Abstract
Background
This study presents a kinematic analysis of an acute lateral ankle sprain incurred during a televised badminton match. The kinematics of this injury were compared to those of 19 previously reported cases in the published literature.
Methods
Four camera views of an acute lateral ankle sprain incurred during a televised badminton match were synchronized and rendered in 3-dimensional animation software. A badminton court with known dimensions was built in a virtual environment, and a skeletal model scaled to the injured athlete's height was used for skeletal matching. The ankle joint angle and angular velocity profiles of this acute injury were compared to the summarized findings from 19 previously reported cases in the published literature.
Results
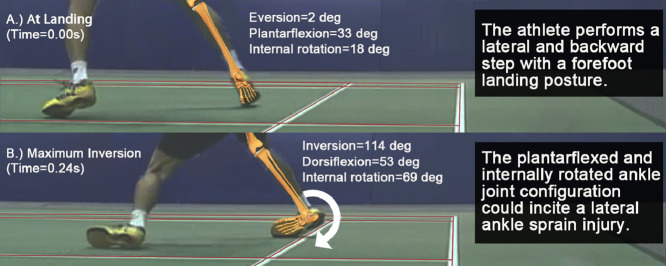
At foot strike, the ankle joint was 2° everted, 33° plantarflexed, and 18° internally rotated. Maximum inversion of 114° and internal rotation of 69° was achieved at 0.24 s and 0.20 s after foot strike, respectively. After the foot strike, the ankle joint moved from an initial position of plantarflexion to dorsiflexion—from 33° plantarflexion to 53° dorsiflexion (range = 86°). Maximum inversion, dorsiflexion, and internal rotation angular velocity were 1262°/s, 961°/s, and 677°/s, respectively, at 0.12 s after foot strike.
Conclusion
A forefoot landing posture with a plantarflexed and internally rotated ankle joint configuration could incite an acute lateral ankle sprain injury in badminton. Prevention of lateral ankle sprains in badminton should focus on the control and stability of the ankle joint angle during forefoot landings, especially when the athletes perform a combined lateral and backward step.
Keywords: Ankle, Biomechanics, Injury prevention, Ligament injuries, Sports medicine
Graphical Abstract
Highlights
-
•
When an athlete performs a lateral and backward step, the forefoot landing posture can result in a plantarflexed and internally rotated ankle joint configuration.
-
•
The forefoot landing increases the moment arm among the subtalar joint and results in an explosive inversion torque, causing the inversion sprain injury.
-
•
At foot strike, the ankle joint was 2° everted, 33° plantarflexed, and 18° internally rotated. The maximum inversion of 114° and internal rotation of 69° was achieved at 0.24 and 0.20 seconds after foot strike, respectively.
1. Introduction
Acute lateral ankle sprains are a commonly incurred injury by individuals who partake in field, court, and indoor sports.1,2 Lateral ankle sprains can result in the development of a multitude of motor–behavioral impairments,3 including changes in lower limb stiffness,4 variations in lower limb joint coupling,5 and inhibited invertor and evertor strength.6 In the longer term, lateral ankle sprains may lead to chronic ankle instability, osteoarthritis, on-going disability, decreased quality of life,7 and reduced self-report ankle joint function.8 The medical costs associated with ankle sprain injuries have been estimated to be USD 6.2 billion and Euro 208 million per year in the United States and the Netherlands, respectively.9 These costs are alarmingly high for an injury that is deemed relatively easy to prevent.9 Both the prevention of lateral ankle sprain and effective rehabilitation management are important because the injured athletes often suffer from a recurrent sprain in the long term.10,11 Prevention of ankle sprain has also been suggested as one of the 8 priority recommendations for future research by the International Ankle Consortium.12
Understanding the mechanisms of injury is central to the implementation of successful injury prevention iniatives,13 as well as for informing decision-making processes to prioritize the clinical assessment of potentially injured tissues.14 The typical mechanism of acute lateral ankle sprain was first suggested as inversion, plantarflexion, and internal rotation by Garrick15 in 1977. In 2004, Andersen and co-workers16 used videos to analyze 26 ankle injuries in Norwegian and Icelandic football and reported qualitative presentation of the most common injury mechanisms. In 2009, Fong and co-workers17 provided the first forensic video analysis of a lateral ankle sprain injury with kinematic quantities, and to date a total of 10 similar reports presenting 19 lateral ankle sprain cases or giving-way episodes have been published, including one in high jumping, one in hockey,18 five in tennis,19 four in basketball,20 and eight in cutting motions captured during laboratory trials.17,21, 22, 23, 24, 25, 26 Furthermore, 2 recent systematic video analyses of injury mechanisms reported that ankle sprains were associated with take-offs in handball27 and with landing on the opponent or front-row teammates in volleyball.28 The findings from these 13 video analyses16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 generally present a rapidly “rolled” or “twisted” ankle,14 or, to be specific, an increase in inversion and internal rotation with or without plantarflexion.29
