Abstract
Introduction:The COVID-19 pandemic has rapidly spread to many countries and has led various primary healthcare services of chronic diseases to be neglected and only partially be replaced by telemedicine services. This study aims to investigate the role of telemedicine in the management of patients with noncommunicable diseases in primary health care during the COVID-19 pandemic.
Method: A narrative review of the literature was carried out through searching the PubMed and Google Scholar databases.
Results: From the initial stages of the pandemic, several scientific medical societies issued guidelines which urged citizens and health personnel to adopt digital means in the provision of regular chronic care as much as possible. The significant benefits of the telemedicine sessions partially only filled the gap of the deferred chronic care. On the other hand, many barriers need to be addressed in order to achieve an equitable and high-quality implementation of telemedicine services.
Conclusion:The widespread application of telemedicine and self-monitoring was brought about by the COVID-19 pandemic and currently, they have become common ways of managing non-communicable diseases in primary health care. Innovations introduced need to be maintained and integrated into conventional traditional practices, so that health systems are more resilient to future public health emergencies.
Keywords:SARS-CoV-2, primary health care, non-communicable diseases, chronic conditions, telehealth, self-monitoring.
INTRODUCTION
The outbreak of the SARS-CoV-2, which started in the Chinese city of Wuhan, has rapidly spread to many countries, infecting millions of people worldwide. In March 2020, the World Health Organization (WHO) declared the COVID-19 infection a pandemic (1). This unprecedented health crisis has caused radical changes and adjustments in the healthcare provision in most countries of the world (2, 3), raising concerns for the efficient and sustainable management of patients with chronic diseases which remain the most common cause of morbidity and mortality worldwide (4, 5).
Due to the high transmissibility of the virus, governments around the world took unprecedented restrictive measures, including social distancing, local and national lockdowns, quarantine and home isolation, radically changing people's daily lives and habits. In addition, from the very first stages of the pandemic, it was seen that health structures and especially hospitals are transmission hotspots of the virus, resulting in the readjustment of healthcare provision with an emphasis on minimizing the contacts of patients with health personnel to those absolutely necessary (3). The previous ones combined with the fear and reluctance of citizens to come to health facilities due to the increased possibility of exposure and therefore infection (3, 6, 7) as well as the ever-increasing shortages in available medical and nursing staff led various primary health care (PHC) services of prevention, treatment and rehabilitation of non-communicable diseases (NCDs) to be neglected and only partially be replaced by telemedicine services (8-10).
The aim of this narrative review was to outline the main adjustments adopted by health systems around the world in order to ensure the continuity of chronic care services in PHC, with particular emphasis being placed on investigating the role of telemedicine in the management of patients with NCDs in primary care during the COVID-19 pandemic.
METHODS
A narrative literature review of the current bibliography was conducted, in order to fill the gap in the international literature and to achieve a detailed and comprehensive composition of the quite heterogeneous data of around the world. The PubMed and Google Scholar databases were searched up to August 2022, using Boolean operators (AND, OR and NOT) with appropriate combinations of the following search terms: ‘chronic diseases’, ‘non communicable diseases’, ‘primary care’, ‘outpatient care’, ‘general practice’, ‘telemedicine’, ‘SARS-CoV-2’, ‘COVID-19’, and ‘pandemic’. Also, for the adequacy of the data, references of articles selected for further analysis in the specific review were screened for relevant sources. Exclusion criteria from this study were articles in a language other than English and Greek, as well as studies from the gray literature.
Out of a large volume of published articles, the duplicate records were initially deleted and a quick assessment of their relevance to the research questions of this study was carried out from the title, abstract and index terms. The articles that have been positively evaluated were then read in their entirety and a short critical appraisal followed. The studies that were relevant to the topic were finally included in the present narrative review. An analysis of concepts and thematic frameworks was then performed; the relevant data of the literature were grouped and the sections of the final text of the narrative review were formulated.
RESULTS
The role of telemedicine during the pandemic
Telemedicine can be defined as the use of twoway information by leveraging telecommunication technologies to provide clinical care through a variety of remote methods (11). Although telemedicine has been used in PHC for many years, its widespread application was brought about by the COVID-19 pandemic, and in the early stages of the health crisis it may have become the primary way of chronic, non-emergency care provision in most countries of the world (12, 13).
