Abstract
BACKGROUND:
Policies protecting children from exposure to secondhand smoke (SHS) may help prevent SHS-related negative health outcomes in children and discourage them from intending to smoke in the future. In this study, we assess the impact of California’s 2007 smoke-free vehicle law on changes in middle and high school students’ reported exposure to smoking in cars. Secondary aims included assessing the association of student-reported exposure to smoking in vehicles and lifetime asthma diagnosis and future intentions to smoke.
METHODS:
Population-weighted data from the California Student Tobacco Survey and the National Youth Tobacco Survey were used to evaluate California and national trends, respectively. Weighted logistic regression models using California Student Tobacco Survey 2011 data assessed the association between the number of days of exposure to smoking in cars and student-reported lifetime asthma diagnosis as well as intention to smoke in the future.
RESULTS:
The proportion of California students reporting exposure to smoking in cars in the last 7 days declined <1% annually from 2001 through 2005, but declined 12% annually from 2007 to 2011. National trends did not show comparable declines after 2006. Students reporting exposure to smoking in vehicles were more likely to report having ever been diagnosed with asthma and intending to smoke in the future than students who were not exposed to SHS.
CONCLUSIONS:
These findings support the legislative intent that public policies that are designed to protect children from exposure to smoking in vehicles will yield better adolescent health outcomes and a lower risk of future adolescent cigarette smoking.
Smoking is the leading cause of preventable death and disease in the United States.1 Smoking causes 1300 deaths every day, and 16 million Americans are currently living with a disease caused by smoking.2 These statistics include not only smokers but also nonsmokers who are exposed to the secondhand smoke (SHS) generated by nearby smokers. The most vulnerable of exposed nonsmokers are young children. Young children of smoking parents have more lung infections and are more likely to cough, wheeze, have shortness of breath, and get more ear infections.3 SHS can also trigger asthma attacks and make asthma symptoms worse.4 The 2012 Surgeon General’s report on preventing tobacco use among youth concluded that there is a causal relationship between active smoking and wheezing severe enough to be diagnosed as asthma in susceptible child and adolescent populations.5 Although active smoking is not secondhand smoking, there is a growing consensus that exposure to secondhand smoking contributes similarly to asthma risk.4,6 Although significant progress has been made in reducing adolescent combustible tobacco use, overall adolescent tobacco use has remained steady because rapidly increasing electronic cigarette use has offset the reductions in conventional tobacco use.7 Research has demonstrated that exposure to adult smoking during childhood may predispose adolescents to smoke as they get older.8,9 Evidence suggests that a nonsmoking adolescent’s risk of future smoking is more powerfully predicted by how much secondhand smoking he or she is exposed to than by peer smoking status,10 which is a recognized precursor to adolescent smoking initiation.11–13
Policies to protect children from exposure to SHS may reduce SHS-related negative health consequences affecting children as well as discourage them from intending to smoke in the future. It is well established that smoke-free laws reduce exposure to SHS in adults.14–18 Evidence shows that smoke-free laws, such as in the workplace, in restaurants, and other outdoor spaces, also reduce exposure to SHS in children and adolescents19,20 by reducing the overall amount of SHS in a community. These policies, in turn, stimulate families to voluntarily adopt bans on smoking in the home, thereby reducing children’s exposure to smoking in the home.21–23 In the United States, localities with comprehensive smoke-free legislation were found to reduce the prevalence and severity of asthma symptoms (eg, wheezing) among those with asthma in homes that did not permit smoking.24 Nonsmoking adults who were exposed to smoking in a car were more likely to report asthma than unexposed nonsmokers.25
Homes and cars are the 2 main sources of exposure to SHS among children.26–29 In the small, enclosed space of a car, nonsmoking passengers who are exposed to smoking are exposed to airborne toxins with concentrations typically many times higher than what is permitted by the Environmental Protection Agency even when a window is down.30,31 Moreover, gaseous and particulate components absorb into upholstery and car surfaces, exposing passengers to toxins long after anyone actually smoked in the car.30 California is currently 1 of 8 states in the United States that has a smoke-free car law.30 California’s smoke-free vehicles law was passed in 2007 and was implemented on January 1, 2008.32 The California law prohibits smoking in a motor vehicle when a minor (age ≤17 years) is present. Law enforcement may not stop a vehicle for a smoking violation alone; it must be secondary to another infraction, and violators of the law can be fined up to $100.
Although smoke-free laws have been shown to reduce the risk of respiratory illnesses4,33,34 and acute myocardial infarction34,35 in adults, the evidence for the effects of smoke-free laws on the health of children is limited.36,37 There is little literature in which researchers evaluate the impact of smoking bans in private vehicles on child exposure to SHS and child-reported asthma diagnosis.
There is widespread public support for government policies that are designed to protect the public from involuntary exposure to cigarette smoke in public settings, but there is less widespread support for government policies regulating private environments, such as homes and cars.38 Smoke-free vehicle laws are controversial because some argue that they represent government overstepping privacy rights; but health policy experts argue that the right of children to breathe smoke-free air is more important than the right of adults to act as they see fit in the privacy of their vehicles.6 Empirical evidence of the health benefits associated with banning smoking in vehicles when children are present may lend support for such laws.
