ABSTRACT
Pancreatic cystic lesions (PCLs) are increasingly being recognized due to improvements and widespread use of cross-sectional imaging. With an estimated prevalence of 15% in general population, incidentally discovered PCLs represent a dilemma in management. While pancreatectomies offer a chance of cure, the morbidity is considerable in patients with high surgical risks. More recently, EUS-guided approaches for cyst ablation are being offered in clinical trials for the management of PCLs. EUS-chemoablation studies have progressed from first investigating safety and efficacy of EUS-guided alcohol lavage to single-agent paclitaxel ablation. Recent studies have shown that alcohol lavage may not be required, and long-term resolution can be achieved by chemoablation alone. EUS-guided lauromacrogol ablation and EUS-guided radiofrequency ablation (RFA) are new techniques that have shown promising results in a few small studies. Overall, the current literature suggests that EUS-guided paclitaxel ablation has better cyst resolution rates compared to other existing minimally invasive techniques including ethanol injection, lauromacrogol ablation, or RFA. This article will review EUS-guided PCL ablation approaches and future directions the field is headed into.
Keywords: EUS-guided ablation, EUS-guided chemoablation, intraductal papillary mucinous neoplasms, mucinous cystic neoplasms, pancreatic cystic lesions, radiofrequency ablation
INTRODUCTION
Pancreatic cystic lesions (PCLs) represent a heterogenous group of lesions that have varying malignant potential. Incidental PCLs in asymptomatic patients are increasingly being recognized due to increase in cross-sectional imaging.[1] Specific cyst types such as mucinous cysts (intraductal papillary mucinous neoplasm [IPMN] and mucinous cystic neoplasms[(MCN]) have the potential for malignant transformation. While there are challenges in specific diagnosis of cyst types, consensus guidelines have established worrisome and high-risk features that predict malignancy and guide appropriate management of mucinous PCLs.[2]
PCLs mainly comprise IPMNs, MCNs, serous cystadenomas (SCAs), cystic neuroendocrine tumors (CNETs), and pseudocysts. Pseudocysts are inflammatory, and SCAs are benign neoplasms with malignant transformation in <0.1% of cases.[3] Mucinous cysts (IPMNs and MCNs) account for over 60% of all identified PCLs.[4] MRI with MRCP has very high sensitivity for identifying these PCLs.[1] It is estimated that 6.6% of general population harbor IPMNs.[5] Main-duct IPMNs (≥1 cm in diameter) carry 60%–92% risk of malignant transformation or harboring malignancy.[2] The risk of malignancy increases with main pancreatic duct diameter >1 cm and presence of mural nodule.[2,6] MCNs also carry a high risk (25%–30%) of progression to malignancy but lack the risk of recurrence or multifocality.[7,8,9] Thus, these lesions warrant surgical interventions.[6] Branch duct IPMNs can be multifocal and are the most frequent neoplastic PCLs. Risk of malignant transformation increases with greater diameter and other associated worrisome and high-risk features.[2] Cyst diameters ≥3 cm carry a risk, although relatively low (18%–25%) of malignant transformation or harboring a malignancy making them a potential candidate for EUS ablation.[6,10,11,12]
Deaths from pancreatic cancer are expected to become the second leading cause of cancer-related death surpassing breast cancer-related deaths by 2030.[13] The dilemma for intervening on incidentally detected PCLs that satisfy worrisome or high-risk criteria for advanced neoplasia arises from the treatment options.[2] While radical resection offers a chance of cure, pancreatic surgeries have reportedly 20%–40% morbidity rate and a 1%–2% mortality rate.[7,14] Therefore, over the last two decades, as accuracy of cyst diagnosis has improved, approach for PCLs has changed from aggressive “surgery-first” to “surveillance-first” approach, and there are specific guideline criteria for resection.[2,15] However, life-long surveillance is resource consuming-if all patients between ages 40 and 79 years with PCLs underwent MRI surveillance, it would cost an estimated $9 billion per year to the health-care system.[16] In addition, the lack of evidence on long-term mortality benefits for surveillance techniques further contends this option.[1,16,17]
Minimally invasive treatments for PCLs are increasingly being recognized as a management option. The efficacy and safety of injection of chemotherapeutic agent directly into malignant lesions in lungs, brain, ovaries, and liver[18,19,20,21] initially led way to injection of antitumoral agents into unresectable pancreatic cancer.[22,23] Subsequently, Gan et al. first demonstrated the efficacy of EUS-guided alcohol ablation of PCLs in asymptomatic patients.[24] EUS-guided alcohol cyst ablation led way to chemoablation which showed better efficacy than prior method and fewer complications. Similarly, radiofrequency ablation (RFA) was initially shown to be successful in gastrointestinal and pancreatic diseases including pancreatic cancer which led to its use in the management of PCLs. This review article summarizes the new literature on EUS-guided ablation and RFA and the future direction of endoscopic approaches for PCL management.
PATIENT SELECTION
EUS-guided ablation should not be performed on high-risk lesions unlikely to respond to ablation, lesions with evidence of pancreatic cancer, small and low-risk lesions which have no malignancy potential or during pregnancy.[25,26] Therefore, the first step prior to EUS-guided ablation is to accurately diagnose and risk-stratify the PCL. Among suitable PCLs, EUS-guided ablation offers a potential management strategy for patients with high risks for surgical procedures due to their age or existing medical conditions. In 2019, an international expert panel reached a consensus that EUS-guided chemoablation was recommended in patients– (i) who are not surgical candidates and have reasonable life expectancy, (ii) confirmed diagnosis of mucinous pancreatic cyst, (iii) cyst diameter of >3 cm, or (iv) enlarging pancreatic cyst with a diameter of >2 cm.[25] The ACG guidelines state that there is insufficient evidence to support the routine use of PCL ablation (EUS chemoablation or RFA) but can be considered in patients who refuse or are not suitable surgical candidates; additionally recommending that these subjects should be treated in a clinical trial to establish the efficacy of EUS ablation.[1] European guidelines have similar recommendation for EUS-guided ablation of PCLs.[27] While experts differ in absolute/relative indications and contraindications for the EUS-guided ablation, Figure 1 summarizes the existing literature for the selection of PCLs for EUS-guided ablation.
Figure 1.
