Abstract
Background
Every woman has the right to receive quality care during pregnancy. It is proven that antenatal care (ANC) reduces maternal and perinatal morbidity and mortality. The government of Ethiopia is also making intense efforts to increase the coverage of ANC. However, among pregnant women, the levels of satisfaction with the care provided are overlooked, as the percentage of women who complete all ANC visits is below 50. Therefore, this study aims to assess maternal satisfaction with ANC services rendered at public health facilities in the West Shewa Zone, Ethiopia.
Methods
A facility-based cross-sectional study was conducted among women who were receiving ANC in public health facilities in Central Ethiopia between September 1 and October 15, 2021. A total of 411 women were selected using the systematic random sampling method. The questionnaire was pretested and the data were collected electronically using CSEntry. The collected data were exported to SPSS version 26. The characteristics of the study participants were described using frequency and percentage. Bivariate and multivariate logistic regression were used to identify the factors associated with maternal satisfaction with focused ANC service.
Result
This study revealed that 46.7% [95% confidence interval (CI) (41.7%–51.6%)] of women were satisfied with ANC service. Factors such as the quality of the health institution [adjusted odd ratio (AOR) = 5.10, (95% CI: 3.33–7.75)], place of residence [AOR = 2.38, (95% CI: 1.21–4.70)], history of abortion [AOR = 0.19, (95% CI: 0.07–0.49)], and previous mode of delivery [AOR = 0.30, (95% CI: 0.15–0.60)] were significantly associated with women's satisfaction with focused ANC service.
Conclusion
More than half of pregnant women who received ANC were dissatisfied with the service they received. This should be a cause for concern, as the level of satisfaction is lower than that of the findings of previous studies conducted in Ethiopia. Institutional variables, interactions with patients, and previous experiences of pregnant women have an impact on the level of satisfaction. Due attention should be paid to primary health and communication of health professionals with pregnant women to improve the levels of satisfaction with focused ANC service.
Keywords: pregnant women, satisfaction, ANC, West Shewa, Central Ethiopia
Plain language summary
Despite a significant decline in maternal deaths globally, the daily loss of life among women continues to increase because of entirely preventable factors prior to, during, and following childbirth. Most maternal deaths primarily occur in low- and middle-income countries. Ethiopia is one of the countries with the highest maternal mortality rates in the world, estimated at 412 per 100,000 live births. This far outstrips the global goal of lowering maternal mortality to less than 70 per 100,000 live births by 2030. Prenatal care (ANC) provides a framework for taking significant healthcare initiatives such as disease prevention and health promotion.
The mother's satisfaction level with the antenatal care offered in the medical institution is clinically relevant and requires a painstaking assessment of the many aspects of healthcare. Although the level of satisfaction with maternal ANC services is crucial for the relevant stakeholders to advance mother and child health, little is known about these levels and their determinants in Ethiopia and the study area. Therefore, studying the satisfaction levels and their determinant factors will provide significant inputs for resource-poor settings in order to scale up maternal ANC service satisfaction. The finding of this result is important for effecting further improvements in maternal and child health.
Introduction
Despite substantial advancement over the past few decades, ending preventable maternal deaths remains an unmet goal and one of the world's most critical concerns. Despite a 38% reduction in maternal deaths globally between 2000 and 2017, 810 women still lose their lives every day to mainly preventable causes before, during, and after childbirth. Low- and middle-income countries account for 94% of all maternal deaths (1, 2). Ethiopia has one of the highest maternal mortality rates in the world at 412 per 100,000 live births, well exceeding the global target of reducing maternal mortality to less than 70 per 100,000 live births by 2030 (3, 4).
One of the top priorities of Sustainable Development Goals (SDGs) is to lower maternal mortality (5). Antenatal care (ANC) remains one of the interventions that has the potential to significantly reduce maternal morbidity and mortality if properly provided (5–8). Focused ANC provides a framework for crucial medical procedures such as disease screening, disease prevention, and the management of pregnancy-related problems. In addition, it offers unique opportunities for the early detection and treatment of problems such as hypertension, gestational diabetes, anaemia, malaria, HIV, and other illnesses that might otherwise put the health of pregnant women and the developing fetus at risk (6, 7, 9, 10).
The women's level of satisfaction with the ANC service offered in the medical institution is clinically significant and requires an assessment of patients on several elements of healthcare, including organizational, interpersonal, and technical components (11–13). According to the literature, satisfaction with many aspects of prenatal care received enhances health outcomes, continuity of care, and treatment compliance (6–8, 14). To enhance the effectiveness and quality of prenatal care, the World Health Organization (WHO) suggests monitoring and evaluating maternal satisfaction with public health care services during pregnancy (7). The Ethiopian government has made great strides towards bringing health facilities closer to the community, mainly through constructing primary healthcare facilities and launching the health extension program, which could help in increasing the coverage of ANC services (15, 16). However, the experiences of pregnant women with the service provided are overlooked, as the percentage of women who complete receiving all ANC services is below 50. Moreover, many health facilities have started service provision without being properly equipped with the necessary equipment and qualified health personnel. For instance, of 80% of the facilities providing focused ANC, only 41% of them are able to provide high-quality ANC service (4).
