Abstract
Primary care access for Medicaid patients is an ongoing area of concern. Most studies of providers’ participation in Medicaid have focused on factors associated with the Medicaid program, such as reimbursement rates. Few studies have examined characteristics of primary care practices associated with Medicaid participation. We use a nationally representative survey of primary care practices to compare practices with no, low, and high Medicaid revenue. Seventeen percent of practices received no Medicaid revenue; 38% and 45% were categorized in the low and high Medicaid revenue categories, respectively. Practices with no Medicaid revenue were more often small, independent, and located in urban areas with higher household income. These practices also have lower population health capabilities. Our findings suggest that difficulties associated with Medicaid participation (such as billing requirements) may be most acutely experienced by providers with fewer resources and infrastructure, particularly when they have sufficient access to other patient populations.
INTRODUCTION
Access to primary care for Medicaid patients has long been a concern among patients and policymakers.1,2 Previous research has demonstrated that up to one-third of all physicians refuse to accept new Medicaid patients,1 and these percentages have not changed significantly over the past decade.3–5 As additional states continue to adopt Medicaid expansion and Medicaid managed care continues to grow,6,7 there is a renewed interest in access to care for Medicaid patients and participation among primary care providers.8–11 Most studies examining primary care providers’ participation in Medicaid investigate how factors related to the Medicaid program may influence providers’ decision to accept Medicaid patients. For example, studies have examined how Medicaid reimbursement rates and billing requirements affect primary care clinicians’ participation in Medicaid.1,2,4,12–14 Similarly, other studies have examined how Medicaid expansion, which increases the number of Medicaid patients in a state, influences provider participation in the Medicaid program.3,15
In contrast, comparatively little scholarship has examined the provider side. The few studies that examined how provider characteristics are associated with Medicaid participation found that physicians who do not accept Medicaid are more likely to operate in smaller, independently owned practices; care for wealthier patients; and earn a fixed salary.1,2 This research is based on physician-level data, meaning that there is the possibility that other physicians, physician assistants, or nurse practitioners in these same practices do accept Medicaid. Thus, there may be important differences in rates of Medicaid participation among physicians as compared to practices. In addition, group practices (rather than individual providers) are often the locus of decisions and activities that shape Medicaid participation. For example, practices share systems for scheduling, billing, staffing, hiring, and practice management; negotiate contracts and reimbursement with insurers; engage in joint purchasing; and determine provider compensation models.16–19 Thus, the group practice is likely a key actor in determining which clinicians care for patients on Medicaid, but currently little literature speaks to this question.
In addition to the lack of data on practice-level characteristics associated with Medicaid participation, there is also an important gap regarding how practices with varying levels of Medicaid participation differ in quality of care activities. Prior research suggests that physicians believe Medicaid’s low reimbursement rates prevent practices from adequately investing resources to improve quality.20 Yet, we are unaware of studies that have examined how population health capabilities, in particular, differ by primary care practices’ Medicaid participation rates. A richer understanding of variation across primary care practices in Medicaid participation can provide insight into provider-side barriers to increasing Medicaid access and routinely engaging in population health activities.
In this piece, we use new, nationally representative survey data on primary care practices in the United States to examine the proportion of primary care practices with no Medicaid revenue and how those practices compare to practices with Medicaid revenue across key organizational characteristics and population health capabilities.
METHODS
Data and Sample
We used data from the National Survey of Healthcare Organizations and Systems (NSHOS) primary care practice survey fielded 2017–2018 (response rate=47%). The NSHOS covered a range of domains about a practice, including size, ownership, and care delivery initiatives and capabilities. Respondents were most commonly a practice manager or administrator. Methods have also been previously reported upon.21–24
The survey sample was extracted from the IQVIA OneKey database and included all medical practices with three or more physicians in an adult primary care specialty (internal medicine, geriatrics, general practice, family practice). The data are developed using the American Medical Association’s physician Masterfile, publicly available sources, and proprietary data collection strategies. Although OneKey data are primarily used for commercial purposes, they have more recently been used by academic and government researchers,25–29 including as a sample frame for a prior national survey.17,18,30
Practices were defined as a set of clinicians delivering care at a single location in group practice. A stratified cluster sample design was used to sample practices under varied organizational structures, including independent practices and those that are part of multitiered corporate structures. Our final analytic sample included 1,731 practices.
