Abstract
Background
People with multimorbidity, defined as the co-existence of two or more chronic conditions in an individual, often suffer from pain and functional limitations caused by musculoskeletal disorders and the chronic conditions. In chiropractic practice, two thirds of patients are treated for low back pain (LBP). It is unknown to what extent LBP is accompanied with chronic conditions in chiropractic practice. The objective was to determine the prevalence of multimorbidity among patients with LBP in chiropractric practice and to investigate if multimorbidity affects pain intensity, self-rated health, physical and mental health. Finally, to explore if individuals with multimorbidity have a different recovery for the LBP.
Methods
Patients presenting with a new episode of LBP were recruited from 10 chiropractic clinics in 2016–2018. Patient-reported data concerning socio-demographics, self-rated health, pain intensity, history of LBP, mental health and chronic conditions were collected at baseline. The prevalence of multimorbidity was determined. To evaluate differences in recovery from the LBP, we estimated changes in the Roland Morris Disability Questionnaire (RMDQ) score and use of pain medication at baseline, 2 weeks, 3 months and 12 months. The analyses were adjusted using regression models.
Results
2083 patients were included at baseline and 71%, 68% and 64% responded to follow-up questionnaires at 2 weeks, 3 and 12 months. 1024 (49%) participants reported to have at least one chronic condition and 421 (20%) had multimorbidity (≥ 2 chronic conditions). The presence of multimorbidity was associated with increased odds of poor self-rated health (OR 2.13), physical fitness (OR 1.79), poor muscular strength (OR 1.52), poor endurance (OR 1.51), and poor balance (OR 1.33). Patients with high LBP intensity combined with multimorbidity showed a poorer recovery than patients without chronic diseases (mean difference in RMDQ score 3.53 at 12 months follow-up). More patients with multimorbidity used pain medication for LBP at 12 months follow-up compared to those without chronic disease (OR 2.36).
Conclusions
Chiropractors should be aware that patients with LBP may suffer from multimorbidity with poor general health. Patients with multimorbidity also have poorer recovery from LBP than people without chronic disease and clinical follow-up may be indicated.
Keywords: Chiropractor, Low back pain, Multimorbidity, Recovery
Background
Multimorbidity is defined as the co-existence of two or more chronic conditions in an individual [1]. Estimates of the prevalence of multimorbidity in people presenting in primary care range from 13% in individuals aged 18 years and older to 95% in a population aged 65 years and older [2], and is projected to become more prevalent as the population ages [3]. Chronic musculoskeletal disorders include degenerative conditions, such as osteoarthritis, inflammatory rheumatic diseases, such as rheumatoid arthritis; fragility conditions, such as osteoporosis; and regional pain syndromes, such as low back pain (LBP), neck pain and fibromyalgia. A substantial proportion of people with musculoskeletal disorders live with multimorbidity [4–6]. People with multimorbidity often suffer from pain and functional limitations caused by musculoskeletal disorders in combination with their other chronic conditions [7]. Musculoskeletal disorders are present in patients with multimorbidity because of their high prevalence, shared risk factors, and shared pathogenic processes amongst other long-term conditions. Such musculoskeletal issues are often associated with decreased ability to work and lower quality of life [7].
Chiropractors are a part of primary care in Denmark and may therefore play an important role for patients with multimorbidity in regaining mobility and reducing pain. Chiropractors in Denmark are self-employed, and almost all clinics (94%) operate under the agreement between the Danish Chiropractor’s Association and the Danish Regions, and for most services, 20% is paid by the region and 80% by the patient directly or by a private health insurance [8]. In chiropractic practice, approximately two thirds of patients are treated for LBP [9, 10]. While it is known that LBP can be associated with co-morbidity [11, 12], it is unknown to what extend LBP is accompanied with chronic conditions and contribute to multimorbidity in chiropractic practice. Recognition, by health professionals, policymakers, non-profit organizations, and research funders, of the impact of multimorbidity in musculoskeletal health is essential when planning support for these patients. However, is it currently unknown to what extend chiropractors treat patients with multimorbidity and how this affects the patients and the clinical course of back pain.
The aim of this paper was therefore to determine the prevalence of multimorbidity among patients with LBP seeking care in chiropractic practice. Secondly, to investigate if the presence of multiple chronic conditions affects pain intensity, self-rated health, mental and physical health. Finally, to explore if individuals with multimorbidity have a different recovery for their LBP problem than individuals without multimorbidity.
Methods
The Danish Chiropractic Low Back Pain Cohort (ChiCo) is a longitudinal observational cohort consisting of adults seeking care for LBP at 10 chiropractic clinics from the Central Denmark Region [8]. Only medium or large size clinics were invited to ensure adequate recruitment of study participants within a reasonable timeframe. Patients were recruited consecutively from November 2016 to December 2018 and followed until 12 months after enrolment. The Regional Research Ethics Committee determined that ChiCo did not require ethical approval because of the absence of a study-initiated clinical intervention. [Project-id: S-20162000-109]. All participants provided written informed consent prior to enrolment.
Participants
Patients presenting in chiropractic clinics with a new episode of LBP with or without leg pain, aged 18 years or older, and who were able to complete electronic questionnaires in Danish were eligible for inclusion. A new episode of LBP was defined as consulting with LBP without this being a follow-up consultation as part of an already initiated course of treatment. Patients with a non-musculoskeletal cause of the LBP were excluded [8].