Badminton is a popular global sport, with about 200 million players around the world.30 A 20-year epidemiology study of racket sports in the United States between 1997 and 2016 suggested that the ankle was the most commonly injured body part in badminton.31 Numerous epidemiology studies suggest that most ankle injuries in badminton are lateral ankle sprains.32,33 Despite being a popular global sport, badminton has received little interest in sports medicine over the last 30 years.34 In April 2020, a search on PubMed for injury mechanism research, using the string “badminton[Title]” AND “injury” AND “mechanism”, generated only seven results, with three on knee injuries,35, 36, 37 two on both knee and ankle injuries,38,39 and one on ocular trauma.40 Because playing badminton is low cost and relatively convenient and feasible for all ages, the popularity of the sport has increased substantially in recent years.31 Therefore, there is a need to initiate research on the mechanisms of the most common injury in badminton, the lateral ankle sprain, to inform future studies on its prevention.
This study presents a kinematic analysis of an acute lateral ankle sprain incurred during a televised badminton match. We also compared the findings from our study with those from 19 previously reported cases in the published literature concerning peak ankle joint angles, peak angular velocities, and the time of the peak joint angle.
2. Methods
2.1. The injury case in badminton
An online video search was performed to obtain an ankle sprain injury sustained in a televised badminton match. The search was performed on the YouTube website (www.youtube.com) with the following keywords: “ankle sprain”, “ankle injury”, and “badminton”, The inclusion criteria were: (1) the badminton player incurred an unwanted excessive ankle inversion during a lateral movement, (2) the badminton player needed to be withdrawn from the match for receiving medical treatment due to the ankle lateral sprain injury, (3) the injury was reported to be an ankle sprain injury to the ligament or tendon at the lateral ankle in the official post-match report, and (4) at least 2 camera views showed the shank, the ankle joint, and the foot segment during the injury motion. One case from the 2012 Thomas & Uber Cup fulfilled the criteria and was selected for the analysis. The athlete stepped laterally and backward to retrieve a shot at the baseline on the right and he landed on the forefoot of his right foot. He then twisted his right ankle with rapid inversion and with the foot rolling over the lateral edge. The athlete's foot then bounced off the ground for a very short time and then the athlete fell to the ground and clutched his right foot. The athlete was not using any prophylactic device such as an ankle brace or tape. After being examined by a physician, the athlete limped toward the opponent, shook hands, and withdrew from the match. The athlete was then side-lined, with cryotherapy immediately administered to his right ankle. A post-match report from an English-language newspaper in the event's hosting country indicated that magnetic resonance imaging was carried out after the incident and confirmed a tendon tear in the right ankle, which would require 3–4 weeks to heal, as suggested by a doctor and disclosed by the athlete's coach. Another post-match report from a newspaper published in the home language of the hosting country reported the injury as a ligamentous tear at the foot.
Ethical approval for our study was obtained from Loughborough University (SSEHS-PG82). We did not obtain written consent for disclosing the athlete's identity, medical diagnosis, or other details related to this injury incident and therefore have only analyzed the case based on the resources we obtained from the public domain.
