Abstract
Background
Sedation and analgesia are the integral components of modern-day upper gastrointestinal (GI) endoscopic procedures. Irrespective of the sedative agent, hypoxia is the most commonly encountered unwarranted event with sedation. The current study intends to scrutinize whether high-flow nasal oxygen (HFNO) is advantageous for providing respiratory support during upper GI endoscopic procedures over other conventional low-flow oxygen delivery modalities, e.g. nasal cannula, facemask, etc.
Methods
An extensive screening of electronic databases was done till July 31, 2022, after enlisting in International prospective register of systematic reviews (PROSPERO) (CRD42021245409). Randomized controlled trials (RCT), comparative cohort studies, case series, cross-sectional studies and case–control studies evaluating the utility of HFNO during upper GI endoscopy under sedation were included in this meta-analysis.
Results
We retrieved eight randomized control studies and one longitudinal study with 3294 patients. The application of HFNO during endoscopy led to lesser incidence of desaturation spells (odds ratio [OR] = 0.23; 95% CI 0.11–0.48; I2 = 71%), reduced procedural interruption (OR = 0.11; 95% CI 0.02–0.60; I2 = 88%), better nadir SpO2 level during procedure (mean difference [MD] = 3.16; 95% CI 0.54–5.78; I2 = 73%), overall lesser incidence of sedation-related adverse events (OR = 0.63; 95% CI 0.42–0.93; I2 = 25%), with no significant impact on the duration of endoscopy (MD = 0.15; 95% CI − 0.02 to 0.31, I2 = 0%).
Conclusion
HFNO is a novel option for upper GI endoscopy under sedation.
Clinical trial number and registry URL
CRD42021245409 (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021245409).
Supplementary Information
The online version contains supplementary material available at 10.1007/s12664-022-01308-6.
Keywords: Adverse events, Endoscopy, High-flow nasal oxygen, Sedation, Upper gastrointestinal system
Bullet points of the study highlights:
What is already known?
Optimum oxygen supplementation during endoscopic procedures under sedation is a necessity.
What is new in this study?
The high-flow nasal oxygen (HFNO) during upper gastrointestinal endoscopic procedures under sedation is advantageous over conventional low-flow oxygen delivery modalities in terms of decreased incidence of desaturation spells, procedural interruptions and sedation-related adverse events without any procedural delay.
What are the future clinical and research implications of the study findings?
HFNO is a novel modality for reducing hypoxic events along with better compliance for both—the patient and endoscopist.
Introduction
The endoscopy suite has become a routine part of anesthesia care due to the paradigm shift in the management of gastrointestinal (GI) diseases from invasive surgeries to minimally invasive techniques. The most common upper GI endoscopic procedures performed include diagnostic endoscopy, variceal banding, endoscopic retrograde cholangiopancreatography (ERCP) and stenting of the common bile duct. These procedures are unpleasant and painful. Thus, sedation and analgesia have become a part of standard care.
Patients require oxygen supplementation during endoscopic procedures, as they often desaturate due to either the collapse of the airway by the sedation itself or the obstruction caused by the endoscope per se [1]. Various methods of supplementing oxygen, while maintaining spontaneous ventilation in these patients, include the use of a simple face mask designed for endoscopy, use of a nasal cannula, non-invasive ventilation, use of high-flow nasal oxygen (HFNO) or oxygenation through a Mapleson circuit [2].
HFNO is a method of delivering heated humidified oxygen at a flow of over 15 l/min, which is the maximum flow that can be used by any conventional oxygen therapy [3]. Additionally, the oxygen concentration can also be titrated up to 100% from a minimum of 25%, making it an attractive, easy and convenient method of oxygen supplementation. It generates a low amount of positive end-expiratory pressure (PEEP), thereby reducing the work of breathing and washing out dead space in the nasopharynx, prevents atelectasis and reduces resistance [4]. It has paved its way into anesthesia practice being used for preoxygenation, as a rescue device, in place of jet ventilation, airway surgeries and procedural sedation [3].
A recent study comparing the conversion to general anesthesia and desaturation in 238 patients, who underwent endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS) with and without HFNO availability in the endoscopy suite, concluded that the use of HFNO was associated with significantly lower utilization of general anesthesia and higher oxygen saturation [5].
Irrespective of the sedative agent, hypoxia is the commonly encountered unwarranted event with sedation. An unnoticed or prolonged event is fatal. The incidence of sedation-related mortality during the various endoscopic procedures is around eight in 1,00,000 [6].
A retrospective analysis of 73,029 endoscopies reported that 44 patients required intubation and 14 lost their lives [7]. Thus, the importance of any endeavor to reduce hypoxic events under sedation during endoscopic procedures is paramount.
