Abstract
OBJECTIVE:
Traumatic brain injury (TBI) is a major cause of disability among US children. Our goal was to obtain population-based data on TBI incidence rates.
METHODS:
We conducted surveillance through a stratified random sample of hospital emergency departments in King County, Washington, to identify children 0 to 17 years of age with medically treated TBIs during an 18-month study period in 2007–2008. Additional cases were identified through hospital admission logs and the medical examiner's office. For a sample of nonfatal cases, parents were interviewed to verify TBIs, and medical record data on severity and mechanisms were obtained.
RESULTS:
The estimated incidence of TBIs in this setting was 304 cases per 100 000 child-years. The incidence was highest for preschool-aged children and lowest for children aged 5 to 9 years. Rates were uniformly higher for boys than for girls; there was a larger gender gap at older ages. Falls were the main mechanism of injury, especially among preschool-aged children, whereas being struck by or against an object and motor vehicle–related trauma were important contributors for older children. Approximately 97% of TBI cases were mild, although moderate/severe TBI incidence increased with age.
CONCLUSIONS:
TBIs led to many emergency department visits involving children, but a large majority of the cases were clinically mild. Incidence rates for King County were well below recent national estimates but within the range reported in previous US studies. Because mechanisms of injury varied greatly according to age, prevention strategies almost certainly must be customized to each age group for greatest impact.
Keywords: brain injury, epidemiology, population surveillance
WHAT'S KNOWN ON THIS SUBJECT:
Traumatic brain injury (TBI) is a major cause of disability among US children. Population-based data on TBI incidence are rare, especially for mild TBIs.
WHAT THIS STUDY ADDS:
TBI incidence rates for King County, Washington, were well below recent national estimates. Because mechanisms of injury varied greatly according to age, prevention strategies almost certainly must be customized to each age group for greatest impact.
Traumatic brain injury (TBI) is a significant cause of death, disability, and health care use among US children. 1,2 Quantitative estimates of the incidence and mortality rates of TBIs can be useful for quantifying the overall public health burden of TBIs in relation to other injuries and illnesses, revealing disparities in TBI frequencies among population subgroups, suggesting hypotheses regarding possible risk factors, and providing data to track the success of prevention efforts.
Population-based epidemiologic studies of TBI occurrence generally have relied on 3 data sources for case identification, namely, death certificates, 3 – 7 hospital discharge records, 5 – 12 and emergency department (ED) records. 13 – 18 Each data source captures a different part of the TBI severity spectrum. To date, few studies have combined data from all 3 sources, 5,7 and even fewer have been able to check the validity of TBI diagnoses against data from parent interviews and medical records.
In 2006, we initiated a study of longer-term disabilities among children with TBIs, the Child Health After Injury (CHAI) study. The CHAI study involves identification of a population-based sample of children with TBIs (mild, moderate, or severe) and assessment of their disability status at baseline and 3, 12, 24, and 36 months after injury. To identify eligible children, we established a population-based surveillance system for TBIs in King County, Washington. This surveillance network provided a rare opportunity to study the incidence and descriptive epidemiologic features of child TBIs in an urban setting.
METHODS
Setting
King County includes the city of Seattle and its suburbs. The county is predominantly urban with an estimated total population in 2008 of 1 884 200. The estimated racial distribution in 2008 was 76% white, 14% Asian/Pacific Islander, 6% black, and 4% other races. 19 Approximately 7% of the population was Hispanic.
Case Identification
Countywide surveillance for child TBIs used a 2-stage sampling design with a stratified sample of hospital EDs and all children with acute TBIs during the study period from each selected ED. In the first stage, the 18 King County hospital EDs serving children were divided into 3 groups, as follows: group A, Seattle Children's Hospital, the county's only exclusively pediatric hospital, and Harborview Medical Center, the region's only level 1 adult and pediatric trauma center; group B, the county's 7 level 3 or level 4 trauma centers; group C, 9 non–trauma center hospitals. Both hospitals in group A, 4 of 7 hospitals in group B, and 3 of 9 hospitals in group C were included. Within groups B and C, hospitals were sampled at random. One originally sampled hospital in group B was replaced, before surveillance began, with another random selection, for logistic and financial reasons.
Children 0 to 17 years of age with acute TBIs were identified initially from computerized patient logs at participating EDs. At this stage, TBI was defined on the basis of (1) an International Classification of Diseases, Ninth Revision (ICD-9), code of 800 to 804 or 850 to 854 or (2) a narrative noting a closed-head injury, a TBI, a loss of consciousness, a skull fracture, amnesia after a head injury, any abnormal level of consciousness after head trauma, or any abnormal computed tomographic scan results after a head injury. Computerized ED log data transmitted electronically to the study center included identifying information (including the address of residence and telephone number), the child's age and gender, the date of injury, and the ED disposition. For the analyses reported here, only children whose zip codes indicated residence in King County were included. Hospital admission logs at Seattle Children's Hospital and at Harborview Medical Center also were reviewed regularly, to identify eligible children. Patients who died at the scene of injury were identified through the King County Medical Examiner's office. The 18-month surveillance period ran from April 2007 through September 2008.
