Abstract
BACKGROUND
This report describes and discusses recurrent intramuscular lipoma (IML) of the extensor pollicis brevis (EPB). An IML usually occurs in a large muscle of the limb or torso. Recurrence of IML is rare. Recurrent IMLs, especially those with unclear boundaries, necessitate complete excision. Several cases of IML in the hand have been reported. However, recurrent IML appearing along the muscle and tendon of EPB on wrist and forearm has not been reported yet.
CASE SUMMARY
In this report, the authors describe clinical and histopathological features of recurrent IML at EPB. A 42-year-old Asian woman presented with a slow-growing lump in her right forearm and wrist area six months ago. The patient had a history of surgery for a lipoma of the right forearm one year ago with a scar of 6 cm on the right forearm. magnetic resonance imaging confirmed that the lipomatous mass, which had attenuation similar to subcutaneous fat, had invaded the muscle layer of EPB. Excision and biopsy were performed under general anesthesia. On histological examination, it was identified as an IML showing mature adipocytes and skeletal muscle fibers. Therefore, surgery was terminated without further resection. No recurrence occurred during a follow-up of five years after surgery.
CONCLUSION
Recurrent IML in the wrist must be examined to differentiate it from sarcoma. Damage to surrounding tissues should be minimized during excision.
Keywords: Intramuscular, Lipoma, Recurrence, Wrist, Case report
Core Tip: Lipoma is one of the most common benign tumors. Intramuscular lipoma (IML) is a lipoma that has invaded the muscular layer, sometimes with unclear boundaries. It may recur if complete resection is not performed. IMLs that recur with unclear boundaries might need to be differentiated from soft tissue sarcoma. Therefore, imaging tests such as computed tomography or magnetic resonance imaging should be performed before surgery and a thorough preoperative plan should be established to reduce recurrence and preserve hand function.
INTRODUCTION
A lipoma is a common benign mesenchymal tumor that can occur anywhere in our body. It is one of the most common soft tissue tumors[1]. Lipomas are usually capsulized and well distinguished from surrounding subcutaneous adipose tissues. However, when they infiltrate structures such as muscles, nerves, or synovium, they are less circumscribed and not-well-distinguished from surrounding tissues than usual lipoma. Among them, cases of invasion of the muscle layer are called intramuscular lipoma (IML) or infiltrating lipoma[2]. As reported in several cases, IML usually occurs in a large muscle of the limb or torso[3-8]. To treat an IML, complete removal including capsules is performed, similar to conventional lipoma treatment methods. However, of all IMLs, 83% are infiltrative and 17% are well-defined. In case of infiltrative IML, it is difficult to distinguish from surrounding tissues[4]. There are also important structures around the periphery of the IML that can make it difficult to achieve complete excision. There is a possibility of recurrence if there is no complete excision[5,8]. Additionally, it might be difficult to differentiate a recurrent IML from well-differentiated liposarcoma, because an IML is clinically or histologically indistinguishable from a well-differentiated liposarcoma[4,9]. Therefore, it is important to perform a preoperative radiology examination. Magnetic resonance imaging (MRI) is a device that can effectively diagnose lipoma. It can also help diagnose IML[10]. In this report, the authors report a recurrent IML in the extensor pollicis brevis (EPB) muscle treated surgically without showing any signs of recurrence after five years of follow-up.
CASE PRESENTATION
Chief complaints
A 42-year-old Asian woman presented with a slow-growing lump in her right forearm and wrist area six months ago.
History of present illness
Symptoms started six months ago with a recurrent lump on the previous operative wounds of wrist and forearm.
History of past illness
The patient had a history of surgery with a lipoma of the right forearm one year ago and had a scar of 6 cm on the right forearm. There was no other medical history or surgical history.
Personal and family history
The patient denied any family history of tumors.
Physical examination
Soft, painless lumps along the EPB of the right thumb were found on physical examination. One had a size of 1 cm × 2 cm in the medial area of the right wrist. One had a size of 2 cm × 5 cm on the medial side of the forearm. Her sensation of fingers and wrists, range of motion, and motor power were all normal (Figure 1).
Figure 1.

