Abstract
Objective: With the increasing effects of stress caused by the COVID-19 pandemic and occupational stress on the mental health of frontline nurses, it is imperative to further investigate how these stresses affect nurses’ mental health and secondary traumatic stress syndrome. This research aimed to investigate the relationship of nurses' occupational stress and concerns about COVID-19 with secondary traumatic stress syndrome, and also to investigate the mediating effect that concerns about the COVID-19 pandemic have on the relationship between nurses' occupational stress and secondary traumatic stress syndrome.
Method : A cross-sectional design was adopted. The population of the study was defined as all front-line nurses in Shiraz hospitals, from which 225 nurses of two corona care hospitals were selected using convenience sampling. The degree of secondary traumatic stress, concerns about the COVID-19, and nurses' occupational stress were assessed using Bride’s Secondary Traumatic Stress Scale (STSS), an adopted version of Level of Concerns about the COVID-19 questionnaire, and the Nurses’ Occupational Stressor Scale (NOSS) among Hospital-based Healthcare Workers. Structural equation modeling (SEM) was used to examine the relationships among variables.
Results: Results showed that nurses’ occupational stresses presented a direct effect on nurses’ level of concern about the COVID-19 pandemic (β = 0.85, P < 0.001), and concern about the COVID-19 pandemic was directly related to front-line nurse's secondary traumatic stress syndrome (β = 0.83, P < 0.001). In addition, nurses’ level of concern about the COVID-19 pandemic fully mediated the effects of nurses’ occupational stresses on their secondary traumatic stress (β = 0.70, P < 0.001). This indirect effect has explained 68% of the variance in nurses’ secondary traumatic stress.
Conclusion: These results emphasized the indirect effect of nurses’ occupational stresses on secondary traumatic stress syndrome via mediating the level of concern about COVID-19. Therefore, to reduce the secondary traumatic stress of nurses who have dealt directly with COVID-19 patients, it seems necessary to pay serious attention to the sources of their occupational stress, which probably existed even before this pandemic and increased their concerns in pandemic conditions.
Key Words: COVID-19, Nurses, Occupational Stress, Secondary Traumatic Stress
The COVID-19 outbreak, which spread from China in late 2019, quickly became an international health emergency issue affecting people's health, economy, and lives (1). Antonio Guterres (2020), United Nations Secretary-General, has called on governments around the world to focus on mental health services provided to their populations, especially for frontline healthcare workers (HCWs) (2). Frontline HCWs play a crucial role in providing care to infected persons. Several stressful conditions are resulting from the pandemic, including a rapid increase in the number of infected patients, employment of nurses from non-pulmonary wards to care for patients with COVID-19, a limited knowledge about the clinical presentations and effective drugs, as well as inadequate protective supplies (3, 4). Thus, those conditions subject HCWs, especially frontline nurses, to heavy psychological and physical pressure (5).
In a systematic review, Cabarkapa et al. (2020) stated that frontline HCWs may develop stress-related disorders, such as Secondary Traumatic Stress Syndrome (STSS), under the COVID-19 pandemic, like previous epidemics including Ebola, Severe Acute Respiratory Syndrome (SARS), and Middle East Respiratory Syndrome (MERS) (6). In addition, studies emphasize that these complications can continue for a long time and affect the mental health and efficiency of nurses (7, 8). Therefore, to deal with those complications, special attention should be paid to how they occur and affect nurses, particularly frontline nurses who are at greater risk of developing such complications during pandemics (9).
In 1982, Figley described secondary trauma as secondary victimization for the first time and developed STSS and compassion fatigue (CF) at a later time (10). Indeed, He argued that STSS and Post Traumatic Stress Disorder (PTSD) are similar in that they have both signs and symptoms such as re-experiencing, avoidance and arousal. However, unlike PTSD, which occurs as a result of a direct (primary) traumatic event, STSS is the result of an indirect (secondary) traumatic event (11).
The model of compassion stress and fatigue (Figley, 1995a-2002) explained how prolonged exposure to suffering clients elevates STSS of HCWs during their work hours (11, 12). Exposure to suffering clients is the first pathway to STSS where workers assume the client suffer and internalize, to an extent, the expressed emotional energy from each encounter (13). Other models, hypotheses, and researches about CF and STSS (13-19) also emphasize the potential increase in STSS because of prolonged, continuous, and intense contact with patients (including time spent with clients with trauma, caseload, and total exposure). They further emphasize the increased use of resources, as well as environmental and work-related stress. Among HCWs, nurses are more likely to be exposed to patients who have experienced trauma and thus may be prone to STSS. Furthermore, stressful situations caused by the COVID-19 pandemic have made these consequences even more complicated. The prevalence of STSS among nurses ranged from 4% to 13% in researches performed before the COVID-19 outbreak (20). However, Orrù et al. (2020) demonstrated that the prevalence of secondary traumatic stress was nearly 47.5% among frontline nurses during the COVID-19 pandemic (21). Taking into account the variables affecting the development of STSS in nurses based on previous studies, it seems that, during the outbreak, two variables, including “concerns about the COVID-19 pandemic” and “occupational stress”, had the highest impact on the development of STSS among frontline nurses (21). Therefore, it is important to pay more attention to how these variables affect the development of STSS.
