2010), we included the K6 measure in several different specifications, including a continuous version and a multi-categorical version. Ultimately, we convert the Kessler scale into a binary indicator of severe mental illness with K6 scores greater than or equal to 13 (Kessler et al., 2003) and include that measure in all models as results were not sensitive to the different specifications. In analyses not provided here, we included an indicator of body mass index (BMI), but this measure did not impact associations between sleep duration, race/ethnicity, and mortality (available upon request).
Sleep duration (our primary independent measure) is a measure available in the Sample Adult File of the NHIS and is derived by asking respondents about their average number of hours of sleep in a 24-h period. We re-code this variable into categories according to the American Academy of Sleep Medicine's recommendations: less than 7 h, 7–9 h (reference, hereafter “ref”), and more than 9 h (Ramar et al., 2021). Work by Kurina et al. (2013) on the importance of sleep duration measurement in the interpretation of associations between sleep duration and mortality prompted us to further break down the less than 7 h category into 5 to less than 7 h and less than 5 h.
We use self-reported race/ethnicity in the NHIS to generate categories for non-Hispanic (NH) White (referent, henceforth White), NH Black (henceforth Black), NH American Indian/Alaska Native (henceforth AIAN), NH Asian (henceforth Asian), and Hispanic. NHIS respondents are asked to identify which race or races they consider themselves to be. For ethnicity, NHIS respondents are asked whether they self-identify as Hispanic or Latino, and list a few examples, such as Mexican, Mexican American, Puerto Rican, Cuban, or Dominican. Identifying with multiple racial identities is allowable and a small number of adults did so during our survey years. However, detail on multiple racial identity adults is not publicly available. We are ultimately able to include the groups listed above based on adequate sample size and deaths available by group, and we are unable to include multiracial adults.
Missing data in the NHIS is minimal across our measures of interest, except for income measures used to assess household poverty status, where roughly 17% of cases are missing. To maximize our sample and avoid working with biased estimates, we employ multiple imputation techniques and create five imputed datasets using chained equations procedures with Stata software, version 16 (StataCorp, 2019). Consistent with best practices, we include the dependent variable in the imputation procedures but then drop imputed dependent variable cases in the final analyses (von Hippel, 2007). All estimates for all multivariate analyses come from the multiply imputed data. Our final analytic sample is 274,836 adults aged 25 and older, of which 8.5%, or 23,382 individuals, died over the follow-up period.
4.3. Method
We use Cox Proportional Hazard models to estimate the associations between sleep duration, race/ethnicity, and mortality (Allison, 1984). The Cox model declares the hazard rate for the jth respondent as h(t|xj) = h0(t) exp(xjβx), where the coefficients βx are estimated from the data using a partial likelihood approach. First, we establish the association between sleep duration and mortality after adjusting for confounding variables. Next, with all confounders included, we interact sleep duration and race/ethnicity to examine if the association between sleep duration and mortality varies by race/ethnicity. We report all results in the form of hazard ratios (HR) and use Stata software (StataCorp, 2019) to incorporate sample weights, adjust for the complex sampling frame, and estimate robust standard errors to account for the clustered sampling design of the NHIS.
5. Results
5.1. Sample description
Table 1 provides descriptive information on the full sample and on the adults who died from any cause over the follow-up period. The majority of adults (65.9%) report sleeping the recommended 7–9 h over a 24-h period. However, nearly a third of adults report sleeping less than 7 h, and among this group, a small but important subset (2.7%) report sleeping less than 5 h. These short sleeping adults may be at particularly high risk for mortality. Finally, while a small portion of adults (4%) report sleeping more than 9 h on average, those adults account for a disproportionate number of deaths (over 12%).
Table 1.