Data collection
All patient-reported data (baseline and follow-up) were collected using electronic questionnaires in REDCap (https://www.project-redcap.org/). To minimize the time for completing questionnaires in the waiting room prior to the consultation, the baseline questionnaire for the ChiCo cohort was split into two separate questionnaires. The first baseline questionnaire (BL1) was completed by the patients before meeting the chiropractor, i.e., in the waiting area. The second baseline questionnaire (BL2) was sent to the patient by email to be completed on the same day after the consultation. Non-responders to BL2 received an electronic reminder after two days. Data on chronic diseases were reported in BL2. As such, only participants who completed both BL1 and BL2 were included in the current analysis. Follow-up questionnaires were collected at 2 weeks, 3 months, and 12 months after inclusion. The data collection procedures are described in detail elsewhere [8].
Patient-reported information
Baseline information on included participants comprise demographics, education and work situation. (Table 1). Overall self-rated health was assessed using a single item with responses from 1, “excellent” to 5, “poor”. Participants then completed a question about their history of chronic conditions, namely: “Did a medical doctor ever tell you that you have or have had [list of 15 chronic conditions]?” The 15 chronic conditions were diabetes, osteoporosis, thrombus (in the hearth, brain or elsewhere), hypertension, psoriasis, rheumatoid arthritis, osteoarthritis, fibromyalgia, metabolic diseases, asthma, migraine, chronic inflammatory bowel disease, cancer, chronic obstructive pulmonary disease or bronchitis, and neurological disease. This method has previously been used in large Danish cohort studies such as in The Danish Twin Registry and applied in analyses relating to back pain in young [13] and older people [14] and radiating spinal pain as risk factor for work disability [15].
Table 1.
Baseline characteristics
| Total | Missing | LBPf Intensity < 7a | LBP Intensity ≥ 7a | p-valuee | |
|---|---|---|---|---|---|
| (n = 2083) | (n = 1217) | (n = 825) | |||
| Sex, n (%) | 0 | ||||
| Male | 1165 (55.9) | 719 (62.9) | 424 (37.1) | 0.0006 | |
| Female | 918 (44.1) | 498 (55.4) | 401 (44.6) | ||
| Age, mean (sd) | 46.07 (13.50) | 0 | 44.74 (13.61) | 46.16 (13.28) | 0.4852 |
| BMI, n (%) | 11 | 0.0122 | |||
| ≤ 25 kg/m2 | 853 (41.2) | 521 (61.9) | 321 (38.1) | ||
| 26–29 kg/m2 | 776 (37.5) | 460 (60.9) | 296 (39.2) | ||
| ≥ 30 kg/m2 | 443 (21.4) | 232 (53.6) | 201 (46.4) | ||
| Smoker, n (%) | 4 | 0.0036 | |||
| Yes | 336 (16.2) | 171 (51.4) | 162 (48.7) | ||
| No, I have stopped smoking | 711 (34.2) | 427 (61.8) | 264 (38.2) | ||
| No, I have never smoked | 1031 (49.6) | 615 (60.7) | 399 (39.4) | ||
| Education n (%) | 61 | 0.0878 | |||
| None | 313 (15.5) | 179 (58.7) | 126 (41.3) | ||
| Vocational or short education | 848 (42.0) | 481 (57.7) | 353 (42.3) | ||
| Middle further education | 553 (27.4) | 320 (58.9) | 223 (41.1) | ||
| University degree | 233 (11.5) | 152 (66.7) | 76 (33.3) | ||
| Other | 74 (3.7) | 48 (67.6) | 23 (32.4) | ||
| Working, n (%) | 32 | 0.1664 | |||
| Yes | 1683 (82.1) | 973 (58.8) | 681 (41.2) | ||
| No | 368 (17.9) | 226 (62.8) | 134 (37.2) | ||
| Pain intensitya, mean (sd) | |||||
| Lower back pain (LBP) | 6.70 (2.02) | 41 | 5.45 (1.62) | 8.55 (0.73) | – |
| Leg pain | 3.04 (2.94) | 44 | 2.51 (2.62) | 3.84 (3.22) | < 0.0001 |
| LBP duration, n (%) | 13 | < 0.0001 | |||
| 1–7 days | 961 (46.4) | 464 (22.9) | 476 (23.5) | ||
| 1 week–3 months | 743 (35.9) | 479 (23.6) | 255 (12.6) | ||
| 3–12 months | 152 (7.3) | 113 (5.6) | 35 (1.7) | ||
| 12 + months | 214 (10.3) | 152 (7.5) | 56 (2.8) | ||
| Medication for LPB, n (%) | 39 | < 0.0001 | |||
| Yes, prescription medication | 355 (17.4) | 142 (40.6) | 208 (59.4) | ||
| Yes, non-prescription medication | 686 (33.6) | 357 (53.6) | 309 (46.4) | ||
| No | 1002 (49.1) | 692 (70.2) | 294 (29.8) | ||
| Roland Morris Disability Questionnaireb, mean (sd) | 12.72 (5.45) | 155 | 10.92 (5.33) | 15.40 (4.39) | < 0.0001 |
| Mental healthc, mean (sd) | |||||
| Depressed | 3.02 (3.96) | 31 | 2.70 (2.76) | 3.52 (3.16) | < 0.0001 |
| Stressed/anxious | 3.85 (2.95) | 25 | 3.62 (2.85) | 4.22 (3.08) | < 0.0001 |
| Muskuloskeletal pain, n (%) | |||||
| Head | 726 (34.9) | 0 | 415 (57.7) | 304 (42.3) | 0.2068 |
| Neck | 910 (43.7) | 0 | 519 (58.1) | 375 (42.0) | 0.2152 |
| Chest | 116 (5.6) | 0 | 65 (56.0) | 51 (44.0) | 0.4232 |
| Stomach | 240 (11.5) | 0 | 130 (54.2) | 110 (45.8) | 0.0689 |
| Shoulders | 850 (40.8) | 0 | 496 (59.5) | 337 (40.5) | 0.9788 |
| Elbows | 147 (7.1) | 0 | 86 (59.7) | 58 (40.3) | 0.9709 |
| Arms | 217 (10.4) | 0 | 117 (55.2) | 95 (44.8) | 0.1688 |
