Abstract
Background
The pandemic has highlighted and exacerbated health inequities in both acute coronavirus disease 2019 (COVID‐19) and its longer‐term sequelae. Given the heterogeneity in definitions of long COVID and the lack of centralized registries of patients with the disease, little is known about the differential prevalence among racial, ethnic, and sex subgroups. This study examines long COVID among Black, White, Asian, and Hispanic Americans and evaluates differences in the associated cognitive symptomology.
Method
Data from four releases of the Census Bureau's Household Pulse Survey detailing COVID-19 incidence and the duration and type of symptoms among a nationally representative sample of adults from June 1, 2022, through October 17, 2022, were combined. Binary logistic regression assessed the relative likelihood of long COVID among those who had been diagnosed COVID between racial, ethnic, and sex subgroups. Among those reporting long COVID, differences in the prevalence of difficulty understanding and difficulty remembering were assessed. Empirical models accounted for household, regional, vaccination, and insurance differences between respondents. Two-stage selection models were applied to test the robustness of the results.
Results
Among respondents who tested positive for COVID-19, Blacks (OR=1.097, CI=1.034-1.163), females (OR=1.849, CI=1.794-1.907), and Hispanics (OR=1.349, CI=1.286-1.414) were more likely to experience long COVID (symptoms lasting for 3 months or longer) compared to Whites, males, and non-Hispanics respectively. However, those with private health insurance (OR=0.634, CI=0.611-0.658) and who received the COVID vaccine (OR=0.901, CI=0.864-0.94) were less likely to have endured COVID symptoms than their counterparts. Symptoms of long COVID varied significantly between population subgroups. Compared to Whites, Blacks were more likely to have trouble remembering (OR=1.878, CI=1.765-1.808) while Hispanics were more likely to report difficult understanding (OR=1.827, CI=1.413, 2.362). Females, compared to males, were less likely to experience trouble understanding (OR=0.664, CI=0.537, 0.821), but more likely to report trouble remembering (OR=1.34, CI=1.237, 1.451).
Conclusions
Long COVID is more prevalent among Blacks, Hispanics, and females, but each group appears to experience long COVID differently. Therefore, additional research is needed to determine the best method to treat and manage this poorly understood condition.
Keywords: COVID, Black, Hispanic, Disparities, Symptoms
Introduction
Some individuals who have been infected with the virus that causes acute coronavirus disease 2019 (COVID‐19) can experience long-term effects from their infection, known as post-COVID conditions (PCC) or long COVID. Long COVID is a multisystem disease of unknown cause whose manifestations, while partially overlapping the acute presentation, vary widely among patients and are exacerbated by comorbidities and vulnerabilities.1 Estimates suggest as approximately 6%2 but as many as 30%1 of adults what are infected by COVID-19 experience long COVID symptoms. Long COVID cognitive symptomology can include difficulty thinking, brain fog, difficulty concentrating, mood changes difficulty sleeping, and fatigue.3 Post-COVID conditions are a wide range of new, returning, or ongoing health problems that people experience after being infected with COVID-19. There is currently no specific diagnostic test designed to diagnose post-COVID conditions, and people may have a wide variety of symptoms making it difficult for healthcare providers to recognize post-COVID conditions It occurs in adults who were hospitalized and those who were not4, 5, 6 and has substantial implications for health services. Given the heterogeneity in definitions of long COVID and the lack of centralized registries of patients with the disease, little is known about those who might suffer from long‐term symptoms and systematic variation in symptomology among different population subgroups.
Acute COVID‐19 is associated with significant racial disparities7, 8, 9, 10 Black, Hispanic, and other non‐white racial groups are less likely to have access to testing;11 , 12 more likely to be infected;12, 13, 14, 15, 16 more likely to be hospitalized overall,16 though less likely to be hospitalized for any given level of severity;8 and more likely to have an adverse clinical outcome (including death).8 , 14 , 17 , 18 Whereas the association between race/ethnicity and health inequity in acute COVID‐19 is now well established, the association of inequities with long COVID is relatively unexplored.9 , 19 , 20 A recent report suggests disparities in long COVID prevalence.1 Being Black and fewer years of education have been identified as a significant predictor of cognitive dysfunction 6-months after hospitalization from COVID-19.21 To improve the care of vulnerable and minoritized populations with long COVID, we need to understand disparities in long COVID, identify variation in long COVID symptomology, and acknowledge that multiple nested domains of inequity interact in a mutually interdependent system to determine these outcomes.1 The objective of this study was to explore racial differences in reports of long covid and characterize the magnitude and differences in long covid cognitive symptomology.
Methods
Data: Data for this study was drawn from four releases of the Household Pulse Survey (HHPS)—a quick deployment data collection instrument designed to collect data on a range of ways in which people's lives have been impacted by the COVID-19 pandemic—collected between June 1, 2022, through October 17, 2022. The result of a collaboration between the US Census Bureau and other federal agencies, the HHPS began on April 23, 2020, and continues to measure how the COVID-19 pandemic is impacting households across the country from a social and economic perspective. This study employed Phase 3.6 which included new questions on the ability to carry out day-to-day activities due to experiencing long COVID as well as COVID-19 vaccinations, education, employment, food sufficiency, household spending, physical and mental health, social assistance, and core demographic household characteristics. The survey instrument utilized an overlapping weekly panel of respondents, each of whom was surveyed once weekly for three weeks before being replaced by a new panel.
