Abstract
CONTEXT:
Although children with attention-deficit/hyperactivity disorder (ADHD) are at elevated risk for comorbid psychopathology, the clinical correlates of ADHD in girls are far less understood relative to boys, despite ADHD being one of the most common childhood disorders in girls.
OBJECTIVE:
To meta-analytically summarize rates of comorbid internalizing (anxiety, depression) and externalizing (oppositional defiant disorder [ODD], conduct disorder [CD]) psychopathology among girls with and without ADHD.
DATA SOURCES:
Literature searches (PubMed, Google Scholar) identified published studies examining comorbid psychopathology in girls with and without ADHD.
STUDY SELECTION:
Eighteen studies (1997 participants) met inclusion criteria and had sufficient data for the meta-analysis.
DATA EXTRACTION:
Odds ratios for each comorbid disorder were calculated from available data. Demographic (eg, age, race/ethnicity) and study characteristics (eg, referral source, diagnostic method) were also coded.
RESULTS:
Compared with girls without ADHD, girls with ADHD were significantly more likely to meet Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for each comorbid disorder assessed. Relative odds were higher for externalizing (ODD: 5.6×; CD: 9.4×) relative to internalizing disorders (anxiety: 3.2×; depression: 4.2×). Meta-regression revealed larger effect sizes of ADHD on anxiety for studies using multiple diagnostic methods, featuring younger children, and including clinic-referred (versus community-referred) girls; the effect of ADHD on ODD varied based on diagnostic informant.
LIMITATIONS:
Findings were derived from cross-sectional studies, precluding causal inferences.
CONCLUSIONS:
Girls with ADHD frequently exhibit comorbid externalizing and internalizing disorders. We discuss future research priorities and consider intervention implications for ADHD and comorbid psychopathology in girls.
Attention-deficit/hyperactivity disorder (ADHD) is a prevalent, childhood-onset neurobehavioral disorder with considerable public health and financial consequences.1,2 Although ADHD is 2 to 3 times more prevalent in boys than in girls,3 greater understanding of the clinical presentation of ADHD in girls is needed. Approximately 5.6% of girls are diagnosed with ADHD in childhood, making it among the most prevalent psychiatric disorders in girls.1,2 Similar to boys, ADHD symptoms in girls frequently persist into adolescence and adulthood, predicting poor mental health, academic, and social outcomes.4–8 Some studies suggest that boys and girls with ADHD are similarly impaired,9 whereas other studies suggest that ADHD is more impairing for girls (eg, peer problems)10 despite being less prevalent. This “gender paradox” is evident across social, academic, and familial domains, which may reflect gender-atypical behavior and marginalization of girls with ADHD.11–13
ADHD frequently co-occurs with oppositional defiant disorder (ODD), conduct disorder (CD), anxiety disorders (eg, generalized anxiety disorder, social anxiety), and depressive disorders (eg, major depression).14–17 However, most studies of ADHD and comorbid psychopathology have relied on predominantly male samples. A meta-analysis of 21 mixed-gender population studies (published between 1987 and 1999) found that children with ADHD were over 10 times more likely to have CD or ODD, whereas they were over 5 times more likely to have depression and 3 times more likely to have an anxiety disorder compared with peers without ADHD.18 Thus, studies including boys with ADHD have typically focused on comorbid externalizing disorders, such as CD and ODD. In contrast, perhaps because girls overall have higher rates of internalizing (eg, anxiety, depression) versus externalizing disorders,3,19,20 many previous studies have somewhat narrowly emphasized the association between ADHD and internalizing problems in girls. Indeed, longitudinal studies show that girls with ADHD often experience internalizing problems,21,22 and children with ADHD and comorbid depressive and/or anxiety disorders exhibit worse outcomes than youth with 1 disorder.23 At the same time, however, girls with ADHD show increased ODD, CD, and aggression as well, which uniquely predicts severe adult impairments, such as risky sexual behavior, involvement in abusive relationships, and criminality.22,24–26 Given that internalizing and externalizing psychopathology may differentially predict long-term outcomes for girls, clarifying early patterns of comorbidity in girls with ADHD is imperative to understanding the impact of childhood ADHD on adult outcomes.
To inform the clinical significance of ADHD in girls, comorbid psychopathology must be adequately characterized. Most research on girls with ADHD has compared girls (the minority group) to boys (the majority group), rather than directly comparing girls with versus without ADHD. The lack of gender-matched comparison groups potentially confounds true gender differences in the association between ADHD and comorbid disorders, which could also simply reflect gender differences in rates of psychopathology regardless of ADHD. Girls overall have higher rates of internalizing versus externalizing disorders, but it is unclear if ADHD affects these patterns; clarifying this is important for several reasons. First, because of the perception that internalizing problems are more relevant than externalizing problems for girls with ADHD, treatment of internalizing symptoms is often prioritized (eg, antidepressants), even when externalizing symptoms are present and impairing.27 Such treatment practices assume that ADHD in girls confers more risk for internalizing than externalizing symptoms. Importantly, results from previous studies of girls with versus without ADHD are mixed, with evidence that ADHD may be particularly predictive of anxiety and depression in girls28,29; alternatively, other studies suggest that ADHD poses a higher risk for externalizing disorders and that girls with ADHD have higher rates of internalizing symptoms than boys simply due to the main effect of gender.30 Similar to ADHD symptoms, externalizing behaviors in girls may reflect the gender paradox: despite its lower prevalence in girls compared with boys, externalizing symptoms are more impairing and produce worse outcomes for girls, underscoring the clinical significance of comorbid externalizing symptoms. Overall, these data suggest that narrowly focusing on internalizing disorders among girls with ADHD may undermine timely detection and treatment of externalizing problems in girls. Clarifying the relative effect of ADHD on comorbid externalizing versus internalizing disorders for girls requires direct comparison of girls with and without ADHD, the primary goal of this meta-analysis.