The purpose of the current study is to assess the association of California’s 2007 smoke-free vehicle law with students’ (grades 6–12) self-reported exposure to SHS in cars and health-related outcomes. In this article, we describe 3 aims. Aim 1 was to assess whether the observed decline in California’s student-reported exposure to smoking in vehicles accelerated significantly after the enactment of Senate Bill 7 (SB 7), the law that banned smoking in vehicles when minors are present. Cross-sectional California Student Tobacco Survey (CSTS) 2011 data were used to evaluate aims 2 and 3. Aim 2 assessed whether California’s student-reported exposure to smoking in vehicles was associated with students’ self-reported lifetime asthma diagnosis. Aim 3 evaluated the association between California’s student-reported exposure to smoking in vehicles and their intention to smoke in the future. If confirmed by prospective data, significant associations involving these 2 aims would suggest at least 2 concrete benefits to be expected from future policies that may successfully reduce student-reported exposure to smoking in passenger vehicles.
Methods
Sample
Data for this study come from the CSTS and the National Youth Tobacco Survey (NYTS). The CSTS is a stratified, 2-stage, cluster sampling design survey of anonymous self-reported student tobacco use administered every 2 years in randomly sampled California public schools. The sampling methodology has been reported elsewhere.39 Data were collected biennially from California students in grades 6 to 12 beginning with school years 2001 to 2002 through 2011 to 2012 (n = 151 074). Three CSTS administrations preceded the 2007 passage of SB 7, and 3 CSTS administrations followed it. Most CSTS survey items were taken verbatim from the NYTS, but the 2011 CSTS also included a question about lifetime diagnosis of asthma. Rates of exposure before and after the law were assessed by using data from 6 waves of the biennial CSTS. These data were compared with national data from the NYTS during comparable time periods to assess whether California trends merely mirrored US trends.
The NYTS is an ongoing, nationally representative, school-based survey that uses a 3-stage cluster sampling design to generate cross-sectional, nationally representative samples of US middle and high school students. More detailed information on the NYTS can be found elsewhere.40 The data used in this study were collected in 2000, 2002, 2004, 2006, 2009, and 2011 (n = 164 570). The present analysis included NYTS participants for whom complete data were available.
Measures
Main Exposure Variable
The main exposure variable of time was measured in school years and used as a continuous variable based on the survey year starting in the fall for the CSTS (typical survey period was October to February) and the spring for the NYTS (typical survey period was February to June).
Dependent Variables
For most years, exposure to a person smoking in the car was assessed in the CSTS and NYTS by the following item: “During the past 7 days, on how many days did you ride in a car with someone who was smoking cigarettes?” Answer options were as follows: 0, 1 to 2, 3 to 4, 5 to 6, and 7 days. This question was slightly altered in the 2011 NYTS to read as follows: “During the past 7 days, on how many days did you ride in a vehicle where someone was smoking a tobacco product?” The 8 answer options provided in the 2011 NYTS were recategorized to conform to the 5 answer options used in previous years. For the main analyses for all years, this variable was dichotomized into 2 categories: 0 days (no exposure) and 1 to 7 days (exposed). For secondary analyses that regressed smoking intention or lifetime asthma status onto SHS, the SHS independent variable was operationalized as a 3-category measure: 0, 1 to 2, and 3 to 7.
Asthma Diagnosis
Self-reported lifetime asthma diagnosis was assessed with 1 item: “Has a doctor or nurse ever told you or your parent/guardian that you have asthma?” Responses to this question were coded as yes or no.
Intention to Smoke
Students were asked, “Do you think you will smoke a cigarette at any time during the next year?” with responses including “definitely yes,” “probably yes,” “probably not,” and “definitely no.” For analysis purposes, answers were dichotomized as yes or no. Measures of intention to smoke have been shown to predict future cigarette smoking irrespective of previous smoking behavior.41,42
Covariates
Sociodemographic characteristics included sex, grade level (6–12), and race and/or ethnicity (Hispanic and/or Latino, non-Hispanic white, non-Hispanic African American, non-Hispanic Asian American, and non-Hispanic native Hawaiian and/or Pacific Islander).
Other SHS Variables
Other SHS exposure questions included the following: “During the past 7 days, on how many days were you in the same room with someone who was smoking cigarettes?” (0 [no exposure] or 1 to 7 days [exposed]); “During the past 7 days, on how many days were you in the same room at home with someone who was smoking cigarettes?” (0 [no exposure] or 1 to 7 days [exposed]); and “Does anyone who lives with you now smoke cigarettes?” (yes or no). These variables were included as covariates in adjusted models to make the results more comparable to those reported by other SHS studies.29,43
Data Analysis
All analyses were conducted by using Stata/SE 13.0 (StataCorp, College Station, TX).44 For aim 1, an unadjusted logistic regression model of SHS exposure status in cars using CSTS data were conducted to assess the trends between 2001 and 2011, followed by an adjusted model that included individual-level sociodemographic characteristics. Parallel analyses of the NYTS data collected in the 1999–2011 time frame were conducted to permit comparing California SHS exposure trends with concurrent national SHS exposure trends. The slopes of the declines for the national NYTS data on student exposure to SHS in vehicles were then compared with the slopes of the declines for the corresponding prevalence of student-reported SHS in vehicles in the CSTS. The differences between the slopes of the observed CSTS declines in the 2001–2005 and 2007–2011 periods and the slopes of the declines in NYTS student-reported SHS in vehicles prevalence estimates in the 2002–2006 and 2006–2011 periods were evaluated by using Stata’s postestimation hypothesis-testing procedures. The decision was made to exclude the 2005–2007 CSTS interval from consideration because of the active political campaign involving SB 7 that took place in California during the period of March through October 2007.45 In all logistic regression analyses, sampling weights were used to reflect the sampling design and correct for variations in nonresponse. Parallel analyses were conducted by using mixed effects regression and multinomial logistical regression when the answer options for the SHS exposure in vehicles question were treated as a 3-level or 5-level outcome instead of as a binary outcome. The results for all models yielded similar findings; thus, only the logistic regression results are reported here for ease of interpretation.