In total, the survey sampled roughly 108,000 responses per week, stratified by race, ethnicity, sex, and age to ensure a representative sample. Furthermore, the educational attainment of the responding adult in each household was collected to align the final weighted distribution with the 2018 American Community Survey estimates of the adult population's educational attainment. While HHPS addresses a variety of topics, this analysis only includes items related to long COVID and potential symptoms; COVID-19, COVID-19 vaccination, and health insurance; and demographic and household characteristics. These survey items are discussed in greater detail below.
Long COVID and potential symptoms: While some content varied between the phases of the HHPS, this study utilized a newly added instrument evaluating the prevalence of long COVID. The question text and answer choices are listed below.
-
•
Did you have any symptoms lasting 3 months or longer that you did not have prior to having coronavirus or COVID-19? Long term symptoms may include: tiredness or fatigue, difficulty thinking, concentrating, forgetfulness, or memory problems (sometimes referred to as "brain fog", difficulty breathing or shortness of breath, joint or muscle pain, fast-beating or pounding heart (also known as heart palpitations), chest pain, dizziness on standing, menstrual changes, changes to taste/smell, or inability to exercise.” [Yes, No]
Phase 3.6 also included additional questions concerning the level of physical, emotional, and cognitive difficulties. Two of these items—difficulty remembering and difficulty understanding—were chosen for this analysis. Response choices included: no difficulty, some difficulty, a lot of difficulty, and cannot do at all. To allow for the estimation of a binary dependent variable, ‘a lot of difficulty’ was combined with ‘cannot do at all’ and ‘no difficulty’ was combined with ‘some difficulty.’
COVID-19, Vaccination, Insurance: HHPS also included several questions related to COVID-19 and the COVID-19 vaccine. First, individuals indicated whether they have ever tested positive for COVID-19 using a rapid point-of-care test, self-test, or laboratory test. Second, respondents indicated whether they have received the COVID-19 vaccine. While subsequent questions concern the type and number of vaccines, this analysis uses only the binary yes/no survey item. Third, respondents were asked several questions regarding their health insurance coverage. HHPS used these responses to create an indicator variable for respondents with private health insurance.
Demographic, Household Characteristics: Respondents indicated their sex at birth which was used to create a binary indicator of female sex. Individuals classified their race as White only, Black only, Asian only, or other race/any combination. Due to sample size limitations, Asian was combined with other race/any combination. Additionally, they classified themselves as Hispanic, Latino, or Spanish origin. To account for heterogeneity within the sample, age, household size, region of residence, and residing in a metropolitan statistical area (MSA) were also included in the analysis.
Mean and frequency values were calculated for the sample as well as racial and ethnic subgroups. Between group differences were tested with F and chi-square tests. Three empirical regression models were estimated to answer three specific research questions.
Research Question 1: Among individuals who tested positive for COVID, does the relative likelihood of long COVID vary between population subgroups?
Empirical Estimation 1: Logistic regression modeled the relatively likelihood of long COVID among individuals who had tested positive for COVID. The regression included age, race, ethnicity, sex, health insurance, region of residence, vaccination status, and week of survey response.
Robustness Tests 1: The likelihood of testing positive for COVID is related to an individual's environment, behavior, health, and social context. Since individuals are only at risk for long COVID if they have first had COVID, their relative likelihood of long COVID is not independent of their environment, behavior, health, and social context. Therefore, logistic regression estimation of the relative likelihood of long COVID could suffer from sample selection bias violating the assumption of independence in the error terms. To account for the non-randomness in the sample, a selection regression model was used. This two-stage, conditional estimation model first estimates the likelihood of testing positive for COVID, then estimates the likelihood of long COVID conditional on the likelihood of having had COVID. The likelihood of testing positive for COVID was modeled as a function of age, race, ethnicity, sex, insurance, household size, region of residence, MSA status of residence, and week of response. The conditional long COVID model included age, race, ethnicity, sex, and vaccination status.
Research Question 2: Among individuals who tested positive for COVID, does the relative likelihood of difficulty remembering/understanding vary between population subgroups?
Empirical Estimation 2: Logistic regression modeled the relatively likelihood of difficulty remembering/ understanding among individuals who had tested positive for COVID. The regression included age, race, ethnicity, sex, health insurance, region of residence, vaccination status, week of survey response, and an indicator of long COVID.
Robustness Tests 2: A two-stage selection model was used to estimate the likelihood of difficulty remembering/understanding, conditional on having tested positive for COVID. The likelihood of testing positive for COVID was modeled as a function of age, race, ethnicity, sex, insurance, household size, region of residence, MSA status of residence, and week of response. Difficulty remember/understanding was modeled as a function of age, race, ethnicity, sex, vaccination status, and long COVID.