In a prospective feasibility study by Service et al. [8], around 5% of the patients experienced desaturation during outpatient diagnostic bronchoscopy. Several other studies on orthodontic and awake bronchoscopic procedures also found no hypoxia or procedural interruption for securing the airway with the concomitant use of HFNO with sedation [9–13].
Based on the emergent literature and the expected utility of HFNO, we performed this meta-analysis to explore the impact of HFNO during upper GI endoscopic procedures in comparison to the conventional low-flow oxygen delivery modalities, e.g. nasal cannula, facemask, etc. under sedation, in terms of hypoxia, procedural interruption, procedural duration, complications, nadir SpO2 level, overall propofol requirement for sedation, patient and endoscopist satisfaction and according to the “Preferred reporting items for systematic review and meta-analysis (PRISMA) statement” [14].
Methods
Protocol and registration
The protocol of this meta-analysis was registered in the International prospective register of systematic reviews (PROSPERO) database (CRD42021245409) prospectively. The meta-analysis was performed according to PRISMA guidelines and Cochrane recommendations.
Search strategy
All major electronic databases (PubMed, MEDLINE, Embase, and Cochrane Library database), Google Scholar (https://scholar.google.com), preprint platform MedRxiv (https://www.medrxiv.org) and a clinical trial database (https://ClinicalTrials.gov) from January 1, 2000, to July 31, 2022, were independently reviewed by two researchers (SS and DH) with the following terminologies: (“HFNO” OR “high-flow nasal oxygen therapy” OR “high-flow nasal cannula oxygen” OR “Humidified high-flow nasal cannula” OR “HHFNO” OR “Oxygen therapy”) AND (“endoscopy” OR “ERCP’’).
Inclusion and exclusion criteria
We included randomized controlled trials (RCTs), comparative cohort studies, case series, cross-sectional studies and case–control studies with the following Patient Problem, (or Population) Intervention, Comparison or Control, and. Outcome (PICO) criteria:
Patients: Adult patients undergoing GI endoscopic procedures under sedation
Intervention(s), exposure(s): Patients receiving high-flow nasal cannula oxygen therapy primarily during endoscopic procedures under sedation
Comparator/Control: Patients receiving low-flow oxygen delivery modalities, e.g. nasal cannula, facemask, etc., during endoscopic procedures under sedation
Outcome(s): Patients experiencing desaturation (SpO2 < 92%)
For assessing articles published, other than in English, we used Google Translate (https://translate.google.co.in). Articles without the full retrievable text were excluded.
Study selection and data extraction
DH and AR retrieved the full text of available literature according to the eligibility criteria after removing the duplications for assessment. Disagreements were settled with the opinion of SS. A pre-conceived data extraction sheet was used for the extraction of the following data: author, year, centre, number of patients receiving the high-flow nasal cannula (HFNO) oxygen therapy or conventional oxygen therapy, type of the endoscopic procedure, events of hypoxia, conversion into general anesthesia, complications and patient satisfaction.
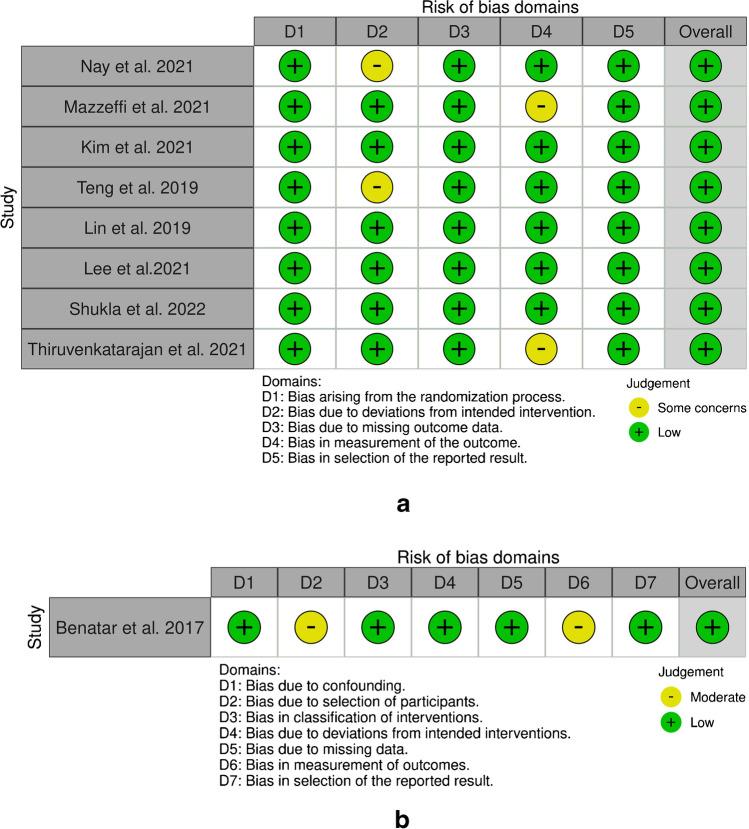
Risk of bias (quality) assessment
SS and AD assessed the risk of bias individually by using the ROBINS-I assessment tool [15] for non-randomized studies and RoB 2.0 tool [16] for RCTs. Any difference of opinion was resolved by consulting with PK.