For aims 2 and 3, CSTS 2011 data were used in logistic regression models to assess the bivariate relationship of student-reported exposure to smoking in the car with lifetime asthma diagnosis (aim 2) and future intentions to smoke (aim 3). Models predicting intention to smoke were limited to current nonsmokers. Subsequent adjusted models included individual-level sociodemographic characteristics, followed by models including potential SHS exposure confounders. All analyses involving aims 2 and 3 used sampling weights to reflect the survey design and correct for variations in nonresponse.
Results
California and National Exposure to SHS in Cars
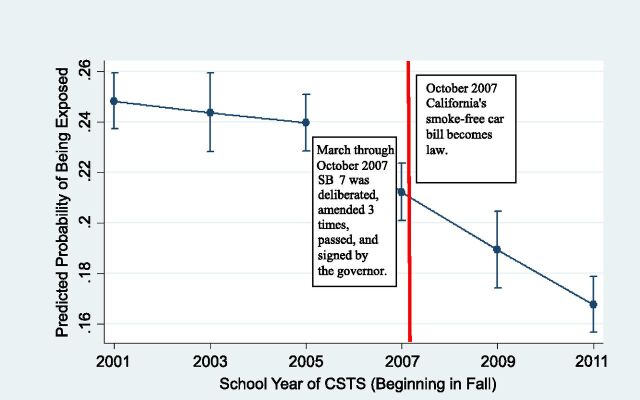
Before the passage of SB 7 in November 2007, California’s prevalence rates of youth exposure to smoking in cars were already ∼50% lower than the corresponding national rates in 2000, with mean estimates of youth exposure to smoking in cars ranging from 17.9% to 25.5% over the 2001–2011 period (compared with the US range of 30.3%–47.6% in the 2000–2011 period). In an unadjusted logistic regression model of exposure by year, a significant reduction was seen between 2001 and 2011, with a 37% reduction in the odds of exposure to smoking in cars in 2011 compared with 2001 (odds ratio [OR] = 0.63; 95% confidence interval [CI]: 0.57 to 0.70). Figure 1 displays the decline in reported exposure to smoking in a car from 2001 to 2011 while controlling for individual-level factors by using weighted data. To test whether there was regression discontinuity in the CSTS data, we compared the annual rate of decline in the predicted probability of exposure during the 2001–2005 period with the corresponding annual rate of decline in the predicted probability of exposure during the 2007–2011 period (Fig 1). Whereas the California rate of decline was negligibly different from 0 during 2001 to 2005 (annual rate of decline = −0.003; 95% CI:−0.006 to 0.007), it accelerated significantly during 2007 to 2011 (annual rate of decline = −0.012; 95% CI: −0.015 to −0.008). If the slope of the decline in the prevalence estimates observed between 2007 and 2011 had been the same as the slope of the decline between 2001 and 2005, the prevalence rates of student-reported SHS in vehicles would have been 23.5% in 2009 and 23.2% in 2011 instead of the observed rates of 20.5% (95% CI: 19.0 to 22.1) in 2009 and 17.9% (95% CI: 16.8 to 18.9) in 2011.
FIGURE 1.
Predicted probability of SHS exposure in the car in the last 7 days in California from 2001 to 2011 (n = 148 664). The figure was adjusted for sex, race and/or ethnicity, and grade level (source: CSTS).
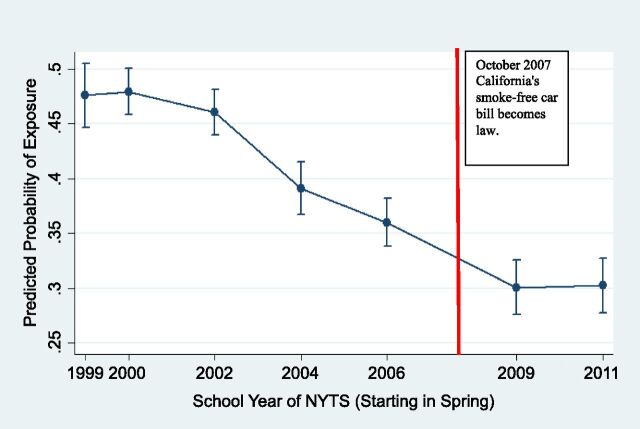
As seen in Fig 2, evidence from the NYTS indicates a secular trend toward reduced child exposure to smoking in cars nationally. The annual rate of decline in the predicted probability of NYTS student-reported exposure to SHS in vehicles was −0.025 (95% CI: −0.033 to −0.018) in the period of spring 2002 to spring 2006, a period largely overlapping with the CSTS period (fall 2001 to fall 2005), but the CSTS annual rate of decline of −0.003 (95% CI: −0.006 to 0.007) was outside of the NYTS 95% CI. The NYTS annual rate of decline for the 2006–2011 period was −0.012 (95% CI: −0.018 to −0.005), which was significantly less than the −0.025 annual NYTS rate of decline in the earlier interval.
FIGURE 2.
Predicted probability of exposure to smoking in a car or vehicle in the last 7 days in the United States from 1999 to 2011 (n = 164 570). The figure was adjusted for sex, race and/or ethnicity, and grade level (source: NYTS).