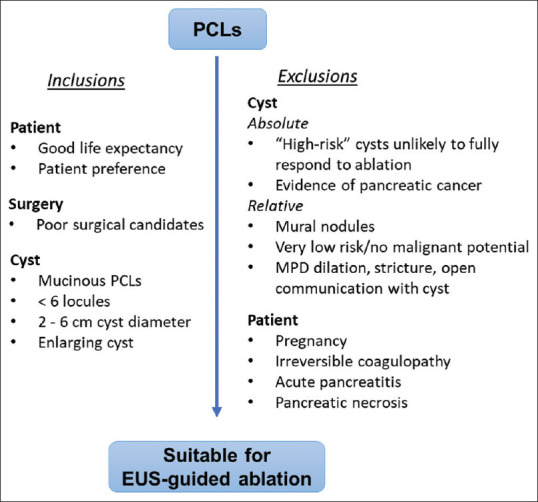
Summary of expert-panel consensus for selection of pancreatic cystic lesions appropriate for EUS-guided ablation techniques. Figure based on expert panel summary.[25,26] High-risk cysts as defined by the revised Fukuoka guidelines,[2] American Gastroenterological Association guidelines,[14] and European guidelines.[27] PCL: Pancreatic cystic lesion; MPD: Main pancreatic duct.
Current literature on PCLs ablation suggests that patients with unilocular cysts have good resolution rates, and increased number of loculations may decrease the efficacy of chemoablation.[26,28,29] Smaller cysts have been associated with higher resolution rates and make for the ideal candidates.[28,29] Contrarily though, small cysts (even IPMNs) may have a very low malignant potential and may not require EUS ablation.[26,30] Given the complicated nature of the decision-making, patients and clinicians should engage in shared-decision making.
EUS-GUIDED ALCOHOL ABLATION
The success of ethanol injections in ablation of cysts in endocrine glands and other internal organs led way to its use on pancreas cyst.[31,32,33,34] Despite alcohol's association with pancreatitis, initial studies on ablation of pancreas pseudocyst and pancreatic tumors reported no risk of pancreatitis.[34,35] Subsequently, Gan et al. prospectively studied the safety and feasibility of ethanol lavage on PCLs in 25 patients.[24] Complete cyst resolution was observed in 35% patients, irrespective of ethanol concentration used for lavage. No immediate complications were reported indicating the safety of this new technique. Similarly, Caillol et al. reported 85% complete resolution rates with no clinical complications in 13 patients with mucinous cysts.[36]
With evidence of safety, DeWitt et al. attempted to evaluate the efficacy of ethanol lavage.[37] In a randomized control trial with 58 patients, ethanol lavage had complete cyst resolution rates of 33%, and single ethanol lavage outperformed saline lavage in mean cyst diameter reduction (-28.1%; 95% confidence interval [CI] – 38.1 to −18.2 vs.−6.9%; 95% CI –14.5-0.7, respectively). Among ethanol lavage group, 12%–16% patients reported abdominal pain and 2 patients had acute pancreatitis, with similar rates of abdominal pain seen in control group. They established that ethanol lavage was a safe and effective approach for PCL ablation.
While DeWitt's study failed to show statistical benefit in cyst size reduction from multiple ethanol lavages, DiMaio et al. attempted to study this further.[38] Among 13 branch-duct IPMNs, single lavage had 0% complete resolution rate and 2 lavages had 38% (5/13) complete resolution rate. The mean diameter changed from 20.1 ± 7.1 mm at baseline to 17.0 ± 9.8 mm (P = 0.06) after 1 lavage and 12.8 ± 9.6 mm (P = 0.0002) after 2 lavages. Only 2 patients underwent 3 lavages and they had further decrease in cyst size. Only 1/13 (7.7%) patients had reported minor abdominal pain, no pancreatitis.
Despite the promising results from previous studies, Gomez et al. followed patients for >80 months postprocedure and reported that ethanol lavage was not a reliable technique for ablation of PCLs.[39] Park et al. showed similarly low reliability of ethanol ablation.[40] Of the 23 patients enrolled in the study, complete long-term resolution was observed in only 9% (2/23) PCLs.[39] Excluding one patient, 50% (10/20) patients had greater than ≥80% reduction in cyst volume. However, considerable number of patients had an increase in cyst size 1-year postprocedure and on subsequent imaging, highlighting the lack of long-term resolution. In addition, nonmucinous cysts had significantly greater cyst size reduction compared to mucinous cysts further minimizing the utility of ethanol lavage. While immediate complications were relatively low, the lack of long-term resolution, especially in mucinous cysts, called for newer methods of EUS-guided ablation. Table 1 describes the existing EUS-guided ethanol ablation studies.
Table 1.
Summary of studies on EUS-guided ethanol ablation of pancreatic cystic lesions
| Reference | n | Number of lavages | Complete resolution (%) | Partial resolution (%) | Complications |
|---|---|---|---|---|---|
| Gan 2005 | 25 | 1 | 35 | 7 | None |
| Dewitt 2009 | 42 (ethanol arm 25; control arm 17) | 1 or 2 | 33 | 0 | Ethanol arm 4% pancreatitis 20% abdominal pain Control arm 12% abdominal pain |
| DiMaio 2011 | 13 | 2 or more | 38 | - | 8% abdominal pain |
| Caillol 2012 | 13 | 1 | 85 | - | None |
| Gomez 2016 | 23 | 1 | 9 | 44 | 4% pancreatitis 4% abdominal pain |
EUS-GUIDED PACLITAXEL ABLATION
Paclitaxel is a chemotherapeutic agent that alters microtubules turnover causing cell death. Microtubules, a polymer of tubulin heterodimer is composed of alpha and beta subunits.[41,42] Paclitaxel binds to the beta-tubulin subunit and induces bundling of microtubules.[43,44,45] This impairs microtubule-dependent functions such as cell division, maintenance of cell shape, motility, intracellular transport, and signal transmission.[41,42,46] Thus, by promoting microtubule stability and impairing disassembly of microtubules, paclitaxel causes cell death.[47] Due to its viscous, hydrophobic nature, it is theorized to be less likely to extravasate out of the cyst and allow for increased duration of contact with the epithelial lining.[17,47,48,49] Studies examining EUS-guided paclitaxel ablation have been summarized in Table 2.
Table 2.