| Hands | 235 (11.3) | 0 | 122 (52.8) | 109 (47.2) | 0.0261 |
| Hips | 552 (26.5) | 0 | 306 (56.9) | 232 (43.1) | 0.1368 |
| Knees | 558 (26.8) | 0 | 314 (57.4) | 233 (42.6) | 0.2258 |
| Legs | 502 (24.1) | 0 | 287 (58.6) | 203 (41.4) | 0.6022 |
| Feet | 371 (17.8) | 0 | 219 (60.5) | 143 (39.5) | 0.6946 |
| Other | 90 (4.3) | 0 | 65 (73.9) | 23 (26.1) | 0.0052 |
| No pain | 337 (16.2) | 0 | 205 (62.1) | 125 (37.9) | 0.3040 |
| Self-rated general health, n (%) | 639 | 0.0037 | |||
| Excellent | 221 (15.3) | 135 (63.1) | 79 (36.9) | ||
| Very good | 604 (41.9) | 369 (62.1) | 225 (37.9) | ||
| Fine | 378 (26.2) | 217 (58.3) | 155 (41.7) | ||
| Fair | 204 (14.1) | 104 (51.5) | 98 (48.5) | ||
| Poor | 36 (2.49) | 13 (37.1) | 22 (62.9) | ||
| Physical ressourcesd, mean (sd) | |||||
| Aerobic fitness | 5.17 (1.86) | 58 | 5.27 (1.80) | 4.99 (1.93) | 0.0007 |
| Muscular strength | 5.86 (1.71) | 57 | 5.88 (1.63) | 5.81 (1.81) | 0.3778 |
| Endurance | 5.71 (1.90) | 59 | 5.78 (1.83) | 5.61 (2.00) | 0.0548 |
| Flexibility | 5.00 (1.95) | 60 | 5.04 (1.87) | 4.92 (2.05) | 0.1544 |
| Balance | 5.65 (1.87) | 60 | 5.66 (1.79) | 5.64 (1.99) | 0.7751 |
aPain was rated on numeric rating scales (NRS) 0–10 (higher score indicating worse pain)
bThe Roland Morris Disability Questionnaire 0–23 (higher score indicating more disability)
cMental health was assessed by the Örebro Musculoskeletal Pain Screening Questionnaire 0–10 (higher score indicating worse mental health)
dPhysical resources was assessed on a visual analog scale from 1 (poor) to 9 (excellent)
ep-value of a chi-squared test (categorical variables) or t-test (continuous variables)
Multimorbidity was defined as the presence of two or more of these chronic conditions [1].
Pain intensity was rated progressively 0–10 on numeric rating scales [NRS] for LBP and leg pain separately [16], and participants were asked about duration of current episode, use of pain medications for LBP, and number of days with LBP within the past year. Participants also reported recent musculoskeletal pain other than LBP. Physical function was measured by assessing activity limitation due to LBP [Roland Morris 23-item Disability Questionnaire [RMDQ]] [16, 17], and self-perceived physical resources including physical fitness, muscle strength, endurance, flexibility and balance [18]. Information collected about mental health included feeling depressed or stressed as assessed by the Örebro Musculoskeletal Pain Screening Questionnaire [19].
Data analysis
Frequencies of demographic variables at baseline were grouped by intensity of LBP (NRS ≥ 7 vs. < 7) and compared using Chi-squared tests. To facilitate comparisons, we dichotomized each outcome variable. Cut points for dichotomization were chosen based on the distribution of the data or according to the scoring of each instrument. High intensity of LBP was defined as NRS ≥ 7 [20]. This intensity of LBP cut-off was used to report frequencies of demographic variables at baseline and compared using Chi-squared tests. Low self-rated health was defined as a score of ≥ 4 indicating fair or poor health. The thresholds for poor mental and physical health and ability to do everyday activities were set at the poorest quartile in the dataset. Logistic regression models were fitted and odds ratios (ORs) and corresponding 95% confidence intervals (95% CIs) were reported adjusting for age, BMI, sex, smoking status, employment status, cohabitation, education, pain duration, and presence of other musculoskeletal pain.
To evaluate differences in recovery from the LBP problem, we evaluated the RMDQ score and use of pain medication across the four time points grouped by chronic disease variables. For the RMDQ score, we reported differences in mean score, with 95% confidence intervals and p-values, from a linear regression model fitted with generalized estimating equation (GEE) to account for repeated observations on the same individuals and the weighting procedure described below. For pain medication, we reported odds ratios with 95% confidence intervals and p-values from a logistic regression model fitted with GEE. Weights were used to adjust for differential dropout [21]. The weights were calculated by inverse probability and estimated using age, BMI, number of children, sex, smoking status, employment status, cohabitation, chronic disease variables, education, pain duration, presence of other musculoskeletal pain, chiropractic clinic, treatment received by other practitioners (i.e., physical therapist), self-rated health, and physical resources. All these analyses were performed adjusting for age, BMI, sex, smoking status, employment status, cohabitation, education, pain duration, and presence of other musculoskeletal pain. All analyses were carried out in the SAS 9.4 statistical package. The significance level was set at p < 0.01.