California Asthma Diagnosis
By using data from the 2011 CSTS, a dose-response relationship was observed between student-reported number of days of exposure to smoking in a vehicle in the last 7 days and students’ self-reported lifetime asthma diagnosis in unadjusted models (test for linearity F1111 = 29.25; P < .001). Mean estimates of the prevalence of asthma diagnosis were 23.5% (95% CI: 22.4% to 24.5%) for no exposure to smoking in vehicles, 27.8% (95% CI: 25.0% to 30.7%) for 1 to 2 days per week of exposure, and 31.4% (95% CI: 28.1% to 34.6%) for 3 to 7 days per week of exposure. Relative to 0 days of exposure, there were increased odds of asthma diagnosis for both 1 to 2 days of exposure (OR = 1.26; 95% CI: 1.09 to 1.45) and 3 to 7 days of exposure (OR = 1.49; 95% CI: 1.28 to 1.73). After adjusting for sociodemographic characteristics, including sex, race and/or ethnicity, and grade level, the dose-response relationship was preserved, with student-reported exposure of 1 to 2 days being associated with 1.24 (95% CI: 1.08 to 1.42) greater odds of asthma diagnosis than those with no exposure and 3 to 7 days of exposure being associated with a 1.46 (95% CI: 1.27 to 1.68) greater odds of asthma diagnosis. When adjusting for other SHS exposure variables, the association with asthma diagnosis of 1 to 2 days of exposure was no longer statistically significant (OR = 1.15; 95% CI: 0.97 to 1.36), but the association with 3 to 7 days of exposure was still statistically significant (OR = 1.24; 95% CI: (1.02 to 1.50), and the linearity of the dose-response relationship remained statistically significant (F1111 = 4.57; P = .03). Of the covariates, sex (male) and ethnicity (non-Hispanic African American) were significantly associated with asthma diagnosis (Table 1). The inclusion of exposure to smoking in the home as a covariate attenuated but did not extinguish the relationship between student-reported exposure to smoking in vehicles and the odds of asthma diagnosis.
TABLE 1.
Exposure to Smoking in Cars in California in 2011 and Lifetime Asthma Diagnosis, Logistic Regression
| Factor | Model 1 | Model 2 | ||
|---|---|---|---|---|
| n = 21 384 | n = 20 941 | |||
| aOR | 95% CI | aOR | 95% CI | |
| SHS exposure in cars, d | ||||
| 0 | Ref | — | Ref | — |
| 1–2 | 1.24 | 1.08 to 1.42** | 1.15 | 0.97 to 1.36 |
| 3–7 | 1.46 | 1.27 to 1.68*** | 1.24 | 1.02 to 1.50* |
| Sex | ||||
| Female | Ref | — | Ref | — |
| Male | 1.11 | 1.03 to 1.20** | 1.11 | 1.02 to 1.20* |
| Grade level | ||||
| Sixth | Ref | — | Ref | — |
| Seventh | 1.01 | 0.69 to 1.46 | 1.00 | 0.69 to 1.44 |
| Eighth | 1.08 | 0.75 to 1.55 | 1.09 | 0.76 to 1.56 |
| Ninth | 1.00 | 0.74 to 1.37 | 1.00 | 0.73 to 1.36 |
| 10th | 0.89 | 0.65 to 1.22 | 0.90 | 0.66 to 1.22 |
| 11th | 0.81 | 0.59 to 1.12 | 0.82 | 0.60 to 1.12 |
| 12th | 0.90 | 0.65 to 1.24 | 0.91 | 0.66 to 1.26 |
| Race and/or ethnicity | ||||
| White, non-Hispanic | Ref | — | Ref | — |
| African American, non-Hispanic | 1.73 | 1.39 to 2.15*** | 1.77 | 1.42 to 2.20*** |
| Hispanic and/or Latino | 0.97 | 0.85 to 1.11 | 0.98 | 0.86 to 1.12 |
| Asian American, non-Hispanic | 0.82 | 0.68 to 0.98* | 0.83 | 0.69 to 1.00* |
| NH and/or PI, non-Hispanic | 1.26 | 0.93 to 1.71 | 1.24 | 0.90 to 1.70 |
| SHS in same room | — | — | 1.04 | 0.92 to 1.17 |
| SHS in home | — | — | 1.10 | 0.96 to 1.27 |
| Live with smoker | — | — | 1.15 | 1.01 to 1.32* |
All data presented are weighted to adjust for differential nonresponse and selection. All analyses in Models 1 and 2 were controlled for sex, grade level, and race and/or ethnicity. Model 2 was further controlled for SHS in the same room, SHS in the home, and living with a smoker. aOR, adjusted odds ratio; NH, native Hawaiian; PI, Pacific Islander; —, not applicable.
P < .05; **P < .01; ***P < .001.