Given the increasing number of studies consisting of girls with and without ADHD,24,31 meta-analysis of comorbidity among girls with ADHD is timely. Thus, this meta-analysis characterized patterns of comorbid anxiety, depression, ODD, and CD among girls with versus without ADHD and also examined potential moderators of comorbidity patterns. Group differences in comorbidity rates may be sensitive to diagnostic procedures (eg, interview versus rating scale), sample characteristics (eg, age, race/ethnicity), and referral sources (eg, clinic-referred versus community-referred).32 For instance, clinic-referred samples typically exhibit elevated rates of comorbidity. Because girls with ADHD are often underreferred relative to boys, clinic-referred girls may be particularly impaired compared with nonreferred girls. Participant age is also relevant given that rates of lifetime ADHD increase from preschool to adolescence.33 Similarly, ADHD is most prevalent in non-Hispanic white children and adolescents.1 Given these divergent patterns of association, a secondary goal of this meta-analysis is to examine study characteristics that may affect estimates of comorbidity among girls with ADHD.
Methods
Search Procedure
Potential studies were identified using separate searches for each comorbid disorder (ODD, CD, anxiety, depression) in PubMed and Google Scholar. PubMed searches targeted studies with ADHD and each comorbid disorder in the title or abstract. For example, the search terms for ODD were: (ADHD OR attention-deficit hyperactivity disorder[Title/Abstract]) AND (ODD OR oppositional defiant disorder[title/abstract]). Additional PubMed filters were activated based on eligibility criteria: “Article types: Clinical Trial, Controlled Clinical Trial, Journal Article, Randomized Controlled Trial, Validation Studies; Publication dates From 1980/01/01; Species: Humans; Language: English; Sex: Female; Ages: Child: birth–18 years, Adolescent: 13–18 years, Child: 6–12 years.” Similarly, Google Scholar searches targeted studies published after 1980 that included ADHD and the comorbid disorder in the title. Sample search terms for ODD were: allintitle: (“Oppositional Defiant Disorder” OR ODD) (ADHD OR ADD OR “attention deficit hyperactivity disorder”). The final search was completed in August 2014.
Study Selection and Data Extraction
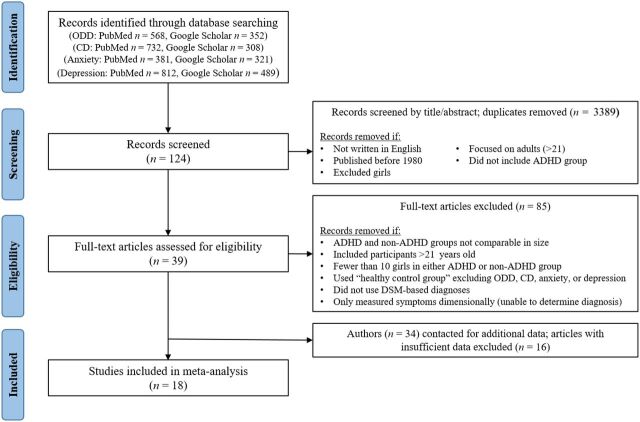
Figure 1 shows the number of citations for each disorder yielded by the initial search as well as the study selection process. Following expert recommendations, 4 coders (I.T., J.I.M., K.L.J., and J.S.K.) screened these citations based on their titles and abstracts.34 After reducing the number of studies based on broad exclusionary criteria and removing duplicates, 124 unique samples were identified and independently coded by 2 extensively trained bachelor-level coders (P.G.H. and P.M.O.) who were highly reliable (average κ = 0.84). Both in the screening and coding stages, coders met weekly with a doctoral-level supervisor (J.J.L. and/or I.T.) to resolve discrepancies. During this time, samples were additionally evaluated according to the inclusion criteria listed in Fig 1. To maximize validity, studies were required to assess ADHD and comorbid disorders using Diagnostic and Statistical Manual of Mental Disorders (DSM)-based measures. Studies that produced diagnostic categories or could reasonably be recoded into diagnostic groups were considered. For studies that described comorbidity dimensionally using DSM-based measures (n = 17), we contacted authors to request raw data to create diagnostic groups. Given the significant variability in the number and types of anxiety disorders assessed, we included studies that assessed at least 1 DSM-based anxiety disorder. For depression, we focused on studies that assessed major depression, but we also included studies based on “any depressive disorder” (eg, including dysthymia) if depressive disorders were not reported separately.
FIGURE 1.
Flowchart of study inclusion.
These procedures produced 39 unique samples that were then coded for the following information: (1) number of girls with and without ADHD and (2) number of girls with ODD, CD, any anxiety disorder, and depression (separately) for the ADHD and non-ADHD groups. For the 3 longitudinal studies, variables were coded from the first available data point. Finally, because few studies exclusively focused on girls with ADHD, most studies (n = 34) did not directly report diagnostic rates separately for girls with and without ADHD. Thus, we contacted authors to request those data. Eighteen unique studies had sufficient data for the final analyses.
Moderator Variables
To explore potential moderators of the association between ADHD and each comorbid disorder, key demographic and methodological characteristics were coded for each study. Demographic factors included: (1) participant age range (child, adolescent, both) and (2) racial/ethnic composition (% white). Methodological variables included: (1) sample source (clinic-referred, community-referred, both), (2) medication status (% medicated), (3) ADHD subtypes included (any subtype, combined only), (4) informant for ADHD and comorbid disorders (parent, child, teacher), and (5) assessment method for ADHD and comorbid disorders (interview, rating scale). Finally, publication year (eg, 2003) was included as a potential moderator.
Calculation of Effect Sizes
Odds ratios (OR) were calculated from data extracted from publications or from data provided by study authors. We estimated 4 separate effect sizes of the association between ADHD (versus non-ADHD) and the following dichotomously measured disorders: (1) ODD, (2) CD, (3), any anxiety disorder, and (4) depression. For example, to estimate the OR for ADHD versus non-ADHD for ODD, we used the formula (a + d)/(b + c), in which a = the number of girls with ADHD and ODD, b = the number of ADHD girls without ODD, c = the number of non-ADHD girls with ODD, and d = the number of non-ADHD girls without ODD. When cell frequencies equaled 0, we added 0.5 to each of the 4 cells to calculate the effect size.34
Statistical Analyses
We employed a random-effects model to estimate the OR, its 95% confidence interval (CI), and its significance. Publication bias was evaluated through visual inspection of Begg’s funnel plot,35 which plots each effect size with its SE,35 as well as using Egger’s test for funnel plot asymmetry, where significant asymmetry indicates potential publication bias.36 To adjust for bias, we implemented Duval and Tweedie’s “trim and fill” method,37 a widely used method of addressing publication bias by first “trimming” (removing) studies causing the funnel plot asymmetry and using the trimmed funnel plot to estimate the true funnel “center,” then “filling in” the funnel by replacing the removed studies and their reflected counterparts around the center to produce a new pooled estimate based on the adjusted funnel plot. Simulation studies suggest that this method improves effect size CIs and detects how much point estimates may change as a result of potentially missing studies.38 Heterogeneity in effect sizes was estimated using the Cochran Q test; for outcomes with significant heterogeneity, we tested moderation separately for each demographic or methodological factor. All data were analyzed in Stata, version 12 (Stata Corp, College Station, TX) by using the meta, metarim, and metareg commands.
