Abstract
BACKGROUND:
Changes in health care delivery create opportunities to improve systems to better meet the needs of low-income families while achieving quality benchmarks.
METHODS:
Families of healthy newborns receiving primary care at a single large urban safety-net hospital participated. Intervention families were randomly assigned a family specialist who provided support until the 6-month routine health care visit. The Developmental Understanding and Legal Collaboration for Everyone (DULCE) intervention is based on the Strengthening Families approach and incorporated components of the Healthy Steps and Medical-Legal Partnership models. Medical record reviews determined use of preventive and emergency care. Surveys conducted at baseline, postintervention (6 months), and follow-up (12 months) were used to determine hardship and attainment of concrete supports.
RESULTS:
Three hundred thirty families participated in the study. At baseline, 73% of families reported economic hardships. Intervention parents had an average of 14 contacts with the family specialist, and 5 hours of total contact time. Intervention infants were more likely to have completed their 6-month immunization schedule by age 7 months (77% vs 63%, P < .005) and by 8 months (88% vs 77%, P < .01). Intervention infants were more likely to have 5 or more routine preventive care visits by age 1 year (78% vs 67%, P < .01) and were less likely to have visited the emergency department by age 6 months (37% vs 49.7%, P < .03). The DULCE intervention accelerated access to concrete resources (P = .029).
CONCLUSIONS:
Assignment to the Project DULCE intervention led to improvements in preventive health care delivery and utilization and accelerated access to concrete supports among low-income families.
What’s Known on This Subject:
US parents trust the health care system and bring their infant children in for preventive care. Previous studies have demonstrated the ability of health care systems to identify, and sometimes address, the economic needs of low-income families.
What This Study Adds:
Families of newborns at a safety-net primary care center have high levels of economic hardship. Compared with controls, Developmental Understanding and Legal Collaboration for Everyone families had accelerated access to concrete supports, improved rates of on-time immunization and preventive care, and decreased emergency department utilization.
As policy changes enable low-income families to gain insurance, the health care system has begun to adapt to the challenge of meeting their specific needs while also attaining quality benchmarks for preventive care. 1 – 4 As a result, health care systems have also begun to address the social determinants of health that play a powerful role in the health trajectories of children living in poverty. 5 , 6
Poverty affects children both directly, when material needs are not met, and indirectly, through amplifying family stress. Children’s health suffers when basic needs such as food, 7 – 12 housing, 13 , 14 and utilities 15 , 16 are not met. Adverse impacts include low weight for age, developmental concerns and behavioral problems, higher risk of hospitalization, and overall poor health as rated by parents. Hardships resulting from inadequate resources to meet basic needs may coexist in >1 domain, and have cumulative impacts on child health. 17 – 20 The health effects of poverty on US children have led the American Academy of Pediatrics to address “child poverty and well-being” as 1 of its current strategic priorities. 21
In addition to the direct health outcomes, economic hardship leads to increased risk for child maltreatment. 22 , 23 As shown in Fig 1, the family stress model 24 suggests that economic hardship leads indirectly to child abuse and neglect.
FIGURE 1.
Theoretical framework. Adapted from Barnett, 17 DULCE leveraged support from MLP | Boston to address upstream factors: food, housing, and utilities hardship, and to identify and support other family legal needs. This intervention was designed to reduce overall family economic pressure and the resultant downstream results.
Abuse and neglect themselves result in harm to child and adult health; the aggregate long-term consequences of a single year’s child maltreatment in the United States have lifetime direct health care costs estimated at over $150 billion. 25 Meeting basic needs for food and housing has been identified as a key strategy in preventing child abuse and neglect through the promotion of protective factors. 26
Poverty also adversely affects the ability of the health care system to address large disparities in the delivery of preventive medical services, which continue to be observed, 27 even though virtually all US children have access to primary care. 3 Some elements of the solution have already been demonstrated: care coordination in the context of the patient-centered medical homes improves health care delivery for children with and without special health care needs. 28 Although a positive association between visit time and delivery of preventive services has been demonstrated, 29 nearly 80% of routine visits involve fewer than 20 minutes of face-to-face time with a medical provider.
This report describes the outcomes of a randomized trial of a new approach to improve care of newborns and their families, Project Developmental Understanding and Legal Collaboration for Everyone (DULCE). DULCE implemented the Strengthening Families approach 26 in a pediatric primary care setting by developing a new program based on previous efforts: the evidence-based Healthy Steps 30 , 31 and Medical-Legal Partnership (MLP) 32 – 34 models.
The DULCE intervention model focused on the time from birth to age 6 months. This age group was selected for several reasons: (1) nearly all US infants are seen in a primary care setting, and up to 5 health care visits are recommended; (2) the birth of a child inevitably changes family relationships and may accentuate existing economic hardships; and (3) the first 6 months of life is a high risk period for serious and lethal child abuse.
As a novel intervention, it was important to ensure that this new service did not diminish the ability of the setting to deliver high quality care. Children’s health care quality metrics include well-child visits during the first 15 months of life, childhood immunization status, and emergency department (ED) visits. 2 , 35 , 36 DULCE tested the hypothesis that the addition of a trained family specialist (FS) in the infants’ health care setting would be able to both support families and facilitate measurable improvements in health care quality.
Methods
Setting
This intervention occurred in the pediatric primary care clinic at a major urban teaching hospital. The practice serves over 11 000 children, the majority of whom (83%) were covered by Medicaid, Medicaid managed care, or other state-subsidized plans. At the time of the study, this state had universal health insurance.