Research Question 3: Among individuals who experience long COVID, does the relative likelihood of difficulty remember/understanding vary between population subgroups?
Empirical Estimation 3: Logistic regression modeled the relatively likelihood of difficulty remembering/understanding among individuals who experienced long COVID. The regression included age, race, ethnicity, sex, and health insurance.
Robustness Tests 3: A two-stage selection model was used to estimate the likelihood of difficulty remembering/understanding, conditional on having long COVID. First, the likelihood of long COVID was estimated as a function of age, race, ethnicity, and sex. Conditional on having experienced long COVID, difficulty remember/understanding was then modeled as a function of age, race, ethnicity, sex, vaccination status, and insurance.
Results
Table 1 lists full sample and subsample descriptive statistics. Respondents were on average 51 (sd=16.14) years old and lived in two to three person households (mean-2.67, sd=1.48). Most respondents were White (75.91%), with smaller percentages of Hispanics (17.15%), Blacks (11.95%) and Asian/other racial groups (12.15%). Over half (51.31%) of the sample was female and respondents from all four geographic regions had robust representation (Northeast 17.35%, South 38.28%, Midwest 20.61%, West 23.75%) and 32.65% lived within an MSA. About 40% of the sample had tested positive for COVID and, among those, about 30% had long COVID. Nearly 90% of the sample had been vaccinated for COVID (n=227.454, 88.5%).
Table 1.
Variable Mean and Frequency Distributions by Race and Ethnicity
| Full Sample (N=257,554) |
White (N=212,649, 76%) |
Black (N=19,641, 12%) |
Asian/Other (N=25,264, 12%) |
Difference Race |
Hispanic (N=22,047, 17%) |
Difference Ethnicity |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std Dev | Mean | Std Dev | Mean | Std Dev | Mean | Std Dev | F-Stat | P-Value | Mean | Std Dev | F-Stat | P-Value | |
| Age (18-86) | 50.26 | 16.14 | 51.42 | 16.22 | 49.14 | 14.73 | 45.1 | 15.34 | 1851.47 | <.0001 | 45.2 | 15.45 | 2759.98 | <.0001 |
| Household Size (1-10) | 2.67 | 1.48 | 2.61 | 1.42 | 2.81 | 1.63 | 3.03 | 1.7 | 1018.93 | <.0001 | 3.19 | 1.76 | 3014.4 | <.0001 |
| Week (1-10) | 2.81 | 1.41 | 2.82 | 1.41 | 2.75 | 1.4 | 2.76 | 1.4 | 42.22 | <.0001 | 2.79 | 1.4 | 5.07 | 0.0244 |
| N | PCT | N | PCT | N | PCT | N | PCT | N | PCT | |||||
| Chi-Squ | P-Value | Chi-Squ | P-Value | |||||||||||
| Female | 148221 | 51.31 | 121177 | 56.98 | 13463 | 68.55 | 13581 | 53.76 | 1148.65 | <.0001 | 13156 | 59.67 | 44.48 | <.0001 |
| Private Health Insurance | 173911 | 80.25 | 145793 | 80.68 | 11397 | 74.73 | 16721 | 80.5 | 315.46 | <.0001 | 12883 | 73.72 | 510.44 | <.0001 |
| Northeast | 38524 | 17.35 | 32757 | 15.4 | 2495 | 12.7 | 3272 | 12.95 | 2768 | 12.55 | ||||
| South | 82762 | 38.28 | 64127 | 30.16 | 11767 | 59.91 | 6868 | 27.18 | 7171 | 32.53 | ||||
| Midwest | 54965 | 20.61 | 48501 | 22.81 | 2974 | 15.14 | 3490 | 13.81 | 2337 | 10.6 | ||||
| West | 81303 | 23.75 | 67264 | 31.63 | 2405 | 12.24 | 11634 | 46.05 | 10570.98 | <.0001 | 9771 | 44.32 | 2639.6 | <.0001 |
| MSA | 80190 | 32.65 | 60108 | 28.27 | 9105 | 46.36 | 10977 | 43.45 | 4725.51 | <.0001 | 9972 | 45.23 | 2234.2 | <.0001 |