Proportions of the total sample and deaths among adults age 25 and older in the NHIS-LMF, 2004–2015.
| % of sample | % dead | |
|---|---|---|
| Overall | 100.0% | 8.5% |
| Sleep duration | ||
| 7–9 h | 65.9% | 61.8% |
| <7 h | 30.1% | 26.0% |
| 5 to <7 h | 27.3% | 22.4% |
| <5 h | 2.7% | 3.6% |
| >9 h | 4.0% | 12.2% |
| Race/ethnicity | ||
| White | 72.3% | 79.9% |
| Black | 11.9% | 10.6% |
| AIAN | 0.5% | 0.6% |
| Asian | 3.9% | 2.2% |
| Hispanic | 11.4% | 6.7% |
| Age (mean) | 51.1 | 70.0 |
| Sex | ||
| Male | 45.1% | 47.2% |
| Region of residence | ||
| Northeast | 18.0% | 18.9% |
| Midwest | 24.2% | 25.2% |
| South | 36.8% | 37.5% |
| West | 21.0% | 18.5% |
| Marital status | ||
| Married | 49.7% | 37.2% |
| Divorced | 16.7% | 15.1% |
| Separated | 3.4% | 2.4% |
| Widowed | 10.9% | 35.9% |
| Never married | 19.3% | 9.3% |
| Education | ||
| High school or less | 41.7% | 61.2% |
| Some college | 28.5% | 22.9% |
| Bachelor's degree | 18.9% | 9.9% |
| Graduate education | 10.9% | 6.0% |
| Employment status | ||
| Employed | 60.3% | 19.3% |
| Unemployed | 3.7% | 1.5% |
| Not in the labor force | 36.0% | 79.2% |
| Household poverty status | ||
| Living at or below poverty | 12.8% | 17.2% |
| Psychological distress | ||
| Severe mental illnessa | 3.5% | 5.1% |
N = 274,836; Deaths = 23,382.
Greater than or equal to 13 on the Kessler 6-item scale (Kessler et al., 2003).
Source: IPUMS NHIS
The majority of the NHIS sample (72.3%) and the deaths over the study period (79.9%) were self-identified Whites. Because of the large overall sample of the NHIS, the relatively smaller proportions of racial/ethnic minorities in the full sample and among the deaths allow for robust analyses. The smallest group, AIAN people, represents about 0.5% of the full sample (over 1300 adults) and 0.6% of all deaths (140 deaths).
Other sociodemographic and socioeconomic covariates resemble patterns consistent with decades of past research (Olshansky et al., 2012; Rogers et al., 2000). For example, a disproportionate number of widowed adults, lower educated adults, adults not in the labor force, and adults living in households at or below the poverty line, died over the follow-up period. Of the total sample of adults aged 25 or older, 3.5% were classified as having severe mental illness. Finally, a larger proportion of adults who died over the follow-up period (5.1%) were classified as having severe mental illness.
5.2. Racial/ethnic disparities in sleep duration
Table 2 provides the proportions of racial and ethnic groups in each of the sleep duration categories and indicators of significance between Whites and the other groups in each of the sleep categories. Across all racial/ethnic groups, the majority of adults sleep the recommended 7–9 h. However, there are some important differences. For example, over 67% of Whites sleep the recommended time, but significantly fewer (56.4%; p ≤ .001) Blacks do so. In fact, relative to Whites, significantly larger proportions of Blacks sleep less than 5 h (4.4%; p ≤ .001), between 5 and 7 h (33.7%; p ≤ .001), and more than 9 h (5.5%; p ≤ .001). To examine the association between sleep duration, race/ethnicity, and mortality in a multivariate setting, we turn to the Cox regression results in Table 3.
Table 2.
Race/ethnicity and sleep duration among adults age 25 and older in the NHIS-LMF, 2004–2015.a
| Sleep duration | ||||||||
|---|---|---|---|---|---|---|---|---|
| <5 h | 5 to <7 h | 7–9 h | >9 h | |||||
| Race/ethnicity | ||||||||
| White | 2.5% | 26.3% | 67.3% | 3.9% | ||||
| Black | 4.4% | *** | 33.7% | *** | 56.4% | *** | 5.5% | *** |
| AIAN | 4.5% | *** | 29.8% | * | 60.4% | *** | 5.4% | * |
| Asian | 1.8% | *** | 29.2% | *** | 66.4% | 2.5% | *** | |
| Hispanic | 2.6% | 26.6% | 67.4% | 3.5% | *** | |||
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
a Significant differences indicated within each sleep category, in reference to White.
