Abstract
OBJECTIVE:
To explore the relationship between prenatal hemoglobin (Hb) concentration and infant cognitive and motor functions.
METHODS:
Our prospective cohort study included 1-year-old children born to women enrolled at their first antenatal care (ANC) visit in Allada, Benin, before 29 weeks of pregnancy, within a trial comparing the efficacy of sulfadoxine-pyrimethamine and mefloquine. Hb concentrations of pregnant women were determined from venous blood samples collected at first and second ANC visits of at least 1-month interval and at delivery. Women were prescribed oral iron, folic acid, and anthelminthics after the first ANC visit. A total of 636 children (76.8% of eligible children) were assessed by trained research nurses for cognitive and motor functions by using the Mullen Scales of Early Learning.
RESULTS:
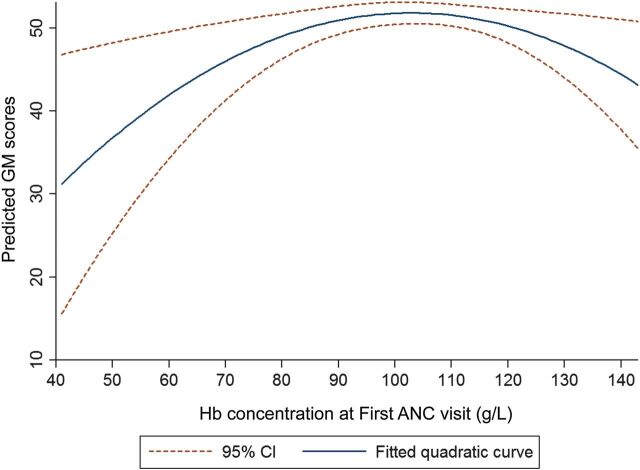
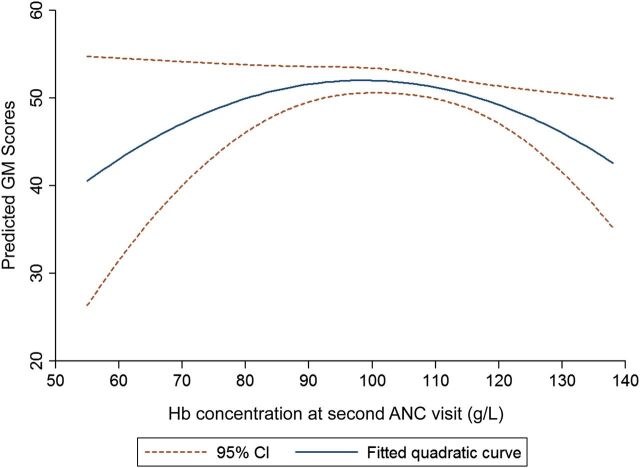
Prevalence of anemia (Hb < 110 g/L) decreased from 67.0% at first ANC visit (mean gestational age [SD], 22.1 [4.0] weeks) to 38.4% at delivery. Mean (SD) Hb concentrations increased from 103.7 (12.3) at first ANC visit to 112.4 (14.1) at delivery. We observed a significant negative quadratic relationship between infant gross motor (GM) function and Hb concentration at first and second ANC visits. Thus, infant GM scores increased sharply with increasing maternal Hb concentration until 90 g/L where increasing GM was mild, and began to decline after 110 g/L.
CONCLUSIONS:
There appears to be an Hb concentration range that may be optimal for GM function of 1-year-old children. This may reflect the importance of physiologic hemodilution, which occurs after the second trimester until 34 weeks of gestation.
What’s Known on This Subject:
Studies on the consequences of abnormal prenatal hemoglobin (Hb) concentration have focused on maternal morbidities and adverse birth outcomes. To date, very little is known about the association between prenatal Hb concentration and infant cognitive and motor functions.
What This Study Adds:
There is an inverted U-shaped relationship between maternal Hb concentration and infant gross motor function. Hb concentration between 90 and 110 g/L appears to be optimal for early gross motor function of children.
Early childhood, defined as the period from the prenatal phase until 8 years, 1 is the most critical developmental chapter of an individual’s life trajectory. During the prenatal phase, the fetus undergoes extensive series of events involving neural migration, synaptogenesis, hippocampal development, and myelination, 2 which provide the structural foundation for brain development and function. This later becomes evident in the early developmental domains (social-emotional, fine-gross motor [GM], and language-cognition) of the growing infant. Due to the sensitivity of the fetal brain, its development could be altered by exposure to prenatal insults such as infections, stress, toxins, nutrient deficiencies and ischemia. 3 , 4 Children with restricted prenatal development may potentially be mentally and socially impaired later in life.
