Abstract
Purpose
In 2020, racially/ethnically minoritized (REMD) youth faced the “dual pandemics” of COVID-19 and racism, both significant stressors with potential for adverse mental health effects. The current study tested whether short- and long-term trajectories of depressive symptoms from before to during the COVID-19 pandemic differed between REMD adolescents who did and did not endorse exposure to COVID-19-era-related racism (i.e., racism stemming from conditions created or exacerbated by the COVID-19 pandemic).
Methods
A community sample of 100 REMD adolescents enrolled in an ongoing longitudinal study of mental health was assessed before and during the COVID-19 pandemic. Participants were 51% girls, mean age = 16, standard deviation = 2.7, and identified as Latinx/Hispanic (48%), Multiethnic (34%), Asian American (12%), and Black (6%).
Results
REMD adolescents' depressive symptoms were elevated during the COVID-19 pandemic compared to pre-pandemic levels, and increases were more pronounced over time for those who endorsed exposure to COVID-19-era-related racism. In general, Asian American participants endorsed racism experiences at the highest rates compared to others, including being called names (42%), people acting suspicious around them (33%), and being verbally threatened (17%). Additionally, more than half of Black and Asian American participants reported worry about experiencing racism related to the COVID-19 pandemic, even if they had not experienced it to date.
Discussion
REMD adolescents are at increased risk for depressive symptoms related to converging stressors stemming from the COVID-19 pandemic and pandemic-related racism, which has the potential to widen racial/ethnic mental health disparities faced by the REMD youth.
Keywords: COVID-19, Adolescent, Depression, Mental health, Racism, Youth, Trajectories, Discrimination, Disparities
Implications and Contributions.
A sample of racially/ethnically minoritized adolescents reported increases in depressive symptoms from before to during COVID-19, and these increases were more pronounced over time for those exposed to COVID-19-era-related racism. Racially/ethnically minoritized adolescents may face unique risk for depression stemming from stressors related to COVID-19 and pandemic-related racism.
In the United States, the year 2020 was characterized by what has been referred to as the “dual pandemics” or “confluence of crises”—comprising the COVID-19 pandemic as well as exacerbated racial inequities and increased frequency and awareness of racism [[1], [2], [3], [4], [5], [6], [7]]. The COVID-19 pandemic disrupted everyday life in unprecedented ways. In addition to the virus infecting hundreds of millions of people across the globe leading to serious illness and death, there were also widespread public lockdowns, school closures, and increases in social isolation, unemployment, and financial insecurity [[8], [9], [10]].
The second crisis, pandemic-spurred racism, manifested among racially/ethnically minoritized (REMD) groups in the United States through both interpersonal and structural pathways. Black, Latinx/Hispanic, and Native American people have higher rates of severe COVID-19 disease and death compared to White people, traceable to structural racism including barriers to care and less-safe living and working conditions (e.g., crowded housing and essential worker positions) [3,11]. These disproportionate death rates have also resulted in a much greater number of REMD youth losing one or more caregivers from COVID, compared to White youth [12]. Additionally, on a recent poll, 50% of Latinx adults stated they felt like outsiders in the US since the pandemic began, stemming from the growth of anti-Latinx rhetoric and immigration policies exacerbated by the pandemic, including the invocation of Title 42 to deny possibly infected migrants from entering the US and seeking asylum [13,14]. Asian Americans also faced a dramatic spike in interpersonal racism as COVID-19 began to spread, in part due to the pandemic outbreak originating in China. In fact, the Center for the Study of Hate and Extremism at California State University reported a 149% increase in hate crimes against Asian Americans between 2019 and 2020 [15]. These incidents spanned verbal harassment and shunning, civil rights violations, online harassment, and serious physical assaults, some that resulted in death [16].