Indeed, from the initial stages of the COVID-19 pandemic, the Center for Disease Control and Prevention (CDC) and several scientific medical societies issued guidelines which, in addition to the observance of health protocols and social distancing measures, urged citizens and health personnel to adopt as much as possible digital means in the provision of regular chronic care and to take advantage of the possibilities offered by telemedicine (11, 14).
Telemedicine facilitates the remote contact of patients with the health team and has been shown to effectively assist in the management of NCDs, since it leads to an improvement in the quality of life and a reduction in hospitalizations and mortality (15-17). A multitude of daily medical practices of chronic care, including diagnosis and treatment services, rehabilitation services, follow-ups, electronic drug prescriptions, interpretation of laboratory and imaging tests, psychological support sessions, information and aware Telemedicine facilitates the remote contact of patients with the health team and has been shown to effectively assist in the management of NCDs, since it leads to an improvement in the quality of life and a reduction in hospitalizations and mortality (15-17). A multitude of daily medical practices of chronic care, including diagnosis and treatment services, rehabilitation services, follow-ups, electronic drug prescriptions, interpretation of laboratory and imaging tests, psychological support sessions, information and aware
Since the onset of the pandemic, there has been a fundamental shift in the balance in the provision of chronic care worldwide, and many regular PHC medical visits have been delayed, postponed, rescheduled or even cancelled (9). A large survey, which was carried out among health professionals from 47 countries on five continents, during the first wave of the pandemic, showed a large reduction of many scheduled appointments, as only 14% of them continued in person, while the majority of visits (reaching 85%) turned into remote sessions using new technologies mainly by phone and, to a lesser extent, by video (e. g., skype, zoom, facebook) (22).
In Belgium and Brazil, PHC professionals frequently used teleconsultation services during the containment measures, mainly through a rapid remote assessment of patients' health status, to fill the gap of chronic care disruption and ensure close and timely monitoring of people with NCDs (23–25). In the UK and China, following official guidance from the relevant authorities, many cardiology clinics suspended traditional in person visits and offered remote chronic care services where possible, managing to keep vulnerable patients out of hospitals (3, 18). Similar examples have been adopted by most countries of the world in an attempt to ensure the continuity of chronic care, to maintain the multidisciplinary nature of the health team and, at the same time, to observe social distancing measures and reduce the possibility of transmission of the virus and thus, the spread of the pandemic (22, 26).
Triage is the process of prioritizing patient care based on the severity of their condition or the likelihood of recovery with and without care (27). A pre-screening system, which screens and assesses vulnerable people with NCDs in the community before they enter the primary care system, emerges as a priority both to ensure the control of pandemic waves and to decongest PHC structures, and to assess the degree of vulnerability and deregulation of patients health status and the risk of adverse consequences from the neglect of their chronic care (21, 28-30).
At McGill University's Center of Excellence for Longevity in Canada, in order to determine the medical, psychological, and functional capabilities of older adults without exposure to overcrowding, an interesting telemedicine application was constructed and implemented with specific design for older adults with multimorbidities and mobility problems. Depending on the responses to the digital screening questionnaire, risk stratification was performed and PHC professionals judged whether there was a need for a telesession (by phone or video) or a in person medical visit and further referral, with ultimate goal to ensure continuous, integrated, patient-centered and multidisciplinary chronic care (28).
In Singapore, primary care and ambulatory care facilities adopted and implemented the phone triage system to clarify the urgency of the medical visit for each patient, so each scheduled appointment had three possible outcomes: postponement and rescheduling, teleconference instead of inperson visit, or finally conventional close medical visit, when the patient's health condition was considered serious (21, 29). Furthermore, in order to ensure the continuity of care and prevent negative health consequences, PHC practitioners in Belgium attempted risk stratification among their population of responsibility and approached the most vulnerable populations (elderly, people with limited mobility, etc). In case the visit was deemed necessary and face-to-face communication was not feasible for either safety reasons or time and constraints, then the health team tried to ensure continuity of care with home visits or, more often, with remote teleconferences (24).
According to the CDC, during the first quarter of 2020, the number of televisits in the US increased by 50%, compared to the same time interval in 2019, and it is worth noting that most of the encounters came from patients seeking care for diseases other than of COVID-19 (11). In fact, 69% of patients who used telemedicine methods during the early pandemic period in 2020 were treated at home, 26% of them were followed by a primary care provider, and just 3% were referred to an urgent care setting when their health condition worsened or not improved (11). This increase in telemedicine use is estimated to have offset about two-thirds of the decline in overall visit volume during the COVID-19 pandemic in America (31).