A recent study in Benin suggests that maternal malnutrition, malaria infection, iron deficiency, helminth infection, and folate deficiency are the major risk factors for anemia in pregnant women at their first antenatal care (ANC) visits before treatments and micronutrient supplementation. 5 Although access to iron and folic acid (IFA) supplements, intermittent preventive treatment of malaria in pregnancy (IPTp), and the use of anthelminthics during pregnancy are being achieved, the burden of anemia in least developed countries remain unacceptably high. 6 In Africa, anemia in pregnancy (hemoglobin [Hb] concentration <110 g/L) is a severe public health problem estimated to be affecting over 17 million pregnant women. 7
Significant increase, as well as decrease, in Hb concentration in pregnancy may imply deprivation of iron, oxygen, and other essential micronutrients to fetus for development. A study by Gonzales et al 8 revealed a U-shaped relationship between prenatal Hb and the risk of adverse birth outcomes. They observed that low prenatal Hb (<90 g/L) is associated with increased odds of stillbirths and preterm births and small-for-gestational age likewise Hb concentrations greater than 150 g/L. 8 However, to date, little is known about the impact of prenatal Hb levels on early child psychomotor development.
Considering the evidence of adverse effects of low and high Hb levels during pregnancy, we hypothesized an inverted U-shaped relationship between infant cognitive and motor scores and maternal Hb during pregnancy. We therefore explored whether there was a nonlinear relationship between prenatal Hb at different periods of pregnancy and cognitive and GM development of 1-year-old children in Benin. We also compared the cognitive and motor functions of children of anemic and nonanemic women.
Methods
Population
This prospective study (called TOVI) included 636 1-year-old surviving singletons born to women enrolled in the Malaria in Pregnancy Preventive Alternative Drugs (MiPPAD) study (NCT00811421). MiPPAD was a clinical trial comparing the efficacy of sulfadoxine pyrimethamine and mefloquine as IPTp. Inclusion and exclusion criteria for the clinical trial are fully explained elsewhere. 9 Briefly, HIV-negative women who were at most 28 weeks pregnant and had not taken IPTp, IFA supplements, anthelmintics, or vitamin B12 since conception were recruited in maternity clinics in 3 subdistricts of Allada, Benin, during their first ANC visit.
Data and Hb Assessment During Pregnancy and at Birth
Maternal education, gravidity, gestational age, weight, and height were determined at first ANC. Maternal prepregnancy BMI was calculated by using a method detailed in a previous publication. 5
At 2 ANC visits, of at least 1-month interval, and at delivery, venous blood was obtained for analyses. Ten microliters of each blood sample was placed into a cuvette of the Hemo-Control photometer (EFK Diagnostics, Magdeburg , Germany) to measure the Hb concentration. Quality control was ensured by daily calibration of the Hemo-Control device by laboratory technicians and by crosschecking the Hb of 1 in 10 consecutive samples at the Allada Central Hospital laboratory by using a hematology analyzer (Erma Laboratory, Tokyo, Japan). Alkaline electrophoresis on cellulose acetate (Helena Laboratories, Beaumont, TX) was used to determine Hb genotypes.
Anemia was defined as Hb <110 g/L. After each assessment, pregnant women with Hb between 70 g/L and 110 g/L were treated with 400 mg of oral ferrous sulfate (200 mg twice daily) in accordance with the national guidelines. Those with Hb below 70 g/L were referred to a district tertiary hospital for blood transfusion. Per the guidelines of Beninese Ministry of Health, oral ferrous sulfate (200 mg daily) and folic acid (5 mg daily) supplements were provided for all pregnant women after the first ANC visit until 3 months after delivery. Additionally, 600 mg of mebendazole were given to pregnant woman in the second trimester. During the study period, drugs and nutrient supplements were given to women without charge.
Assessments at Age 1 Year
Research nurses were trained specifically to administer and score the cognitive and motor tests. Cognitive and motor functions of 636 1-year-old children were assessed by using the Mullen Scales of Early Learning (MSEL), 10 which was translated and adapted for this setting. 11 The MSEL encompasses the developmental domains of childhood and consists of 5 scales: GM, fine motor, language reception, language expression, and visual reception. After scoring each item, crude scores obtained from each of the 5 scales were transformed into normalized age-specific scores called T scores. Three children who obtained crude scores lower than 5 were given the least T score in the corresponding scale. T scores of all but GM scale were summed and converted to obtain the Early Learning Composite (ELC) scores. 12
The quality of the home environment (using the Home Observatory Measurement of the Environment [HOME] inventory), 13 postnatal depression (using the Edinburgh Postnatal Depression Scale), 14 maternal nonverbal intelligent quotient (using the Raven’s Progressive Matrices test), 15 and infant anthropometric measurements were also assessed at 1 year of age.
