Abstract
Purpose
To report an unusual case of interstitial keratitis and lipid keratopathy in a pregnant woman with unknown etiology and atypical clinical course.
Observations
A 15 weeks pregnant 32-year-old female daily soft contact lens wearer presented with 1 month of right eye redness and intermittent blurry vision. Slit lamp examination revealed sectoral interstitial keratitis with stromal neovascularization and opacification. No underlying ocular or systemic etiology was identified. The corneal changes were unresponsive to treatment with topical steroids and progressed over the ensuing months of her pregnancy. On continued follow up, the cornea demonstrated spontaneous partial regression of the opacification in the post-partum period.
Conclusions and importance
This case illustrates a possible rare manifestation of pregnancy physiology in the cornea. It also emphasizes the utility of close follow-up and conservative management in pregnant patients with idiopathic interstitial keratitis not only to avoid intervention during pregnancy but also because of the possibility of spontaneous improvement or resolution of the corneal changes.
Keywords: Interstitial keratitis, Lipid keratopathy, Pregnancy
1. Introduction
Ocular manifestations of pregnancy may arise due to physiologic hormonal, metabolic, and immunologic changes, worsening of pre-existing systemic diseases, new concurrent diseases, or conditions that occur uniquely in pregnancy.1, 2, 3 Interstitial keratitis may be seen in pregnant patients with concurrent infectious or autoimmune processes, with the most common etiologies in the United States overall being herpes simplex virus, idiopathic, and syphilis.4,5 Lipid deposition in the cornea may occur in areas of corneal neovascularization following infection, inflammation, or trauma – a condition known as lipid keratopathy.
We report the case of idiopathic interstitial keratitis and lipid keratopathy in a pregnant patient that began to regress spontaneously in the post-partum period.
2. Case report
A 32-year-old woman presented with a one month history of redness, foreign body sensation, and intermittent blurred vision in the right eye. The patient was a daily soft contact lens wearer (Acuvue Oasys). She denied sleeping in her contact lenses, dry eye symptoms, prior similar episodes, or any symptoms in her left eye. She reported multiple prior unremarkable eye exams. The patient had taken a week-long contact lens holiday with no improvement in her symptoms. At the time of presentation, she was 15 weeks pregnant (second pregnancy). Apart from myopia and pregnancy, the patient had no prior ocular or medical history. Her family history was notable for cataracts, glaucoma, diabetes mellitus, and hypertension in first degree relatives. Her only medication was a prenatal vitamin and she had no known drug or environmental allergies. She denied alcohol, tobacco, or illicit substance use and had not traveled recently. Her ophthalmologic and general review of systems were otherwise negative.
At presentation, BCVA was 20/20 OU. Intraocular pressure (IOP) was 15 mm Hg in the right eye and 14 mm Hg in the left eye by Goldmann applanation tonometry. Slit lamp examination of the right eye revealed 2+ injection inferonasally and an adjacent area of stromal thickening, opacification and neovascularization (Fig. 1). The marginal tear strip was not deficient and there was no ocular surface staining. Corneal sensation was intact and the anterior chamber was quiet. The rest of the anterior and posterior segment exams of the right and left eyes were unremarkable. The patient was started on prednisolone acetate 1% drops QID to the right eye, preservative free artificial tears as needed for comfort, and was asked to refrain from contact lens wear. Due to minimal change in the patient's symptoms and exam one week later, she was also started on oral acyclovir 400 mg TID. Gonioscopy did not reveal any abnormality in the anterior chamber beneath the corneal opacity and ultrasound biomicroscopy did not identify foreign body or other pathology. Due to lack of clinical improvement (Fig. 2A), laboratory workup was undertaken to explore possible infectious and autoimmune etiologies. Labs were notable for presence of EBV early antigen IgG and EBV nuclear antigen IgG antibodies (negative EBV IgM), elevated erythrocyte sedimentation rate of 41 (reference range 0–33), and mildly elevated C-reactive protein of 11 (reference range <10). HSV-1 IgG and HSV-2 IgG titers were negative. CBC, CMP, FTA-ABS, RPR, VZV IgM, ANA, ANCA profile, Lyme, Rheumatoid factor, and QuantiFERON-TB Gold were within normal limits. The patient was then trialed on difluprednate ophthalmic 0.05% drops, initially six times per day then decreased to QID, however the density of the corneal opacity seemed to increase (Fig. 2B). Her BCVA remained at 20/20. The patient deferred biopsy until after she delivered a healthy full term baby following an otherwise uncomplicated pregnancy. 7 months after presentation (and 1 month post-partum) the patient underwent a right corneal biopsy/superficial keratectomy (treated in the post-operative period with Polytrim drops QID, prednisolone drops QID, Ketorolac as needed for pain). Pathology was notable for chronic non-granulomatous inflammation with fibrosis and vascularization in the corneal stroma and limbal conjunctiva, reportedly most compatible with an inflammatory or infectious process that resulted in subepithelial conjunctival and corneal stromal scarring with active neovascularization. There was no evidence of acute or granulomatous inflammation, viral cytopathic effect, dermoid-like lesion, or malignancy. The patient elected not to pursue additional treatment or interventions such as subconjunctival bevacizumab injections and corneal argon laser photocoagulation. She was evaluated again 1 and 1.5 years from initial presentation and was noted to have spontaneous improvement in her symptoms and appearance of the cornea, with decreased stromal vascularization and opacification noted on exam (Fig. 2C and D).