Statistical Analyses
We split practices into three groups: no Medicaid revenue, Medicaid revenue of 10% or less, and Medicaid revenue greater than 10%. We tested several thresholds as part of sensitivity analyses. Results were similar across specifications, so we selected the 10% threshold as it splits practices fairly evenly. We compared unadjusted differences across groups on several practice-level characteristics using chi-square tests for categorical variables, adjusted Wald tests for normally distributed continuous variables, and Mann Whitney U tests for non-normally distributed continuous variables.
Next, we compared unadjusted practice capabilities by Medicaid revenue category. We calculated seven composite measures representing engagement with population health and quality initiatives: extent of care processes for complex patients; participation in payment reform; use of registries across clinical conditions; screening for social factors; patient engagement and activation initiatives; health information exchange capabilities; and health information technology capabilities for patient access. We standardized all composite measures to a 0–1 scale for ease of comparison. We tested for differences in mean composite scores across Medicaid revenue categories using adjusted Wald tests.
Finally, we estimated a generalized ordered logistic regression model predicting practices’ probability of being in the 0%, <=10%, and >10% Medicaid revenue groups. We chose to use a generalized ordered logistic regression model because our ordered logistic regression model failed the proportional odds assumption. We adjusted our model for practice ownership, total number of PCPs, proportion of clinicians who are PCPs, FQHC status, whether the practice resided in a Medicaid expansion state, rural/urban location of the practice, the median income of patients in the practice’s zip code, and whether 20% or more of patients in a practice’s zip code lived under the census poverty level. We calculated predicted probabilities at the mean for each variable.
Survey weights were developed and applied in all analysis to account for sample design and non-response. As shown in Appendix Exhibit A1,31 we compared respondents, non-respondents, and the entire sample frame across several measures; analysis showed no systematic non-response bias.
Limitations
We acknowledge several limitations to our methodology. First, as with any survey, there is the possibility of measurement error due to self-reporting and we recognize that practices’ reported payer mix may differ from their actual payer mix. In general, this type of error in our dependent variable would not bias our regression estimates unless the error was also correlated with our independent variables.32 Second, our survey excluded solo or dual physician practices. Thirty-five percent of family physicians operate in solo or dual practices.33 These practices may represent a distinct group of clinicians and our results may not reflect their experiences. Third, slightly more than half of practices failed to respond to our survey. While internal analyses demonstrated no significant differences between respondents and non-respondents, as shown in Appendix Exhibit A1,31 it is possible that our survey does not fully represent our sample frame.
RESULTS
Practice Characteristics
A total of 288 (17%) practices reported receiving no revenue from Medicaid, 655 (38%) had Medicaid revenue of <=10%, and 788 (46%) had greater than 10% Medicaid revenue (Exhibit 1). In Exhibit 1 we present row proportions for each variable by Medicaid revenue category. As practices moved across Medicaid categories, from no Medicaid revenue to greater than 10% Medicaid revenue, they were generally more likely to be larger practices owned by a health system or hospital, operating in Medicaid expansion states, caring for less affluent patients, and classified as FQHCs. For example, the proportion of practices with no Medicaid revenue was three times larger for independent practices than practices owned by a health system (0.27 vs. 0.09). The proportion of FQHCs with no Medicaid revenue (0.05) was significantly lower than the proportion of FQHCs with greater than 10% Medicaid revenue (0.79). The proportion of practices’ caring for large percentages of patients living in poverty was more than six times higher in practices with greater than 10% Medicaid revenue (0.65) than practices with no Medicaid revenue (0.10).