A similar increase in the use of telemedicine and in general new technologies in health services was also observed in a large survey conducted by the Health Foundation in UK, which included more than 4 000 patients and 1 000 healthcare professionals (32). Despite the simultaneous increase in remote sessions, the significant decrease in total visits, showed the broad scope of deferred care during the first months of the COVID-19 pandemic (33). Although some deferred care represented ambulatory care that could be postponed without immediate risk, these results also substantiated concerns that patients may delay managing chronic diseases or experience complications from deferred acute medical issues (31, 34).
The use of telematic chronic care services during the COVID-19 pandemic appears to be widely accepted by both primary care staff and patients with NCDs, who have shown an admirable adaptability in many cases (35, 36). Of course, it is worth mentioning that medical visits via teleconferences turned out to be less necessary or desirable than previously thought, with telephone calls being equally or more acceptable in most cases (37). Furthermore, while video counseling has advantages due to visual contact, it can also significantly increase the workload of PHC health professionals compared to telephone counseling (38). However, telephone sessions have been shown to be more effective for patients with higher health literacy who are able to express their condition over the telephone, and health professionals should take this into account (17).
The adaptability of health professionals in many countries (e. g., the UK and Belgium) to the rapid changes and contemporary challenges regarding the use of telemedicine in chronic patients, posed and continues to pose by the pandemic (3, 24, 32, 33) is extraordinary. In England, both patients and healthcare professionals who used telematic medical services overwhelmingly expressed positive impressions. Nevertheless, negative experiences were also reported mainly by people aged over 55 years, the elderly, unemployed and uninsured and, in general, by vulnerable populations and especially in the poorest countries of Asia and Africa (32, 39, 40).
In addition, in a survey among high-risk patients on the use of new monitoring methods during the pandemic, it appeared that patients were rather willing to adopt the new technologies for medical visits. More specifically, 82% of patients were satisfied with the asynchronous consultation, while regarding the synchronous consultation, 89% were satisfied with the follow-up via telephone and 63% via video (14). In fact, even in non-health crisis settings, patients stated that they would be satisfied with the possibility of using a more modern care delivery model that would include health feedback (e.g., laboratory results) through both synchronous and asynchronous means (14, 35).
Benefits, barriers and conditions of successful implementation of telemedicine services in PHC during the COVID-19 pandemic
Telemedicine has multiple benefits for public and individual health during the COVID-19 pandemic (11). Perhaps the most important advantage of telemedicine during an outbreak of a communicable infection is the prophylaxis it can offer to both chronic patients (a vulnerable population at high risk of serious illness) and health personnel by avoiding overcrowding and ensuring reduced possibility of exposure and infection (4, 11, 28, 32). In addition, its contribution to the saving of precious resources due to the limited use of personal protective equipment (FFP2/FFP3 masks, protective suits, caps, boots) was decisive (11), as significant shortages were observed from the very first stages of the pandemic (41, 42). The fact that it can be carried out by health personnel quarantined remotely, leaving space and time for frontline doctors and nurses to deal not only with suspected and confirmed cases of COVID-19, but also with the other aspects of chronic care, which cannot be converted into remote sessions, also indicates the essential contribution of telemedicine to the saving of human resources (43).
The increased availability of remote health services make telemedicine necessary to ensure the uninterrupted and continuous provision of chronic care especially in a period characterized by limited and deferred care (4, 18, 22, 24). Increased access to telemedicine services from the comfort of patients' homes, especially for people who care for children or the elderly, or who live far from a PHC facility (rural and island areas), or who wish to consult a doctor in a remote location is one of the most important advantages (12). After all, the ability to provide care to patients with NCDs from a distance significantly expands the geographic footprint of a health care system (12), overcoming any economic and social barriers regarding the access to PHC services (44). Also, access to teletherapy services may be particularly valuable for those patients who were reluctant to seek in-person care or experienced mobility difficulties (11, 45). Finally, even before the pandemic, patients expressed great satisfaction with televisits (35, 46), perhaps for the reason that they enjoy the time and money saving benefits offered by telemedicine meetings. Besides, the waiting time and cost travel are significantly reduced compared to conventional visits (17, 21, 44, 47). In any case, the increased use of information and communication technologies in the field of health care is accompanied by an indirect benefit for societies, regarding digital reconstruction, increased ease of use and a smoother integration of digital media in everyday life (32).