Various studies have found varying levels of women's satisfaction with ANC services. These levels are as follows: approximately 69% of women in America (11), 90% in Kazakhstan (17), 98.5% in Nigeria (18), and 41.1% in Egypt (19). In Ethiopia, maternal satisfaction with ANC service varies by location, ranging from 30.3% to 83.9% (20, 21).
Studies have shown that factors such as the frequency of ANC visits, monthly income, educational level, age, pregnancy status, type of health facility, history of stillbirths, information on the potential risks of pregnancy, respectful maternity care, location, place of residence, provider of male sex services, occupation, and waiting time are important predictors of maternal satisfaction with ANC service (11, 19–25).
Coronavirus disease (COVID-19) has a major impact on the quality, satisfaction, and use of maternal and reproductive healthcare services, including ANC. Therefore, regular monitoring and evaluation of service performance is essential (26–28). The level of maternal satisfaction with ANC services is crucial for the relevant stakeholders to effect improvements in the area of mother and child health. However, most of the past studies conducted in Ethiopia assessed maternal satisfaction levels at single health facilities, and little is known about these levels and their determinants in present-day Ethiopia and the study area in particular. In light of this, this study aims to assess the level and determinants of maternal satisfaction with focused ANC services rendered at public health facilities in the West Shewa Zone in Central Ethiopia. The study's findings can aid policymakers, regulating authorities, health institutions, communities, and other groups working in the field of maternal, new-born, and child health to improve service quality.
Materials and Methods
Study design, area, and period
A facility-based cross-sectional study was conducted in public health facilities found in the West Shewa Zone, Central Ethiopia, from September 1 to October 15, 2021. The zone is located in the Oromia Regional State to the west of Addis Ababa, the capital city of Ethiopia. Ambo, the capital of the West Shewa Zone, is located 114 km away from Addis Ababa. According to information from the West Shewa Zonal Health Office in 2021, the total population in the zone is estimated to be 2,381,079, of which 1,214,350 are women. There are 9 government hospitals, 96 health centers, and 529 health posts in the zone. Women aged 15–49 are estimated to be 21.3%.
Population
All mothers who have been receiving ANC service follow-up during the study period at public health facilities in the West Shewa Zone constitute the source population, while pregnant women who have been receiving ANC service in select public health facilities in the zone during this period form the study population. All pregnant women who resided in the study area for at least 6 months are included in the study.
Sample size determination
The sample size was calculated using the single-population proportion formula, with the assumptions of a 95% (α/2 = 1.96) confidence level, 5% marginal error, 10% non-response rate, and a 53.8% level of antenatal care service satisfaction from Debra Tabor's previous study (22). Hence, after adding a 10% non-response rate, the final sample size was 420.
Sampling procedure
Within the West Shewa Zone, where the study was done, there are 96 health centers and 9 public hospitals. A total of 3 hospitals and 20 health centers were randomly selected. In order to estimate the monthly calculable number of pregnant women for ANC service, 3-month ANC registration books at the chosen health institutions were reviewed. The total number of pregnant women who received ANC services in a given month was then divided by the calculated sample size of 420 to estimate the number of pregnant women from each public health facility. Finally, a systematic random sampling technique was used to select study participants.
There were 5,424 pregnant women who received focused ANC service in all public health facilities, which meant that, on average, 1,808 pregnant women received ANC service every month in all public health facilities. By proportionally allocating the calculated 420 sample size to the total number of pregnant women who received ANC services in each month (420/1,808), the sampling fraction became one-fourth. Then, every four pregnant women registered for ANC service throughout the data collection period were recruited from every health facility for this study.
Data collection tool, procedure, and quality control
The data collection tool was adapted by reviewing similar kinds of literature to assess pregnant women's satisfaction with focused ANC services (10, 19–25) and others. The questionnaire was prepared in English and translated into the local language, Afan Oromo, and the translated version was used to collect the data. The questionnaire was designed in CSPRO version 7.3 software and exported to CSEntry for Android for electronic data collection. Data were collected by 13 BSC registered midwives, and five master’s holders supervised the data collection.
At Ginchi Primary Hospital, the questionnaire was pretested on 5% of the sample size, and any necessary corrections were made 1 week before the actual data collection time. A reproductive health expert assessed the content and face validity. The Cronbach alpha value, which was determined to assess the tool's internal consistency, was 0.86. Finally, data collectors and supervisors received 2 days of training on the study's objectives.