For the larger CHAI study, all children admitted to the hospital with TBIs and their parents, as well as an age- and gender-stratified random sample of children seen in an ED for a TBI but not admitted, were approached as potential participants. A brief screening interview was conducted with a parent, usually by telephone, to determine whether the child had experienced a loss of consciousness; had seemed less aware or awake than normal; had been disoriented, agitated, or confused after the injury; or, if 5 years of age or older, had exhibited posttraumatic amnesia. A child was considered eligible if ≥1 of those features was reported. If the family agreed to participate in the CHAI study, then permission was sought to review the child's medical record, from which information was abstracted to verify the presence of TBI and to determine TBI mechanism and severity.
TBI Case Definition and Severity Classification
During medical record review for the subsample enrolled in the CHAI study, mild TBI was defined on the basis of criteria recommended by the Centers for Disease Control and Prevention, 20 that is, (1) ≥1 of any period of observed or self-reported transient confusion, disorientation, or impaired consciousness, as recorded in the medical record; any period of observed or self-reported amnesia lasting <24 hours; or observed signs of other neurologic or other neuropsychological dysfunction, such as posttraumatic seizures or irritability, lethargy, or vomiting after head injury among very young children; and (2) a worst Glasgow Coma Scale (GCS) score of ≥13 at the time of the first medical evaluation and a GCS score of 15 at discharge from the ED or at 24 hours after injury, if hospitalized.
Moderate TBI was defined as TBI according to criterion 1 detailed above plus a motor GCS score of 4 to 5 at 24 hours after injury or a motor GCS score of 6 but not meeting the criteria for mild TBI. Severe TBI was defined as TBI according to criterion 1 plus a maximal motor GCS score of <4 (without pharmacologic paralysis) during the 24 hours after injury.
Analysis
Initiation of TBI surveillance was delayed at 4 sampled hospitals pending necessary administrative approval. Accordingly, 5 analytic groups were formed on the basis of hospital type and period of active participation, as shown in Table 1. ED-identified TBI cases in each analytic group were assigned a weight as follows: (total number of hospitals in group)/(number of actively participating hospitals in group). 21 Sums of weighted case counts, plus any out-of-hospital deaths, became the numerators for incidence rates. All hospitalized TBI cases and all except 2 fatalities were first seen in an ED; therefore, ED cases, hospitalized cases, and fatal cases were not mutually exclusive groups. Population estimates for King County according to age, gender, and calendar year were obtained from the Washington State Office of Financial Management 19 and were used to estimate child-years at risk. 22
TABLE 1.
Numbers of TBI Cases Among Children Sampled in King County and Estimated Total Numbers Seen at King County Hospitals, According to Hospital Group and Analytic Group
| Group |
Description | No. of Hospitals |
No. of Child ED Visits for TBIs |
No. of Children With Confirmed TBIs |
||||
|---|---|---|---|---|---|---|---|---|
| Hospital | Analytic | In Sample | In County | In Sample | In County | In Sample | In County | |
| A | 1 | Children's/Harborview | 2 | 2 | 1319 | 1319 | 861 | 861 |
| B | Other trauma centers | 7 | ||||||
| 2 | Apr 1, 2007, to May 15, 2007 | 2 | 35 | 122 | 27 | 96 | ||
| 3 | May 16, 2007, to Sep 30, 2008 | 4 | 586 | 1026 | 423 | 740 | ||
| C | Non–trauma centers | 9 | ||||||
| 4 | Apr 1, 2007, to Oct 31, 2007 | 1 | 9 | 81 | 7 | 62 | ||
| 5 | Nov 1, 2007, to Sep 30, 2008 | 3 | 18 | 54 | 15 | 46 | ||
| Total | 5–9 | 18 | 1967 | 2602 | 1333 | 1805 | ||
Children's indicates Seattle Children's Hospital; Harborview, Harborview Medical Center.
Four key variables had missing values for some study children. Verification that the child had experienced a TBI, on the basis of a telephone screening interview with a parent, was established for 1001 children whose parents were reached successfully by telephone but was not established for 524 children who were not sampled and 442 who were sampled but whose parents could not be contacted. Medical record validation of TBI, TBI severity, and TBI mechanism was established only for the 405 children who were recruited into the CHAI study and whose medical records were abstracted. Restriction of the analysis to children with complete data would imply that this subsample is representative of all eligible children, an assumption that rarely is satisfied in practice and clearly is not in this case. Instead, we used multiple imputation. This approach relies on a weaker assumption, that the distribution of true values among children with missing data is the same as the distribution among similar children with known values. “Similar” is defined on the basis of relevant characteristics that are known for all children. Several plausible data values are imputed for each child with missing data. Variability among these imputed values reflects the degree of uncertainty about the true value. This variability is explicitly incorporated into significance tests and confidence intervals (CIs).