On the other hand, while telemedicine enables remote medical care during the pandemic, there are many challenges that need to be addressed (12). Although televisits reduce the direct exposure of patients with chronic problems to SARS-CoV-2, they cannot fully restore in-person medical visits, because it is much more difficult to properly assess the condition of patients without life and close communication (11, 12, 24). Indeed, telemedicine undermines the importance and role of the clinical examination and its findings, which can not only lead to specific diagnoses in time, but also help to develop and establish a healthy doctor-patient relationship based on mutual trust (45, 48, 49). It is not, after all, a coincidence that teleconsultations in primary care have often been limited to those with an well-established doctor-patient relationship, with the argument that an established therapeutic relationship contributes to better continuity of care and leads to better clinical outcomes in long terms (17).
For example, there are several practical difficulties in continuous and holistic monitoring of most chronic diseases such as diabetes and hypertension from a distance, without clinical examination, without laboratory control or by bypassing useful diagnostic and therapeutic interventions, with possible negative impact on effective diseases management (12, 50). Perhaps this was the main reason why about 40% of patients and 33% of health workers who took part in a large survey in the UK said that new digital approaches, although useful in a period of pandemic, remain inferior than traditional models of care and should be applied sparingly in the future(32).
One of the major problems in the use of telemedicine in chronic care is the limited access of certain population groups to the opportunities of new technologies. Indeed, people from low socioeconomic groups, the elderly, persons with dementia, refugees and immigrants and socially vulnerable populations in general – who, on the one hand, are disproportionately affected by entrenched health inequalities, and on the other hand are plagued by a multitude of NCDs (and, as a result, they have an increased need to use chronic care services) – usually face difficulties in safely accessing good quality and high speed internet and in the proper use of modern digital media and applications (smartphones, tablets, laptops, desktops) (11, 12, 22, 32, 33, 39, 48, 51, 52). In fact, several vulnerable populations often use public structures providing free Internet access (libraries, public places with WiFi) for their connectivity to telemedicine services, which not only lead to overcrowding and violation of social distancing measures, but also abolish the concepts of privacy and anonymity by jeopardizing the successful completion of a digital medical visit (53) and intensifying the synergistic effects of the pandemic on these vulnerable population groups (9, 52, 54, 55).
Relevant problems of technological equipment and internet access can be a barrier on the application of telemedicine in rural, island areas or poor developing countries (9, 51). In addition, problems concerning the linguistic communication of minority groups (23) and the reluctance of some patients to use new technologies have been identified, possibly due to a more general resistance to changes and a difficulty in adapting to the new conditions of chronic care provision established by the unprecedented healthcare crisis (48, 51).
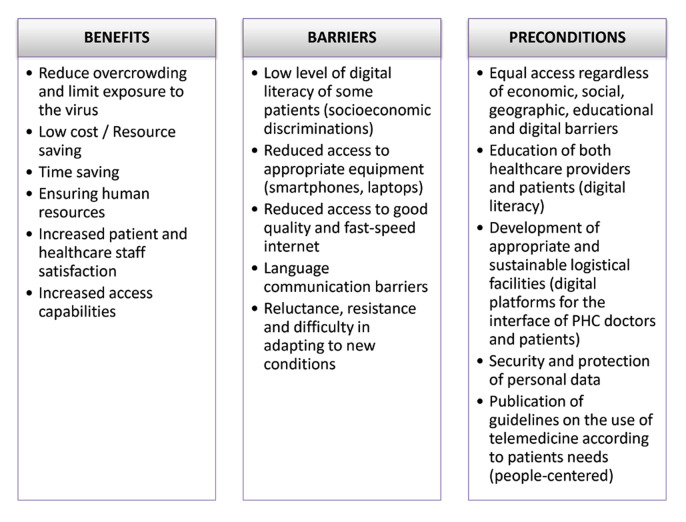
The digital divide is not an argument against the use of digital health, but a strong argument for ensuring optimal access to low-cost, high-quality digital health services. It must be realized that the implementation of telemedicine is more than just the development of new technologies or devices, but it requires systems-level thinking and a coherent national and international strategy that includes effective legislation, regulation and oversight as well as issuing appropriate guidelines (as recently published by the European Society of Hypertension on the use of telemedicine in the management of hypertension during and after the pandemic (56), to ensure the quality, security and interoperability of digital health services (57). It is critical patients and institutions within the community to be engaged in discussions with healthcare networks in an effort to address patient concerns and potential mistrust on telemedicine (58). Figure 1 summarizes the benefits, barriers, and preconditions for successful implementation of telemedicine services in chronic care during the pandemic.