Quality of the evidence
SS and AD evaluated the quality of evidence using the “Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool” [17–19] separately and PK resolved the difference in opinions.
Data synthesis
SS and AD conducted the statistical analysis with Review manager version 5.4. Odds ratio (OR) with 95% confidence intervals (CIs) was calculated for dichotomous data and mean differences (MDs) with 95% CI were assessed for continuous data, as per the Cochrane Handbook for Systematic Reviews of Interventions [20]. Statistical heterogeneity was evaluated with the I2 statistic, > 50% pointing out substantial heterogeneity. The risk of publication bias was estimated with the funnel plot.
Results
Basic characteristics
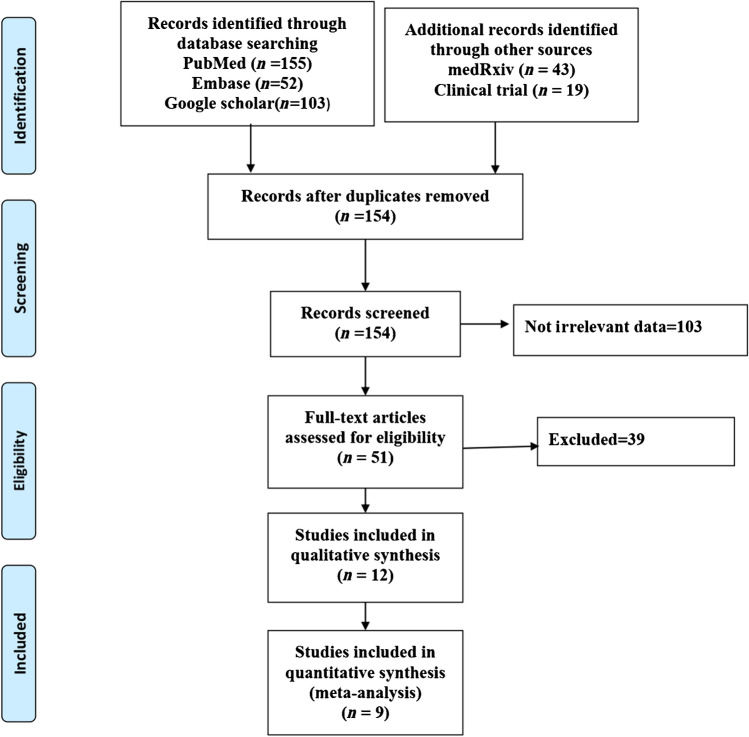
Eight randomized control studies [21–28] and one longitudinal study [29] of 154 publications were included in the final analysis (Fig. 1; Table 1). Among the included studies, none had a severe concern of bias (Fig. 2).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-2009 flow diagram
Table 1.
Characteristics of included studies
| S. no | Author [ref] | Design | Country | Sample size | Intervention | Comparator | Procedures performed | Primary outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Nay et al. [21], 2021 |
RCT, MC |
France | 379 | HFNO at 70 l/min (FiO2 of 0.50) | Nasal cannula or face mask ± nasopharyngeal catheter at an oxygen flow rate ≤ 8 l/min (FiO2 of 0.50) | Esophagogastroduodenoscopy (EGD) comprising biopsy, resection, variceal ligation, ERCP, dilation, etc. | HFNO significantly reduced the incidence of desaturation episodes |
| 2 | Mazzeffi et al. [22], 2021 |
RCT, SC |
USA | 262 | HFNO at 20 l/min | Nasal cannula at 6 l/min | Advanced EGD with an anticipated duration > 15 min primarily either in prone (29%) or lateral (70%) position comprising radiofrequency ablation, endoscopic ultrasound, endoscopic retrograde cholangiopancreatography (ERCP) procedures, etc. | HFNO is associated with lesser desaturation episodes and hypoxia |
| 3 | Kim et al. [23], 2021 |
RCT, SC |
South Korea | 72 | HFNO at 50 l/min (FiO2 of 1.0) | Nasal cannula at 5 l/min | ERCP in the prone position | HFNO provided a better nadir SpO2 level under sedation and lesser procedural interruption |
| 4 | Teng et al. [24], 2019 |
RCT, SC |