Compared to previous epidemics, Corona virus has spread more rapidly, in part due to increased communication and globalization (3). The high number of patients and mortality rate due to the COVID-19 virus (22) as well as its rapid spread have made this pandemic unique and one of the main sources of stress, which in turn cause STSS in HCWs (21). Different sources of stress have been reported among frontline HCWs. They include physical exhaustion, uncertainty about the disease progression and treatment, fear of getting infected, stigma, overwhelming workload, isolation, lack of personal protective equipment, and exposure to the suffering and death of patients (23-31). These stressful sources can altogether be considered as one independent variable, namely the variable of “concerns about the COVID-19 pandemic” among frontline nurses (32). Based on researches conducted on the SARS, MERS, and avian influenza epidemics, these concerns are classified into 5 distinct domains including workplace-related, social status, self-satisfaction, government-related, and infection-control-related domains (33-35). Due to the prominent role of concerns related to COVID-19 and the five distinct domains in stressing and their consequences during the pandemic, this study considered the effect of this variable on STSS development among frontline nurses.
Another variable that seems to play a major role during the coronavirus epidemic and affects STSS is occupational stress (36), which is generally one of the most influential factors on mental and physical health in the nursing profession (37-39). As demonstrated in previous researches, nurses are the most exposed to occupational stress among HCWs (40). Indeed, when nurses' needs are not met in the workplace, they are more likely to experience varying levels of occupational stress, which can harm their mental health and job performance (38, 41, 42). Long working hours, night shifts, conflict between work roles, lack of support, workplace violence and bullying, insufficient salaries, and strictness on taking leave, are factors that can contribute to occupational stress (43, 44). Dagget, Molla & Belachew (2016) estimated the prevalence of job stress in the range of 9.2 - 68% among nurses in different countries (37).
Of the factors that can be attributed to the occupational stress of nurses in several countries are the measures that health organizations have taken to improve their working conditions. These measures are especially important during the COVID-19 outbreak, which, in addition to the usual occupational stress, expose nurses to physical and psychological problems (45). Oh et al. (2017) mentioned that nurses who were exposed to the MERS experienced lower levels of stress when they were properly supplied with goods and training in the hospital (46). Considering the organizational factors, it can be said that a lower level of occupational stress is expected for nurses in organizations where necessary interventions have been taken for reducing stressors. Given the current concern with the COVID-19 pandemic, identifying the factors affecting mental health is required to allow policymakers to enact guidance for protecting HCWs and frontline nurses in pandemics. In addition, Research conducted among front-line nurses in Western and Asian countries such as China has also identified the need to improve their psychological well-being (5, 25, 26). However, it needs to be determined whether the support measures and plans implemented in other geographical and cultural areas are applicable here as well. Therefore, it is necessary to study the psychological effects of COVID-19 in Iran and to understand the associated risks and possible protective factors. Then, optimal and efficient strategies to support and help mental health can be designed. For these reasons, this study examines the relationship of occupational stress and concerns about the COVID-19 Pandemic with STSS of frontline nurses and its pathway. Based on what was said, the proposed model of the present study is shown in Figure 1.
Figure 1.
Conceptual Model of the Relationship between Occupational Stress, Concerns about the COVID-19 and Secondary Traumatic Stress Syndrome
Materials and Methods
Design
A descriptive and cross-sectional design was adopted.
Participants
Two hospitals that have been introduced as corona care centers in Iran since the beginning of the COVID-19 pandemic were selected. The inclusion criteria of participants were as follows: 1) holding a valid registered nurse license; 2) being in direct contact with hospitalized patients with COVID-19; 3) consenting to participate in this study. Finally, 225 front-line nurses from these hospitals, selected by convenience sampling, participated in this study. Kline (2015) had suggested that 200 or more participants would be adequate for structural equation modeling (SEM) studies (47).
Data collection
After receiving the ethical approval from the Azad University of Kazeroon (IR.IAU.KAU.REC.1399.051), data was collected through an online questionnaire investigation in October and November 2020, which contained demographic characteristics, Secondary Traumatic Stress Scale, Nurses’ level of concerns about the COVID-19 outbreak, and Nurses’ occupational stressors. The purpose of the study was explained to participants, and they were also informed that participation in this study was anonymous and voluntary, and they could withdraw from the study at any time.
Instruments
The Secondary Traumatic Stress Scale was used to measure nurses' secondary traumatic stress (48). This scale includes 17 items that measure three components of secondary traumatic stress: intrusion (e.g., “Reminders of my work with clients upset me”), avoidance (e.g., “I had little interest in being around others”), and arousal (e.g., “I had trouble concentrating”). All the questions were based on a 5-point Likert scale from 1 (never) to 5 (very often). In Bride’s study, internal consistency of the STSS instrument was reported as 0.93 for the full STSS and 0.80, 0.87, and 0.83 for intrusion, avoidance, and arousal respectively. Also, fitness indices values of confirmatory factor analysis (CFA) for the three components were acceptable (48). In Iran, Ahmadi et al. (2013) reported Cronbach's alpha for intrusion, avoidance, arousal, and total score as 0.88, 0.80, 0.85 and 0.92 (P < 0.001) respectively (49). In the present study, STSS showed excellent internal consistency for the total score (Chronbach’s α = 0.97 and McDonald’s ω = 0.97), and the three components (intrusion: α = 0.88, avoidance: α = 0.92 and arousal: α = 0.93).