Preoperative photographs. A: One 2 cm × 5 cm in size in the medial part of the forearm; B and C: A soft, painless lump was palpated along the extensor pollicis brevis of the right thumb, one 1 cm × 2 cm in size on the medial side of the right wrist. The black dotted line signifies the border of the lump to the touch. The patient’s sensation, range of motion of fingers and wrists, and motor power were normal. The previously operated scar is identified about 6 cm on the radial side of the right forearm.
Laboratory examinations
There were no specific findings in laboratory examinations.
Imaging examinations
MRIs showed lumps in muscles and ligaments of EPB that appeared to be due to fat attenuation. Invaded muscles and ligaments showed unclear boundaries (Figure 2).
Figure 2.

Preoperative magnetic resonance imaging showing lipomatous masses with fat-like attenuation in extensor pollicis brevis muscles and ligaments. A: In the coronal view, lipomatous mass infiltrated in the muscle was identified. Boundaries with surrounding muscles and ligaments were unclear; B: In the axial view, lipomatous mass of similar attenuate to fat was identified. An orange arrow indicates a lipomatous mass that infiltrates muscle and ligaments.
FINAL DIAGNOSIS
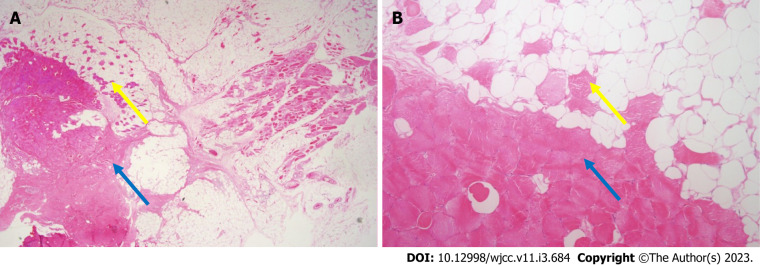
Biopsy results also confirmed the IML of EPB (Figure 3).
Figure 3.
Histological findings. A: Microscopic findings of intramuscular lipomas showing mature adipocytes and skeletal muscle fibers (pink color) (× 10.25 magnification, hematoxylin and eosin staining); B: Skeletal muscle fibers (pink color) are observed between mature adipocytes (× 100 magnification, hematoxylin and eosin staining). Yellow arrows indicate muscle components in fat. Blue arrows indicate muscle belly of extensor pollicis brevis.
TREATMENT
General anesthesia was performed with inhalation anesthesia using sevoflurane after induction using intravascular propofol. After drawing a longitudinal 12 cm incision along the path of the EPB and previous scars, incision was performed with No 15-scalpel blade. Intact presence of the superficial radial nerve and artery running next to the EPB was confirmed. After meticulous dissection of adjacent normal tissues (including muscles, ligaments, nerves, blood vessels, etc.), the IML was exposed using sharp mosquito. A lipomatous mass with a lobulated aspect measuring 12 cm × 4 cm × 5 cm was invading muscles and ligaments (Figures 4 and 5). Blunt Metzenbaum scissor and electrocautery were then used to remove the mass. 200cc HemoVAC was inserted after normal saline irrigation. The superficial fascia and subcutaneous layer were sutured layer by layer with 4-0 Maxon and the skin was sutured with 5-0 Nylon.
Figure 4.
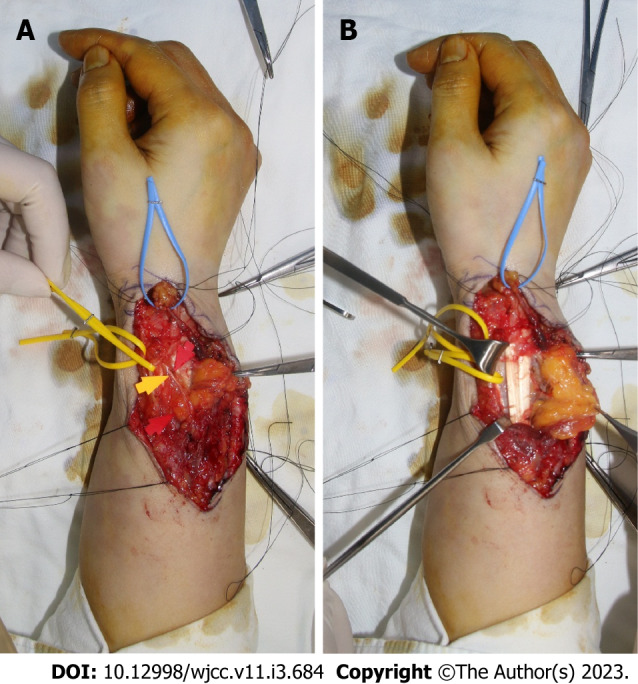
Intraoperative photographs. A: The previous surgical scar was used, and an incision was applied along the run of the extensor pollicis brevis (EPB) to expose the lipomatous mass. A radial artery marked with yellow vessel loop and lipoma in the EPB tendon sheath marked with blue vessel loop were identified; B: Lipoma infiltrating into the muscle portion of EPB was removed while preserving the superficial radial nerve marked with yellow and red arrows.