Summary of studies on EUS chemoablation of pancreatic cystic lesions
| Reference | n | Ablative agent | Complete resolution (n) | Partial resolution (n) | Complications |
|---|---|---|---|---|---|
| Oh 2008 | 14 | Ethanol lavage with paclitaxel injection | 11 | 2 | 7% abdominal pain 43% hyperamylasemia 7% pancreatitis |
| Oh 2009 | 10 | Ethanol lavage with paclitaxel injection | 6 | 2 | 10% pancreatitis |
| Oh 2011 | 52 | Ethanol lavage with paclitaxel injection | 29 | 6 | 2% fever 2% pancreatitis 2% abdominal pain 2% splenic vein obstruction |
| DeWitt 2014 | 22 | Ethanol lavage with paclitaxel injection | 10 | 5 | 13% abdominal pain 10% pancreatitis 3% peritonitis 3% gastric wall cyst |
| Moyer 2016 | 10 (alcohol arm 4; alcohol-free arm 6) | Saline or ethanol lavage followed by paclitaxel and gemcitabine injection | 67% in saline arm versus 75% in ethanol arm |
- | Ethanol arm: 20% pancreatitis Saline arm: None reported |
| Kim 2017 | 36 (ethanol ablation 8; ethanol lavage with paclitaxel ablation 28) | Ethanol ablation or ethanol lavage followed by paclitaxel injection | 19 | 7 | 7% abdominal pain 7% pancreatitis 2% intracystic hemorrhage |
| Choi 2017 | 164 | Ethanol lavage with paclitaxel injection | 114 | 31 | 4% pancreatitis 1% psuedocyst 1% abscesses, 0% (1/164) risk of portal vein thrombosis, fever, splenic vein obstruction, pancreatic duct stricture Pericystic spillage, intracystic hemorrhage |
Safety and efficacy of paclitaxel ablation
After the success of EUS-guided ethanol ablation for PCLs, Oh et al. attempted at improving the efficacy of cyst resolution by adding a chemotherapeutic agent – paclitaxel. They performed EUS-guided ethanol lavage with paclitaxel injection (EUS-EP) in asymptomatic PCLs.[48] In this prospective study, 14 patients with either indeterminate cyst, MCN, SCA, or lymphangioma underwent EUS-EP. At a median follow-up of 9 months (range: 6–23 months), complete resolution was shown in 11 patients (78.5%) and partial resolution in two patients (14%). Cyst characteristics of patients with complete resolution included a median diameter of 21.0 mm (range: 17–52 mm) and median volume of 2.75 mL (range: 1.2–67.7 mL). The median diameter and volume of partial and unresolved cysts were larger (28.0 mm (range: 27–40 mm) and 5.31 mL (range 5.1–30.6 mL), respectively, however, no significant difference was reported. The study demonstrated the safety and efficacy of EUS-EP with the complication of acute pancreatitis reported in one patient (7%). In a subsequent study, Oh et al. retrospectively demonstrated effectiveness of EUS-EP in patients with oligolocular cyst (2–6 locules). Complete resolution was achieved in 6 patients (60%) with complications seen in 1 patient (10%).[50] The group demonstrated that by puncturing lobules to create communications using angulated needles, EUS-EP was an effective therapy even in oligolocular PCLs.
DeWitt et al. prospectively studied patients with PCLs measuring 15 mm–50 mm who had a potential indication for surgery but instead underwent EUS chemoablation.[51] Complete resolution was seen in 10/20 (50%) patients. DNA analysis showed elimination of all mutations (K-ras mutations and loss of heterozygosity) present in preablation cyst fluid in 8 of 11 (72%) patients. The study demonstrated that among patients with radiologic regression of cyst, analysis showed elimination of mutant DNA in majority of cases.[51] Kim et al. followed 36 patients for a median of 22.3 months (range 3–120) and found complete resolution in 19 (56%) patients.[52] They performed cytological analysis and found decrease/elimination of cellular atypia in 5 (15%) patients and increased atypia in 3 (9%) patients. However, no significant difference in histopathological change was observed in complete resolution and partial resolution group. While both studies showed a few cases with new mutations or increased cellularity/atypia postablation, the significance of these changes after cyst ablation is still unknown. Overall, both studies aimed at identifying the DNA and or histologic changes after cyst ablation.
Predictors of EUS-EP efficacy
Following the demonstration of EUS-EP safety and efficacy, Oh et al. prospectively studied 52 patients with PCLs to identify predictors of PCL resolution at long-term follow-up.[53] Multivariate analysis showed that original volume <14 mL (which correlated with cyst diameter <35 mm) was predictive of cyst resolution (P < 0.02). Of note, type of cyst and locularity were not found to be predictors of cyst resolution.
The CHARM trial– role of alcohol lavage
The first randomized, double-blinded control study known as the CHARM trial,[54] evaluated the necessity of ethanol lavage for PCL ablation. The trial randomized 10 patients into the alcohol arm (ethanol lavage followed by paclitaxel and gemcitabine injection) or the alcohol-free arm (saline lavage followed by paclitaxel and gemcitabine injection). Alcohol arm had 75% complete resolution at 12 months compared to 67% in nonalcohol arm. While 1 (20%) patient in the alcohol arm had acute pancreatitis, there were no complications in the alcohol-free arm. This was the first study that evaluated the need for ethanol lavage and suggested that alcohol may not be required for effective cyst ablation. Further, it also implied that complication from EUS-guided cyst ablation may be secondary to ethanol extravasation.
Phase 2 of the CHARM trial had similar findings.[55] A total of 39 patients were randomized to either receive saline lavage or an ethanol lavage, both followed by paclitaxel and gemcitabine injection. Complete resolution rates in saline lavage and alcohol lavage groups were similar, 67% and 61%, respectively (95 CI – 0.38-0.24; P = 0.01). Univariate analysis of pretreatment parameters showed no significant difference in PCL diameter, locularity, cyst fluid carcinoembryonic antigen level, or type of cyst for the primary outcome of resolution. Complications were only reported in ethanol lavage arm and included pancreatitis and abdominal pain. Phase 3 of the CHARM trial, CHARM II: Chemotherapy for ablation and resolution of mucinous pancreatic cysts (CHARM) (https://clinicaltrials.gov/ct2/show/NCT03085004) is currently underway with estimated 100 participants randomized to either the ethanol lavage group or saline lavage group, both followed by the same dual-agent chemotherapeutic cocktail (paclitaxel and gemcitabine).