Source: IPUMS NHIS; N = 274,836
Table 3.
Cox hazard ratios [standard errors] of all-cause mortality by sleep duration and race/ethnicity, NHIS-LMF 2004–2015.
| Model 0 | Model 1a | Model 2b | Model 3c | |||||
|---|---|---|---|---|---|---|---|---|
| Sleep duration | ||||||||
| 7–9 h | ref | ref | ref | ref | ||||
| 5 to <7 h | 0.88 | *** | 1.06 | ** | 1.02 | 1.04 | ||
| [0.02] | [0.02] | [0.02] | [0.02] | |||||
| < 5 h | 1.47 | *** | 1.65 | *** | 1.28 | *** | 1.34 | *** |
| [0.06] | [0.07] | [0.06] | [0.07] | |||||
| > 9 h | 3.86 | *** | 2.01 | *** | 1.77 | *** | 1.88 | *** |
| [0.10] | [0.05] | [0.05] | [0.06] | |||||
| Race/ethnicity | ||||||||
| White | ref | ref | ref | |||||
| Black | 1.16 | *** | 0.97 | 1.04 | ||||
| [0.03] | [0.02] | [0.03] | ||||||
| AIAN | 1.33 | * | 1.17 | 1.14 | ||||
| [0.15] | [0.13] | [0.17] | ||||||
| Asian | 0.79 | *** | 0.85 | ** | 0.97 | |||
| [0.04] | [0.04] | [0.06] | ||||||
| Hispanic | 0.98 | 0.85 | *** | 0.92 | * | |||
| [0.03] | [0.03] | [0.04] | ||||||
| Interaction | ||||||||
| 5 to < 7 h * Black | 0.92 | |||||||
| [0.05] | ||||||||
| 5 to < 7 h * AIAN | 1.09 | |||||||
| [0.26] | ||||||||
| 5 to < 7 h * Asian | 0.77 | * | ||||||
| [0.08] | ||||||||
| 5 to < 7 h * Hispanic | 0.85 | * | ||||||
| [0.06] | ||||||||
| < 5 h * Black | 0.86 | |||||||
| [0.09] | ||||||||
| < 5 h * AIAN | 1.14 | |||||||
| [0.51] | ||||||||
| < 5 h * Asian | 0.93 | |||||||
| [0.25] | ||||||||
| < 5 h * Hispanic | 0.69 | ** | ||||||
| [0.10] | ||||||||
| > 9 h * Black | 0.74 | *** | ||||||
| [0.05] | ||||||||
| > 9 h * AIAN | 0.93 | |||||||
| [0.25] | ||||||||
| > 9 h * Asian | 0.59 | ** | ||||||
| [0.10] | ||||||||
| > 9 h * Hispanic | 0.80 | * | ||||||
| [0.08] | ||||||||
N = 274,836; Deaths = 23,382.
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
Model 1 controls for age, age2, sex.
Model 2 adds controls for region, marital status, education, employment, household poverty, and severe mental illness.
Model 3 includes all controls.
Source: IPUMS NHIS.
5.3. Sleep duration and mortality
Model 0 of Table 3 presents hazard ratios for all-cause mortality by sleep duration before any adjustments. Relative to sleeping 7–9 h, sleeping less than 5 h and sleeping more than 9 h is associated with a higher risk of death from any cause. Relative to the referent group, mortality risk is nearly 4 times higher (HR = 3.86) for those sleeping greater than 9 h in this baseline model. Sleeping 5 to less than 7 h, relative to sleeping 7–9 h, is associated with a slightly lower risk of all-cause mortality (HR = 0.88) in this baseline model.
5.4. Mortality risk by sleep duration and race/ethnicity
Model 1 of Table 3 presents hazard ratios for all-cause mortality by sleep duration and race/ethnicity, controlling for age and sex. Relative to sleeping the recommended 7–9 h, adults who reported sleeping between 5 and less than 7 h experienced 6% higher risk of all-cause mortality. Adults sleeping less than 5 h had 1.65 times the risk of death from any cause, and adults who reported sleeping more than 9 h had over 2 times the risk of death over the follow-up period, relative to sleeping 7–9 h. Differences by racial and ethnic identity show that, relative to Whites, Black and AIAN adults experienced higher risk and Asian adults experienced lower risk of mortality over the follow-up period.