California Youth Intention to Smoke
An analysis of the 2011 CSTS data revealed a dose-response relationship between nonsmoking students’ exposure to smoking in vehicles and their reported intention to smoke in the future (test for linearity = F1111 = 56.5; P <.001). The mean predicted probability of smoking during the next year was 6.6% (95% CI: 6.1% to 7.0%) for students who were not at all exposed to smoking in vehicles, 13.9% (95% CI: 11.5% to 16.3%) for students who were exposed 1 to 2 days per week, and 17.1% (95% CI: 13.2% to 21.0%) for students who were exposed 3 to 7 days per week. In an unadjusted model, exposure to smoking in cars both 1 to 2 days per week (OR = 3.40; 95% CI: 3.00 to 3.88) and 3 to 7 days per week (OR = 6.30; 95% CI: 5.23 to 7.58) were related to intention to smoke during the next year. In Table 2, models adjusted for sociodemographic characteristics (model 1) show a similar dose-response relationship that increases by the number of days exposed, with students who were exposed from 1 to 2 days (OR = 2.27; 95% CI: 1.86 to 2.76) and 3 to 7 days (OR = 3.03; 95% CI: 2.31 to 3.99) stating a greater likelihood of intending to smoke in the following year than those who were not exposed within the past week. This relationship persisted even after statistically controlling for other SHS exposure, although the relationship was attenuated (test for linearity = F1111 = 31.8; P < .001). Table 2 shows that intention to smoke increased with increasing grade level when controlling for sociodemographic characteristics. It also shows that non-Hispanic African Americans reported lower odds and Hispanics reported higher odds of intention to smoke compared with non-Hispanic whites when controlling for sociodemographic and other SHS exposure.
TABLE 2.
Exposure to Smoking in Cars in California in 2011 and Nonsmokers’ Intention to Smoke in the Next Year, Logistic Regression
| Factor | Model 1 | Model 2 | ||
|---|---|---|---|---|
| n = 23 394 | n = 21 716 | |||
| aOR | 95% CI | aOR | 95% CI | |
| SHS exposure in cars, d | ||||
| 0 | Ref | — | Ref | — |
| 1–2 | 2.27 | 1.86 to 2.76*** | 1.54 | 1.25 to 1.90*** |
| 3–7 | 3.03 | 2.31 to 3.99*** | 1.92 | 1.53 to 2.41*** |
| Sex | ||||
| Female | Ref | — | Ref | — |
| Male | 1.08 | 0.94 to 1.23 | 1.08 | 0.94 to 1.25 |
| Grade level | ||||
| Sixth | Ref | — | Ref | — |
| Seventh | 1.97 | 0.95 to 4.09 | 1.97 | 0.92 to 4.22 |
| Eighth | 3.29 | 1.57 to 6.90** | 3.45 | 1.62 to 7.35** |
| Ninth | 3.21 | 1.55 to 6.63** | 3.22 | 1.54 to 6.74** |
| 10th | 2.83 | 1.38 to 5.83** | 2.90 | 1.39 to 6.05** |
| 11th | 3.38 | 1.63 to 7.01** | 3.50 | 1.67 to 7.36** |
| 12th | 4.12 | 2.01 to 8.47*** | 4.20 | 2.02 to 8.76*** |
| Race and/or ethnicity | ||||
| White, non-Hispanic | Ref | — | Ref | — |
| African American, non-Hispanic | 0.74 | 0.56 to 0.98* | 0.60 | 0.46 to 0.79*** |
| Hispanic and/or Latino | 1.48 | 1.28 to 1.71*** | 1.54 | 1.33 to 1.79*** |
| Asian American, non-Hispanic | 0.86 | 0.67 to 1.11 | 0.86 | 0.65 to 1.13 |
| NH and/or PI, non-Hispanic | 1.12 | 0.67 to 1.85 | 1.04 | 0.61 to 1.78 |
| SHS in same room | — | — | 1.69 | 1.37 to 2.08*** |
| SHS in home | — | — | 0.77 | 0.54 to 1.08 |
| Live with smoker | — | — | 1.72 | 1.41 to 2.11*** |
All data presented are weighted to adjust for differential nonresponse and selection. All analyses in Models 1 and 2 were controlled for sex, grade level, and race and/or ethnicity. Model 2 further controlled for SHS in the same room, SHS in the home, and living with a smoker. aOR, adjusted odds ratio; NH, native Hawaiian; PI, Pacific Islander; —, not applicable.
P < .05 level; **P < .01; ***P < .001.
Discussion
The primary purpose of this study was to evaluate the association of California’s 2007 smoke-free vehicle law with students’ rates of self-reported exposure to smoking in vehicles. In this study, we showed that the observed 2001–2005 decline in California’s rates was smaller than the decline in US rates and accelerated significantly during the years of 2007 to 2011, during and after implementation of California’s smoke-free vehicle law, in contrast to the rate in United States as a whole, where the corresponding annual decline in 2006 to 2011 was only half of what it was from 2002 to 2006. Secondary analyses showed a positive dose-response relationship between exposure to smoking in vehicles and both students’ self-reported lifetime asthma diagnosis and intention to begin smoking in the future.
This current study builds on previous research in Canada and the United States showing decreasing rates of student-reported exposure to smoking in vehicles.46–48 Despite secular, national trends dating to 2000, a similar rate of decline was not observed for California’s middle and high school students during the period 2001 and 2005. It was only when a smoke-free vehicle law was being negotiated in 2007 by California legislators and ultimately signed into law that rates of California students reporting exposure to smoking in cars showed significant decreases over time.