Parents of all eligible newborns younger than 10 weeks of age who presented for pediatric primary care at the clinic were recruited to participate in a randomized controlled trial from February 2010 to September 2012, with data collection completed by November 2013. Approval for this study was obtained from the Boston University Medical Campus Institutional Review Board. Families were excluded if the parent was younger than 18 years old, received medical care in a language other than English or Spanish, intended to change their primary care provider from the study site within the first 6 months of life, or if the infant had been hospitalized for >1 week after birth. Immediately after consent was obtained, the research assistant opened an opaque envelope and assigned families to control or intervention conditions. Subjects were randomly assigned in blocks of 10. Control group families were offered an unrelated infant safety intervention. Although data collection was masked as to group assignment, participants were aware of their group assignment.
Intervention
In addition to usual care, families randomly assigned to the intervention group were assigned to a DULCE FS. FSs had postgraduate training in child development or a related field and underwent additional training by the Healthy Steps National Director and the staff of MLP | Boston (the nation’s founding MLP site). All cases were discussed in weekly case conferences that included the Healthy Steps Director, an MLP | Boston staff member, and a primary care pediatrician. The intervention itself consisted of 3 types of patient contact: (1) collaborative routine visits with the family, the medical provider, and the FS; (2) home visits by the FS; and (3) contact with the FS by telephone, e-mail, text, or in person. Further details of the staff recruitment and training, and the content of the intervention are described elsewhere 37 and may be obtained online (http://www.bmc.org/Project-DULCE.htm).
Data Collection
Surveys were administered in our general clinical research center by trained research staff who were not involved in the intervention and were not informed of the participant’s group assignment. Assessments, conducted in English or Spanish, were administered at baseline, after the 6-month well-child visit (postintervention), and after the child turned 12 months of age (follow-up). Items concerning family hardship were adapted from the Fragile Families study 38 with the addition of an item regarding telephone service. Initial findings indicated that some resources were available quickly, whereas others involved long waiting lists. Before data collection and analysis, the pediatric clinic’s 2 primary care social workers classified types of support as being “likely,” “possible,” or “impossible” for families to obtain within 6 months. Receipt of concrete supports (ie, food stamps, utilities assistance, or a housing voucher) was measured by participant self-report: respondents were asked whether they had heard about, attempted to get, or received specific resources. See results for a complete list of benefits assessed.
All MLP advocate communications with the FS and all of MLP’s work performed on behalf of intervention families were recorded in the MLP | Boston case management database. This database was also used to identify all MLP referrals from the practice site. FS activity was measured through analysis of an electronic activity log in which DULCE FSs recorded each participant contact.
Immunization and ED utilization data were obtained from the electronic health record. Immunization data were computed by using the age in days at the time of administration of the infant’s third diphtheria-tetanus-acellular pertussis (DTaP) immunization (per the 6-month recommended vaccine schedule), including any combined immunization preparation, and age in days at the time of administration of first measles-mumps-rubella immunization (per the 12-month recommended vaccine schedule 39 ).
The total number of infants who had at least 1 ED visit recorded in the medical record and the total number of ED visits were analyzed. Visits to EDs at other hospitals were not consistently captured in the medical record and were not included in analyses.
Statistical Analysis
Descriptive statistics were generated as means and SDs for continuous variables and counts with percentages for categorical variables. Bivariate analyses comparing the study groups were conducted by using cross-tabulations with χ2 tests for categorical variables and 2-sample t tests for continuous variables. Means for measures repeated over time per subject were compared between the study groups by using mixed linear models. The intention-to-treat principle was applied in all comparative analyses. All statistical analyses were conducted by using SAS version 9.3 (SAS Institute, Inc, Cary, NC).
P values < .05 were deemed throughout as statistically significant.
Results
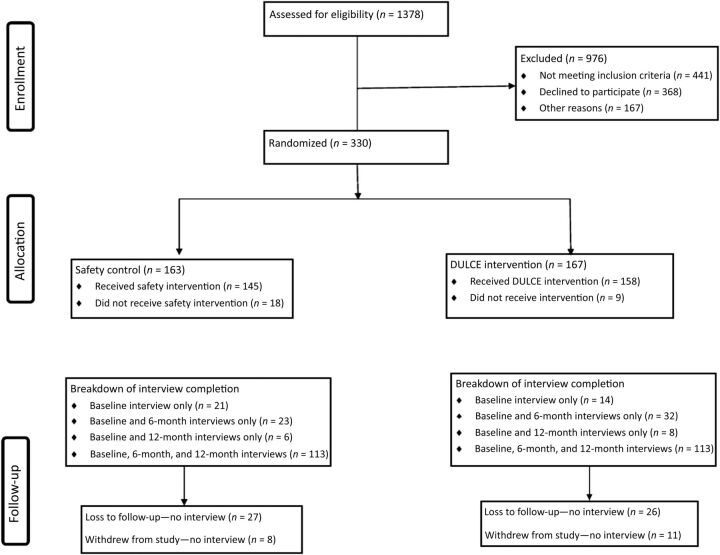
Figure 2 shows the Consolidated Standards of Reporting Trials diagram, illustrating that 1378 infant families were screened for recruitment. Infants were excluded if they spent more than 7 days in the hospital after birth (102 infants) or had a maltreatment report filed before recruitment (50 infants). Families who had a parent who was younger than 18 years of age (19 families), who intended to leave the primary care practice within 6 months of birth (76 families), who received other home visiting services (35 families), or who did not receive pediatric medical care in either English or Spanish (149 families) were excluded. Parents who consented but did not complete baseline assessments were excluded (68 families: 31 intervention and 37 control) from all analyses. Of these, 23 (31.5%) notified us of their decision to withdraw before baseline, and 12 (9.6%) transferred their infant’s primary care to another primary care site before completing baseline assessment.
