Abstract
Background
There is emerging evidence that the neuroanatomy of autism forms a spectrum which extends into the general population. However, whilst several studies have identified cortical morphology correlates of autistic traits, it is not established whether morphological differences are present in the subcortical structures of the brain. Additionally, it is not clear to what extent previously reported structural associations may be confounded by co-occurring psychopathology. To address these questions, we utilised neuroimaging data from the Adolescent Brain Cognitive Development Study to assess whether a measure of autistic traits was associated with differences in child subcortical morphology, and if any observed differences persisted after adjustment for child internalising and externalising symptoms.
Methods
Our analyses included data from 7005 children aged 9–10 years (female: 47.19%) participating in the Adolescent Brain Cognitive Development Study. Autistic traits were assessed using scores from the Social Responsiveness Scale (SRS). Volumes of subcortical regions of interest were derived from structural magnetic resonance imaging data.
Results
Overall, we did not find strong evidence for an association of autistic traits with differences in subcortical morphology in this sample of school-aged children. Whilst lower absolute volumes of the nucleus accumbens and putamen were associated with higher scores of autistic traits, these differences did not persist once a global measure of brain size was accounted for.
Limitations
It is important to note that autistic traits were assessed using the SRS, of which higher scores are associated with general behavioural problems, and therefore may not be wholly indicative of autism-specific symptoms. In addition, individuals with a moderate or severe autism diagnosis were excluded from the ABCD study, and thus, the average level of autistic traits will be lower than in the general population which may bias findings towards the null.
Conclusions
These findings from our well-powered study suggest that other metrics of brain morphology, such as cortical morphology or shape-based phenotypes, may be stronger candidates to prioritise when attempting to identify robust neuromarkers of autistic traits.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13229-023-00538-5.
Keywords: Autism, Autistic traits, Subcortex, MRI, Brain morphology, Neuroimaging, ABCD
Introduction
Autism is a neurodevelopmental condition characterised by difficulties in social interaction and communication, together with restricted interests and a tendency to engage in repetitive behaviours [1]. Aetiology is complex, with an interaction of genetic, environmental, and neurodevelopmental pathways thought to lead to clinical manifestation [2]. The first behavioural signs typically emerge in early childhood [3] and are accompanied by atypical development of brain structure, function, and connectivity, which are hypothesised to play a role in behaviours across the lifespan [4]. Characterising the neural correlates of autism has therefore remained a focus of the field [5].
Advances in neuroimaging technology in the last two decades have allowed the development of novel in vivo imaging methods of the human brain. Of these, structural magnetic resonance imaging (sMRI) has been most widely used to characterise the neuroanatomy of autism [6, 7]. The identification of a neural endophenotype could help inform clinical care, such as earlier diagnosis and intervention, and be used in the subtyping of individuals within the heterogeneous autism umbrella [8]. An additional motivating factor has been that a robust biomarker could help distinguish autism from other neurodevelopment disorders that have overlapping clinical features, enabling individuals to access targeted treatments. For example, a recent study investigated whether distinct morphological differences could be detected when comparing autistic participants to those with obsessive–compulsive disorder (OCD) and attention-deficit/hyperactivity disorder (ADHD) [9]. However, whilst differences were identified, including thicker cortical grey matter in frontal regions of autistic participants compared to the other clinical groups, significant overlap between groups was observed. Finally, if associations were identified to be causal, knowledge of the specific regions implicated could provide mechanistic insights and help inform novel therapeutic strategies [10].
The neuroimaging literature demonstrates considerable heterogeneity regarding direction and effect size of brain morphology differences in autism [5, 11–13]. Whilst this may reflect the high level of aetiological and neurobiological heterogeneity across the autistic spectrum [14], methodological factors are thought to be a contributing factor. Firstly, existing studies tend to be in relatively small samples, leading to overestimation of effect sizes and low reproducibility [15]. Secondly, there is substantial heterogeneity in study design, including differences in participant characteristics such as age and symptom severity, covariates controlled for, and neuroimaging outcomes assessed. Finally, analytic differences, such as variation in MRI acquisition, processing, and analytic pipelines, impact results derived from individual studies [5]. Two mega-analyses (n ~ 3000) from the Enhancing Neuro-Imaging Genetics through Meta-Analysis consortium aimed to characterise the neuroanatomical correlates of autism, whilst addressing these issues [16]. Global measures were found to be higher in autistic participants, including intracranial volume (ICV), total grey matter, and mean cortical thickness. Regional differences in cortical thickness, including increases in the frontal regions and decreases in the temporal regions, were also observed. In contrast, no differences in cortical surface area were found [17]. Altered lateralised neurodevelopment was also revealed, with reduced regional asymmetry in cortical thickness and area, and increased asymmetry in the putamen [18]. In addition, a recent landmark study of autism identified early differences in brain morphology associated with a diagnosis. In a cohort of infants at high likelihood of being autistic, Shen et al. [19] identified that those who went on to be diagnosed with autism showed a faster amygdala growth between 6 and 24 months, and larger volumes at 12 months, when compared to typically developing controls.
An additional limitation of the existing literature is the use of categorical diagnoses when assessing neural correlates of autism [6]. There has been little focus on identifying the brain morphology correlates associated with subclinical autism in typically developing populations. Subclinical autistic traits include social communication differences alongside restricted behaviour patterns, which does not cause difficulties for everyday functioning [20]. The behaviours associated with autism can therefore be considered continuous traits, which extend into the general population [21, 22]. Genetic studies have demonstrated that liability to autism influences typical variation in the population of social–emotional interaction and communication ability, providing further evidence for the importance of studying autism-related phenotypes in a quantitative manner [23]. With this wealth of evidence that autistic traits fall along a continuum in the general population, it can therefore be hypothesised that the neuroanatomical differences associated with autism also extend into the general population.
Two longitudinal studies have examined cortical correlates of autistic traits in community-based samples, using measures from the Social Responsiveness Scale (SRS) [24]. Higher SRS scores were correlated with reduced regional cortical thickness including the right superior temporal sulcus [25] and the middle temporal gyri, ventral precentral and postcentral gyri, anterior cingulate, and right frontopolar cortex [26], which remained stable from childhood to adolescence.
Associations between autistic traits and brain morphology have also been examined in the Generation R Study, a population-based longitudinal cohort. Cross-sectional vertex-wise modelling was used to demonstrate autistic traits measured at age 6 years were associated with properties of cortical morphology, including surface area, thickness, and gyrification in late childhood [27], and adolescence [28]. Importantly, differences persisted after exclusion of autism cases, providing further evidence for the extension of autistic traits into the general population. Differences in brain structure associated with varying levels of autistic traits may therefore reflect alternate trajectories of brain development, which in turn are associated with behavioural differences across this continuum.