Exhibit 1:
Unadjusted key characteristics of primary care practices by Medicaid revenue group
|
|
|||
|---|---|---|---|
| No Medicaid (N=288) Mean | Medicaid >0–10% (N=655) Mean | Medicaid >10% (N=788) Mean | |
| Ownership**** | |||
| Health System | 0.09 | 0.36 | 0.54 |
| Hospital | 0.11 | 0.38 | 0.51 |
| Larger Physician Group | 0.23 | 0.43 | 0.34 |
| Independent Physician Practice | 0.27 | 0.39 | 0.33 |
| Total Number of PCPs**** | |||
| 3–10 | 0.20 | 0.37 | 0.42 |
| 11–50 | 0.09 | 0.33 | 0.58 |
| 50+ | 0.11 | 0.36 | 0.53 |
| Proportion clinicians who are PCPs**** | 0.72 | 0.69 | 0.62 |
| FQHC**** | |||
| Yes | 0.05 | 0.16 | 0.79 |
| No | 0.19 | 0.42 | 0.39 |
| Medicaid Expansion State** | |||
| Yes | 0.15 | 0.35 | 0.51 |
| No | 0.21 | 0.39 | 0.40 |
| Proportion of patients in poverty a, **** | 0.10 | 0.25 | 0.65 |
| Rural-urban category**** | |||
| Metropolitan | 0.19 | 0.39 | 0.42 |
| Micropolitan | 0.04 | 0.22 | 0.74 |
| Rural | 0.02 | 0.25 | 0.72 |
Source: Authors’ analysis of the National Survey of Healthcare Organizations and Systems
Defined as 20% or more of individuals in zip code living below census poverty level
Significance indicators are from chi-square tests for categorical variables, adjusted Wald tests for normally distributed continuous variables, and Mann Whitney U tests for non-normally distributed continuous variables. Analysis applies survey sample weights to account for clustered sampling design and non-response.
p < 0.1
p < 0.05
p < 0.01
p < 0.001
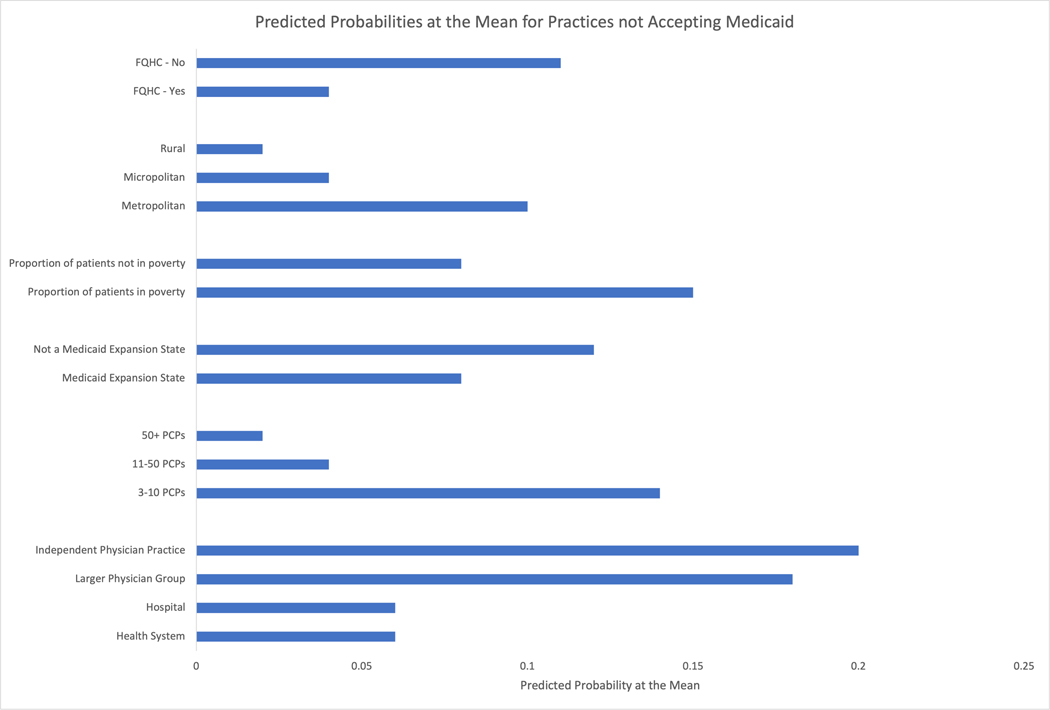
Adjusted Results
The results of our generalized ordered logistic model were similar to unadjusted results. Holding all other variables at their means, we observed similar proportions across most of our study variables. We include the full table of predicted probabilities at the means in Appendix Exhibit A2.31 When looking at predicted probabilities at the means for only those practices not accepting Medicaid, we observed several key patterns (Exhibit 2). Practices with zero Medicaid revenue had significantly higher predicted probabilities of being independently owned than being owned by a hospital or health system. These practices also had significantly higher predicted probabilities of operating in a metropolitan area (vs. rural or micropolitan areas) and employing 3–10 PCPs (vs. 11–50 or 50+). Practices with zero Medicaid revenue had significantly lower predicted probabilities of being located in a Medicaid expansion state, being classified as an FQHC, or caring for patients living in census tracts with lower median household income.
