Abstract
AIM
To investigate the practice patterns of optometrists in Saudi Arabia regarding myopia management.
METHODS
An internet-based survey was distributed to all practicing optometrists in Saudi Arabia (n=1886). The survey contained questions related to 1) demographics, 2) knowledge about myopia and its associated complications, 3) current clinical care, 4) type and frequency of myopia treatment prescribed, and 5) potential barriers limiting treatment adoption.
RESULTS
The completed surveys were collected from 171 optometrists (9.06% response rate, 60% male). Knowledge regarding myopia-associated complications was prevalent but somewhat inaccurate among the respondents. Cycloplegic refraction at initial visit was used by 59% of the respondents. The cover test was the most reported binocular vision test (83%), and 38% of optometrists did not perform any ocular biometrics. Two-thirds prescribed single-vision spectacles for children with myopia. Increased time spent outdoors was selected by 80% of the practitioners who prescribed myopia control treatment as the primary approach. Insufficient support and lack of clinical experience in providing myopia treatment were reported as the most important factors limiting the adoption of myopia management strategies.
CONCLUSION
The current optometric practices in Saudi Arabia require further investigation. Optometrists appear to be somewhat aware of myopia and the associated risks. However, most evidence-based myopia treatments are not being locally adopted, primarily because of lack of support, lack of experience, and limited availability.
Keywords: myopia, myopia management, optometry, clinical practice, Saudi Arabia
INTRODUCTION
Myopia prevalence has dramatically increased worldwide, reaching epidemic levels. In the United States, one-third of individuals aged 12 years and older are reported as myopic[1]. European countries such as Hungary revealed that myopic refractive error was three times higher in young adult individuals compared to older age groups (>55y)[2]. Some Asian countries have documented an even higher prevalence of myopia. In China, the prevalence is more than 80% among schoolchildren older than 12y[3], where the myopia prevalence in Chinese university students exceeded 90%[4]. It is estimated that by 2050, approximately half of the world's population will be myopic[5]. Despite the significant increase in myopia prevalence worldwide, the prevalence varies across populations of different regions and ethnicities. In Saudi Arabia, studies reported a myopia prevalence of 49% among adults in the Riyadh region[6], and a similar prevalence was reported in adults in the eastern region of the country[7]. Few cross-sectional studies examined the prevalence of myopia among children in Saudi Arabia and found that the prevalence of uncorrected myopia varied between 4% and 6%[8]–[9].
The issue of myopia is not only the reduced visual acuity but also the potential for substantial vision loss. It has been reported that patients with moderate (spherical equivalent ≤-3.0 to >-6.0 D) to high myopia (spherical equivalent ≤-6.0 D) are significantly more susceptible to ocular abnormalities and at a higher risk of developing vision-threatening ocular diseases, such as cataracts, retinal detachment, chorioretinal atrophy, and glaucoma[10]–[11]. Additionally, the earlier the onset of myopia, the greater the risk of its progression and severity. This increases the risk of serious ocular diseases associated with myopia and the lifetime economic burden[12]–[13]. Therefore, early management of myopia progression with effective strategies should be a priority.
Slowing myopia progression can be accomplished by either of two mechanisms of action, optical or pharmaceutical, both of which have clinically relevant therapeutic effects. There are three main evidence-based myopia control strategies: two based on optical defocus (overnight orthokeratology and multifocal soft contact lenses) and one pharmaceutical agent (topical atropine)[14]–[19]. Based on available evidence from clinical trials, atropine appears to be the most promising single therapy for myopia retardation, with up to a 70% myopia control rate depending on the atropine dose. However, significant side effects are associated with higher concentrations[14]–[15]. In contrast, optical modalities showed significant anti-myopia efficacy in children, varying between 43% and 46% for orthokeratology and multifocal contact lenses[16].
Therefore, understanding the current clinical habits of myopia management is essential. Practitioners in countries such as the US and China are early adopters of myopia control treatment modalities in optometric practices to address the dramatic increase in myopia prevalence and severity; however, there are significant intra-regional differences. The vast majority of practitioners still prescribe single-vision spectacles as the primary management of pediatric myopia[20]–[21].