Whilst this work has begun to reveal the neurobiological differences associated with autistic traits, there remains a gap in the literature regarding differences in subcortical morphology. Given that previous studies show differences in subcortical structures when comparing autistic participants with typically developing controls, which has included reports of both increases [19, 29] and decreases [17] in volumes of specific ROIs, and the plausible role of these structures in the socio-motivational, cognitive, and motor symptoms seen in autism, it will be important to explore whether differences in these structures are observed in non-clinical samples.
In addition, children with autism are at increased risk of mental health issues and frequently present with problems in emotion, attention, and behaviour [30]. Whilst prevalence varies greatly, anxiety disorders, depression, OCD, ADHD, and specific phobias are most consistently reported as secondary psychiatric disorders co-occurring with autism [30–32]. Autistic traits have also been identified as a risk factor for poorer mental health, with associations appearing stronger in childhood than adulthood [33]. Whilst co-occurring psychopathology will confound behavioural-brain associations, such traits are not routinely controlled for in the existing autism neuroimaging literature [6]. The fact that the majority of studies are in clinical or community-based samples will bias towards a high occurrence of multiple diagnoses, and therefore, there is a gap in the literature for the application of methods in epidemiological cohorts. The identification of brain morphology features that remain associated with autistic traits beyond correction for co-morbidities will help delineate the biological underpinning of autism from other neurodevelopment disorders with overlapping clinical features.
In our study, we aim to expand on existing literature by exploring whether autistic traits are associated with differences in subcortical morphology, and whether any observed differences are explained by co-morbid psychopathology. We present the first population-based analysis of subcortical morphology associated with autistic traits, in an epidemiological sample of 9-to-10-year-old children participating in the Adolescent Brain Cognitive Development (ABCD) Study (n = 7005). Firstly, we explored whether a quantitative measure of autistic traits was associated with differences in child subcortical morphology (Aim 1). Secondly, to understand if any identified neural endophenotypes were specific to autistic traits, we tested whether associations persisted after controlling for co-occurring internalising and externalising symptoms (Aim 2).
Methods
Study sample
The ABCD Study® is a longitudinal study of brain development and child health. The study design and recruitment strategy have previously been described [34], but in brief, the study used school-based recruitment to enrol 11,875 children from 21 metropolitan sites across the USA. Children were aged between 9 and 10 years at time of enrolment, and they and their caregiver completed the baseline visit between 1 October 2016 and 31 October 2018, which consisted of questionnaires, clinical interviews, neurocognitive interviews, and a neuroimaging protocol. Exclusionary diagnoses include a current diagnosis of schizophrenia, a moderate/severe autism diagnosis, intellectual disability, or alcohol/substance use disorder.
Our study received approval from the institutional review board of the University of Southern California. The ABCD Study obtained centralised institutional review board approval from the University of California, San Diego, and each of the 21 study sites obtained local institutional review board approval. Ethical regulations were followed during data collection and analysis. Parents or caregivers provided written informed consent, and children gave written assent. Data can be accessed through registration with the ABCD study at https://nda.nih.gov/abcd. The present analyses used data from the baseline (demographic information, co-occurring psychopathology) and follow-up phase one visits (SRS). A total of 11,878 children were recruited at baseline, and of these, 11,736 participated in sMRI scanning. As the ABCD cohort contains data from siblings, measures from a random sample of 7875 unrelated individuals were used, of which 345 were excluded due to poor quality sMRI data. Of the remaining 7521 participants, 7005 had available data on autistic traits, and thus made up the present sample. During the screening process, caregivers were asked if their child had previously received a diagnosis of a mental health condition. In the present sample, a total of 107 (1.53%) children were reported to have an autism diagnosis, and 1053 (15.03%) were reported to have a diagnosis of another mental condition including ADHD, depression, bipolar disorder, anxiety, or a specific phobia.
Neuroimaging measures
All neuroimaging data were collected, processed, and quality checked by the ABCD Data Analysis, Informatics & Resource Center (DAIRC). Structural MRI scans were acquired at twenty-one sites across the USA using twenty-six different scanners from two vendors (Siemens and General Electric). Data were acquired when children were 9-to-10 years of age. Methods were optimised and harmonised across ABCD study sites for 3-T scanners, of which the full details have been published previously [35]. To summarise, after completion of a pre-scan assessment, a simulation session in a mock scanner, and motion compliance training, children participated in the ABCD neuroimaging protocol. T1-weighted structural scans with 1-mm isotropic resolution were collected using adult size multi-channel coils with image acquisition protocols for 3-Tesla Siemens, Phillips, and General Electric scanners, harmonised across all testing sites. Quality control procedures were based on automated means and SDs of extracted brain measures, and trained raters checked images for poor quality (i.e. motion artefacts, blurring, or ringing). Structural MRI data were processed by the ABCD DAIRC (Data Analysis, Informatics & Resource Center) team using FreeSurfer v5.3 (http://surfer.nmr.mgh.harvard.edu/) and subjected to quality control procedures [36].
FreeSurfer extracts cortical and subcortical region of interests (ROIs) based on the Desikan–Killiany atlas [37]. The automated pipeline consists of co-registration based on a template reference surface, motion correction, and averaging. Any intensity variation across the image due to magnetic field heterogeneity is corrected, and the skull stripped from the normalised intensity image. Images are then segmented using a connected components algorithm, where connectivity is not permitted across established cutting planes. Any holes within white matter are filled, producing a single volume for each hemisphere. Volumetric segmentation are used to delineate and label global (total brain volume, subcortical volume) and regional [nucleus accumbens (NAcc), amygdala, caudate nucleus, hippocampus, pallidum, putamen, and thalamus] measures [34]. A global subcortical volume was also derived, consisting of the total volume of the thalamus, caudate, putamen, pallidum, hippocampus, amygdala, NAcc, ventral DC, and substantia nigra). Subcortical volumetric measures were derived by averaging the homotopic regional volumes.
The resulting output was then visually examined by a trained DAIC technician, who rated them from zero to three in five categories: motion, intensity homogeneity, white matter underestimation, pial overestimation, and magnetic susceptibility artefact. From this, an overall “pass” or “fail” score was generated. Participants whose images failed QC were excluded from the present analyses [34].
Post-processed FreeSurfer derived phenotypes from the ABCD cohort have been widely used in studies assessing predictors of interest with brain morphology outcomes, including those examining subcortical ROIs [35, 36, 38, 39].