Data processing and analysis
The CS-Entry android app was used to collect the data, which was then exported to SPSS version 25 for data analysis. Descriptive statistics were used for determining the frequency, percentage, mean, and standard deviation. The factors associated with the outcome variable were found using binary logistic regression. The multivariable logistic regression model included all explanatory variables that, in the bivariate analysis, had a significant relationship with the outcome variable. Crude and adjusted odds ratios with their 95% confidence interval (CI) were determined and a statistically significant association was found based on a P-value of less than 0.05. Multi-collinearity between the independent variables was also assessed using multiple linear regressions, and the variance inflation factor (VIF) for all variables was less than 10. The fitness of the logistic regression model was also evaluated using the Hosmer–Lemeshow statistic greater than 0.05.
Operational definition
Women's satisfaction with focused ANC services meant that the women scored greater than or equal to the overall mean satisfaction score, from the total satisfaction with ANC service–related questionnaires (22).
Results
The demographic characteristics of the respondents
A total of 411 pregnant women receiving focused ANC services participated in this study, with the response rate being 97.8%. The mean age of the study participants was 25.8 years, with a standard deviation of ±4.6 years. A majority of the participants, 388 (94.4%), were of Oromo ethnicity. A total of 241 (60.1%) women were urban residents (Table 1).
Table 1.
Socio-demographic characteristics of pregnant women receiving antenatal care at public health facilities in the West Shewa Zone, Central Ethiopia, 2021.
| Variable | Category | Frequency (N = 420) | Percentage |
|---|---|---|---|
| Age in years | <20 | 53 | 12.9 |
| 21–34 | 335 | 81.5 | |
| >35 | 23 | 5.6 | |
| Marital status | Married | 401 | 97.6 |
| Not married | 10 | 2.4 | |
| Ethnicity | Oromo | 388 | 94.4 |
| Amhara | 17 | 4.1 | |
| Gurage | 6 | 1.5 | |
| Religion | Protestant | 226 | 55 |
| Orthodox | 160 | 38.9 | |
| Othersa | 25 | 6.1 | |
| Mother occupation | Housewife | 227 | 55.2 |
| Private employee | 80 | 19.5 | |
| Government employee | 64 | 15.6 | |
| Othersb | 40 | 9.7 | |
| Husband occupation | Not working | 19 | 4.6 |
| Private employee | 231 | 56.2 | |
| Government employee | 149 | 36.3 | |
| Othersb | 12 | 2.9 | |
| Mothers’ education | No formal education | 41 | 10 |
| Primary school | 110 | 26.8 | |
| High school | 131 | 31.9 | |
| College and above | 129 | 31.4 | |
| Husband education | No formal education | 34 | 8.3 |
| Primary school | 59 | 14.4 | |
| Secondary school | 128 | 31.1 | |
| College and above | 190 | 46.2 | |
| Residence | Rural | 241 | 60.1 |
| Urban | 164 | 39.9 | |
| Average monthly incomec | <1,380 | 67 | 16.3 |
| 1,381–6,900 | 222 | 54 | |
| >6,901 | 122 | 29.7 |
Wakefata and Catholic.
Students, daily labourers, and non-government organization employee.
WHO income classification for developing countries using Ethiopian Birr.
Obstetric and reproductive health characteristics of the participants
The median age at pregnancy of the study participants was 22 years, with an interquartile range of 4 years. More than half (60.8%) of the participants, 250, were multigravida. A total of 203 (49.3%) pregnant women underwent ANC follow-up during their past pregnancy, while only 58 (23.2%) received postnatal care during their previous pregnancy. Forty-eight (11.7%) study participants had a history of abortion. Of the abortion cases, 42 (87.5%) were spontaneous in nature. A majority of the 244 participants (84.7%) delivered in a health facility. Nearly one-fifth (19.6%) of pregnant women, 49, had a history of medical disorders during their past pregnancy. More than half (60.1%) of them, 247, did not remember their last normal menstrual period during their pregnancy (Table 2).
Table 2.
Obstetrics and reproductive health characteristics of pregnant women receiving ANC service at public health facilities in the West Shewa Zone, Central Ethiopia, 2021.
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Gravida | Primigravida | 161 | 39.2 |
| Multigravida | 250 | 60.8 | |
| Number of children | No child | 165 | 40.1 |
| 1–3 children | 219 | 53.3 | |
| ≥4 children | 27 | 6.6 | |
| Place of last delivery | Home | 44 | 15.3 |
| Health facility | 244 | 84.7 | |
| Past illness during pregnancy | Pre-eclampsia | 24 | 48.9 |
| HEG | 17 | 34.7 | |
| Gestation diabetes | 8 | 16.3 | |
| Heart disease | 3 | 6.1 | |
| Anaemia | 5 | 10.2 | |
| Othersa | 8 | 16.3 | |
| Number of past ANC visits | 1–2 | 27 | 13.3 |
| ≥3 | 176 | 86.7 | |
| Mode of delivery | SVD | 178 | 61.8 |
| Vacuum/forceps | 33 | 11.5 | |
| Caesarean section | 77 | 26.7 | |
| Pregnancy status | Intended | 375 | 91.2 |
| Unintended | 36 | 8.8 |
Epilepsy, goitre, tuberculosis.