Results
The final analyses included 1997 participants across 18 independent studies,10,28,39–47 described in Table 1. Although the initial search included studies published since 1980, all of the final 18 studies were published in or after 1999, with 12 studies published since 2005. Sample sizes varied (mean n = 100 girls total) with studies being more likely to include whites (mean, 77% white) and school-aged girls (mean age range, 8.5–13.5 years). Of the 18 studies, 11 included community- and clinic-referred participants, 6 used community-referred samples, and 1 exclusively featured clinic-referred youth. Most studies (n = 14) included any ADHD subtype in the ADHD group, and diagnoses were typically based on a diagnostic interview (n = 10) or a combination of interview and rating scale (n = 4). All studies used parents as informants, although some combined parent and child (n = 5) or parent and teacher report (n = 4) to establish diagnostic status. Fifteen studies used computerized and comprehensive structured diagnostic interviews (ie, Diagnostic Interview Schedule for Children, Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children, Diagnostic Interview for Children and Adolescents-IV) and 3 studies used standardized rating scales (ie, Swanson, Nolan and Pelham Parent and Teacher Rating Scales or ADHD Rating Scale IV) to diagnose DSM-IV ADHD. In addition to construct validity based on DSM symptoms, these widely used diagnostic tools also have superior psychometric properties, including test–retest reliability and convergent validity.48–50 Thus, the studies included in the meta-analysis employed rigorous diagnostic procedures to ascertain ADHD.
TABLE 1.
Demographic and Methodological Characteristics of Studies Included in the Meta-analysis
| Source | Girls (N) | Referral Source | Age Range (y) | % White | % Medicated | ADHD Subtypes | Assessment Method | Informant | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Becker et al (39) | ADHD: 45 | ADHD: community | 7–11 | 71.21 | Not provided | Any | Interview | Parent | Anxiety, depression, ODD, CD |
| Control: 25 | Control: community | ||||||||
| Bussing et al (51) | ADHD: 29 | ADHD: community | 14–21 | 59.43 | 55.17 | Any | Interview | Parent | ODD, CD |
| Control: 146 | Control: community | ||||||||
| Chang et al (52) | ADHD: 63 | ADHD: clinic | 7–13 | 97.56 | Not provided | Any | Interview | Parent | ODD, CD |
| Control: 19 | Control: community | ||||||||
| Chronis et al (40) | ADHD: 18 | ADHD: clinic/community | 4–6 | 65.22 | 10 | Any | Interview and rating scale | Parent and teacher | Anxiety, depression, ODD, CD |
| Control: 24 | Control: community | ||||||||
| Hinshaw (41) | ADHD: 140 | ADHD: clinic/community | 6–12 | 52.62 | 50.71 | Combined only | Interview | Parent | Anxiety, depression, ODD, CD |
| Control: 88 | Control: clinic/community | ||||||||
| Humphreys and Lee (42) | ADHD: 32 | ADHD: clinic/community | 5–10 | 51.56 | Not provided | Any | Interview | Parent | Anxiety, depression, ODD, CD |
| Control: 41 | Control: clinic/community | ||||||||
| Hurtig et al (53) | ADHD: 29 | ADHD: community | 16–18 | 100 | 0 | Any | Interview | Parent and child | Anxiety, depression, ODD, CD |
| Control: 69 | Control: community | ||||||||
| Kadesjö et al (54) | ADHD: 30 | ADHD: clinic | 3–7 | 100 | 0 | Any | Interview | Parent | ODD |
| Control: 16 | Control: community | ||||||||
| Laucht et al (43) | ADHD: 15 | ADHD: clinic | 14–16 | 99.4 | 60 | Any | Interview | Parent and child | Anxiety, depression, ODD, CD |
| Control: 144 | Control: clinic | ||||||||
| Martel et al (55) | ADHD: 98 | ADHD: clinic/community | 6–17 | 79.1 | Not provided | Combined only | Interview | Parent and child | ODD, CD |
| Control: 103 | Control: clinic/community | ||||||||
| Mikami et al (44) | ADHD: 11 | ADHD: clinic/community | 6–9 | 87.32 | 4 | Any | Interview and rating scale | Parent and teacher | Anxiety, depression, ODD, CD |
| Control: 60 | Control: community | ||||||||
| Mikami et al (56) | ADHD: 20 | ADHD: clinic/community | 6–10 | 85 | 65 | Combined only | Rating scale | Parent | Anxiety, depression, ODD, CD |
| Control: 20 | Control: community | ||||||||
| Ohan and Johnston (57) | ADHD: 40 | ADHD: clinic/community | 9–12 | 83 | Not provided | Any | Rating scale | Parent | ODD |
| Control: 40 | Control: clinic/community | ||||||||
| Pheula et al (45) | ADHD: 32 | ADHD: community | 6–16 | 62.5 | 43.75 | Combined only | Interview | Parent and child | Anxiety, depression, ODD, CD |
| Control: 32 | Control: community | ||||||||
| Rucklidge and Tannock (28) | ADHD: 24 | ADHD: clinic | 13–16 | Not provided | 45.8 | Any | Interview and rating scale | Parent, teacher, and child | Anxiety, depression, ODD, CD |
| Control: 28 | Control: clinic/community | ||||||||
| Sciberras et al (58) | ADHD: 22 | ADHD: clinic/community | 12–18 | Not provided | 72.73 | Any | Rating scale | Parent | ODD |
| Control: 20 | Control: community | ||||||||
| Seymour et al (46) | ADHD: 12 | ADHD: community | 10–14 | 63.33 | 66.67 | Any | Interview and rating scale | Parent and teacher | Depression, ODD, CD |
| Control: 18 | Control: community | ||||||||
| Willcutt et al (47) | ADHD: 136 | ADHD: community | 8–18 | 75 | Not provided | Any | Rating scale | Parent and teacher | Anxiety, depression, ODD, CD |
| Control: 308 | Control: community |
ADHD and ODD
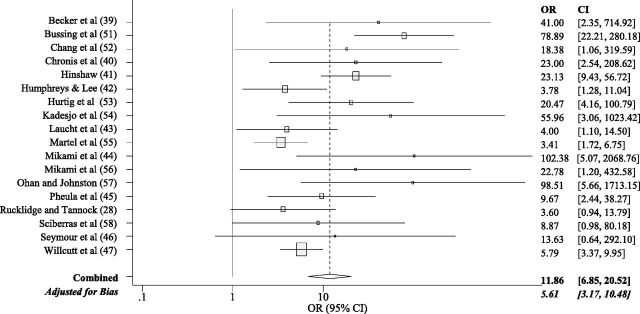
All 18 studies (n = 1997 participants) were included in this analysis. Among girls with ADHD, 42% were diagnosed with ODD relative to 5% of girls without ADHD. The initial pooled random effects OR estimated that girls with ADHD were >11 times more likely to have ODD than girls without ADHD (Fig 2). However, potential publication bias was indicated by Egger’s test (t = 2.65, P = .02) and marginally by Begg’s test (τ = 51, P = .06); the Begg’s funnel plot suggested that smaller studies were more likely to yield larger ORs for ODD than larger studies. After adjusting for potential bias using the trim and fill method, the re-estimated effect indicated that girls with ADHD were 5.6 times more likely to be diagnosed with ODD than girls without ADHD.