Social Responsiveness Scale (SRS)
Autistic traits were assessed using the SRS, which is primarily used to assess the severity of social difficulties across the full range of severity in both autistic and non-autistic children [24]. Statistical properties of the SRS have previously been evaluated in a UK population-based sample of 5-to-8-year-old children [38]. In the ABCD sample, parents answered an 11-item abridged version of the questionnaire which has previously shown strong loadings on the first unrotated factor of a principal components analysis of the SRS in a paediatric sample [39]. Parents were asked to rate statements on a four-point Likert scale; 0 (not true); 1 (sometimes true); 2 (often true); and 3 (almost always true). It encompasses the three DSM-IV autism domains, with items relating to reciprocal social behaviour (e.g. “Has difficulty making friends, even when trying his or her best”.), stereotyped and repetitive behaviours (e.g. “Has more difficulty than other children with changes in his or her routine”.), and communication impairments (e.g. “Has trouble keeping up with the flow of normal conversation”.). Total raw summary scores from participants were calculated (mean 3.49 SD = 0.49, range = 0–39).
Covariates
Potential confounders of the exposure-outcome relationship were defined a priori based on the previous literature. A minimum set of confounders required to adequately account for confounding were defined as: age, sex, ethnicity, cognition score, and a measure of socioeconomic status (family-level income). To assess the impact of co-occurring psychopathology, separate models were conducted with the inclusion of T-scores of externalising and internalising symptoms extracted from the Child Behaviour Checklist (CBCL) [40].
Demographic information (child sex, age at time of MRI, ethnicity, and total household income) was extracted from a demographics survey answered by the child’s main caregiver. Child cognitive ability was assessed using the NIH Toolbox® cognition measures (http://www.nihtoolbox.org) [41]. The toolbox consists of seven tasks that cover episodic memory, executive function, attention, working memory, processing speed, and language abilities and is used to generate a total cognitive score composite. The composite score demonstrates good test re-test reliability and validity in children [42].
The CBCL parent report was used to measure internalising and externalising symptoms in participants [43]. This is a well-established parent-completed measure of emotional, behavioural, and social problems in children and adolescents [44]. Composite scores of internalising and externalising problems were used for these analyses. Raw scores were converted to standardised t-scores, scaled so that fifty was average for child age and sex, with a standard deviation (SD) of ten points. Higher scores indicate increased behavioural and emotional problems.
Statistical analysis
Differences in covariates across tertials of SRS scores were examined using χ2-testing for categorical variables, and univariate regression modelling for continuous variables. The association of covariates with total subcortical volume was assessed using univariate regression modelling.
The association between SRS and brain morphology outcomes (volumes of the thalamus, caudate, putamen, pallidum, amygdala, hippocampus, and NAcc) was modelled using seemingly unrelated regression (SUR). The SUR system allows for a single model containing a number of linear equations, permitting correlation among the error terms. As SUR is used to analyse correlated outcomes, correlations between measures were assessed as a preliminary step in the analysis.
Models were conducted in three steps to assess the impact of confounding variables. Model 1: adjustment for child age, sex, ethnicity, family income, and ABCD recruitment site. Model 2: model 1 with the addition of cognition score (Aim 1). Model 3: model 2 with the addition of externalising symptoms and internalising symptoms (Aim 2). Raw p-values were adjusted for multiple testing by using Holm correction. All models were conducted with the inclusion of ICV to explore whether differences in subcortical volume were explained by differences in global brain size. Analyses were conducted in Stata v16.0 [45], with the -sureg command utilised to conduct SUR. Correlation between individual ROIs was assessed using the -pwcorr command.
Sensitivity analyses
A number of sensitivity analyses were conducted. Firstly, to explore whether associations were lateralised, analyses were replicated using homotopic ROIs. Secondly, to examine whether sex was a moderator of any observed associations, analyses were conducted with the addition of an interaction term. Finally, to explore the specific impact of dimensions of co-occurring mental health conditions, additional analyses were conducted controlling for internalising, externalising, and attention problems separately.
Results
Association of autistic traits with covariates
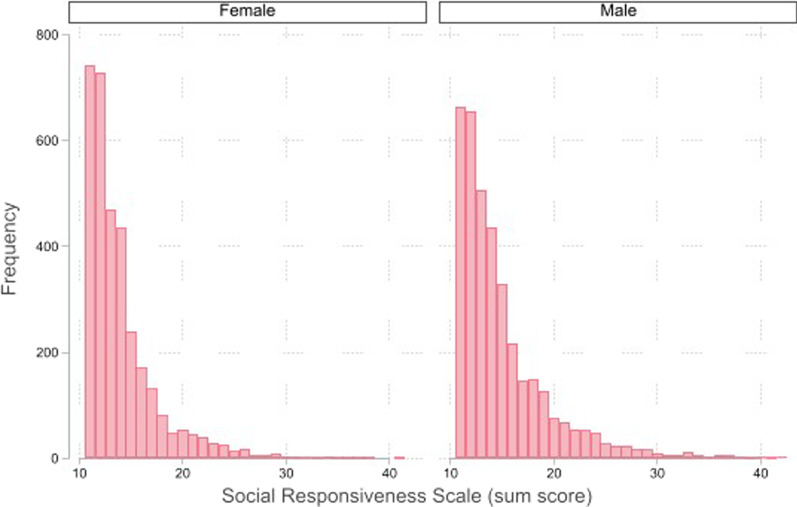
In our sample of children, male children of white ethnicity tended to score higher on the SRS compared to their peers (Table 1). A higher SRS score was negatively correlated with cognition score, and increased scores of total externalising and internalising problems. A strong negative gradient of family-level income with SRS score was observed. Children in the highest scoring SRS group demonstrated a lower ICV on average. The quality of sMRI data, which can be lower in autistic children due to increased participant motion inside the scanner [46], was not correlated with SRS score (Fig. 1).
Table 1.