In Saudi Arabia, most healthcare services are provided free of charge to all citizens. Ministry of Health is the government and primary service provider through its public hospitals and health centers across the country, making up 60% of the health care services[22]. In 2002, Health Insurance Council was formed in Saudi Arabia that introduced the first guideline for mandatory health insurance that was implemented gradually. Free-of-charge healthcare services are a unique advantage of the Saudi Arabian healthcare system. However, significant population growth and increased life expectancy have led to long waiting times for many healthcare services that can easily exceed several weeks to months, including vision care services. A referral from a primary care physician to an eye clinic is required for a child with myopia to obtain vision care services. This process will most likely take weeks for a myopic child to receive necessary vision care services. Parents may seek private eye clinics and pay for vision care services to avoid long waits and processes. Since the healthcare system in Saudi Arabia is quite different from that in western countries such as the United States, it may impact the early detection of childhood myopia as well as the adoption and implementation of myopia control management approaches in the region, which may differ from what has been observed in other countries with different healthcare systems.
To the best of our knowledge, several gaps remain with respect to understanding the current clinical practice in Saudi Arabia. There are no published data discussing the current clinical approach of practitioners in Saudi Arabia and their knowledge of the condition. There is a critical need to obtain information that sheds light on the clinical examination and treatment of children with myopia.
The aim of the present study was to assess optometrists' knowledge and understanding of myopia in Saudi Arabia, their self-reported practices in the diagnosis of childhood myopia, and their level of engagement in myopia management. In addition, we investigated the potential limitations that restrict the adoption of myopia treatment modalities in the region.
SUBJECTS AND METHODS
Ethical Approval
This study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of King Saud University College of Medicine (approval number: E-21-6366). Informed consent was obtained from all participants.
Participants
As of 2021, there are a total of 1886 practicing optometrists in Saudi Arabia (64% male), with 45% practicing in the capital of the country (i.e., Riyadh), according to the Saudi Commission for Health Specialties. An online questionnaire was created in English with an available Arabic translated version using Google Forms. The questionnaire was directly distributed to optometrists via email and social media platforms, beginning in November 2021. The questionnaire was available and received responses over 12wk. Reminders were sent every three weeks.
Survey Design
The questionnaire was designed to measure:1) optometrists' knowledge and awareness of myopia, including its associated risk of ocular diseases, 2) self-reported clinical practice performed by optometrists for myopia diagnosis and management for children, 3) myopia control treatment, and 4) self-reported barriers by optometrists that limit the adoption of myopia control treatments. Multiple answers were permitted for some questions about the myopia-associated risk of ocular diseases and the routinely performed clinical procedures.
Statistical Analysis
Statistical analyses were conducted using SPSS (v28 IBM, New York, USA). Descriptive analyses were performed to determine the percentage of respondents for each question. Graphs were plotted using SPSS v28 and Microsoft Excel 2019. A Chi-square analysis was performed to examine the differences between the sample of respondents and the population of optometrists in Saudi Arabia.
RESULTS
Practitioner Demographics
Of the 1886 practitioners, 171 complete responses were collected from 171 optometrists (9.06% response rate) over a period of 12wk, beginning in November 2021. Over 50% of the practitioners were practicing in the Riyadh region as the primary practice location. Approximately 60% of respondents were male optometrists. Almost two-thirds (65%) of the respondents reported having a clinical and research interest in myopia management. Seventy percent of the respondents reported working in public health clinics or hospitals, while the rest worked in independent clinics or academic institutes. Over half of the respondents reported that they routinely provided clinical care to 6 to 15 children with myopia every week. The proportion of respondents who completed the survey did not significantly differ from the population of practicing optometrists in Saudi Arabia based on sex (χ2=0.44, P=0.5) and region (χ2=2.05, P=0.36). The percentage of respondents in this study was greater than that reported in previous studies that targeted optometrists and other healthcare practitioners in Saudi Arabia[23]–[24].