In preliminary analyses, hospital group and ED disposition for children seen at Harborview Medical Center or Seattle Children's Hospital were strongly associated with missingness and with the values of 3 of the variables when known, namely, parental verification of TBI status, medical record validation of TBI status, and TBI severity. Accordingly, hospital group and ED disposition were used as predictors in the imputation model for these variables. Appendix 1 shows results related to this strategy for TBI severity. For TBI mechanism, age group and gender were used as predictors for the imputation model. Imputation was conducted by using the approximate Bayesian bootstrap method. 23,24
Analyses were conducted by using the survey package in the statistical language R, version 2.13.0. 25 CIs were determined by using a resampling method that mimicked the sampling design. At each replication, first a sample of hospitals was drawn; Harborview Medical Center and Seattle Children's Hospital were included automatically, whereas a bootstrap sample of hospitals in other hospital groups was drawn. 26 Then, for hospital i, the number of eligible TBI cases ni was determined, according to results from multiple imputation of eligibility status. A random number ki was drawn from a Poisson distribution with mean ni for each hospital. Finally, ki cases were drawn at random, with replacement, from the ni eligible cases at each hospital. CIs were based on the 2.5th and 97.5th percentiles of case counts across 4000 replications. Final estimates and CIs thus accounted for the 2-stage sampling design, the nonrandom nature of the subsample with complete data, the uncertainty involved in imputing missing values, and the expected random variation in case occurrence over time. The study was approved by the institutional review boards at Seattle Children's Hospital and at other participating hospitals.
RESULTS
During the 18-month study period, participating EDs reported 1967 patient visits in which a King County child was seen for treatment of an injury recorded as acute TBI. Nine of those ED visits were for an apparently new occurrence of TBI for a child who had made a previous visit for TBI ≥2 weeks earlier. From the total identified, 1443 children were sampled for possible participation in the CHAI study. For 1001 of them, a parent was contacted successfully and completed a screening interview for determination of whether the child had experienced a TBI that met the study's case definition. The TBI screening criteria described above were met in 724 of those cases; for 419 of those cases, consent to participate in the CHAI study was obtained. Medical records were available and abstracted for 405 of those 419 children.
On the basis of the sampling design, data from participating EDs were used to estimate the total number of child visits with a recorded diagnosis of acute TBI in the entire county (Table 1). Overall, an estimated 2602 such visits occurred throughout the county during the study period. Approximately 51% of those visits were to either Seattle Children's Hospital or Harborview Medical Center, 44% to a level 3 or level 4 trauma center ED, and the remaining 5% to non–trauma center EDs.
On the basis of information gathered subsequently from parental interviews and medical record reviews, it was determined that not all children recorded in ED logs as having been seen for acute TBIs actually met the study's case definition for TBI. With the application of results for the subsample of children with TBI validation data to the full sample identified from ED logs, an estimated 1333 of the 1967 children originally identified actually had TBIs (Table 1). With further extrapolation from the full study sample to the county at large, an estimated 1805 children were seen at a King County ED during the study period for an injury that would actually meet our TBI case definition. All subsequent results are based on the estimated number of cases that would meet the study's TBI case definition.
Table 2 shows the estimated numbers of patients with TBIs who were seen in an ED (regardless of disposition), were admitted to a hospital, or experienced fatal injuries, according to age and gender. It should be noted that being seen in an ED, being hospitalized, and dying as a result of TBI were not mutually exclusive. Overall, ∼1.2% of the patients died, ∼5.0% were hospitalized, and ∼93.7% were seen only in an ED. The overall TBI incidence rate was 304 cases per 100 000 child-years (95% CI: 229–383 cases per 100 000 child-years). The rates for boys were greater than those for girls in every age group, but the relative risk (boys/girls) generally increased with age, being 1.35 for ages 0 to 4 years, 1.68 for 5 to 9 years, 2.39 for 10 to 14 years, and 2.41 for 15 to 17 years. Children 0 to 4 years of age had the highest incidence (421 cases per 100 000 child-years), and those 5 to 9 years of age had the lowest (213 cases per 100 000 child-years); rates increased again for the older age groups.
TABLE 2.