Results
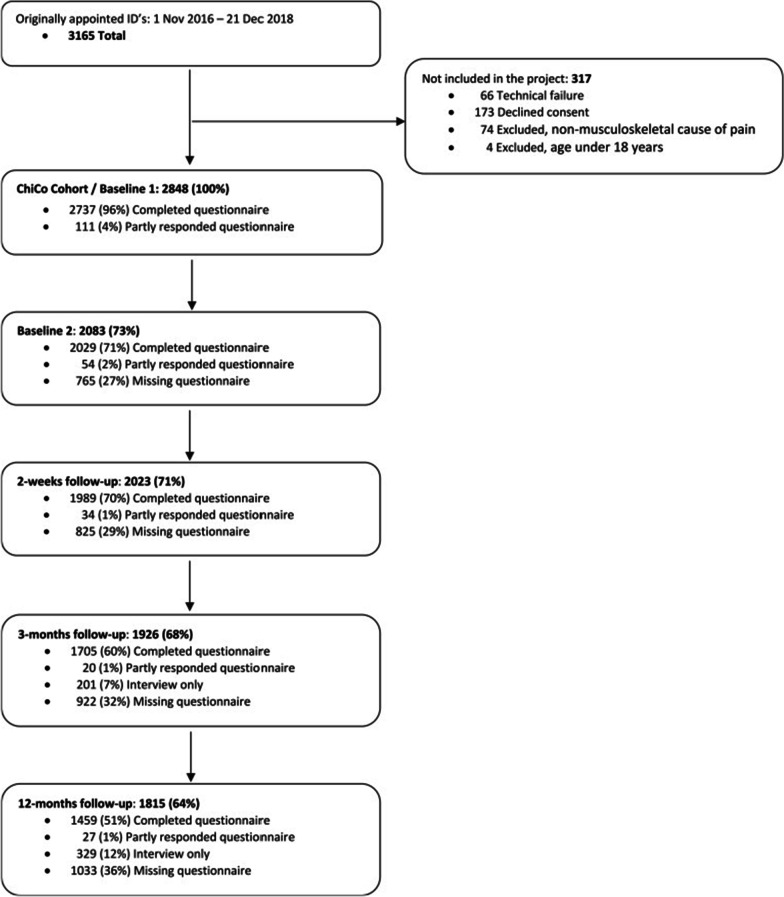
A total of 2848 patients consented of whom 2083 (74%) completed both the BL1 and BL2 and were included in the analysis. Of the consenting patients 71%, 68% and 64% responded to follow-up questionnaires at 2 weeks, 3 months and 12 months. (Fig. 1: Flow chart). Most participants were males (56%) with an average age of 46 (SD 13) years (Table 1). The most common chronic conditions were high blood pressure (19%) and osteoarthritis (15%) (Table 2).
Fig. 1.
Flow chart
Table 2.
Prevalence of chronic disease among patients with LBP at baseline (n = 2083)
| Disease | Prevalence (%) |
|---|---|
| Diabetes | 73 (3.5) |
| Osteoporosis | 33 (1.6) |
| Stroke/heart attack | 81 (3.9) |
| High blood pressure | 395 (19.0) |
| Psoriasis | 105 (5.0) |
| Rheumatoid arthritis | 34 (1.6) |
| Osteoarthritis | 305 (14.6) |
| Fibromyalgia | 9 (0.4) |
| Metabolic diseases | 97 (4.7) |
| Asthma | 180 (8.6) |
| Migraine | 182 (8.7) |
| Chronic inflammatory bowel disease | 27 (1.3) |
| Cancer | 79 (3.8) |
| COPD or chronic bronchitis | 42 (2.0) |
| Neurological disease | 16 (0.8) |
| No disease | 890 (42.7) |
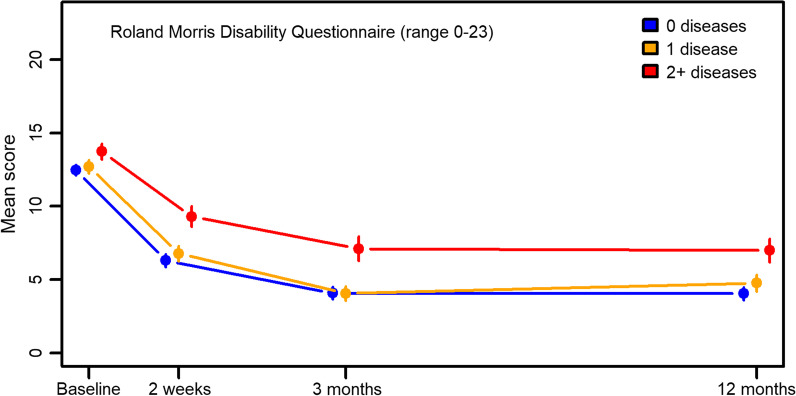
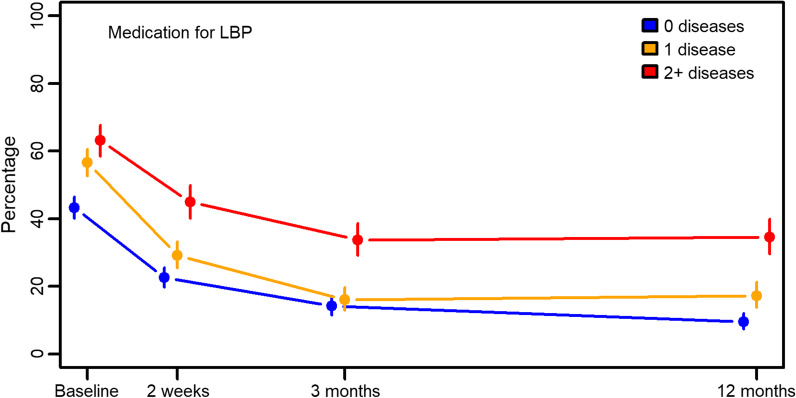
Of the total sample, 1024 (49%) participants reported to have at least one chronic condition and 421 (20%) had multimorbidity (≥ 2 chronic conditions) (Table 3). At baseline, 825 (40%) participants reported high LBP intensity (Table 3). The presence of multimorbidity was associated with increased odds of poor self-rated health (OR 2.13, 95% CI 1.46; 3.11), poor physical fitness (OR 1.79, 95% CI 1.35; 2.38), poor muscular strength (OR 1.52, 95% CI 1.18; 1.96), poor endurance (OR 1.51, 95% CI 1.17; 1.96), and poor balance (OR 1.33, 95% CI 1,03; 1.72) (Table 3). Multimorbidity was not seen to be associated with depression or anxiety (Table 3). All participants regardless of pain intensity at baseline and presence of multimorbidity improved over time and fewer used pain medication (Figs. 2, 3). Patients with high LBP intensity combined with multimorbidity showed a poorer recovery than patients with high LBP intensity but without chronic diseases (mean difference 3.53, 95% CI 1.85; 5.20 at 12 months follow-up) (Table 4, adjusted). A clinical significant change is a score ranging from 2 to 4 points [22]. For patients with low LBP intensity, no such association was present (Table 4, adjusted). More patients with multimorbidity used pain medication for LBP at 12 months follow-up compared to those without chronic disease (OR 2.36 (1.52; 3.66)) (Fig. 3 and Table 4, adjusted).