Other adaptations of health systems
In order to limit the frequent visits of chronic patients to health structures and with a focus on the safety of both patients and health personnel, an intensive and targeted effort was carried out to use and issue intangible electronic prescriptions for drugs repeated for long periods of time (three and six months), during the strict restrictive measures (19, 20, 24, 59). Similar strategies and policies to facilitate chronic care have been followed by many countries around the world (Greece, Brazil, India), where the distribution of drugs and medical supplies to chronic patients (especially in socioeconomically vulnerable groups and in elderly patients or in people with disabilities and reduced mobility) applied by non-governmental organizations, volunteers (e. g. medical students) and other social services, in order to achieve a restriction of movements to and from pharmacies and of crowding in waiting lines (9, 19, 21, 25, 60-62).
Another practice that gained significant ground during the COVID-19 pandemic in the management of NCDs in PHC was self-monitoring, allowing patients to remain at home while transmitting health data and receiving follow-up services (21, 63). A large study among Hypertension Centers of Excellence in Europe during the first wave of the pandemic showed that over 60% of hypertensive patients systematically used the technique of self-monitoring and routine blood pressure (BP) measurement at home (26). Indeed, it has been shown that close monitoring and regular measurement of BP and other modifiable risk factors (smoking, diet, exercise) by patients at home with the help of digital applications, provided that they have first acquired the appropriate equipment and have been trained in its correct use, in combination with parallel remote counseling by members of the interdisciplinary health team of the PHC can lead to the correct regulation of NCDs, the early diagnosis of complications and an increase of adherence to drug therapy (21, 44, 56, 64).
Similar practices have been adopted for other chronic diseases such as continuous monitoring of blood glucose levels for patients with diabetes (21, 30, 40, 65), and empowering patients with heart failure (HF) to regularly monitor their body weight for early detection of potential deregulation and regular measurement and recording of blood pressure at home to avoid further complications (3). The education of patients with HF also included familiarizing them with appropriately designed scales for evaluating their clinical situation, with the ultimate goal of empowering patients in collaboration with the PHC team to make decisions regarding the escalation and de-escalation of diuretic therapy (3). A recent meta-analysis found that combined telemonitoring and counseling for HF patients was associated with a reduced risk of cardiovascular mortality and morbidity in short terms. Future research in the field is needed to evaluate the effectiveness of these telemedicine interventions over time (66). Ultimately, health literacy (having the necessary information, skills and judgment to manage health issues) and patient mobilization appear to be two key conditions for self-management of chronic diseases to be more effective (9).
Conflict of interests: none declared.
Financial support: none declared.
Ethical approval and informed consent: Ethical approval and informed consent were not required for this study.
FIGURE 1.
Benefits, barriers and preconditions of successful implementation of telemedicine services in primary health care during the COVID-19 pandemic
Contributor Information
Panagiotis STACHTEAS, Laboratory of Primary Health Care, General Practice and Health Services Research, Faculty of Medicine, Aristotle University of Thessaloniki, Greece.
Charalampos STACHTEAS, Laboratory of Primary Health Care, General Practice and Health Services Research, Faculty of Medicine, Aristotle University of Thessaloniki, Greece.
Emmanouil K. SYMVOULAKIS, Laboratory of Primary Health Care, General Practice and Health Services Research, Faculty of Medicine, Aristotle University of Thessaloniki, Greece
Emmanouil SMYRNAKIS, Laboratory of Primary Health Care, General Practice and Health Services Research, Faculty of Medicine, Aristotle University of Thessaloniki, Greece.