Taiwan | 101 | HFNO at 30 l/min (FiO2 of 1.0) | Nasal cannula at 5 l/min | Endoscopic retrograde cholangiopancreatography and endoscopic ultrasound in lateral position | HFNO reduced hypoxemic events during sedative endoscopic procedure |
| 5 | Lin et al. [25], 2019 |
RCT, MC |
China | 1994 | HFNO at 30 l/min (FiO2 of 1.0) | High-flow nasal cannula at 2 l/min | Elective gastroscopy in lateral position | Hypoxia was significantly lower in patients receiving HFNO |
| 6 | Lee et al. [26], 2021 |
RCT, SC |
South Korea | 187 | HFNO at 50 l/min (FiO2 of 0.5) | Nasal cannula at 5 l/min | 33% underwent ERBD, 25% ENBD, 3% EST, 22% stone removal and 14% stent deployment | HFNO provided lesser desaturation and hypoxic events during ERCP under sedation |
| 7 | Shukla et al. [27], 2022 |
RCT, SC |
India | 60 | HFNO at 60 l/min (FiO2 of 0.4) | Nasal cannula at 5 l/min | Endoscopic ultrasound | HFNO was not associated with reduced risk of desaturation and interruption in comparison to nasal cannula |
| 8 | Thiruvenkatarajan et al. [28], 2021 |
RCT, SC |
Australia | 131 | HFNO at 30–60 l/min (FiO2 of 1) | Nasal cannula at 4 l/min | ERCP | HFNO did not significantly decrease hypoxaemia, hypercarbia and the need for airway interventions, in comparison to nasal low-flow oxygen |
| 9 | Benatar et al. [29], 2017 | Prospective, longitudinal study | Mexico | 108 | HFNO at 40 l/min (FiO2 of 0.4) | Nasal cannula at 6 l/min (FiO2 of 0.4) | Gastrointestinal endoscopy | High-flow cannulas not only prevented desaturation episodes, but also provided better patient compliances |
RCT randomized control trial, SC single centre, HFNO high-flow nasal oxygen, ERBD endoscopic retrograde biliary drainage, ENBD endoscopic nasobiliary drainage, EST endoscopic sphincterotomy, ERCP endoscopic retrograde cholangiopancreatography
Fig. 2.
a ROB2 tool assessment for the included RCTs. b ROBINS-I assessment for the included non-randomized cohort studies
Meta-analyses
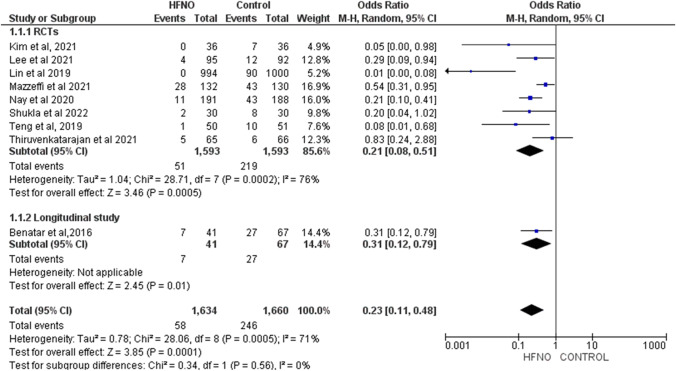
Desaturation episodes during the procedure
Nine studies with 3294 patients were assessed for the risk of desaturation episodes (SPO2 < 92%) during endoscopic procedures. Patients receiving HFNO under sedation had a lesser risk of desaturation in comparison to patients with low-flow oxygen delivery devices. (OR = 0.23; 95% CI 0.11–0.48; I2 = 71%, p < 0.0001) (Fig. 3).
Fig. 3.