Clinical Examination and Diagnosis of Myopia in Children
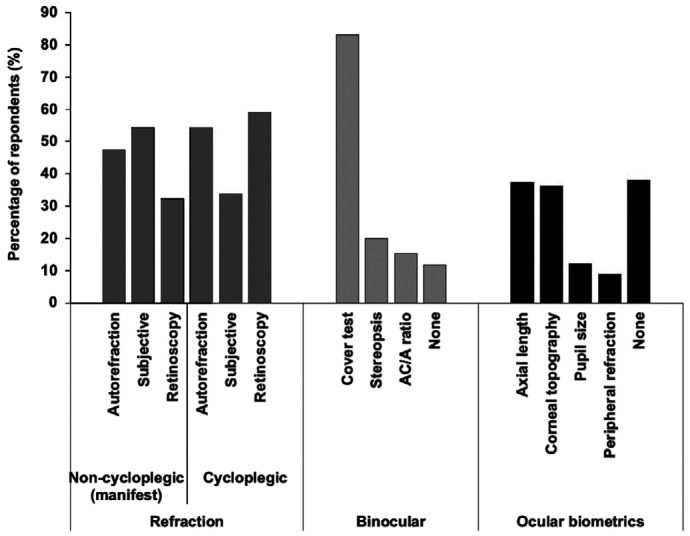
Figure 1 provides an overview of responses regarding the clinical tests that are routinely used to examine schoolchildren with myopia, defined between the ages of 6 and 16y, on initial presentation.
Figure 1. Percentage of reported routinely performed clinical procedures on all school-aged children (5-16y) with myopia on initial presentation.
Three lists of clinical examinations (i.e., refraction, binocular vision, and ocular biometrics) were included in the questionnaire. All respondents indicated that they would perform refraction, with 59% reporting cycloplegic retinoscopy and 53% indicating non-cycloplegic (manifest) subjective refraction. Cycloplegic measures of refraction have been reported to manifest slightly more frequently. Over 80% of respondents indicated that they would perform the cover test, whereas about 12% reported that they did not perform binocular vision assessments in children with myopia. Most respondents (62%) reported that they performed at least one of the listed ocular biometric tests (i.e., axial length, corneal topography, pupil size measurement, and peripheral refraction), whereas approximately 38% reported that they did not perform any of the biometric tests. Axial length measurements and corneal topography were most frequently reported in children with myopia (37% and 36%, respectively; Figure 1).
Practitioners' Awareness of Ocular Complications of High Myopia
Practitioners were asked about their knowledge of the association between high myopia (≤-6.0 D) and ocular pathology with a total of seven ocular conditions being listed in this survey. Interestingly, three ocular conditions (i.e., diabetic retinopathy, age-related macular degeneration, and angle-closure glaucoma) were also listed with the perception of being associated with high myopia, which has not been demonstrated in clinical studies. Association of retinal detachment/breaks with high myopia were reported by 75% of participants whilst approximately one-third of respondents selected cataract to be associated with myopia. The other listed ocular conditions (i.e., choroidal neovascularization, primary open angle glaucoma, angle-closure glaucoma, diabetic retinopathy, and age-related macular degeneration) were reported in the range of 13% to 20%.
Management Approaches to Childhood Myopia in Saudi Arabia
Sixty-five percent of the respondents reported that they did not use any type of myopia treatment modality and prescribed only single-vision distance full correction lenses for children with myopia. Thirty-five percent of respondents reported that they would prescribe myopia control treatment. In the survey, three questions were asked about practitioners' type of myopia management choice as the first, second, and third most commonly prescribed treatment modalities. The questions consisted of a list of myopia control treatment strategies, including atropine, orthokeratology, multifocal contact lenses, multifocal spectacles, and advising patients to increase the time spent outdoors. Interestingly, 80% of the respondents who prescribed myopia control treatments reported that advising patients to increase the time spent outdoors was their first choice. However, high-dose atropine (1%) was not administered by any of the practitioners (Table 1).