Despite California’s reputation as a leader in tobacco control and its early adoption of policies prohibiting smoking in public spaces, the failure of California’s students to report any significant decline in exposure to smoking in cars during the 2001–2005 period, a time when US students were reporting a rapid decline, is striking. An obvious defense for California’s lack of progress in the 2001–2005 period is that its student-reported rates of exposure to smoking in cars were already so low that there was a floor effect. However, this possible explanation was dramatically undermined in the 2007–2011 period, immediately after the passage of California’s smoke-free car law, when California’s rates fell by 12% per year despite the absolute prevalence rates being already one-third lower than 2007 US rates. The relatively large drop in student-reported exposure to smoking in vehicles on the fall 2007 CSTS, even before the law’s official implementation, might have reflected increasing public awareness of the issue occasioned by the editorials, media attention, and legislative deliberations that preceded SB 7’s passage.45 Smoke-free car legislation having an effect just before its official implementation is a phenomenon that is also documented in the adoption of smoke-free car laws in several Canadian provinces.48
Overall trends at the national level showed increasingly steep declines in student exposure to smoking in cars during 2000 to 2006 but decreasingly steep declines after 2006. A small part of the decline up to 2006 may be attributed to smoke-free vehicle laws in Arkansas and Louisiana and smaller geographic locations affecting no more than 3 percent of the US population as of 2007.49 According to the Americans for Nonsmokers’ Rights Foundation, as of 2016, 12 localities and 8 states have adopted some kind of restriction on smoking in vehicles.30 The other states with current smoke-free vehicle laws include Utah, Louisiana, Arkansas, Oregon, Maine, Vermont, and Virginia.30 When including California, they represent ∼20% of the US population.50
Our secondary analyses showed a positive dose-response relationship between the frequency of exposure to SHS in cars with (1) lifetime risk of asthma diagnosis and (2) intention to begin smoking during the next year. This is 1 of the first studies in which researchers assess the relationship between lifetime asthma risk and exposure to smoking in cars among adolescents and supports previous findings in adults.25 This relationship persisted after adjusting for other potential SHS-exposure confounders. A greater exposure to smoking in cars was also positively associated with an increase in intention to smoke in the future among current nonsmokers. These findings support the expectation that decreasing exposure to SHS in cars will reduce the incidence of asthma and adolescent vulnerability to future cigarette smoking, thereby improving the health prospects of adolescents.
Findings based on the CSTS and the NYTS are subject to the usual limitations of self-report, cross-sectional surveys. More specifically, the CSTS was a tobacco use–specific self-report survey administered every other year between 2001 and 2012, administered only in California’s public schools, and completed anonymously to protect students’ privacy, so individuals could not be followed over time. Causal inferences are not possible with cross-sectional data. Nonetheless, these results are consistent with the expectation that prospective data would show that adopting a public policy to ban smoking in cars when minors are present could yield reductions in children’s exposure to smoking in vehicles.
Although student response rates typically exceeded 70%, and school response rates typically exceeded 80%,39 some bias was introduced by differential nonresponse in both the NYTS and CSTS. With both surveys, samples excluded dropouts, a significant problem for low-income school districts, such as the Los Angeles Unified School District, where the dropout rate is 17%.51 High school dropouts typically have a higher smoking prevalence than high school graduates.52 Comparing the California student tobacco use data with the corresponding NYTS data was problematic inasmuch as the NYTS data included California respondents, who could not be distinguished from respondents from other states by using the publicly available NYTS data. Therefore, the California-US differences over time in the rates of exposure to smoking in cars are even more striking given this bias toward null differences. Additionally, other states (representing 5% of US population) have adopted smoke-free vehicle laws during the survey periods examined here and thereby probably attenuated the contrasts between the United States and California. Yet another limitation in the NYTS data is that the question about exposure to smoking in vehicles was changed in 2011 to include exposure in any vehicle and to any combustible tobacco product. The relative lack of decline in student-reported exposure to smoking in vehicles between the 2009 and 2011 NYTS could be partly an artifact of the change in question wording. Despite these limitations, our findings offer guidance to researchers of future prospective studies of the health impact of statewide bans on smoking in cars when children are present.
Conclusions
Our findings suggest that the California smoke-free vehicle law was associated with reductions in student exposure to SHS not explainable by secular trends either in California or in the United States. We also found consistently positive associations between the number of days of exposure to smoking in cars with the probability of lifetime asthma diagnosis and the probability of nonsmokers intending to smoke in the future. The precautionary principle suggests that localities that are concerned with minimizing tobacco-related harms to children would be prudent to consider adopting smoke-free car laws similar to those implemented in 8 states and >12 other US political entities (eg, cities). Although there is reluctance among legislators to regulate smoking behavior in vehicles because they are private spaces where individuals have historically been protected from government intrusion, part of their reluctance may stem also from a lack of information about the possible health benefits of such laws. Legislators may not be aware that in a recent study in Canada limited to smokers with cars, most adult smokers, particularly those with university degrees, believed that protecting children from exposure to cigarette smoke in cars is necessary and that legislation designed to promote this would be effective.53 Furthermore, another recent repeated cross-sectional study of child reports of exposure to smoke in cars in the United Kingdom suggested that voluntary, self-imposed bans on smoking in cars yielded smaller declines in exposure than legislated bans.54 Our findings offer reassurance that smoke-free vehicle laws are likely to have salubrious effects on adolescent exposure to SHS and associated health outcomes. Our findings should encourage other researchers to prospectively evaluate the impact of future smoke-free vehicle laws adopted by other localities on SHS exposure and other SHS-related outcomes.