2.2. The forensic biomechanics analysis method
Video footage of 4 views at a 25 Hz framing rate was obtained. The footage was trimmed from 0.08 s before the foot strike until the foot bounced off and left the ground 0.36 s after the foot strike. It was transferred from the original format into uncompressed Audio Video Interleave image sequences by using Adobe Premiere Pro (Version CS4; Adobe Systems Inc., San Jose, CA, USA). The image sequences were then synchronized and rendered into 1 Hz video sequences using Adobe After-Effects (Version CS4; Adobe Systems Inc.). Poser 4 and Poser Pro Pack (Curious Labs Inc., Santa Cruz, CA, USA) were used to perform the matching of the skeleton. The surroundings were built into the virtual environment using the real dimensions of a badminton court as defined by the Badminton World Federation.41 After matching the virtual environment to the video frame-by-frame, a skeletal model (Zygote Media Group Inc., Provo, UT, USA), proportionally scaled to the athlete's height as obtained from the Badminton World Federation webpage (https://bwfbadminton.com/players/), was used for skeletal matching. The skeletal model was matched frame by frame, starting at the hip, then distally to the thigh, then to the shank segment, and finally to the foot and toe segments (Supplementary Fig. 1). The details of the motion analysis method can be found in a previous study.42 The axis of rotation and convention was defined with reference to International Society of Biomechanics recommendations.43 The line connecting the knee joint center and the ankle joint center was defined as the longitudinal axis of the shank segment (X1). The anterior–posterior axis of the shank segment (X2) was the cross product of X1 and the line joining the lateral femoral epicondyle and medial femoral epicondyle. The medial–lateral axis of the shank segment was the cross product of X1 and X2. The foot segment was alighted with the local coordinate system of shank in the anatomical position. The positive angles were defined as inversion, plantarflexion, and internal rotation. The profiles of the ankle joint angles and angular velocities in all 3 planes were calculated. The peak values for each variable and the time of the peak joint angle were extracted for comparison with the range provided in the 19 previously reported cases.17, 18, 19, 20, 21, 22, 23, 24, 25, 26
3. Results
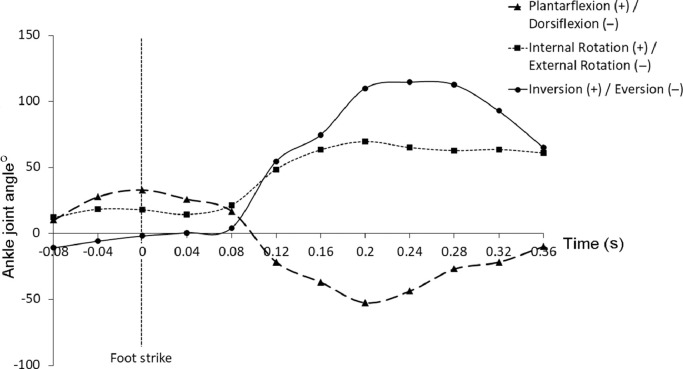
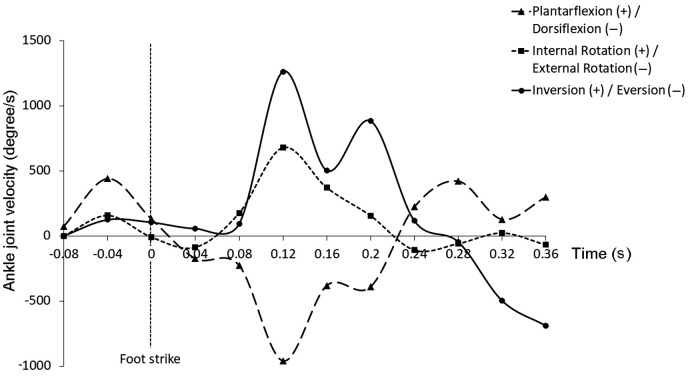
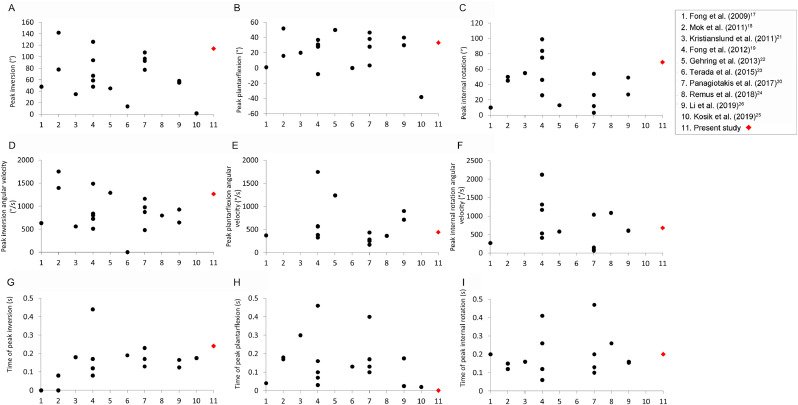
The linesmen's view video sequence (at 0.04-s intervals) of the lateral ankle sprain injury with the matched skeletal model is shown in Supplementary Fig. 2. The profiles of the ankle joint angles and angular velocities are shown in Fig. 1, Fig. 2, respectively. At the foot strike, the ankle joint was 2° everted, 33° plantarflexed, and 18° internally rotated. After the foot strike, there were some fluctuations of about 20° within the first 0.08 s. Then, there was a peak inversion of 114° and a peak internal rotation of 69° at 0.24 s and 0.20 s after foot strike, respectively. The ankle joint dorsiflexed after foot strike, reaching a maximum of 53° dorsiflexion at 0.20 s after foot strike. The ankle joint angular velocity fluctuated a great deal, with the inversion, dorsiflexion, and internally rotating angular velocities reaching their maximum values, which were 1262°/s, 961°/s, and 677°/s, respectively, at 0.12 s after foot strike. Table 1 shows the peak ankle joint angle, angular velocity, and time to peak ankle joint angle for our study, and Fig. 3 shows the peak ankle joint angle, angular velocity, and time to peak ankle joint angle for our study relative to those reported in the 19 previously published case studies. The findings in our study are generally within the ranges reported in the other studies, except for the time of plantarflexion, which was before foot strike (a negative value).