Estimated Numbers of TBI Cases According to Level of Care and Incidence Rates According to Age and Gender
| Gender | Age, y | No. of Children With TBIs, Estimate |
Exposure, Child-Years | Incidence Rate, Estimate (95% CI), Cases per 100 000 Child-Years | |||
|---|---|---|---|---|---|---|---|
| Seen in ED | Hospitalized | Died a | All a | ||||
| Male | 0–4 | 412 | 18 | 6 | 412 | 85 481 | 482 (339–666) |
| 5–9 | 220 | 11 | 0 | 220 | 83 078 | 265 (177–373) | |
| 10–14 | 306 | 12 | 3 | 307 | 82 282 | 373 (236–518) | |
| 15–17 | 236 | 21 | 4 | 236 | 53 155 | 444 (270–674) | |
| 0–17 | 1174 | 62 | 13 | 1175 | 303 996 | 387 (283–490) | |
| Female | 0–4 | 289 | 8 | 5 | 290 | 81 334 | 357 (244–503) |
| 5–9 | 125 | 3 | 0 | 125 | 78 981 | 158 (102–228) | |
| 10–14 | 123 | 6 | 1 | 123 | 78 699 | 156 (93–225) | |
| 15–17 | 94 | 10 | 2 | 94 | 51 152 | 184 (107–271) | |
| 0–17 | 631 | 27 | 8 | 632 | 290 165 | 218 (163–279) | |
| Both | 0–4 | 701 | 26 | 11 | 702 | 166 815 | 421 (303–581) |
| 5–9 | 345 | 14 | 0 | 345 | 162 059 | 213 (147–290) | |
| 10–14 | 429 | 18 | 4 | 430 | 160 981 | 267 (173–360) | |
| 15–17 | 330 | 31 | 6 | 330 | 104 307 | 316 (206–458) | |
| 0–17 | 1805 | 89 | 21 | 1807 | 594 161 | 304 (229–383) | |
Includes 2 out-of-hospital deaths.
Table 3 shows the distribution according to TBI severity among the 405 children for whom medical record data were available, the estimated severity distribution among all cases, and the resulting incidence rate estimates for mild TBIs and for moderate, severe, or fatal TBIs, according to age and gender. Overall, the incidence of mild TBIs was ∼296 cases per 100 000 child-years, that is, ∼39 times the incidence of moderate, severe, and fatal TBIs combined (7.6 cases per 100 000 child-years). The estimated incidence rates for moderate and severe nonfatal TBIs were 6.5 and 0.8 cases per 100 000 child-years, respectively, but there were too few such cases to yield stable age- and gender-specific rate estimates. Although mild TBIs were far more common than more-severe TBIs within each age and gender category, the incidence rates for moderate, severe, or fatal TBIs were highest at ages 15 to 17 years for both boys and girls.
TABLE 3.
Estimated Incidence of TBIs in King County According to Severity, Age, and Gender
| Gender | Age, y | No. of Cases in Abstracted Sample |
Total No. of Cases in County, Estimate
a
|
Incidence Rate, Estimate (95% CI), Cases per 100 000 Child-Years |
|||
|---|---|---|---|---|---|---|---|
| Mild | Moderate or Severe | Mild | Moderate, Severe, or Fatal | Mild | Moderate, Severe, or Fatal | ||
| Male | 0–4 | 60 | 6 | 401 | 10.7 | 469 (329–654) | 12.5 (4.7–22.2) |
| 5–9 | 61 | 2 | 218 | 2.5 | 262 (175–370) | 3.0 (0.0–7.2) | |
| 10–14 | 71 | 6 | 299 | 8.2 | 363 (228–510) | 10.0 (3.6–17.0) | |
| 15–17 | 47 | 5 | 225 | 11.1 | 423 (251–655) | 20.9 (7.5–39.5) | |
| 0–17 | 239 | 19 | 1143 | 32.5 | 376 (272–479) | 10.7 (6.6–15.5) | |
| Female | 0–4 | 57 | 2 | 286 | 3.9 | 352 (239–497) | 4.8 (1.2–9.8) |
| 5–9 | 31 | 1 | 123 | 1.4 | 156 (100–226) | 1.8 (0.0–6.3) | |
| 10–14 | 35 | 2 | 120 | 2.8 | 152 (89–220) | 3.6 (0.0–8.9) | |
| 15–17 | 17 | 2 | 89 | 4.8 | 174 (96–260) | 9.4 (2.0–21.5) | |
| 0–17 | 140 | 7 | 618 | 12.9 | 213 (158–274) | 4.4 (2.1–7.2) | |
| Both | 0–4 | 117 | 8 | 687 | 14.6 | 412 (294–571) | 8.8 (4.2–14.4) |
| 5–9 | 92 | 3 | 341 | 3.9 | 210 (145–289) | 2.4 (0.0–5.6) | |
| 10–14 | 106 | 8 | 419 | 11.0 | 260 (167–354) | 6.8 (3.1–11.2) | |
| 15–17 | 64 | 7 | 314 | 15.9 | 301 (191–443) | 15.2 (6.7–25.9) | |
| 0–17 | 379 | 26 | 1761 | 45.4 | 296 (221–375) | 7.6 (5.2–10.6) | |
Averaged over 50 imputations.
