Abstract
OBJECTIVE
To evidently assess the applicability of regulate menstrual cycle (MC) characteristics in Traditional Chinese Medicine (TCM) as an indicator for fertility.
METHODS
A community-based prospective cohort study was conducted in China. Between January 2010 and December 2012, women who were willing to conceive within 2 years were enrolled in the study. Other than the MC length pattern, a well-adopted MC characteristic, menstrual blood color and clots were specifically concerned for women enrolled. All participants were followed up in 2 years by trained nurses. Pregnancy rate, fecundability odds ratio (FOR) and risk of miscarriage were assessed as fertility outcomes.
RESULTS
A total of 2109 women were effectively included in this cohort for analysis. Results show that women with irregular MC length were less likely to achieve conception (FORirregular = 0.59; 95% CI = 0.45-0.77, P < 0.001). Menstrual blood in bright red color was also associated with decline in likelihood of conception (FOR = 0.79; 95% CI = 0.63-0.98, P = 0.04). Women with menstrual blood in light red were at higher risk of miscarriage (OR = 2.39; 95% CI = 0.91-6.28, P = 0.08). No significant impact was found between menstrual blood clots and fertility outcomes (FOR = 1.02, 95% CI = 0.83-1.25, P = 0.88; OR = 1.26 95% CI = 0.77-2.07, P = 0.35).
CONCLUSIONS
MC characteristics can be an effective and simple indicator for women’s fertility. Increasing the knowledge of MC characteristics for women in reproductive ages would bring great benefits to their preconception health conditions.
Keywords: menstrual cycle; fertility; odds ratio; abortion, spontaneous; medicine, Chinese traditional; preconception care
1. INTRODUCTION
Menstrual cycles (MC) of women, the consequences of physiological and hormonal changes in women's body, perform in complex but coordinated patterns. A healthy menstrual cycle is generally defined as approximately 28-day per cycle, within 3-5 d menstrual bleeding, bright or dark red color of blood.1,2 If any imbalance in body occurs, disorders in MC characteristics may happen as a consequence. For instance, advanced ovarian aging can shorten the length of luteal phase, leading to MC lengths shorter than 28 d.3 Later rise in Follicle-stimulating hormone and Luteinizing hormone peaks in follicular phase can cause MC length longer than 31 d.2 Disorder of hypothalamic-pituitary-ovarian axis, or extreme low- or over- body weights can increase the risk of anovulation, resulting in irregularities in MC length.4,5 Low estrogen levels in the body may cause the unstable of endometrium, which leads to spotting of blood in light red color.6 Fibroids in uterine or other tumor microenvironment can result in dark menstrual blood color, also visible blood clots.7
Studies showed that MC length can be a marker of women's potential to conceive and fertility outcome. Irregularities in MC length may decrease the odds of conceiving in that cycle,8 leading to infertility,4 or low birth weight.5 Both longer and shorter cycles were more likely to be spontaneously aborted after conception, comparing with 30- to 31-day cycles.9 However, evidence assessing the association between MC length and fecundability is inconsistent. In one study, women with a MC length of < 26 d only have half chance of giving birth, comparing with women with MC length of > 34 d.3 In another study, longer cycles (> 31 d) were associate with decreased fecundability.10 Those findings meant that MC length may be not proper as a sole indicator to women's fertility.
Other than MC length, menstrual blood color and texture may also act as indicators of women's health. Physiologically, menstrual blood is a blood mixed with secretions from the vagina and uterus, old cellular tissue, red blood cells and mesenchymal stem cells.11 The pathologic changes of vagina, uterus or whole body will have effects on the physical status of menstrual blood, which can be visually reflected by color.12 The cessation of bleeding relies on an intact endometrial coagulation system to achieve hemostasis.7 An overactive fibrinolytic system can interfere with hemostasis and contribute to visible blood clots. However, few studies take menstrual blood color or texture into account as markers of women's health or fertility.
Differed from Western Medicine, Traditional Chinese Medicine (TCM) practitioners concern more and broader on menstrual cycles in a holistic and integrative manner. As a matter of fact, menstrual blood color, texture, length and frequency are all involved in TCM diagnosis, to assess women's reproductive status.13 Also, improving menstrual cycles is one of the most important core principles in TCM infertility treatment.14 A research launched in Australia showed that,15 all women with infertility reported menstrual changes after 1-3 months of TCM therapy, including regulations of MC length and changes to blood color and texture. Almost half of them conceived after TCM therapy. As the number of women using TCM for fertility enhancement has increasingly risen,16,17 it is urgently needed to deepen the understandings in MC characteristics and fertility of women before TCM diagnosis and treatment.18
By exploring the association between these three MC characteristics and fertility outcomes, the aim of this study was to unravel the potential impacts of menstrual color and clots on women's fertility outcomes.