| Difficulty Understanding | 1563 | 0.71 | 1095 | 0.59 | 170 | 1.11 | 298 | 1.43 | 223.38 | <.0001 | 285 | 1.61 | 223.8 | <.0001 |
| Difficulty Remembering | 12945 | 5.86 | 10564 | 5.72 | 918 | 5.99 | 1463 | 7.01 | 56.84 | <.0001 | 1452 | 8.21 | 192.65 | <.0001 |
| Covid-19 | 108758 | 42.23 | 90339 | 42.48 | 7614 | 38.77 | 10805 | 42.77 | 105.18 | <.0001 | 11102 | 50.36 | 653.06 | <.0001 |
| Long Covid-19 | 32357 | 30.17 | 26566 | 29.8 | 2553 | 34.19 | 3238 | 30.45 | 63.34 | <.0001 | 4010 | 36.77 | 250.82 | <.0001 |
| Received Vaccine | 227454 | 88.5 | 187682 | 88.45 | 17232 | 87.97 | 22540 | 89.39 | 25.72 | <.0001 | 19175 | 87.18 | 41.46 | <.0001 |
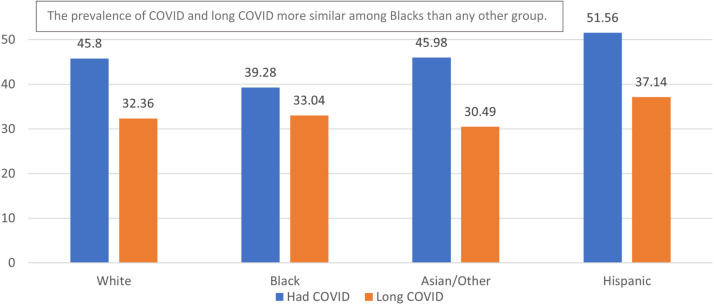
Analyses showed several significant differences between the racial and ethnic groups. As seen in Fig. 1 , a larger proportion of Whites tested positive for COVID than Blacks (χ2=105.18, p<.0001), but Blacks were significantly more likely to experience long COVID than Whites (χ2=63.34, p<.0001). Additionally, a larger proportion of Blacks (Remembering-5.99%; Understanding-1.11%), Asian/Other (Remembering-7.01%; Understanding-1.43%), and Hispanics (Remembering-8.21%; Understanding-1.61%) reported cognitive symptomology related to difficulty understanding and remembering compared to Whites (Remembering-5.72%; Understanding-0.59%)—statistically significant differences (Remembering: χ2=56.84, p<.0001; Understanding: χ2=223.38, p<.0001).
Fig. 1.
Prevalence of COVID-19 and "Long COVID" by Race/Ethnicity.
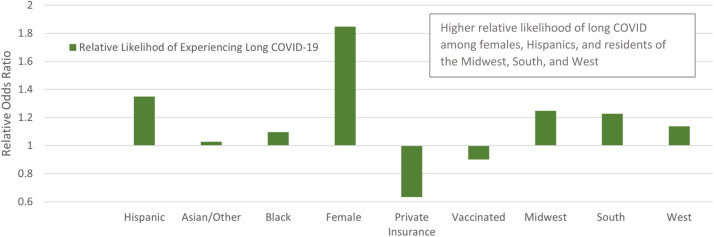
Research Question 1: Fig. 2 lists results from the logistic regression estimating the relative likelihood of long COVID. Among individuals who tested positive for COVID, Blacks (OR=1.097, CI=1.034, 1.163) and Hispanics (OR=1.349, CI=1.286, 1.414) were significantly more likely to report long COVID compared to Whites, non-Hispanics. Females (OR=1.849, CI=1.794, 1.907) were more likely than males to report long COVID, but respondents with private health insurance (OR=0.634, CI=0.611, 0.658) and those who received the COVID vaccine (OR=0.901, CI=0.864, 0.94) were comparatively less likely to report long COVID than the reference group.
Fig. 2.
Relative Likelihood of Long COVID-19 among Individuals who had COVID-19. Models the likelihood of long COVID. Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine; Region: Northeast. Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density. Sample: All individuals who tested positive for COVID.
Table 2 presents estimates from the selection model. In the first stage, the relatively likelihood of testing positive for COVID was estimated. Results showed that Blacks (β=-0.158, SE=0.011) and Asian/Other (β=-0.105, SE=0.010) were less likely to test positive for COVID, while Hispanics (β=0.131, SE=0.010), Females (β=0.059, SE=0.006), and members of larger household (β=0.085, SE=0.002) had a comparatively higher likelihood of testing positive. In the second stage, the relatively likelihood of long COVID was estimated contingent on having tested positive for COVID. Results resembled to those from the logistic regression indicating that Hispanics (β=0.0582, SE=0.0052), Blacks (β=0.0256, SE=0.0063), and females (β=0.1204, SE=0.0031) have a comparatively higher likelihood of long COVID compared to non-Hispanic Whites and males.
Table 2.