Fig. 1.
Ankle joint angle profiles during the ankle sprain incident.
Fig. 2.
Ankle joint angular velocity profiles during the ankle sprain incident.
Table 1.
Peak ankle joint angle, angular velocity, and time to peak ankle joint angle in the present study.
| Variable | Value |
|---|---|
| Peak inversion (°) | 114 |
| Peak inversion angular velocity (°/s) | 1262 |
| Time of peak inversion (s) | 0.24 |
| Peak plantarflexion (°) | 33 |
| Peak plantarflexion angular velocity (°/s) | 440 |
| Time of peak plantarflexion (s) | 0.00 |
| Peak internal rotation (°) | 69 |
| Peak internal rotation angular velocity (°/s) | 677 |
| Time of peak internal rotation (s) | 0.20 |
Fig. 3.
Peak ankle joint angle (A–C), angular velocity (D–F), and time to peak ankle joint angle (G–I) in the present study and in the 19 previously published case reports.
4. Discussion
Our findings suggest that the movement patterns found in our study on the badminton injury are quite similar to the findings in the 19 previously published cases, which involve different sports and different kinds of landing and cutting movements. The peak inversion angle in our study was 114°, which is quite a large inverted joint configuration for the ankle, and the corresponding peak angular velocity in our study was 1262°/s, which was in agreement with all the other 19 reported cases. Internal rotation and angular velocity in our study were also within the range reported in the other studies. For both inversion and internal rotation, the peak values in our study occurred at a relatively late time (0.24 s and 0.20 s after the foot strike, respectively). This may be due to the forefoot contacting the ground, with 33° plantarflexed ankle, followed by a short duration of about 0.08 s of fluctuation of ankle joint angles, as shown in Fig. 1. This was probably caused by the sudden lateral and backward movement, which occurs frequently in badminton. In performing this kind of movement, athletes usually land on the forefoot; thus, the ankle joint is in a plantarflexed configuration. This forefoot landing posture increases the moment arm among the subtalar joint and results in a greater inversion torque,44 causing the inversion sprain injury. This also explains why the athlete's ankle dorsiflexed after the foot strike. Even when the ankle joint has reached the maximum inversion at 0.24 s, with the heel still off the ground, the ankle joint is still in a dorsiflexed configuration as the lower leg tilts forward as a result of the backward-stepping movement (Supplementary Fig. 2).