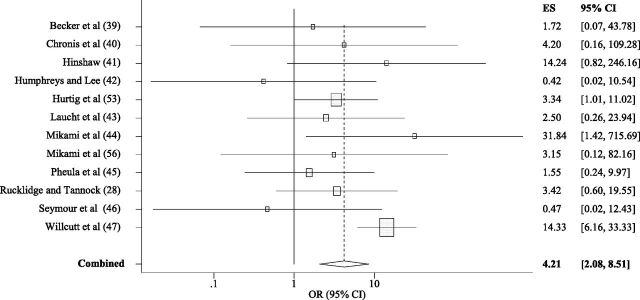
FIGURE 2.
Forest plot graphing ORs for ODD among girls with versus without ADHD. Each study is represented by 1 horizontal line and box, with location of the box on the x-axis corresponding to the point estimate for each study, and the size of the box indicating the weight (inverse of variance) of the study. The diamond and dotted vertical line depict the overall effect estimate for all 18 studies, with the width of the diamond representing the CI.
Given significant heterogeneity in effect sizes for ODD (Q = 41.51, df = 17, P < .01), we employed meta-regression to test potential moderators of heterogeneous effect sizes (Supplemental Table 2). Age, race, sample source, medication status, ADHD subtypes, assessment method, and publication year did not influence the association between ADHD and comorbid ODD. Only informant (parent, child, teacher) significantly moderated the effect; relative to parent-report only, studies that combined parent and child ratings for ADHD and ODD produced smaller effect sizes. However, there were no significant differences between parent-report only versus combined parent- and teacher-report.
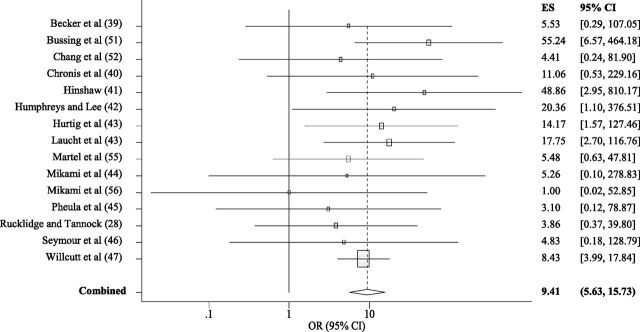
ADHD and CD
Fifteen studies were included in the meta-analysis of ADHD and CD. A total of 12.8% of girls with ADHD were diagnosed with CD relative to 0.8% of girls without ADHD. The pooled effect revealed that girls with ADHD were >9 times more likely to be diagnosed with CD than girls without ADHD (Fig 3). Egger’s (t = –0.28, P = .79) and Begg’s test (τ = –31, P = .14) did not suggest publication bias, and there was no evidence of significant heterogeneity (Q = 8.01, df = 14, P = .89).
FIGURE 3.
Forest plot graphing ORs for CD among girls with versus without ADHD. Each study is represented by 1 horizontal line and box, with location of the box on the x-axis corresponding to the point estimate for each study, and the size of the box indicating the weight (inverse of variance) of the study. The diamond and dotted vertical line depict the overall effect estimate for all 15 studies, with the width of the diamond representing the CI. ES, effect size.
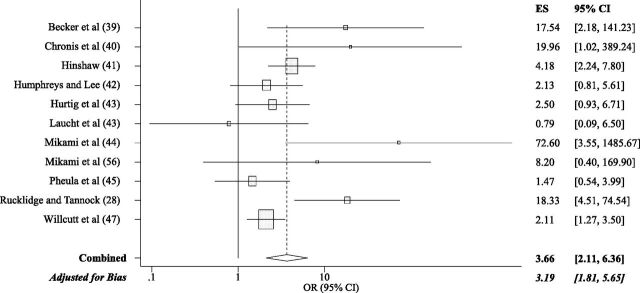
ADHD and Anxiety
Eleven studies were included in the meta-analysis of ADHD and anxiety disorders. Compared with 13.9% of girls without ADHD, 37.7% of girls with ADHD met diagnostic criteria for an anxiety disorder. Girls with ADHD were 3.66 times more likely to meet criteria for an anxiety disorder than girls without ADHD (Fig 4). Begg’s test (τ = 17, P = .21) did not suggest potential publication bias, although Egger’s test was marginal (t = 1.82, P = .10). Visual examination of Begg’s test suggested that smaller studies may be slightly more likely to report larger effects. After adjusting for potential bias using the trim and fill method, the effect size for comorbid anxiety (OR = 3.19) was relatively similar.
FIGURE 4.
Forest plot graphing ORs for anxiety among girls with versus without ADHD. Each study is represented by 1 horizontal line and box, with location of the box on the x-axis corresponding to the point estimate for each study, and the size of the box indicating the weight (inverse of variance) of the study. The diamond and dotted vertical line depict the overall effect estimate for all 11 studies, with the width of the diamond representing the CI.