Glossary
- CI
confidence interval
- CSTS
California Student Tobacco Survey
- NYTS
National Youth Tobacco Survey
- OR
odds ratio
- SB 7
Senate Bill 7
- SHS
secondhand smoke
Footnotes
Dr Patel conceptualized and designed the study, conducted the initial analyses, and drafted the manuscript; Dr Thai assisted with drafting the manuscript and reviewed and revised the manuscript; Dr Meng provided crucial feedback in the conceptualization and design of the study; Dr Kuo assisted in conceptualizing and designing the study and provided crucial feedback on the initial analyses; Ms Zheng assisted with data management; Dr Dietsch helped design the data collection instruments, coordinated and supervised data collection for the California Student Tobacco Survey, and reviewed the manuscript; Dr McCarthy supervised the study, conceptualized and designed the study, conducted the final analyses, and drafted the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: Dr McCarthy was supported by contract CER-130601150 from the Patient-Centered Outcomes Research Institute and contract 01-90916 from the California Department of Public Health, and Dr Patel is currently a Cancer Prevention Postdoctoral Fellow at the National Cancer Institute. The opinions expressed in this article are the authors’ own and do not reflect the views of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1.Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality–beyond established causes. N Engl J Med. 2015;372(7):631–640 [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services . The Health Consequences of Smoking–50 Years of Progress. Atlanta, GA: Centers for Disease Control and Prevention; 2014 [Google Scholar]
- 3.Fuentes-Leonarte V, Estarlich M, Ballester F, et al. Pre- and postnatal exposure to tobacco smoke and respiratory outcomes during the first year. Indoor Air. 2015;25(1):4–12 [DOI] [PubMed] [Google Scholar]
- 4.Wang Z, May SM, Charoenlap S, et al. Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2015;115(5):396.e2–401.e2 [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health . 2012 Surgeon General’s report—preventing tobacco use among youth and young adults. 2012. Available at: www.cdc.gov/tobacco/data_statistics/sgr/2012/. Accessed December 30, 2012
- 6.Farber HJ, Groner J, Walley S, Nelson K; Section on Tobacco Control . Protecting children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5). Available at: www.pediatrics.org/cgi/content/full/136/5/e1439 [DOI] [PubMed] [Google Scholar]
- 7.Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2016;65(14):361–367 [DOI] [PubMed] [Google Scholar]
- 8.Distefan JM, Gilpin EA, Choi WS, Pierce JP. Parental influences predict adolescent smoking in the United States, 1989-1993. J Adolesc Health. 1998;22(6):466–474 [DOI] [PubMed] [Google Scholar]
- 9.Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, Niaura RS. Parental smoking exposure and adolescent smoking trajectories. Pediatrics. 2014;133(6):983–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander C, Piazza M, Mekos D, Valente T. Peers, schools, and adolescent cigarette smoking. J Adolesc Health. 2001;29(1):22–30 [DOI] [PubMed] [Google Scholar]
- 11.Song AV, Glantz SA, Halpern-Felsher BL. Perceptions of second-hand smoke risks predict future adolescent smoking initiation. J Adolesc Health. 2009;45(6):618–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilman SE, Rende R, Boergers J, et al. Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics. 2009;123(2). Available at: www.pediatrics.org/cgi/content/full/123/2/e274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Prev Med. 2003;36(3):272–281 [DOI] [PubMed] [Google Scholar]
- 14.Pickett MS, Schober SE, Brody DJ, Curtin LR, Giovino GA. Smoke-free laws and secondhand smoke exposure in US non-smoking adults, 1999-2002. Tob Control. 2006;15(4):302–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernando D, Fowles J, Woodward A, et al. Legislation reduces exposure to second-hand tobacco smoke in New Zealand bars by about 90%. Tob Control. 2007;16(4):235–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Callinan JE, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010;(4):CD005992. [DOI] [PubMed] [Google Scholar]
- 17.Farrelly MC, Nonnemaker JM, Chou R, Hyland A, Peterson KK, Bauer UE. Changes in hospitality workers’ exposure to secondhand smoke following the implementation of New York’s smoke-free law. Tob Control. 2005;14(4):236–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisner MD, Smith AK, Blanc PD. Bartenders’ respiratory health after establishment of smoke-free bars and taverns. JAMA. 1998;280(22):1909–1914 [DOI] [PubMed] [Google Scholar]
- 19.Akhtar PC, Currie DB, Currie CE, Haw SJ. Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ. 2007;335(7619):545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dove MS, Dockery DW, Connolly GN. Smoke-free air laws and secondhand smoke exposure among nonsmoking youth. Pediatrics. 2010;126(1):80–87 [DOI] [PubMed] [Google Scholar]
- 21.Akhtar PC, Haw SJ, Currie DB, Zachary R, Currie CE. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control. 2009;18(5):409–415 [DOI] [PubMed] [Google Scholar]
- 22.Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl 3):iii42–iii50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng K-W, Glantz SA, Lightwood JM. Association between smoke-free laws and voluntary smoke-free–home rules. Am J Prev Med. 2011;41(6):566–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dove MS, Dockery DW, Connolly GN. Smoke-free air laws and asthma prevalence, symptoms, and severity among nonsmoking youth. Pediatrics. 2011;127(1):102–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen KH, King BA, Dube SR. Association between current asthma and secondhand smoke exposure in vehicles among adults living in four US states. Tob Control. 2015;24(4):376–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson KM, Klein JD, Blumkin AK, Gottlieb M, Winickoff JP. Tobacco-smoke exposure in children who live in multiunit housing. Pediatrics. 2011;127(1):85–92 [DOI] [PubMed] [Google Scholar]