Women's satisfaction levels with focused ANC services
Pregnant women's levels of satisfaction were measured using 15 tools. Respondents were categorized as satisfied if they scored above the mean value and not satisfied if they scored below the mean value. Accordingly, 192 [46.7% (95% CI: 41.7–51.6)] pregnant women were satisfied with the focused ANC services offered at the public health facilities in the West Shewa Zone (Figure 1).
Figure 1.
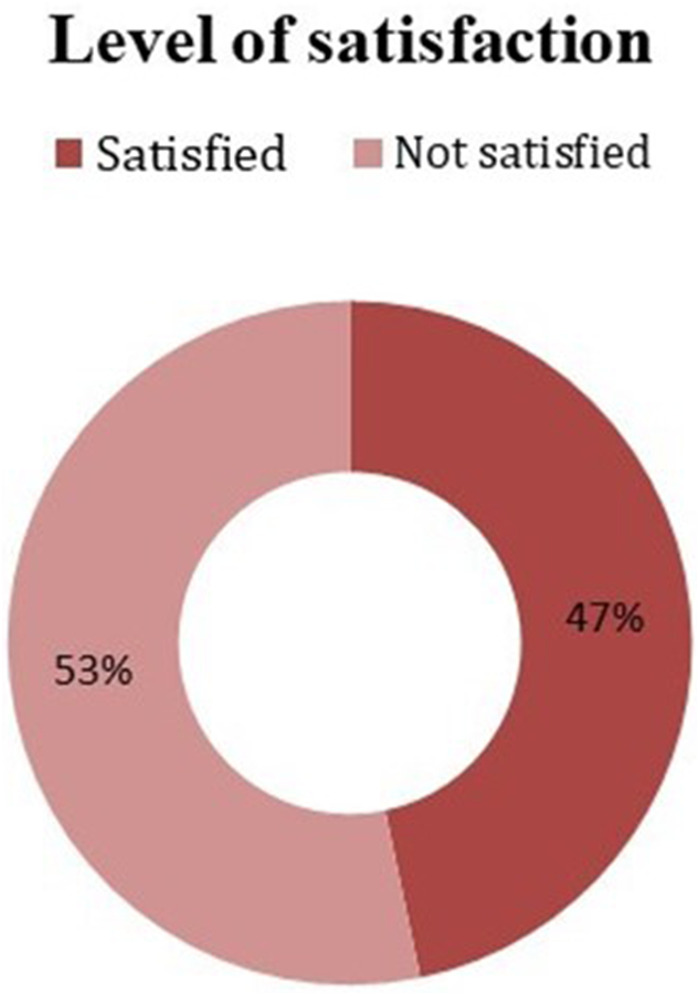
Satisfaction levels of pregnant women with focused ANC service at public health facilities of the West Shewa Zone, Central Ethiopia, 2021.
Pregnant women's satisfaction with different domains of focused ANC services
The participants were highly satisfied with respectful maternal care (359, 87.3%) and supplementation of iron and folic acid (352, 85.6%).
However, 288 (70.1%) participants were dissatisfied with the way in which health professionals explained the rationale behind, and provided an interpretation of, laboratory investigation. About half (50.6%) of the women, 208, were dissatisfied with both auditory and visual privacy during the examination (Table 3).
Table 3.
Level of client satisfaction with different domains of satisfaction in public health facilities of the West Shewa Zone, Central Ethiopia (N = 411).
| Components | Level of satisfaction | P-value | |
|---|---|---|---|
| Satisfied (%) | Not satisfied (%) | ||
| Auditory and visual privacy during examination | 203 (49.4) | 208 (50.6) | 0.001 |
| Iron and folic acid supplementation | 352 (85.6) | 59 (14.4) | 0.0001 |
| Return home without receiving the service | 171 (41.6) | 240 (58.4) | 0.409 |
| Respectful maternity care | 359 (87.3) | 52 (12.7) | 0.0001 |
| Payment for the service received | 360 (87.6) | 51 (12.4) | 0.0001 |
| Willingness to give birth in this facility | 307 (74.7) | 104 (25.3) | 0.0001 |
| Received the needed care | 286 (69.6) | 125 (30.4) | 0.001 |
| Willingness to continue the follow-up (ANC) service | 349 (84.9) | 62 (15.1) | 0.0001 |
| Recommending others to be booked for ANC here | 303 (73.7) | 108 (26.3) | 0.0001 |
| Received counselling on the potential risks of pregnancy | 197 (47.9) | 214 (52.1) | 0.0001 |
| Waiting time to receive the care | 282 (68.6) | 129 (31.4) | 0.0001 |
| Distance from nearby facility | 317 (77.1) | 94 (22.9) | 0.001 |
| Rationale and interpretation of investigation | 123 (29.9) | 288 (70.1) | 0.0001 |
| History taking during ANC visit | 262 (63.7) | 149 (36.3) | 0.249 |
| Health education and information | 246 (59.9) | 165 (40.1) | 0.0001 |
| Overall satisfaction | 46.70% | 53.30% | |
Determinants of maternal satisfaction with focused ANC services
Both bivariate and multivariable binary logistic regression analyses were conducted to identify the determinants of maternal satisfaction with focused ANC services.