Exhibit 2.
Predicted probabilities of a practice having no Medicaid revenue across key practice characteristics
Source: Authors’ analysis of the National Survey of Healthcare Organizations and Systems
Note: Generalized ordered logistic regression model adjusted for ownership, FQHC status, number of providers, percentage of providers who are PCPs, Medicaid expansion state, median household income of patients in practice’s zip code, urban/rural location, and indicator for practices with 20% or more of individuals living below the census poverty line. Predicted probabilities shown were calculated holding all other variables in the model at their means. Analysis applies survey sample weights to account for clustered sampling design and non-response.
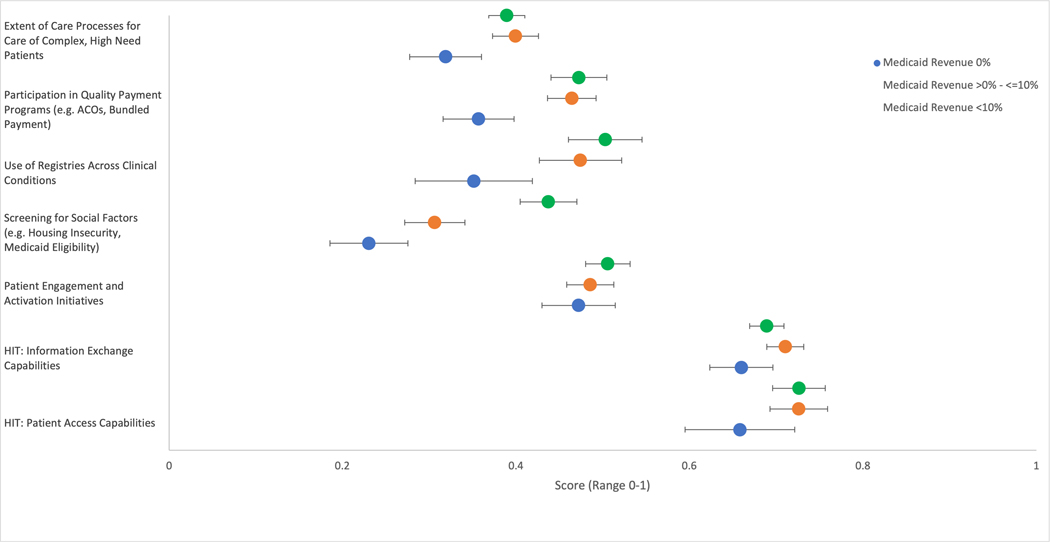
Population health and quality capabilities
When examining unadjusted measures of population health and quality capabilities, we found that practices without Medicaid revenue possessed generally less robust capabilities than those with 0–10% and >10% revenue (Exhibit 3). These differences were significant for care of complex, high need patients (0.32 vs. 0.40 vs. 0.39; p=0.003), use of registries across clinical conditions (0.35 vs. 0.47 vs. 0.50; p<0.001), screening for social factors (0.23 vs. 0.31 vs. 0.44; p<0.001), and participation in quality payment programs (0.36 vs. 0.46 vs. 0.47; p<0.001). There were no significant differences between practices with and without Medicaid revenue on patient engagement and activation activities (0.47 vs. 0.49 vs. 0.51; p=0.334), health information exchange capabilities (0.66 vs. 0.71 vs. 0.69; p=0.051), or health information technology patient access capabilities (0.66 vs. 0.73 vs. 0.73; p=0.136).