Selection Estimation of Long Covid Likelihood
| Log Likelihood | -197389 | |||
| AIC | 394832 | |||
| Schwarz Criterion | 395110 | |||
| Std Err | t Value | Pr > |t| | ||
| Dependent Variable: COVID symptoms > 3 months | ||||
| Intercept | 0.5753 | 0.0099 | 58.1500 | <.0001 |
| Age | 0.0004 | 0.0001 | 3.0600 | 0.0022 |
| Hispanic | 0.0582 | 0.0052 | 11.1100 | <.0001 |
| Asian/Other | 0.0094 | 0.0052 | 1.8100 | 0.0707 |
| Black | 0.0256 | 0.0063 | 4.0400 | <.0001 |
| Female | 0.1204 | 0.0031 | 38.9300 | <.0001 |
| Received COVID Vaccine | -0.0211 | 0.0045 | -4.6900 | <.0001 |
| Selection Equation | ||||
| Dependent Variable: Tested Positive for COVID | ||||
| Intercept | 0.072 | 0.018 | 4.000 | <.0001 |
| Age | -0.013 | 0.000 | -71.660 | <.0001 |
| Hispanic | 0.131 | 0.010 | 12.770 | <.0001 |
| Asian/Other | -0.105 | 0.010 | -11.040 | <.0001 |
| Black | -0.158 | 0.011 | -14.090 | <.0001 |
| Female | 0.059 | 0.006 | 10.550 | <.0001 |
| Private Health Insurance | 0.119 | 0.007 | 16.820 | <.0001 |
| Household Size | 0.085 | 0.002 | 43.310 | <.0001 |
| MSA | -0.012 | 0.006 | -1.830 | 0.067 |
| Week | 0.071 | 0.002 | 36.030 | <.0001 |
| Midwest | 0.042 | 0.008 | 5.290 | <.0001 |
| Northeast | 0.051 | 0.009 | 5.860 | <.0001 |
| South | 0.051 | 0.007 | 7.310 | <.0001 |
Indicates significant at 95% confidence level
Models the likelihood of long COVID
Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine; Region: Northeast
Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density.
Sample: All individuals with valid indicators for the dependent variables
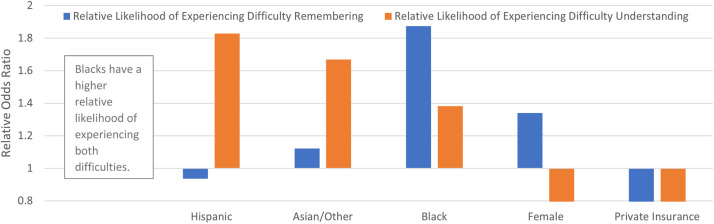
Research Question 2: Fig. 3 lists results from the logistic regression estimating the relative likelihood of cognitive symptomology (difficulty understanding and remembering), respectively. Among those who tested positive for COVID, Hispanics (OR=1.877, CI=1.528, 2.304) and Asian/other (OR=1.831, CI=1.475, 2.272) were more likely to have difficulty understanding, while females (OR=0.725, CI=0.615, 0.854) and those with private health insurance (OR=0.528, CI=0.443, 0.629) had a comparatively lower likelihood of difficulty understanding than the reference groups. Respondents with long COVID were, however, 300% to 400% (OR=3.306, CI=2.803, 3.899) more likely to have difficulty understanding than those without long COVID.
Fig. 3.
Relative Likelihood of Difficulty Understanding and Remembering among Individuals with Long COVID-19. Models the likelihood of difficulty understanding/remembering. Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine; Region: Northeast
Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density. Sample: All individuals with long COVID.
Blacks (OR=1.853, CI=1.765, 1.952) and Asian/other (OR=1.054, CI=0.967, 1.15) were more likely than Whites to have difficulty remembering, but Hispanics did not show a statistically significant differences from non-Hispanics. Females (OR=1.383, CI=1.305, 1.466) and residents of the South (OR=1.246, CI=1.143, 1.359) also showed relatively higher likelihoods of memory difficulties compared to men and residents of other regions. Those with long COVID (OR=3.744, CI=3.546, 3.953) were significantly more likely to have difficulty remembering even after controlling for other factors than those without long COIVD.
Table 3 shows results from the selection model in which stage one evaluated the likelihood of testing positive for COVID and stage two estimated the conditional likelihood of difficulty remembering/understanding. Results were very similar to those presented above.
Table 3.