2. MATERIAL AND METHODS
2.1. Study design and population
The prospective cohort study was conducted in Fengtai District of Beijing, China. The cohort was a subset of the population who accepted National Free Pre-pregnancy Checkups20 (NFPC) and the routine preconception care service provided by Fengtai family plan committee. Fengtai district is mainly composed by counties and urban-rural fringes, with a predominantly migrant population from different areas of China. Between January 2010 and December 2012, a total of 2265 women who were new married, and held the willing to conceive in 2 years, registered in our database were included in the study. According to the diagnosis standard of NFPC, participants who were diagnosed as: polycystic ovarian disease, pelvic inflammatory disease, endometriosis, pelvic radiation, vaginal inflammation, anemia, viral infections (TORCH, rubella, cyto-megalovirus and Herpes), liver, kidney or thyroid dysfunction, were excluded in this study. Participant with self or partner history of infertility were also excluded.
Face to face interviews were conducted by trained nurses, all information was collected in the database at the same time. Baseline information includes demographic characteristic (date of birth, date of marriage, educational attainment and current occupation), behavior characteristics (smoking, alcohol drinking, noise, poison materials, radiation, or pet exposure), family history (diabetes, congenital heart disease), personal medical history, age at menarche, abortion history and assessment of menstrual cycle characteristics.
2.2. Assessment of menstrual cycle characteristics
MC characteristics include three aspects: length pattern, menstrual blood color, and blood clots. The MC characteristics of subjects were evaluated by self-report questionnaire involving participants' symptom happened during the past 3 months, with good reliability (coefficient of stability = 0.81) (Table 1).
Table 1.
Questionnaire for menstrual cycle characteristics
| Question | Option | Category |
|---|---|---|
| Length pattern: How long menstrual cycle on an average have you had during the past 3 months? |
Usually 27 to 32 d | Normal |
| Usually 26 d or less | Short | |
| Usually longer than 32 d | Long | |
| Irregular length | Irregular | |
| Menstrual Blood color: What is the color of your menstrual bleeding during past 3 months? |
Usually dark red | Dark red |
| Usually bright red | Bright red | |
| Usually light red | Light red | |
| Unknown | Unknown | |
| Blood clots: Do you have blood clots during your menstrual flow during the past 3 months? |
Sometimes, or usually | Yes (1) |
| Never or occasionally | No (0) |
MC length measures the duration of a menstrual cycle from the first day of menstrual bleeding to the last day before the next bleeding. A normal MC length pattern is between 27 and 32 d, with no more than 3 days' variations among months.21 Abnormal length patterns can be classified into three types below: short, long, and irregular length patterns. The short length pattern was defined as a menstrual cycle shorter than 27 d in last three months, while the long length pattern was longer than 32 d.22 The irregular length pattern was defined as high variance in MC length over 5 d among different months. If the cycle length varies more than 3 d from month to month continually, it will be considered as irregular pattern, even if some MC length data fell within the 27 to 32 d range.
Blood color was self-judged by participants based on blood color scale. As an example, Figure 1 demonstrates the reference MC color card with three shades of red, from light to dark (i.e., Light Red, Bright Red, Dark Red).
Figure 1. Menstrual blood color scale.
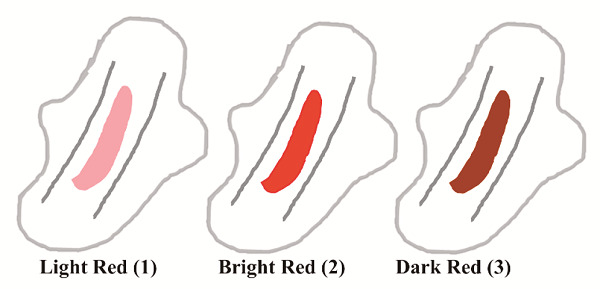
(1) Light Red, RGB: (255, 153, 153), (2) Bright Red, RGB: (255, 0, 0), (3) Dark Red, RGB: (102, 0, 0).
2.3. Follow-up
Trained nurses made follow-up telephone interviews. The first follow up was conducted within 12 months after baseline examination. Information about clinical pregnancy was obtained, including the last menstrual period (date), live birth, ongoing birth, or self-report miscarriage. In this study, we defined miscarriage as a pregnancy loss before 20 weeks of gestation.23 If the participant was not pregnant at this interview, repeated a 12-month inquiry was made.
2.4. Ethical approval and trial register
The institutional review board at Institute of Basic Research in Clinical Medicine, China academy of Chinese Medical Science, Beijing, approved the protocol and all participants provided informed consent (No. 2009NO7). Additionally, the protocol was registered in Chinese Clinical Trial Registry (No. ChiCTR-RCH-13003082).