Table 1. Percentage of optometrists' selections of childhood myopia management approaches.
| Myopia management option | Percentage of most common myopia treatment modality prescribed by practitioners (%) |
||
| 1st choice | 2nd choice | 3rd choice | |
| Atropine eye drops | |||
| High dose (1%) | 0 | 0 | 0 |
| Moderate-dose (0.05%-0.5%) | 0 | 5 | 8.3 |
| Low-dose (0.01%) drops | 1.7 | 20.0 | 11.7 |
| Contact lenses | |||
| Competing defocus soft contact lenses (for example, Misight and distance-center multifocal) | 0 | 11.7 | 13.3 |
| Overnight orthokeratology | 0 | 3.3 | 0 |
| Spectacles | |||
| Progressive addition spectacle lenses | 1.7 | 16.7 | 6.7 |
| Bifocal spectacles | 6.7 | 13.3 | 11.7 |
| Bifocal spectacles with prism | 1.7 | 3.3 | 10 |
| Advice to increase time spent outdoors | 80 | 11.7 | 8.3 |
| Othera | 8.3 | 15 | 30 |
aOther options involved specification of the myopia management approach by the optometrist, including vision therapy, vision training, binocular vision skills, and modifications to indoor lighting.
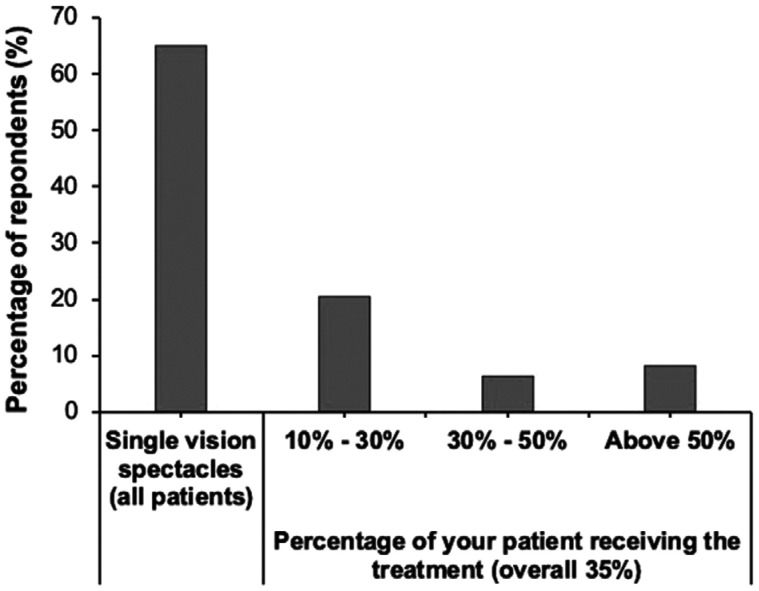
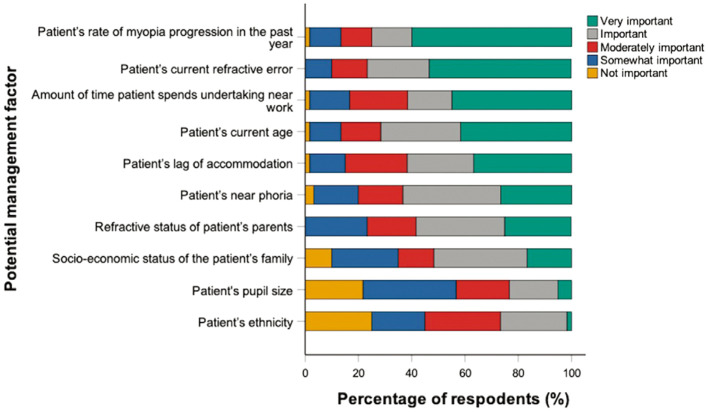
Furthermore, practitioners were asked about the frequency of myopia treatment prescriptions. Sixty percent of the optometrists who reported that they would prescribe myopia treatment indicated that they only prescribed it to approximately 30% or less of their patients with childhood myopia (Figure 2). Practitioners who reported that they would prescribe myopia control treatments were asked to rate the relative importance of several potential factors that are considered important when deciding on a myopia control strategy for a child. The child's rate of myopia progression and the child's current refraction were rated to be “very important” and “important” by over 75% of the respondents. Factors such as the child's pupil size and ethnicity were the least important factors reported when deciding upon myopia treatment (Figure 3).