Nurses’ level of concerns about the COVID-19 outbreak was measured with an adapted version of a questionnaire designed by Abolfotouh et al. (2017) (35). This scale is a 31-item measure and was designed to assess the level of concern among hospital-based HCWs regarding MERS-Coronavirus. It consists of five dimensions, including self-satisfaction (e.g., “I feel unsafe working at my workplace”), social status (e.g., “I feel that I should limit my social activities due to COVID-19”), workplace (e.g., “I feel I should change my current job due to the COVID-19 crisis), infection control (e.g., “don’t feel an infection specialist is accessible to respond to my concerns”), and government (e.g., “I don’t feel COVID-19 has been highlighted and discussed efficiently in the media”). All items were assessed using a 4-point Likert scale from 1 (strongly disagree) to 4 (strongly agree). Since the Persian version of the psychometric properties of this questionnaire was not available, Cronbach's alpha was used to determine the internal consistency. For the five dimensions, including self-satisfaction, social status, workplace, infection control, and government, Cronbach's alphas were 0.90, 0.76, 0.86, 0.87 and 0.72 (P < 0.001) respectively. Also, the scale demonstrated good reliability for the total score (Chronbach’s α = 0.95 and McDonald’s ω = 0.95).
Nurses’ occupational stresses were measured by the Nurses’ Occupational Stressor Scale (NOSS) (50), which composes of nine subscales (workplace violence and bullying, work demands, insufficient support from coworkers or caregivers, work-family conflict, organizational issues, difficulty taking leave, powerlessness, occupational hazards, and unmet basic physiological needs). This measure comprises of 21 items, assessed using a 4-point Likert scale from 1 (strongly agree) to 4 (strongly disagree). However, the Persian version of NOSS (51) consists of two components: stress related to environmental-organizational factors and stress related to high workload. The internal consistency of these subscales was respectively α = 0.91 (ω = 0.91) and α = 0.90 (ω = 0.91). In the CFA process, fitness indices values for this two-factor structure were also acceptable (RMSEA = 0.06, GFI = 0.96, NFI = 0.95, CFI = 0.96, and CMIN/DF = 2.02).
Data analysis
Preliminary analysis was implemented by the SPSS 22.0 software. Checking of statistical assumptions, univariate and multivariate outliers as well as calculation of the mean, standard deviation, range, skewness and kurtosis, and correlation coefficients between research variables have been performed in this software. All analyses related to SEM were implemented in the AMOS 22.0 software. In SEM, full information maximum likelihood was used to confirm interrelationships and parameters among the variables. For model fit, the goodness of fit indices, such as the chi-square/degree of freedom ratio (CMIN/DF), the comparative fit index (CFI), the goodness of fit index (GFI), the normed fit index (NFI), the Tucker–Lewis Index (TLI), and the root mean square error of approximation index (RMSEA) were used. According to Kline (2016), an RMSEA ≤ 0.08, CMIN/DF < 5, and that of the rest of the indices such as GFI ≥ 0.90 indicated an adequate model fit (53).
Results
Demographic characteristics
A total of 225 qualified questionnaires were collected. Of the respondents, 170 (75.6%) were females, and 55 (24.4%) were males, aged between 23 to 52 years, (Mean = 34.32, SD = 6.73). The educational level of 89.3% of the nurses was bachelor of nursing, and of 10.7% of them was master of nursing. Participants had worked as a nurse for an average of 11.48 years (SD = 6.60). The majority of participants were married (61.8%, n = 139).
Descriptive and bivariate statistics
Descriptive statistics of observed variables used in the structural model (SM) are presented in Table 1. As shown in this Table, the values of skewness and kurtosis were calculated to determine the normality of the observed measures. The data met Kline’s (2016) thresholds for normality with a skewness of less than 3 and a kurtosis of less than 10 (52). In addition, Multivariate kurtosis (in AMOS) was also used to examine the multivariate normality, in which values less than 5 indicate the assumption of multivariate normality (53). In the present study, the value of this index was estimated to be 4.46. It should be noted that in the preliminary analysis, Mahalanobis distance has been used to identify multivariate outliers.
Table 1.