Long-term outcomes
Long-term outcomes after EUS chemoablation of PCLs were studied by Choi et al.[29] The study enrolled 164 patients who underwent EUS-EP. The cohort included a diagnosis of IPMN or MCN in 82/164 (50%) patients and 66/164 (40%) had an oligolocular cyst. Postprocedure follow-up was for a median of 72 months (range: 50–85 months). While a complete resolution of the PCL was seen in 114 patients, a partial resolution was seen in 31; however, two patients had recurrence of PCL during the study period. Univariate analysis showed that a diameter <35 mm (P = 0.04) and unilocularity (P < 0.001) were associated with complete resolution. No significant difference was noted between type of cyst and response rate. Similar to the findings of Oh et al.,[53] multivariate analysis showed that unilocular cysts (odds ratio [OR]: 7.12, 95% CI: 2.72-18.67; P < 0.001) and small cyst diameter (OR: 2.39, 95% CI: 1.11–5.16; P = 0.02) were independent predictors of complete resolution.
EUS-GUIDED LAUROMACROGOL ABLATION
Lauromacrogol, an agent typically used as an ablative agent for esophageal variceal bleeding, is a sclerosant and a mild anesthetic that causes vascular injury. Linghu et al. first demonstrated the safety and feasibility of lauromacrogol in ablation of PCLs.[56] In a prospective study with 29 patients, they reported complete and partial resolution rate of 37.9% (11/29) and 31% (9/29) at 9 months, respectively. PCL diameter reduced from 28.6 ± 14.5 mm to 13.4 ± 10.5 mm (P < 0.001) and only two patients had mild acute pancreatitis and one patient had fever. Following this success, researchers from the same group prospectively followed 35 patients for a longer duration and found that lauromacrogol ablation offered complete resolution rate of 51.4% (18/35) and partial resolution rate of 25.7% (9/35) at 1 year.[57] Major adverse event rate was reported at 3.6% and included fever and acute pancreatitis.
RADIOFREQUENCY ABLATION
Delivering high-frequency (460–500 kHz) alternating current, RFA induces coagulative necrosis of targeted tissues to cause cell apoptosis.[58] In addition to physical damage, RFA also has immunomodulatory effects as seen by increased levels of pro-inflammatory cytokines and lower levels of immunosuppressive cytokines.[59] Within the realm of pancreatic diseases, RFA was initially used to treat patients with locally advanced/metastatic pancreatic cancer who were not good candidates for surgery and later in neuroendocrine tumors. RFA showed positive results with reduction of tumor burden and no major complications in both populations.[60,61,62,63,64,65,66,67] Consequently, RFA was studied in animal studies for PCLs and subsequently studied in human PCLs.
The first RFA study in human PCL was conducted by Pai et al.[68] They demonstrated that RFA was a feasible approach with 33% (n = 2/6) complete resolution rate and additional 50% cases (n = 3/6) achieving 48.4% size reduction at 3–6 months (mean pre-RFA 38.8 mm [standard deviation (SD) ± 21.7 mm] vs. mean post-RFA 20 mm [SD ± 17.1 mm]). They reported no major complications. Another prospective multicenter study on 31 PCLs (14 NETs, 16 IPMNs, 1 MCN) showed that at 1-year follow-up, 86% (12/14) NETs had complete resolution and 71% (12/17) mucinous cysts had diameter decreased >50%. They also showed resolution rate of 100% in mural nodules. Excluding the first 2 cases, only one case had a complication of pancreatic duct stenosis (3.5%, overall 10%).[69] A phase II multicenter clinical trial (NCT02343692) for RFA is currently recruiting participants with PCLs to evaluate outcomes at 12 months following RFA (https://clinicaltrials. gov/ct2/show/study/NCT02343692).
DISCUSSION
EUS-guided ablation of PCLs is a promising approach to treating precancerous lesions. Ethanol ablation has shown complete resolution in 9%–85% cases with majority of studies reporting complete resolution in 33%–45% range.[24,36,37,38,39,40] EUS chemoablation with or without ethanol lavage has reported rates of complete resolution ranging from 50% to 78.5% and with most studies reporting close to 60% efficacy. Lauromacrogol ablation and RFA have very limited data comprising of only 2 studies each with resolution rates 37%–51% and 33%–71%, respectively.[56,57,68,69] Another treatment modality is EUS-guided cyroablation, however, data is limited to one study for locally advanced pancreatic adenocarcinoma and not PCLs.[70] At present, chemoablation has better cyst resolution rates compared to other existing minimally invasive techniques including alcohol, lauromacrogol, and RFA as summarized in Table 3.
Table 3.
Efficacy comparison between available EUS guided ablative therapies (N is the sum of all patients from studies examining specific ablative technique; complete resolution is the sum of all patients that had this outcome in each study)
| PCLs ablative technique | n | Complete resolution, n (%) |
|---|---|---|
| Paclitaxel ablation | 347 | 221 (63.6) |
| Ethanol ablation | 201 | 68 (32.8) |
| Lauromacrogol ablation | 64 | 29 (45.3) |
| Radiofrequency ablation | 30 | 12 (70.6) |
PCLs: Pancreatic cystic lesions
Novel therapies have aimed at improving the efficacy of EUS chemoablation. Multiple nanotechnology-based drug delivery systems have been developed to allow for targeted drug delivery and prevent clearance by the immune and circulatory system.[71,72] Augmentation of chemoablation is also being studied by direct administration of large surface area microparticle (LSAM) paclitaxel called Nanopac® (NanOlogy, Fort Worth, TX). In an open-label trial, 19 participants were enrolled and using EUS-guided technique, LSAM paclitaxel was injected into mucinous PCL.[73] All participants that finished the study had low to undetectable systemic paclitaxel concentrations and 12/17 (71%) patients had reduction in cyst volume. This preliminary data suggests that LSAM paclitaxel may be retained inside the cyst, thereby prolonging the duration of chemotherapy to the PCL epithelial lining. It also implies that LSAM paclitaxel may prevent some of the systemic toxicity associated with chemotherapy. While more data is required before conclusions can be drawn regarding EUS-guided LSAM paclitaxel cyst ablation, the Phase 2 of this study, intracystic injection of NanoPac® in subjects with mucinous cystic pancreatic neoplasms (https://clinicaltrials.gov/ct2/show/study/NCT03188991), is currently underway. This study comprises 19 participants; outcomes include the safety and tolerability of two sequential EUS-guided LSAM paclitaxel doses.