Fig. 1.
Slit lamp image of the patient's right eye at the time of presentation showing significant nasal conjunctival injection and adjacent stromal interstitial keratitis with fine vascularization.
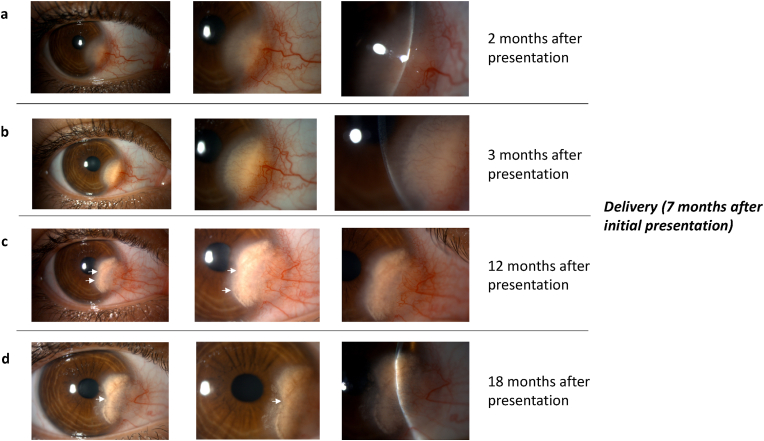
Fig. 2.
Slit lamp images of the patient's right eye at various time points in the clinical course including 2 (A), 3 (B), 12 (C), and 18 (D) months after initial presentation. At 2 months following initial presentation, clinical exam showed focal injection and an adjacent area of interstitial keratitis with worsening stromal opacification and neovascularization (A). A month later, the cornea demonstrated increased opacification and lipid deposition (B). In the post-partum period and 12 months after initial presentation, the region of opacification was beginning to regress clinically (arrows; angle at which slit lamp photo was taken at month 12 more oblique compared to B and D). 1.5 years after initial presentation (and 11 months post-partum), decreased stromal vascularization and opacification was seen (arrow).
3. Discussion
Ocular changes in pregnancy can be categorized as physiologic and pathologic. Examples of physiologic changes include increased corneal and lens thickness leading to refractive changes, as well as decreased IOP due to progesterone's effect on aqueous dynamics. Pathologic changes may be further subdivided into worsening of pre-existing ocular diseases, such as dry eye and diabetic retinopathy, or worsening of systemic diseases with ocular manifestations, including preeclampsia and idiopathic intracranial hypertension.1,2 The ocular findings may improve or resolve spontaneously after delivery but clinical course depends on the underlying etiology and overall health status of the patient.
Interstitial keratitis most frequently occurs due to infectious or inflammatory processes. The most common causes of interstitial keratitis in the United States include herpetic infection, idiopathic, and syphilis.4, 5, 6 Immune-mediated diseases including sarcoidosis, Cogan's syndrome, and contact lens-associated keratitis have also been shown to present with inflammation of the corneal stroma.4,5 Although the aforementioned disease processes may affect pregnant individuals, to our knowledge, there is not an overall increased incidence of interstitial keratitis in pregnancy.