Given evidence of significant heterogeneity (Q = 22.46, df = 10, P < .01), we employed meta-regression to examine potential moderators (Supplemental Table 3). Effect sizes were smaller for studies that included adolescents (versus children aged <13 years), and the association between ADHD and anxiety was larger in samples with clinic-referred girls (versus community-referred). Finally, multimethod assessments of ADHD (interview and rating scale) produced higher rates of comorbid anxiety compared with interview-only assessments. Participant race, medication status, ADHD subtypes, diagnostic informant, publication year, and the number of anxiety disorders assessed (varying from 1–7 disorders across studies) were not significant moderators.
ADHD and Depression
Twelve studies were included in the meta-analysis of ADHD and comorbid depression. A total of 10.3% of girls with ADHD were diagnosed with depression relative to 2.9% of non-ADHD girls. Girls with ADHD were >4 times more likely to be diagnosed with depression than non-ADHD girls (Fig 5). Although Begg’s test for publication bias was not significant (τ = –10, P = .54), Egger’s test marginally suggested bias (t = –2.03, P = .07); examination of Begg’s funnel plot suggested that smaller studies tended to report smaller effect sizes for depression. There was no evidence of significant heterogeneity (Q = 15.05, df = 11, P < .18).
FIGURE 5.
Forest plot graphing ORs for depression among girls with versus without ADHD. Each study is represented by 1 horizontal line and box, with location of the box on the x-axis corresponding to the point estimate for each study, and the size of the box indicating the weight (inverse of variance) of the study. The diamond and dotted vertical line depict the overall effect estimate for all 12 studies, with the width of the diamond representing the CI.
Discussion
Across 18 studies, girls with ADHD were significantly more likely to meet DSM-IV criteria for externalizing (ODD, CD) and internalizing (anxiety, depression) disorders than non-ADHD girls. Despite having generally higher rates of internalizing psychopathology relative to boys,3,19,20 this meta-analysis indicated that girls with ADHD have significantly higher odds of having comorbid CD and ODD than either anxiety or depression. Overall, effect sizes for ADHD and comorbid CD and depression were consistent across studies, but heterogeneity was observed for ODD and anxiety. The effect of ADHD on comorbid anxiety was larger in studies with clinic-referred (versus community-referred) girls, using diagnostic methods that combined interview and rating scale, and including children aged <13 years only (versus adolescents). The effect of ADHD on ODD was moderated by informant, with smaller effects for studies employing child self-report in addition to parent-report. We observed evidence of potential publication bias where studies with smaller samples reported larger effect sizes for ODD and, to a lesser extent, anxiety.59 Effect sizes were unaffected by sample racial/ethnic composition, ADHD subtypes, and study publication year. These findings suggest that girls with ADHD are at substantially higher odds for comorbid externalizing and internalizing disorders than girls without ADHD.
The high rate of comorbid anxiety disorders (37.7%) and relatively lower rate of comorbid CD (12.8%) among girls with ADHD is consistent with previous studies comparing girls to boys with ADHD.30,60,61 However, compared with girls without ADHD, girls with ADHD were most likely to have comorbid CD (9.4 times) and ODD (5.6 times), followed by depression (4.2 times) and anxiety (3.2 times). The finding that ADHD posed higher odds for comorbid externalizing than internalizing disorders is consistent with a previous meta-analysis of mixed-gender studies,18 suggesting that patterns of comorbidity in boys and girls with ADHD are comparable. Although CD is less prevalent in girls than boys, girls with ADHD were >9 times more likely to be diagnosed with CD than non-ADHD girls. Importantly, compared with girls with ADHD only, girls with ADHD and comorbid ODD and/or CD symptoms have particularly poor health and behavioral outcomes (eg, risky sexual behaviors).6,62,63 Furthermore, because of the perception that girls with ADHD exhibit fewer behavior problems than boys, girls who are clinic-referred for ADHD are often treated for their internalizing symptoms, even when externalizing symptoms are also evident.27 Given the substantial odds that ADHD poses to girls for externalizing problems in this meta-analysis, careful assessment of early ADHD and ODD/CD in girls should be emphasized in clinical settings to facilitate early intervention of ADHD and comorbid externalizing symptoms to prevent later negative outcomes.
These meta-analytic results suggest that, compared with girls without ADHD, girls with ADHD have significantly higher odds of having a comorbid externalizing disorder than an internalizing disorder. The pathways of risk for developing internalizing disorders among girls with ADHD may be due to individual and environmental factors that are independent of their ADHD, such as cognitive factors (eg, perceived control), temperament (eg, inhibition), and unique family factors (eg, parental overprotectiveness).64–66 Thus, future studies should focus on understanding the factors that independently contribute to anxiety and depression for girls beyond those associated with ADHD. In addition to the direct treatment of ADHD symptoms in girls, reduction of comorbid internalizing psychopathology likely necessitates more complex treatment plans that separately target anxiety/depression symptoms (eg, cognitive behavioral therapy).67
Significant variability in effect sizes was observed across studies for ADHD with ODD and anxiety disorders. No single moderator explained the heterogeneity in effect sizes for ODD and anxiety; moderators were disorder-specific. Compared with studies relying on parent-report only, studies that combined parent and child reports yielded smaller effect sizes of the association between ADHD and ODD, but no differences were observed between parent and teacher reports. This is consistent with lower rates of youth self-reported psychopathology compared with parent- and teacher-report.68 Studies including clinic-referred girls reported stronger associations between ADHD and anxiety, whereas combined diagnostic methods (interview and rating scale) yielded higher effect sizes for anxiety than interview-only methods. Finally, girls with ADHD in samples including adolescents (versus children aged <13 years) had lower rates of comorbid anxiety, which is somewhat surprising given that anxiety generally increases with age.69 The present findings may reflect that samples exclusively focused on childhood assess different types of anxiety disorders (eg, separation anxiety, specific phobia) compared with other forms of anxiety (eg, generalized anxiety); however, the number of anxiety disorders assessed among studies did not influence effect sizes of ADHD and anxiety.