- 27.Thaqi A, Franke K, Merkel G, Wichmann HE, Heinrich J. Biomarkers of exposure to passive smoking of school children: frequency and determinants. Indoor Air. 2005;15(5):302–310 [DOI] [PubMed] [Google Scholar]
- 28.Global Tobacco Surveillance System Collaborative Group . A cross country comparison of exposure to secondhand smoke among youth. Tob Control. 2006;15(suppl 2):ii4–ii19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agaku IT, Singh T, Rolle I, Olalekan A-Y, King BA. Prevalence and determinants of secondhand smoke exposure among middle and high school students. Pediatrics. 2016;137(2):e20151985. [DOI] [PubMed] [Google Scholar]
- 30.Americans for Nonsmokers’ Rights Foundation . Smokefree cars. 2016. Available at: www.no-smoke.org/learnmore.php?id=616. Accessed May 28, 2016
- 31.Ott W, Klepeis N, Switzer P. Air change rates of motor vehicles and in-vehicle pollutant concentrations from secondhand smoke. J Expo Sci Environ Epidemiol. 2008;18(3):312–325 [DOI] [PubMed] [Google Scholar]
- 32.Oropeza J. California smoke-free cars law (SB 7). In: Senate Bill 7. California Legislature , ed. Sacramento, CA: California Legislature; 2007 [Google Scholar]
- 33.Larsson M, Boëthius G, Axelsson S, Montgomery SM. Exposure to environmental tobacco smoke and health effects among hospitality workers in Sweden–before and after the implementation of a smoke-free law. Scand J Work Environ Health. 2008;34(4):267–277 [DOI] [PubMed] [Google Scholar]
- 34.Tan CE, Glantz SA. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126(18):2177–2183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glantz SA. Meta-analysis of the effects of smoke-free laws on acute myocardial infarction: an update. Prev Med. 2008;47(4):452–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rayens MK, Burkhart PV, Zhang M, et al. Reduction in asthma-related emergency department visits after implementation of a smoke-free law. J Allergy Clin Immunol. 2008;122(3):537.e3–541.e3 [DOI] [PubMed] [Google Scholar]
- 37.Farber HJ, Walley SC, Groner JA, Nelson KE; Section on Tobacco Control . Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):1008–1017 [DOI] [PubMed] [Google Scholar]
- 38.Roeseler A, Solomon M, Beatty C, Sipler AM. The tobacco control network’s policy readiness and stage of change assessment: what the results suggest for moving tobacco control efforts forward at the state and territorial levels. J Public Health Manag Pract. 2016;22(1):9–19 [DOI] [PubMed] [Google Scholar]
- 39.Park H-Y, Dent C, Abramsohn E, Dietsch B, McCarthy WJ. Evaluation of California’s in-school tobacco use prevention education (TUPE) activities using a nested school-longitudinal design, 2003-2004 and 2005-2006. Tob Control. 2010;19(suppl 1):i43–i50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention . Current tobacco use among middle and high school students–United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(31):581–585 [PubMed] [Google Scholar]
- 41.Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addiction. 2001;96(2):313–323 [DOI] [PubMed] [Google Scholar]
- 42.Wakefield M, Kloska DD, O’Malley PM, et al. The role of smoking intentions in predicting future smoking among youth: findings from Monitoring the Future data. Addiction. 2004;99(7):914–922 [DOI] [PubMed] [Google Scholar]
- 43.Healey B, Hoek J, Wilson N, Thomson G, Taylor S, Edwards R. Youth exposure to in-vehicle second-hand smoke and their smoking behaviours: trends and associations in repeated national surveys (2006-2012). Tob Control. 2015;24(2):146–152 [DOI] [PubMed] [Google Scholar]
- 44.StataCorp . Release 13. Statistical Software. College Station, Texas: StataCorp LP; 2013 [Google Scholar]
- 45.California Legislature . SB-7 Smoking in vehicles with minor passengers. 2007. Available at: http://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=200720080SB7. Accessed May 30, 2016
- 46.King BA, Dube SR, Tynan MA. Secondhand smoke exposure in cars among middle and high school students–United States, 2000-2009. Pediatrics. 2012;129(3):446–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.King BA, Dube SR, Homa DM. Smoke-free rules and secondhand smoke exposure in homes and vehicles among US adults, 2009-2010. Prev Chronic Dis. 2013;10:E79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elton-Marshall T, Leatherdale ST, Driezen P, Azagba S, Burkhalter R. Do provincial policies banning smoking in cars when children are present impact youth exposure to secondhand smoke in cars? Prev Med. 2015;78:59–64 [DOI] [PubMed] [Google Scholar]
- 49.US Department of Commerce . Statistical abstract of the United States: 2008. Available at: www.census.gov/library/publications/2007/compendia/statab/127ed.html. Accessed June 11, 2016
- 50.US Department of Commerce . Statistical abstract of the United States: 2012. Available at: www.census.gov/library/publications/2011/compendia/statab/131ed.html. Accessed June 11, 2016
- 51.Los Angeles Unified School District . Graduation rates in L.A. Unified improve by race. 2014. Available at: https://home.lausd.net/apps/news/article/414445. Accessed June 5, 2017
- 52.Pirie PL, Murray DM, Luepker RV. Smoking prevalence in a cohort of adolescents, including absentees, dropouts, and transfers. Am J Public Health. 1988;78(2):176–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Montreuil A, Tremblay M, Cantinotti M, et al. Frequency and risk factors related to smoking in cars with children present. Can J Public Health. 2015;106(6):e369–e374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moore GF, Moore L, Littlecott HJ, et al. Prevalence of smoking restrictions and child exposure to secondhand smoke in cars and homes: a repeated cross-sectional survey of children aged 10-11 years in Wales. BMJ Open. 2015;5(1):e006914. [DOI] [PMC free article] [PubMed] [Google Scholar]