Multivariable logistic regression analysis showed that the odds of satisfaction were 5 times higher among pregnant women who availed of ANC service at a hospital compared with those utilizing the service at a health center [AOR = 5.10, (95% CI: 3.33–7.75)]. Urban residents were 2.38 times more likely to be satisfied with ANC service [AOR = 2.38, (95% CI: 1.21–4.70)]. The history of abortion was also a significant predictor of maternal satisfaction. Women with a history of abortion were 19% less likely to be satisfied with ANC service [AOR = 0.19, (95% CI: 0.07–0.49)]. Moreover, the previous mode of delivery was also found to be associated with satisfaction with ANC service. Women whose previous mode of delivery was the caesarean section had lower odds of satisfaction compared with those with spontaneous vaginal delivery [AOR = 0.25, (95% CI: 0.12–0.54)] (Table 4).
Table 4.
Determinants of maternal satisfaction with ANC service among pregnant women receiving ANC at public health facilities in the West Shewa Zone, Central Ethiopia, 2021.
| Variables | Overall satisfaction with ANC | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Satisfied (%) | Dissatisfied (%) | ||||
| Age of participants | |||||
| <20 | 22 (41.5) | 31 (58.5) | 2.56 (0.82–7.92) | 3.49 (0.67–18.2) | 0.138 |
| 21–34 | 165 (49.3) | 170 (50.7) | 3.49 (1.27–9.63) | 3.12 (0.85–11.5) | 0.086 |
| ≥35 | 5 (21.7) | 18 (78.3) | 1 | 1 | |
| Level of health institution | |||||
| Hospital | 137 (65.6) | 72 (34.4) | 5.27 (3.01–9.40) | 5.10 (3.33–7.75) | 0.0001 |
| Health centre | 55 (27.2) | 147 (72.8) | 1 | 1 | |
| Place of residence | |||||
| Rural | 99 (40.1) | 148 (59.9) | 1 | 1 | |
| Urban | 93 (56.7) | 71 (43.3) | 1.96 (1.31–2.92) | 2.38 (1.21–4.70) | 0.013 |
| Average monthly income (in Ethiopian Birr) | |||||
| <1,380 | 27 (40.3) | 40 (59.7) | 1 | 1 | |
| 1,381–6,900 | 90 (40.5) | 132 (59.5) | 1.01 (0.58–1.76) | 0.99 (0.43–2.33) | 0.992 |
| >6901 | 75 (61.5) | 47 (38.5) | 2.36 (1.29–4.35) | 2.69 (0.97–7.42) | 0.057 |
| Mode of delivery of the last pregnancy | |||||
| SVD | 100 (56.2) | 78 (43.8) | 1 | 1 | |
| Vacuum/forceps | 14 (42.4) | 19 (57.6) | 0.58 (0.27–1.22) | 0.64 (0.26–1.57) | 0.327 |
| Caesarean section | 21 (27.3) | 56 (72.7) | 0.29 (0.16–0.52) | 0.30 (0.15–0.60) | 0.001 |
| Antenatal care follow-up during last pregnancy | |||||
| No | 29 (34.1) | 56 (65.9) | 1 | 1 | |
| Yes | 106 (52.2) | 97 (47.8) | 2.11 (1.25–3.57) | 1.86 (0.97–3.54) | 0.060 |
| History of abortion | |||||
| No | 183 (52.1) | 168 (47.9) | 1 | 1 | |
| Yes | 9 (15) | 51 (85) | 0.16 (0.08–0.34) | 0.19 (0.07–0.49) | 0.001 |
| Place of last delivery | |||||
| Home | 11 (25) | 33 (75) | 1 | 1 | |
| Health facility | 124 (50.8) | 120 (49.2) | 3.1 (1.49–6.41) | 2.39 (0.99–5.71) | 0.050 |
Discussion
This study assessed pregnant women's satisfaction with focused ANC services and the associated factors in public health facilities in the West Shewa Zone, central Ethiopia. Accordingly, women's satisfaction with focused ANC services was found to be 46.7% [95% CI: (41.7–51.6)], which was lower than that of most previous studies conducted in different places of Ethiopia, for example, 60.4% in Jimma Town (29), 79.2% in Hawassa city (30), 74% in Hossana (25), 70.3% in the Harari region (23), and 68% in Southwest Ethiopia (31). It was also lower than that of the studies done in Nigeria and Kazakhstan, where 90% of pregnant women were satisfied with ANC services (17, 18).