Figure 5.
Photograph of the specimen. A lipomatous mass of 12 cm × 4 cm × 5 cm was excised. It infiltrated the extensor pollicis brevis (EPB) muscle and tendon sheath. Most of the mass burden was located in the muscle portion of the EPB, presenting as yellow tissue with lobulated aspect and muscular fibers throughout.
OUTCOME AND FOLLOW-UP
Immediately after the surgery, her sensory function was intact and circulation was well maintained (Figure 6). Her extension power was slightly weakened by partial excision of the EPB. However, her extension function was preserved. After 5 years of follow-up, there were no recurrences, side effects, or functional limitations.
Figure 6.

Postoperative photographs. A and B: Primary closure was performed after removal of the intramuscular lipoma and 200cc Hemovac was inserted. There was no contour deformity on postoperative physical examination. Sensory function was intact, and circulation was well maintained; C: However, some extensor pollicis brevis motor weakness occurred. Nevertheless, no deformation of the thumb was seen in the neutral state. Other ranges of motion remained intact.
DISCUSSION
An IML can be distinguished from a conventional lipoma by its rarity and its clinical and pathological characteristics[2]. Histologically, IML can be divided into an infiltrative type, a well-circumscribed type, and a mixed type. Among them, the infiltrative type of IML has distinctive features[11-13]. Clinically, IMLs are characterized by a slow-growing mass that is asymptomatic or accompanied by local edema. Pain is a rare symptom that appears at the end of the course of the disease. It can occur when a deep, huge lipoma causes nerve compression with a mass effect or compresses surrounding soft tissues[12]. In some cases, it has been reported that IML itself is associated with functional limitation of muscles[13,14]. Paresthesia and nerve distribution caused by nerve impingement are also among symptoms that might appear[15,16]. Trauma, chronic irritation, obesity, developmental disorders, endocrine, dysmetabolic factors, and genetic factors have been suggested to play roles in the pathogenesis of IML[17-19].
Papakostas et al[6] have reported cases of IML of the thenar. Lui[7] have reported cases of IML occurring in the abductor digiti minimi. Kim et al[1] have presented a lipoma occurring in the flexor tenosynovium. Kostas-Agnantis et al[20] have reported a lipoma case in the palmaris longus tendon. Lee et al[15] have reported cases of IML occurring in thenar and hypothenar area. However, cases of recurrent IML involving both extensor muscle and tendinous portion at the wrist and forearm level have not been reported yet.
Murphey et al[10] have stated that there is no possibility of malignant transformation of lipomas. It was often claimed that the reports were probably sampling errors or misdiagnoses.
Currently, the recurrence rate of IML is believed to be very low[21]. The patient in this case had previously undergone a surgery. However, it was not completely removed during the previous operation, which might have led to the recurrent. Therefore, attention should be paid to complete excision to reduce the possibility of recurrence and to exclude the possibility of malignancy. By minimizing trauma and meticulous dissection during the surgical procedure, both nerves and blood vessels were preserved with only the area with lipoma invasion removed. The patient has been observed for five years without showing any signs of recurrence.
Computed tomography scan and MRI are both useful for detecting IML and evaluating its invasion in surrounding tissues[10,22]. On computed tomography (CT) scan, IML in the muscle shows a hypodense mass, similar to dense subcutaneous fat[23]. Its morphology can vary widely, ranging from ovoid to fusiform. Its margin might be well-circumscribed or infiltrative[24]. In MRI, IML appears to show a high signal in both T1 and T2, similar to fatty tissue with low signal similar to normal fat in fat-suppressed sequences[10]. MRI can identify IML more specifically than CT. However, results seen on the image might not be exactly the same as actual histological examination results[10].