The distribution of injury mechanisms varied substantially according to age and gender (Table 4). Falls were by far the most common mechanism for both boys and girls at age 0 to 4 years, and the incidence of fall-related TBIs was much higher among preschool-aged children than among older children. The rates of being struck by or against an object increased steadily with age among boys but not girls. The incidence of TBIs associated with motor vehicle collisions generally increased with age. Among the 18 patients with motor vehicle–related TBIs who were 15 to 17 years of age and had medical record data available for review, 9 were passengers, 4 were drivers, 4 were pedestrians, and 1 was a cyclist. Other cycling-related TBIs were most common at 10 to 14 years of age. It should be noted that, for some age, gender, and mechanism combinations, no TBI cases were observed, which resulted in an estimated incidence rate of 0, although the true rate is likely not to be 0. These estimates reflect limited sample size and should be interpreted as low but not necessarily 0.
TABLE 4.
Incidence of TBIs According to Mechanism, Age, and Gender
| Gender and Age | Fall | Struck by/Against | Motor Vehicle | Cycling | Other |
|---|---|---|---|---|---|
| No. of cases in subsample with medical record review | |||||
| Male | |||||
| 0–4 y | 57 | 5 | 2 | 1 | 1 |
| 5–9 y | 35 | 17 | 5 | 5 | 1 |
| 10–14 y | 34 | 28 | 4 | 10 | 0 |
| 15–17 y | 13 | 25 | 12 | 0 | 1 |
| Female | |||||
| 0–4 y | 51 | 7 | 0 | 0 | 1 |
| 5–9 y | 18 | 11 | 1 | 1 | 0 |
| 10–14 y | 11 | 16 | 3 | 6 | 0 |
| 15–17 y | 7 | 4 | 6 | 2 | 0 |
| Both | |||||
| 0–4 y | 108 | 12 | 2 | 1 | 2 |
| 5–9 y | 53 | 28 | 6 | 6 | 1 |
| 10–14 y | 45 | 44 | 7 | 16 | 0 |
| 15–17 y | 20 | 29 | 18 | 2 | 1 |
| Incidence rate, estimate, cases per 100 000 child-years | |||||
| Male | |||||
| 0–4 y | 416 | 36 | 15 | 7 | 7 |
| 5–9 y | 147 | 72 | 21 | 21 | 4 |
| 10–14 y | 167 | 137 | 20 | 49 | 0 |
| 15–17 y | 113 | 218 | 105 | 0 | 9 |
| Female | |||||
| 0–4 y | 308 | 42 | 0 | 0 | 6 |
| 5–9 y | 92 | 56 | 5 | 5 | 0 |
| 10–14 y | 48 | 69 | 13 | 26 | 0 |
| 15–17 y | 67 | 39 | 58 | 19 | 0 |
| Both | |||||
| 0–4 y | 363 | 39 | 7 | 4 | 7 |
| 5–9 y | 120 | 64 | 13 | 13 | 2 |
| 10–14 y | 109 | 104 | 16 | 38 | 0 |
| 15–17 y | 91 | 130 | 82 | 9 | 4 |
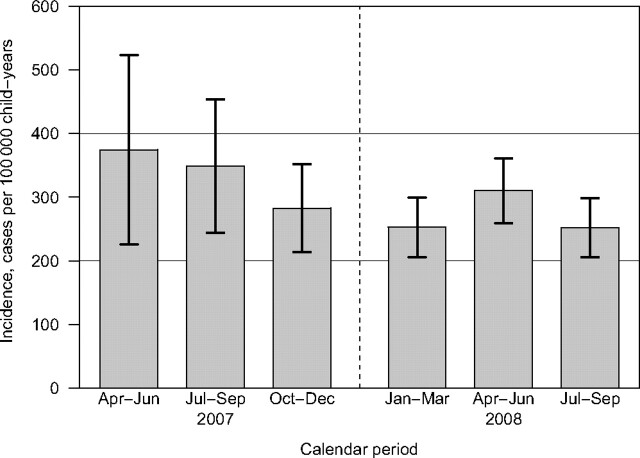
Figure 1 shows that the incidence rates of TBIs varied somewhat according to calendar quarter; generally higher rates were found in warmer months (April through September) than in colder months (October through March), but these differences fell short of statistical significance (P = .3; 5 degrees of freedom). CIs for rates in the first 2 calendar quarters were wide because fewer hospitals contributed data in the early quarters. The overall seasonally adjusted rate was 295 cases per 100 000 child-years (95% CI: 263–326 cases per 100 000 child-years).
FIGURE 1.