Selection Estimation of Difficulty Remembering/Understanding among Individuals testing Positive for COVID
| Log Likelihood | -169003 | -75136 | ||||||
| AIC | 338051 | 150313 | ||||||
| Schwarz Criterion | 338290 | 150531 | ||||||
| Dependent Variable: Difficulty Remembering | Dependent Variable: Difficulty Understanding | |||||||
| Std Err | t Value | Pr > |t| | Std Err | t Value | Pr > |t| | |||
| Intercept | 0.239 | 0.004 | 57.85 | <.0001 | 0.016 | 0.002 | 10.2 | <.0001 |
| Age | -0.001 | 0.000 | -20.14 | <.0001 | 0.000 | 0.000 | 0.35 | 0.7239 |
| Hispanic | -0.005 | 0.002 | -1.21 | 0.0273 | 0.005 | 0.001 | 6.29 | <.0001 |
| Asian/Other | 0.010 | 0.003 | 3.66 | 0.0003 | 0.009 | 0.001 | 8.73 | <.0001 |
| Black | 0.040 | 0.003 | 2.41 | 0.1587 | 0.005 | 0.001 | 1.04 | <.0001 |
| Female | 0.019 | 0.002 | 10.56 | <.0001 | -0.004 | 0.001 | -5.62 | <.0001 |
| Long COVID | 0.100 | 0.002 | 52.23 | <.0001 | 0.011 | 0.001 | 15.69 | <.0001 |
| Received COVID Vaccine | -0.001 | 0.002 | -0.61 | 0.5412 | -0.004 | 0.001 | -4.61 | <.0001 |
| Selection Equation | Selection Equation | |||||||
| Dependent Variable: Tested Positive for COVID | Dependent Variable: Tested Positive for COVID | |||||||
| Intercept | 0.045 | 0.014 | 3.13 | 0.0018 | 0.047 | 0.014 | 3.3 | 0.001 |
| Age | -0.010 | 0.000 | -65.04 | <.0001 | -0.010 | 0.000 | -65.54 | <.0001 |
| Hispanic | 0.040 | 0.007 | 5.46 | <.0001 | 0.040 | 0.007 | 5.39 | <.0001 |
| Asian/Other | -0.103 | 0.008 | -12.38 | <.0001 | -0.104 | 0.008 | -12.48 | <.0001 |
| Black | -0.254 | 0.009 | -29.6 | <.0001 | -0.257 | 0.009 | -29.82 | <.0001 |
| Female | 0.105 | 0.005 | 20.1 | <.0001 | 0.105 | 0.005 | 19.93 | <.0001 |
| Private Health Insurance | -0.018 | 0.006 | -2.78 | 0.0054 | 0.012 | 0.006 | 1.89 | 0.0592 |
| Household Size | 0.032 | 0.002 | 20.86 | <.0001 | 0.032 | 0.002 | 20.74 | <.0001 |
| MSA | 0.023 | 0.006 | 3.94 | <.0001 | 0.026 | 0.006 | 4.51 | <.0001 |
| Week | 0.058 | 0.002 | 31.66 | <.0001 | 0.058 | 0.002 | 31.4 | <.0001 |
| Midwest | -0.003 | 0.008 | -0.43 | 0.6698 | -0.003 | 0.008 | -0.34 | 0.7366 |
| Northeast | 0.034 | 0.008 | 4.1 | <.0001 | 0.034 | 0.008 | 4.11 | <.0001 |
| South | 0.004 | 0.007 | 0.55 | 0.5792 | 0.002 | 0.007 | 0.32 | 0.7478 |
Indicates significant at 95% confidence level
Models the likelihood of long COVID
Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine; Region: Northeast
Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density.
Sample: All individuals with valid indicators for the dependent variables
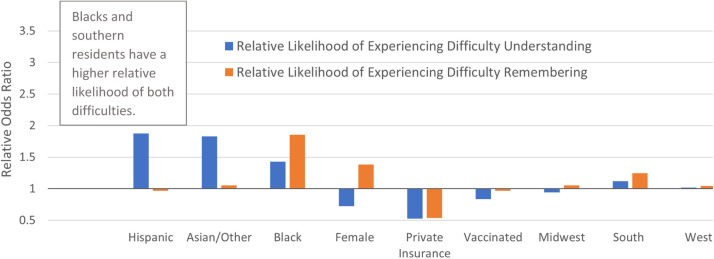
Research Question 3: Given the strong association between long COVID and difficulty remember/concentrating, the relatively likelihood among those with long COVID was estimated. Fig. 4 present logistic regression estimates of difficulty remembering and understanding, respectively, and results from the selection model are in Table 4 . Results were like those presented above. Hispanics (OR=1.827, CI=1.413, 2.362) and Asian/other (OR=1.668, CI=1.255, 2.216) had a higher likelihood of difficulty understandings than non-Hispanics and Whites, while females (OR=0.664, CI=0.537, 0.821) and those with private insurance (OR=0.606, CI=0.486, 0.755) had a lower likelihood of difficulty understanding compared to males and those with other types of insurance. Compared to Whites, Asian/other (OR=1.122, CI=1.004, 1.255) and Blacks (OR=1.874, CI=1.762, 1.904) were significantly more likely to have difficulty remembering. Female (OR=1.34, CI=1.237, 1.451) compared to males, were more likely to have difficulty remembering, while those with private insurance (OR=0.58, CI=0.537, 0.626) were less likely compared to other insurance types.
Fig. 4.
Relative Likelihood of Difficulty Understanding and Remembering among Individuals who Experienced COVID-19. Models the likelihood of difficulty understanding/remembering. Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine; Region: Northeast. Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density. Sample: All individuals who tested positive for COVID.
Table 4.