FIGURE 2.
DULCE Consolidated Standards of Reporting Trials diagram showing flow of participants from initial assessment through data analysis. Please see text for detailed explanation.
Baseline data were obtained from 330 families, including 163 control families and 167 intervention families. Table 1 describes the population demographics of participants. As shown, there were no significant differences between intervention and control families. The study population was largely African-American; 12% of families reported that they were originally from Africa or the Caribbean. Ninety-three percent of parent participants were the infant’s mothers; the remaining participants were fathers. The median age of participants was 29 years. This was the first child for half of the enrolled families. The median household income for participants was in the $10 000 to $30 000 range. Two-thirds of respondents reported an annual household income of $30 000 or less, including 36% who reported annual income of $10 000 or less. Fifty-nine percent of respondents reported being unemployed (as opposed to being on maternity or parental leave) at the time of the survey. Race, ethnicity, and insurance status of the population recruited generally reflected the population served at the practice.
TABLE 1.
Participant Demographics
| Total, N = 330, % | Intervention, N = 167, % | Control, N = 163, % | |
|---|---|---|---|
| Parent gender | |||
| Woman | 93.0 | 92.8 | 93.3 |
| Parent race/ethnicity | |||
| African American/Black | 55.5 | 55.1 | 55.8 |
| Caucasian, White, or European American | 8. 5 | 6.6 | 10.4 |
| Hispanic or Latino | 12.4 | 15.6 | 9.2 |
| Other (includes multiracial, biracial, Caribbean islander, or African national) | 23.6 | 22.8 | 24.5 |
| Parent age, y | |||
| 18–24 | 27.0 | 25.2 | 28.8 |
| 25–29 | 27.9 | 28.1 | 27.6 |
| 30–34 | 27.9 | 32.3 | 23.3 |
| >34 | 17.3 | 14.4 | 20.3 |
| Marital status | |||
| Never married | 43.6 | 41.3 | 46.0 |
| Married to father or mother of child in project | 31.5 | 34.7 | 28.2 |
| Not married but living with the father or mother of child in project | 12.4 | 13.2 | 11.7 |
| Other (includes divorced, separated, married but not to father/mother of child, not married but living with boyfriend, girlfriend, partner who is not the parent of the child in the project) | 12.4 | 10.8 | 14.1 |
| Education | |||
| Less than high school graduation | 9.4 | 9.6 | 9.2 |
| Completed high school or earned GED | 48.5 | 50.3 | 46.6 |
| Completed trade/technical school; received 2-y college degree (Associate’s) | 23.0 | 24.6 | 21.5 |
| Received 4-y college degree (Bachelor’s); received a graduate degree | 19.1 | 15.6 | 22.7 |
| Employment status | |||
| Unemployed | 59.1 | 62.3 | 55.8 |
| Employed | 40.9 | 37.7 | 44.2 |
| Household income | |||
| $0–$10 000 | 36.3 | 40.9 | 31.6 |
| $10 000–$30 000 | 30.3 | 28.3 | 32.3 |
| $30 000–$50 000 | 17.2 | 17.0 | 17.4 |
| >$50 000 | 16.2 | 13.8 | 18.7 |
| Reported any material hardship | |||
| Food | 60.6 | 63.9 | 57.1 |
| Utilities | 42.8 | 46.4 | 39.1 |
| Housing | 44.9 | 48.2 | 41.5 |
| Total | 74.9 | 77.1 | 72.5 |
Data were collected at baseline as described in the text. There were no significant differences between intervention and control groups for any of the measures shown.
Prevalence of Hardship at Baseline
At baseline, most respondents (73%) reported at least 1 type of hardship during the 12-month period before the baseline survey, which included the entire pregnancy for all participants. More than half of participants (61%) reported food insecurity. Families also reported facing significant housing concerns: 45% of respondents reported housing insecurity, with 28% reporting not having been able to pay rent or mortgage and 6% reporting eviction. Additionally, many families struggled to pay utility bills: 42% of respondents reported missing a payment for gas, electricity, or water in the past year, and 12% reported utility shut-off due to lack of payment. Finally, almost half of respondents (44%) reported disconnection of telephone service due to failure to pay.
A majority of respondents (55%) faced hardship in more than 1 domain, including 22% who reported hardships in all 3 domains. χ2 analysis was performed to analyze associations between family characteristics and hardships reported. Families with >1 child were more likely to experience hardship (81% vs 68%, P = .05). There were no significant differences between intervention and control families in any type of baseline hardship reported, or in overall hardship.
Delivery of DULCE Services
Although the study design called for visits with both the pediatrician and FS at all routine health visits and at least 1 home visit, the actual services delivered resulted from joint decision-making between the FS and the parents. As shown in Table 2, 92% of families had at least 1 collaborative health care visit, with a median of 3 visits during the 6-month intervention period. Home visits were accomplished for 52% of families, with a median of 1 home visit and a maximum of 4 visits. FSs had extensive telephone contact with participants, and also provided support in person at the clinic and in the community, and via e-mail and text messaging. Altogether, FSs had a median of 5 contact hours with each family, spread over a median of 14 separate contacts.