Descriptive and Bivariate Statistics of Occupational Stress, Concerns about the COVID-19 and Secondary Traumatic Stress Syndrome (N = 225)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
|
---- | |||||||||
|
0.76** | ---- | ||||||||
|
0.50** | 0.60** | ---- | |||||||
|
0.48** | 0.54** | 0.62** | ---- | ||||||
|
0.72** | 0.70** | 0.69** | 0.70** | ---- | |||||
|
0.60** | 0.63** | 0.65** | 0.63** | 0.81** | ---- | ||||
|
0.33** | 0.40** | 0.47** | 0.41** | 0.48** | 0.48** | ---- | |||
|
0.61** | 0.57** | 0.66** | 0.67** | 0.72** | 0.64** | 0.34** | ---- | ||
|
0.65** | 0.58** | 0.63** | 0.65** | 0.73** | 0.65** | 0.37** | 0.92** | ---- | |
|
0.65** | 0.58** | 0.59** | 0.65** | 0.72** | 0.60** | 0.30** | 0.86** | 0.85** | ---- |
| M | 27.49 | 29.30 | 20.27 | 14.99 | 20.76 | 13.08 | 17.41 | 18.83 | 14.24 | 12.29 |
| SD | 7.23 | 7.42 | 4.87 | 3.57 | 5.29 | 3.71 | 2.36 | 7.27 | 5.69 | 4.81 |
| Range | 12-39 | 12-40 | 7-28 | 7-24 | 10-32 | 5-20 | 6-20 | 7-33 | 5-25 | 5-22 |
| Skewness | -0.28 | -0.83 | -0.31 | 0.39 | 0.11 | -0.05 | -1.00 | 0.23 | 0.10 | 0.21 |
| Kurtosis | -0.94 | -0.25 | -0.45 | -0.48 | -0.85 | -0.70 | 2.10 | -1.00 | -1.00 | -1.12 |
Notes: Stress-SEO stress related to environmental-organizational factors; Stress-SHW stress related to high workload; COV-Se concerns about COVID-19-(self-satisfaction); COV-Ss concerns about COVID-19-(social status); COV-WO concerns about COVID-19-(workplace); COV-IN concerns about COVID-19-(infection); COV-GOV concerns about COVID-19-(government); Second-AV secondary traumatic stress-(avoidance); Second-AR secondary traumatic stress-(arousal); Second-IN secondary traumatic stress-(intrusion).
As shown in the Table 1, means, ranges, and standard deviations were used to describe the scores of the observed variables. In addition, Pearson’s correlation coefficients were used to assess the relationship between research variables. These coefficients indicated that most variables shared suitable levels of variation.
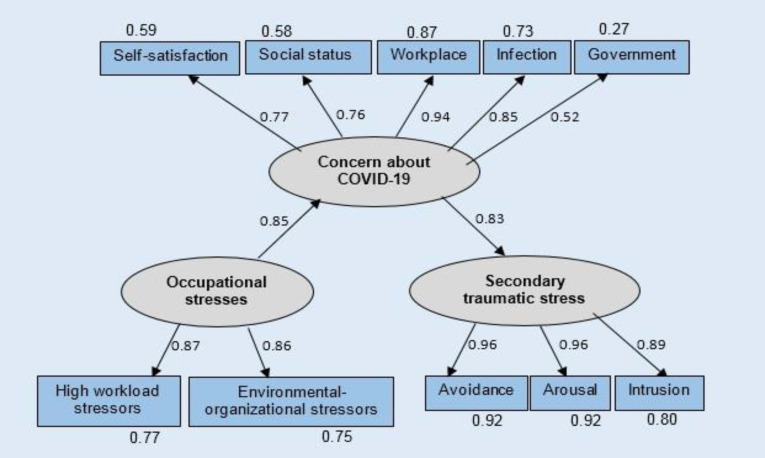
Structural model
After confirming the statistical assumptions, the proposed research model was tested using the SEM method. In the model, three subscales of the secondary traumatic stress scale (avoidance, arousal, and intrusion) were considered as indicators of the latent variable of secondary traumatic stress. For the latent variable of concerns about COVID-19, five subscales of self-satisfaction, social status, workplace, infection, and government were considered as observed variables. For the latent variable of occupational stress, the subscales of this scale (high workload stressors and environmental-organizational stressors) were selected as observed variables. In addition, in this model, the secondary traumatic stress variable was selected as an endogenous variable, the variable of concern about COVID- 19 was selected as a mediator variable and, the occupational stress variable was selected as an exogenous variable.
The values of goodness of fit indexes for the final model are reported in Table 2. As shown in this Table, the value of GFI, CFI, NFI and TLI are more than 0.95, which indicate an acceptable fitness (54). Also, the value of Normed Chi-square (CMIN/DF) was 2.78, which lies within the acceptable range (< 3). Moreover, the value of RMSEA was 0.075 which is very close to the acceptable value for this index. Therefore, generally, the goodness of fit indices for this model are appropriate.
Table 2.
Model Fit Indices for Structural Model of Secondary Traumatic Stress Syndrome
| CMIN/DF | GFI | CFI | IFI | NFI | TLI | RMSEA | |
|---|---|---|---|---|---|---|---|
| Value in the present model | 2.78 | 0.95 | 0.97 | 0.97 | 0.96 | 0.96 | 0.075 |
| Acceptable value | < 3 | > 0.95 | > 0.95 | > 0.95 | > 0.95 | > 0.95 | < 0.07 |
In this model (Figure 2), among the three indicators of the secondary traumatic stress, avoidance and arousal had more weight in defining this latent variable. But in the case of the latent variable of occupational stress, both indicators had equal shares in defining the variable. Among the indicators of the concerns about COVID-19 variable, workplace had more weight in defining the latent variable. The explained variance of the indices related to all latent variables is also reported in Figure 2. Additionally, as shown in Figure 2, nurses’ occupational stresses, as an endogenous variable, presented a direct effect on nurses’ level of concern about the COVID-19 pandemic (β = 0.84, P < 0.001). This direct effect has explained 71% of the variance in nurses’ level of concern about COVID-19. Moreover, nurses’ level of concern about the COVID-19 pandemic fully mediated the effects of nurses’ occupational stresses on their secondary traumatic stress (β = 0.70, P < 0.001). This indirect effect has explained 68% of the variance in nurses’ secondary traumatic stress.