Exhibit 3:
Population health and quality capabilities across practices by Medicaid revenue group
Source: Authors’ analysis of the National Survey of Healthcare Organizations and Systems
Notes: Means are represented by the dots, and the bars represent the 95% confidence interval. Composites are standardized such that each composite can take values ranging from 0 to 1. Analysis applies survey sample weights to account for clustered sampling design and non-response. Cronbach’s alpha for each composite is >0.8, except for HIT: Patient Access Capabilities.
DISCUSSION
Our study documents that primary care practices with no Medicaid revenue are different in key ways from practices with low or high Medicaid revenue. Practices with no Medicaid revenue are on average smaller, independent, and have a higher proportion of primary care physicians in the practice, suggesting that organizational capabilities and infrastructure likely play a key role in practices’ decisions to take Medicaid. Second, practices with no Medicaid are more likely to be urban, in low poverty areas, and in states that have not expanded Medicaid; this finding suggests that providers who have access to a large enough patient base outside of Medicaid may be less willing to take Medicaid. Finally, our findings show that practices with no Medicaid revenue are less advanced on several population health capabilities. While we frame this about practices with no Medicaid revenue, many of the same patterns exist when comparing practices with low Medicaid revenue to practices with high Medicaid revenue.
Our findings sit within the larger body of work examining Medicaid participation, particularly factors that induce the choice to accept Medicaid15,34–37 and the effects of this decision. Notably, measuring Medicaid participation is challenging,38,39 and we focus on primary care practices in order to highlight organizational features salient to Medicaid participation. Our finding that 17% of practices have no Medicaid revenue is lower than older studies1,4 but closer to more recent work on this topic.40 This difference may be likely attributable to two key factors. First, our study focuses on primary care practices as opposed to individual physicians as the unit of analysis, changing both the unit as well as including nurse practitioners and physician assistants delivering primary care who were excluded in analysis of physicians. Second, our outcome was current Medicaid revenue as opposed to physician willingness to accept new Medicaid patients, incorporating practices where some physicians retain existing Medicaid patients but no longer take new patients.
While some of our findings mirror those in the literature (such as associations with area income or Medicaid expansion state), our study highlights how organizational features, such as practice size and ownership, play key roles in participation. Moreover, we also examine how practices’ Medicaid revenue is associated with practice capabilities, suggesting that practices with no Medicaid revenue also have fewer capabilities around quality of care and population health than practices with low or high Medicaid revenue. While the evidence on how such capabilities influence patient outcomes is scant, our results suggest that practices opting out of Medicaid are generally less advanced than those that accept Medicaid and may lack key capabilities for caring for patients with complex needs.
Our results have several implications, and policymakers or Medicaid managed care organizations may consider tailoring policy to the state and local context. First, there are likely multiple viable approaches to increasing the share of primary care practices participating in Medicaid that focus on key segments of primary care practices. One approach may be to target small, independent practices. Administrative burden has been cited as a reason physicians are reluctant to accept Medicaid.2 While our data do not directly test the role of administrative burden, our results are suggestive that the burden may be heaviest on small, independent practices due in part to having less infrastructure to handle billing. Efforts to ease the administrative burden for these practices may increase Medicaid acceptance.
In other cases, it may be more productive to focus efforts on key segments of primary care that may be poised to best serve Medicaid patients. For example, focusing on non-participating practices in areas with high concentration of Medicaid patients may be most valuable.
It is likely some combination of strategies may be most effective such as state efforts to reduce the administrative burden of Medicaid coupled with targeted outreach or technical assistance to key segments of a state’s primary care practices. Of course, clinicians also choose where they practice. Some clinicians may choose to practice independently and locate in affluent areas, giving them sufficient revenue to forgo Medicaid participation. Further research is needed to disentangle these choices and their effects on Medicaid participation.