2.5. Statistical analysis
Statistical tests were conducted through Univariate analysis, χ2 tests or Fisher's exact test to evaluate the means and standard deviation, or distribution of demographic data and covariates across categories of study participation and by fertility outcomes. Pregnancy rate (PR) was calculated by the number of women achieved clinical pregnancy during the study divided by the number of women included in final analyses. Fecundability odds ratio (FOR) was also calculated to evaluate probability of conception in last three years (fecundability).
Both fit linear model and multivariable regression model were created to determine the impact of MC characteristics on fecundability. The fit linear model was primarily used to assess the association between MC characteristics and PR. Subsequently, the multivariable regression model was applied to calculate FORs and 95% confidence intervals (95% CI) for each measure relative to its reference category. FOR of less than 1.0 suggests reduced fecundability (likelihood of conception) and P-values < 0.05 indicate statistical significance. Moreover, a logistic regression model was employed to determine the relationship between MC characteristics and pregnancy outcome (“live birth”, “miscarriage”). To adjust for potential confounders, covariates were added to all models above, including age, education level, age at menarche, and abortion history.
All data were analyzed using R software (version 3.4.2 and version 3.6.1). Using the mean imputation method, the missing data of age and age at menarche were replaced by average value.
3. RESULTS
A total of 2265 women were initially enrolled in this cohort, with 29 women changed to conception control, 127 women lost to follow-up. Finally, 2109 women were effectively included in this study. Around two-thirds of participants (1394, 66.10%) achieved conception during the study, of which 1119 gave live birth, 187 were ongoing pregnancy, and 88 ended with miscarriage at the time of follow-up. Study flow diagram of this study was shown in Figure 2.
Figure 2. Study flow of women enrollment, follow up and pregnancy diagnosis.
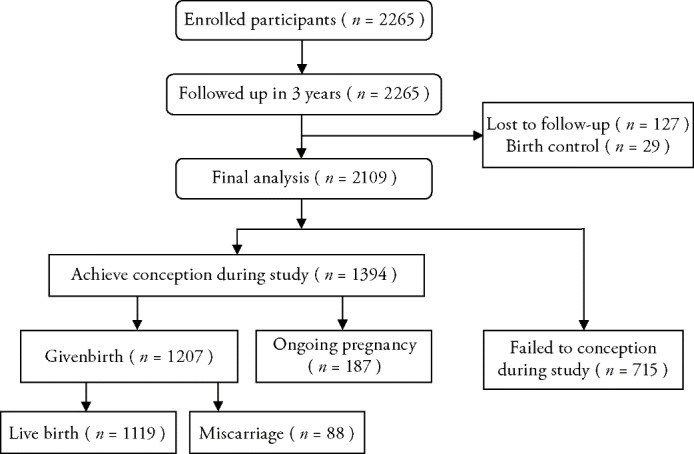
Table 2 shows the demographic as well as MC characteristics of the study population from the initial interview. The participants were aged 20-44 years with a mean age of (27.85 ± 2.88) years. Most of women were in a high-education level (84.97% with bachelor's degree or above). Very few women (less than 0.6%) were smokers or drank alcohol, or were exposed to radiation, noise or poison environments. The mean age at menarche was (13.22 ± 1.36) years. Around three-quarter (73.02%) women reported no abortion history, while 457 (21.67%) and 19 (0.90%) women suffered pregnancy loss 1-2 times and more than 3 times, respectively. Approximately 1 in 4 women (24.47%) reported in normal MC length pattern, but the number of women with light menstrual blood color was much higher (54.24%). More than half women (53.83%) reported sometimes or usually having blood clots during menstrual flow. No statistical significance of distributions of MC characteristics were found among different abortion groups.
Table 2.