Distribution of covariates of interest stratified by SRS group
| Social responsiveness score | p value | Total N (prop) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Middle | Upper | ||||||||
| 2791 | (39.84) | 2417 | (34.50) | 1797 | (25.65) | 7005 | ||||
| Sex, N (%) | ||||||||||
| Female | 1471 | (44.49) | 1145 | (34.63) | 690 | (20.87) | ||||
| Male | 1320 | (35.69) | 1272 | (34.39) | 1107 | (29.92) | < 0.0001 | 7005 | (100.00) | |
| Age, mean (SD) | ||||||||||
| Years | 9.88 | (± 0.01) | 9.90 | (± 0.01) | 9.90 | (± 0.01) | 0.2090 | 7005 | (100.00) | |
| Ethnicity, N (%) | ||||||||||
| White | 1494 | (42.07) | 1196 | (33.68) | 861 | (24.25) | ||||
| Black/African American | 364 | (36.25) | 365 | (36.35) | 275 | (27.39) | ||||
| Hispanic | 585 | (37.40) | 547 | (34.97) | 432 | (27.62) | ||||
| Other | 348 | (39.28) | 309 | (34.88) | 229 | (25.85) | 0.0060 | 7005 | (100.00) | |
| Cognition, mean (SD) | ||||||||||
| Standardised score | 103.77 | (± 0.33) | 102 | (0.38) | 97.76 | (± 0.45) | < 0.0001 | < 0.0001 | 6769 | (96.63) |
| Externalising symptoms, mean (SD) | ||||||||||
| Standardised score | 42.21 | (± 0.16) | 45.69 | (0.19) | 52.22 | (± 0.26) | < 0.0001 | < 0.0001 | 7003 | (99.97) |
| Internalising symptoms, mean (SD) | ||||||||||
| Standardised score | 44.72 | (± 0.17) | 49.04 | (0.20) | 56.01 | (± 0.25) | < 0.0001 | < 0.0001 | 7003 | (99.97) |
| ICV, mean (SD) | ||||||||||
| mm3 | 1,510,210 | (± 2795.58) | 1,512,337 | (± 2986.24) | 1,506,107 | (± 3554.96) | 0.605 | 0.3600 | 7005 | (100.00) |
| SC volume, mean (SD) | ||||||||||
| mm3 | 60,301 | (± 94.51) | 60,296 | (± 99.73) | 60,101 | (± 121.24) | 0.972 | 0.1860 | 7005 | (100.00) |
| Family income, N (%) | ||||||||||
| $34,999 or less | 400 | (29.50) | 491 | (36.21) | 465 | (34.29) | ||||
| $99,999 or less | 882 | (39.10) | 789 | (34.97) | 585 | (25.93) | ||||
| $199,999 or less | 917 | (45.13) | 686 | (33.76) | 429 | (21.11) | ||||
| $200,000 + | 407 | (49.69) | 256 | (31.26) | 156 | (19.05) | < 0.0001 | 6463 | (92.26) | |
Reported p values generated by univariate regression modelling for continuous variables and chi2 testing for categorical variables
ICV Intracranial volume, SC Subcortical
Fig. 1.
Histograms depicting distribution of Social Responsiveness Scale scores across study sample, stratified by sex
Association of global subcortical volume with covariates of interest
The association of covariates of interest with global subcortical volume was examined (Table 2). Male sex and older age were strongly predictive of higher subcortical volume. Non-white ethnicity, across all categories, was associated with lower subcortical volume. Children with increased scores on the total composite cognition score showed a higher subcortical volume. Whilst scores of total internalising problems showed little association, externalising symptoms were robustly associated with lower subcortical volume. Family-level income was positively associated with subcortical volume at all levels. Levels of correlation between individual subcortical ROIs were high across all comparisons justifying our use of SUR (Table 3).
Table 2.
Results from univariate regression modelling of the association between covariates of interest and total subcortical volume
| Total subcortical volume | Total | ||||
|---|---|---|---|---|---|
| B | SE | p value | |||
| Sex | |||||
| Female | |||||
| Male | 4055.83 | 109.43 | < 0.0001 | 7005 | (100.00) |
| Age | |||||
| Years | 483.50 | 98.12 | < 0.0001 | 7005 | (100.00) |
| Ethnicity | |||||
| White* | |||||
| Black/African American | − 3187.04 | 173.91 | < 0.0001 | ||
| Hispanic | − 1775.08 | 147.66 | < 0.0001 | ||
| Other | − 1338.85 | 182.72 | < 0.0001 | 7005 | (100.00) |
| Cognition | |||||
| Raw score | 58.08 | 3.27 | < 0.0001 | 6769 | (96.63) |
| SRS | |||||
| Standardised score | 4.66 | 14.55 | 0.7490 | 7005 | (100.00) |
| Externalising symptoms | |||||
| Standardised score | − 17.29 | 5.83 | 0.0030 | 7003 | (100.00) |
| Internalising symptoms | |||||
| Standardised score | − 0.02 | 5.60 | 0.9970 | 7003 | (100.00) |
| ICV | |||||
| mm3 | 0.03 | 0.00 | < 0.0001 | 7003 | (100.00) |
| Family income | |||||
| $34,999 or less* | |||||
| $99,999 or less | 1586.39 | 169.03 | < 0.0001 | ||
| $199,999 or less | 2415.20 | 172.49 | < 0.0001 | ||
| $200,000 + | 3027.52 | 217.70 | < 0.0001 | 6463 | (92.26) |
ICV intracranial volume
*Indicator variable
Table 3.
Correlation between subcortical regions of interest
| Thalamus | Pallidum | Caudate | NAcc | Putamen | Hippocampus | Amygdala | |
|---|---|---|---|---|---|---|---|
| Thalamus | 1 | ||||||
| Pallidum | 0.55 | 1 | |||||
| < 0.00001 | |||||||
| Caudate | 0.52 | 0.51 | 1 | ||||
| < 0.00001 | < 0.00001 | ||||||
| NAcc | 0.41 | 0.48 | 0.47 | 1 | |||
| < 0.00001 | < 0.00001 | < 0.00001 | |||||
| Putamen | 0.54 | 0.54 | 0.47 | 0.48 | 1 | ||
| < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 | ||||
| Hippocampus | 0.63 | 0.47 | 0.39 | 0.4 | 0.51 | 1 | |
| < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 | |||
| Amygdala | 0.56 | 0.41 | 0.38 | 0.45 | 0.51 | 0.65 | 1 |
| < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 | < 0.00001 |
Aim 1: association of SRS traits with subcortical morphology
Overall, in our sample of 7005 children from the ABCD study we found little evidence to suggest autistic traits are associated with disproportionate differences in volumes of seven subcortical structures (Fig. 2).
Fig. 2.