Prevention of lateral ankle sprain in badminton should focus on the control and stability of the ankle joint angle during forefoot landing postures, especially when the athletes perform a lateral and backward step. Although badminton is a sport that is played across a net and can be said to be relatively safe due to its non-contact nature, the incidence rate of the lateral ankle sprain (0.134 per 1000 h of play) is still considered high.45 The high incidence rate of lateral ankle sprain is likely related to frequent sudden lateral and backward stepping, which puts the ankle in a risky position. Therefore, balance and joint control while landing is very important for badminton players because it allows them to maintain fast movements and body balance during a match.46 A summary of ankle joint kinematics from current and previous studies indicates that a large ankle plantarflexion is not mandatory for a lateral ankle sprain to occur. However, the development of inversion and internal rotation were observed shortly after foot strike. Neuromuscular training has been proven to be effective in improving joint configuration during stepping or landing.47,48 However, stability of the ankle joint decreases with fatigue.49 Therefore, athletes should utilize taping50, 51, 52 or bracing,53, 54, 55 which provides a mechanical effect that prevents unwanted ankle movements. In our study, dorsiflexion was found after the foot strike. Therefore, taping and bracing may not be always helpful in preventing ankle sprains, but may limit the jumping performance and movement agility as they restrict ankle plantarflexion
Injuries and their mechanisms may be different for the dominant and non-dominant sides in badminton because the sport is asymmetrical in nature. Regarding anterior cruciate ligament knee injuries in badminton, it has been reported that the knee opposite the racket-hand side tends to sustain a larger number injuries during single-leg landing after a backhand overhead stroke, while the knee on the racket-hand side has a higher injury rate during sidestep cuts during side or backward stepping.35 A detailed biomechanical analysis identified increased knee valgus alignment and moment during single-leg landing after overhead strokes as a potential risk factor for anterior cruciate ligament injuries in badminton.56 Similarly, the risk of a lateral sprain on the 2 ankles may be different due to the asymmetrical movement in badminton. In the case we reported on, the player was a right-handed player; he used his right hand to hold the racket according to the website of the Badminton World Federation. It was observed that he leaned his body backward when hitting a right-sided (dominant side) backhand overhead stroke, with lateral backward stepping. When the backhand overhead stroke occurred on the left (non-dominant) side, it was observed that he twisted his body instead of leaning backward. Thus, the difference in whole-body biomechanics between the dominant and non-dominant sides may have created a substantial difference in ankle joint loading during the step.57 Additional studies using motion analysis in match-like situations are needed to reveal the differences in ankle joint configuration between the dominant and non-dominant sides. These differences could affect approaches to sprain prevention, such as taping and bracing, depending on the injury to be prevented.
Analysis of ankle sprain injuries using a model-based, image-matching technique is more feasible for badminton than for other sports. The use of this method requires having sufficient perpendicular straight lines in the background, which is quite difficult to achieve in other sports. First, the size of the badminton court is always fixed and is much smaller than in other sports, which means that the entire side-lengths are visible. Second, there are always 2 parallel lines at all 4 sides (singles and doubles), which means that the entire rectangle shape at a corner is fully seen and can already help the matching of the environment. Badminton is played either as a solo sport or as doubles, so it is easier to have a camera that can provide a “zoomed” view of an athlete. Finally, in recent years, televised badminton matches place cameras in positions that provide both a linesman's view and a “sky” view. The linesman's view is especially useful because the camera is usually set parallel to the 2 baselines in order to check whether the shuttle lands in or out of the court. This zoomed-up view, which can be zoomed, allows the athlete's injured body part, such as the ankle, to occupy a larger area on the screen, making an analysis of the injury easier and more accurate.
However, a limitation of this method is the relatively low frame rate used in standard televised video footage available online. In our case study, The current case length is 0.36 s, therefore, only 10 data points could be obtained from the 25 Hz video footage. The data points started at the foot strike and ended at the restoration of normal ankle motion after excessive inversion. The ankle joint angle profiles were smooth, and the missing peak error was unlikely (Fig. 1). However, the ankle joint velocity profiles were affected by the low frame rate, in that a wobbling effect was observed in these profiles (Fig. 2). In future studies, researchers should try to acquire video with a higher frame rate from the broadcasting company.
In addition to lateral ankle sprain injuries, many other injuries occur in badminton (e.g., Achilles tendon ruptures, anterior cruciate ligament injuries, meniscus injuries, and so forth).35,58 Researchers using model-based, image-matching, motion analysis techniques to study ankle and knee injuries in sports should consider using badminton as the sport of choice in order to take advantage of the above-mentioned features of the badminton court environment.
5. Conclusion
We analyzed a single lateral ankle sprain case in badminton and compared it to 19 previously reported cases in the literature. Our findings suggested that a forefoot landing posture with a plantarflexed and internally rotated ankle joint configuration could cause a lateral ankle sprain injury in badminton. Prevention of lateral ankle sprains in badminton should focus on the control and stability of the ankle joint angle during a forefoot landing posture, especially when the athlete takes a lateral and backward step.
Acknowledgments
Acknowledgment
The authors acknowledge funding from the Badminton World Federation for this study.
Authors’ contributions
DTPF designed the study, interpreted the data, drafted the manuscript, and approved the final version of the manuscript; KMM acquired the data, interpreted the data, and critically revised the manuscript; IMT, YW, and WS analyzed and interpreted the data and critically revised the manuscript; MAK designed and approved the study. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.03.007.