Statistical Analyses
Summary statistics and distributional analyses were performed for all variables independently. The 2 dependent variables used in the analyses were the ELC and GM scores. The main independent variables were Hb concentrations (g/L) measured at first and second ANC visits and at delivery. The Hb concentrations were also categorized to reflect the anemia status of pregnant women.
We performed crude linear regression analyses between ELC and GM scores, and Hb concentration and anemia at each ANC visit and at delivery, separately. Bivariate analyses were performed to determine the correlation between covariates maternal and infant characteristics and ELC and GM scores. Direct acyclic graph was used to justify potential confounding. 16 Covariates that were associated with the ELC and crude GM scores at P < .20 were selected for multiple regression analyses. Stepwise removal of covariates was performed until all covariates in the models remained significant. 17 Because Hb physiologically varies with gestational age, gestational age (trimesters) at time of Hb assessment was kept in the adjusted models even if it was not significant. Because of the physiologic increase in Hb toward the end of pregnancy, 18 preterm births were excluded only when establishing the association between Hb concentration at delivery and infant ELC and GM scores (model II).
Afterward, we explored possible nonlinearity of the association between the ELC and GM scores and Hb at each ANC visit and at delivery by using Box-Cox right-hand-side only transformation with a maximum iteration of 10. We fixed the Box-Cox regression such that only Hb was transformable as specified in the equation:
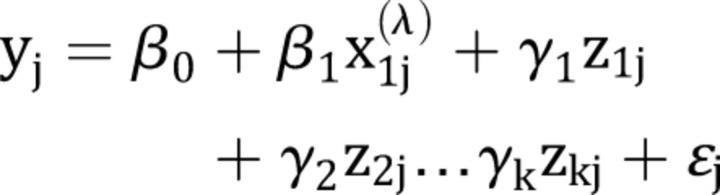 |
where y is the ELC or GM score, x1 is the Hb concentration (the only variable transformed by a Box-Cox transform parameter λ), and z1, z2…zk are the covariates selected into the model and they were untransformed. 19
The Box-Cox regression analyses were run for the association between GM and ELC scores and Hb concentrations at each ANC visit and at delivery. When nonlinearity was confirmed, a quadratic transformation of the Hb variable was used in the multiple regression models as we had hypothesized a plausible inverted U-shaped relationship (model III). Selected confounders were not in the causal pathway of prenatal Hb concentration and infant GM scores.
In a subsequent sensitivity analysis, we further adjusted model III for other known causes of anemia during pregnancy such as iron deficiency, malaria, and helminth infection at the time of assessment while retaining the previous covariates in the model (model IV).
All statistical analyses were conducted by using Stata IC/12.1 (Stata Corp, College Station, TX).
Ethical Considerations
The study was approved by the institutional review boards of the University of Abomey-Calavi (Benin), New York University, Michigan State University, and the Research Institute for Development’s Consultative Ethics Committee (France). At recruitment, we obtained informed consent from all pregnant women and guardians of children who participated in this study.
Results
A total of 636 children (76.8% of 828 eligible) were followed until age 1 year. A flowchart of the follow-up of pregnant women and children has been published elsewhere. 20 Maternal baseline characteristics were similar between children not assessed and those assessed at age 1 year. 20 Mean maternal age (SD) at first ANC visit was 26.8 (5.6) years. The prevalence of malaria was 16.0% at first ANC visit, declined to 3.7% at second ANC visit, and then increased to 10.6% at delivery. Seven percent of children were born preterm, and 9.6% weighed <2500 g at birth (Supplemental Table 5). Mean (SD) Hb at first ANC visit was 103.7 (12.3), 105.4 (10.6) at second ANC visit, and 112.4 (14.1) at delivery. Anemia during pregnancy declined from 67.0% at first ANC visit to 38.4% at delivery (Table 1).
TABLE 1.
Gestational Age and Hb Distribution Among Women Whose Children Were Assessed for Cognitive and Motor Function at Age 1 y
| First ANC Visit, N = 636 | Second ANC Visit, N = 627 | Delivery, N = 609 | |
|---|---|---|---|
| Gestational age, wk | |||
| Mean | 22.0 | 28.8 | 38.3 a |
| SD | 3.9 | 3.8 | 3.2 |
| Range | 10–28 | 18–40 | 23–55 |
| Hb, g/L | |||
| Mean | 103.7 | 105.4 b | 112.4 |
| SD | 12.3 | 10.6 | 14.1 |
| Range | 41–143 | 55–138 | 40–168 |
| Anemia, Hb < 110 g/L | |||
| n (%) | 426 (67.0) | 403 (64.4) | 234 (38.4) |
N = 596.
N = 626.