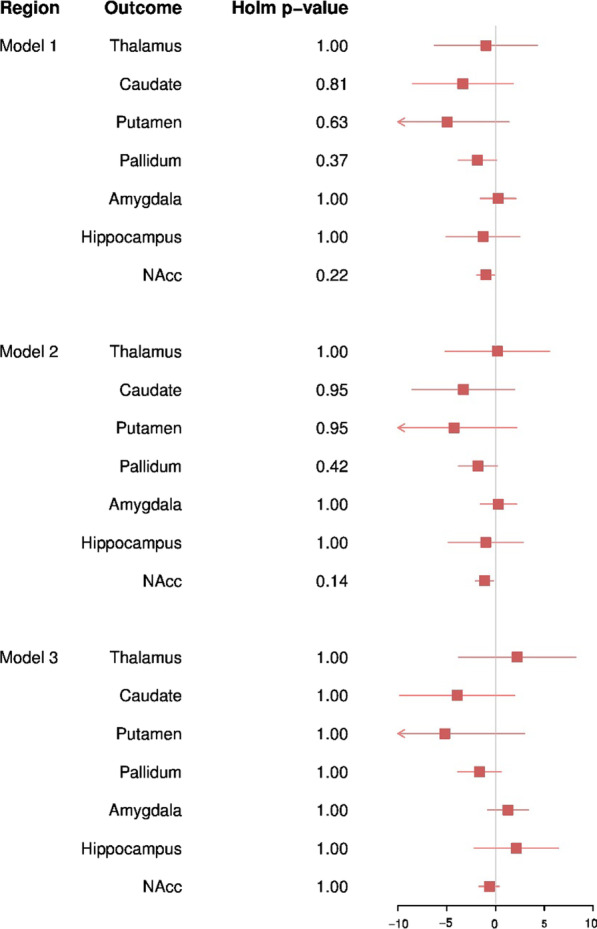
Forest plot depicting results from regression modelling of the association between the SRS and subcortical ROIs when adjusted for ICV. Corrected p values were generated using holm correction for multiple testing. NAcc: nucleus accumbens. Model 1 was adjusted for child age, sex, ethnicity, family income, and ABCD recruitment site. Model 2 was adjusted for the covariates included in model 1 with the addition of cognition score. Model 3 was adjusted for the covariates included in model 2 with the addition of externalising symptoms and internalising symptoms
In model 1, adjusted for age, sex, ethnicity, ABCD recruitment site, and family-level income, autistic traits were found to be predictive of absolute values of subcortical ROIs, with the strongest reductions with the NAcc (B = − 1.68, SE = 0.54, pholm = 0.013) and pallidum (B = − 3.31, SE = 1.14, pholm = 0.023). Suggestive associations were observed with the caudate and putamen (B = − 7.60, SE = 3.12, pholm = 0.059 and B = − 9.38, SE = 3.67, pholm = 0.053). The inclusion of total cognition score in model 2 attenuated these estimates towards the null, with only the reduction in NAcc volume remaining associated with SRS (β = − 1.51, SE = 0.55, pholm = 0.039) (Fig. 3). In contrast, little difference in subcortical ROI volumes was observed once ICV was corrected for, suggesting that these observed small differences are not beyond proportional differences of overall brain size in children.
Fig. 3.
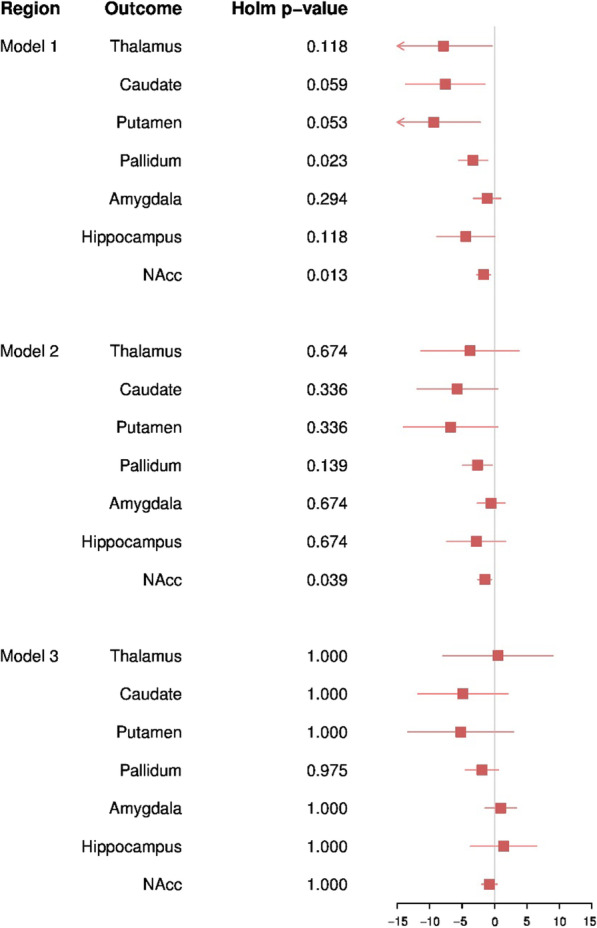
Forest plot depicting results from regression modelling of the association between the SRS and subcortical ROIs. Corrected p values were generated using holm correction for multiple testing. NAcc: nucleus accumbens. Model 1 was adjusted for child age, sex, ethnicity, family income, and ABCD recruitment site. Model 2 was adjusted for the covariates included in model 1 with the addition of cognition score. Model 3 was adjusted for the covariates included in model 2 with the addition of externalising symptoms and internalising symptoms
Aim 2: adjustment for co-morbid psychopathology
To assess whether any observed differences persisted after adjustment for co-occurring psychopathology, model 3 incorporated t-scores of total scores of externalising and internalising problems.
The observed weak reduction in absolute NAcc volume attenuated towards the null once externalising and internalising symptoms were accounted for (β = − 0.79, SE = 0.61, pholm = 1.00), suggesting that differences are not specific to autistic traits. Inclusion of externalising and internalising symptoms had little impact on effect estimates for the additional six subcortical ROIs. Similarly, analyses examining the impact of inclusion of ICV did not alter effect estimates substantially. Results from all models are presented in Additional file 1: Tables S1 and S2.
Findings from sensitivity analyses assessing the impact of lateralisation, sex modification, and specific dimensions of co-occurring mental health conditions on the association of autistic traits with subcortical brain morphology can be found in Additional file 1: Tables S3–S6. Results across all sensitivity analyses demonstrated little difference in effect estimates from those in the main analyses.
Discussion
There is emerging evidence that the neuroanatomy of autism falls along a continuum within the general population. Whilst several studies have assessed cortical phenotypes of autistic traits [26, 47], there remains a distinct gap in the literature regarding subcortical morphology. Thus, the primary aim of the present study was to investigate the association of autistic traits in childhood, measured by parent reported SRS score, with subcortical brain morphology. Our second aim was to test whether any observed differences were robust to adjustment for co-occurring psychopathology, measured as total scores of externalising and internalising symptoms. To our knowledge, this is the first such study to examine this association within the general population and therefore represents a novel contribution to the current body of literature.
To summarise, in this study of school aged children in the ABCD cohort, we did not find strong evidence for an association of autistic traits with differences in the subcortical volumes assessed, with results compatible with the null hypothesis and generally wide confidence intervals throughout.
Whilst we observed lower absolute volumes of the NAcc and putamen in those scoring higher on the SRS, this attenuated towards the null once overall brain size was accounted for. As univariate analyses had demonstrated children in the upper group of SRS scores had on average a lower ICV, this suggests the observed differences were not beyond that of proportional differences in brain size of the children in our sample. This finding of a reduced global measure of brain volume is in line with other studies assessing the neural correlates of autistic traits in epidemiological samples [27, 47]; however, it is important to note this is not consistent with findings from clinical populations [5, 13].