An additional implication of our study is that greater Medicaid acceptance may be an unintended result of increasing consolidation of primary care, particularly as the financial realities of the COVID19 pandemic have increased pressure on practices to consolidate. As practices join larger health care systems, centralized administration and billing handled by the system may result in practices seeing more Medicaid patients. Similarly, in states with a strong Medicaid managed care presence, the negotiating power that providers secure through consolidation may result in higher negotiated reimbursements or payments (such as care management payments) that make Medicaid participation more attractive.
Finally, our results suggest that Medicaid expansion is associated with increased participation in Medicaid but by itself is insufficient to increase participation. Even in expansion states, 15 percent of practices still have no Medicaid revenue, and another 35 percent derive less than a tenth of their revenue from Medicaid. Overall 21 percent of the US population is covered by Medicaid,41 with proportions higher in expansion than non-expansion states, suggesting that the uneven share of Medicaid revenue across practices is likely still a barrier to care for many patients, even in expansion states.
CONCLUSION
In sum, efforts by policymakers and health plans to improve Medicaid access may be most successful if focused on removing barriers faced by independent, small practices in accepting Medicaid. Policies to reduce administrative burden and improve infrastructure for population health may help equip primary care practices to accept Medicaid payment.
Supplementary Material
REFERENCES
- 1.Decker SL. In 2011 Nearly One-Third Of Physicians Said They Would Not Accept New Medicaid Patients, But Rising Fees May Help. Health Aff (Millwood). 2012;31(8):1673–1679. doi: 10.1377/hlthaff.2012.0294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sommers AS, Paradise J, Miller C. Physician willingness and resources to serve more Medicaid patients: perspectives from primary care physicians. Medicare Medicaid Res Rev. 2011;1(2). doi: 10.5600/mmrr.001.02.a01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neprash HT, Zink A, Gray J, Hempstead K. Physicians’ Participation In Medicaid Increased Only Slightly Following Expansion. Health Aff (Millwood). 2018;37(7):1087–1091. doi: 10.1377/hlthaff.2017.1085 [DOI] [PubMed] [Google Scholar]
- 4.Decker SL. Two-Thirds Of Primary Care Physicians Accepted New Medicaid Patients In 2011–12: A Baseline To Measure Future Acceptance Rates. Health Aff (Millwood). 2013;32(7):1183–1187. doi: 10.1377/hlthaff.2013.0361 [DOI] [PubMed] [Google Scholar]
- 5.Holgash K, Heberlein M. Physician Acceptance Of New Medicaid Patients: What Matters And What Doesn’t | Health Affairs. Health Affairs Blog. Published April 10, 2019. Accessed April 30, 2020. 10.1377/hblog20190401.678690/full/ [DOI] [Google Scholar]
- 6.Hinton E, Diaz M, Dec 16 NSP, 2019. 10 Things to Know about Medicaid Managed Care. The Henry J. Kaiser Family Foundation Published December 16, 2019. Accessed January 24, 2020. https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-managed-care/ [Google Scholar]
- 7.Status of State Action on the Medicaid Expansion Decision. The Henry J. Kaiser Family Foundation. Published January 10, 2020. Accessed January 24, 2020. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 8.Candon M, Zuckerman S, Wissoker D, et al. Declining Medicaid Fees and Primary Care Appointment Availability for New Medicaid Patients. JAMA Intern Med. 2018;178(1):145–146. doi: 10.1001/jamainternmed.2017.6302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polsky D, Candon M, Saloner B, et al. Changes in Primary Care Access Between 2012 and 2016 for New Patients With Medicaid and Private Coverage. JAMA Intern Med. 2017;177(4):588–590. doi: 10.1001/jamainternmed.2016.9662 [DOI] [PubMed] [Google Scholar]