Figure 2.
Structural Equation Modeling Analysis of the Direct and Indirect Effect of Occupational Stress and the Mediating Role of Concerns about COVID-19 on Secondary Traumatic Stress Syndrome
Table 3 listed the size of total effects, direct effects and indirect effects among these variables in the research model. All coefficients in this Table are standardized and significant at level 0.01.
Table 3.
The Result of Structural Equation Modeling for the Direct Effect of Occupational Stress, Concerns about the COVID-19 and Secondary Traumatic Stress Syndrome
| Paths | Direct effect | Indirect effect | Total effect |
|---|---|---|---|
| Occupational stresses→ Environmental-organizational stressors | 0.86 | 0.86 | |
| Occupational stresses→ High workload stressors | 0.87 | 0.87 | |
| Occupational stresses→ Concern about COVID-19 | 0.85 | 0.85 | |
| Concern about COVID-19→ Self-satisfaction | 0.77 | 0.77 | |
| Concern about COVID-19→ Social status | 0.76 | 0.76 | |
| Concern about COVID-19→ Workplace | 0.94 | 0.94 | |
| Concern about COVID-19→ Infection | 0.85 | 0.85 | |
| Concern about COVID-19→ Government | 0.52 | 0.52 | |
| Concern about COVID-19→ Secondary traumatic stress | 0.83 | 0.83 | |
| Secondary traumatic stress→ Arousal | 0.96 | 0.96 | |
| Secondary traumatic stress→ Avoidance | 0.96 | 0.96 | |
| Secondary traumatic stress→ Intrusion | 0.89 | 0.89 | |
| Occupational stresses→ Secondary traumatic stress | 0.70 | 0.70 | |
| Occupational stresses→ Arousal | 0.67 | 0.67 | |
| Occupational stresses→ Avoidance | 0.67 | 0.67 | |
| Occupational stresses→ Intrusion | 0.63 | 0.63 | |
| Occupational stresses→ Self-satisfaction | 0.65 | 0.65 | |
| Occupational stresses→ Social status | 0.65 | 0.65 | |
| Occupational stresses→ Workplace | 0.79 | 0.79 | |
| Occupational stresses→ Infection | 0.72 | 0.72 | |
| Occupational stresses→ Government | 0.44 | 0.44 | |
| Concern about COVID-19→ Arousal | 0.79 | 0.79 | |
| Concern about COVID-19→ Avoidance | 0.79 | 0.79 | |
| Concern about COVID-19→ Intrusion | 0.74 | 0.74 |
Notes: Stress-SEO stress related to environmental-organizational factors; Stress-SHW stress related to high workload; COV-Se concerns about COVID-19-(self-satisfaction); COV-Ss concerns about COVID-19-(social status); COV-WO concerns about COVID-19-(workplace); COV-IN concerns about COVID-19-(infection); COV-GOV concerns about COVID-19-(government); Second-AV secondary traumatic stress-(avoidance); Second-AR secondary traumatic stress-(arousal); Second-IN secondary traumatic stress-(intrusion).
To investigate the mediating role of the latent variable of concerns about COVID-19, we conducted the bootstrap analysis with 200 samples with a significance level of 0.05. The results of the bootstrap test showed that the indirect effect of occupational stress on secondary traumatic stress was significant, with the standard coefficient of 0.70 at P < 0.001 (95% confidence interval = 0.65-0.77). Therefore, concerns about COVID-19 had a mediating effect on the relationship of occupational stress with secondary traumatic stress.
Discussion
This research aimed at studying the relationship of occupational stress and concerns about COVID-19 with STSS and how the first two variables affect STSS among Iranian nurses, who are engaged in the front line of the COVID-19 pandemic. As the report by Kirkpatrick and Marshal (2020) show, Iran was the second-most infected country around the world by coronavirus followed by China (55). When this research was completed (24 February 2021), Iran was at the threshold of entering the fourth peak of the COVID-19 pandemic. Like other countries, the health care system in Iran was also in a critical condition resulting from the quick spread of the virus and a high rate of deaths. The mental and physical impacts of this pandemic on HCWs, particularly nurses, have been noted considerably.
As findings of this research demonstrate, the first hypothesis of this study, which held that there is a positive relationship between occupational stress and STSS of nurses working in frontline, is not confirmed. According to the study by Gupta & Sahoo (2002), performed on factors creating STSS, it is expected that increased occupational stress will result in increased STSS in HCWs including nurses (36). To justify this finding, it is guessed that the COVID-19 pandemic has put HCWs around the world, including Iran, under not experienced and unique conditions, where the World Health Organization (2020) declared the COVID-19 outbreak as pandemic within less than 4 months (56).
Thereby, people’s lives were affected because of compulsory quarantines, closed educational centers, restricted or banned transportation between cities of countries, and so on. Conditions were different at the time of SARS, MERS, and Ebola outbreaks, especially in Iran. Therefore, Iranian healthcare workers are facing a completely new occupational position, which they had never experienced it before, whether mentally, emotionally, or occupationally. In other words, it is possible that concerns about the COVID-19 pandemic may have turned into the focus of attention and the main resource of stress among Iranian nurses, who work in the frontline, and have marginalized the earlier mental and psychological effects of occupational stress.