In the ABCD sample, being male or of white ethnicity was associated with higher SRS scores. It has been previously reported that in samples from the general population, male children tend to have higher SRS scores than female [27, 38, 48]. In contrast, there is little published literature regarding distribution across ethnic groups, and therefore, this is an area which requires further investigation.
The existing literature is composed predominantly of studies using a case-cohort design. Most notably, findings from the ENGIMA consortium identified lower volumes of the pallidum, putamen, and NAcc in participants with autism compared to controls [9]. Post hoc analyses demonstrated these differences were related to the degree of autism symptom severity, measured by scores extracted from the Autism Diagnostic Observation Schedule (ADOS) [49]. Although it must be noted that there are qualitative differences between the SRS and ADOS [50] and that these findings from the ENGIMA consortium have not yet been replicated, we had hypothesised we may see similar effects of a smaller magnitude focussed on these specific ROIs when examining the correlates of SRS scores in our sample. One possible explanation for our null results is that the differences in subcortical morphology observed in autism cases may represent neurobiology associated with a higher degree of autistic symptoms that meet the criteria for a clinical diagnosis.
A further study from the Generation R neuroimaging cohort, whilst predominantly focussed on cortical morphology, examined one subcortical ROI in relation to autistic traits [26]. The authors utilised a sample from 9- to 12-year-olds in the Netherlands (n = 2400), examining amygdala volume in relation to SRS scores. In line with our findings, amygdala volume was found to not differ significantly with SRS score when covariates were accounted for. In contrast, strong evidence was found for differences in metrics of cortical morphology, including lower gyrification, thickness, and surface area, suggesting that autistic traits in this sample are primarily associated with cortical, rather than subcortical ROI, differences.
Our second aim was to explore the role of co-occurring psychopathology, to understand if neural phenotypes were specific to autistic traits or simply a reflection of generalised psychopathology. Inclusion of these covariates had little impact on effect estimates; however, given that we found little association with SRS scores alone and that univariate analyses did not demonstrate strong associations of these covariates with our outcomes of interest, this is unsurprising.
It is important to note that whilst we did not detect significant group differences in subcortical ROIs, it is possible these volumetric measures are not sensitive to what may be more subtle differences exerted by autistic traits in the general population. Aggregate measures such as volume do not fully capture the complexity of subcortical structures and may be insensitive to specific local effects, or obscure heterogeneous local effects by averaging out subtle differences in shape [51]. This is particularly true for phenotypes which are likely characterised by specific associations with functionally distinct subfields of subcortical structures, such as traits of autism. Therefore, our lack of detectable volumetric differences in subcortical ROIs may be due to analytic methods, which do not allow for these subtler differences to be assessed. Whilst no studies have specifically used shape-based methods when assessing the subcortical correlates of autism, it has been demonstrated that for other neurobehavioral phenotypes, these methods provide more information than volumetric methods alone. For example, a recent study examining the subcortical alterations associated with major depressive disorder found little difference in subcortical volumes, beyond that of lower hippocampal volume [52]. In contrast, subsequent analyses using shaped-based methods identified specific effects localised to regions of the amygdala and hippocampus associated with patients in comparison to controls [53]. Complementary analyses, using shape-based analytic methods, will therefore be necessary to understand if autistic traits are associated with more sensitive markers of difference in subcortical morphology.
Limitations
When interpreting our findings, several limitations must be considered. Firstly, as the ABCD cohort excluded participants with a moderate or severe autism diagnosis (based on whether a child’s caregiver reported they did not attend mainstream school), the average severity of autistic traits will be artificially lower than in the general population, and therefore, findings may be biased towards the null. Secondly, as information regarding whether children had received a clinical diagnosis of autism was not available, it was not possible to conduct sensitivity analyses excluding these participants. Thirdly, neuroimaging measures and SRS scores were not contemporaneous; however, given the relatively short time period between clinics, and that autistic traits have been shown to remain stable over time [54, 55], this will likely have had limited impact. Fourthly, it is important to note that the SRS is contaminated by general behavioural problems [50] and therefore may not be wholly indicative of autism-specific symptoms. For example, SRS scores have been shown to be higher when co-occurring conditions are present, such as mood disorders [56], and child behaviour problems account for a significant proportion of the variance in SRS scores [57]. In addition, the 11-item SRS, rather than full 65-item SRS, was used in the ABCD cohort to reduce participant burden. Whilst the brief measure has been used previously [39], it is possible it may be a less sensitive marker of autistic traits than the full scale. This point, alongside the exclusion of participants with moderate/severe autism, may have reduced power to detect brain morphology correlates of autistic traits in this sample. It will be important to replicate this analysis in samples fully representative of the general population to enrich the higher end of score distribution for these traits.
Fifthly, our analyses were based on sMRI data obtained at a single time point, limiting our analyses to a cross-sectional design. Currently, there is limited longitudinal analysis of brain morphology outcomes associated with autistic traits in the general population, with a single study finding cortical morphology differences associated with autistic traits in the general population remain relatively stable over time [28]. Interestingly, this finding is not consistent with studies examining brain morphology associated with an autism diagnosis, with differences in developmental trajectories of total brain volume and subcortical morphology identified [19, 58]. It will therefore be important to replicate these previous epidemiological findings, and test associations in the context of subcortical morphology. As the ABCD cohort is an ongoing, longitudinal study, it will provide the ideal sample to continue examining these trends as further data are released, to understand if autistic traits are associated with individual or group differences in trajectories of subcortical volumes [59]. Finally, it is also important to note that neuroimaging phenotypes were derived using FreeSurfer 5.3, as described in the ABCD Release Notes for Data Release 3.0 (https://nda.nih.gov/abcd/). As newer versions are now available, this must be considered as a source of heterogeneity if comparing study findings to those using updated software.
These limitations must be also contrasted against the multiple strengths of our study. Firstly, data were drawn from a large population-based cohort with autistic traits measured continuously. The use of a dimensional approach, rather than a case-cohort design, is better suited to the idea of an autism spectrum and allowed us to test whether the underlying subcortical neurobiology of these traits extends into the general population. In addition, the ABCD cohort is socioeconomically, ethnically, and racially diverse, whilst being relatively homogenous regarding the age of participants. This allowed the generation of a representative estimate of the association of autistic traits with subcortical morphology, minimising the selection bias that has hindered previous studies in clinical samples. In addition, the wealth of phenotypic data available allowed us to control for all identified potential confounders of the exposure-outcome relationship, a significant source of bias in existing studies. In addition, utilising data from the ABCD cohort allowed a large sample size, with a total of 7005 included participants, twofold greater than that of the largest published study in this area.