Incidence of TBIs among children in King County according to calendar quarter.
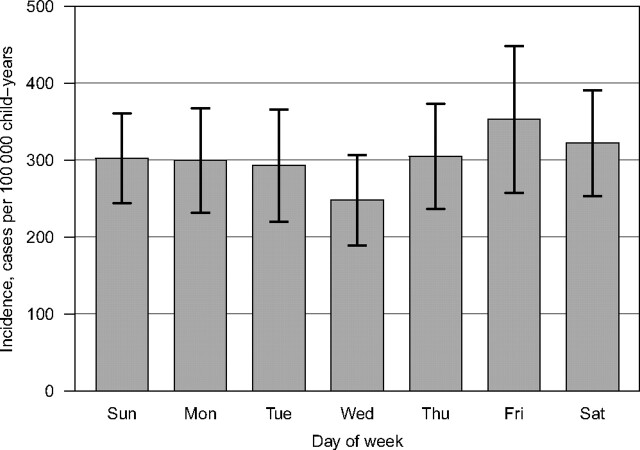
Finally, Fig 2 shows modest variations in the incidence rates of TBIs according to the day of the week (P = .8; 6 degrees of freedom). Rates were slightly higher on Fridays and Saturdays.
FIGURE 2.
Incidence of TBIs among children in King County according to day of the week.
DISCUSSION
The overall incidence of TBIs among children in King County over an 18-month period in 2007–2008 was ∼304 cases per 100 000 child-years. More than 97% of those children had mild TBIs, and ∼94% were seen only in an ED, without being hospitalized. TBI incidence was greater for boys than for girls in every age group; there were larger gender gaps at older ages. Children 0 to 4 years and 15 to 17 years of age were at highest risk, and those 5 to 9 years of age were at lowest risk. Falls predominated as the mechanism among preschool-aged children, whereas being struck by or against an object and motor vehicle collision-related trauma were more common mechanisms among older children. TBI incidence rates did not vary significantly according to season or weekday.
Previous population-based studies of out-of-hospital, nonfatal TBIs among US children yielded variable estimates of incidence (Table 5). Our overall incidence estimate of 304 cases per 100 000 child-years falls well within the range seen in previous studies. Part of the observed variability is no doubt attributable to methodologic differences, including TBI case definitions and data sources. In particular, our incidence estimates are considerably lower than those reported by Langlois et al 5 and by Faul et al, 7 who used data from the National Hospital Ambulatory Medical Care Survey. Our TBI case definition for ED surveillance was narrower than the definitions used by those authors. Langlois et al 5 included ICD-9 code 959.01 (head injury, unspecified), whereas we did not. Faul et al 7 used a still broader case definition, adding ICD-9 codes 950.1 to 950.3 (injury to optic nerve and pathways) and 995.55 (shaken infant syndrome). It also should be noted that those 2 studies could not validate diagnoses in National Hospital Ambulatory Medical Care Survey records against original medical records or against parental interview data by using a standardized clinical case definition of TBI, as we did. We found that ∼28% of children who were reported by a participating ED as having made a visit for acute TBI did not meet our case definition for TBI.
TABLE 5.
Selected Previous US Studies of TBI Incidences Among Children
| Study | Setting | Years | Data Source | Case Definition | Incidence Rate, Cases per 100 000 Child-Years |
|---|---|---|---|---|---|
| Kraus et al 29 (1986) | San Diego County, California | 1981 | Countywide surveillance through EDs, hospital discharges, and coroner records | Physical damage to, or functional impairment of, cranial contents by acute mechanical energy exchange, exclusive of birth trauma | 0–14 y: 185 |
| Sosin et al 30 (1996) | United States | 1991 | National Health Interview Survey | Self-report of medically attended head injury with loss of consciousness in previous 12 mo | 0–14 y: ∼380 |
| Jager et al 16 (2000) | United States | 1992–1994 | National Hospital Ambulatory Medical Care Survey | ICD-9-CM codes 800–801.9, 803–804.9, 850–854.1, 959.01 | 0–4 y: 1091; 5–14 y: 571 |
| Guerrero et al 15 (2000) | United States | 1995–1996 | National Hospital Ambulatory Medical Care Survey | ICD-9-CM codes 800–801.9, 803–804.9, 850–854.1, 959.01 | 0–14 y: 692 |
| Minnesota Department of Health 31 (2005) | Minnesota | 1995–2001 | Statewide ED surveillance, medical records | ICD-9-CM codes 800–804, 850–854.1, 950–953, 959.01, 995.55 | 0–4 y: ∼180; 5–9 y: 147; 10–14 y: 221; 15–19 y: 330 |
| Langlois et al 5 (2006) | United States | 1995–2001 | National Hospital Ambulatory Medical Care Survey | ICD-9-CM codes 800–801.9, 803–804.9, 850–854.1, 959.01 | 0–4 y: 1035; 5–9 y: 603; 10–14 y: 567; 15–19 y: 661 |
| Faul et al 7 (2010) | United States | 2002–2006 | National Hospital Ambulatory Medical Care Survey | ICD-9-CM codes 800–801.9, 803–804.9, 850–854.1, 950.1–950.3, 959.01, 995.55 | 0–4 y: 1256; 5–9 y: 533; 10–14 y: 560; 15–19 y: 757 |
ICD-9-CM indicates ICD-9 Clinical Modification.