Although EUS chemoablation has been practiced for over a decade and has reported long-term efficacy and safety, it has not substituted surgery. Our current EUS chemoablation data is from a few studies with a total of 347 patients where EUS chemoablation completely resolved 63.6% cysts ranging from MCNs, IPMNs, SCN, pseudocyst, and other indeterminate cysts. These studies have consistently shown good rates of resolution. In addition, recurrence rates after cyst resolution are very low.[29] Trials have shown that the most common major complication after EUS chemoablation is acute pancreatitis. Moyer et al.[54,55] showed that this complication can be reduced by avoiding ethanol lavage. While the highest rates of acute pancreatitis following EUS-guided ablation procedures have approached 20%, over 60% of patients undergoing pancreatic surgery (pancreatoduodenectomy) developed postoperative acute pancreatitis.[74] Postoperative acute pancreatitis is associated with increased morbidity, pancreatic fistula, and prolonged hospitalization.[74] In addition, none of the EUS ablation studies have reported mortality from the procedure, which is not the case for pancreatic surgeries. The risk of mortality after pancreatic surgeries ranges from 1.3% to 2.5% at 30 days and 4.1%–7.1% at 90 days.[75] Therefore, compared to the morbidity and mortality rates from surgery, EUS-guided ablation offers a relatively safer option for PCL management in appropriate patients.
The heterogeneity in patient inclusion criteria across the studies in terms of cyst diameter and cyst type along with the variation in EUS-guided ablation techniques limit comparison between them. Due to the lack of high-accuracy in EUS-guided diagnostic evaluation of PCLs, most studies have included nonmucinous cysts such as SCA or pseudocysts for chemoablation which have very low malignant potential. Only 4 studies have reported resolution rates for various cyst diagnosis.[29,50,53,55] The complete resolution after EUS-guided paclitaxel ablation for mucinous cysts (IPMNs and MCNs) was observed in 82/125 (65.6%) cases, which is comparable to those of all cyst types. Individual data on MCNs and IPMNs is further limited to one study which reported complete resolution in 4/9 (44%) cases for MCN and 19/27 (70%) cases for IPMN.[55] For ethanol ablation, only one study enrolled exclusively branch duct IPMNs and reported similar rates of complete resolution as other studies with various PCLs.[38] One of the primary reasons for limited data is the dependence on suboptimal diagnostic techniques for PCLs. This limits the data on EUS-guided ablation of purely mucinous pancreatic cysts.
Utilization of cyst fluid molecular analysis and confocal endomicroscopy improves diagnosis of PCLs and should be used for screening patients for mucinous lesions and CNETs before endoscopic chemoablation.[76,77,78] Enrolling patients with accurate diagnosis (IPMN, MCN, CNETs) and performing with standardized techniques (same number of chemoablation injections, RFA voltage) will provide more comparable data. Further, close monitoring of cyst size and intracystic fluid change analysis can provide additional data for resolution. Future trials can also aim at enrolling patients who will undergo surgery to assess for the ablative effect on cyst epithelium. Data from novel chemotherapeutics including LSAM paclitaxel will also play an important role in the management guidelines of PCLs. A case study performed RFA followed by lauromacrogol ablation reported complete resolution at 3-month follow-up.[79] Similar studies that combine of multiple ablative techniques should also be evaluated for PCL management.
More studies on newer techniques such as RFA and cryoablation are needed. RFA destroys septation which would improve chemoablation effects on PCL and simultaneously, chemoablation compensates for heterogenous destruction by RFA. Future studies should combine various ablative techniques to assess for enhancement in complete resolution rates of PCLs. Overall, data on complications and safety will be critical for the success of these techniques in the future.
CONCLUSION
EUS-guided ablation of PCLs is becoming increasingly recognized as a therapeutic option for patients not undergoing surgery. Further, application of advanced EUS diagnostics with confocal laser endomicroscopy and cyst fluid molecular analysis will provide higher specificity in the diagnosis of cyst type facilitating EUS-guided ablation specifically in precancerous cyst types. With multiple open-label studies on RFA, EUS chemoablation, or its variants currently underway, there will be more data coming in the next 5 years that will define the course of these techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Elta GH, Enestvedt BK, Sauer BG, et al. ACG clinical guideline: Diagnosis and management of pancreatic cysts. Am J Gastroenterol. 2018;113:464–79. doi: 10.1038/ajg.2018.14. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738–53. doi: 10.1016/j.pan.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Jais B, Rebours V, Malleo G, et al. Serous cystic neoplasm of the pancreas: A multinational study of 2622 patients under the auspices of the International Association of Pancreatology and European Pancreatic Club (European Study Group on Cystic Tumors of the Pancreas) Gut. 2016;65:305–12. doi: 10.1136/gutjnl-2015-309638. [DOI] [PubMed] [Google Scholar]