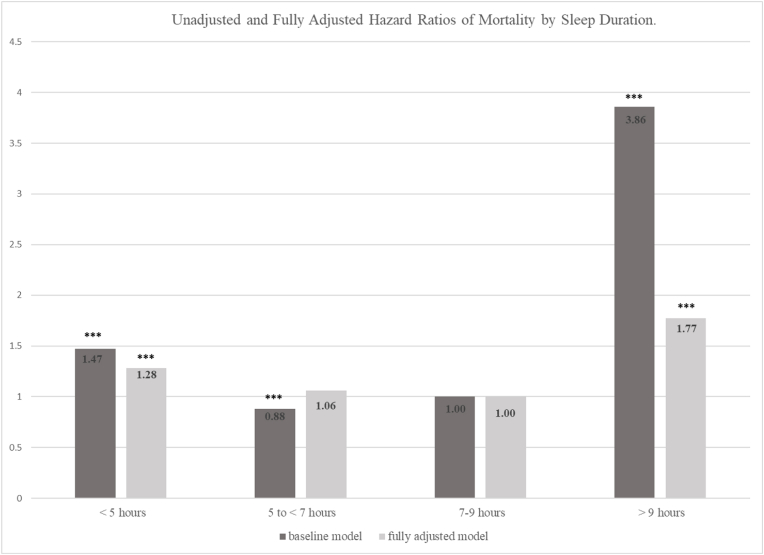
Model 2 includes all other controls for region of residence, marital status, socioeconomic status (SES), and severe mental illness. These controls attenuate the mortality risks associated with sleep considerably. The higher risk of mortality for adults sleeping between 5 and less than 7 h, relative to adults sleeping the recommended 7–9 h, is explained away in Model 2. Risks for adults sleeping less than 5 h are 1.28 times higher than the referent group in Model 2. Risks for adults sleeping greater than 9 h are 1.77 times higher in Model 2, relative to sleeping the recommended 7–9 h. The differences in mortality risks associated with sleep duration from the baseline Model 0 to the fully adjusted Model 2 are illustrated in Fig. 1. The controls in Model 2 also account for the higher risk of mortality, relative to Whites, among Black and AIAN adults. Model 2 further shows that, after accounting for SES and other mortality risk factors, relative to Whites, Asian and Hispanic adults have a lower risk of mortality.
Fig. 1.
Unadjusted and Fully Adjusted Hazard Ratios of Mortality by Sleep Duration.
Notes: Fully adjusted model controls for age, age2, sex, region of residence, marital status, education, employment status, household poverty, and severe mental illness. *p ≤ .05; **p ≤ .01; ***p ≤ .001.
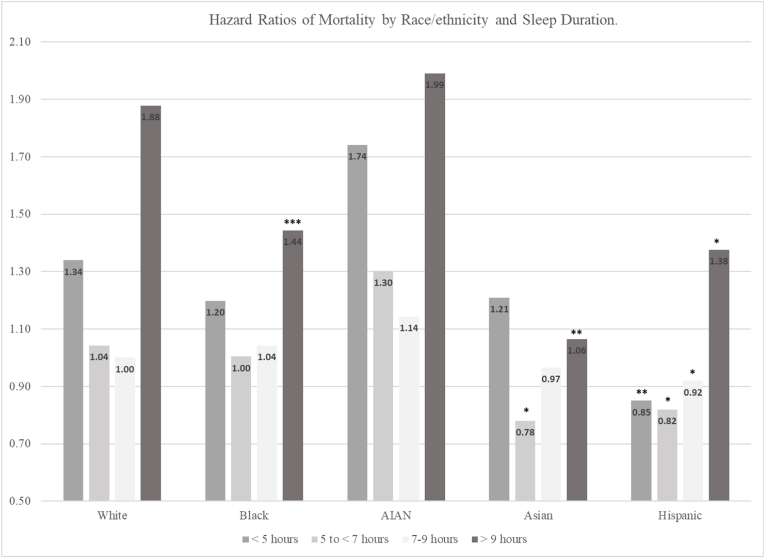
Model 3 in Table 3 provides a fully adjusted model and introduces an interaction between sleep duration and race/ethnicity. The significant interactions suggest that the association between sleeping less than 5 h and mortality risk is significantly less for Hispanic adults, relative to White adults. The association of sleeping between 5 and less than 7 h and mortality risk is significantly less for Asian and Hispanic adults, compared to White adults. The association between sleeping more than 9 h and mortality risk is significantly less for Black, Asian, and Hispanic adults, compared to White adults.