Compounding stressors
Preliminary evidence suggests that the confluence of COVID-19 and racism-related stressors throughout 2020 had extreme negative impacts on the health and well-being of the nation, particularly for REMD groups. The American Psychological Association's 2020 Stress in America survey reported that the compounding of ongoing external stressors with the COVID-19 pandemic resulted in “a national mental health crisis that could yield serious health and social consequences for years to come.” On the survey, 44% of REMD respondents reported discrimination to be a significant stressor in their lives, compared to 38% in 2019. Preliminary research has also tied experiences of COVID-19-era-related discrimination directly to worse mental health. For example, a cross-sectional study by Chae et al found higher levels of vicarious racism and racism-related vigilance (i.e., hearing about racism directed toward one's racial group and heightened, preemptive vigilance to avoid and/or cope with racism) among Asian American and Black adults between May and July 2020 to be associated with more symptoms of depression and anxiety [4].
Racially/ethnically minoritized adolescent vulnerability
REMD adolescents may be particularly vulnerable to the negative mental health effects of COVID-19 and racism-related stress. Developmentally, adolescence is a sensitive period when many common mental health disorders first emerge, often spurred by the presence of environmental stressors such as those related to the COVID-19 pandemic, including school closures, compromised health of oneself and loved ones, and isolation. Indeed, we previously reported evidence that adolescents experienced a heightening of depressive symptoms following the onset of the COVID-19 pandemic, and that this increase was earlier and more pronounced among girls [8]. Our findings contributed to a growing body of literature showing links between COVID-19 and poor mental health among adolescents [10,[17], [18], [19], [20], [21]].
Adolescence is characterized by an increased awareness of, and sensitivity to, social stressors, including how they and the groups they belong to are perceived by others, and also by fewer emotional regulation skills than adults [[22], [23], [24], [25]]. Identity formation is a hallmark of adolescence, and particularly for REMD youth, this includes reflection on racial/ethnic identity and its influence on current and future life experiences [[25], [26], [27]]. Given the presence of these developmental processes, it is likely that REMD adolescents are uniquely impacted by experiences of racism compared to REMD populations in other stages of development—an idea that is supported by existing research. Specifically, experiences of racism have been repeatedly linked to depression and related outcomes in adolescents, with some research suggesting adolescents are more vulnerable than adults to the negative effects of racism [28].
The distinct developmental period of adolescence coupled with the occurrence of both COVID-19 and COVID-19-era-related racism in recent years necessitates further research to better understand the impact of these stressors on REMD adolescent mental health. Recent qualitative findings suggest that COVID-19-related mental health challenges among REMD college students are compounded by experiencing and witnessing racial discrimination [5]. Several other recent quantitative studies of REMD adolescents and young adults document associations between discrimination experienced during the COVID-19 pandemic and poorer mental health, including stress, anxiety, depression, and posttraumatic stress [[29], [30], [31], [32], [33]]. However, these studies were largely cross-sectional and did not examine change in mental health symptoms across time from before to during the pandemic. Therefore, the purpose of the current study is to extend our previous research findings of increased adolescent depression from before to during the COVID-19 pandemic by examining if perceived experience of COVID-19-era-related racism (i.e., racism stemming from conditions created or exacerbated by the COVID-19 pandemic) among REMD adolescents influenced trajectories of depressive symptoms. Prior evidence supports increased vulnerability to depression among female adolescents in response to environmental stressors [8,34], and among REMD adolescents in response to experiences of racism [28]. Therefore, we predicted an increase in depressive symptoms from before to during COVID-19 in our sample, with more pronounced effects for girls and those with perceived experience of COVID-19-era-related racism.
Methods
Participants
Participants include all REMD youth in a sample of participants from Southern California who participated in a longitudinal study of mental health from before to during the pandemic (N = 175, see Liu et al. 2021 for more details). The original study from which this cohort was recruited began when participants were in-utero and entailed periodic visits. The most recent visit participants completed prior to the pandemic was on average 2 years prior to the state's pandemic-related shutdown, but ranged for individual participants between 5 years and 1 week prior. Our final sample was composed of 100 adolescents. Participants' sex assigned at birth and self-reported gender aligned, with 51% of participants identifying as female and 49% as male. Average participant age at the date of the first California COVID-19 related state shutdown was 16 years old (standard deviation [SD] = 2.7). Income-to-needs ratio (family income expressed as a proportion of the federal poverty line for a family of a particular size) among participants ranged from 18% to 2523%, with a median of 438%. Reported household income ranged from $6,000 to $1,000,000, with a median of $100,000. The majority of participants identified as Latinx/Hispanic (48%) followed by Multiethnic (34%), Asian American (12%), and Black (6%).