These findings were derived from cross-sectional studies, thus precluding causal inferences. It is unclear how variability in ADHD symptoms across development prospectively affects adult psychopathology, an important area of inquiry given the frequent persistence of ADHD. For example, rates of depression and CD were less prevalent in the non-ADHD groups compared with epidemiologic samples, which likely reflects the relative youth of study participants (versus adolescents or adults). Given that the median age of onset for CD and depression is in early adolescence and young adulthood,70 respectively, studies must include a full range of development to clarify how patterns of comorbidity change over time. Especially for girls, ADHD may be particularly salient in initiating cascading effects that lead to long-term impairments because of the elevated stigma associated with the disorder.10,11 Thus, longitudinal studies are necessary to describe the developmental outcomes of girls with and without ADHD.
Importantly, an accurate estimation of comorbidity in girls with ADHD depends on knowing the true prevalence of ADHD in girls, a critical issue that remains largely unresolved.29,71 Some studies suggest that ADHD may be underdiagnosed in girls,27,72 whereas others suggest that ADHD is overdiagnosed in boys.73 The assumption of underdiagnosis of ADHD in girls may suggest that the comorbidity estimates derived in this study are inflated, because they are based on girls with particularly severe (ie, impairing) ADHD symptoms. Alternatively, it is also possible that rates of psychopathology in girls without ADHD were underestimated because these girls were more likely to be drawn from community versus clinical samples compared with girls with ADHD. Furthermore, relative to girls, boys with ADHD are more likely to be referred for treatment, reflecting a general delay in recognizing, diagnosing, and treating ADHD in girls that contributes to more severe symptoms among referred girls.74 This is consistent with the present findings that clinic-referred samples reported higher rates of comorbid anxiety than community-referred samples, although this was not the case for comorbid ODD, CD, or depression. Thus, despite our findings that indicate substantially higher odds for comorbidity among girls with versus without ADHD, securing the true estimates of comorbidity for girls with ADHD demands first improving diagnostic accuracy of childhood ADHD in girls.
Furthermore, although this meta-analysis included any subtype of ADHD, and studies did not consistently report subtype differences for girls, the number of children with the inattentive subtype may be higher in community samples, whereas combined type cases are more common in clinic-referred samples.60,75 Because inattention may be specifically linked to separation anxiety,76 whereas hyperactivity predicts more externalizing problems,77 generalized anxiety disorder,76 and suicide attempts and self-injury,5 clarifying these differential associations has important implications for the assessment of ADHD and prevention of psychopathology. Future studies that directly explore ADHD subtypes and comorbidity patterns will elucidate how inattention and hyperactivity may differentially relate to comorbid psychopathology in girls.
This meta-analysis provides the first formal characterization that girls with ADHD are at substantially higher odds for comorbid CD, ODD, depression, and anxiety disorders compared with girls without ADHD. Given the rising prevalence and significant impairment of ADHD among girls,78 these findings attest to the need for increased scientific and clinical efforts to improve the diagnosis and treatment of girls with ADHD. Furthermore, these meta-analytic findings suggest that ADHD poses particularly higher odds for comorbid externalizing compared with internalizing disorders in girls. Careful assessment of early ADHD and ODD/CD in girls should be emphasized in clinical settings to facilitate early intervention and to prevent later negative outcomes associated with externalizing behaviors. Future longitudinal studies that investigate the developmental course of these associations are necessary to identifying the putative mechanisms underlying pathways between ADHD and other psychopathology in girls.
Supplementary Material
Acknowledgments
This research was partially supported by a National Science Foundation graduate research fellowship awarded to Ms Tung.
We thank the authors of the studies who provided additional data for this meta-analysis.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- CD
conduct disorder
- CI
confidence interval
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ODD
oppositional defiant disorder
- OR
odds ratio
Footnotes
Ms Tung collected and coded studies for inclusion, supervised the acquisition of data, carried out the analyses, and drafted the initial manuscript; Dr Li conceptualized and designed the study, supervised the acquisition of data, assisted with interpretation of analyses, and critically reviewed and revised the manuscript; Ms Meza and Ms Jezior collected and coded the studies for inclusion, assisted with drafting the initial manuscript, and reviewed and revised the manuscript; Ms Kianmahd, Mr Hentschel, and Mr O’Neil collected and coded the studies for inclusion and reviewed and revised the manuscript; Dr Lee supervised the acquisition of data, assisted with interpretation of analyses, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FUNDING: No external funding.
References
- 1.Visser SN, Zablotsky B, Holbrook JR, Danielson ML, Bitsko RH. Diagnostic experiences of children with attention-deficit/hyperactivity disorder. Natl Health Stat Rep. 2015; No. 81:1–7 [PubMed] [Google Scholar]
- 2.Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34–46.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association (APA) . Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington: American Psychiatric Association; 2000 [Google Scholar]
- 4.Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet. 2005;366(9481):237–248 [DOI] [PubMed] [Google Scholar]
- 5.Hinshaw SP, Owens EB, Zalecki C, et al. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. J Consult Clin Psychol. 2012;80(6):1041–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lehti V, Niemelä S, Heinze M, et al. Childhood predictors of becoming a teenage mother among Finnish girls. Acta Obstet Gynecol Scand. 2012;91(11):1319–1325 [DOI] [PubMed] [Google Scholar]
- 7.Thurber JR, Heller TL, Hinshaw SP. The social behaviors and peer expectation of girls with attention deficit hyperactivity disorder and comparison girls. J Clin Child Adolesc Psychol. 2002;31(4):443–452 [DOI] [PubMed] [Google Scholar]