Table 2 shows the associations between maternal and infant characteristics and mean ELC and GM scores. Women who had at least primary education had children with significantly better cognitive and motor function than those who had never schooled (P < .001). Underweight women had children with the least GM scores. Family possession scores, Raven’s Progressive Matrices, and HOME scores and infant weight at age 1 year were positively correlated with both ELC and GM scores.
TABLE 2.
Associations Between Characteristics of Pregnant Women and Children and ELC and GM Scores
| Characteristics | ELC Score | GM Score | ||
|---|---|---|---|---|
| N = 636 | Mean | P | Mean | P |
| Gender | ||||
| Girl | 99.2 | .21 | 50.2 | .14 |
| Boy | 97.8 | 51.8 | ||
| Weight-for-age z score a | 0.2 c | <.001 | 0.3 c | <.001 |
| Gravidity | ||||
| Primigravida | 99.8 | .28 | 48.2 | .02 |
| Multigravida | 98.2 | 51.6 | ||
| Maternal education | ||||
| Never schooled | 96.2 | <.001 | 49.4 | <.001 |
| Primary or more | 102.9 | 54.1 | ||
| Maternal occupation | ||||
| Housewives | 96.1 | <.001 | 49.2 | .002 |
| Employed | 100.8 | 52.8 | ||
| Prepregnancy BMI | ||||
| Underweight | 96.4 | .07 | 48.9 | .03 |
| Normal | 98.6 | 50.9 | ||
| Overweight/obese | 101.5 | 54.8 | ||
| Family possession score b | 0.1 c | .005 | 0.2 c | <.001 |
| HOME score b | 0.2 c | <.0001 | 0.2 c | <.001 |
| RPM score b | 0.1 c | .03 | 0.1 c | .002 |
| EPDS score b | −0.0 c | .98 | −0.0 c | .67 |
EPDS, Edinburgh Postnatal Depression Scale; RPM, Raven’s Progressive Matrices.
N = 629.
N = 631.
Represented as correlation coefficients not means.
As shown in Table 3, prenatal anemia at both ANC visits and at delivery were not associated to ELC scores even after adjusting for confounders. However, in the adjusted model, children of anemic mothers had better GM scores 2.3 (95% confidence interval [CI]: 0.1 to 4.6) than those of nonanemic mothers.
TABLE 3.
Relationship Between Prenatal Anemia and ELC and GM Scores
| Anemia | ELC Score | GM Score | ||
|---|---|---|---|---|
| Crude Mean Difference (95% CI) | Adjusted Mean Difference (95% CI) a | Crude Mean Difference (95% CI) | Adjusted Mean Difference (95% CI) b | |
| First ANC visit | ||||
| No anemia | Reference | Reference | Reference | Reference |
| Anemia | −1.0 (−3.4 to 1.4) | −0.4 (−2.7 to 1.9) | 0.4 (−2.0 to 2.7) | 1.6 (−0.7 to 3.9) |
| Second ANC visit | ||||
| No anemia | Reference | Reference | Reference | Reference |
| Anemia | 0.5 (−1.8 to 2.8) | 0.6 (−1.6 to 2.9) | 2.2 (−0.2 to 4.5) | 2.3 (0.1 to 4.6)* |
| Delivery | ||||
| No anemia | Reference | Reference | Reference | Reference |
| Anemia | −0.7 (−3.1 to 1.7) | −0.6 (−2.9 to 1.8) | −1.1 (−3.5 to 1.4) | −0.6 (−3.0 to 1.8) |
P < 0.05
Adjusted for maternal education, infant weight-for-age z score, HOME score, and gestational age at blood assessment.
Adjusted for maternal education, gravidity, family possession, infant weight-for-age z score, HOME score, and gestational age at Hb assessment.
The HOME score, maternal education, and infant weight-for-age covariates that were strongly related to both GM and ELC scores were selected for the Box-Cox regression. The coefficients of the transformed Hb at all 3 assessments (β1) were not significant for the models for ELC score and Hb concentrations. For the adjusted models involving GM score and Hb, we found that β1 were significant for Hb at first and second ANC visits and in addition, the model rejected the hypothesis that the model is linear; indicating that quadratic transformation of Hb at the first and second ANC could be used as hypothesized.
As shown in Table 4, the regression coefficient of the quadratic terms was negative and significant for the associations between Hb at first and second ANC visits and GM function at age 1 year. Diagrammatic representation of the nature of the association between prenatal Hb at first and second ANC visit and GM score are shown in Figs 1 and 2, respectively. In both figures, the GM for 1-year-old children increased sharply with increasing prenatal Hb until 90 g/L where the increase was steady then declined sharply over Hb level of 110 g/L. The peak for the quadratic curves was 98 g/L and 97 g/L at first and second ANC visits, respectively.