Fig. 2 uses the information from Model 3 in Table 3 to calculate the hazard ratios (HR) for each racial/ethnic group by sleep duration. As an illustration, for Blacks who sleep greater than 9 h, the risk of mortality is higher (HR = (1.88*1.04*0.74) = 1.44), but it is significantly lower than that of Whites who sleep greater than 9 h (HR = 1.88). We know that the risk of mortality is significantly lower than that of Whites by the significance of the interaction HR in Model 3 of Table 3 for Blacks (HR = 0.74; p ≤ .001). Risks for AIAN people in Fig. 2 appear elevated at every level of sleep duration, compared to Whites, but those risks do not reach statistical significance, partially due to the elevated standard errors for the AIAN estimates in Table 3 as a result of a smaller sample and small number of deaths among AIAN people in the dataset. In other words, none of the statistical interactions in Table 3, Model 3 for AIAN people reached significance. Asian adults have statistically significantly lower risks from Whites in the 5 to less than 7 h and the greater than 9 h groups. Hispanics have significantly lower risks of death from Whites in every category. As an illustration, compared to Whites who sleep 5 to less than 7 h (HR = 1.04), the risk of mortality is significantly lower for Asians (HR = (1.04*0.97*0.77) = 0.78) and Hispanics (HR = (1.04*0.92*0.85) = 0.82). As another illustration, compared to Whites who sleep greater than 9 h (HR = 1.88), the hazard ratio of mortality for Asians (HR = (1.88*0.97*0.59) = 1.06) and Hispanics (HR = (1.88*0.92*0.80) = 1.38) is statistically significantly lower.
Fig. 2.
Hazard Ratios of Mortality by Race/ethnicity and Sleep Duration.
Notes: Hazard ratios presented are calculated using the regression equation from Table 3, Model 3. Significance is indicated based on the interactions in Model 3, Table 3. *p ≤ .05; **p ≤ .01; ***p ≤ .001.
5.5. Supplementary analyses
To examine whether the results presented for all-cause mortality showed different patterns for cause-specific mortality, we examined links between sleep duration and race/ethnicity for cardiovascular disease (CVD) deaths and cancer deaths. The number of deaths for cause-specific analyses were considerably smaller—3342 CVD deaths and 5483 cancer deaths. The cause-specific mortality results are quite similar to the all-cause mortality results and are available in Supplementary Tables 1 and 2.
6. Discussion
Current evidence on the association between sleep duration and health across racial and ethnic groups is limited. This study used data from a large, nationally representative sample of U.S. adults, linked to prospective mortality status, to measure the association between sleep duration and all-cause mortality and the extent to which this association varies by several racial and ethnic groups.
First, across the entire sample, we find that there are elevated risks of mortality from any cause for adults who sleep less than 7 h—particularly for those who sleep less than 5 h—or more than 9 h in a 24-h period. This increased risk is robust to adjustments for relevant sociodemographic, SES, and psychological distress covariates. Adjusted risks of death from any cause for adults who sleep greater than 9 h are particularly troubling—over 1.7 times that of adults who sleep the recommended 7–9 h. These results are consistent with previous studies (Cappuccio et al., 2010; da Silva et al., 2016).