TABLE 2.
Number of FS Contacts per Subject by Activity Type (N = 143)
| Activity | Mean No. per Participant | SD | Median No. per Participant | Maximum No. | % of Participants With Activity |
|---|---|---|---|---|---|
| Routine health care visit | 3.2 | 2.1 | 3 | 11 | 92 |
| Home visit | 0.7 | 0.87 | 1 | 4 | 52 |
| Summary: protocol-required contacts | 3.9 | 2.4 | 4 | 15 | 99 |
| Telephone call | 11.9 | 11.0 | 9 | 75 | 97 |
| Meeting with FS not associated with routine visit | 0.7 | 1.3 | 0 | 9 | 39 |
| Community agency visit | 0.1 | 0.5 | 0 | 4 | 8 |
| 0.9 | 2.8 | 0 | 25 | 29 | |
| Other | 0.4 | 0.8 | 0 | 5 | 31 |
| Summary: participant-initiated contacts | 14.1 | 12.5 | 10 | 77 | 98 |
| Overall summary | 17.0 | 14.0 | 14 | 90 | 100 |
This table demonstrates the types of services provided to participants through Project DULCE. The intervention specifically required collaborative routine health care visits; each family was also offered a home visit. In addition to the protocol-required contacts, families could access the FS by telephone, e-mail, text, or personal visits at the clinic. Telephone calls may have been initiated by either FS or participant; 17% were under 2 minutes. E-mail, text, and community visits were initiated or requested by participant.
DULCE participation in collaborative routine health care visits did not interfere with patient flow. DULCE FSs spent a median of 1 hour with each family during the collaborative clinic visit, mirroring the 1.1 hours from check-in to check-out observed during a contemporaneous time-study conducted by the hospital administration.
Delivery of MLP Services
The FS initiated consults with MLP | Boston on behalf of 75 intervention families. Active MLP consultation involved an average of 2.3 telephone calls per family between the FS and MLP | Boston. Of these 75 consults, 72 (96%) were resolved without direct MLP involvement in the form of legal intake and representation. Exact statistics comparing study participants to other infants are not available. However, during the DULCE study time period, MLP | Boston received 174 consults from primary care doctors, nurses, and social workers concerning patients of any age from 0 to 21, excluding the 75 DULCE calls.
Effects of the Intervention on Receipt of Pediatric Preventive Care
Routine immunizations are recommended at 2, 4, and 6 months of age. 32 We examined the distribution of ages at which the third (6-month) DTaP immunizations were delivered. As shown in Table 3, intervention children were significantly more likely to have received these immunizations on time (by 7 months of age) or delayed by no more than 1 month (by 8 months of age). The difference in immunization rates was not statistically significant at the 12-month follow-up (59% vs 52%). These data were obtained from the medical records of the practice site, and may not include immunizations received elsewhere.
TABLE 3.
Immunization Adherence, 6-mo Recommended Immunizations
| Age at Third DTaP | DULCE, N = 165, % | Control Group, N = 161, % | P |
|---|---|---|---|
| <7 mo (211d) | 78 | 63 | .002 |
| <8 mo (241d) | 89 | 78 | .008 |
| Ever | 95 | 89 | .06 |
This table reveals the proportion of participants who received their third DTaP immunization on time. In adherence with American Academy of Pediatrics and Centers for Disease Control and Prevention's Advisory Committee on Immunization Practices standards, patients receive DTaP immunizations at the 2-mo, 4-mo, and 6-mo visits. Therefore, patients who comply with recommended preventive health care will receive immunizations before age 7 mo.
Bright Futures 40 recommends up to 8 routine health care maintenance (RHCM) visits during the first year of life (2 days postnewborn discharge, 2 weeks, 1 month, 2 months, 4 months, 6 months, 9 months, and 12 months); generally 6 of these occurred after study recruitment. In an exploratory analysis, we found that intervention infants were more likely than controls to have 5 or more RHCM visits in the period from initial recruitment until 1 year of life (78% vs 67%, P = .01). The higher number of RHCM visits may reflect improved retention of patients at the clinic, as families discontinued primary care at the study site during the first year of life. By 12 months of age, 93% of intervention families continued to receive primary care at the study site, compared with 86% of control families (P = .056).
ED Utilization
We observed a decrease in the proportion of infants who had at least 1 ED visit by age 6 months: 36.5% of intervention infants had at least 1 visit compared with 49.7% of control infants (P = .021). By 12 months of age, the trend, although still favoring the intervention group, was no longer significant (59.3% vs 65.0%, P = .40). Similarly, the total number of ED visits was significantly lower in the DULCE group than in the control group at 6 months (P = .023) but no longer significant by age 12 months (P = .08).
Intervention Effects on Access to Resources
Participants were asked about their receipt of specified public benefits and protections at baseline, postintervention (6 months), and follow-up (12 months). Table 4 lists these benefits, and Table 5 shows the results of a mixed linear model analyses of these data; models with group, time, and group-by-time interaction. Compared with controls, research subjects had significantly more success in obtaining utilities assistance and in obtaining resources overall. Maternal age, education, and parity did not significantly modify these outcomes. There was a significant difference between the intervention and control groups in access to 8 resources (local food pantry or food program, Supplemental Nutrition Assistance Program, Special Supplemental Nutritional Program for Women, Infants, and Children, discounted telephone service, low-income utility discount or shut-off protection, Emergency Aid to the Elderly, Disabled, and Children, and Transitional Aid to Families With Dependent Children) that clinical social workers had previously categorized as being likely to be attainable within the 6-month study time frame (P = .0072), and a trend toward improvement in areas deemed possible (P = .2), and no difference between the groups in resources that were judged to be impossible to obtain within 6 months such as housing.