Supplementary materials
References
- 1.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44:123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 2.Fong DTP, Hong Y, Chan LK, Yung PSH, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54:572–588. doi: 10.4085/1062-6050-344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeon K, Kim K, Kang K. Leg stiffness control during drop landing movement in individuals with mechanical and functional ankle disabilities. Sports Biomech. 2022;21:1093–1106. doi: 10.1080/14763141.2020.1726997. [DOI] [PubMed] [Google Scholar]
- 5.Lilley T, Herb CC, Hart J, Hertel J. Lower extremity joint coupling variability during gait in young adults with and without chronic ankle instability. Sports Biomech. 2018;17:261–272. doi: 10.1080/14763141.2017.1287215. [DOI] [PubMed] [Google Scholar]
- 6.Khalai N, Vicenzino B, Heales LJ, Smith MD. Is chronic ankle instability associated with impaired muscle strength? Ankle, knee and hip muscle strength in individuals with chronic ankle instability: A systematic review with meta-analysis. Br J Sports Med. 2020;54:839–847. doi: 10.1136/bjsports-2018-100070. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk CN, Vuurberg G. There is no such thing as a simple ankle sprain: Clinical commentary on the 2016 International Ankle Consortium position statement. Br J Sports Med. 2017;51:485–486. doi: 10.1136/bjsports-2016-096733. [DOI] [PubMed] [Google Scholar]
- 8.Kosik KB, McCann RS, Terada M, Gribble PA. Therapeutic interventions for improving self-reported function in patients with chronic ankle instability: A systematic review. Br J Sports Med. 2017;51:105–112. doi: 10.1136/bjsports-2016-096534. [DOI] [PubMed] [Google Scholar]
- 9.Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 10.Kaminski TW, Needle AR, Delahunt E. Prevention of lateral ankle sprains. J Athl Train. 2019;54:650–661. doi: 10.4085/1062-6050-487-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janssen KW. Infographic: Ankle sprain treatment and prevention timeline. Br J Sports Med. 2018;52:953–954. doi: 10.1136/bjsports-2016-097183. [DOI] [PubMed] [Google Scholar]
- 12.Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1493–1495. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 13.Bahr R, Krosshaug T. Understanding injury mechanisms: A key component of preventing injuries in sports. Br J Sports Med. 2005;39:324–329. doi: 10.1136/bjsm.2005.018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delahunt E, Gribble PA. Structured clinical assessment: A brake to stop the ankle joint “rolling”. Br J Sports Med. 2018;52:1294. doi: 10.1136/bjsports-2017-098789. [DOI] [PubMed] [Google Scholar]
- 15.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 16.Andersen TE, Floerences TW, Arnason A, Bahr R. Video analysis of the mechanisms for ankle injuries in football. Am J Sports Med. 2004;32(Suppl. 1):S69–S79. doi: 10.1177/0363546503262023. [DOI] [PubMed] [Google Scholar]
- 17.Fong DTP, Hong Y, Shima Y, Krosshaug T, Yung PSH, Chan KM. Biomechanics of supination ankle sprain – A case report of an accidental injury event in laboratory. Am J Sports Med. 2009;37:822–827. doi: 10.1177/0363546508328102. [DOI] [PubMed] [Google Scholar]
- 18.Mok KM, Fong DTP, Krosshaug T, et al. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: 2 cases during the 2008 Beijing Olympics. Am J Sports Med. 2011;39:1548–1552. doi: 10.1177/0363546511399384. [DOI] [PubMed] [Google Scholar]
- 19.Fong DTP, Ha SCW, Mok KM, Chan CWL, Chan KM. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: Five cases from televised tennis competitions. Am J Sports Med. 2012;40:2627–2632. doi: 10.1177/0363546512458259. [DOI] [PubMed] [Google Scholar]
- 20.Panagiotakis E, Mok KM, Fong DTP, Bull AMJ. Biomechanical analysis of ankle ligamentous sprain injury cases from televised basketball games: Understanding when, how and why ligament failure occurs. J Sci Med Sport. 2017;20:1057–1061. doi: 10.1016/j.jsams.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Kristianslund E, Bahr R, Krosshaug T. Kinematics and kinetics of an accidental lateral ankle sprain. J Biomech. 2011;44:2576–2578. doi: 10.1016/j.jbiomech.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 22.Gehring D, Wissler S, Mornieux G, Gollhofer A. How to sprain your ankle – A biomechanical case report of an inversion trauma. J Biomech. 2013;4:175–178. doi: 10.1016/j.jbiomech.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 23.Terada M, Gribble P. Jump landing biomechanics during a laboratory recorded recurrent ankle sprain. Foot Ankle Int. 2015;36:842–848. doi: 10.1177/1071100715576517. [DOI] [PubMed] [Google Scholar]