Conclusions
In conclusion, in our population-based sample of 9- to 10-year-olds, we did not find evidence for an association between autistic traits and subcortical volumetric differences, with results across all models compatible with the null hypothesis. Although higher scores of the SRS were predictive of lower absolute volumes of the NAcc and putamen, these differences were not robust to correction for overall brain size.
Our findings suggest autistic traits are not associated with subcortical brain morphology in school-age children from population-based samples. However, it will be important to replicate these findings in an independent cohort which includes individuals presenting with moderate/severe autism, to enrich the higher end of score distribution for these traits, in addition to studying other metrics of brain morphology which may prove better targets when attempting to identify robust biomarkers of these traits.
Supplementary Information
Acknowledgements
Not applicable
Abbreviations
- SRS
Social Responsiveness Scale
- sMRI
Structural magnetic resonance imaging
- NAcc
Nucleus accumbens
- OCD
Obsessive–compulsive disorder
- ADHD
Attention-deficit/hyperactivity disorder
- ICV
Intracranial volume
- ABCD Study
Adolescent Brain Cognitive Development Study
- ROI
Region of interest
- CBCL
Child Behaviour Checklist
- SUR
Seemingly unrelated regression
Author contributions
All authors were involved in the methodology. The initial study proposal was conceived by TS and RB. TS performed the formal analysis and wrote the original draft of the manuscript in consultation with RB, AP, and ME. All authors read the manuscript and provided critical feedback. All authors read and approved the final manuscript.
Funding
ME is funded by the Canadian Institutes of Health Research and Fonds de Recherche du Québec. RB was supported by a King’s Prize Fellowship (204823/Z/16/Z). AP was part funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London and SI award NF-SI-0617-10120. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. All authors report no biomedical financial interests or potential conflicts of interest.
Availability of data and materials
The data that support the findings of this study are available from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The process for applying for access to this data is described on the study website (https://abcdstudy.org).
Declarations
Ethics approval and consent to participate
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cooper R. Diagnostic and statistical manual of mental disorders (DSM) Knowl Organ. 2017;44(8):668–676. [Google Scholar]
- 2.Hallmayer J, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry. 2011;68(11):1095–1102. doi: 10.1001/archgenpsychiatry.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landa R, Garrett-Mayer E. Development in infants with autism spectrum disorders: a prospective study. J Child Psychol Psychiatry. 2006;47(6):629–638. doi: 10.1111/j.1469-7610.2006.01531.x. [DOI] [PubMed] [Google Scholar]
- 4.Ecker C, Bookheimer SY, Murphy DG. Neuroimaging in autism spectrum disorder: brain structure and function across the lifespan. Lancet Neurol. 2015;14(11):1121–1134. doi: 10.1016/S1474-4422(15)00050-2. [DOI] [PubMed] [Google Scholar]
- 5.Stanfield AC, et al. Towards a neuroanatomy of autism: a systematic review and meta-analysis of structural magnetic resonance imaging studies. Eur Psychiatry. 2008;23(4):289–299. doi: 10.1016/j.eurpsy.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Pagnozzi AM, et al. A systematic review of structural MRI biomarkers in autism spectrum disorder: a machine learning perspective. Int J Dev Neurosci. 2018;71:68–82. doi: 10.1016/j.ijdevneu.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Li D, Karnath HO, Xu X. Candidate biomarkers in children with autism spectrum disorder: a review of MRI studies. Neurosci Bull. 2017;33(2):219–237. doi: 10.1007/s12264-017-0118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ecker C, et al. Describing the brain in autism in five dimensions–magnetic resonance imaging-assisted diagnosis of autism spectrum disorder using a multiparameter classification approach. J Neurosci. 2010;30(32):10612–10623. doi: 10.1523/JNEUROSCI.5413-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boedhoe PSW, et al. Subcortical brain volume, regional cortical thickness, and cortical surface area across disorders: findings from the ENIGMA ADHD, ASD, and OCD working groups. Am J Psychiatry. 2020;177(9):834–843. doi: 10.1176/appi.ajp.2020.19030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loth E, Murphy DG, Spooren W. Defining precision medicine approaches to autism spectrum disorders: concepts and challenges. Front Psychiatry. 2016;7:188. doi: 10.3389/fpsyt.2016.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernhardt BC, et al. Neuroimaging-based phenotyping of the autism spectrum. Curr Top Behav Neurosci. 2017;30:341–355. doi: 10.1007/7854_2016_438. [DOI] [PubMed] [Google Scholar]
- 12.Nickl-Jockschat T, et al. Brain structure anomalies in autism spectrum disorder–a meta-analysis of VBM studies using anatomic likelihood estimation. Hum Brain Mapp. 2012;33(6):1470–1489. doi: 10.1002/hbm.21299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Redcay E, Courchesne E. When is the brain enlarged in autism? A meta-analysis of all brain size reports. Biol Psychiatry. 2005;58(1):1–9. doi: 10.1016/j.biopsych.2005.03.026. [DOI] [PubMed] [Google Scholar]
- 14.Jeste SS, Geschwind DH. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat Rev Neurol. 2014;10(2):74–81. doi: 10.1038/nrneurol.2013.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Button KS, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14(5):365–376. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]
- 16.Thompson PM, et al. The ENIGMA Consortium: large-scale collaborative analyses of neuroimaging and genetic data. Brain Imaging Behav. 2014;8(2):153–182. doi: 10.1007/s11682-013-9269-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Rooij D, et al. Cortical and subcortical brain morphometry differences between patients with autism spectrum disorder and healthy individuals across the lifespan: results from the ENIGMA ASD working group. Am J Psychiatry. 2018;175(4):359–369. doi: 10.1176/appi.ajp.2017.17010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Postema MC, et al. Altered structural brain asymmetry in autism spectrum disorder in a study of 54 datasets. Nat Commun. 2019;10(1):4958. doi: 10.1038/s41467-019-13005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen MD, et al. Subcortical brain development in autism and fragile X syndrome: evidence for dynamic, age- and disorder-specific trajectories in infancy. Am J Psychiatry. 2022;179(8):562–572. doi: 10.1176/appi.ajp.21090896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruzich E, et al. Measuring autistic traits in the general population: a systematic review of the Autism-Spectrum Quotient (AQ) in a nonclinical population sample of 6,900 typical adult males and females. Mol Autism. 2015;6:2. doi: 10.1186/2040-2392-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baron-Cohen S, et al. The autism-spectrum quotient (AQ): evidence from asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31(1):5–17. doi: 10.1023/a:1005653411471. [DOI] [PubMed] [Google Scholar]
- 22.Ronald A, Hoekstra RA. Autism spectrum disorders and autistic traits: a decade of new twin studies. Am J Med Genet B Neuropsychiatr Genet. 2011;156B(3):255–274. doi: 10.1002/ajmg.b.31159. [DOI] [PubMed] [Google Scholar]