- 10.Callison K, Nguyen BT. The Effect of Medicaid Physician Fee Increases on Health Care Access, Utilization, and Expenditures. Health Serv Res. 2018;53(2):690–710. doi: 10.1111/1475-6773.12698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sommers BD, Blendon RJ, Orav EJ. Both The ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults. Health Aff (Millwood). 2016;35(1):96–105. doi: 10.1377/hlthaff.2015.0917 [DOI] [PubMed] [Google Scholar]
- 12.Polsky D, Richards M, Basseyn S, et al. Appointment Availability after Increases in Medicaid Payments for Primary Care. 10.1056/NEJMsa1413299. doi: 10.1056/NEJMsa1413299 [DOI] [PubMed]
- 13.Barnes H, Maier CB, Altares Sarik D, Germack HD, Aiken LH, McHugh MD. Effects of Regulation and Payment Policies on Nurse Practitioners’ Clinical Practices. Med Care Res Rev. 2017;74(4):431–451. doi: 10.1177/1077558716649109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Decker SL. No Association Found Between The Medicaid Primary Care Fee Bump And Physician-Reported Participation In Medicaid. Health Aff (Millwood). 2018;37(7):1092–1098. doi: 10.1377/hlthaff.2018.0078 [DOI] [PubMed] [Google Scholar]
- 15.Tipirneni R, Rhodes KV, Hayward RA, Lichtenstein RL, Reamer EN, Davis MM. Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan. Health Aff (Millwood). 2015;34(8):1399–1406. doi: 10.1377/hlthaff.2014.1425 [DOI] [PubMed] [Google Scholar]
- 16.Shortell SM, Schmittdiel J, Wang MC, et al. An empirical assessment of high-performing medical groups: results from a national study. Med Care Res Rev MCRR. 2005;62(4):407–434. doi: 10.1177/1077558705277389 [DOI] [PubMed] [Google Scholar]
- 17.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small And Medium-Size Physician Practices Use Few Patient-Centered Medical Home Processes. Health Aff (Millwood). 2011;30(8):1575–1584. doi: 10.1377/hlthaff.2010.1210 [DOI] [PubMed] [Google Scholar]
- 18.Rittenhouse DR, Ramsay PP, Casalino LP, McClellan S, Kandel ZK, Shortell SM. Increased Health Information Technology Adoption and Use Among Small Primary Care Physician Practices Over Time: A National Cohort Study. Ann Fam Med. 2017;15(1):56–62. doi: 10.1370/afm.1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez HP, McClellan SR, Bibi S, Casalino LP, Ramsay PP, Shortell SM. Increased Use of Care Management Processes and Expanded Health Information Technology Functions by Practice Ownership and Medicaid Revenue. Med Care Res Rev. 2016;73(3):308–328. doi: 10.1177/1077558715613233 [DOI] [PubMed] [Google Scholar]
- 20.Gordon SH, Gadbois EA, Shield RR, Vivier PM, Ndumele CD, Trivedi AN. Qualitative perspectives of primary care providers who treat Medicaid managed care patients. BMC Health Serv Res. 2018;18(1):728. doi: 10.1186/s12913-018-3516-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenthal M, Shortell S, Shah ND, et al. Physician practices in Accountable Care Organizations are more likely to collect and use physician performance information, yet base only a small proportion of compensation on performance data. Health Serv Res. 2019;54(6):1214–1222. doi: 10.1111/1475-6773.13238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.King AC, Schwartz LM, Woloshin S. A National Survey of the Frequency of Drug Company Detailing Visits and Free Sample Closets in Practices Delivering Primary Care. JAMA Intern Med. 2020;180(4):592–595. doi: 10.1001/jamainternmed.2019.6770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals. JAMA Netw Open. 2019;2(9):e1911514-e1911514. doi: 10.1001/jamanetworkopen.2019.11514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ouayogodé MH, Fraze T, Rich EC, Colla CH. Association of Organizational Factors and Physician Practices’ Participation in Alternative Payment Models. JAMA Netw Open. 2020;3(4):e202019-e202019. doi: 10.1001/jamanetworkopen.2020.