TABLE 4.
Public Resources Included in Participant Survey
| Food assistance |
| Local food pantry or other food program a |
| SNAP: Supplemental Nutrition Assistance Program (“food stamps”) a |
| WIC: Special Supplemental Nutritional Program for Women, Infants, and Children a |
| Utility assistance |
| Discounted cell phone or landline service a |
| Low-income utility discount a |
| Utility shut-off protection a |
| Housing assistance |
| Rental voucher (state subsidy programs) |
| Section 8 voucher (federal subsidy program) |
| Income assistance |
| Child support |
| EAEDC: Emergency Aid to the Elderly, Disabled, and Children a |
| TAFDC: Transitional Aid to Families With Dependent Children a |
| SSI: Supplemental Security Income |
| SSDI: Social Security Disability Income |
| Unemployment benefits |
As described in the text, participants were asked whether they had heard about, tried to get, or obtained each of 14 public resources. This table lists the times included, divided by assistance type.
Resources were described by Boston Medical Center Department of Pediatrics clinical social work team as likely to be obtainable within 6 months of application.
TABLE 5.
Family Resources Received by Group and Time
| Resource | Baseline, N = 330 | 6 mo, N = 281 | 12 mo, N = 237 | P, Group by Time Interaction | |||
|---|---|---|---|---|---|---|---|
| DULCE, N = 167, % | Control, N = 163, % | DULCE, N = 145, % | Control, N = 136, % | DULCE, N = 119, % | Control, N = 118, % | ||
| Food assistance | 43.0 | 40.6 | 44.8 | 39.5 | 43.5 | 42.2 | .179 |
| Housing assistance | 9.4 | 11.2 | 11.0 | 10.3 | 13.9 | 12.7 | .285 |
| Income assistance | 21.5 | 16.6 | 23.8 | 18.4 | 21.1 | 18.8 | .453 |
| Utility and telephone assistance | 4.2 | 6.4 | 9.3 | 4.6 | 12.7 | 10.6 | .006 |
| Summary result: mean number of resources received | 2.8 | 2.6 | 3.2 | 2.7 | 3.7 | 3.2 | .029 |
Participants were asked whether they had heard about, tried to get, or obtained specific resources at the baseline, 6-mo, and 12-mo interviews. This table reveals the results of these surveys for each type of assistance. Probabilities were computed based on participants who had complete follow-up through 12 mo (N = 223).
Discussion
The families of infants who received primary care at our urban safety-net hospital experienced high levels of hardship. DULCE added the services of a specially trained FS to services available in the clinic for families with children from birth to 6 months of age and led to significant acceleration in attainment of concrete supports, and in measures of preventive care delivery.
Families of newborns may experience particularly high levels of hardship. Our finding that 61% of the families of newborns experienced food insecurity is higher than reported in a recent study of the entire pediatric age span conducted at an urban pediatric clinic reported (33% incidence), 41 and then reported by the 5-city Children’s Health Watch (22% for 2012). 42 Although direct comparison is complicated by methodological differences, there is little doubt that many low-income families of newborns experience high levels of hardship. This high level was observed despite demographic factors that would seem likely to mitigate hardship: most participating mothers were at least 25 years old, almost half of the households included 2 parents, and half of parents had attained at least a high school degree.
Government agencies administer public benefits programs in accordance with complex laws and regulations. MLP | Boston provided training and ongoing consultation to the FSs throughout the intervention. This study represents the added effects of a trained FS in a system that already includes MLP services; physicians caring for control group patients also had access to MLP resources. Integration of a FS allowed MLP to reserve direct legal services for the small number of families facing complex situations. This model’s success in amplifying the impact of a relatively low dose of MLP resources carries important implications for evolution of the MLP network, which currently has over 250 sites and has been endorsed by the American Medical and Bar Associations. 43 – 45
DULCE accelerated access to concrete supports for newborns and their families; intervention families received greater support for their concrete needs during the infants’ first 6 months of life. Previous research suggests that the early provision of concrete support may protect against child neglect and abuse and reduce parental stress, 46 and promote the formation of positive attachment relationships. 47 , 48 Other programs to address the concrete needs of families through improvements in primary health care have been described: WE CARE features a simplified, self-administered needs assessment coupled with practice guidance to specific resources. 49 Safe Environment for Every Kid uses a screening instrument, originally administered by physicians, to refer selected families to social work support. 50 , 51 DULCE differs from these interventions in that a specially trained FS who has established a trusting relationship with families both conducts the needs assessment and provides direct assistance to families in obtaining resources.
DULCE support was delivered universally within the health care setting and is intended to implement the Strengthening Families approach. 26 , 37 Although this study was not designed to directly assess costs in routine implementation, several features may reduce costs: the intervention is based in the primary care setting, reducing the costs of case identification, outreach, and travel. In general, the cost is expected to compare favorably with universal home visiting models and be a fraction of the cost of more intensive maternal–infant early childhood home visiting programs.