Selection Estimation of Difficulty Remembering/Understanding among Individuals with Long COVID
| N | 102270 | 102289 | ||||||
| AIC | 140415 | 83557 | ||||||
| Schwarz Criterion | 140567 | 83710 | ||||||
| Std Err | t Value | Pr > |t| | Std Err | t Value | Pr > |t| | |||
| Dependent Variable: Difficulty Remembering | Dependent Variable: Difficulty Understanding | |||||||
| Intercept | 0.323 | 0.011 | 28.51 | <.0001 | 0.040 | 0.004 | 9.96 | <.0001 |
| Age | -0.002 | 0.000 | -14.85 | <.0001 | 0.000 | 0.000 | -3.09 | 0.002 |
| Hispanic | -0.026 | 0.005 | -4.83 | <.0001 | 0.011 | 0.002 | 5.65 | <.0001 |
| Asian/Other | 0.029 | 0.007 | 4.28 | <.0001 | 0.010 | 0.003 | 4.14 | <.0001 |
| Black | -0.030 | 0.007 | -4.15 | <.0001 | 0.000 | 0.003 | -0.04 | 0.969 |
| Female | 0.025 | 0.005 | 5.13 | <.0001 | -0.009 | 0.002 | -5.18 | <.0001 |
| Selection Equation | Selection Equation | |||||||
| Dependent Variable: COVID symptoms> 3 months | Dependent Variable: COVID symptoms> 3 months | |||||||
| Intercept | -0.541 | 0.018 | -30.87 | <.0001 | -0.536 | 0.018 | -30.55 | <.0001 |
| Age | 0.001 | 0.000 | 5.01 | <.0001 | 0.001 | 0.000 | 5.07 | <.0001 |
| Hispanic | 0.089 | 0.011 | 8.23 | <.0001 | 0.090 | 0.011 | 8.36 | <.0001 |
| Asian/Other | -0.089 | 0.013 | -6.76 | <.0001 | -0.089 | 0.013 | -6.75 | <.0001 |
| Black | -0.071 | 0.014 | -4.94 | <.0001 | -0.070 | 0.014 | -4.92 | <.0001 |
| Female | 0.308 | 0.009 | 36.09 | <.0001 | 0.309 | 0.009 | 36.2 | <.0001 |
| Private Health Insurance | -0.405 | 0.010 | -38.95 | <.0001 | -0.398 | 0.010 | -38.08 | <.0001 |
| Received COVID Vaccine | 0.049 | 0.011 | 4.37 | <.0001 | 0.046 | 0.011 | 4.11 | <.0001 |
Indicates significant at 95% confidence level
Models the likelihood of difficulty remembering/understanding
Reference Group: Ethnicity: Non-Hispanic; Race: White; Sex: Male; Insurance: Public Insurance, Other Insurance, No Insurance; Vaccination: Did not received COVID-19 Vaccine
Estimates are weighted using person-level sampling weights to adjust for sampling framework, response bias, and residential density.
Sample: All individuals who tested positive for COVID
Discussion
The findings showed racial differences in the likelihood of developing long COVID. Blacks and Hispanics demonstrated a higher likelihood of developing long COVID than their White counterparts. Racial differences in development of long COVID may be partially explained by racial differences in likelihood of having private health insurance which is believed to be a protective factor from developing long COVID. In prior studies of COVID-19, Blacks and Hispanics are more likely to be infected,22 more likely to be hospitalized, less likely to have access to testing, less likely to have private health insurance.23 The findings reported here suggest these same disparities translate to long COVID.
This study also found females to demonstrate an increased likelihood of developing long COVID compared to their male counterparts. This is similar to previous findings that have identified being female as a risk factor for developing long COVID controlling for severity of the disease.24 Sex differences may in part be explained by immune response differences. While males tend to be more susceptible to viral infections than female, due to females’ higher response to viral infections they tend to have worse disease outcomes.25 , 26 These differences in prevalence of long COVID are compounded with the disproportionate impact of lifestyle changes brought upon by the COVID-19 pandemic compared to males. More importantly, females appear to have worse post COVID outcomes associated with life stressors that may translate in to greater complications among those with long COVID symptomology.27
Not only were racial and sex differences identified in the prevalence of long COVID but also cognitive symptomology. Blacks were more likely to have trouble remembering whereas Hispanics were more likely to report difficulty understanding than remembering. These differences mirror racial differences in general COVID-19 symptomology.28 In addition, females were more likely to report trouble remembering compared to their male counterparts. It is not clear why these racial, ethnic and sex differences present in long COVID. There is some literature that suggests there are racial differences in symptomology of acute COVID-19 that may translate into long COVID differences. Valdes and colleagues21 found lower cognitive scores on the Montreal Cognitive Assessments among Blacks with COVID-19 however the authors concluded observed differences in cognitive impairment may have been related to undiagnosed baseline cognitive dysfunction, implicit biases of the test used or other unmeasured social and economic disparities. It is possible that these same underlying disparities are the driving foundational causes of racial disparities in long COVID.
The lack of clarity surrounding these factors are particularly concerning given that little is known about the prognosis of long COVID or whether current inequalities are exacerbated in the chronic phases of the disease.22 In addition, the complexity of barriers believed to contribute to lack of equity in management of long COVID may be difficult to untangle in attempts to identify the optimal intervention targets. For example, barriers proposed include economic (medical expenses, lack of insurance, etc.), geographic (underserved areas, access to care, etc.), housing and segregation, and occupational that negatively impact vulnerable and minoritized populations.22 Additionally, the cognitive impairments resulting from long COVID currently will impact employment outcomes and future physical and mental health outcomes because of the high proportion of minoritized populations who are more likely to be frontline workers.22
Conclusion
The novelty, significance, and lack of understanding of long COVID poses significant challenges for the US healthcare systems. The disparities identified in this study further highlights the need to understand racial disparities observed in all other aspects of COVID-19 and chronic disease in general. The observed disparities in cognitive symptomology will have a dramatic impact on return to work, school and retaining family and societal roles among vulnerable and minoritized adults. Ultimately, largescale data collection must be urgently designed to explore the root causes of observed disparities and develop interventions to reduce the impact of the condition and the current racial disparity gap that exists.29
Availability of data and material
Data are publicly available from sources provided in the manuscript.