The efficacy of high-flow nasal oxygen on prevention of desaturation spells during upper gastrointestinal endoscopic procedures
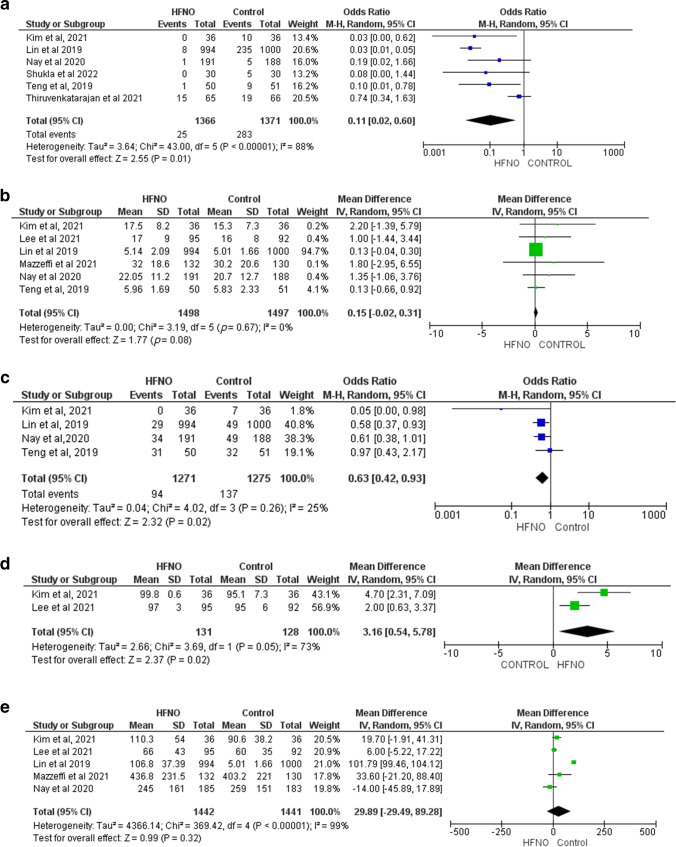
Procedural interruption
Six studies with 2737 patients were evaluated for the incidence of procedural interruption. The application of HFNO with sedation during upper GI endoscopic procedures had a lower risk of interruption in between than low-flow oxygen delivery devices. (OR = 0.11; 95% CI 0.02–0.60; I2 = 88%, p < 0.0001) (Fig. 4a).
Fig. 4.
(a) The utility of HFNO in upper gastrointestinal endoscopic procedures in terms of procedural interruption, (b) Duration of procedure, (c) Overall adverse events related to sedation, (d) Nadir SpO2 level, and (e) Cumulative propofol administration
Procedural duration
No significant alteration in the overall duration of endoscopic procedures was found with the use of either HFNO or low-flow oxygen delivery devices in seven studies with 2995 patients (mean difference [MD] = 0.15, 95% CI − 0.02 to 0.31, I2 = 0%, p = 0.0001) (Fig. 4b).
Adverse events related to sedation
The overall incidence of adverse events due to sedation was assessed in four studies with 2546 patients. The application of HFNO was associated with a reduced risk of adverse events in comparison to patients with low-flow oxygen delivery devices (OR = 0.63; 95% CI 0.42–0.93; I2 = 25%, p < 0.0001) (Fig. 4c).
Nadir SpO2 level
Two studies with 259 patients assessed the nadir SpO2 level during the procedure. The patients with HFNO showed significantly elevated nadir lowest SpO2 than patients with low-flow oxygen delivery devices (MD = 3.16, 95% CI 0. 54–5.78, I2 = 73%, p = 0.02) (Fig. 4d).
Overall propofol requirement
No significant difference in overall propofol consumption during endoscopic procedures was found with the use of HFNO and low-flow oxygen delivery devices in five studies with 2883 patients (mean difference [MD] = 29.89, 95% CI − 29.49 to 89.28, I2 = 99%, p = 0.32) (Fig. 4e).
Except for the studies assessing procedural duration, overall adverse events related to sedation and significant heterogeneity were found among studies assessing other parameters.
Quality of evidence
The quality of evidence on the utility of HFNO for reducing desaturation during upper GI gastrointestinal endoscopic procedures is low quality owing to significant indirectness in terms of difference in population and settings of HFNO (Table 2).
Table 2.
Grading Recommendatioss Assessment, Development, and Evaluation (GRADE) evidence profile
| Outcome | No. of participants | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Quality of evidence (grade) | Relative effect | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Total no | Intervention | Control | ||||||||
| Desaturation episodes | 3294 | 1634 | 1660 | No | No | Yes | No | None | Low ⊕ ⊕ ⊝ ⊝ |
OR = 0.23 (95% CI 0.11 to 0.48) |
| Procedural interruption | 2737 | 1366 | 1371 | No | No | Yes | No | None | Low ⊕ ⊕ ⊝ ⊝ |
OR = 0.11 (95% CI 0.02 to 0.60) |
| Procedural duration | 2995 | 1498 | 1497 | No | No | Yes | Yes | None | Very low ⊕ ⊝ ⊝ ⊝ |
MD = 0.15 (95% CI − 0.02 to 0.31) |
| Adverse events related to sedation | 2546 | 1271 | 1275 | No | No | Yes | No | None | Low ⊕ ⊕ ⊝ ⊝ |
OR = 0.63 (95% CI 0.42 to 0.93) |
| Nadir SpO2 level | 259 | 131 | 128 | No | No | Yes | No | None | Low ⊕ ⊕ ⊝ ⊝ |
MD = 3.16 (95% CI 0.54 to 5.78) |
| Propofol consumption | 2883 | 1442 | 1441 | No | No | Yes | Yes | None | Very low ⊕ ⊝ ⊝ ⊝ |
MD = 29.89 (95% CI − 29.49 to 9.28) |
CI confidence interval, COVID-19 coronavirus disease 19, MD mean difference, OR odds ratio
Publication bias
The funnel plot indicates a publication bias qualitatively is unlikely (supplementary Fig. 1).