Table 3.
Impact on physical and mental health of chronic disease and multimorbidity at baseline
| Total | LBP intensity ≥ 7 | Low SRH | Depressed | Stressed anxious | Poor physical fitness | Poor muscular strength | Poor endurance | Poor flexibility | Poor balance | |
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | 2083 (100.00) | 825 (40.40) | 240 (16.63) | 513 (25.00) | 486 (23.62) | 649 (32.07) | 848 (41.88) | 918 (45.38) | 769 (38.03) | 1029 (50.89) |
| Number of diseases | N (%) | OR (95% CI) | ||||||||
| 0 | 1059 (50.8) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (ref) | (Ref) | (Ref) |
| 1 | 603 (29.0) | 1.04 (0.83; 1.31) | 1.25 (0.85; 1.85) | 1.35 (1.05; 1.75) | 1.40 (1.08; 1.82) | 1.30 (1.01; 1.68) | 0.93 (0.74; 1.16) | 1.12 (0.89; 1.40) | 1.11 (0.88; 1.39) | 1.08 (0.87; 1.34) |
| 2 | 271 (13.0) | 1.21 (0.88; 1.67) | 1.91 (1.19; 3.09) | 1.31 (0.91; 1.89) | 0.99 (0.67; 1.45) | 1.82 (1.29; 2.57) | 1.37 (1.00; 1.86) | 1.49 (1.09; 2.04) | 1.30 (0.95; 1.78) | 1.34 (0.98; 1.82) |
| 3 | 109 (5.2) | 1.42 (0.89; 2.27) | 3.34 (1.76; 6.32) | 1.17 (0.69; 1.99) | 1.25 (0.73; 2.15) | 2.39 (1.46; 3.93) | 1.51 (0.95; 2.37) | 1.76 (1.10; 2.82) | 1.09 (0.69; 1.73) | 1.39 (0.88; 2.19) |
| 4 | 29 (1.4) | 1.16 (0.51; 2.66) | 6.00 (1.99; 18.07) | 0.70 (0.24; 2.00) | 0.96 (0.33; 2.77) | 6.06 (2.42; 15.18) | 3.40 (1.41; 8.19) | 2.70 (1.11; 6.58) | 1.90 (0.85; 4.23) | 1.43 (0.63; 3.24) |
| 5+ | 12 (0.6) | 0.60 (0.13; 2.73) | 1.81 (0.36; 9.17) | 0.11 (0.01; 1.25) | 0.16 (0.02; 1.50) | 0.88 (0.22; 3.37) | 0.95 (0.27; 3.37) | 1.40 (0.33; 5.88) | 0.77 (0.21; 2.82) | 5.18 (0.70; 47.94) |
| Multimorbidity (≥ 2 diseases) | ||||||||||
| No | 1662 (79.8) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) |
| Yes | 421 (20.2) | 1.22 (0.93; 1.59) | 2.13 (1.46–3.11) | 1.02 (0.76; 1.39) | 0.86 (0.63; 1.18) | 1.79 (1.35; 2.38) | 1.52 (1.18; 1.96) | 1.51 (1.17; 1.96) | 1.20 (0.93; 1.56) | 1.33 (1.03; 1.72) |
| Missing | 0 | 41 | 640 | 31 | 25 | 59 | 58 | 60 | 61 | 61 |
Fig. 2.
Roland Morris 23-item Disability Questionnaire (RMDQ) score
Fig. 3.
Medication for low back pain (LBP) k pain (LBP).
Table 4.