- 24.Remus A, Caulfield B, Doherty C, Crowe C, Severini G, Delahunt E. A laboratory captured “giving way” episode in an individual with chronic ankle instability. J Biomech. 2018;76:241–246. doi: 10.1016/j.jbiomech.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 25.Kosik KB, Hock MC, Heebner NR, Hartzell J, Gribble PA. A laboratory captured “giving way” episode during a single-leg landing task in an individual with unilateral chronic ankle instability. J Biomech. 2019;90:153–158. doi: 10.1016/j.jbiomech.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Li Y, Ko J, Zhang S, Brown CN, Simpson KJ. Biomechanics of ankle giving way: A case report of accidental ankle giving way during the drop landing test. J Sport Health Sci. 2019;8:494–502. doi: 10.1016/j.jshs.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luig P, Krutsch W, Henke T, et al. Contact–but not foul play–dominates injury mechanisms in men's professional handball: A video match analysis of 580 injuries. Br J Sports Med. 2020;54:984–990. doi: 10.1136/bjsports-2018-100250. [DOI] [PubMed] [Google Scholar]
- 28.Skazalski C, Kruczynski J, Bahr MA, Bere T, Whiteley R, Bahr R. Landing-related ankle injuries do not occur in plantarflexion as once thought: A systematic video analysis of ankle injuries in world-class volleyball. Br J Sports Med. 2018;52:74–82. doi: 10.1136/bjsports-2016-097155. [DOI] [PubMed] [Google Scholar]
- 29.Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52:1304–1310. doi: 10.1136/bjsports-2017-098885. [DOI] [PubMed] [Google Scholar]
- 30.Phomsoupha M, Laffaye G. The science of badminton: Game characteristics, anthropometry, physiology, visual fitness and biomechanics. Sports Med. 2015;45:473–495. doi: 10.1007/s40279-014-0287-2. [DOI] [PubMed] [Google Scholar]
- 31.Nhan DT, Klyce W, Lee RJ. Epidemiological patterns of alternative racquet-sport injuries in the United States, 1997–2016. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118786237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goh SL, Mokhtar AH, Ali MRM. Badminton injuries in youth competitive players. J Sports Med Phys Fitness. 2013;53:65–70. [PubMed] [Google Scholar]
- 33.Yung PSH, Chan RHK, Wong FCY, Cheuk PWL, Fong DTP. Epidemiology of injuries in Hong Kong elite badminton athletes. Res Sports Med. 2007;15:133–146. doi: 10.1080/15438620701405263. [DOI] [PubMed] [Google Scholar]
- 34.Jørgensen U, Winge S. Injuries in badminton. Sports Med. 1990;10:59–64. doi: 10.2165/00007256-199010010-00006. [DOI] [PubMed] [Google Scholar]
- 35.Kimura Y, Ishibashi Y, Tsuda E, Yamamoto Y, Tsukada H, Toh S. Mechanisms of anterior cruciate ligament injuries in badminton. Br J Sports Med. 2010;44:1124–1127. doi: 10.1136/bjsm.2010.074153. [DOI] [PubMed] [Google Scholar]
- 36.Sasaki S, Nagano Y, Ichikawa H. Loading differences in single-leg landing in the forehand- and backhand-side courts after an overhead stroke in badminton: A novel tri-axial accelerometer research. J Sports Sci. 2018;36:2794–2801. doi: 10.1080/02640414.2018.1474535. [DOI] [PubMed] [Google Scholar]
- 37.Valldecabres R, de Benito AM, Littler G, Richards J. An exploration of the effect of proprioceptive knee bracing on biomechanics during a badminton lunge to the net, and the implications to injury mechanisms. PeerJ. 2018;20:e6033. doi: 10.7717/peerj.6033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fu L, Ren F, Baker JS. Comparison of joint loading in badminton lunging between professional and amateur badminton players. Appl Bionics Biomech. 2017;2017 doi: 10.1155/2017/5397656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang P, Fu L, Zhang Y, Fekete G, Ren F, Gu Y. Biomechanics analysis methods to assess professional badminton players’ lunge performance. J Vis Exp. 2019;148:e58842. doi: 10.3791/58842. [DOI] [PubMed] [Google Scholar]