Figure 2. Percentage of respondents reporting the frequency of prescribing myopia control treatment strategies to their school children with myopia.
Figure 3. Percentage of optometrists rating the relative importance of factors when deciding on a myopia management approach for children.
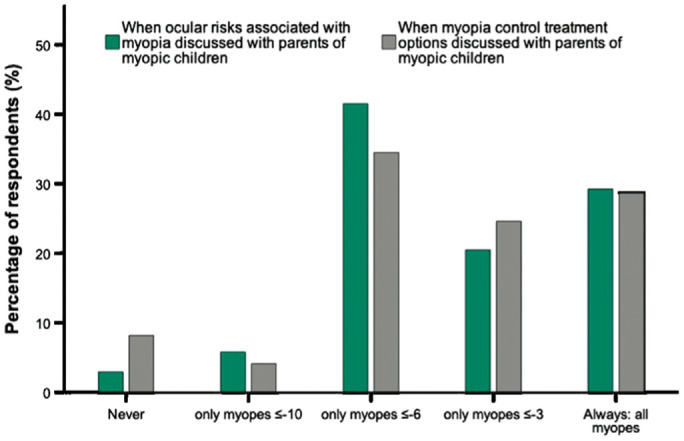
Role of Optometrists in Parent Education
Respondents were asked when and how frequently they discussed the long-term ocular risk associated with myopia and options for management. Approximately 30% of the practitioners reported that they would discuss these topics with parents or adult caregivers of myopic children. Over the third of respondents only discussed the condition and the treatments with an adult caregiver if the child had high myopia (≤-6 D; Figure 4).
Figure 4. Percentage of respondents who indicated discussing the risk of ocular diseases associated with myopia and myopia treatment options with adult caregivers.
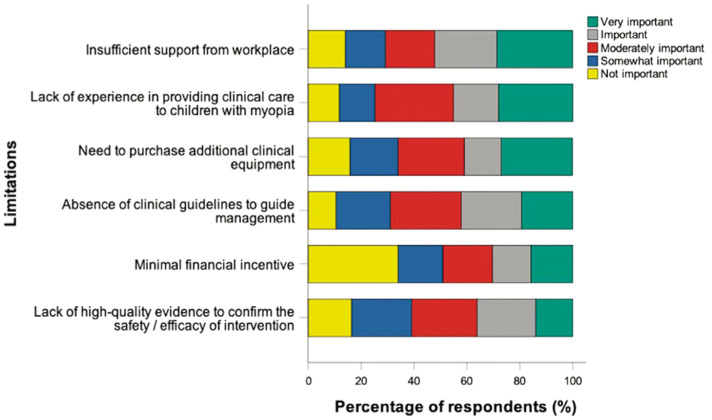
Potential Barriers in Providing Childhood Myopia Treatment
Several potential factors are listed in the survey. Practitioners were asked to rate the relative importance of each factor as a barrier limiting the adoption of myopia control treatment in their practice. The factors that were considered most important were insufficient support from the workplace and the lack of experience needed to provide clinical care to children with myopia (Figure 5).
Figure 5. Percentage of optometrists rating the relative importance of barriers that limit the adoption of myopia management approaches in clinical practices.
DISCUSSION
The major aim of this study was to investigate the knowledge and understanding of optometrists in Saudi Arabia in relation to childhood myopia, current clinical practice in diagnosing childhood myopia, and level of practitioners' engagement in myopia management. The survey also assessed the potential limitations that restrict the adoption of myopia treatment in the country. To the best of our knowledge, this is the first study to report on the current practice of childhood myopia management in Saudi Arabia.