TABLE 4.
Linear and Quadratic Models for the Association Between Maternal Hb Concentration and Infant ELC and GM Scores
| Model I, β (95% CI) | Model II, β (95% CI) | Model III, β (95% CI) a | Model IV, β (95% CI) a | |
|---|---|---|---|---|
| ELC score | ||||
| First ANC visit | 0.05 (−0.04 to 0.14) | 0.03 (−0.06 to 0.11) | NA | NA |
| Second ANC visit | 0.02 (−0.09 to 0.12) | −0.00 (−0.10 to 0.10) | NA | NA |
| Delivery | 0.03 (−0.06 to 0.12) | 0.02 (−0.07 to 0.10) | NA | NA |
| GM score | ||||
| First ANC visit | 0.02 (−0.07 to 0.11) | −0.04 (−0.13 to 0.05) | −5.5 × 10−3 (−9.5 × 10−3 to −1.4 × 10−3)** | −5.6 × 10−3 (−9.6 × 10−3 to −1.6 × 10−3)** |
| Second ANC visit | −0.06 (−0.17 to 0.04) | −0.09 (−0.19 to 0.01) | −6.6 × 10−3 (−1.2 × 10−2 to −9.2 × 10−4)** | −7.0 × 10−3 (−1.3 × 10−2 to −1.2 × 10−3)* |
| Delivery | −0.02 (−0.11 to 0.07) | −0.04 (−0.13 to 0.05) | NA | NA |
Model I, crude (unadjusted); Model II, linear model adjusted for maternal education, infant weight-for-age z score, HOME score, and gestational age at blood assessment (for ELC score) and in addition, gravidity, family possession (for GM score); Model III, quadratic model adjusted for maternal education, gravidity, family possession, infant weight-for-age z score, HOME score, and gestational age at Hb assessment; Model IV, Model III + adjusting for iron deficiency, helminth, and malaria at respective ANC visit; NA, not applicable. *P < .05; **P < .01.
β (95% CI) for the quadratic term for Hb.
FIGURE 1.
Relationship between Hb concentration at first ANC visit and infant GM scores. The solid line indicates the fitted model, whereas the dash lines represent 95% CIs.
FIGURE 2.
Relationship between Hb concentration at second ANC visit and infant GM scores. The solid line indicates the fitted model, whereas the dash lines represent 95% CIs.
Discussion
To our knowledge, this study is the first to investigate the relationship between Hb levels at different periods during pregnancy and infant cognitive development. This study reveals that there is an inverted U-shaped relationship between prenatal Hb at first and second ANC visits and infant GM function indicating that low and high Hb concentrations during pregnancy may be detrimental to the early motor functions of 1-year-old children. Peak infant GM scores were observed at prenatal Hb of 98 g/L and 97 g/L at first and second ANC visits, respectively. However, prenatal anemia was associated with high GM scores at second ANC visit.
An important strength of our study is that we assessed Hb at different times during pregnancy. Also, the follow-up of 76.4% of eligible children recorded in this study is appreciable because it compares well to other mother–child cohorts in Africa. 21 Additionally, the MSEL used is a comprehensive tool for cognitive and motor assessment of children. Further, the consideration of several potential confounders in our study such as socioeconomic factors, mother–child interaction, maternal postnatal depression, and maternal IQ based on statistical significance and direct acyclic graphs contributes to the strength of this study.
During pregnancy, there is a ∼50% physiologic increase in plasma volume, peaking between 28 to 34 weeks of gestation, and a disproportionate 20% to 30% increase in red cell mass, which results in a decrease Hb concentration. 22 This hemodilution during the second and third trimesters may be essential for fetal growth as the reduced thickness of the blood enhances effective flow of oxygen and other nutrients to the fetus. 22 This could explain 2 observations in our results. Firstly, the observed high motor function among children of anemic women at second ANC visit when more than 50% of women were between 28 and 34 weeks of gestation. Secondly, the optimum GM function observed among children of pregnant women with Hb levels between 90 and 110 g/L at first and second ANC visits even after adjusting for other known risk factors for low maternal Hb. This Hb range (90–100 g/L) for optimum GM function, considered anemic, raises questions about the cutoff for anemia.