Roland Morris Questionnaire score and pain medication in relation to multimorbidity and chronic disease (adjusted)
| Baseline | 2 weeks | 3 months | 12 months | |||||
|---|---|---|---|---|---|---|---|---|
| Difference (95%CI) | p-value | Difference (95%CI) | p-value | Difference (95%CI) | p-value | Difference (95%CI) | p-value | |
| Roland Morris Questionnaire | ||||||||
| Total | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | (Ref) | ||||
| 1 disease | − 0.18 (− 0.74; 0.39) | 0.535 | 0.16 (− 0.54; 0.86) | 0.653 | − 0.33 (− 1.11; 0.45) | 0.411 | 0.49 (− 0.37; 1.35) | 0.259 |
| 2+ diseases | − 0.11 (− 0.79; 0.58) | 0.760 | 1.42 (0.59; 2.25) | 0.001 | 1.30 (0.31; 2.29) | 0.010 | 1.46 (0.39; 2.52) | 0.007 |
| LBP intensity < 7 | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | (Ref) | ||||
| 1 disease | 0.21 (− 0.53; 0.96) | 0.575 | − 0.34 (− 1.19; 0.52) | 0.440 | − 0.75 (− 1.70; 0.19) | 0.118 | − 0.08 (− 1.07; 0.90) | 0.866 |
| 2+ diseases | 0.74 (− 0.18; 1.67) | 0.117 | 1.04 (− 0.05; 2.13) | 0.063 | 0.12 (− 1.13; 1.37) | 0.849 | 0.38 (− 0.96; 1.72) | 0.581 |
| LBP intensity ≥ 7 | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | (Ref) | ||||
| 1 disease | − 1.03 (− 1.84; − 0.22) | 0.013 | 1.20 (− 0.01; 2.41) | 0.051 | 0.61 (− 0.67; 1.90) | 0.3493 | 1.62 (0.18; 3.07) | 0.0274 |
| 2+ diseases | − 1.57 (− 2.54; − 0.58) | 0.002 | 2.38 (1.08; 3.69) | < .001 | 3.24 (1.71; 4.77) | < .001 | 3.53 (1.85; 5.20) | < .001 |
| Pain medication for LBP | ||||||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | p-value | OR (95%CI) | p-value | OR (95%CI) | p-value | OR (95%CI) | p-value | |
| Total | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | |||||
| 1 disease | 1.45 (1.16; 1.82) | 0.001 | 0.79 (0.59; 1.05) | 0.110 | 0.67 (0.46; 0.99) | 0.043 | 1.19 (0.78; 1.81) | 0.428 |
| 2+ diseases | 1.35 (1.03; 1.79) | 0.032 | 1.15 (0.83; 1.57) | 0.4004 | 1.42 (0.95; 2.11) | 0.0890 | 2.36 (1.52; 3.66) | < .001 |
| LBP intensity < 7 | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | (Ref) | ||||
| 1 disease | 1.44 (1.07; 1.94) | 0.018 | 0.71 (0.48; 1.06) | 0.0940 | 0.64 (0.38; 1.06) | 0.0853 | 1.21 (0.66; 2.22) | 0.529 |
| 2+ diseases | 1.44 (0.99; 2.09) | 0.054 | 1.07 (0.70; 1.65) | 0.7541 | 1.32 (0.78; 2.24) | 0.2966 | 2.43 (1.31; 4.51) | 0.005 |
| LBP intensity ≥ 7 | ||||||||
| 0 diseases | (Ref) | (Ref) | (Ref) | (Ref) | ||||
| 1 disease | 1.38 (0.95; 2.03) | 0.095 | 0.91 (0.58; 1.44) | 0.692 | 0.77 (0.41; 1.41) | 0.394 | 1.13 (0.60; 2.14) | 0.710 |
| 2+ diseases | 1.13 (0.72; 1.78) | 0.594 | 1.44 (0.87; 2.37) | 0.1543 | 2.13 (1.12; 4.02) | 0.0203 | 2.80 (1.44; 5.44) | 0.002 |
Discussion
This is the first manuscript to report on the prevalence and impact of multimorbidity among patients with LBP treated in chiropractic practice. Approximately 20% of patients had multimorbidity, which was associated with poorer self-rated health, physical fitness, muscular strength, endurance, and balance at baseline. In addition, patients with multimorbidity and high LBP intensity had poorer recovery in terms of disability in everyday activities and continued need for pain medication.
In a systematic review from primary care, prevalence rates of multimorbidity of 20–50% were found for patients of similar age as those included in our study. Thus for most settings in primary care, the prevalence of multimorbidity was higher than that observed in the current study (20%) [2]. For people seeking care from chiropractors specifically, not much is known about patterns of multimorbidity. In Australia, Charity et al. studied profiles of patients seeking care from chiropractors for multiple reasons and found that 24% reported circulatory, 24% reported endocrine and metabolic, and 12% reported respiratory comorbidities [23]. These numbers are somewhat higher than ours, which might be explained by the fact that we included only patients presenting with a new episode of LBP and not consecutive patients such as in the Australian study. In Denmark, profiles of people seeking care for LBP in general practice and chiropractors have been compared, and chiropractic patients were fund to be younger, more often males and better on all LBP disease-related parameters [24]. De Luca et al. also found that older Australians who sought care from chiropractors had significantly fewer comorbidities compared to those who sought care from general practitioners [25]. The observed general good health of patients in chiropractic practice may explain the relatively low prevalence of multimorbidity in our study.