Measures
All study procedures were approved by the responsible Human Subjects Review Board. Depressive symptoms were assessed at three time points: (1) before the COVID-19 pandemic (on average, 2 years prior to state shutdown on March 19th, 2020; range 5 years–1 month); (2) the “acute” period eight weeks after the initial state shutdown (range 6–13 weeks); and (3) the “persistent” period 8.5 months after the shutdown (range eight–9.25 months). On average, participants were 14, 16, and 17 years old at time points 1, 2, and 3, respectively. Symptoms were measured with the Children's Depression Inventory (CDI-2:SR [S]), a 12 item self-report questionnaire (Kovacs, 2011). Scores range from 0 to 24, and higher scores indicate more severe symptoms. This measure demonstrated good internal consistency in our sample with alpha coefficients averaging at 7 across time points.
Perceived exposure to COVID-19-era-related racism was assessed at the third time point (approximately early December, 2020) with five questions adapted from Pew Research Center's American Trends Panel June 2020 [35]. Specifically, participants were asked if they experienced “any of the following forms of racism because of the COVID-19 pandemic”: (a) people acted uncomfortable around them, (b) people acted suspicious around them, (c) people called them names, including racial slurs, or made jokes about them, (d) they were verbally threatened, (e) they were physically attacked. Participants could respond with three choices: (1) not at all, (2) a little, or (3) a lot. Based on the distribution of responses, we dichotomized this measure into any versus no reported experiences of racism to simplify model fitting and interpretation. Participants were also asked a yes or no question regarding whether they worried about experiencing racism because of the COVID-19 pandemic, even if they had not yet experienced it.
Data analyses
Analyses characterized trajectories of depressive symptoms from before to during the pandemic, assessing both acute and persisting responses. First, we evaluated whether these depressive symptom trajectories differed by gender (model 1). Next, we assessed how reported experiences of COVID-19-era-related racism affected depression trajectories for boys and girls (model 2). We fit a linear mixed effects model with CDI score at each time point regressed on a 3-way interaction among time, gender and racism exposure, adjusting for participant age at the time of the shutdown (centered at the mean) to account for age-related variability in depressive symptoms. Time was operationalized as months elapsed since the time of the COVID shutdown in California (March 2020) and modeled as a linear spline with a knot at 1.75 months post shutdown to allow for different acute and persistent effects of the shutdown on depressive symptoms. Trajectories were plotted by calculating model-estimated mean CDI scores at the median number of months from the shutdown for each assessment (pre-COVID: 27.25 months before; acute time point: 1.75 months after; persistent time point: 8.25 months after). Model fit was assessed using Nakagawa's marginal and conditional R 2 [36].
Results
Participant experiences of and worry about racism
In total, 30% (n = 30) of adolescents endorsed experiencing any COVID-19-era-related racism. Figure 1 illustrates participants' self-reported experiences of and worry about racism, by race/ethnicity. Asian Americans endorsed being called names (42%, n = 5), people acting suspicious around them (33%, n = 4), and being verbally threatened (17%, n = 2) at the highest rates compared to other racial/ethnic groups. Additionally, more than half of Black and Asian American participants reported worry about experiencing racism related to the COVID-19 pandemic, even if they had not actually experienced it.
Figure 1.
Percentage of participants who endorsed experiences of and worry about COVID-19-era-related racism. Note. Endorsement percentages are shown separately for youth of different race/ethnicity. There were 48 Latinx/Hispanic, 34 Multiethnic, 12 Asian, and six Black respondents. Due to small sample sizes, statistical differences between racial/ethnic groups were not tested.