References
- 1.Anderson RM, Heesterbeek H, Klinkenberg D, et al. World Health Organisation Director-General’s opening remarks at the media briefing on COVID19 [Internet] Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Anderson RM, Heesterbeek H, Klinkenberg D, et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fersia O, Bryant S, Nicholson R, et al. The impact of the COVID-19 pandemic on cardiology services. Open Hear. 2020;7:1–6. doi: 10.1136/openhrt-2020-001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mauro V, Lorenzo M, Paolo C, et al. Treat all COVID 19-positive patients, but do not forget those negative with chronic diseases. Intern Emerg Med. 2020;15:787–790. doi: 10.1007/s11739-020-02395-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmot M, Bell R. Social determinants and non-communicable diseases: Time for integrated action. BMJ. 2019;364:1–2. doi: 10.1136/bmj.l251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinstein E, Ragazzoni L, Burkle F, et al. Delayed Primary and Specialty Care: The Coronavirus Disease-2019 Pandemic Second Wave. Disaster Med Public Health Prep. 2020;14:e19–e21. doi: 10.1017/dmp.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szymanski FM, Smuniewski C, Platek AE. Will the COVID-19 Pandemic Change National Security and Healthcare in the Spectrum of Cardiovascular Disease? Curr Probl Cardiol. 2020;45:1–9. doi: 10.1016/j.cpcardiol.2020.100645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smyrnakis E, Symintiridou D, Andreou M, et al. Primary care professionals’ experiences during the first wave of the COVID-19 pandemic in Greece: a qualitative study. BMC Fam Pract. 2021;22:174. doi: 10.1186/s12875-021-01522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yadav UN, Rayamajhee B, Mistry SK, et al. A Syndemic Perspective on the Management of Non-communicable Diseases Amid the COVID-19 Pandemic in Low- and Middle-Income Countries. Front Public Health. 2020;8:508. doi: 10.3389/fpubh.2020.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koonin LM, Hoots B, Tsang CA, et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1595–1599. doi: 10.15585/mmwr.mm6943a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kronenfeld JP, Penedo FJ. Novel Coronavirus (COVID-19): telemedicine and remote care delivery in a time of medical crisis, implementation, and challenges. Transl Behav Med. 2021;11:659–663. doi: 10.1093/tbm/ibaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Britton E, Richardson P, Mian I, et al. Letter: Covid-19—re-initiating clinical services for chronic gastrointestinal diseases. How and when? Aliment Pharmacol Ther. 2020;52:1414–1415. doi: 10.1111/apt.16061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steventon A, Bardsley M, Billings J, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ. 2012;344:e3874–e3874. doi: 10.1136/bmj.e3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg LR, Piette JD, Walsh MN, et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the Weight Monitoring in Heart Failure (WHARF) trial. Am Heart J. 2003;146:705–712. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 17.Carrillo de Albornoz S, Sia K-L, Harris A. The effectiveness of teleconsultations in primary care: systematic review. Fam Pract. 2022;39:168–182. doi: 10.1093/fampra/cmab077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng X, Ma C, Han Y. Changes in the work mode of cardiologists during the COVID-19 epidemic in Wuhan. Eur Heart J. 2020;41:2729–2730. doi: 10.1093/eurheartj/ehaa424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basu S. Non-communicable disease management in vulnerable patients during Covid-19. Indian J Med Ethics. [DOI] [PubMed]
- 20.Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395:1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong W-Z, Chan G-C, Chua H-R. Continuing Chronic Disease Care During COVID-19 and Beyond. J Am Med Dir Assoc. 2020;21:991–992. doi: 10.1016/j.jamda.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab Syndr Clin Res Rev. 2020;14:965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verhoeven V, Tsakitzidis G, Philips H, et al. Impact of the COVID-19 pandemic on the core functions of primary care: Will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10:e039674. doi: 10.1136/bmjopen-2020-039674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Danhieux K, Buffel V, Pairon A, et al. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21:1–6. doi: 10.1186/s12875-020-01326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barone Mark Thomaz Ugliara Harnik SB, de Luca PV, de Souza L, et al. The impact of COVID-19 on people with diabetes in Brazil. Diabetes Res Clin Pract. 2020;166:108304. doi: 10.1016/j.diabres.2020.108304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tam HL, Chung SF, Lou CK. A review of triage accuracy and future direction. BMC Emerg Med. 2018;18:58. doi: 10.1186/s12873-018-0215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beauchet O, Cooper-Brown L, Ivensky V, et al. Telemedicine for housebound older persons during the Covid-19 pandemic. Maturitas. 2020;142:8–10. doi: 10.1016/j.maturitas.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sek KSY, Tan ATH, Yip AWJ, et al. Singapore’s experience in ensuring continuity of outpatient care during the COVID‐19 pandemic. Int J Clin Pract. 2020;74:e13573. doi: 10.1111/ijcp.13573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wake DJ, Gibb FW, Kar P, et al. Endocrinology in the time of covid-19: Remodelling diabetes services and emerging innovation. Eur J Endocrinol. 2020;183:G67–77. doi: 10.1530/EJE-20-0377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel SY, Mehrotra A, Huskamp HA, et al. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern Med. 2021;181:388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joy M, McGagh D, Jones N, et al. Reorganisation of primary care for older adults during COVID-19: a cross-sectional database study in the UK. Br J Gen Pract. 2020;70:e540–e547. doi: 10.3399/bjgp20X710933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stachteas P, Symvoulakis M, Tsapas A, et al. The impact of the COVID-19 pandemic on the management of patients with chronic diseases in Primary Health Care. Popul Med. 2022;4:1–13. [Google Scholar]
- 35.Vosburg RW, Robinson KA. Telemedicine in Primary Care During the COVID-19 Pandemic: Provider and Patient Satisfaction Examined. Telemed e-Health. 2022;28:167–175. doi: 10.1089/tmj.2021.0174. [DOI] [PubMed] [Google Scholar]
- 36.Pagliari C. Digital health and primary care: Past, pandemic and prospects. J Glob Health. 2021;11:01005. doi: 10.7189/jogh.11.01005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murphy M, Scott LJ, Salisbury C, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. 2021;71:e166–e177. doi: 10.3399/BJGP.2020.0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salisbury C, Murphy M, Duncan P. The Impact of Digital-First Consultations on Workload in General Practice: Modeling Study. J Med Internet Res. 2020;22:e18203. doi: 10.2196/18203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tuijt R, Rait G, Frost R, et al. Remote primary care consultations for people living with dementia during the COVID-19 pandemic: experiences of people living with dementia and their carers. Br J Gen Pract. 2021;71:e574–e582. doi: 10.3399/BJGP.2020.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anjana RM, Pradeepa R, Deepa M, et al. Acceptability and Utilization of Newer Technologies and Effects on Glycemic Control in Type 2 Diabetes: Lessons Learned from Lockdown. Diabetes Technol Ther. 2020;22:527–534. doi: 10.1089/dia.2020.0240. [DOI] [PubMed] [Google Scholar]
- 41.Boškoski I, Gallo C, Wallace MB, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointest Endosc. 2020;92:519–523. doi: 10.1016/j.gie.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jessop ZM, Dobbs TD, Ali SR, et al. Personal protective equipment for surgeons during COVID-19 pandemic: systematic review of availability, usage and rationing. Br J Surg. 2020;107:1262–1280. doi: 10.1002/bjs.11750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harky A, Chiu CM, Yau THL, et al. Cancer Patient Care during COVID-19. Cancer Cell. 2020;37:749–750. doi: 10.1016/j.ccell.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mirsky J, Horn D. Chronic Disease Management in the COVID-19 Era. Am J Manag Care. 2020;26:329–330. doi: 10.37765/ajmc.2020.43838. [DOI] [PubMed] [Google Scholar]
- 45.Breton M, Sullivan EE, Deville-Stoetzel N, et al. Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Fam Pract. 2021;22:192. doi: 10.1186/s12875-021-01543-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sirintrapun SJ, Lopez AM. Telemedicine in Cancer Care. Am Soc Clin Oncol Educ B. 2018;38:540–545. doi: 10.1200/EDBK_200141. [DOI] [PubMed] [Google Scholar]