Generally, people with multimorbidity and co-occurring musculoskeletal pain report higher levels of disability [12, 26] as well as more mental health problems [27], physical inactivity and obesity [28]. Therefore, it is not surprising that those with multimorbidity report poorer self-rated health in our study. The observed poorer outcomes among patients in this cohort with multimorbidity and high pain levels is to be expected. It is well-known that people with back pain and other musculoskeletal conditions and multimorbidity respond less well to treatments including pharmacological and non-pharmacological interventions as well as surgical treatment [29]. Therefore, the challenge for chiropractors—and indeed for all healthcare professionals who treat people with LBP—is to not view LBP as an isolated regional pain condition but one manifestation of poor health that for many include pain at other body sites as well as disease in other body systems [6, 29]. Chiropractors in Denmark generally have a broad approach to care suited to patients with more complex problems such as people with multimorbidity. It includes patient education, exercise facilities, and promotion of physical activity in addition to more traditional manual treatment. Of the chiropractors in Denmark, 45% work in a multidisciplinary setting with physical therapists [30, 31]. In addition, more than 90% communicate electronically with the broader healthcare system including with general practitioners [31]. In their contract, the chiropractors have special obligations to inform the general practitioner about patients with complex problems, but the quality of this knowledge exchange is unknown.
Strengths and limitations
The cohort is the largest and most comprehensive cohort of patients with LBP seeking care from chiropractors. The participation rates at both short- and long-term follow-up were satisfactory, and our drop-out analyses indicate minimal attrition bias over the one year [8]. The procedures in the study were pre-tested in a feasibility study and validated scales for the outcomes were chosen.
Only medium or large size clinics were invited. It is, however, possible that only recruiting from larger clinics may have introduced some bias into the sample. Finally, it is a limitation that the chronic conditions were self-reported without validation in for example medical records. Some rare chronic conditions may not be covered by the list.
Conclusions
Approximately 20% of patients with LBP in this cohort of Danish chiropractric practices have multimorbidity. Patients with multimorbidity reported higher pain levels, poorer self-rated health, and poorer physical functioning compared to those without multimorbidity. The LBP problem improved with time both for those with multimorbidity and those without. However, patients with high baseline pain levels and multimorbidity, had poorer recovery in terms of self-reported back-related disability. Furthermore, patients with multimorbidity had a continued use of pain medications for LBP compared to those without chronic disease. Chiropractors should be aware that patients with high levels of LBP and multimorbidity have a poorer recovery than patients without chronic disease, and clinical follow-ups may be indicated. The challenge of multimorbidity to chiropractors is not to view LBP as an isolated pain condition but rather it may be a part of a complex of diseases.
Acknowledgements
The authors thank M.Sc. Christine Winther Bang for her valuable contribution to the statistical analyses.
Abbreviations
- LBP
Low back pain
- ChiCo
The Danish Chiropractic low back pain Cohort
- RMDQ
The Roland Morris Disability Questionnaire
- BL1
The first baseline questionnaire
- BL2
The second baseline questionnaire
- NRS
Numeric rating scale
- GEE
Generalized estimating equation
- BMI
Body mass index
Author contributions
BSR, JH, VS and JSA have made significant contributions to the ideas and the design of the work and participated in obtaining, analyzing, or interpreting data. They have contributed significant to the intellectual content in formulating the work, interpreting of the results and critical revising of the manuscript. All the authors agree to be responsible for all aspects of the completed work by ensuring that questions relating to precision or integrity of any part of the work have been satisfactorily investigated and resolved. All authors read and approved the final manuscript.
Funding
This work was funded by the Danish Chiropractor Foundation, award number RLTN 5550-16/621 and The Research Council of the Practice Sector in the Municipality Region, Denmark. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The full data set are available. Contact: Professor Jan Hartvigsen, Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, Denmark e-mail: jhartvigsen@health.sdu.dk.
Declarations
Ethical approval and consent to participate
The Research Ethics Committee for Central Jutland determined that ChiCo did not require ethical approval because of the absence of a study-initiated clinical intervention. (Project-id: S-20162000-109). All participants provided written informed consent prior to enrolment.
Consent for publication
Not applicable.
Competing interests
Jan Hartvigsen is member of the Editorial Board of the Chiropractic and Manual Therapies. Otherwise, the authors declare that they have no other competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Willadsen TG, Bebe A, Køster-Rasmussen R, Jarbøl DE, Guassora AD, Waldorff FB, et al. The role of diseases, risk factors and symptoms in the definition of multimorbidity: a systematic review. Scand J Prim Health Care. 2016;34:112–121. doi: 10.3109/02813432.2016.1153242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS ONE. 2014 doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pefoyo AJK, Bronskill SE, Gruneir A, Calzavara A, Thavorn K, Petrosyan Y, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015 doi: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lowe DB, Taylor MJ, Hill SJ. Cross-sectional examination of musculoskeletal conditions and multimorbidity: influence of different thresholds and definitions on prevalence and association estimates. BMC Res Not. 2017 doi: 10.1186/s13104-017-2376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Zee-Neuen A, Putrik P, Ramiro S, Keszei A, de Bie R, Chorus A, et al. Work outcome in persons with musculoskeletal diseases: comparison with other chronic diseases & the role of musculoskeletal diseases in multimorbidity. BMC Musculoskelet Disord. 2017 doi: 10.1002/acr.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Luca KE, Parkinson L, Haldeman S, Byles JE, Blyth F. The Relationship between spinal pain and comorbidity: a cross-sectional analysis of 579 community-dwelling, older Australian women. J Manipulative Physiol Ther. 2017 doi: 10.1016/j.jmpt.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Duffield SJ, Ellis BM, Goodson N, Walker-Bone K, Conaghan PG, Margham T, et al. The contribution of musculoskeletal disorders in multimorbidity: implications for practice and policy. Best Pract Res Clin Rheumatol. 2017;31:129–144. doi: 10.1016/j.berh.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Kongsted A, Nielsen OL, Christensen HW, Hartvigsen J, Doktor K, Kent P, et al. The danish chiropractic low back pain cohort (ChiCo): description and summary of an available data source for research collaborations. Clin Epidemiol. 2020;12:1015–1027. doi: 10.2147/CLEP.S266220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Profil af den danske kiropraktorpatient. [Profile of the Danish chiropractic patient]. Dansk Kiropraktor Forening 2014. www.danskkiropraktorforening.dk/media/1367/patientundersoegelse-v2-2014.pdf. Accessed 12 Sept 2022.