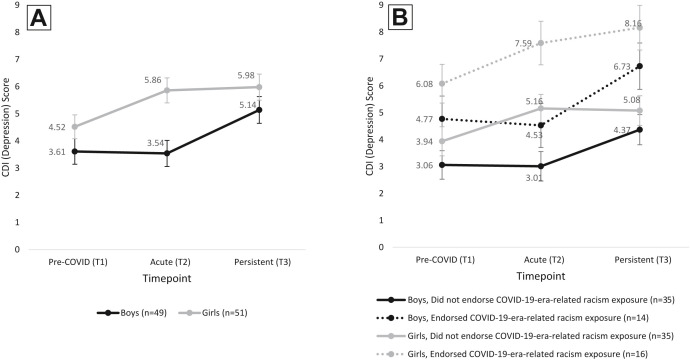
Trajectories of depressive symptoms by gender
Depression trajectory modeling results by gender are reported in Table 1 and illustrated in Figure 2 A,B. In line with our previous findings in the full cohort [8], Model 1 results indicate that depressive symptoms among the subset of REMD adolescents increased significantly in the acute period for girls (M[SD] Δ CDI = 1.35[.35], p < .01) but not boys, leading to a significant disparity in acute depressive symptom severity by gender (boys M[SD] = 3.54[.48]; girls M[SD] = 5.86[.46], p < .01) that was not observed in the pre-COVID period (boys M[SD]) = 3.61[.47], girls M[SD] = 4.52[.44], p = .16). However, depressive symptoms among boys significantly increased in the persistent period (M [SD] Δ CDI = 1.60[.49], p < .01), closing the observed gap in depressive symptoms between sexes.
Table 1.
REMD adolescent boys' (n = 49) and girls' (n = 51) trajectories of depression from before to after COVID-19 pandemic onset
| Model 1 | Model 2 (+ any reported exposure to COVID-19-era-related racism) | |||||
|---|---|---|---|---|---|---|
| Time point | Boys (n = 49) | Girls (n = 51) | Boys versus girls pa | Boys (n = 49) | Girls (n = 51) | Boys versus girls pa |
| Full Sample | No reported exposure to racism | |||||
| Mean CDI score (95% CI) | ||||||
| Pre-COVID (T1) | 3.61 (2.69, 4.53) | 4.52 (3.66, 5.38) | −0.91 (−2.18, 0.37) p = .16 | 3.06 (2.02, 4.10) | 3.94 (2.88, 5.00) | −0.88 (−2.37, 0.60) p = .66 |
| Acute (T2) | 3.54 (2.60, 4.48) | 5.86 (4.96, 6.76) | −2.32 (−3.62, −1.01) p = .00∗∗ | 3.01 (1.93, 4.09) | 5.16 (4.14, 6.18) | −2.14 (−3.63, −0.65) p = .03∗ |
| Persistent (T3) | 5.14 (4.18, 6.10) | 5.98 (5.04, 6.92) | −0.84 (−2.19, 0.50) p = .22 | 4.37 (3.27, 5.47) | 5.08 (4.00, 6.16) | −0.71 (−2.26, 0.84) p = .80 |
| Change over time (95% CI)b | ||||||
| Δ Acute–Pre-COVID | −0.07 (−0.87, .73) | 1.35 (.66, 2.04)∗∗ | −1.41 (−1.47, −1.36) p = .00∗∗ | −.04 (−0.98, 0.90) | 1.22 (.20, 2.24) | −1.26 (−1.37, −1.16) p = .00∗∗ |
| Δ Persistent–Acute | 1.60 (.64, 2.56)∗∗ | 0.12 (−.82, 1.06) | −1.47 (−1.53, −1.41) p = .01∗∗ | 1.36 (0.20, 2.52) | −.08 (−1.22, 1.06) | 1.44 (1.31, 1.56) p = .00∗∗ |
| Any reported exposure to racism | ||||||
| Mean CDI score (95% CI) | ||||||
| Pre-COVID (T1) | 4.77 (3.10, 6.44) | 6.08 (4.67, 7.49) | −1.31 (−3.47, 0.85) p = .64 | |||
| Acute (T2) | 4.53 (2.92, 6.14) | 7.59 (6.00, 9.18) | −3.05 (−5.30, −0.80) p = .04∗ | |||
| Persistent (T3) | 6.73 (5.04, 8.42) | 8.16 (6.53, 9.79) | −1.43 (−3.76, 0.90) p = .63 | |||
| Change over time (95% CI)b | ||||||
| Δ Acute–Pre-COVID | −.24 (−1.77, 1.29) | 1.51 (.53, 2.49)∗ | −1.75 (−1.88, −1.61) p = .00∗∗ | |||
| Δ Persistent–Acute | 2.20 (.46, 3.94) | .58 (−1.18, 2.34) | 1.62 (1.44, 1.81) p = .00∗∗ | |||
| Differences by high versus lowc | Any versus no exposure to racism | |||||
| Mean CDI score (95% CI) | ||||||
| Pre-COVID (T1) | 1.72 (−.26, 3.70) | 2.14 (.38, 3.90) | ||||
| Acute (T2) | 1.52 (−.42, 3.46) | 2.43 (.55, 4.31) | ||||
| Persistent (T3) | 2.36 (.34, 4.38) | 3.08 (1.12, 5.04) | ||||