The second hypothesis of the study, which held that there is a positive significant relationship between concerns about the COVID-19 pandemic and the development of STSS was confirmed. Based on the findings of this research, it can be suggested that as concerns about the COVID-19 pandemic increase among Iranian nurses who work in centers of care for patients infected by the COVID-19, the prevalence of STSS is highly expected. It is obvious that when nurses are highly concerned about the accuracy of governmental decisions on the COVID-19 pandemic; their family members’, friends’, and relatives’ infection; lack of suitable management in hospitals; restricted social activities; and inefficiency or inadequacy in confronting the coronavirus, they become also extremely vulnerable in the face of critically ill patients and quickly show the symptoms of STSS. As suggested in Oh et al. (2007), this may be a consequence of being not prepared for coping with a crisis and its effects on the prevalence of stress among HCWs (46).
The research findings also demonstrate that concerns about the COVID-19 pandemic mediate the relationship between occupational stress and STSS among Iranian nurses working in the frontline during the coronavirus pandemic. In other words, the third hypothesis, which holds that concerns about COVID-19 mediate the relationship between occupational stress and STSS among nurses working in the frontline, is also confirmed. Based on this finding, it can be demonstrated that the stress experienced by nurses under occupational conditions has affected considerably their concerns during the COVID-19 pandemic. Indeed, the high stress level experienced by a nurse in the workplace (salary, leave, work hours, physician behavior, and insurance) has direct and considerable effects on their concerns about the accuracy of governmental decisions controlling the disease; their family members’, relatives’ and co-workers’ infection by COVID-19; lack of suitable management in hospitals; restricted social activities; and inefficiency or inadequacy in coping with the coronavirus. On the other hand, the pressure resulting from such concerns has made the nurse highly vulnerable and prone to STSS when exposed to the suffering of infected patients. This indirect effect contributes to 68% of stress scores variance for STSS of nurses in this research model and implies the significance of nurses’ occupational stress during the current pandemic.
As mentioned earlier, the effect of concerns about COVID-19 on nurses’ STSS has been supported in Orrù et al. (2020) (21). Indeed, the new finding of this research is that occupational stress affects concerns about the COVID-19 pandemic and how such stresses indirectly affect STSS, which has been observed at least among Iranian nurses during the COVID-19 pandemic.
The significance of occupational stress of nurses has been highlighted earlier in other researches including Poursadeghiyan et al., (2017) and Dagget, Molla, & Belachew (2016) (38, 37). However, this research considers the specific effect that such stresses can have on nurses’ performance and mental health during a crisis like a global pandemic.
Limitation
This research faced several limitations. First, because of difficulties in the data collection process, effects of gender on the relationship between variables could not be studied among nurses. However, it can be expected that the COVID-19 pandemic has been more strict and difficult for female nurses who experience family conflicts and occupational issues even under normal conditions and are responsible for child nurturing in most communities. Thus, it is recommended that future studies consider and note the effects of gender and occupational stress on concerns resulting from the pandemic as well as STSS. Moreover, it should be noted that data for this research was collected shortly after the second peak of the pandemic in Iran. Therefore, researches that will be performed after development of the next peaks of the pandemic, which will naturally make nurses more tired and worn out, can reveal more about the relationships between these variables. On the other hand, the COVID-19 vaccine was not available at the time of the study. Therefore, about the relationships between these variables. On the other hand, the COVID-19 vaccine was not available at the time of the study. Therefore, another point that can be examined is whether vaccination has reduced concerns about COVID-19 and, consequently, STSS or not.
Conclusion
The findings revealed the mediating role of concerns about the COVID-19 pandemic on the relationship between front-line nurses' occupational stress and STSS. It means that, with a high level of occupational stress during a pandemic, the prevalence of STSS among front-line nurses will be higher. Therefore, to reduce the secondary traumatic stress of nurses who have dealt directly with COVID-19 patients, it seems necessary to pay serious attention to the sources of their occupational stress, which probably existed even before this pandemic and have raised nurses’ concerns in pandemic conditions. Therefore, the main contribution of this research may be considered as a clear message to healthcare systems that the psychological conditions of nurses during pandemics, like the current one, can be controlled mainly by improving their occupational conditions and thereby reducing their occupational stress.
Acknowledgment
The authors would like to express their gratitude to all frontline nurses who participated in this study and the managers of Shahid Chamran and Ali Asghar hospitals in Shiraz city, Iran, for their support.
Conflict of Interest
None.
References
- 1.World Health Organization (WHO, 2020) Archived from the original on 31 January 2020. [Accessed 30 January 2020]. Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.Guterres, A. UN leads call to protect most vulnerable from mental health crisis during and after COVID-19. UN News. 2020. Available from: https://news.un.org/feed/view/en/story/2020/05/1063882.