Responses were received from all regions of Saudi Arabia. The majority were male optometrists in the Riyadh region. According to recent data obtained from the Saudi Commission for Health Specialties, there are 1886 practicing optometrists in Saudi Arabia, of which 64% are male, and 45% are in Riyadh. Based on the results, the distribution of respondents by region and gender was similar to that obtained from the Saudi Commission for Health Specialties in 2021. The obtained response rate of the current study was 9.06%, which is higher than the rates reported in previous studies that targeted optometrists and other healthcare professionals in Saudi Arabia at 2.6% and 1.6%, respectively[23]–[24].
With respect to the clinical tests used to examine school-aged children with myopia, there was a slightly higher preference for cycloplegic refraction measures (59% and 54%, respectively). Cycloplegic refraction is considered the “gold standard” for measuring refractive error in children. Failure to use cycloplegic measures likely overestimates the degree of myopia in children[25]. Given there is a strong association between higher myopia and longer ocular axial length[26], ocular biometric measures such as axial length have become essential in monitoring the ocular changes with myopia interventions. Other biometric measures are essential when implementing certain myopia control treatments (i.e., corneal topography for orthokeratology, multifocal contact lens fitting, and pupil size to monitor the induced dilation from atropine treatment). Considering that this study reports current clinical practice rather than research, 37% of practitioners reported taking axial length at the initial examination of a myopic child with myopia, whereas 38% indicated that they would not take any ocular biometric measures. This finding likely reflects the limited accessibility of expensive optical-based biometry medical instruments within optometric practices.
Myopia is a risk factor for several serious ocular diseases that lead to irreversible vision impairment. The risk is significantly higher in highly myopic eyes (≤-6 D). Most respondents were aware of the associated incident risk of retinal breaks/detachments with myopia. However, most respondents were unaware of the risks of cataract, choroidal neovascularization, and primary open angle glaucoma. On the other hand, a proportion of respondents (13% to 16%) reported that there was an association between increased incidence of angle-closure glaucoma, diabetic retinopathy, and age-related macular degeneration with high myopia, which have not been linked with myopia[27]. Although it is well known that several complications are related to high myopia. In this study, there were misconceptions from respondents that some other ocular conditions such as diabetic retinopathy and age-related macular degeneration are also associated with high myopia. Therefore, further education is necessary to provide accurate and recent knowledge about myopia-related complications and to elucidate the mechanisms by which high myopia leads to increased risks of these ocular conditions.
The results of several clinical trials have established that overnight orthokeratology is one of the most effective myopia treatments[28]. The survey asked about the types of myopia management options prescribed by practitioners and how frequently they were prescribed to children with myopia. Approximately two-thirds (65%) reported that they would prescribe only a single vision correction for children with myopia. A similar percentage was found in a study that investigated myopia control global trends in Asia, Australia, Europe, North America, and South America in year 2015[20]. The same study was repeated after between the years 2018 and 2019 and reveal that the primary approach was still prescribing single vision correction for myopic children (64%)[29]. Another study that surveyed Australian optometrists found that about half of practitioners prescribed single vision distance correction to manage myopia in children[21]. Only 35% of the respondents indicated that they would prescribe myopia management approaches to their patients. Notably, advising optometrists to increase the time spent outdoors was the most reported myopia management approach (80%) as a first choice. The beneficial protective effect of increasing time spent outdoors against myopia development and progression has been reported while ensuring adequate outdoor time[30]–[31]. On other hand, other studies have shown no clear benefit against myopia[32]. Interestingly, myopia management approaches such as overnight orthokeratology and high-dose atropine were the least reported by practitioners, which could be linked primarily to lack of experience and knowledge, lack of clinical equipment, and insufficient clinical guidance. Since advising adult caregivers to increase time spent outdoors for their children does not require clinical experience or possession of clinical devices, it is plausible that this management approach was reported to be the most used among practitioners. One of the factors reported as the most important barrier to myopia management adoption was the lack of experience needed to provide clinical care to children with myopia, which supports the high percentage with this particular approach.