| Change over time (95% CI)b | ||||||
| Δ Acute–pre-COVID | −.19 (−.33, −.05) | .29 (.19, 0.39)∗ | ||||
| Δ Persistent–acute | .84 (0.68, 1.00)∗∗ | .66 (.50, 0.82)∗∗ | ||||
∗p < .05, ∗∗p < .01. Mean CDI score is estimated by the fitted model at the median time point of assessment for each period (median no. weeks from state shutdown: T1: −109, T2: 7, T3: 33). All models are adjusted for age. Model 2 additionally includes endorsed exposure to COVID-19-era-related racism; this was modeled using a 3-way interactions between racism exposure∗gender∗time. Contrasts of mean CDI scores over time are adjusted for multiple comparisons using Tukey's honestly significant difference (p-values denoted by asterisks).
CDI = Children's Depression Inventory; CI = confidence interval; REMD = racially/ethnically minoritized.
Differences by gender were compared using two-tailed Welch's t-test.
Mean change between time points were estimated using model-predicted CDI score at median weeks from shutdown, stratified by gender.
p-values are for test of differences between any versus no endorsed exposure to COVID-19 related racism in CDI score and change in CDI score over time.
Figure 2.
Trajectories of depressive symptoms by gender (A) and reported exposure to COVID-19-era-related racism (B). Markers and error bars indicate model-estimated marginal means and standard errors for CDI score at each time point by gender and racism exposure (B only).
Trajectories of depressive symptoms by gender and perceived racism exposure
Model 2 shows that participants who endorsed exposure to COVID-19-era-related racism had higher levels of depressive symptoms compared to those who did not endorse exposure. Notably all adolescents who reported exposure showed steeper increases in depressive symptoms. Girls reporting racism exposure had significantly greater increases in depressive symptoms compared to girls who did not report racism exposure in both the acute and persistent period (acute period M[SD] Δ CDI = .29 [.05], p < .01; persistent period M[SD] Δ CDI = .66 [.08], p < .01). Boys who endorsed exposure to COVID-19-era-related racism had a significantly greater increase in depression levels in the persistent period compared to their counterparts who did not endorse racism exposure (M [SD] Δ CDI = .84 [.08], p < .01). Corresponding trajectories are displayed in Figure 2. The mixed effects models exhibited adequate goodness-of-fit with much of the outcome variance being explained by between-subject differences: Marginal and conditional R 2 values for model one were 14.6% and 51.4%, respectively, and for model two were 21.7% and 51.5%, respectively. Plots of average depression levels across time by race/ethnicity and endorsement of COVID-19-era-related discrimination can be found in the Supplemental Material. Across race/ethnicity, adolescents who reported perceived exposure to COVID-19-era-related discrimination had higher levels of depression symptoms at T2 and T3 compared to those adolescents who did not report exposure.