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Furukawa MF, Machta RM, Barrett KA, et al. Landscape of Health Systems in the United States. Med Care Res Rev. Published online 2019:1077558718823130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen GR, Jones DJ, Heeringa J, et al. Leveraging Diverse Data Sources to Identify and Describe U.S. Health Care Delivery Systems. EGEMs Gener Evid Methods Improve Patient Outcomes. 2017;5(3):9. doi: 10.5334/egems.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang Y, Chang C-CH, Lave JR, Gellad WF, Huskamp HA, Donohue JM. Patient, Physician and Organizational Influences on Variation in Antipsychotic Prescribing Behavior. J Ment Health Policy Econ. 2016;19(1):45–59. [PMC free article] [PubMed] [Google Scholar]
- 28.Marcum ZA, Bellon JE, Li J, Gellad WF, Donohue JM. New chronic disease medication prescribing by nurse practitioners, physician assistants, and primary care physicians: a cohort study. BMC Health Serv Res. 2016;16(1):312. doi: 10.1186/s12913-016-1569-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agency for Healthcare Research and Quality. Compendium of U.S. Health Systems, 2018.; 2019. https://www.ahrq.gov/chsp/data-resources/compendium-2018.html
- 30.Shortell SM, McClellan SR, Ramsay PP, Casalino LP, Ryan AM, Copeland KR. Physician practice participation in accountable care organizations: the emergence of the unicorn. Health Serv Res. 2014;49(5):1519–1536. doi: 10.1111/1475-6773.12167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.To Access the Appendix, Click on the Appendix Link in the Box to the Right of the Article Box Online.
- 32.Wooldridge JM. Introductory Econometrics: A Modern Approach. 5 edition. Cengage Learning; 2012. [Google Scholar]
- 33.Lee D, Fiack KJ, Knapp KM, Peterson LE, Bazemore AW. A Profile of Solo/Two-Physician Practices. J Health Hum Serv Adm. 2013;36(3):297–322. [PubMed] [Google Scholar]
- 34.Adams EK, Herring B. Medicaid HMO Penetration and Its Mix: Did Increased Penetration Affect Physician Participation in Urban Markets? Health Serv Res. 2008;43(1p2):363–383. doi: 10.1111/j.1475-6773.2007.00763.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mulcahy AW, Gracner T, Finegold K. Associations Between the Patient Protection and Affordable Care Act Medicaid Primary Care Payment Increase and Physician Participation in Medicaid. JAMA Intern Med. 2018;178(8):1042–1048. doi: 10.1001/jamainternmed.2018.2610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saulsberry L, Seo V, Fung V. The Impact of Changes in Medicaid Provider Fees on Provider Participation and Enrollees’ Care: a Systematic Literature Review. J Gen Intern Med. 2019;34(10):2200–2209. doi: 10.1007/s11606-019-05160-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilk AS. Differential Responses among Primary Care Physicians to Varying Medicaid Fees. Inq J Health Care Organ Provis Financ. 2013;50(4):296–311. doi: 10.1177/0046958014522914 [DOI] [PubMed] [Google Scholar]
- 38.Sommers BD, Kronick R. Measuring Medicaid Physician Participation Rates and Implications for Policy. J Health Polit Policy Law. 2016;41(2):211–224. doi: 10.1215/03616878-3476117 [DOI] [PubMed] [Google Scholar]
- 39.Coffman JM, Rhodes KV, Fix M, Bindman AB. Testing the Validity of Primary Care Physicians’ Self-Reported Acceptance of New Patients by Insurance Status. Health Serv Res. 2016;51(4):1515–1532. doi: 10.1111/1475-6773.12435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.R T, Ec K, Jz A, et al. Factors influencing primary care providers’ decisions to accept new Medicaid patients under Michigan’s Medicaid expansion. Am J Manag Care. 2019;25(3):120–127. [PMC free article] [PubMed] [Google Scholar]
- 41.May 27 P, 2020. Medicaid State Fact Sheets. KFF. Published May 27, 2020. Accessed June 23, 2020. https://www.kff.org/interactive/medicaid-state-fact-sheets/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.