Low GM function was observed at low Hb levels on the left end of the inverted U-shaped curve. The observed low levels of Hb among pregnant women at first ANC visit could be a result of pathologic anemia due to malaria, helminths, and iron deficiency among other unmeasured micronutrient deficiencies that are risk factors. Low Hb levels at second ANC visit could be due to a combination of the aforementioned etiologies and physiologic increase in plasma volume. 23 Extremely low Hb concentration implies deficient oxygen transport to the fetus. 24 Although the fetus has mechanisms to adapt to decreased maternal oxygen delivery, the costs of such adaptation could be expensive, possibly leading to impaired fetal growth. 22
Low Hb levels during pregnancy could diminish the amount of accessible iron for the fetus. Iron availability is essential for effective fetal growth and function of several organ systems including the brain and skeletal muscle. 25 Prenatal iron deficiency is associated with decreased apical dendrite length and could alter the hippocampal development even in the early stages of pregnancy. 25 , 26 The apical dendrites in the hippocampus play a substantial role in memory and sensory functions. Studies in pregnant mice have also revealed that there is a direct relationship between maternal iron levels and fetal brain iron. 27 Low fetal brain iron could be responsible for the poor neuromotor skills in infants as a study revealed that 1-year-old children with brain iron deficiency (≤34 µg/L) had slower motor development compared with those with adequate brain iron. 27 , 28 However, the inverted U-shaped association persisted at second ANC visit after women were given IFA supplements and even after adjusting for iron deficiency, helminth, and malaria suggesting that we really measured the effect of Hb on motor function.
Conversely, higher than normal prenatal Hb could be due to nonexpansion of plasma and as a result, increased blood viscosity. Increased viscosity implies reduced blood flow to the intervillous space. 22 This could lead to fetal stress due to placental-fetal perfusion and consequently impair the development of essential fetal organs. 22 This condition of hemoconcentration could explain the right-hand-side of the quadratic curves where increasing Hb concentrations during pregnancy were associated with decreasing infant GM scores and may reflect the disadvantage of hemoconcentration during pregnancy.
The curvilinear nature of the observed relationship in our study is analogous to that between prenatal Hb and low birth weight. 29 , 30 Maternal Hb concentration is a predictor of pregnancy complications and several adverse birth outcomes such as low birth weight, stillbirth, and preterm birth ,which could mediate the pathway between prenatal Hb and infant GM function. 31 These adverse birth outcomes have been identified to be risk factors for poor cognitive and motor development. 32 , 33 A study of ∼223 000 singleton pregnancies also revealed a U–shaped relationship between maternal Hb concentration and early neonatal mortality with the lowest perinatal mortality in the 90 to 110 g/L Hb range. 34
Chang et al 35 suggested that children born to women who were anemic at the third trimester performed significantly lower than those of nonanemic women in cognitive assessment tests, but the authors did not assess the relationship between Hb concentration, as a continuous variable, and the cognitive scores. Contrary to the findings of Chang et al, 35 we observed no significant association between maternal anemia and infant cognitive function of our study. In the aforementioned study, the authors only assessed Hb in the third trimester with anemia prevalence of 45.2%. They also stated that anemia in the study population was mainly due to iron deficiency, which could explain the difference in findings. In our study population, prenatal anemia was multifactorial. 5
Pregnant women were enrolled in a clinical trial and as a result received several interventions that are likely to improve maternal health, birth outcomes, and neonatal health and potentially influence the cognitive function of children. Hence, our study is likely to underestimate the real magnitude of the effect of low and high maternal Hb on offspring cognitive development in the population who may seek fewer than 2 ANC visits during pregnancy. Also, caution should be taken in interpreting our results especially in the extreme ends of the curve as the CIs are wider due to the small number of observations.
Conclusions
This study reveals that there is an inverted U-shaped relationship between maternal Hb concentration during pregnancy and motor function of 1-year-old children. There appears to be an optimal range maternal Hb (90–110 g/L) that may be beneficial to infant GM function. It is the first study to report a quadratic relationship between prenatal Hb concentration and GM development of infants. Further studies are required to corroborate this curvilinear association. A follow-up study to investigate if this association persists even in the later life of the children is also necessary.
Supplementary Material
Acknowledgments
We thank all mothers and children who participated in this study. We also thank the staff of the 3 health centers (Allada, Attogon, and Sékou). We thank Dr Jules Alao for his contribution to this work. We also thank Gilles Cottrell for reviewing our statistical analysis. Finally, we thank the entire TOVI and MiPPAD field personnel, especially Romeo Zoumenou, who were involved in data collection.