Discussion
This study adds important evidence of the unique detrimental impact of the COVID-19 pandemic and exposure to COVID-19-era-related racism on depressive symptoms among REMD adolescents. To our knowledge, there are no studies examining short- and long-term trajectories of mental health during the pandemic and how these trajectories differ by gender and COVID-19-era-related racism experiences. Consistent with our prior study of both REMD and White youth [8], in the current study of REMD adolescents we observed that on average, depressive symptoms increased from before to during the COVID-19 pandemic, and these effects were most pronounced for girls. Additionally, we report that increases in depressive symptoms during the pandemic were more pronounced over time among adolescents who reported exposure to COVID-19-era-related racism. Specifically, both boys and girls endorsing COVID-19-era-related racism had significantly greater increases in depressive symptoms than their counterparts who did not report racism exposure.
Our descriptive findings provide important context regarding the ways in which adolescents in our sample perceived and experienced COVID-19-era-related racism. Specifically, we show that many REMD adolescents endorsed worry about COVID-19-era-related racism. Many participants also reported experiencing several racism types, especially name-calling or people acting suspicious and uncomfortable around them. Although our sample size did not allow for testing of statistically significant differences, Asian American youth in our sample endorsed three of these experiences at the highest rates. This pattern aligns with the historical context of our study, during which Asian Americans were being scapegoated for the spread of the virus.
There are several important limitations to this study that can also inform future research. This was a community sample drawn from Southern California, and findings may not be representative of adolescents in different populations. Additionally, although all REMD groups are impacted by racism, there are between and within-group differences in the nature and impact of these experiences. For example, Asian Americans were more likely than members of other racial/ethnic groups to be seen as spreaders of COVID-19 because the virus originated in China. However, because of our limited sample size, we are unable to examine differences among racial/ethnic groups. We also see important evidence in our study that Black adolescents are being negatively impacted by COVID-19-era-related racism. Concurrent with the COVID-19 pandemic, there was a massive increase in attention to and protests related to the #BlackLivesMatter movement in response to the killing of George Floyd and other recent victims of racial and police violence. These events may have influenced participant responses to our questions about COVID-19-era-related racism; however, we are unable to separate these effects in our current study. Research on larger racially/ethnically diverse samples with more detailed questions about types of racism exposure could provide further insight.
Despite limitations, this study provides compelling evidence that REMD adolescents are at increased risk for depressive symptoms related to converging stressors stemming from the COVID-19 pandemic. The mental health crisis faced by adolescents has recently gained more awareness and attention [37,38] but there is less discussion about the potential for a widening of racial/ethnic mental health disparities faced by REMD youth related to COVID-19-era-related racism. Further, these disparities may be exacerbated by existing barriers to mental health care that disproportionately impact REMD populations, such as underdiagnosis or misdiagnosis of mental illness, a lack of access to mental health services and/or culturally-competent providers, mental health stigma, and medical mistrust within communities of color stemming from past experiences of mistreatment [[39], [40], [41], [42]]. Thus, it is critical that practitioners and policy-makers recognize this issue and take action to address it, including through incorporating culturally-responsive and trauma-informed screening and intervention methods and enhancing protective factors shown to mitigate the impact of racism such as positive racial/ethnic identity and racial socialization [3].
Acknowledgments
This work was supported by the National Institute of Health (grant no. MH096889).
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Disclaimer: Study sponsor had no role in study design, collection, analysis, or interpretation of data, writing of report, or decision to submit manuscript for publication. Sabrina Liu wrote the first draft of this manuscript.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2022.12.020.