Project DULCE improved the delivery of preventive health care. Although the physician spends less than 20 minutes with each family during a routine health care visit, families often spend over 1 hour at the health care site. DULCE made use of this time. Families who have been actively engaged in their infant’s health care and may be more likely to prioritize their routine health care visits. Reminder systems have been shown to promote adherence 52 , 53 ; DULCE, by making the visits more valuable for families, may offer another avenue for improvement in delivery of preventive health care. As health care systems become accountable for the delivery of preventive services, the cost of this intervention may be partially offset by reduction in case management costs.
The single site involved in this study has on-site social work support available, extended services through availability of MLP, and a help desk staffed by HealthLeads. 54 Higher effectiveness of the intervention may be seen in clinical sites with less robust preexisting integrated support resources. Even so, the findings reported here support the conclusion that a FS trained and supported by MLP and Healthy Steps and embedded in pediatric primary care can measurably assist low-income families with infants in securing concrete supports, and improve the overall quality of primary care and preventive care delivery.
Limitations
This study was conducted at a single hospital-based primary care site, 1 with previous experience with each of the programs that formed the basis for the intervention: Healthy Steps and MLP | Boston. Quantitative measures reported here were restricted to unverified self-report of specific public benefits and review of medical records. For many outcomes, the effect size diminished by 6 months postintervention (12 months) to the point that it was not significant in this population. Future studies may examine the impact of a DULCE model in supporting other family strengths.
This project was implemented in the context of a randomized controlled trial design requiring that the initial innovation be completed with fidelity; further improvements in effectiveness may be sought by using quality improvement techniques. 55
Conclusions
Project DULCE offers a promising method of delivering services that appears to improve the quality of preventive service delivery without disrupting core clinical operations. This may prove to be a useful innovation in developing comprehensive, family-centered, community-based systems to support low-income families with young children.
Acknowledgments
Project DULCE, through its Advisory Board, included representatives from the Boston Public Health Commission, The Massachusetts Children’s Trust, the Massachusetts Department of Children and Families, the Massachusetts Department of Public Health, Smart from the Start, and Thrive in 5 Boston. Finally, we thank the technical support of Kymberly Byrd, Ammarah Iqbal, and Fatima Sammy, and the contributions of family specialists Genevieve Birkner, Julie Krathen, Kena Mena, and Carolina Velasco-Hodgson.
Glossary
- DTaP
diphtheria-tetanus-acellular pertussis
- DULCE
Developmental Understanding and Legal Collaboration for Everyone
- ED
emergency department
- FS
family specialist
- MLP
Medical-Legal Partnership
- RHCM
routine health care maintenance
Footnotes
Dr Sege conceptualized and designed the study, supervised its implementation and analysis, and drafted the initial manuscript; Drs Preer, Morton, and Kaplan-Sanoff participated in the clinical implementation of the intervention, wrote sections of the initial manuscript, and participated in its editing; Drs Cabral and De Vos led the evaluation team, which also included Ms Lee and Ms Abreu; each participated in conducting statistical analyses, preparing tables, and editing the manuscript; Ms Morakinyo coordinated all aspects of the project, and ensured regulatory and human subjects compliance; she participated in reviewing and editing the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01343940).
Dr Sege’s current affiliation is Health Resources in Action, Boston, MA, and Center for the Study of Social Policy, Washington, District of Columbia.
FUNDING: This study was funded by the US Department of Health and Human Services, Administration for Children, Youth, and Families, Office on Child Abuse and Neglect, under Cooperative Agreement 90CA1763 with the Center for the Study of Social Policy. Matching funding was provided by the Child Health Foundation at Boston University.
POTENTIAL CONFLICT OF INTEREST: Ms Morton is an employee of Medical-Legal Partnership | Boston, a program whose model was integrated into the study intervention. Medical-Legal Partnership | Boston received a subgrant to support our work on Project Developmental Understanding and Legal Collaboration for Everyone from Boston Medical Center, the lead grantee. After completion of this project, but prior to this publication, Dr Sege became a consultant for the nonprofit Center for the Study of Social Policy; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Racine AD, Long TF, Helm ME, et al; Committee on Child Health Financing. Children’s Health Insurance Program (CHIP): accomplishments, challenges, and policy recommendations. Pediatrics. 2014;133(3). Available at: www.pediatrics.org/cgi/content/full/133/3/e784 [DOI] [PubMed]
- 2. Mangione-Smith R , Schiff J , Dougherty D . Identifying children’s health care quality measures for Medicaid and CHIP: an evidence-informed, publicly transparent expert process. Acad Pediatr. 2011;11(suppl 3):S11–S21 [DOI] [PubMed] [Google Scholar]