Histopathologic exam is one of the essential tests for diagnosis. In most cases, there is a uniform appearance of mature uni-vacuolated adipocytes with uniform size and shape. In rare cases, IML can invade muscles, fascia, and tendon[11]. Histological and cytological analyses of IML are extremely important for differentiating it from well-differentiated liposarcoma. Well-differentiated liposarcomas differ from normal IMLs in the presence of atypical cells, vacuolated lipoblasts admixed with fibroblasts-like spindle cells, and several other features[25].
CONCLUSION
In conclusion, considering that IML can occur and recur in hand muscles as observed in this case, careful physical examination and imaging examination should be performed before surgery to diagnose it and completely remove it to reduce the recurrence rate. Additionally, since hands have many important structures, careful attention should be paid to effectively removing the IML s while preserving surrounding nerves, blood vessels, and ligaments.
Footnotes
Informed consent statement: Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016). The manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: November 1, 2022
First decision: December 13, 2022
Article in press: January 9, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alfaqih MS, Indonesia; Singh M, United States S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
Contributor Information
Je Yeon Byeon, Plastic and Reconstructive Surgery, Soonchunhyang University Hospital, Cheonan-si 31151, South Korea.
Yong Seon Hwang, Plastic and Reconstructive Surgery, Soonchunhyang University Hospital, Cheonan-si 31151, South Korea.
Ji Hye Lee, Department of Pathology, Soonchunhyang University Hospital, Cheonan-si 31151, South Korea.
Hwan Jun Choi, Plastic and Reconstructive Surgery, Soonchunhyang University Hospital, Cheonan-si 31151, South Korea. iprskorea@gmail.com.
References
- 1.Kim HW, Lee KJ, Choi SK, Jang IT, Lee HJ. A large palmar lipoma arising from flexor tenosynovium of the hand causing digital nerve compression: A case report. Jt Dis Relat Surg. 2021;32:230–233. doi: 10.5606/ehc.2021.75678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charifa A, Azmat CE, Badri T. Lipoma Pathology. 2022 Dec 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [PubMed] [Google Scholar]
- 3.Wolfe SW, Bansal M, Healey JH, Ghelman B. Computed tomographic evaluation of fatty neoplasms of the extremities. A clinical, radiographic, and histologic review of cases. Orthopedics. 1989;12:1351–1358. doi: 10.3928/0147-7447-19891001-12. [DOI] [PubMed] [Google Scholar]
- 4.McTighe S, Chernev I. Intramuscular lipoma: a review of the literature. Orthop Rev (Pavia) 2014;6:5618. doi: 10.4081/or.2014.5618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalfe Y, Orengo I, Buren GV, Rosen T. Intramuscular lipoma of the scapular region. Dermatol Online J. 2021;27 doi: 10.5070/D327754370. [DOI] [PubMed] [Google Scholar]
- 6.Papakostas T, Tsovilis AE, Pakos EE. Intramuscular Lipoma of the Thenar: A Rare Case. Arch Bone Jt Surg. 2016;4:80–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Lui TH. Intramuscular lipoma of the abductor digiti minimi mimicking intramuscular haemangioma. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-200897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Su CH, Hung JK, Chang IL. Surgical treatment of intramuscular, infiltrating lipoma. Int Surg. 2011;96:56–59. doi: 10.9738/1396.1. [DOI] [PubMed] [Google Scholar]
- 9.Ohguri T, Aoki T, Hisaoka M, Watanabe H, Nakamura K, Hashimoto H, Nakamura T, Nakata H. Differential diagnosis of benign peripheral lipoma from well-differentiated liposarcoma on MR imaging: is comparison of margins and internal characteristics useful? AJR Am J Roentgenol. 2003;180:1689–1694. doi: 10.2214/ajr.180.6.1801689. [DOI] [PubMed] [Google Scholar]