- 8.Young S, Heptinstall E, Sonuga-Barke EJS, Chadwick O, Taylor E. The adolescent outcome of hyperactive girls: self-report of psychosocial status. J Child Psychol Psychiatry. 2005;46(3):255–262 [DOI] [PubMed] [Google Scholar]
- 9.Newcorn JH, Halperin JM, Jensen PS, et al. Symptom profiles in children with ADHD: effects of comorbidity and gender. J Am Acad Child Adolesc Psychiatry. 2001;40(2):137–146 [DOI] [PubMed] [Google Scholar]
- 10.Mikami AY, Lorenzi J. Gender and conduct problems predict peer functioning among children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40(5):777–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elkins IJ, Malone S, Keyes M, Iacono WG, McGue M. The impact of attention-deficit/hyperactivity disorder on preadolescent adjustment may be greater for girls than for boys. J Clin Child Adolesc Psychol. 2011;40(4):532–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eme RF. Selective females affliction in the developmental disorders of childhood: A literature review. J Clin Child Psychol. 1992;21(4):354–364 [Google Scholar]
- 13.Loeber R, Keenan K. Interaction between conduct disorder and its comorbid conditions: Effects of age and gender. Clin Psychol Rev. 1994;14(6):497–523 [Google Scholar]
- 14.Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jensen PS, Hinshaw SP, Kraemer HC, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry. 2001;40(2):147–158 [DOI] [PubMed] [Google Scholar]
- 16.Mitchison GM, Njardvik U. Prevalence and gender differences of ODD, anxiety, and depression in a sample of children with ADHD [published online ahead of print October 5, 2015]. J Atten Disord. doi:10.1177/1087054715608442 [DOI] [PubMed] [Google Scholar]
- 17.Pliszka SR. Patterns of psychiatric comorbidity with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2000;9(3):525–540, vii [PubMed] [Google Scholar]
- 18.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87 [PubMed] [Google Scholar]
- 19.Bongers IL, Koot HM, van der Ende J, Verhulst FC. The normative development of child and adolescent problem behavior. J Abnorm Psychol. 2003;112(2):179–192 [DOI] [PubMed] [Google Scholar]
- 20.Martel MM. Individual differences in attention deficit hyperactivity disorder symptoms and associated executive dysfunction and traits: sex, ethnicity, and family income. Am J Orthopsychiatry. 2013;83(2 Pt 3):165–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biederman J, Ball SW, Monuteaux MC, et al. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry. 2008;47(4):426–434 [DOI] [PubMed] [Google Scholar]
- 22.Biederman J, Petty CR, Monuteaux MC, et al. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. Am J Psychiatry. 2010;167(4):409–417 [DOI] [PubMed] [Google Scholar]
- 23.Daviss WB. A review of co-morbid depression in pediatric ADHD: etiology, phenomenology, and treatment. J Child Adolesc Psychopharmacol. 2008;18(6):565–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Monuteaux MC, Faraone SV, Michelle Gross L, Biederman J. Predictors, clinical characteristics, and outcome of conduct disorder in girls with attention-deficit/hyperactivity disorder: a longitudinal study. Psychol Med. 2007;37(12):1731–1741 [DOI] [PubMed] [Google Scholar]
- 25.Biederman J, Petty CR, Monuteaux MC, et al. The longitudinal course of comorbid oppositional defiant disorder in girls with attention-deficit/hyperactivity disorder: findings from a controlled 5-year prospective longitudinal follow-up study. J Dev Behav Pediatr. 2008;29(6):501–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moretti MM, Catchpole REH, Odgers C. The dark side of girlhood: recent trends, risk factors and trajectories to aggression and violence. Can Child Adolesc Psychiatr Rev. 2005;14(1):21–25 [PMC free article] [PubMed] [Google Scholar]
- 27.Quinn P, Wigal S. Perceptions of girls and ADHD: results from a national survey. MedGenMed. 2004;6(2):2. [PMC free article] [PubMed] [Google Scholar]
- 28.Rucklidge JJ, Tannock R. Psychiatric, psychosocial, and cognitive functioning of female adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2001;40(5):530–540 [DOI] [PubMed] [Google Scholar]
- 29.Skogli EW, Teicher MH, Andersen PN, Hovik KT, Øie M. ADHD in girls and boys--gender differences in co-existing symptoms and executive function measures. BMC Psychiatry. 2013;13:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biederman J, Mick E, Faraone SV, et al. Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry. 2002;159(1):36–42 [DOI] [PubMed] [Google Scholar]
- 31.Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74(3):489–499 [DOI] [PubMed] [Google Scholar]
- 32.Abikoff H, Klein RG. Attention-deficit hyperactivity and conduct disorder: comorbidity and implications for treatment. J Consult Clin Psychol. 1992;60(6):881–892 [DOI] [PubMed] [Google Scholar]
- 33.Pastor P, Reuben C, Duran C, Hawkins L. Association between diagnosed ADHD and selected characteristics among children aged 4-17 years: United States, 2011-2013. NCHS Data Brief. 2015;No. 201 [PubMed] [Google Scholar]
- 34.Lipsey MW, Wilson DW. Practical Meta-Analysis. Vol 49. New York: Sage; 2001 [Google Scholar]
- 35.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101 [PubMed] [Google Scholar]
- 36.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463 [DOI] [PubMed] [Google Scholar]
- 38.Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98 [Google Scholar]
- 39.Becker SP, Langberg JM, Vaughn AJ, Epstein JN. Clinical utility of the Vanderbilt ADHD diagnostic parent rating scale comorbidity screening scales. J Dev Behav Pediatr. 2012;33(3):221–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chronis AM, Lahey BB, Pelham WE Jr, Kipp HL, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2003;42(12):1424–1432 [DOI] [PubMed] [Google Scholar]
- 41.Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. J Consult Clin Psychol. 2002;70(5):1086–1098 [DOI] [PubMed] [Google Scholar]
- 42.Humphreys KL, Lee SS. Risk taking and sensitivity to punishment in children with ADHD, ODD, ADHD+ODD, and controls. J Psychopathol Behav Assess. 2011;33(3):299–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laucht M, Hohm E, Esser G, Schmidt MH, Becker K. Association between ADHD and smoking in adolescence: Shared genetic, environmental and psychopathological factors. J Neural Transm (Vienna). 2007;114(8):1097–1104 [DOI] [PubMed] [Google Scholar]