Discussion
The current study found low-quality evidence of better oxygenation, lesser incidence of procedural interruption and elevated nadir SpO2 level without any significant difference in procedural duration are associated with the application of HFNO during upper gastrointestinal endoscopic procedures under sedation in comparison to the conventional low-flow oxygen supplementation modalities.
Similarly, another systematic review also reported a lesser incidence of hypoxia (OR 0.02, 95% CI 0.00 to 0.07; heterogeneity I2 = 39%) and airway interventions (OR 0.02, 95% CI 0.01 to 0.04; heterogeneity I2 = 15%) with the use of high-flow nasal cannula in comparison to standard nasal cannula during digestive endoscopic procedures under sedation [30].
A few recent studies also acknowledged the role of HFNO in reducing the risk of hypoxia in moderate to high-risk patients and preventing severe hypoxia [31, 32].
However, none addressed the impact of HFNO on the overall duration, types of different procedures and cumulative dosage of administered propofol for procedural sedation.
A recent randomized cross-over study of healthy volunteers also acknowledged the role of HFNO in attenuating CO2 retention, hypoventilation and associated complications under sedation with propofol [33].
The application of HFNO was found to be beneficial for preventing desaturation in patients undergoing sedative ERCP with midazolam [34].
Conventional oxygen delivery through the nasal cannula is often inadequate under deep sedation, as it can provide oxygen with a FiO2 ≤ 0.4. On the other hand, although the Venturi mask can provide FiO2 ≤ 0.6, it is not feasible for the oral endoscopic approach. Even the endoscopic masks hinder the procedure, particularly during prone positions. The ability of HFNO to deliver hot and humidified 100% oxygen along with dead-space washout effects and PEEP improves patient and endoscopist compliance [23].
However, the use of increased supplementary oxygen may aggravate hypercarbia in chronic obstructive pulmonary disease (COPD) patients by altering the physiological dead space and hypoxemic respiratory drive [35, 36].
Mazzei et al. [22] also reported an increased risk of hypercarbia (HR 5.89; 95% CI 1.33–26.11) with the application of HFNO among patients with chronic lung disease while undergoing ERCP under sedation.
Another study evaluating the respiratory stability of children undergoing upper gastrointestinal tract endoscopy under sedation did not find any significant difference in respiratory adverse incidents or requirement of the airway with the application of HFNO in comparison to low‐flow nasal oxygen cannula. The authors justified that the duration of procedural sedations was short; thereby, the risk of hypoxia may not be evident among children with normal pulmonary function [37].
While a few studies [27, 28] reported similar patient satisfaction scores, one study [28] has found that the endoscopist satisfaction was satisfactory in 100% of patients with HFNO in comparison to 93% of patients with nasal cannula.
A significant variation in flowrate and FiO2 selection during the application of HFNO and positioning of the patients during the procedure is found across the studies. Apart from the sedation-related adverse events, HFNO-related unwarranted incidences such as xeromycteria and rhinalgia were reported infrequently. However, most of the time, they were self-resolved within 30 minutes.
Strengths and limitations
The present study is a robust one including the maximum peer-reviewed published article without any language barrier till date. We found that the application of HFNO had an elevated nadir SpO2 level, no significant impact on procedural duration, cumulative administration of propofol and similar patient and endoscopist satisfaction.
However, except for studies assessing procedural duration, all our study variables had significant heterogeneity, owing to the non-uniformity in patient selection criteria, indications, types of endoscopic procedures, application of HFNO and positioning of the patients. Due to lack of data, specific subgroup analysis also could not be done according to the different settings of HFNO.
To conclude, HFNO can be considered a novel endeavour to reduce or minimize hypoxic events along with better compliance for the patient as well as the endoscopist for upper gastrointestinal endoscopic procedures under sedation.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
None
Author contribution
Puneet Khanna (PK): conceptualization, risk of bias assessment, quality of the evidence assessment and editing. Damarla Haritha (DH): search strategy, study selection, data extraction, risk of bias assessment, quality of the evidence assessment. Aditi Das (AD): data synthesis, risk of bias assessment, quality of the evidence assessment and editing. Soumya Sarkar (SS): conceptualization, search strategy, study selection, data extraction, data synthesis, risk of bias assessment, quality of the evidence assessment, and drafted the manuscript. Avishek Roy (AR): study selection, data extraction.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Conflict of interest
PK, DH, AD, SS, and AR declare no competing interests.