- 3.Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49(3):717–26. doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bambi S, Iozzo P, Lucchini A. New Issues in Nursing Management During the COVID-19 Pandemic in Italy. Am J Crit Care. 2020;29(4):e92–e3. doi: 10.4037/ajcc2020937. [DOI] [PubMed] [Google Scholar]
- 5.Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020;131:132–7. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav Immun Health. 2020;8:100144. doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233–40. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- 8.McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52(4):241–7. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 9.Batra K, Singh TP, Sharma M, Batra R, Schvaneveldt N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int J Environ Res Public Health. 2020;17(23):9096. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Figley CR. Traumatization and comfort: Close relationships may be hazardous to your health; Keynote address for Families and Close Relationships: Individuals in Social Interaction, Conference at Texas Tech University; 1982 Feb; Lubbock, TX: [Google Scholar]
- 11.Figley CR. Compassion fatigue: Toward a new understanding of the cost of caring. In: Stamm BH, editor. Secondary Traumatic Stress Self-Care Issue for Clinicians, Researchers, & Educators. (2nd Ed.) Baltimore, MD, USA: Sidran Press; 1995a. pp. 3–28. [Google Scholar]
- 12.Figley CR. Compassion fatigue: psychotherapists' chronic lack of self-care. J Clin Psychol. 2002;58(11):1433–41. doi: 10.1002/jclp.10090. [DOI] [PubMed] [Google Scholar]
- 13.Ludick M, Figley CR. Toward a mechanism for secondary trauma induction and reduction: Reimagining a theory of secondary traumatic stress. Traumatology. 2017;23(1):112–3. [Google Scholar]
- 14.Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: a concept analysis. Nurs Health Sci. 2010;12(2):235–43. doi: 10.1111/j.1442-2018.2010.00526.x. [DOI] [PubMed] [Google Scholar]
- 15.Geoffrion S, Morselli C, Guay S. Rethinking Compassion Fatigue Through the Lens of Professional Identity: The Case of Child-Protection Workers. Trauma Violence Abuse. 2016;17(3):270–83. doi: 10.1177/1524838015584362. [DOI] [PubMed] [Google Scholar]
- 16.Brady JL, Guy JD, Poelstra PL, Brokaw BF. Vicarious traumatization, spirituality, and the treatment of sexual abuse survivors: A national survey of women psychotherapy STSS. P Psychol: Res Prac. 1999;30:386–93. [Google Scholar]
- 17.Meyers TW, Comille TA. treating compassion fatigue. Routledge; 2013. The trauma of working with traumatized children; pp. 39–55. [Google Scholar]
- 18.Pfefferbaum B, North CS, Bunch K, Wilson TG, Tucker P, Schorr JK. The impact of the 1995 Oklahoma City bombing on the partners of firefighters. J Urban Health. 2002;79(3):364–72. doi: 10.1093/jurban/79.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gale K, Flannelly KJ, Greene PB, Kudler T. Burnout, secondary traumatic stress, and social support. Past Psychol. 2011;60(5):633–49. [Google Scholar]
- 20.Greinacher A, Derezza-Greeven C, Herzog W, Nikendei C. Secondary traumatization in first responders: a systematic review. Eur J Psychotraumatol. 2019;10(1):1562840. doi: 10.1080/20008198.2018.1562840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orrù G, Marzetti F, Conversano C, Vagheggini G, Miccoli M, Ciacchini R, et al. Secondary Traumatic Stress and Burnout in Healthcare Workers during COVID-19 Outbreak. Int J Environ Res Public Health. 2021;18(1):337. doi: 10.3390/ijerph18010337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization, Last update: 14 February 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 23.Albott CS, Wozniak JR, McGlinch BP, Wall MH, Gold BS, Vinogradov S. Battle Buddies: Rapid Deployment of a Psychological Resilience Intervention for Health Care Workers During the COVID-19 Pandemic. Anesth Analg. 2020;131(1):43–54. doi: 10.1213/ANE.0000000000004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shanafelt T, Ripp J, Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. Jama. 2020;323(21):2133–4. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 25.Ayanian JZ. Mental Health Needs of Health Care Workers Providing Frontline COVID-19 Care. JAMA Health Forum. 2020;1(4):e200397. doi: 10.1001/jamahealthforum.2020.0397. [DOI] [PubMed] [Google Scholar]
- 26.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e8. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Temsah MH, Al-Sohime F, Alamro N, Al-Eyadhy A, Al-Hasan K, Jamal A, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. 2020;13(6):877–82. doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsamakis K, Rizos E, Manolis AJ, Chaidou S, Kympouropoulos S, Spartalis E, et al. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med. 2020;19(6):3451–3. doi: 10.3892/etm.2020.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohindra R, R R, Suri V, Bhalla A, Singh SM. Issues relevant to mental health promotion in frontline health care providers managing quarantined/isolated COVID19 patients. Asian J Psychiatr. 2020;51:102084. doi: 10.1016/j.ajp.2020.102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Susta. 2020 May 8;12(9):3834. [Google Scholar]