- 10.Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433–1466. doi: 10.1148/rg.245045120. [DOI] [PubMed] [Google Scholar]
- 11.Kindblom LG, Angervall L, Stener B, Wickbom I. Intermuscular and intramuscular lipomas and hibernomas. A clinical, roentgenologic, histologic, and prognostic study of 46 cases. Cancer. 1974;33:754–762. doi: 10.1002/1097-0142(197403)33:3<754::aid-cncr2820330322>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 12.Patil S, Goel A, Mandal S. Re: Morsi HA, Mursi K, Abdelaziz AY, Elsheemy MS, Salah M, Eissa MA. Renal pelvis reduction during dismembered pyeloplasty: is it necessary? J Pediatr Urol. 2013;9:306–307. doi: 10.1016/j.jpurol.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Han HH, Choi JY, Seo BF, Moon SH, Oh DY, Ahn ST, Rhie JW. Treatment for intramuscular lipoma frequently confused with sarcoma: a 6-year restrospective study and literature review. Biomed Res Int. 2014;2014:867689. doi: 10.1155/2014/867689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warner JJ, Madsen N, Gerber C. Intramuscular lipoma of the deltoid causing shoulder pain. Report of two cases. Clin Orthop Relat Res. 1990:110–112. [PubMed] [Google Scholar]
- 15.Lee YH, Jung JM, Baek GH, Chung MS. Intramuscular lipoma in thenar or hypothenar muscles. Hand Surg. 2004;9:49–54. doi: 10.1142/s0218810404002005. [DOI] [PubMed] [Google Scholar]
- 16.Joshua BZ, Bodner L, Shaco-Levy R. Intramuscular (Infiltrating) Lipoma of the Floor of the Mouth. Case Rep Med. 2018;2018:3529208. doi: 10.1155/2018/3529208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Awad P. Rare Intramuscular Lipoma of the Foot: A Case Report. J Am Podiatr Med Assoc. 2021;111 doi: 10.7547/19-118. [DOI] [PubMed] [Google Scholar]
- 18.Pichierri A, Marotta N, Raco A, Delfini R. Intramuscular infiltrating lipoma of the longus colli muscle. a very rare cause of neck structures compression. Cent Eur Neurosurg. 2010;71:157–159. doi: 10.1055/s-0029-1241189. [DOI] [PubMed] [Google Scholar]
- 19.Copcu E. Can intramuscular lipoma have a post-traumatic origin? Br J Dermatol. 2003;149:1084–1085. doi: 10.1111/j.1365-2133.2003.05615.x. [DOI] [PubMed] [Google Scholar]
- 20.Kostas-Agnantis I, Gkiatas I, Korompilia M, Kosmas D, Motsis E, Pakos E, Korompilias A. Lipoma Arborescens of the Upper Extremity With Anatomic Variation of the Palmaris Longus: A Case Report. JBJS Case Connect. 2022;12 doi: 10.2106/JBJS.CC.22.00334. [DOI] [PubMed] [Google Scholar]
- 21.Ramos-Pascua LR, Guerra-Álvarez OA, Sánchez-Herráez S, Izquierdo-García FM, Maderuelo-Fernández JÁ. Intramuscular lipomas: Large and deep benign lumps not to underestimated. Review of a series of 51 cases. Rev Esp Cir Ortop Traumatol. 2013;57:391–397. doi: 10.1016/j.recot.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Stacy GS, Bonham J, Chang A, Thomas S. Soft-Tissue Tumors of the Hand-Imaging Features. Can Assoc Radiol J. 2020;71:161–173. doi: 10.1177/0846537119888356. [DOI] [PubMed] [Google Scholar]
- 23.Pant R, Poh AC, Hwang SG. An unusual case of an intramuscular lipoma of the pectoralis major muscle simulating a malignant breast mass. Ann Acad Med Singap. 2005;34:275–276. [PubMed] [Google Scholar]
- 24.Naruse T, Yanamoto S, Yamada S, Rokutanda S, Kawakita A, Takahashi H, Matsushita Y, Hayashida S, Imayama N, Morishita K, Yamashita K, Kawasaki G, Umeda M. Lipomas of the oral cavity: clinicopathological and immunohistochemical study of 24 cases and review of the literature. Indian J Otolaryngol Head Neck Surg. 2015;67:67–73. doi: 10.1007/s12070-014-0765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans HL, Soule EH, Winkelmann RK. Atypical lipoma, atypical intramuscular lipoma, and well differentiated retroperitoneal liposarcoma: a reappraisal of 30 cases formerly classified as well differentiated liposarcoma. Cancer. 1979;43:574–584. doi: 10.1002/1097-0142(197902)43:2<574::aid-cncr2820430226>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]