Glossary
- ANC
antenatal care visit
- CI
confidence interval
- ELC
Early Learning Composite
- GM
gross motor
- Hb
hemoglobin
- HOME
Home Observatory Measurement of the Environment
- IFA
iron and folic acid
- IPTp
intermittent preventive treatment of malaria in pregnancy
- MiPPAD
Malaria in Pregnancy Preventive Alternative Drugs
- MSEL
Mullen Scales of Early Learning
Footnotes
Mr Mireku coordinated and supervised data collection of the TOVI study from the 3 study sites, performed and interpreted data analyses, drafted the initial manuscript, and revised the final manuscript; Dr Davidson designed the TOVI study and critically reviewed and revised the manuscript; Dr Koura supervised initial data collection of the TOVI study and critically reviewed and revised the manuscript; Drs Ouédraogo and Accrombessi designed, coordinated, and supervised data collection of the Malaria in Pregnancy Preventive Alternative Drugs (MiPPAD) clinical trial from the 3 study sites and reviewed the manuscript; Dr Boivin trained research nurses to use the Mullen Scales of Early Learning cognitive assessment, and critically reviewed and revised the manuscript; Dr Xiong designed the TOVI study, assisted in statistical analyses, and reviewed and revised the initial manuscript; Drs Massougbodji and Cot acquired funding for the MiPPAD study, conceptualized, designed, and supervised the MiPPAD trial, and reviewed and revised the initial manuscript; Dr Bodeau-Livinec conceptualized and designed the TOVI study, acquired funding for the TOVI study, trained research nurses to use the Mullen Scales of Early Learning cognitive assessment, supervised initial data collection, and reviewed and revised the initial manuscript; and all authors approved the final manuscript as submitted.
FUNDING: The Eunice Kennedy Shriver National Institute of Child Health and Human Development funded The TOVI study, grant R21-HD060524. The Malaria in Pregnancy Preventive Alternative Drugs trial (NCT00811421) was co-funded by the European and Developing Countries Clinical Trials Partnership (EDCTP- IP.07.31080.002).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.World Health Organization. Early child development: a powerful equalizer. Geneva, Switzerland: World Health Organization; 2007. Available at: www.who.int/maternal_child_adolescent/documents/ecd_final_m30/en/. Accessed May 12, 2014
- 2. Tau GZ , Peterson BS . Normal development of brain circuits. Neuropsychopharmacology. 2010;35(1):147–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barth AMI , Mody I . Changes in hippocampal neuronal activity during and after unilateral selective hippocampal ischemia in vivo. J Neurosci. 2011;31(3):851–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garner AS , Shonkoff JP Committee on Psychosocial Aspects of Child and Family Health Committee on Early Childhood, Adoption, and Dependent Care Section on Developmental and Behavioral Pediatrics . Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e224 [DOI] [PubMed] [Google Scholar]
- 5. Ouédraogo S , Koura GK , Accrombessi MMK , Bodeau-Livinec F , Massougbodji A , Cot M . Maternal anemia at first antenatal visit: prevalence and risk factors in a malaria-endemic area in Benin. Am J Trop Med Hyg. 2012;87(3):418–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Klemm RDW , Sommerfelt AE , Boyo A , et al. Are We Making Progress on Reducing Anemia in Women? Cross-Country Comparison of Anemia Prevalence, Reach, and Use of Antenatal Care and Anemia Reduction Interventions. Washington, DC: Academy for Educational Development, A2Z: The USAID Micronutrient and Child Blindness Project; 2011. [Google Scholar]
- 7.World Health Organization. Worldwide prevalence of anaemia 1993–2005. Geneva, Switzerland: World Health Organization; 2008. Available at: www.who.int/vmnis/publications/anaemia_prevalence/en/. Accessed March 24, 2014
- 8. Gonzales GF , Steenland K , Tapia V . Maternal hemoglobin level and fetal outcome at low and high altitudes. Am J Physiol Regul Integr Comp Physiol. 2009;297(5):R1477–R1485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. González R , Mombo-Ngoma G , Ouédraogo S , et al. Intermittent preventive treatment of malaria in pregnancy with mefloquine in HIV-negative women: a multicentre randomized controlled trial. PLoS Med. 2014;11(9):e1001733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mullen EM . Mullen Scales of Early Learning: AGS Edition. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 11. Koura KG , Boivin MJ , Davidson LL , et al. Usefulness of Child Development Assessments for Low-Resource Settings in Francophone Africa. J Dev Behav Pediatr. 2013;34(7):486–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dumont R , Cruse CL , Alfonso V , Levine C . Book Review: Mullen Scales of Early Learning: AGS Edition. J Psychoed Assess. 2000;18(4):381–389 [Google Scholar]