- 23.Robinson EB, et al. Genetic risk for autism spectrum disorders and neuropsychiatric variation in the general population. Nat Genet. 2016;48(5):552–555. doi: 10.1038/ng.3529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Constantino JN, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord. 2003;33(4):427–433. doi: 10.1023/a:1025014929212. [DOI] [PubMed] [Google Scholar]
- 25.Wallace GL, et al. Distinct cortical correlates of autistic versus antisocial traits in a longitudinal sample of typically developing youth. J Neurosci. 2012;32(14):4856–4860. doi: 10.1523/JNEUROSCI.6214-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hedrick A, et al. Autism risk gene MET variation and cortical thickness in typically developing children and adolescents. Autism Res. 2012;5(6):434–439. doi: 10.1002/aur.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blanken LM, et al. Cortical morphology in 6- to 10-year old children with autistic traits: a population-based neuroimaging study. Am J Psychiatry. 2015;172(5):479–486. doi: 10.1176/appi.ajp.2014.14040482. [DOI] [PubMed] [Google Scholar]
- 28.Durkut M, et al. The longitudinal bidirectional relationship between autistic traits and brain morphology from childhood to adolescence: a population-based cohort study. Mol Autism. 2022;13(1):31. doi: 10.1186/s13229-022-00504-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langen M, et al. Caudate nucleus is enlarged in high-functioning medication-naive subjects with autism. Biol Psychiatry. 2007;62(3):262–266. doi: 10.1016/j.biopsych.2006.09.040. [DOI] [PubMed] [Google Scholar]
- 30.Simonoff E, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 31.Leyfer OT, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006;36(7):849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- 32.Matson JL, Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: an overview. Res Dev Disabil. 2007;28(4):341–352. doi: 10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 33.Lundstrom S, et al. Autistic-like traits and their association with mental health problems in two nationwide twin cohorts of children and adults. Psychol Med. 2011;41(11):2423–2433. doi: 10.1017/S0033291711000377. [DOI] [PubMed] [Google Scholar]
- 34.Garavan H, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. 2018;32:16–22. doi: 10.1016/j.dcn.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hagler DJ, Jr, et al. Image processing and analysis methods for the Adolescent Brain Cognitive Development Study. Neuroimage. 2019;202:116091. doi: 10.1016/j.neuroimage.2019.116091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fischl B. FreeSurfer. Neuroimage. 2012;62(2):774–781. doi: 10.1016/j.neuroimage.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desikan RS, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31(3):968–980. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 38.Wigham S, et al. The reliability and validity of the social responsiveness scale in a UK general child population. Res Dev Disabil. 2012;33(3):944–950. doi: 10.1016/j.ridd.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 39.Reiersen AM, et al. Evidence for shared genetic influences on self-reported ADHD and autistic symptoms in young adult Australian twins. Twin Res Hum Genet. 2008;11(6):579–585. doi: 10.1375/twin.11.6.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rescorla LA. Assessment of young children using the Achenbach system of empirically based assessment (ASEBA) Ment Retard Dev Disabil Res Rev. 2005;11(3):226–237. doi: 10.1002/mrdd.20071. [DOI] [PubMed] [Google Scholar]
- 41.Luciana M, et al. Adolescent neurocognitive development and impacts of substance use: overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev Cogn Neurosci. 2018;32:67–79. doi: 10.1016/j.dcn.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akshoomoff N, et al. VIII. NIH toolbox cognition battery (CB): composite scores of crystallized, fluid, and overall cognition. Monogr Soc Res Child Dev. 2013;78(4):119–132. doi: 10.1111/mono.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Achenbach TM. Manual for the child behaviour checklist/4–18 and 1991 profile. Burlington: University of Vermont; 1991. [Google Scholar]
- 44.Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles : an integrated system of multi-informant assessment. Burlington: ASEBA; 2001. [Google Scholar]
- 45.Stata Statistical Software: Release 16. College Station, T.S.L.S.
- 46.Pardoe HR, Kucharsky Hiess R, Kuzniecky R. Motion and morphometry in clinical and nonclinical populations. Neuroimage. 2016;135:177–185. doi: 10.1016/j.neuroimage.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 47.Alemany S, et al. Brain morphology, autistic traits, and polygenic risk for autism: a population-based neuroimaging study. Autism Res. 2021 doi: 10.1002/aur.2576. [DOI] [PubMed] [Google Scholar]
- 48.Constantino JN, Todd RD. Autistic traits in the general population: a twin study. Arch Gen Psychiatry. 2003;60(5):524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- 49.Lord C, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185–212. doi: 10.1007/BF02211841. [DOI] [PubMed] [Google Scholar]
- 50.Hus V, et al. Factors influencing scores on the social responsiveness scale. J Child Psychol Psychiatry. 2013;54(2):216–224. doi: 10.1111/j.1469-7610.2012.02589.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roshchupkin GV, et al. Heritability of the shape of subcortical brain structures in the general population. Nat Commun. 2016;7:13738. doi: 10.1038/ncomms13738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schmaal L, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major depressive disorder working group. Mol Psychiatry. 2016;21(6):806–812. doi: 10.1038/mp.2015.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ho TC, et al. Subcortical shape alterations in major depressive disorder: findings from the ENIGMA major depressive disorder working group. Hum Brain Mapp. 2020;38:1068. doi: 10.1002/hbm.24988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robinson EB, et al. Stability of autistic traits in the general population: further evidence for a continuum of impairment. J Am Acad Child Adolesc Psychiatry. 2011;50(4):376–384. doi: 10.1016/j.jaac.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haraguchi H, et al. Stability of autistic traits from 5 to 8 years of age among children in the general population. J Autism Dev Disord. 2019;49(1):324–334. doi: 10.1007/s10803-018-3770-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pine DS, et al. Autism spectrum disorder scale scores in pediatric mood and anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2008;47(6):652–661. doi: 10.1097/CHI.0b013e31816bffa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Constantino JN, Hudziak JJ, Todd RD. Deficits in reciprocal social behavior in male twins: evidence for a genetically independent domain of psychopathology. J Am Acad Child Adolesc Psychiatry. 2003;42(4):458–467. doi: 10.1097/01.CHI.0000046811.95464.21. [DOI] [PubMed] [Google Scholar]
- 58.Schumann CM, et al. Longitudinal magnetic resonance imaging study of cortical development through early childhood in autism. J Neurosci. 2010;30(12):4419–4427. doi: 10.1523/JNEUROSCI.5714-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Casey BJ, et al. The adolescent brain cognitive development (ABCD) study: imaging acquisition across 21 sites. Dev Cogn Neurosci. 2018;32:43–54. doi: 10.1016/j.dcn.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The process for applying for access to this data is described on the study website (https://abcdstudy.org).