- 10.Sorensen LP, Stochkendahl MJ, Hartvigsen J, Nilsson NG. Chiropractic patients in Denmark 2002: an expanded description and comparison with 1999 survey. J Manipulative Physiol Ther. 2006;29:419–424. doi: 10.1016/j.jmpt.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018;39:2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 12.Øverås CK, Johansson MS, de Campos TF, Ferreira ML, Natvig B, Mork PJ, et al. Distribution and prevalence of musculoskeletal pain co-occurring with persistent low back pain: a systematic review. BMC Musculoskelet Disord. 2021 doi: 10.1186/s12891-020-03893-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hestbaek L, Leboeuf-Yde C, Kyvik KO. Is comorbidity in adolescence a predictor for adult low back pain? A prospective study of a young population. BMC Musculoskelet Disord. 2006 doi: 10.1186/1471-2474-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernandez M, Boyle E, Hartvigsen J, Ferreira ML, Refshauge KM, Maher CG. Is this back pain killing me? All-cause and cardiovascular-specific mortality in older Danish twins with spinal pain. Eur J Pain. 2017 doi: 10.1002/ejp.996. [DOI] [PubMed] [Google Scholar]
- 15.Kristman VL, Hartvigsen J, Leboeuf-Yde C, Kyvik KO, Cassidy JD. Does radiating spinal pain determine future work disability? A retrospective cohort study of 22,952 Danish twins. Spine. 2012 doi: 10.1097/BRS.0b013e31823a426f. [DOI] [PubMed] [Google Scholar]
- 16.Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord. 2006 doi: 10.1186/1471-2474-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Albert HB, Jensen AM, Dahl D, Rasmussen MN. A Danish translation and validation of the Roland-Morris Questionnaire. Ugeskr Laeger. 2003;165:1875–1880. [PubMed] [Google Scholar]
- 18.Strøyer J, Essendrop M, Jensen LD, Warming S, Avlund K, Schibye B. Validity and reliability of self-assessed physical fitness using visual analogue scales. Percept Mot Skills. 2007;104:519–533. doi: 10.2466/pms.104.2.519-533. [DOI] [PubMed] [Google Scholar]
- 19.Linton SJ, Halldén K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain. 1998;14:209–215. doi: 10.1097/00002508-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Dufouil C, Brayne C, Clayton D. Analysis of longitudinal studies with death and drop-out: a case study. Stat Med. 2004;23:2215–2226. doi: 10.1002/sim.1821. [DOI] [PubMed] [Google Scholar]
- 22.Ostelo RWJG, de Vet HCW. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607. doi: 10.1016/j.berh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 23.Charity MJ, Britt HC, Walker BF, Gunn JM, Forsdike-Young K, Polus BI, et al. Who consults chiropractors in Victoria, Australia?: Reasons for attending, general health and lifestyle habits of chiropractic patients. Chiropr Man Ther. 2016 doi: 10.1186/s12998-016-0110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hestbaek L, Munck A, Hartvigsen L, Jarbøl DE, Søndergaard J, Kongsted A. Low back pain in primary care: a description of 1250 patients with low back pain in danish general and chiropractic practice. Int J Fam Med. 2014 doi: 10.1155/2014/106102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Luca K, Hogg-Johnson S, Funabashi M, Mior S, French SD. The profile of older adults seeking chiropractic care: a secondary analysis. BMC Geriatr. 2021 doi: 10.1186/s12877-021-02218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calderón-Larrañaga A, Vetrano DL, Ferrucci L, Mercer SW, Marengoni A, Onder G, et al. Multimorbidity and functional impairment-bidirectional interplay, synergistic effects and common pathways. J Intern Med. 2019;285:255–271. doi: 10.1111/joim.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heikkinen J, Honkanen R, Williams L, Leung J, Rauma P, Quirk S, et al. Depressive disorders, anxiety disorders and subjective mental health in common musculoskeletal diseases: a review. Maturitas. 2019;127:18–25. doi: 10.1016/j.maturitas.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Wertli MM, Held U, Campello M, Schecter WS. Obesity is associated with more disability at presentation and after treatment in low back pain but not in neck pain: findings from the OIOC registry. BMC Musculoskelet Disord. 2016 doi: 10.1186/s12891-016-0992-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hartvigsen J, Natvig B, Ferreira M. Is it all about a pain in the back? Best Pract Res Clin Rheumatol. 2013;27:613–623. doi: 10.1016/j.berh.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Nielsen OL, Kongsted A, Christensen HW. The chiropractic profession in Denmark 2010–2014: a descriptive report. Chiropr Man Ther. 2015 doi: 10.1186/s12998-015-0072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirofakta 2020. Praksistælling i kiropraktorpraksis. [Chirofacts 2020. Practice count in chiropractor practice]. Dansk Kiropraktor Forening 2020. https://d1gyukz65nrk4d.cloudfront.net/KiroFAKTA_2020.pdf. Accessed 12 Sept 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The full data set are available. Contact: Professor Jan Hartvigsen, Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, Denmark e-mail: jhartvigsen@health.sdu.dk.