Supplementary Data
References
- 1.Burrell P.M. A confluence of crises. J Transcult Nurs. 2020;31:625. doi: 10.1177/1043659620945007. [DOI] [PubMed] [Google Scholar]
- 2.Wegemer C.M., von Keyserlingk L. Dual pandemics of COVID-19 and systemic racism: The roles of perceptions of inequities, civic values, and conservatism in mask-wearing behavior. Anal Soc Issues Public Policy. 2022;22:66–88. [Google Scholar]
- 3.Liu S.R., Modir S. The outbreak that was always here: Racial trauma in the context of COVID-19 and implications for mental health providers. Psychol Trauma Theory, Res Pract Policy. 2020;12:439–442. doi: 10.1037/tra0000784. [DOI] [PubMed] [Google Scholar]
- 4.Chae D.H., Yip T., Martz C.D., et al. Vicarious racism and vigilance during the COVID-19 pandemic: Mental health implications among Asian and Black Americans. Public Health Rep. 2021;136:508–517. doi: 10.1177/00333549211018675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molock S.D., Parchem B. The impact of COVID-19 on college students from communities of color. J Am Coll Health. 2020;0:1–7. doi: 10.1080/07448481.2020.1865380. [DOI] [PubMed] [Google Scholar]
- 6.Zhou X., Nguyen-Feng V.N., Wamser-Nanney R., et al. Racism, posttraumatic stress symptoms, and racial disparity in the U.S. COVID-19 syndemic. Behav Med. 2022;48:85–94. doi: 10.1080/08964289.2021.2006131. [DOI] [PubMed] [Google Scholar]
- 7.Seedat S. Commentary on the special issue on disproportionate adversity: Trauma, stress, and adversities and health disparities among disenfranchised groups globally during the COVID pandemic. J Trauma Stress. 2021;34:1061–1067. doi: 10.1002/jts.22746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu S.R., Davis E.P., Palma A.M., et al. The acute and persisting impact of COVID-19 on trajectories of adolescent depression: Sex differences and social connectedness. J Affect Disord. 2021;299:246–255. doi: 10.1016/j.jad.2021.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52:177–187. [Google Scholar]
- 10.Kujawa A., Green H., Compas B.E., et al. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37:1280–1288. doi: 10.1002/da.23109. [DOI] [PubMed] [Google Scholar]
- 11.Tai D.B.G., Shah A., Doubeni C.A., et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020;72:1–4. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hillis S.D., Blenkinsop A. COVID-19 – associated orphanhood and caregiver death in the United States 2021. Pediatrics. 2021;148 doi: 10.1542/peds.2021-053760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gramlich J. Pew Research Center; Washington, D.C.: 2022. Title 42 and immigration enforcement at U.S.-Mexico border: Key facts. [Google Scholar]
- 14.Foxen P. UnidosUS; 2021. Latinos, COVID-19, and social belonging: Voices from the community. [Google Scholar]
- 15.Sherman A. Poynter; St. Petersburg, FL: 2021. Hate crimes against Asian Americans: What the numbers show, and don’t. [Google Scholar]
- 16.Yellow Horse A.J., Jeung R., Matriano R. Stop AAPI hate; 2021. Stop AAPI hate national report, March 19, 2020 - December 31, 2021. [Google Scholar]
- 17.Copeland W.E., McGinnis E., Bai Y., et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2021;60:134–141.e2. doi: 10.1016/j.jaac.2020.08.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murata S., Rezeppa T., Thoma B., et al. The psychiatric sequelae of the COVID - 19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2020;38:1–14. doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panchal U., Salazar de Pablo G., Franco M., et al. The impact of COVID-19 lockdown on child and adolescent mental health: Systematic review. Eur Child Adolesc Psychiatry. 2021:1–27. doi: 10.1007/s00787-021-01856-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Octavius G.S., Silviani F.R., Lesmandjaja A., et al. Impact of COVID-19 on adolescents’ mental health: A systematic review. Middle East Curr Psychiatry. 2020;27:4–11. [Google Scholar]