Apart from these methodologic differences, true TBI incidence rates almost certainly vary according to place, time, and demographic subgroup. For example, the Seattle area has been the site of child injury prevention programs to increase the use of bicycle helmets 27 and booster seats. 28 More broadly, a secular decrease in TBI hospitalization rates among US children over the 15-year period of 1991–2005 has been found. 8
The predominant mechanisms for TBIs varied substantially according to age, which has implications for the types of preventive interventions that may be needed to reduce the burden of TBIs. Fall-related TBIs were particularly common among preschool-aged children, which suggests that interventions aimed at household safety or parental supervision might have greatest potential impact. At ages 5 to 14, being struck by or against an object also was found to be common. Although the children's activities at the time of injury were not captured here, recreational injuries (including cycling-related injuries) that are preventable through helmet use might be an appropriate intervention target, especially for boys. Motor vehicle–related trauma was a larger factor for older teenagers, even as passengers.
Several study limitations should be noted. As with most previous epidemiologic studies of TBIs, TBI episodes that did not result in medical care being sought, those that were treated in physicians' offices or clinics other than EDs, and those listed with erroneous or nonspecific diagnosis codes in ED logs were not captured. Data for children who resided in King County but were treated elsewhere for TBIs were not captured. Parental interview data and medical record data were available only for a subset of cases, which necessitated imputation of some variables for the remaining cases. Bias might be present if cases with missing data were systematically different in ways that were not captured by other measured characteristics. We also assumed that the distribution of mechanisms among children with available medical records was representative of the distribution among children of similar age and gender. Lastly, the sociodemographic profile and environmental characteristics of King County make generalizability to other settings uncertain.
CONCLUSIONS
A large proportion of child TBI episodes were treated only in the ED and were classified as clinically mild. Because of the large number of mild TBI episodes, however, even modest adverse, long-term effects on daily functioning and academic performance might translate into a significant public health burden of mild TBIs. We hope that the CHAI follow-up study, which provided an opportunity to characterize the descriptive epidemiologic features of child TBIs in this setting, can also shed light on the longer-term consequences of mild TBIs among children.
ACKNOWLEDGMENT
This work was supported by Centers for Disease Control and Prevention grant R49 CE 001021.
APPENDIX.
Imputation Groups for Imputation of TBI Severity When Not Available From Medical Record Review
| Imputation Group |
TBI Severity Verified Through Medical Record Review |
TBI Severity Among Cases Verified Through Record Review |
|||||
|---|---|---|---|---|---|---|---|
| No. | Description | Yes, n | No, n | Proportion Verified, % | Mild, n | Moderate/Severe, n | Proportion Moderate/Severe, % |
| 1 | HMC, admitted | 53 | 31 | 63.1 | 33 | 20 | 37.7 |
| 2 | HMC, sent home | 37 | 64 | 36.6 | 33 | 4 | 10.8 |
| 3 | SCH, admitted | 3 | 9 | 25.0 | 1 | 2 | 66.7 |
| 4 | SCH, sent home | 194 | 928 | 17.3 | 194 | 0 | 0.0 |
| 5 | Neither HMC nor SCH | 118 | 530 | 18.2 | 118 | 0 | 0.0 |
SCH indicates Seattle Children's Hospital; HMC, Harborview Medical Center.