Lipid keratopathy is a condition that occurs due to lipid deposition in the cornea in areas of corneal neovascularization. It may be idiopathic or occur following infection, inflammation, or trauma.6 The cornea relies on several mechanisms to maintain its clarity and avascularity by balancing pro-angiogenic factors with antiangiogenic factors. Infection, inflammation, or trauma may disrupt this balance towards a pro-angiogenic state. As such, current treatment options target the elimination of corneal neovascularization to halt the leakage of lipid from incompetent newly-formed stromal vessels. This is done by suppressing the activity of inflammatory mediators that release pro-angiogenic growth factors using topical steroids and/or anti-VEGF agents. Other therapeutic modalities such as photodynamic therapy, argon laser and/or needlepoint cautery are also helpful in reducing/eliminating the corneal vascularization.6
We postulate that our patient may have had a small area of corneal neovascularization from prior infection, contact lens wear, or trauma which remained sub-clinical until she became pregnant. Due to the change in physiologic state and the production of pro-angiogenic factors, including placental growth factor (PlGF) by the placenta, the cornea may have developed increased neovascularization leading to clinically-significant lipid keratopathy.7, 8, 9 What remains unusual in this case is the initial lack of response to topical steroids contrasted with the spontaneous improvement without treatment in the post-partum period. We hypothesize that, following delivery, the serum PlGF levels returned to normal thus tipping the balance away from a pro-angiogenic state, resulting in reduced angiogenesis while allowing the fibroblasts to remove the deposited lipid. Regardless of the presumed mechanism of the spontaneous partial regression of our patient's corneal stromal vascularization and opacification, this case highlights the importance of careful follow-up in managing pregnant patients with presumed non-infectious interstitial keratitis and lipid keratopathy. Topical steroids and oral antiviral/antibiotic therapy are reasonable therapeutic options when appropriate. However, as long as the visual axis remains clear, the clinical course of our patient suggests it might be prudent to wait until after delivery before considering treatment with invasive procedures such as subconjunctival bevacizumab injections (for which pregnancy is a relative contraindication), argon laser photocoagulation, fine needle cautery and photodynamic therapy.
4. Patient consent
Consent to publish this case was obtained. This report does not contain any personal information that could lead to the identification of the patient.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors wish to thank Dr. Zeba Syed for providing the initial presentation clinical photo. No funding or grant support. The following authors have no financial disclosures: PD, IR. All authors attest that they meet the current ICMJE criteria for Authorship.
References
- 1.Naderan M. Ocular changes during pregnancy. J Curr Ophthalmol. Sep. 2018;30(3):202–210. doi: 10.1016/j.joco.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheth B.P., Mieler W.F. Ocular complications of pregnancy. Curr Opin Ophthalmol. Dec. 2001;12(6):455–463. doi: 10.1097/00055735-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Kalogeropoulos D., Sung V.C., Paschopoulos M., Moschos M.M., Panidis P., Kalogeropoulos C. The physiologic and pathologic effects of pregnancy on the human visual system. J Obstet Gynaecol. Nov. 2019;39(8):1037–1048. doi: 10.1080/01443615.2019.1584891. [DOI] [PubMed] [Google Scholar]
- 4.Tu E.Y. Principles and Practice of Ophthalmology 3e. Jakobiec; 2007. Interstitial keratitis. [Google Scholar]
- 5.Schwartz G.S., Harrison A.R., Holland E.J. Etiology of immune stromal (interstitial) keratitis. Cornea. May. 1998;17(3):278–281. [PubMed] [Google Scholar]
- 6.Hall M.N., Moshirfar M., Amin-Javaheri A., Ouano D.P., Ronquillo Y., Hoopes P.C. Lipid keratopathy: a review of pathophysiology, differential diagnosis, and management. Ophthalmol Ther. Dec. 2020;9(4):833–852. doi: 10.1007/s40123-020-00309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Falco S., Gigante B., Persico M.G. Structure and function of placental growth factor. Trends Cardiovasc Med. Aug. 2002;12(6):241–246. doi: 10.1016/s1050-1738(02)00168-8. [DOI] [PubMed] [Google Scholar]
- 8.Chau K., Hennessy A., Makris A. Placental growth factor and pre-eclampsia. J Hum Hypertens. Dec. 2017;31(12):782–786. doi: 10.1038/jhh.2017.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Autiero M., Waltenberger J., Communi D., et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt 1 and Flk 1. Nat Med. Jul. 2003;9(7):936–943. doi: 10.1038/nm884. [DOI] [PubMed] [Google Scholar]