Second, we find evidence that the association between sleep duration and mortality varies by racial and ethnic identity. Based on previous research on risk factors for mortality (Williams, 2012; Williams et al., 2010), we expected that short and long sleep duration might represent a greater risk factor for racial and ethnic minorities. We found in many but not all cases that shorter and longer sleep was a greater risk factor for Whites than for many of the other racial and ethnic minority groups.
More data and research are needed to clarify pathways and determine the extent to which sleep duration associates with mortality risk for minority populations. Researchers might start by gaining a better understanding of sleep health across several racial/ethnic groups. For instance, what are the reasons behind disparities in sleep duration? Inadequate sleep for some could be grounded in employment or other socioeconomic disadvantages, while inadequate sleep for others may be related to important and beneficial familial relationships and responsibilities (Braveman et al., 2011; C. L. Jackson et al., 2020; J. W. Jackson et al., 2016; Olshansky et al., 2012). The former is harmful for health, while the latter may hold some benefits for health status rooted in important mechanisms related to social networks and social support (Berkman & Glass, 2000). Drawing on the recent work by Hale et al. (2020), future research on racial/ethnic differences in sleep health and the link with mortality needs to consider important factors at the individual, social, and contextual levels. Improved knowledge can then facilitate more effective and culturally-tailored interventions around sleep health, with the potential to improve overall well-being and longevity in all racial/ethnic groups (Joo & Liu, 2021).
Third, we find some evidence that suggests concerns over sleep duration and all-cause mortality should concentrate on the problems associated with longer rather than shorter sleep duration, at least for some groups. Though inadequate sleep, particularly sleeping less than 5 h, may be associated with higher risk of mortality among some groups (i.e., Whites), it may have less to do with mortality risk among other groups (i.e., Hispanics). However, sleeping longer than 9 h may increase risk among most adults, although the degree of risk varies. This variation in risk suggests that future studies need to consider both the role of race/ethnicity, as well as the potential contributions of the social determinants of health, in the link between sleep duration and mortality. Indeed, this may help elucidate some of the differences we report on here. Asian and Hispanic adults in our sample do not follow the higher mortality risk patterns of other groups, particularly that of Whites and Blacks. These associations with regard to sleep and mortality follow well-established patterns in the general mortality literature (Olshansky et al., 2012). Researchers cite a Hispanic paradox for lower Hispanic mortality, given the relatively low mortality in spite of socioeconomic deficits for Hispanics (Ruiz et al., 2013).
This study has important limitations. First, our sleep duration data is all self-reported, so we do not know whether respondents might have misrepresented their actual sleep amounts. Future research combining self-reported and objective sleep data is needed to assess potential respondent bias. Second, health behavioral controls, such as smoking, alcohol consumption, and physical activity are important considerations in establishing associations between sleep and mortality. However, these measures are only available in the Sample Adult File of the NHIS. To include them here would substantially limit our sample size and our ability to include such diverse racial and ethnic groups. Related to this, our sample might have already been underpowered to fully elaborate on the association between sleep duration and mortality in some specific groups, such as AIAN people, which is unfortunate given the disproportionate burden of disease in this racial/ethnic group (Breathett et al., 2020). We did conduct power analyses and found that with over 1300 AIAN people we could detect HRs of 1.70 or larger at power of 0.8 and a significance level of 0.05 in this study (available upon request). However, future studies on sleep health disparities should oversample minority populations to allow fully powered comparisons across racial/ethnic groups.
Despite these limitations, this study contributes to the literature on sleep duration, mortality, and health disparities, in at least three ways using a large, diverse, and nationally representative sample. First, inadequate sleep, particularly less than 5 h in a 24-h period, may have consequences for mortality that are greater than sleeping 5–7 h. Second, long sleep duration, i.e., greater than 9 h, may have larger consequences for mortality than inadequate sleep. And third, we show that the association between sleep duration and mortality varies substantially across racial/ethnic groups. Longitudinal data and objective sleep data are needed to track the association between sleep duration and all-cause mortality over the life course in all racial/ethnic groups. Addressing this gap in the literature is critical to design interventions that can effectively use sleep duration to extend longevity and improve quality of life in all racial/ethnic groups.