Footnotes
- TBI
- traumatic brain injury
- ED
- emergency department
- CHAI
- Child Health After Injury
- ICD-9
- International Classification of Diseases, Ninth Revision
- CI
- confidence interval
- GCS
- Glasgow Coma Scale
REFERENCES
- 1. Keenan HT , Bratton SL . Epidemiology and outcomes of pediatric traumatic brain injury. Dev Neurosci. 2006;28(4–5):256–263 [DOI] [PubMed] [Google Scholar]
- 2. Atabaki SM . Pediatric head injury. Pediatr Rev. 2007;28(6):215–224 [DOI] [PubMed] [Google Scholar]
- 3. Rodriguez SR , Mallonee S , Archer P , Gofton J . Evaluation of death certificate-based surveillance for traumatic brain injury: Oklahoma 2002. Public Health Rep. 2006;121(3):282–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sills MR , Libby AM , Orton HD . Prehospital and in-hospital mortality: a comparison of intentional and unintentional traumatic brain injuries in Colorado children. Arch Pediatr Adolesc Med. 2005;159(7):665–670 [DOI] [PubMed] [Google Scholar]
- 5. Langlois JA , Rutland-Brown W , Thomas KE . Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 6. Rutland-Brown W , Langlois JA , Thomas KE , Xi YL . Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548 [DOI] [PubMed] [Google Scholar]
- 7. Faul M , Xu L , Wald MM , Coronado VG . Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 8. Bowman SM , Bird TM , Aitken ME , Tilford JM . Trends in hospitalizations associated with pediatric traumatic brain injuries. Pediatrics. 2008;122(5):988–993 [DOI] [PubMed] [Google Scholar]
- 9. Eisele JA , Kegler SR , Trent RB , Coronado VG . Nonfatal traumatic brain injury-related hospitalization in very young children: 15 states, 1999. J Head Trauma Rehabil. 2006;21(6):537–543 [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Incidence rates of hospitalization related to traumatic brain injury: 12 states, 2002. MMWR Morb Mortal Wkly Rep. 2006;55(8):201–204 [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Rates of hospitalization related to traumatic brain injury: nine states, 2003. MMWR Morb Mortal Wkly Rep. 2007;56(8):167–170 [PubMed] [Google Scholar]
- 12. Schneier AJ , Shields BJ , Hostetler SG , Xiang H , Smith GA . Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006;118(2):483–492 [DOI] [PubMed] [Google Scholar]
- 13. Day H , Roesler J , Gaichas A , Kinde M . Epidemiology of emergency department-treated traumatic brain injury in Minnesota. Minn Med. 2006;89(5):40–44 [PubMed] [Google Scholar]
- 14. Bazarian JJ , McClung J , Cheng YT , Flesher W , Schneider SM . Emergency department management of mild traumatic brain injury in the USA. Emerg Med J. 2005;22(7):473–477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guerrero JL , Thurman DJ , Sniezek JE . Emergency department visits associated with traumatic brain injury: United States, 1995–1996. Brain Inj. 2000;14(2):181–186 [PubMed] [Google Scholar]
- 16. Jager TE , Weiss HB , Coben JH , Pepe PE . Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Acad Emerg Med. 2000;7(2):134–140 [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries from sports and recreation activities: United States, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56(29):733–737 [PubMed] [Google Scholar]
- 18. Xiang H , Sinclair SA , Yu S , Smith GA , Kelleher K . Case ascertainment in pediatric traumatic brain injury: challenges in using the NEISS. Brain Inj. 2007;21(3):293–299 [DOI] [PubMed] [Google Scholar]
- 19. Washington State Office of Financial Management. Racial categories as a percent of county population, 2008. Available at: www.ofm.wa.gov/pop/race/08estimates/table3_08.xls . Accessed May 7, 2010
- 20. National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the US: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 21. Levy PS , Lemeshow S . Sampling of Populations: Methods and Applications. 3rd ed. New York, NY: Wiley; 1999. [Google Scholar]
- 22. Koepsell TD , Weiss NS . Epidemiologic Methods: Studying the Occurrence of Illness. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 23. Fleiss JL , Levin B , Paik MC . Statistical Methods for Rates and Proportions. 3rd ed. New York, NY: Wiley; 2003. [Google Scholar]
- 24. Rubin DB , Schenker N . Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10(4):585–598 [DOI] [PubMed] [Google Scholar]
- 25. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- 26. Efron B , Tibshirani RJ . An Introduction to the Bootstrap. New York, NY: Chapman and Hall; 1993. [Google Scholar]
- 27. DiGuiseppi CG , Rivara FP , Koepsell TD , Polissar L . Bicycle helmet use by children: evaluation of a community-wide helmet campaign. JAMA. 1989;262(16):2256–2261 [PubMed] [Google Scholar]
- 28. Ebel BE , Koepsell TD , Bennett EE , Rivara FP . Use of child booster seats in motor vehicles following a community campaign: a controlled trial. JAMA. 2003;289(7):879–884 [DOI] [PubMed] [Google Scholar]
- 29. Kraus JF , Fife D , Ramstein K , Conroy C , Cox P . The relationship of family income to the incidence, external causes, and outcomes of serious brain injury, San Diego County, California. Am J Public Health. 1986;76(11):1345–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sosin DM , Sniezek JE , Thurman DJ . Incidence of mild and moderate brain injury in the United States, 1991. Brain Inj. 1996;10(1):47–54 [DOI] [PubMed] [Google Scholar]
- 31. Minnesota Department of Health, Injury and Violence Prevention Unit. Emergency Department-Treated Traumatic Brain Injury, Minnesota 1998–2003. St Paul, MN: Minnesota Department of Health; 2005. [Google Scholar]