Ethics statement
The study was performed conforming to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way is the Editor-in-Chief, Editorial Board members the Indian Society of Gastroenterology or the printer/publishers responsible for the results/findings and content of this article.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bell GD, Quine A, Antrobus JH, et al. Upper gastrointestinal endoscopy: a prospective randomized study comparing continuous supplemental oxygen via the nasal or oral route. Gastrointest Endosc. 1992;38:319–25. doi: 10.1016/S0016-5107(92)70424-6. [DOI] [PubMed] [Google Scholar]
- 2.Atkins JH. Ventilation strategies in gastrointestinal endoscopy. Tech Gastrointest Endosc. 2009;11:192–6. doi: 10.1016/j.tgie.2009.09.005. [DOI] [Google Scholar]
- 3.Kim HJ, Asai T. High-flow nasal oxygenation for anesthetic management. Korean J Anesthesiol. 2019;72:527–47. doi: 10.4097/kja.19174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renda T, Corrado A, Iskandar G, Pelaia G, Abdalla K, Navalesi P. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br J Anaesth. 2018;120:18–27. doi: 10.1016/j.bja.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Schumann R, Natov NS, Rocuts-Martinez KA, et al. High-flow nasal oxygen availability for sedation decreases the use of general anesthesia during endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol. 2016;22:10398–405. doi: 10.3748/wjg.v22.i47.10398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: a worldwide safety experience.Gastroenterology. 2009;137:1229-37;quiz 1518-9. [DOI] [PubMed]
- 7.Goudra B, Nuzat A, Singh PM, Borle A, Carlin A, Gouda G. Association between type of sedation and the adverse events associated with gastrointestinal endoscopy: an analysis of 5 years’ data from a tertiary center in the USA. Clin Endosc. 2017;50:161–9. doi: 10.5946/ce.2016.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Service JA. Bain JS, Gardner CP, McNarry AF. Prospective experience of high-flow nasal oxygen during bronchoscopy in 182 patients: a feasibility study. J Bronchology Interv Pulmonol. 2019;26:66–70. doi: 10.1097/LBR.0000000000000533. [DOI] [PubMed] [Google Scholar]
- 9.Sago T, Harano N, Chogyoji Y, Nunomaki M, Shiiba S, Watanabe S. A nasal high-flow system prevents hypoxia in dental patients under intravenous sedation. J Oral Maxillofac Surg. 2015;73:1058–64. doi: 10.1016/j.joms.2014.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Badiger S, John M, Fearnley RA, Ahmad I. Optimizing oxygenation and intubation conditions during awake fibre-optic intubation using a high-flow nasal oxygen-delivery system. Br J Anaesth. 2015;115:629–632. doi: 10.1093/bja/aev262. [DOI] [PubMed] [Google Scholar]
- 11.Irfan M, Ahmed M, Breen D. Assessment of high flow nasal cannula oxygenation in endobronchial ultrasound bronchoscopy: a randomized controlled trial. J Bronchology Interv Pulmonol. 2021;28:130–7. doi: 10.1097/LBR.0000000000000719. [DOI] [PubMed] [Google Scholar]
- 12.Longhini F, Pelaia C, Garofalo E, et al. High-flow nasal cannula oxygen therapy for outpatients undergoing flexible bronchoscopy: a randomised controlled trial. Thorax. 2022;77:58–64. doi: 10.1136/thoraxjnl-2021-217116. [DOI] [PubMed] [Google Scholar]
- 13.Lucangelo U, Vassallo FG, Marras E, et al. High-flow nasal interface improves oxygenation in patients undergoing bronchoscopy. Crit Care Res Pract. 2012;2012:506382. [DOI] [PMC free article] [PubMed]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [PMC free article] [PubMed]
- 15.Sterne JAC, Hernán MA, Reeves BC, Savović J, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898 [DOI] [PubMed]
- 17.Norris SL, Meerpohl JJ, Akl EA, et al. The skills and experience of GRADE methodologists can be assessed with a simple tool. J Clin Epidemiol. 2016;79:150–158.e1. doi: 10.1016/j.jclinepi.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 18.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 19.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6. [DOI] [PubMed]
- 20.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [DOI] [PMC free article] [PubMed]
- 21.Nay MA, Fromont L, Eugene A, et al. High-flow nasal oxygenation or standard oxygenation for gastrointestinal endoscopy with sedation in patients at risk of hypoxaemia: a multicentre randomised controlled trial (ODEPHI trial). Br J Anaesth. 2021;127:133–42. [DOI] [PubMed]