- 21.Ren Z., Xin Y., Wang Z., et al. What factors are most closely associated with mood disorders in adolescents during the COVID-19 pandemic? A cross-sectional study based on 1,771 adolescents in Shandong Province, China. Front Psychiatry. 2021;12:1–11. doi: 10.3389/fpsyt.2021.728278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Somerville L.H. The teenage brain: Sensitivity to social evaluation. Curr Dir Psychol Sci. 2013;22:121–127. doi: 10.1177/0963721413476512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hankin B.L. Depression from childhood through adolescence: Risk mechanisms across multiple systems and levels of analysis. Curr Opin Psychol. 2015;4:13–20. doi: 10.1016/j.copsyc.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Somerville L.H., Jones R.M., Casey B.J. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cogn. 2010;72:124–133. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Umaña-Taylor A.J., Toomey R.B., Williams D.R., et al. Latino adolescents’ perceived discrimination in online and offline settings: An examination of cultural risk and protective factors. Dev Psychol. 2015;51:87–100. doi: 10.1037/a0038432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Umaña-Taylor A.J., Quintana S.M., Lee R.M., et al. Ethnic and racial identity during adolescence and into young adulthood: An integrated conceptualization. Child Dev. 2014;85:21–39. doi: 10.1111/cdev.12196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gummadam P., Pittman L.D., Ioffe M. School belonging, ethnic identity, and psychological adjustment among ethnic minority college students. J Exp Educ. 2016;84:289–306. [Google Scholar]
- 28.Seaton E.K. A Luta Continua1: Next steps for racism research among Black American youth. Child Dev Perspect. 2020;14:244–250. [Google Scholar]
- 29.Fisher C.B., Tao X., Yip T. The effects of COVID-19 victimization distress and racial bias on mental health among AIAN, Asian, Black, and Latinx young adults. Cult Divers Ethn Minor Psychol. 2022 doi: 10.1037/cdp0000539. [DOI] [PubMed] [Google Scholar]
- 30.Lu Y., Wang C. Asian Americans’ racial discrimination experiences during COVID-19: Social support and locus of control as moderators. Asian Am J Psychol. 2021;13 [Google Scholar]
- 31.Kiss O., Alzueta E., Yuksel D., et al. The pandemic’s toll on young adolescents: Prevention and intervention targets to preserve their mental health. J Adolesc Heal. 2022;70:387–395. doi: 10.1016/j.jadohealth.2021.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hahm H.C., Ha Y., Scott J.C., et al. Perceived COVID-19-related anti-Asian discrimination predicts post traumatic stress disorder symptoms among Asian and Asian American young adults. Psychiatry Res. 2021;303:114084. doi: 10.1016/j.psychres.2021.114084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huynh V.W., Raval V.V., Freeman M. Ethnic-racial discrimination towards Asian Americans amidst COVID-19, the so-called “China” virus and associations with mental health. Asian Am J Psychol. 2022;13:259–269. [Google Scholar]
- 34.Hankin B.L., Abramson L.Y., Moffitt T.E., et al. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 35.Ruiz N.G., Horowitz J.M., Tamir C. Pew Research Center; Washington, D.C.: 2020. Many Black, Asian Americans say they have experienced discrimination amid coronavirus. [Google Scholar]
- 36.Nakagawa S, Schielzeth H. A general and simple method for obtaining R2 from generalized linear mixed-effects models 2012. Method Ecol Evol. 4:133–142.
- 37.Murthy V.H. Office of the Surgeon General (OSG); Washington, D.C.: 2021. Protecting youth mental health: The U.S. Surgeon General’s Advisory. [Google Scholar]
- 38.American Academy of Pediatrics American Academy of Child and Adolescent Psychiatry, Children’s Hospital Association . AAP-AACAP-CHA declaration of a national emergency in child and adolescent mental health. American Academy of Pediatrics; Itasca, IL: 2021. [Google Scholar]
- 39.DuPont-Reyes M.J., Villatoro A.P., Phelan J.C., et al. Adolescent views of mental illness stigma: An intersectional lens. Am J Orthopsychiatry. 2019;90:201–211. doi: 10.1037/ort0000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liang J., Matheson B.E., Douglas J.M. Mental health diagnostic considerations in racial/ethnic minority youth. J Child Fam Stud. 2016;25:1926–1940. doi: 10.1007/s10826-015-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siegel C.E., Laska E.M., Wanderling J.A., et al. Prevalence and diagnosis rates of childhood ADHD among racial-ethnic groups in a public mental health system. Psychiatr Serv. 2016;67:199–205. doi: 10.1176/appi.ps.201400364. [DOI] [PubMed] [Google Scholar]
- 42.Fripp J.A., Carlson R.G. Exploring the influence of attitude and stigma on participation of African American and Latino populations in mental health services. J Multicult Couns Devel. 2017;45:80–94. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.