Code availability
Not applicable.
Declaration of competing interest
The authors have no relevant financial or non-financial interests to disclose.
Funding
The authors did not receive support from any organization for the submitted work.
References
- 1.Chen J, Sullivan CM. SW; Room 404E Washington, DC 20201: 2022. Office of the Assistant Secretary for Planning and Evaluation US Department of Health and Human Services 200 Independence Ave. Published online. [Google Scholar]
- 2.Hanson SW, Abbafati C, Aerts JG, et al. A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv. Published online 2022.
- 3.Aiyegbusi OL, Hughes SE, Turner G, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114(9):428–442. doi: 10.1177/01410768211032850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenhalgh T, Knight M, Buxton M, Husain L. Management of post-acute covid-19 in primary care. bmj. 2020:370. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 5.Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. Morb Mortal Wkly Rep. 2020;69(30):993–998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. Jama. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhala N, Curry G, Martineau AR, Agyemang C, Bhopal R. Sharpening the global focus on ethnicity and race in the time of COVID-19. Lancet. 2020;395(10238):1673–1676. doi: 10.1016/S0140-6736(20)31102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holtgrave DR, Barranco MA, Tesoriero JM, Blog DS, Rosenberg ES. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9–14. doi: 10.1016/j.annepidem.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Heal. 2020;5(6) doi: 10.1136/bmjgh-2020-002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim SR, Vann M, Bronner L, Manthey G. Which cities have the biggest racial gaps in COVID-19 testing access. FiveThirtyEight July. 2020:22. [Google Scholar]
- 12.Hatcher SM, Agnew-Brune C, Anderson M, et al. COVID-19 among American Indian and Alaska native persons—23 states, January 31–July 3, 2020. Morb Mortal Wkly Rep. 2020;69(34):1166. doi: 10.15585/mmwr.mm6934e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yancy CW. COVID-19 and african americans. Jama. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 14.Moore JT, Ricaldi JN, Rose CE, et al. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020—22 states, February–June 2020. Morb Mortal Wkly Rep. 2020;69(33):1122. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez DA, Hinson JS, Klein EY, et al. SARS-CoV-2 positivity rate for latinos in the baltimore–Washington, DC region. Jama. 2020;324(4):392–395. doi: 10.1001/jama.2020.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karaca-Mandic P, Georgiou A, Sen S. Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Intern Med. 2021;181(1):131–134. doi: 10.1001/jamainternmed.2020.3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan D, Sze S, Minhas JS, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahajan U V, Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. J Public Health (Bangkok) 2020;42(3):445–447. doi: 10.1093/pubmed/fdaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang CH, Schwartz GG. Spatial disparities in coronavirus incidence and mortality in the United States: an ecological analysis as of May 2020. J Rural Heal. 2020;36(3):433–445. doi: 10.1111/jrh.12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. Jama. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valdes E, Fuchs B, Morrison C, et al. Demographic and social determinants of cognitive dysfunction following hospitalization for COVID-19. J Neurol Sci. 2022 doi: 10.1016/j.jns.2022.120146. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger Z, Altiery DE Jesus V, Assoumou SA, Greenhalgh T. Long COVID and health inequities: the role of primary care. Milbank Q. 2021;99(2):519–541. doi: 10.1111/1468-0009.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Council NR. Understanding racial and ethnic differences in health in late life: a research agenda. Published online 2004. [PubMed]
- 24.Bai F, Tomasoni D, Falcinella C, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022;28(4):611. doi: 10.1016/j.cmi.2021.11.002. -e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein SL. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. Bioessays. 2012;34(12):1050–1059. doi: 10.1002/bies.201200099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kopel J, Perisetti A, Roghani A, Aziz M, Gajendran M, Goyal H. Racial and gender-based differences in COVID-19. Front public Heal. 2020;8:418. doi: 10.3389/fpubh.2020.00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frontera JA, Sabadia S, Yang D, et al. Life stressors significantly impact long-term outcomes and post-acute symptoms 12-months after COVID-19 hospitalization. J Neurol Sci. 2022;443 doi: 10.1016/j.jns.2022.120487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel JR, Amick BC, Vyas KS, Bircan E, Boothe D, Nembhard WN. Racial disparities in symptomatology and outcomes of COVID-19 among adults of Arkansas. Prev Med Reports. 2022 doi: 10.1016/j.pmedr.2022.101840. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abbasi J. The US now has a research plan for long COVID—is it enough? JAMA. 2022;328(9):812–814. doi: 10.1001/jama.2022.14536. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are publicly available from sources provided in the manuscript.