Nonetheless, the satisfaction level in this study was higher than that in the ones conducted in the Bursa district (33%) and Northwest Ethiopia, 30.3% (20, 32). This discrepancy could be due to differences in the study period, socio-demographic characteristics, and the measurement scale used to determine the satisfaction levels. Moreover, the variation might be due to the difference in the study settings, as some studies included only health centers (21, 30, 32), while this study included both hospitals and health centers.
The odds of maternal satisfaction with ANC service were 5 times higher among pregnant women utilizing the service at hospitals compared with those receiving the service at health centers. Likewise, the study conducted in the Harari region, eastern Ethiopia (23), revealed that the levels of satisfaction were higher among those who received the service within the hospital than those who availed it in health centers. This could be due to the fact that hospitals have more resources, infrastructure, human power, medical equipment, and other facilities compared with health centers (33).
Place of residence was also found to be a significant determinant factor associated with maternal satisfaction with ANC service. Urban residents had 2.38 times higher odds of satisfaction with the service than rural residents. This was supported by previous studies conducted in the Tullo and Chencha districts of Ethiopia (34, 35). This was also supported by the finding of the Ethiopian demographic health survey, which revealed that urban women were more likely (85%) than rural women (70%) to receive ANC service from a skilled provider (3). This could be attributed to the fact that rural dwellers travel a long distance to reach health facilities and are forced to wait for a long time to receive the desired care (36). There could also be discrepancies between urban women and rural residents in terms of communication (37).
Compared with their counterparts who had normal deliveries, pregnant women who previously had an abortion had a 19% lower likelihood of being satisfied with ANC service. The potential explanation for this is that they anticipate receiving high-quality care for their current pregnancy in order to avoid issues that occurred during their previous pregnancy. There is a high likelihood that they would be unhappy with ANC service if they feel that it falls short of their expectations. Finally, this study revealed that women whose previous mode of delivery was caesarean section had 30% lower odds of satisfaction compared with those with spontaneous vaginal delivery. Caesarean birth entails the physiologic stresses of anaesthesia, a major surgical procedure, physical recovery, and postoperative complications. Caesarean birth adds additional stress, including the stress of surgery. Women who experience caesarean delivery have reported feelings of depression, anxiety, guilt, less satisfaction with the birth experience, loss of control, and loss of self-esteem (38). Furthermore, they may expect high-quality care for the early detection of problems in order to avoid harming their fetus and having to undergo a repeat caesarean section.
Strengths and limitations of the study
Social desirability bias might have affected the quality of the collected data. However, interviews were conducted after women received care upon exit by non-staff members to minimize bias. The other possible limitation could be that pregnant women were included irrespective of past obstetric history and gestational age, because of which primigravida mothers and those on their first visit might have faced difficulty judging some domains of satisfaction at first exposure. Moreover, the quantitative nature of the study could be another limitation. Therefore, we recommend that readers consider this limitation while citing and interpreting the findings of this study.
Conclusion
Only approximately 47% percent of the participants felt satisfied with the focused ANC services rendered at public health facilities in Central Ethiopia. The participants were highly satisfied with respectful maternal care and iron and folic acid supplementation. However, they were highly dissatisfied with the way health professionals explained the rationale behind and provided an interpretation of laboratory investigation and privacy during examination. Moreover, factors such as the type of health institution, place of residence, history of abortion, and mode of delivery during last pregnancy were found to be significantly associated with maternal satisfaction with ANC service. Therefore, health facilities and the stakeholders concerned need to take necessary measures to scale up the satisfaction levels of pregnant women as these are also a reflection of standard care. They also ought to focus on infrastructure within the facilities as well as manpower to minimize waiting time and provide high-quality service, including counseling on the potential risks of pregnancy.
Acknowledgments
We would like to express our heartfelt gratitude to Ambo University for funding and support in carrying out this research. We also thank data collectors, supervisors, and study participants for offering their valuable time to this study.
Funding Statement
This study was funded by Ambo University. The funders had no role in the study design, data collection, and analysis, in the decision to publish, or in the preparation of the manuscript.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding author.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval for this study was obtained from the Ambo University College of Medicine and Health Sciences ethical institutional review committee with reference number AURH/M114/2/5/2013. A support letter was obtained from the zonal health office and selected public health facilities. Participants were informed about the objective of the study. Written informed consent was obtained from the participants. In order to keep confidentiality of any information provided by study subjects, the data collection procedure was anonymous. Participation was on a voluntary basis, and they were told they could withdraw from the study at any time during data collection.