This study sheds light on the clinical behaviour of optometrists in relation to childhood myopia in Saudi Arabia. The findings demonstrated that most clinical diagnostic tools were performed on myopic children on the first presentation. Distance single-vision spectacle lenses are considered the main approach by most practitioners. Among the prescribed myopia management approaches, increasing the time spent outdoors is the most commonly used approach.
Moving forward, some public health efforts should focus on promoting the importance of early establishment of ocular growth profiles and possible government subsidies for optical biometers to allow the earliest possible detection of abnormal axial elongation preceding the refractive onset of myopia. Moreover, note that currently, none of the novel spectacles designed for myopia control are available in Saudi Arabia; however, once available, they will likely play an important role in the public health effort for myopia management, considering their safety, convenience, and feasibility in the primary care setting.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research, College of Applied Medical Sciences Research Center at King Saud University, for funding this work.
Conflicts of Interest: Alanazi MK, None; Almutleb ES, None; Badawood YS, None; Kudam MA, None; Liu M, None.
REFERENCES
- 1.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 2.Németh J, Daiki T, Dankovics G, Barna I, Limburg H, Nagy ZZ. Prevalence of refractive errors in Hungary reveals three-fold increase in myopia. Int J Ophthalmol. 2022;15(7):1174–1179. doi: 10.18240/ijo.2022.07.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lam CS, Goldschmidt E, Edwards MH. Prevalence of myopia in local and international schools in Hong Kong. Optom Vis Sci. 2004;81(5):317–322. doi: 10.1097/01.opx.0000134905.98403.18. [DOI] [PubMed] [Google Scholar]
- 4.Shi XY, Ke YF, Jin N, Zhang HM, Wei RH, Li XR. The prevalence of vision impairment and refractive error in 3654 first year students at Tianjin Medical University. Int J Ophthalmol. 2018;11(10):1698–1703. doi: 10.18240/ijo.2018.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Almudhaiyan T, Alhamzah A, AlShareef M, Alrasheed A, Jaffar R, Alluhidan A, Al-Hazazi M, Aldebasi T. The prevalence of refractive errors among Saudi adults in Riyadh, Saudi Arabia. Saudi J Ophthalmol. 2020;34(1):30–34. doi: 10.4103/1319-4534.301297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alsaif BA, Aljindan MY, Alrammah HM, Almulla MO, Alshahrani SS. Refractive errors among Saudi college students and associated risk factors. Clin Ophthalmol. 2019;13:437–443. doi: 10.2147/OPTH.S193213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alsaqr AM, Ibrahim G, Sharha AA, Fagehi R. Investigating the visual status of preschool children in Riyadh, Saudi Arabia. Middle East Afr J Ophthalmol. 2017;24(4):190–194. doi: 10.4103/meajo.MEAJO_123_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aldebasi YH. Prevalence of correctable visual impairment in primary school children in Qassim Province, Saudi Arabia. J Optom. 2014;7(3):168–176. doi: 10.1016/j.optom.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25(5):381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 11.Ha A, Kim CY, Shim SR, Chang IB, Kim YK. Degree of myopia and glaucoma risk: a dose-response meta-analysis. Am J Ophthalmol. 2022;236:107–119. doi: 10.1016/j.ajo.2021.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Holden B, Sankaridurg P, Smith E, Aller T, Jong M, He M. Myopia, an underrated global challenge to vision: where the current data takes us on myopia control. Eye (Lond) 2014;28(2):142–146. doi: 10.1038/eye.2013.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen YX, Liao CM, Tan Z, He MG. Who needs myopia control? Int J Ophthalmol. 2021;14(9):1297–1301. doi: 10.18240/ijo.2021.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2) Ophthalmology. 