Ethical statement
Hereby, I, Justin Denney, consciously assure that for the manuscript, Race/ethnicity, Sleep Duration, and Mortality Risk in the United States, the following is fulfilled:
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
5)
The results are appropriately placed in the context of prior and existing research.
-
6)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
7)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
CRediT author statement
Justin Denney: Conceptualization, Data Curation, Methodology, Formal analysis, Writing- Original draft preparation, Writing- Review & Editing.
Anna Zamora-Kapoor: Conceptualization, Methodology, Writing- Original draft preparation, Writing- Review & Editing.
Devon A. Hansen: Conceptualization, Writing- Original draft preparation, Writing- Review & Editing.
Paul Whitney: Conceptualization, Methodology, Writing- Original draft preparation, Writing- Review & Editing.
Declaration of competing interest
The authors have no conflicts or financial interests to disclose.
Footnotes
We thank the Health Equity Research Center (HERC) at Washington State University for supporting this research. The research was supported by a 2021 Pilot Program Grant from HERC.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101350.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Akerstedt T., Ghilotti F., Grotta A., Bellavia A., Lagerros Y.T., Bellocco R. Sleep duration, mortality and the influence of age. European Journal of Epidemiology. 2017;32:881–891. doi: 10.1007/s10654-017-0297-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison P.D. Sage Publications; Beverly Hills, CA: 1984. Event history analysis: Regression for longitudinal event data. [Google Scholar]
- Berkman L.F., Glass T. In: Social epidemiology. Berkman L.F., Kawachi I., editors. Oxford University Press; Oxford: 2000. Social integration, social networks, social support, and health; pp. 137–173. [Google Scholar]
- Blewett L.A., Rivera Drew J.A., King M.L., Williams K.C.W., Del Ponte N., Convey P. In: IPUMS health surveys: National health Interview survey. Minnesota U.o., editor. 2021. https://nam11.safelinks.protection.outlook.com/?url=https%3A%2F%2Fnhis.ipums.org%2Fnhis%2F&data=05%7C01%7Ct.deenthayalan%40elsevier.com Minneapolis, MN. [Google Scholar]
- Braveman P., Egerter S., Williams D.R. The social determinants of health: Coming of age. Annual Review of Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Breathett K., Sims M., Gross M., Jackson E.A., Jones E.J., Navas-Acien A., et al. Cardiovascular health in American Indians and Alaska natives: A scientific statement from the American heart association. Circulation. 2020;141:e948–e959. doi: 10.1161/CIR.0000000000000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M.J., Spruill T.M., Johnson D.A., Redline S., Sims M., Jenkins B.C., et al. Suboptimal sleep and incident cardiovascular disease among African Americans in the Jackson Heart Study (JHS) Sleep Medicine. 2020;76:89–97. doi: 10.1016/j.sleep.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio F.P., D'Elia L., Strazzullo P., Miller M.A. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chattu V.K., Chattu S.K., Spence D.W., Manzar M.D., Burman D., Pandi-Perumal S.R. Do disparities in sleep duration among racial and ethnic minorities contribute to differences in disease prevalence? J Racial Ethn Health Disparities. 2019;6:1053–1061. doi: 10.1007/s40615-019-00607-7. [DOI] [PubMed] [Google Scholar]
- Grandner M.A. Sleep, health, and society. Sleep Med Clin. 2017;12:1–22. doi: 10.1016/j.jsmc.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner M.A., Chakravorty S., Perlis M.L., Oliver L., Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Medicine. 2014;15:42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner M.A., Williams N.J., Knutson K.L., Roberts D., Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Medicine. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L., Troxel W., Buysse D.J. Sleep health: An opportunity for public health to address health equity. Annual Review of Public Health. 2020;41:81. doi: 10.1146/annurev-publhealth-040119-094412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel P.T. Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology. 2007;37:83–117. [Google Scholar]