- 4.Valsangkar NP, Morales-Oyarvide V, Thayer SP, et al. 851 resected cystic tumors of the pancreas: A 33-year experience at the Massachusetts General Hospital. Surgery. 2012;152:S4–12. doi: 10.1016/j.surg.2012.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laurent L, Vullierme MP, Rebours V, et al. Estimation of the prevalence of intraductal papillary mucinous neoplasm of the pancreas in the French population through patients waiting for liver transplantation. United European Gastroenterol J. 2017;5:499–503. doi: 10.1177/2050640616664842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–97. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Allen PJ, D’Angelica M, Gonen M, et al. A selective approach to the resection of cystic lesions of the pancreas: Results from 539 consecutive patients. Ann Surg. 2006;244:572–82. doi: 10.1097/01.sla.0000237652.84466.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maggi G, Guarneri G, Gasparini G, et al. Pancreatic cystic neoplasms: What is the most cost-effective follow-up strategy? Endosc Ultrasound. 2018;7:319–22. doi: 10.4103/eus.eus_44_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karoumpalis I, Christodoulou DK. Cystic lesions of the pancreas. Ann Gastroenterol. 2016;29:155–61. doi: 10.20524/aog.2016.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Machado NO, Al Qadhi H, Al Wahibi K. Intraductal papillary mucinous neoplasm of pancreas. N Am J Med Sci. 2015;7:160–75. doi: 10.4103/1947-2714.157477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta R, Mortelé KJ, Tatli S, et al. Pancreatic intraductal papillary mucinous neoplasms: Role of CT in predicting pathologic subtypes. AJR Am J Roentgenol. 2008;191:1458–64. doi: 10.2214/AJR.07.3302. [DOI] [PubMed] [Google Scholar]
- 12.Bae SY, Lee KT, Lee JH, et al. Proper management and follow-up strategy of branch duct intraductal papillary mucinous neoplasms of the pancreas. Dig Liver Dis. 2012;44:257–60. doi: 10.1016/j.dld.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 14.Scheiman JM, Hwang JH, Moayyedi P. American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148:824–48.e22. doi: 10.1053/j.gastro.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Stark A, Donahue TR, Reber HA, et al. Pancreatic cyst disease: A review. JAMA. 2016;315:1882–93. doi: 10.1001/jama.2016.4690. [DOI] [PubMed] [Google Scholar]
- 16.Moayyedi P, Weinberg DS, Schünemann H, et al. Management of pancreatic cysts in an evidence-based world. Gastroenterology. 2015;148:692–5. doi: 10.1053/j.gastro.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 17.Ofosu A, Ramai D, Adler DG. Endoscopic ultrasound-guided ablation of pancreatic cystic neoplasms: Ready for prime time? Ann Gastroenterol. 2019;32:39–45. doi: 10.20524/aog.2018.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Celikoglu SI, Celikoglu F, Goldberg EP. Endobronchial intratumoral chemotherapy (EITC) followed by surgery in early non-small cell lung cancer with polypoid growth causing erroneous impression of advanced disease. Lung Cancer. 2006;54:339–46. doi: 10.1016/j.lungcan.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Brem H, Piantadosi S, Burger PC, et al. Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. The Polymer-brain Tumor Treatment Group. Lancet. 1995;345:1008–12. doi: 10.1016/s0140-6736(95)90755-6. [DOI] [PubMed] [Google Scholar]
- 20.Hader WJ, Steinbok P, Hukin J, et al. Intratumoral therapy with bleomycin for cystic craniopharyngiomas in children. Pediatr Neurosurg. 2000;33:211–8. doi: 10.1159/000055955. [DOI] [PubMed] [Google Scholar]
- 21.Markman M, Rowinsky E, Hakes T, et al. Phase I trial of intraperitoneal taxol: A Gynecoloic Oncology Group study. J Clin Oncol. 1992;10:1485–91. doi: 10.1200/JCO.1992.10.9.1485. [DOI] [PubMed] [Google Scholar]
- 22.Chang KJ, Nguyen PT, Thompson JA, et al. Phase I clinical trial of allogeneic mixed lymphocyte culture (cytoimplant) delivered by endoscopic ultrasound – Guided fine-needle injection in patients with advanced pancreatic carcinoma. Cancer. 2000;88:1325–35. doi: 10.1002/(sici)1097-0142(20000315)88:6<1325::aid-cncr8>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 23.Hecht JR, Bedford R, Abbruzzese JL, et al. A phase I/II trial of intratumoral endoscopic ultrasound injection of ONYX-015 with intravenous gemcitabine in unresectable pancreatic carcinoma. Clin Cancer Res. 2003;9:555–61. [PubMed] [Google Scholar]
- 24.Gan SI, Thompson CC, Lauwers GY, et al. Ethanol lavage of pancreatic cystic lesions: Initial pilot study. Gastrointest Endosc. 2005;61:746–52. doi: 10.1016/s0016-5107(05)00320-2. [DOI] [PubMed] [Google Scholar]
- 25.Teoh AY, Seo DW, Brugge W, et al. Position statement on EUS-guided ablation of pancreatic cystic neoplasms from an international expert panel. Endosc Int Open. 2019;7:E1064–77. doi: 10.1055/a-0959-5870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moyer MT, Maranki JL, DeWitt JM. EUS-guided pancreatic cyst ablation: A clinical and technical review. Curr Gastroenterol Rep. 2019;21:19. doi: 10.1007/s11894-019-0686-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67:789–804. doi: 10.1136/gutjnl-2018-316027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh HC, Brugge WR. EUS-guided pancreatic cyst ablation: A critical review (with video) Gastrointest Endosc. 2013;77:526–33. doi: 10.1016/j.gie.2012.10.033. [DOI] [PubMed] [Google Scholar]
- 29.Choi JH, Seo DW, Song TJ, et al. Long-term outcomes after endoscopic ultrasound-guided ablation of pancreatic cysts. Endoscopy. 2017;49:866–73. doi: 10.1055/s-0043-110030. [DOI] [PubMed] [Google Scholar]
- 30.Pergolini I, Sahora K, Ferrone CR, et al. Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology. 2017;153:1284–94.e1. doi: 10.1053/j.gastro.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 31.Larssen TB, Jensen DK, Viste A, et al. Single-session alcohol sclerotherapy in symptomatic benign hepatic cysts.Long-term results. Acta Radiol. 1999;40:636–8. doi: 10.3109/02841859909175601. [DOI] [PubMed] [Google Scholar]