Author contributions
GGB drafted the proposal and made a significant contribution to the write-up of the result section. BS and EYR designed the proposal, interpretation of the result and drafted the manuscript. Generally, all authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.World Health; Organization. Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. World Health Organization; (2019). [Google Scholar]
- 2.WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF. UNFPA, World Bank Group and The United Nations Population Division. WHO (2015). [Google Scholar]
- 3.EPHIEE I. Ethiopia mini demographic and health survey 2019: key indicators. USA: EPHI and ICF; (2019). [Google Scholar]
- 4.Ethiopian Public Health Institute (EPHI) FMoHF, World Health Organization (WHO), Addis Ababa E. EthiopiaService Availability and Readiness Assessment 2016 Summary Report. (2016).
- 5.Yamey G, Shretta R, Binka FN. The 2030 sustainable development goal for health. British Medical Journal Publishing Group; (2014). [DOI] [PubMed] [Google Scholar]
- 6.World Health; Organization. Strategies towards ending preventable maternal mortality (EPMM). World Health Organization; (2015). [Google Scholar]
- 7.World Health; Organization. WHO Recommendations on antenatal care for a positive pregnancy experience. World Health Organization; (2016). [PubMed] [Google Scholar]
- 8.World Health; Organization. World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; (2016). [Google Scholar]
- 9.Kebede TT, Godana W, Utaile MM, Sebsibe YB. Effects of antenatal care service utilization on maternal near miss in Gamo Gofa zone, southern Ethiopia: retrospective cohort study. BMC Pregnancy Childbirth. (2021) 21(1):1–9. 10.1186/s12884-020-03485-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohammed AY, Wanamo TE, Wodera AL. Prevalence of antenatal care services satisfaction among mothers attending antenatal care in Goba Hospital, Bale Zone, Oromia Region, Southeast Ethiopia. J Health Sci. (2021) 15(7):1–8. [Google Scholar]
- 11.Adeyinka O, Jukic AM, McGarvey ST, Muasau-Howard BT, Hawley NL. Predictors of prenatal care satisfaction among pregnant women in American Samoa. BMC Pregnancy Childbirth. (2017) 17(1):1–14. 10.1186/s12884-017-1563-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Batbaatar E, Dorjdagva J, Luvsannyam A, Savino MM, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. (2017) 137(2):89–101. 10.1177/1757913916634136 [DOI] [PubMed] [Google Scholar]
- 13.Galle A, Van Parys A-S, Roelens K, Keygnaert I. Expectations and satisfaction with antenatal care among pregnant women with a focus on vulnerable groups: a descriptive study in Ghent. BMC Womens Health. (2015) 15(1):1–12. 10.1186/s12905-015-0266-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hollowell J, Oakley L, Kurinczuk JJ, Brocklehurst P, Gray R. The effectiveness of antenatal care programmes to reduce infant mortality and preterm birth in socially disadvantaged and vulnerable women in high-income countries: a systematic review. BMC Pregnancy Childbirth. (2011) 11(1):1–20. 10.1186/1471-2393-11-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.FMoH. Reproductive, maternal, new born and child health, urban health extension program integrated refresher training. Addis Ababa, Ethiopia: Federal ministry of Health (FMoH) (2017). [Google Scholar]
- 16.Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. (2012) 12(1):1–9. 10.1186/1472-6963-12-352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dauletyarova MA, Semenova YM, Kaylubaeva G, Manabaeva GK, Toktabayeva B, Zhelpakova MS, et al. Are Kazakhstani women satisfied with antenatal care? Implementing the WHO tool to assess the quality of antenatal services. Int J Environ Res Public Health. (2018) 15(2):325. 10.3390/ijerph15020325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Onyeajam DJ, Xirasagar S, Khan MM, Hardin JW, Odutolu O. Antenatal care satisfaction in a developing country: a cross-sectional study from Nigeria. BMC Public Health. (2018) 18(1):1–9. 10.1186/s12889-018-5285-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ismail NIAA, Essa RM. Pregnant women’s satisfaction with the quality of antenatal care at Maternal and Child Health Centers in El-Beheira Governorate. Therapy. (2017) 14:15. [Google Scholar]
- 20.Emiru AA, Alene G, Debelew GT. Women’s satisfaction with the quality of antenatal care services rendered at public health facilities in Northwest Ethiopia: the application of partial proportional odds model. BMJ Open. (2020) 10(9):e037085. 10.1136/bmjopen-2020-037085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fseha B. Assessment of mothers level of satisfaction with antenatal care services provided at alganesh health center Shire, North West Tigray, Ethiopia. Biomed J Sci Tech Res. (2019) 16(1):11798–802. 10.26717/BJSTR.2019.16.002803 [DOI] [Google Scholar]