- 47.Jalalabadi F, Shultz K, Sussman N, et al. Initiating Telehealth in a Complex Organization. Semin Plast Surg. 2018;32:159–161. doi: 10.1055/s-0038-1672132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levene L, Seidu S, Greenhalgh T, et al. Pandemic threatens primary care for long term conditions. BMJ. 2020;371:m3793. doi: 10.1136/bmj.m3793. [DOI] [PubMed] [Google Scholar]
- 49.Gomez T, Anaya YB, Shih KJ, et al. A Qualitative Study of Primary Care Physicians’ Experiences With Telemedicine During COVID-19. J Am Board Fam Med. [DOI] [PubMed]
- 50.Ye S, Anstey DE, Grauer A, et al. The Impact of Telemedicine Visits on the Controlling High Blood Pressure Quality Measure During the COVID-19 Pandemic: Retrospective Cohort Study. JMIR Form Res. 2022;6:e32403. doi: 10.2196/32403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elbeddini A, Tayefehchamani Y. Amid COVID-19 pandemic: Challenges with access to care for COPD patients. Res Soc Adm Pharm. 2021;17:1934–1937. doi: 10.1016/j.sapharm.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anderson KE, McGinty EE, Presskreischer R, et al. Reports of Forgone Medical Care Among US Adults During the Initial Phase of the COVID-19 Pandemic. JAMA Netw Open. 2021;4:e2034882. doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zach L, Dalrymple PW, Rogers ML, et al. Assessing Internet access and use in a medically underserved population: implications for providing enhanced health information services. Heal Inf Libr J. 2012;29:61–71. doi: 10.1111/j.1471-1842.2011.00971.x. [DOI] [PubMed] [Google Scholar]
- 54.Stachteas P, Stachteas F. Η πανδημία Covid-19 ως παράγοντας επιδείνωσης των ανισοτήτων υγείας. Επιθεώρηση Κοινωνικών Ερευνών. 2020;154:129–148. [Google Scholar]
- 55.Chan EYY, Kim JH, Lo ESK, et al. What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies. Int J Environ Res Public Health. 2020;17:5588. doi: 10.3390/ijerph17155588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khan NA, Stergiou GS, Omboni S, et al. Virtual management of hypertension: lessons from the COVID-19 pandemic–International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40:1435–1448. doi: 10.1097/HJH.0000000000003205. [DOI] [PubMed] [Google Scholar]
- 58.Kronenfeld JP, Penedo FJ. Novel Coronavirus (COVID-19): telemedicine and remote care delivery in a time of medical crisis, implementation, and challenges. Transl Behav Med. 2021;11:659–663. doi: 10.1093/tbm/ibaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bell JS, Reynolds L, Freeman C, et al. Strategies to promote access to medications during the COVID-19 pandemic. Aust J Gen Pract. 2020;49:530–532. doi: 10.31128/AJGP-04-20-5390. [DOI] [PubMed] [Google Scholar]
- 60.Stachteas P, Vlachopoulos N, Smyrnakis E. Medical students during the COVID-19 pandemic: Considerations and arguments on their clinical engagement. J Adv Med Educ Prof. 2021;9:238–242. doi: 10.30476/JAMP.2021.89092.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stachteas P, Vlachopoulos N, Smyrnakis E. Deploying Medical Students During the COVID-19 Pandemic. Med Sci Educ. 2021;31:2049–2053. doi: 10.1007/s40670-021-01393-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vlachopoulos N, Smyrnakis E, Stachteas P, et al. Medical Students during COVID-19 Pandemic: Lessons Learned from Response Teams in Greece. Int J Med Students. 2020;8:191–193. [Google Scholar]
- 63.Muller AE, Berg RC, Jardim PSJ, et al. Can Remote Patient Monitoring Be the New Standard in Primary Care of Chronic Diseases, Post-COVID-19? Telemed e-Health. 2022;28:942–969. doi: 10.1089/tmj.2021.0399. [DOI] [PubMed] [Google Scholar]
- 64.Boffa RJ, Constanti M, Floyd CN, et al. Hypertension in adults: summary of updated NICE guidance. BMJ. 2019;367:l5310. doi: 10.1136/bmj.l5310. [DOI] [PubMed] [Google Scholar]
- 65.Park S-D, Kim S-W, Moon JS, et al. Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus. Diabetes Metab J. 2021;45:109–114. doi: 10.4093/dmj.2020.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kuan PX, Chan WK, Fern Ying DK, et al. Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis. Lancet Digit Heal. 2022;4:e676–e691. doi: 10.1016/S2589-7500(22)00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Narla A, Paruchuri K, Natarajan P. Digital health for primary prevention of cardiovascular disease: Promise to practice. Cardiovasc Digit Heal J. 2020;1:59–61. doi: 10.1016/j.cvdhj.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]