- 13. Caldwell BM , Bradley RH . Home Inventory Administration Manual. Little Rock, AR: University of Arkansas for Medical Sciences; 2001. [Google Scholar]
- 14. Cox JL , Holden JM , Sagovsky R . Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786 [DOI] [PubMed] [Google Scholar]
- 15. Raven J . The Raven’s progressive matrices: change and stability over culture and time. Cognit Psychol. 2000;41(1):1–48 [DOI] [PubMed] [Google Scholar]
- 16. Merchant AT , Pitiphat W . Directed acyclic graphs (DAGs): an aid to assess confounding in dental research. Community Dent Oral Epidemiol. 2002;30(6):399–404 [DOI] [PubMed] [Google Scholar]
- 17. Hosmer DW Jr , Lemeshow S , Sturdivant RX . Applied Logistic Regression, 3rd ed. Hoboken, NJ: John Wiley & Sons; 2013:107–133 [Google Scholar]
- 18. Klebanoff MA , Shiono PH , Selby JV , Trachtenberg AI , Graubard BI . Anemia and spontaneous preterm birth. Am J Obstet Gynecol. 1991;164(1 pt 1):59–63 [DOI] [PubMed] [Google Scholar]
- 19. Drukker DM . sg130: Box–Cox regression models. Stata Tech Bull. 2000;54:27–36 [Google Scholar]
- 20. Mireku MO , Boivin MJ , Davidson LL , et al. Impact of Helminth Infection during Pregnancy on Cognitive and Motor Functions of One-Year-Old Children. PLoS Negl Trop Dis. 2015;9(3):e0003463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Campbell A , Rudan I . Systematic review of birth cohort studies in Africa. J Glob Health. 2011;1(1):46–58 [PMC free article] [PubMed] [Google Scholar]
- 22. Blackburn S . Maternal, Fetal, & Neonatal Physiology: A Clinical Perspective, 4th ed. Amsterdam, The Netherlands: Elsevier Health Sciences; 2014:216–218 [Google Scholar]
- 23. Blackburn ST . Maternal, Fetal, & Neonatal Physiology: A Clinical Perspective, 3rd ed. Amsterdam, The Netherlands: Elsevier Health Sciences; 2007:227–237 [Google Scholar]
- 24. Lyndon A , Ali LU , eds. Fetal Heart Monitoring Principles and Practices. 4th ed. Dubuque, IA: Kendall Hunt; 2009:27–30 [Google Scholar]
- 25. He M , Jiang J , Liu S , Cheng H . Effect of iron supplementation on glucose transporter 4 expression in adipose tissue and skeletal muscle of pregnant rats. Open J Obstet Gynecol. 2013;3(6):500–507 [Google Scholar]
- 26. McLane JA , Fell RD , McKay RH , Winder WW , Brown EB , Holloszy JO . Physiological and biochemical effects of iron deficiency on rat skeletal muscle. Am J Physiol. 1981;241(1):C47–C54 [DOI] [PubMed] [Google Scholar]
- 27. Hubbard AC , Bandyopadhyay S , Wojczyk BS , Spitalnik SL , Hod EA , Prestia KA . Effect of dietary iron on fetal growth in pregnant mice. Comp Med. 2013;63(2):127–135 [PMC free article] [PubMed] [Google Scholar]
- 28. Siddappa AM , Georgieff MK , Wewerka S , Worwa C , Nelson CA , Deregnier R-A . Iron deficiency alters auditory recognition memory in newborn infants of diabetic mothers. Pediatr Res. 2004;55(6):1034–1041 [DOI] [PubMed] [Google Scholar]
- 29. Sekhavat L , Davar R , Hosseinidezoki S . Relationship between maternal hemoglobin concentration and neonatal birth weight. Hematology. 2011;16(6):373–376 [DOI] [PubMed] [Google Scholar]
- 30. Chumak EL , Grjibovski AM . Association between different levels of hemoglobin in pregnancy and pregnancy outcomes: a registry-based study in Northwest Russia. Int J Circumpolar Health. 2011;70(5):457–459 [DOI] [PubMed] [Google Scholar]
- 31. Stephansson O , Dickman PW , Johansson A , Cnattingius S . Maternal hemoglobin concentration during pregnancy and risk of stillbirth. JAMA. 2000;284(20):2611–2617 [DOI] [PubMed] [Google Scholar]
- 32. Tong S , Baghurst P , McMichael A . Birthweight and cognitive development during childhood. J Paediatr Child Health. 2006;42(3):98–103 [DOI] [PubMed] [Google Scholar]
- 33. Larroque B , Ancel P-Y , Marret S , et al. EPIPAGE Study group . Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371(9615):813–820 [DOI] [PubMed] [Google Scholar]
- 34. Little MP , Brocard P , Elliott P , Steer PJ . Hemoglobin concentration in pregnancy and perinatal mortality: a London-based cohort study. Am J Obstet Gynecol. 2005;193(1):220–226 [DOI] [PubMed] [Google Scholar]
- 35. Chang S , Zeng L , Brouwer ID , Kok FJ , Yan H . Effect of iron deficiency anemia in pregnancy on child mental development in rural China. Pediatrics. 2013;131(3). Available at: www.pediatrics.org/cgi/content/full/131/3/e755 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.