- 22.Ayalew MM, Nebeb GT, Bizuneh MM, Dagne AH. Women’s satisfaction and its associated factors with antenatal care services at public health facilities: a cross-sectional study. Int J Womens Health. (2021) 13:279. 10.2147/IJWH.S293725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birhanu S, Demena M, Baye Y, Desalew A, Dawud B, Egata G. Pregnant women’s satisfaction with antenatal care services and its associated factors at public health facilities in the Harari region, Eastern Ethiopia. SAGE Open Med. (2020) 8:2050312120973480. 10.1177/2050312120973480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gelaw KA, Gebeyehu NA. Maternal satisfaction and associated factors among pregnant women attended at antenatal care service in Bedessa Health Center, Wolaita zone, Ethiopia, 2018. J Sci Res. (2020) 8(2):39. 10.11648/j.sr.20200802.12 [DOI] [Google Scholar]
- 25.Kebede DB, Belachew YB, Selbana DW, Gizaw AB. Maternal satisfaction with antenatal care and associated factors among pregnant women in Hossana town. Int J Reprod Med. (2020) 2020:1–8. 10.1155/2020/2156347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tadesse E. Antenatal care service utilization of pregnant women attending antenatal care in public hospitals during the COVID-19 pandemic period. Int J Womens Health. (2020) 12:1181. 10.2147/IJWH.S287534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banke-Thomas A, Semaan A, Amongin D, Babah O, Dioubate N, Kikula A, et al. A mixed-methods study of maternal health care utilisation in six referral hospitals in four sub-Saharan African countries before and during the COVID-19 pandemic. BMJ Glob Health. (2022) 7(2):e008064. 10.1136/bmjgh-2021-008064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebreegziabher SB, Marrye SS, Kumssa TH, Merga KH, Feleke AK, Dare DJ, et al. Assessment of maternal and child health care services performance in the context of COVID-19 pandemic in Addis Ababa, Ethiopia: evidence from routine service data. Reprod Health. (2022) 19(1):1–11. 10.1186/s12978-022-01353-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chemir F, Alemseged F, Workneh D. Satisfaction with focused antenatal care service and associated factors among pregnant women attending focused antenatal care at health centers in Jimma town, Jimma zone, South West Ethiopia; a facility based cross-sectional study triangulated with qualitative study. BMC Res Notes. (2014) 7(1):1–8. 10.1186/1756-0500-7-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lire T, Megerssa B, Asefa Y, Hirigo AT. Antenatal care service satisfaction and its associated factors among pregnant women in public health centres in Hawassa city, Southern Ethiopia. Proc Singapore Healthc. (2021) 31:1–8. 20101058211007881 [Google Scholar]
- 31.Lakew S, Ankala A, Jemal F. Determinants of client satisfaction to skilled antenatal care services at Southwest of Ethiopia: a cross-sectional facility based survey. BMC Pregnancy Childbirth. (2018) 18(1):1–13. 10.1186/s12884-018-2121-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tesfaye T, Mekonnen H, Negesa L. Maternal antenatal care service satisfaction and factors associated with rural health centers, Bursa district, Sidama zone, Southern Ethiopia: a cross-sectional study. J Womens Health Care. (2017) 6(363):4–20. 10.4172/21670420.1000363 [DOI] [Google Scholar]
- 33.Arsenault C, Yakob B, Tilahun T, Nigatu TG, Dinsa G, Woldie M, et al. Patient volume and quality of primary care in Ethiopia: findings from the routine health information system and the 2014 service provision assessment survey. BMC Health Serv Res. (2021) 21(1):1–10. 10.1186/s12913-021-06524-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jima GH, Tejineh S. Women’s satisfaction with antenatal care service and associated factors in Tullo district, Eastern Ethiopia. J Womens Health Care. (2021) 10(5):1–6. [Google Scholar]
- 35.Abebe S, Alemayehu A, Gebremariam A, Dirar A. Quality of antenatal care service in public health facilities of Chencha district, Gamo Gofa zone, Southern Ethiopia. MOJ Womens Health. (2017) 4(3):00086. [Google Scholar]
- 36.Okwaraji YB, Webb EL, Edmond KM. Barriers in physical access to maternal health services in rural Ethiopia. BMC Health Serv Res. (2015) 15(1):1–8. 10.1186/s12913-015-1161-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen X, Orom H, Hay JL, Waters EA, Schofield E, Li Y, et al. Differences in rural and urban health information access and use. J Rural Health. (2019) 35(3):405–17. 10.1111/jrh.12335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Miovech SM, Knapp H, Borucki L, Roncoli M, Arnold L, Brooten D. Major concerns of women after cesarean delivery. J Obstet Gynecol Neonatal Nurs. (1994) 23(1):53–9. 10.1111/j.1552-6909.1994.tb01850.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding author.