- 22.Mazzeffi MA, Petrick KM, Magder L, et al. High-flow nasal cannula oxygen in patients having anesthesia for advanced esophagogastroduodenoscopy: HIFLOW-ENDO, a randomized clinical trial. Anesth Analg. 2021;132:743–51. [DOI] [PubMed]
- 23.Kim SH, Bang S, Lee KY, et al. Comparison of high flow nasal oxygen and conventional nasal cannula during gastrointestinal endoscopic sedation in the prone position: a randomized trial. Can J Anaesth. 2021;68:460–466. doi: 10.1007/s12630-020-01883-2. [DOI] [PubMed] [Google Scholar]
- 24.Teng WN, Ting CK, Wang YT, et al. High-flow nasal cannula and mandibular advancement bite block decrease hypoxic events during sedative esophagogastroduodenoscopy: a randomized clinical trial. Biomed Res Int. 2019;2019:4206795. doi: 10.1155/2019/4206795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin Y, Zhang X, Li L, et al. High-flow nasal cannula oxygen therapy and hypoxia during gastroscopy with propofol sedation: a randomized multicenter clinical trial. Gastrointest Endosc. 2019;90:591–601. doi: 10.1016/j.gie.2019.06.033. [DOI] [PubMed] [Google Scholar]
- 26.Lee MJ, Cha B, Park JS, et al. Impact of high-flow nasal cannula oxygenation on the prevention of hypoxia during endoscopic retrograde cholangiopancreatography in elderly patients: a randomized clinical trial. Dig Dis Sci. 2022;67:4154–60. doi: 10.1007/s10620-021-07272-z. [DOI] [PubMed] [Google Scholar]
- 27.Shukla K, Parikh B, Kumar A, Nakra M. Comparative evaluation of efficacy of oxygenation using high flow nasal cannula vs. conventional nasal cannula during procedural sedation for endoscopic ultrasound: a pilot study. J Anaesthesiol Clin Pharmacol. 2021;37:648–54. [DOI] [PMC free article] [PubMed]
- 28.Thiruvenkatarajan V, Dharmalingam A, Arenas G, et al. Effect of high-flow vs. low-flow nasal plus mouthguard oxygen therapy on hypoxaemia during sedation: a multicentre randomised controlled trial. Anaesthesia. 2022;77:46–53. [DOI] [PubMed]
- 29.Benatar PF, Galaviz ODA, Chávez RMA, et al. High-flow nasal cannula versus conventional oxygen therapy for patients undergoing gastrointestinal endoscopy. An Med Asoc Med Hosp ABC. 2017;62:187–91.
- 30.Zhang YX, He XX, Chen YP, Yang S. The effectiveness of high-flow nasal cannula during sedated digestive endoscopy: a systematic review and meta-analysis. Eur J Med Res. 2022;27(1):30. doi: 10.1186/s40001-022-00661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee CC, Ju TR, Lai PC, Lin HT, Huang YT. Should we use high-flow nasal cannula in patients receiving gastrointestinal endoscopies? Critical appraisals through updated meta-analyses with multiple methodologies and depiction of certainty of evidence. J Clin Med. 2022;11:3860. doi: 10.3390/jcm11133860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doulberis M, Sampsonas F, Papaefthymiou A, et al. High-flow versus conventional nasal cannula oxygen supplementation therapy and risk of hypoxia in gastrointestinal endoscopies: a systematic review and meta-analysis. Expert Rev Respir Med. 2022;16:323–32. doi: 10.1080/17476348.2022.2042256. [DOI] [PubMed] [Google Scholar]
- 33.Mishima G, Sanuki T, Revie J, et al. Nasal high flow improves ventilation during propofol sedation: a randomized cross-over study in healthy volunteers. Respir Physiol Neurobiol. 2020;277:103429. doi: 10.1016/j.resp.2020.103429. [DOI] [PubMed] [Google Scholar]
- 34.Cha B, Lee MJ, Park JS, et al. Clinical efficacy of high-flow nasal oxygen in patients undergoing ERCP under sedation. Sci Rep. 2021;11:350. doi: 10.1038/s41598-020-79798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanson CW, 3rd, Marshall BE, Frasch HF, Marshall C. Causes of hypercarbia with oxygen therapy in patients with chronic obstructive pulmonary disease. Crit Care Med. 1996;24:23–28. doi: 10.1097/00003246-199601000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Abdo WF, Heunks LM. Oxygen-induced hypercapnia in COPD: myths and facts. Crit Care. 2012;16:323. doi: 10.1186/cc11475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klotz D, Seifert V, Baumgartner J, Teufel U, Fuchs H. High-flow nasal cannula vs standard respiratory care in pediatric procedural sedation: a randomized controlled pilot trial. Pediatr Pulmonol. 2020;55:2706–12. doi: 10.1002/ppul.24975. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.