- Jackson C.L., Walker J.R., Brown M.K., Das R., Jones N.L. A workshop report on the causes and consequences of sleep health disparities. Sleep. 2020;43:1–11. doi: 10.1093/sleep/zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J.W., Williams D.R., VanderWeele T.J. Disparities at the intersection of marginalized groups. Social Psychiatry and Psychiatric Epidemiology. 2016;51:1349–1359. doi: 10.1007/s00127-016-1276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joo J.Y., Liu M.F. Culturally tailored interventions for ethnic minorities: A scoping review. Nursing open. 2021;8:2078–2090. doi: 10.1002/nop2.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., et al. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Green J.G., Gruber M.J., Sampson N.A., Bromet E., Cuitan M., et al. Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO world mental health (WMH) survey initiative. International Journal of Methods in Psychiatric Research. 2010;19:4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurina L.M., McClintock M.K., Chen J.-H., Waite L.J., Thisted R.A., Lauderdale D.S. Sleep duration and all-cause mortality: A critical review of measurement and associations. Annals of Epidemiology. 2013;23:361–370. doi: 10.1016/j.annepidem.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T.Z., Xu C., Rota M., Cai H., Zhang C., Shi M.J., et al. Sleep duration and risk of all-cause mortality: A flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Medicine Reviews. 2017;32:28–36. doi: 10.1016/j.smrv.2016.02.005. [DOI] [PubMed] [Google Scholar]
- McGrath R.P., Al Snih S., Markides K.S., Faul J.D., Vincent B.M., Hall O.T., et al. The burden of health conditions across race and ethnicity for aging Americans: Disability-adjusted life years. Medicine. 2019;98 doi: 10.1097/MD.0000000000017964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirel L.B., El Bural Felix S., Zhang C., Golden C., Cox C.S. Natl Health Stat Report; 2020. Comparative analysis of the national health Interview survey public-use and restricted-use linked mortality files. [PubMed] [Google Scholar]
- Olshansky S.J., Antonucci T., Berkman L., Binstock R.H., Boersch-Supan A., Cacioppo J.T., et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs. 2012;31:1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- Ramar K., Malhotra R.K., Carden K.A., Martin J.L., Abbasi-Feinberg F., Aurora R.N., et al. Sleep is essential to health: An American Academy of sleep medicine position statement. Journal of Clinical Sleep Medicine, 2021;17:2115–2119. doi: 10.5664/jcsm.9476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R.G., Hummer R.A., Nam C.B. Academic Press; New York: 2000. Living and dying in the USA: Behavioral, health, and social differentials of adult mortality. [Google Scholar]
- Ruiz J.M., Steffen P., Smith T.B. Hispanic mortality paradox: A systematic review and meta-analysis of the longitudinal literature. American Journal of Public Health. 2013;103:e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sands‐Lincoln M., Grandner M., Whinnery J., Keenan B.T., Jackson N., Gurubhagavatula I. The association between obstructive sleep apnea and hypertension by race/ethnicity in a nationally representative sample. Journal of Clinical Hypertension. 2013;15:593–599. doi: 10.1111/jch.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan Z., Ma H., Xie M., Yan P., Guo Y., Bao W., et al. Sleep duration and risk of type 2 diabetes: A meta-analysis of prospective studies. Diabetes Care. 2015;38:529–537. doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- da Silva A.A., de Mello R.G., Schaan C.W., Fuchs F.D., Redline S., Fuchs S.C. Sleep duration and mortality in the elderly: A systematic review with meta-analysis. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-008119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . Vol. 16. Stata Corporation; College Station, TX: 2019. (Stata statistical software: Release). [Google Scholar]
- Tao F., Cao Z., Jiang Y., Fan N., Xu F., Yang H., et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: A prospective cohort study of 407,500 UK biobank participants. Sleep Medicine. 2021;81:401–409. doi: 10.1016/j.sleep.2021.03.015. [DOI] [PubMed] [Google Scholar]
- Whinnery J., Jackson N., Rattanaumpawan P., Grandner M.A. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–611. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior. 2012;53:279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioecnomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zizi F., Pandey A., Murrray-Bachmann R., Vincent M., McFarlane S., Ogedegbe G., et al. Race/ethnicity, sleep duration, and diabetes mellitus: Analysis of the national health Interview survey. The American Journal of Medicine. 2012;125:162–167. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.