- 32.Bennedbaek FN, Hegedüs L. Treatment of recurrent thyroid cysts with ethanol: A randomized double-blind controlled trial. J Clin Endocrinol Metab. 2003;88:5773–7. doi: 10.1210/jc.2003-031000. [DOI] [PubMed] [Google Scholar]
- 33.Fletcher S, Kanagasundaram NS, Rayner HC, et al. Assessment of ultrasound guided percutaneous ethanol injection and parathyroidectomy in patients with tertiary hyperparathyroidism. Nephrol Dial Transplant. 1998;13:3111–7. doi: 10.1093/ndt/13.12.3111. [DOI] [PubMed] [Google Scholar]
- 34.Völk M, Rogler G, Strotzer M, et al. Post-traumatic pseudocyst of the spleen: Sclerotherapy with ethanol. Cardiovasc Intervent Radiol. 1999;22:246–8. doi: 10.1007/s002709900375. [DOI] [PubMed] [Google Scholar]
- 35.Yamamoto S, Miyake I, Takatori K, et al. Percutaneous ethanol injection for unresectable pancreatic cancer-report of two cases. Gan To Kagaku Ryoho. 1998;25:1969–71. [PubMed] [Google Scholar]
- 36.Caillol F, Poincloux L, Bories E, et al. Ethanol lavage of 14 mucinous cysts of the pancreas: A retrospective study in two tertiary centers. Endosc Ultrasound. 2012;1:48–52. doi: 10.7178/eus.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeWitt J, McGreevy K, Schmidt CM, et al. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: A randomized, double-blind study. Gastrointest Endosc. 2009;70:710–23. doi: 10.1016/j.gie.2009.03.1173. [DOI] [PubMed] [Google Scholar]
- 38.DiMaio CJ, DeWitt JM, Brugge WR. Ablation of pancreatic cystic lesions: The use of multiple endoscopic ultrasound-guided ethanol lavage sessions. Pancreas. 2011;40:664–8. doi: 10.1097/MPA.0b013e3182128d06. [DOI] [PubMed] [Google Scholar]
- 39.Gómez V, Takahashi N, Levy MJ, et al. EUS-guided ethanol lavage does not reliably ablate pancreatic cystic neoplasms (with video) Gastrointest Endosc. 2016;83:914–20. doi: 10.1016/j.gie.2015.08.069. [DOI] [PubMed] [Google Scholar]
- 40.Park JK, Song BJ, Ryu JK, et al. Clinical Outcomes of Endoscopic Ultrasonography–Guided Pancreatic Cyst Ablation. Pancreas. 2016;45:889–894. doi: 10.1097/MPA.0000000000000567. [DOI] [PubMed] [Google Scholar]
- 41.Rowinsky EK, Cazenave LA, Donehower RC. Taxol: A novel investigational antimicrotubule agent. J Natl Cancer Inst. 1990;82:1247–59. doi: 10.1093/jnci/82.15.1247. [DOI] [PubMed] [Google Scholar]
- 42.Wilson L. Microtubules as drug receptors: Pharmacological properties of microtubule protein. Ann N Y Acad Sci. 1975;253:213–31. doi: 10.1111/j.1749-6632.1975.tb19201.x. [DOI] [PubMed] [Google Scholar]
- 43.Manfredi JJ, Parness J, Horwitz SB. Taxol binds to cellular microtubules. J Cell Biol. 1982;94:688–96. doi: 10.1083/jcb.94.3.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parness J, Horwitz SB. Taxol binds to polymerized tubulin in vitro . J Cell Biol. 1981;91:479–87. doi: 10.1083/jcb.91.2.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rao S, Krauss NE, Heerding JM, et al. 3’-(p-azidobenzamido) taxol photolabels the N-terminal 31 amino acids of beta-tubulin. J Biol Chem. 1994;269:3132–4. [PubMed] [Google Scholar]
- 46.Crossin KL, Carney DH. Microtubule stabilization by taxol inhibits initiation of DNA synthesis by thrombin and by epidermal growth factor. Cell. 1981;27:341–50. doi: 10.1016/0092-8674(81)90417-7. [DOI] [PubMed] [Google Scholar]
- 47.Rowinsky EK, Donehower RC. Paclitaxel (Taxol) N Engl J Med. 1995;332:1004–14. doi: 10.1056/NEJM199504133321507. [DOI] [PubMed] [Google Scholar]
- 48.Oh HC, Seo DW, Lee TY, et al. New treatment for cystic tumors of the pancreas: EUS-guided ethanol lavage with paclitaxel injection. Gastrointest Endosc. 2008;67:636–42. doi: 10.1016/j.gie.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 49.Kandula M, Moole H, Cashman M, et al. Success of endoscopic ultrasound-guided ethanol ablation of pancreatic cysts: A meta-analysis and systematic review. Indian J Gastroenterol. 2015;34:193–9. doi: 10.1007/s12664-015-0575-2. [DOI] [PubMed] [Google Scholar]
- 50.Oh HC, Seo DW, Kim SC, et al. Septated cystic tumors of the pancreas: Is it possible to treat them by endoscopic ultrasonography-guided intervention? Scand J Gastroenterol. 2009;44:242–7. doi: 10.1080/00365520802495537. [DOI] [PubMed] [Google Scholar]
- 51.DeWitt JM, Al-Haddad M, Sherman S, et al. Alterations in cyst fluid genetics following endoscopic ultrasound-guided pancreatic cyst ablation with ethanol and paclitaxel. Endoscopy. 2014;46:457–64. doi: 10.1055/s-0034-1365496. [DOI] [PubMed] [Google Scholar]
- 52.Kim KH, McGreevy K, La Fortune K, et al. Sonographic and cyst fluid cytologic changes after EUS-guided pancreatic cyst ablation. Gastrointest Endosc. 2017;85:1233–42. doi: 10.1016/j.gie.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 53.Oh HC, Seo DW, Song TJ, et al. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancreatic cysts. Gastroenterology. 2011;140:172–9. doi: 10.1053/j.gastro.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 54.Moyer MT, Dye CE, Sharzehi S, et al. Is alcohol required for effective pancreatic cyst ablation? The prospective randomized CHARM trial pilot study. Endosc Int Open. 2016;4:E603–7. doi: 10.1055/s-0042-105431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moyer MT, Sharzehi S, Mathew A, et al. The safety and efficacy of an alcohol-free pancreatic cyst ablation protocol. Gastroenterology. 2017;153:1295–303. doi: 10.1053/j.gastro.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 56.Linghu E, Du C, Chai N, et al. A prospective study on the safety and effectiveness of using lauromacrogol for ablation of pancreatic cystic neoplasms with the aid of EUS. Gastrointest Endosc. 2017;86:872–80. doi: 10.1016/j.gie.2017.03.1525. [DOI] [PubMed] [Google Scholar]