- 31.Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55(9):1055–7. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 32.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J Psychiatr. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong TY, Koh G, Cheong SK, Lee HY, Fong YT, Sundram M, et al. Concerns, perceived impact and preparedness in an avian influenza pandemic--a comparative study between healthcare workers in primary and tertiary care. Ann Acad Med Singap. 2008;37(2):96–102. [PubMed] [Google Scholar]
- 34.Koh D, Lim MK, Chia SE, Ko SM, Qian F, Ng V, et al. Risk perception and impact of Severe Acute Respiratory Syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med Care. 2005;43(7):676–82. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- 35.Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017;17(1):4. doi: 10.1186/s12879-016-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiatr. 2020;33(5):e100284. doi: 10.1136/gpsych-2020-100284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dagget T, Molla A, Belachew T. Job related stress among nurses working in Jimma Zone public hospitals, South West Ethiopia: a cross sectional study. BMC Nurs. 2016;15:39. doi: 10.1186/s12912-016-0158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poursadeghiyan M, Moghimian M, Amjad R, Baneshi M, Yari A, Noroozi M, Hami M, Khammar A, Farrokhi M. Effects on job stress on Iranian clinical nurses. Anna Trop Med. 2017 Jul 1;10(4) [Google Scholar]
- 39.Lee E, Jang I. Nurses' Fatigue, Job Stress, Organizational Culture, and Turnover Intention: A Culture-Work-Health Model. West J Nurs Res. 2020;42(2):108–16. doi: 10.1177/0193945919839189. [DOI] [PubMed] [Google Scholar]
- 40.Van Bogaert P, Peremans L, Van Heusden D, Verspuy M, Kureckova V, Van de Cruys Z, et al. Predictors of burnout, work engagement and nurse reported job outcomes and quality of care: a mixed method study. BMC Nurs. 2017;16:5. doi: 10.1186/s12912-016-0200-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bagheri Hosseinabadi M, Etemadinezhad S, Khanjani N, Ahmadi O, Gholinia H, Galeshi M, et al. Evaluating the relationship between job stress and job satisfaction among female hospital nurses in Babol: An application of structural equation modeling. Health Promot Perspect. 2018;8(2):102–8. doi: 10.15171/hpp.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chin WS, Chen YC, Ho JJ, Cheng NY, Wu HC, Shiao JSC. Psychological Work Environment and Suicidal Ideation Among Nurses in Taiwan. J Nurs Scholarsh. 2019;51(1):106–13. doi: 10.1111/jnu.12441. [DOI] [PubMed] [Google Scholar]
- 43.Mamashli L, Mohammadpour Y, Moghadam A, Esmaeilzadeh S. Examination of the Occupational Stressors among the Nurses Working in Educational Centers in Urmia. Spec J Med Res Health Sci. 2019;4(1):6–13. [Google Scholar]
- 44.Chatzigianni D, Tsounis A, Markopoulos N, Sarafis P. Occupational Stress Experienced by Nurses Working in a Greek Regional Hospital: A Cross-sectional Study. Iran J Nurs Midwifery Res. 2018;23(6):450–7. doi: 10.4103/ijnmr.IJNMR_120_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arnetz JE, Goetz CM, Sudan S, Arble E, Janisse J, Arnetz BB. Personal Protective Equipment and Mental Health Symptoms Among Nurses During the COVID-19 Pandemic. J Occup Environ Med. 2020;62(11):892–7. doi: 10.1097/JOM.0000000000001999. [DOI] [PubMed] [Google Scholar]
- 46.Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring Nursing Intention, Stress, and Professionalism in Response to Infectious Disease Emergencies: The Experience of Local Public Hospital Nurses During the 2015 MERS Outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci) 2017;11(3):230–6. doi: 10.1016/j.anr.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kline RB. Principles and practice of structural equation modeling. Guilford publications; 2015 Nov 3; [Google Scholar]
- 48.Bride BE, Robinson MM, Yegidis B, Figley CR. Development and validation of the secondary traumatic stress scale. Res soc prac. 2004 Jan;14(1):27–35. [Google Scholar]
- 49.Ahmadi K, Rezapour Y, Davoudi F, Saberi M. Investigate of validity and reliability of secondary trauma stress scale for evaluation of PTSD symptoms in samples of warfare victims’ wives. Iri J War Pub. 2013 Jun 10;5(3):47–57. [Google Scholar]
- 50.Chen YC, Guo YL, Lin LC, Lee YJ, Hu PY, Ho JJ, et al. Development of the Nurses' Occupational Stressor Scale. Int J Environ Res Public Health. 2020;17(2):649. doi: 10.3390/ijerph17020649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Safari Shirazi M, Sadeghzadeh M, Abbasi M. Psychometric Properties of Persian Version of Condensed Nurses' Occupational Stress Scale in Covid-19 Pandemic Period. Avicenna J Nurs Midwifery Care. 2021;29(3):245–55. [Google Scholar]
- 52.Kline RB. Principles and practice of structural equation modeling . (4th Ed.) New York, NY: The Guilford Press; 2016. [Google Scholar]
- 53.Bentler PM. EQS structural equations program manual. Encino, CA: Multivariate software; 1995. [Google Scholar]
- 54.Hooper CJ, Mullen M. Structural equation modelling: guidelines for determining model fit. Elec J Bus Res Meth. 2008;6(1):53–60. [Google Scholar]
- 55.Kirkpatrick DD, Fassihi F, Mashal M. The New York Times. Times. Retrieved Mar 24, 2020. Available from: https://www.nytimes.com/by/david-d-kirkpatrick.
- 56.World Health Organization (WHO, 1 February to 30 June 2020) COVID-19 Preparedness and Response Progress Report. [accessed 6 Nov 2020]. Available from: https://www.who.int/publications/m/item/who-covid-19-preparedness-and-response-progress-report---1-february-to-30-june-2020.