- 40.Khandelwal R, Majumdar MR, Gupta A. An usual mechanism of ocular trauma in badminton players: Two incidental cases. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr-2012-006363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Badminton World Federation . Stadium Badminton Kuala Lumpar;; Kuala Lumpar: 2011. BWF Handbook II (Laws of Badminton & Regulations) [Google Scholar]
- 42.Mok KM, Fong DTP, Krosshaug T, Hung ASL, Yung PSH, Chan KM. An ankle joint model-based image-matching motion analysis technique. Gait Posture. 2011;34:71–75. doi: 10.1016/j.gaitpost.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 43.Wu G, Siegler S, Allard P, et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J Biomech. 2002;35:543–548. doi: 10.1016/s0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]
- 44.Wright IC, Neptune RR, van den Bogert AJ, Nigg BM. The influence of foot positioning on ankle sprains. J Biomech. 2000;33:513–519. doi: 10.1016/s0021-9290(99)00218-3. [DOI] [PubMed] [Google Scholar]
- 45.Marchena-Rodriguez A, Gijon-Nogueron G, Cabello-Manrique D, Ortega-Avila AB. Incidence of injuries among amateur badminton players: A cross-sectional study. Medicine (Baltimore) 2020;99:e19785. doi: 10.1097/MD.0000000000019785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamed I, Hassan I. The effect of core stability training on dynamic balance and smash stroke performance in badminton players. Int J Sports Sci Physical Educ. 2017;2:44–52. [Google Scholar]
- 47.O'Driscoll J, Kerin F, Delahunt E. Effect of a 6-week dynamic neuromuscular training programme on ankle joint function: A case report. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:13. doi: 10.1186/1758-2555-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Minoonejad H, Karimizadeh Ardakani M, Rajabi R, Wikstrom EA, Sharifnezhad A. Hop stabilization training improves neuromuscular control in college basketball players with chronic ankle instability: A randomized controlled trial. J Sport Rehabil. 2019;28:576–583. doi: 10.1123/jsr.2018-0103. [DOI] [PubMed] [Google Scholar]
- 49.Herbaut A, Delannoy J. Fatigue increases ankle sprain risk in badminton players: A biomechanics study. J Sports Sci. 2020;38:1560–1565. doi: 10.1080/02640414.2020.1748337. [DOI] [PubMed] [Google Scholar]
- 50.Moore C, Donovan L, Murray AM, Armstrong C, Glaviano NR. External ankle taping does not alter lower extremity side-step and straight sprint biomechanics in young adult males. Sports Biomech. 2020;19:395–410. doi: 10.1080/14763141.2018.1493743. [DOI] [PubMed] [Google Scholar]
- 51.Sato N, Nunome H, Hattori M, Ikegami Y. Effect of individual ankle taping components on the restriction of ankle external inversion moment. Sports Biomech. 2020 doi: 10.1080/14763141.2020.1792539. [DOI] [PubMed] [Google Scholar]
- 52.Sato N, Nunome H, Hopper LS, Ikegami Y. Ankle taping can reduce external ankle joint moments during drop landings on a tilted surface. Sports Biomech. 2019;18:28–38. doi: 10.1080/14763141.2017.1375552. [DOI] [PubMed] [Google Scholar]
- 53.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51:113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 54.Henderson ZJ, Sanzo P, Zerpa C, Kivi D. Ankle bracing's effects during a modified agility task: Analysis of sEMG, impulse, and time to completeusing a crossover, repeated measures design. Sports Biomech. 2020;9:1–15. doi: 10.1080/14763141.2020.1778777. [DOI] [PubMed] [Google Scholar]
- 55.Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br J Sports Med. 2018;52:956. doi: 10.1136/bjsports-2017-098106. [DOI] [PubMed] [Google Scholar]
- 56.Kimura Y, Ishibashi Y, Tsuda E, Yamamoto Y, Hayashi Y, Sato S. Increased knee valgus alignment and moment during single-leg landing after overhead stroke as a potential risk factor of anterior cruciate ligament injury in badminton. Br J Sports Med. 2012;46:207–213. doi: 10.1136/bjsm.2010.080861. [DOI] [PubMed] [Google Scholar]
- 57.Masu Y, Muramatsu K, Hayashi N. Characteristics of sway in the center of gravity of badminton players. J Phys Ther Sci. 2014;26:1671–1674. doi: 10.1589/jpts.26.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fahlstrom M, Bjornstig U, Lorentzon R. Acute Achilles tenon rupture in badminton players. Am J Sports Med. 1998;26:467–470. doi: 10.1177/03635465980260032201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.