- 3.Urban Institute, Robert Wood Johnson Foundation. Gains for children: increased participation in Medicaid and CHIP in 2009. Available at: www.rwjf.org/content/dam/farm/reports/reports/2011/rwjf70806. Published 2011. Accessed March 25, 2014
- 4. Chien AT , Song Z , Chernew ME , et al. Two-year impact of the alternative quality contract on pediatric health care quality and spending. Pediatrics. 2014;133(1):96–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Conroy K , Sandel M , Zuckerman B . Poverty grown up: how childhood socioeconomic status impacts adult health. J Dev Behav Pediatr. 2010;31(2):154–160 [DOI] [PubMed] [Google Scholar]
- 6. Raphael JL . Differences to determinants: elevating the discourse on health disparities. Pediatrics. 2011;127(5). Available at: www.pediatrics.org/cgi/content/full/127/5/e1333 [DOI] [PubMed] [Google Scholar]
- 7. Alaimo K , Olson CM , Frongillo EA Jr . Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics. 2001;108(1):44–53 [PubMed] [Google Scholar]
- 8. Alaimo K , Olson CM , Frongillo EA Jr , Briefel RR . Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health. 2001;91(5):781–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Weinreb L , Wehler C , Perloff J , et al. Hunger: its impact on children’s health and mental health. Pediatrics. 2002;110(4). Available at: www.pediatrics.org/cgi/content/full/110/4/e41 [DOI] [PubMed] [Google Scholar]
- 10. Cook JT , Frank DA , Berkowitz C , et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–1438 [DOI] [PubMed] [Google Scholar]
- 11. Jyoti DF , Frongillo EA , Jones SJ . Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr. 2005;135(12):2831–2839 [DOI] [PubMed] [Google Scholar]
- 12. Rose-Jacobs R , Black MM , Casey PH , et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72 [DOI] [PubMed] [Google Scholar]
- 13. Meyers A , Cutts D , Frank DA , et al. Subsidized housing and children’s nutritional status: data from a multisite surveillance study. Arch Pediatr Adolesc Med. 2005;159(6):551–556 [DOI] [PubMed] [Google Scholar]
- 14. Cutts DB , Meyers AF , Black MM , et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Frank DA , Neault NB , Skalicky A , et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics. 2006;118(5). Available at: www.pediatrics.org/cgi/content/full/118/5/e1293 [DOI] [PubMed] [Google Scholar]
- 16. Cook JT , Frank DA , Casey PH , et al. A brief indicator of household energy security: associations with food security, child health, and child development in US infants and toddlers. Pediatrics. 2008;122(4). Available at: www.pediatrics.org/cgi/content/full/122/4/e867 [DOI] [PubMed] [Google Scholar]
- 17. Bhattacharya J , DeLeire T , Haider S , Currie J . Heat or eat? Cold-weather shocks and nutrition in poor American families. Am J Public Health. 2003;93(7):1149–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ma CT , Gee L , Kushel MB . Associations between housing instability and food insecurity with health care access in low-income children. Ambul Pediatr. 2008;8(1):50–57 [DOI] [PubMed] [Google Scholar]
- 19. Frank DA , Casey PH , Black MM , et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics. 2010;125(5). Available at: www.pediatrics.org/cgi/content/full/125/5/e1115 [DOI] [PubMed] [Google Scholar]
- 20. Kirkpatrick SI , Tarasuk V . Housing circumstances are associated with household food access among low-income urban families. J Urban Health. 2011;88(2):284–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Academy of Pediatrics. Strategic priorities and AAP initiatives 2013–2014. Available at: www.aap.org/en-us/Documents/Strategic_Priorities_and_AAP_Initiatives.pdf. Published 2013. Accessed July 24, 2014
- 22. Berger RP , Fromkin JB , Stutz H , et al. Abusive head trauma during a time of increased unemployment: a multicenter analysis. Pediatrics. 2011;128(4):637–643 [DOI] [PubMed] [Google Scholar]
- 23. Fowler PJ , Henry DB , Schoeny M , Landsverk J , Chavira D , Taylor JJ . Inadequate housing among families under investigation for child abuse and neglect: prevalence from a national probability sample. Am J Community Psychol. 2013;52(1–2):106–114 [DOI] [PubMed] [Google Scholar]
- 24. Barnett MA . Economic disadvantage in complex family systems: expansion of family stress models. Clin Child Fam Psychol Rev. 2008;11(3):145–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fang X , Brown DS , Florence CS , Mercy JA . The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl. 2012;36(2):156–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Center for the Study of Social Policy. Strengthening families: the protective factors framework. Available at: www.cssp.org/reform/strengthening-families/the-basics/protective-factors. Published 2014. Accessed April 27, 2014
- 27. Toomey SL , Chien AT , Elliott MN , Ratner J , Schuster MA . Disparities in unmet need for care coordination: the national survey of children’s health. Pediatrics. 2013;131(2):217–224 [DOI] [PubMed] [Google Scholar]
- 28. Long WE , Bauchner H , Sege RD , Cabral HJ , Garg A . The value of the medical home for children without special health care needs. Pediatrics. 2012;129(1):87–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Halfon N , Stevens GD , Larson K , Olson LM . Duration of a well-child visit: association with content, family-centeredness, and satisfaction. Pediatrics. 2011;128(4):657–664 [DOI] [PubMed] [Google Scholar]
- 30. Zuckerman B , Parker S , Kaplan-Sanoff M , Augustyn M , Barth MC . Healthy Steps: a case study of innovation in pediatric practice. Pediatrics. 2004;114(3):820–826 [DOI] [PubMed] [Google Scholar]