- 57.Du C, Chai N, Linghu E, et al. Long-term outcomes of EUS-guided lauromacrogol ablation for the treatment of pancreatic cystic neoplasms: 5 years of experience. Endosc Ultrasound. 2021 doi: 10.4103/EUS-D-20-00231. [doi: 10.4103/EUS-D-20-00231] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Paiella S, Salvia R, Ramera M, et al. Local ablative strategies for ductal pancreatic cancer (radiofrequency ablation, irreversible electroporation): A review. Gastroenterol Res Pract. 2016;2016:4508376. doi: 10.1155/2016/4508376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Giardino A, Innamorati G, Ugel S, et al. Immunomodulation after radiofrequency ablation of locally advanced pancreatic cancer by monitoring the immune response in 10 patients. Pancreatology. 2017;17:962–6. doi: 10.1016/j.pan.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 60.Wang D, Jin Z, Lei W, et al. Mo1524 endoscopic ultrasound guided radiofrequency ablation for the treatment of advanced pancreatic carcinoma. Gastrointest Endosc. 2013;77:AB414. [Google Scholar]
- 61.Song TJ, Seo DW, Lakhtakia S, et al. Initial experience of EUS-guided radiofrequency ablation of unresectable pancreatic cancer. Gastrointest Endosc. 2016;83:440–3. doi: 10.1016/j.gie.2015.08.048. [DOI] [PubMed] [Google Scholar]
- 62.Scopelliti F, Pea A, Conigliaro R, et al. Technique, safety, and feasibility of EUS-guided radiofrequency ablation in unresectable pancreatic cancer. Surg Endosc. 2018;32:4022–8. doi: 10.1007/s00464-018-6217-x. [DOI] [PubMed] [Google Scholar]
- 63.Yang J, Zhang X. Tu1357 FEASIBILITY AND SAFETY OF EUS-GUIDED RADIOFREQUENCY ABLATION IN UNRESECTABLE PANCREATIC CANCER. Gastrointest Endosc. 2019;89:AB588–9. [Google Scholar]
- 64.Crinò SF, D’Onofrio M, Bernardoni L, et al. EUS-guided radiofrequency ablation (EUS-RFA) of solid pancreatic neoplasm using an 18-gauge needle electrode: feasibility, safety, and technical success. J Gastrointestin Liver Dis. 2018;27:67–72. doi: 10.15403/jgld.2014.1121.271.eus. [DOI] [PubMed] [Google Scholar]
- 65.Choi JH, Seo DW, Song TJ, et al. Endoscopic ultrasound-guided radiofrequency ablation for management of benign solid pancreatic tumors. Endoscopy. 2018;50:1099–104. doi: 10.1055/a-0583-8387. [DOI] [PubMed] [Google Scholar]
- 66.Oleinikov K, Dancour A, Epshtein J, et al. Endoscopic ultrasound-guided radiofrequency ablation: A new therapeutic approach for pancreatic neuroendocrine tumors. J Clin Endocrinol Metab. 2019;104:2637–47. doi: 10.1210/jc.2019-00282. [DOI] [PubMed] [Google Scholar]
- 67.Lakhtakia S, Ramchandani M, Galasso D, et al. EUS-guided radiofrequency ablation for management of pancreatic insulinoma by using a novel needle electrode (with videos) Gastrointest Endosc. 2016;83:234–9. doi: 10.1016/j.gie.2015.08.085. [DOI] [PubMed] [Google Scholar]
- 68.Pai M, Habib N, Senturk H, et al. Endoscopic ultrasound guided radiofrequency ablation, for pancreatic cystic neoplasms and neuroendocrine tumors. World J Gastrointest Surg. 2015;7:52–9. doi: 10.4240/wjgs.v7.i4.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barthet M, Giovannini M, Lesavre N, et al. Endoscopic ultrasound-guided radiofrequency ablation for pancreatic neuroendocrine tumors and pancreatic cystic neoplasms: A prospective multicenter study. Endoscopy. 2019;51:836–42. doi: 10.1055/a-0824-7067. [DOI] [PubMed] [Google Scholar]
- 70.Arcidiacono PG, Carrara S, Reni M, et al. Feasibility and safety of EUS-guided cryothermal ablation in patients with locally advanced pancreatic cancer. Gastrointest Endosc. 2012;76:1142–51. doi: 10.1016/j.gie.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 71.Brigger I, Dubernet C, Couvreur P. Nanoparticles in cancer therapy and diagnosis. Adv Drug Deliv Rev. 2002;54:631–51. doi: 10.1016/s0169-409x(02)00044-3. [DOI] [PubMed] [Google Scholar]
- 72.Zhao M, Liu M. New avenues for nanoparticle-related therapies. Nanoscale Res Lett. 2018;13:136. doi: 10.1186/s11671-018-2548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Othman M, Tabash A, Verco S, et al. 69 NanoPac-2017-01 Mid-study eport: Safety, tolerability, and preliminary efficacy of intracystic submicron particle paclitaxel (SPP) for the treatment of mucinous cysts. J Am Coll Gastroenterol. 2019;114:S42. [Google Scholar]
- 74.Ikenaga N, Ohtsuka T, Nakata K, et al. Clinical significance of postoperative acute pancreatitis after pancreatoduodenectomy and distal pancreatectomy. Surgery. 2021;169:732–7. doi: 10.1016/j.surg.2020.06.040. [DOI] [PubMed] [Google Scholar]
- 75.Wegner RE, Verma V, Hasan S, et al. Incidence and risk factors for post-operative mortality, hospitalization, and readmission rates following pancreatic cancer resection. J Gastrointest Oncol. 2019;10:1080–93. doi: 10.21037/jgo.2019.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Konjeti VR, McCarty TR, Rustagi T. Needle-based confocal laser endomicroscopy (nCLE) for evaluation of pancreatic cystic lesions: A systematic review and meta-analysis. J Clin Gastroenterol. 2022;56:72–80. doi: 10.1097/MCG.0000000000001468. [DOI] [PubMed] [Google Scholar]
- 77.Krishna SG, Hart PA, Malli A, et al. Endoscopic ultrasound-guided confocal laser endomicroscopy increases accuracy of differentiation of pancreatic cystic lesions. Clin Gastroenterol Hepatol. 2020;18:432–40.e6. doi: 10.1016/j.cgh.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 78.Singhi AD, McGrath K, Brand RE, et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 2018;67:2131–41. doi: 10.1136/gutjnl-2016-313586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Feng X, Linghu E, Chai N, et al. New treatment of the pancreatic cystic neoplasm: Endoscopic ultrasonography-guided radiofrequency ablation combined with lauromacrogol ablation. Turk J Gastroenterol. 2018;29:101–4. doi: 10.5152/tjg.2017.17340. [DOI] [PMC free article] [PubMed] [Google Scholar]