2012;119(2):347–354. doi: 10.1016/j.ophtha.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Huang JH, Wen DZ, Wang QM, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016;123(4):697–708. doi: 10.1016/j.ophtha.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Walline JJ. Myopia control: a review. Eye Contact Lens. 2016;42(1):3–8. doi: 10.1097/ICL.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 17.Ma JX, Tian SW, Liu QP. Effectiveness of peripheral defocus spectacle lenses in myopia control: a Meta-analysis and systematic review. Int J Ophthalmol. 2022;15(10):1699–1706. doi: 10.18240/ijo.2022.10.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao Y, Feng K, Liu RB, Pan JH, Zhang LL, Xu ZP, Lu XJ. Atropine 0.01% eye drops slow myopia progression: a systematic review and Meta-analysis. Int J Ophthalmol. 2019;12(8):1337–1343. doi: 10.18240/ijo.2019.08.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan SY, Wang YZ, Li J, Zhang XH, Wang J, Zhu XP, Xiao XH, Liu JT. Short-term effect of 0.01% atropine sulphate eye gel on myopia progression in children. Int J Ophthalmol. 2022;15(7):1122–1127. doi: 10.18240/ijo.2022.07.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolffsohn JS, Calossi A, Cho P, et al. Global trends in myopia management attitudes and strategies in clinical practice. Cont Lens Anterior Eye. 2016;39(2):106–116. doi: 10.1016/j.clae.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Douglass A, Keller PR, He MG, Downie LE. Knowledge, perspectives and clinical practices of Australian optometrists in relation to childhood myopia. Clin Exp Optom. 2020;103(2):155–166. doi: 10.1111/cxo.12936. [DOI] [PubMed] [Google Scholar]
- 22.Yusuf N. Private and public healthcare in Saudi Arabia: future challenges. Int J Bus Econ Dev. 2014;2:114–118. [Google Scholar]
- 23.Ovenseri-Ogbomo GO, Alghamdi W. Knowledge, attitudes, and practices of optometrists regarding low vision services in Saudi Arabia. Open Ophthalmol J. 2021;15(1):217–288. [Google Scholar]
- 24.Al-Dabaan R, Newton JT, Asimakopoulou K. Knowledge, attitudes, and experience of dentists living in Saudi Arabia toward child abuse and neglect. Saudi Dent J. 2014;26(3):79–87. doi: 10.1016/j.sdentj.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fotedar R, Rochtchina E, Morgan I, et al. Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study. Am J Ophthalmol. 2007;144(2):307–309. doi: 10.1016/j.ajo.2007.03.041. [DOI] [PubMed] [Google Scholar]
- 26.Ip JM, Huynh SC, Kifley A, Rose KA, Morgan IG, Varma R, Mitchell P. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. 2007;48(10):4846–4853. doi: 10.1167/iovs.07-0101. [DOI] [PubMed] [Google Scholar]
- 27.Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622–660. doi: 10.1016/j.preteyeres.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Hiraoka T. Myopia control with orthokeratology: a review. Eye Contact Lens. 2022;48(3):100–104. doi: 10.1097/ICL.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 29.Wolffsohn JS, Calossi A, Cho P, et al. Global trends in myopia management attitudes and strategies in clinical practice - 2019 Update. Cont Lens Anterior Eye. 2020;43(1):9–17. doi: 10.1016/j.clae.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Deng L, Pang Y. Effect of outdoor activities in myopia control: meta-analysis of clinical studies. Optom Vis Sci. 2019;96(4):276–282. doi: 10.1097/OPX.0000000000001357. [DOI] [PubMed] [Google Scholar]
- 31.Cao K, Wan Y, Yusufu M, Wang NL. Significance of outdoor time for myopia prevention: a systematic review and meta-analysis based on randomized controlled trials. Ophthalmic Res. 2020;63(2):97–105. doi: 10.1159/000501937. [DOI] [PubMed] [Google Scholar]
- 32.Xiong SY, Sankaridurg P, Naduvilath T, Zang JJ, Zou HD, Zhu JF, Lv MZ, He XG, Xu X. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551–566. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]