- 31. Minkovitz CS , Hughart N , Strobino D , et al. A practice-based intervention to enhance quality of care in the first 3 years of life: the Healthy Steps for Young Children Program. JAMA. 2003;290(23):3081–3091 [DOI] [PubMed] [Google Scholar]
- 32. Cohen E , Fullerton DF , Retkin R , et al. Medical-legal partnership: collaborating with lawyers to identify and address health disparities. J Gen Intern Med. 2010;25(suppl 2):S136–S139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weintraub D , Rodgers MA , Botcheva L , et al. Pilot study of medical-legal partnership to address social and legal needs of patients. J Health Care Poor Underserved. 2010;21(suppl 2):157–168 [DOI] [PubMed] [Google Scholar]
- 34. Sandel M , Hansen M , Kahn R , et al. Medical-legal partnerships: transforming primary care by addressing the legal needs of vulnerable populations. Health Aff (Millwood). 2010;29(9):1697–1705 [DOI] [PubMed] [Google Scholar]
- 35. Fairbrother G , Simpson LA . Measuring and reporting quality of health care for children: CHIPRA and beyond. Acad Pediatr. 2011;11(suppl 3):S77–S84 [DOI] [PubMed] [Google Scholar]
- 36. Greene-McIntyre M , Caldwell C . State Medicaid and Children’s Health Insurance Program’s perspective on CHIPRA core measures. Acad Pediatr. 2011;11(suppl 3):S89–S90 [DOI] [PubMed] [Google Scholar]
- 37. Sege R , Kaplan-Sanoff M , Morton S , Velasco-Hodgson C , Preer G , DeVos E , Krathen J . Project DULCE: Strengthening Families though Enhanced Primary Care. Zero to Three. 2014;35(1):10–18 [Google Scholar]
- 38.Bendheim-Thoman Center for Research on Child Wellbeing, Social Indicators Survey Center. Mothers’ and children’s poverty and material hardship in the years following a non-marital birth wellbeing. Available at: http://crcw.princeton.edu/workingpapers/WP11-02-FF.pdf. Published 2008. Accessed August 1, 2014
- 39. Akinsanya-Beysolow I , Advisory Committee on Immunization Practices (ACIP) ACIP Child/Adolescent Immunization Work Group. Centers for Disease Control and Prevention (CDC) . Advisory Committee on Immunization Practices recommended immunization schedules for persons aged 0 through 18 years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(5):108–109 [PMC free article] [PubMed] [Google Scholar]
- 40. Hagan J , Shaw J , Duncan P , eds. Bright Futures: Guidelines for Health Supervision, 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 41. DeMartini TL , Beck AF , Kahn RS , Klein MD . Food insecure families: description of access and barriers to food from one pediatric primary care center. J Community Health. 2013;38(6):1182–1187 [DOI] [PubMed] [Google Scholar]
- 42.Children’s Health Watch. Food insecurity and child health. Available at: www.childrenshealthwatch.org/finding/food-insecurity-and-child-health/. Accessed July 1, 2014
- 43.American Medical Association. Report 15 to the Board of Trustess-A-10. Medical-legal partnerships to improve health and well-being. Resolution 7, I-09, 2010. Available at: http://medical-legalpartnership.org/wp-content/uploads/2014/02/American-Medical-Association-MLP-Resolution.pdf. Accessed June 21, 2014
- 44.American Academy of Pediatrics. Medical-Legal Partnership: promoting child health through preventative law. Resolution 8. Available at: http://medical-legalpartnership.org/wp-content/uploads/2014/02/American-Academy-of-Pediatrics-MLP-Resolution.pdf. Published December 11, 2007. Accessed June 21, 2014
- 45.Medical-Legal Partnerships Pro Bono Project. Available at: http://medical-legalpartnership.org/wp-content/uploads/2014/02/American-Bar-Association-MLP-Resolution.pdf. Accessed April 29, 2015
- 46. Huang CY , Costeines J , Ayala C , Kaufman JS . Parenting Stress, Social Support, and Depression for Ethnic Minority Adolescent Mothers: Impact on Child Development. J Child Fam Stud. 2014;23(2):255–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Langley-Evans SC . Nutrition in early life and the programming of adult disease: a review. J Hum Nutr Diet. 2015;28(suppl 1):1–14 [DOI] [PubMed] [Google Scholar]
- 48. Liu Y , Njai RS , Greenlund KJ , Chapman DP , Croft JB . Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Prev Chronic Dis. 2014;11:E37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Garg A , Butz AM , Dworkin PH , Lewis RA , Thompson RE , Serwint JR . Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558 [DOI] [PubMed] [Google Scholar]
- 50. Dubowitz H , Lane WG , Semiatin JN , Magder LS , Venepally M , Jans M . The safe environment for every kid model: impact on pediatric primary care professionals. Pediatrics. 2011;127(4). Available at: www.pediatrics.org/cgi/content/full/127/4/e962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dubowitz H , Feigelman S , Lane W , Kim J . Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) Model. Pediatrics. 2009;123(3):858–864 [DOI] [PubMed] [Google Scholar]
- 52. Dombkowski KJ , Costello LE , Harrington LB , Dong S , Kolasa M , Clark SJ . Age-specific strategies for immunization reminders and recalls: a registry-based randomized trial. Am J Prev Med. 2014;47(1):1–8 [DOI] [PubMed] [Google Scholar]
- 53. Szilagyi PG , Albertin C , Humiston SG , et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Acad Pediatr. 2013;13(3):204–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Garg A , Marino M , Vikani AR , Solomon BS . Addressing families’ unmet social needs within pediatric primary care: the health leads model. Clin Pediatr (Phila). 2012;51(12):1191–1193 [DOI] [PubMed] [Google Scholar]
- 55. Berwick DM . Broadening the view of evidence-based medicine. Qual Saf Health Care. 2005;14(5):315–316 [DOI] [PMC free article] [PubMed] [Google Scholar]