- 44.Mikami AY, Griggs MS, Lerner MD, et al. A randomized trial of a classroom intervention to increase peers’ social inclusion of children with attention-deficit/hyperactivity disorder. J Consult Clin Psychol. 2013;81(1):100–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pheula GF, Rohde LA, Schmitz M. Are family variables associated with ADHD, inattentive type? A case-control study in schools. Eur Child Adolesc Psychiatry. 2011;20(3):137–145 [DOI] [PubMed] [Google Scholar]
- 46.Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T. Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. J Abnorm Child Psychol. 2012;40(4):595–606 [DOI] [PubMed] [Google Scholar]
- 47.Willcutt EG, Pennington BF, Chhabildas NA, Friedman MC, Alexander J. Psychiatric comorbidity associated with DSM-IV ADHD in a nonreferred sample of twins. J Am Acad Child Adolesc Psychiatry. 1999;38(11):1355–1362 [DOI] [PubMed] [Google Scholar]
- 48.Collett BR, Ohan JL, Myers KM. Ten-year review of rating scales. V: scales assessing attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2003;42(9):1015–1037 [DOI] [PubMed] [Google Scholar]
- 49.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988 [DOI] [PubMed] [Google Scholar]
- 50.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38 [DOI] [PubMed] [Google Scholar]
- 51.Bussing R, Mason DM, Bell L, Porter P, Garvan C. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J Am Acad Child Adolesc Psychiatry. 2010;49(6):595–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang HT, Klorman R, Shaywitz SE, et al. Paired-associate learning in attention-deficit/hyperactivity disorder as a function of hyperactivity-impulsivity and oppositional defiant disorder. J Abnorm Child Psychol. 1999;27(3):237–245 [DOI] [PubMed] [Google Scholar]
- 53.Hurtig T, Ebeling H, Taanila A, et al. ADHD and comorbid disorders in relation to family environment and symptom severity. Eur Child Adolesc Psychiatry. 2007;16(6):362–369 [DOI] [PubMed] [Google Scholar]
- 54.Kadesjö C, Hägglöf B, Kadesjö B, Gillberg C. Attention-deficit-hyperactivity disorder with and without oppositional defiant disorder in 3- to 7-year-old children. Dev Med Child Neurol. 2003;45(10):693–699 [DOI] [PubMed] [Google Scholar]
- 55.Martel MM, Nikolas M, Jernigan K, Friderici K, Waldman I, Nigg JT. The dopamine receptor D4 gene (DRD4) moderates family environmental effects on ADHD. J Abnorm Child Psychol. 2011;39(1):1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mikami AY, Jack A, Emeh CC, Stephens HF. Parental influence on children with attention-deficit/hyperactivity disorder: I. Relationships between parent behaviors and child peer status. J Abnorm Child Psychol. 2010;38(6):721–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ohan JL, Johnston C. Gender appropriateness of symptom criteria for attention-deficit/hyperactivity disorder, oppositional-defiant disorder, and conduct disorder. Child Psychiatry Hum Dev. 2005;35(4):359–381 [DOI] [PubMed] [Google Scholar]
- 58.Sciberras E, Ohan J, Anderson V. Bullying and peer victimisation in adolescent girls with attention-deficit/hyperactivity disorder. Child Psychiatry Hum Dev. 2012;43(2):254–270 [DOI] [PubMed] [Google Scholar]
- 59.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323(7304):101–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1036–1045 [DOI] [PubMed] [Google Scholar]
- 61.Nøvik TS, Hervas A, Ralston SJ, Dalsgaard S, Rodrigues Pereira R, Lorenzo MJ; ADORE Study Group . Influence of gender on attention-deficit/hyperactivity disorder in Europe--ADORE. Eur Child Adolesc Psychiatry. 2006;15(suppl 1):I15–I24 [DOI] [PubMed] [Google Scholar]
- 62.Flory K, Molina BSG, Pelham WE Jr, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. J Clin Child Adolesc Psychol. 2006;35(4):571–577 [DOI] [PubMed] [Google Scholar]
- 63.Sarver DE, McCart MR, Sheidow AJ, Letourneau EJ. ADHD and risky sexual behavior in adolescents: conduct problems and substance use as mediators of risk. J Child Psychol Psychiatry. 2014;55(12):1345–1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chorpita BF, Brown TA, Barlow DH. Perceived control as a mediator of family environment in etiological models of childhood anxiety. Behav Ther. 1998;29(3):457–476 [DOI] [PubMed] [Google Scholar]
- 65.Degnan KA, Almas AN, Fox NA. Temperament and the environment in the etiology of childhood anxiety. J Child Psychol Psychiatry. 2010;51(4):497–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: origins and treatment. Annu Rev Clin Psychol. 2009;5(1):311–341 [DOI] [PubMed] [Google Scholar]
- 67.Bowen R, Chavira DA, Bailey K, Stein MT, Stein MB. Nature of anxiety comorbid with attention deficit hyperactivity disorder in children from a pediatric primary care setting. Psychiatry Res. 2008;157(1-3):201–209 [DOI] [PubMed] [Google Scholar]
- 68.Youngstrom EA, Findling RL, Calabrese JR. Who are the comorbid adolescents? Agreement between psychiatric diagnosis, youth, parent, and teacher report. J Abnorm Child Psychol. 2003;31(3):231–245 [DOI] [PubMed] [Google Scholar]
- 69.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176 [PMC free article] [PubMed] [Google Scholar]
- 71.Quinn PO, Madhoo M. A review of attention-deficit/hyperactivity disorder in women and girls: uncovering this hidden diagnosis. Prim Care Companion CNS Disord. 2014;16(3):PCC.13r01596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Biederman J, Faraone SV, Spencer T, Wilens T, Mick E, Lapey KA. Gender differences in a sample of adults with attention deficit hyperactivity disorder. Psychiatry Res. 1994;53(1):13–29 [DOI] [PubMed] [Google Scholar]
- 73.Bruchmüller K, Margraf J, Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J Consult Clin Psychol. 2012;80(1):128–138 [DOI] [PubMed] [Google Scholar]
- 74.Ohan JL, Visser TAW. Why is there a gender gap in children presenting for attention deficit/hyperactivity disorder services? J Clin Child Adolesc Psychol. 2009;38(5):650–660 [DOI] [PubMed] [Google Scholar]
- 75.Carlson CL, Mann M. Attention-deficit/hyperactivity disorder, predominantly inattentive subtype. Child Adolesc Psychiatr Clin N Am. 2000;9(3):499–510, vi [PubMed] [Google Scholar]
- 76.Levy F, Hay DA, Bennett KS, McStephen M. Gender differences in ADHD subtype comorbidity. J Am Acad Child Adolesc Psychiatry. 2005;44(4):368–376 [DOI] [PubMed] [Google Scholar]
- 77.Grevet EH, Bau CHD, Salgado CAI, et al. Lack of gender effects on subtype outcomes in adults with attention-deficit/hyperactivity disorder: support for the validity of subtypes. Eur Arch Psychiatry Clin Neurosci. 2006;256(5):311–319 [DOI] [PubMed] [Google Scholar]
- 78.Collins KP, Cleary SD. Racial and ethnic disparities in parent-reported diagnosis of ADHD: national survey of children’s health (2003, 2007, and 2011). J Clin Psychiatry. 2016;77(1):52–59 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.