Characteristics of Study participants with different age group [n (%)]
| Item | Total (n = 2109) | Age (years) | P value | |||
|---|---|---|---|---|---|---|
| ≤ 25 (n = 409) |
25-30 (n = 1379) |
30-35 (n = 289) |
35-45 (n = b32) |
|||
| Education | < 0.001 | |||||
| High school or less | 300 (14.22) | 129 (31.54) | 132 (9.57) | 31 (10.73) | 8 (25.00) | |
| Bachelor | 1514 (71.79) | 257 (62.84) | 1027 (74.47) | 210 (72.66) | 20 (62.50) | |
| Master/doctor | 278 (13.18) | 15 (3.67) | 213 (15.45) | 46 (15.92) | 4 (12.50) | |
| Missing | 17 (0.81) | 8 (1.96) | 7 (0.51) | 2 (0.69) | 0 (0.00) | |
| Age at menarche | 13.22 (1.36) | 13.3 (1.47) | 13.21 (1.33) | 13.14 (1.32) | 13.48 (1.7) | 0.326 |
| Abortion history | < 0.001 | |||||
| 0 | 1540 (73.02) | 304 (74.33) | 1041 (75.49) | 176 (60.90) | 19 (59.38) | |
| 1-2 | 457 (21.67) | 87 (21.27) | 270 (19.58) | 90 (31.14) | 10 (31.25) | |
| ≥3 | 19 (0.90) | 0 (0.00) | 11 (0.80) | 8 (2.77) | 0 (0.00) | |
| Missing | 93 (4.41) | 18 (4.40) | 57 (4.13) | 15 (5.19) | 3 (9.38) | |
| Menstrual Cycle Length | 0.47 | |||||
| Regular | 516 (24.47) | 97 (23.72) | 342 (24.80) | 69 (23.88) | 8 (25.00) | |
| Short | 318 (15.08) | 65 (15.89) | 206 (14.94) | 44 (15.22) | 3 (0.38) | |
| Long | 700 (33.19) | 142 (34.72) | 459 (33.28) | 93 (32.18) | 6 (18.75) | |
| Irregular | 575 (27.26) | 105 (25.67) | 372 (26.98) | 83 (28.72) | 15 (46.88) | |
| Menstrual Blood Color | 0.35 | |||||
| Dark Red | 735 (34.85) | 134 (32.76) | 491 (35.61) | 99 (34.26) | 11 (34.38) | |
| Bright Red | 1144 (54.24) | 224 (54.77) | 738 (53.52) | 167 (57.79) | 15 (46.88) | |
| Light Red | 75 (3.56) | 19 (4.65) | 44 (3.19) | 9 (3.11) | 3 (9.38) | |
| Unknown | 155 (7.35) | 32 (7.82) | 106 (7.69) | 14 (4.84) | 3 (9.38) | |
| Blood Clots | 0.86 | |||||
| Yes | 1135 (53.82) | 227 (55.50) | 738 (53.52) | 154 (53.29) | 16 (50.00) | |
| No | 974 (46.18) | 182 (44.50) | 641 (46.48) | 135 (46.71) | 16 (50.00) | |
| Fertility outcome | 0.01 | |||||
| Fail to conception | 715 (33.90) | 116 (28.36) | 494 (35.82) | 90 (31.14) | 15 (46.88) | |
| Achieve conception | 1394 (66.10) | 293 (71.64) | 885(64.18) | 199(68.86) | 17 (53.13) | |
| include: | ||||||
| Ongoing Pregnancy | 187 (13.41) | 17 (5.80) | 125 (14.12) | 38 (19.10) | 7 (41.18) | |
| Given birth | 1207 (86.59) | 276 (94.20) | 760 (85.88) | 161 (80.90) | 10 (58.82) | |
| Pregnancy outcome | 0.05 | |||||
| Live Birth | 1119 (92.71) | 265 (96.01) | 699 (91.97) | 147 (91.30) | 8 (80.00) | |
| Miscarriage | 88 (7.29) | 11 (3.99) | 61 (8.03) | 14 (8.70) | 2 (20.00) | |
We also summarized the baseline characteristics according to age in Table 3. As expected, women with elder age were less likely to achieve pregnancy (P = 0.01), and more likely to end in miscarriage (P = 0.05). However, no statistical significance of distributions of MC length pattern, blood color or clots was found among different age groups.The FOR data among different MC characteristics can be found in Table 3. Women with irregular MC length pattern reported the lowest pregnancy rate (59.13%), followed by those with short cycle (66.67%), long cycle (69.00%) and normal cycle (69.57%). The results from multivariable regression model, using normal pattern as reference level, indicated that the irregular MC women were less likely to become pregnant (crude FORirregular = 0.63; 95% CI = 0.49-0.82). After adjusting for the main confounders, the effect remained similar [adjusted (adj.) FORirregular = 0.59; 95% CI = 0.45-0.77]. Short or long cycles were also assoCIated with a potential decline in likelihood of conception, albeit in slight extents, with an adj. FORshort of 0.82 (95% CI = 0.6-1.12) and FORlong of 0.92 (95% CI = 0.72-1.2), respectively, in the adjust model (Table 3).
Table 3.
Pregnancy outcome (live birth, miscarriage) by MC characteristics (n = 1394)
| crude OR | adj. ORa |
P value (wald's test) |
P value (LR-test) |
||
|---|---|---|---|---|---|
| Menstrual Cycle Length | 0.33 | ||||
| Regular | 1 | 1 | |||
| Short | 1.74 (0.88, 3.44) | 1.71 (0.85, 3.42) | 0.13 | ||
| Long | 0.99 (0.53, 1.85) | 0.97 (0.51, 1.84) | 0.92 | ||
| Irregular | 1.31 (0.69, 2.48) | 1.23 (0.64, 2.38) | 0.53 | ||
| Menstrual Blood Color | 0.41 | ||||
| Dark Red | 1 | 1 | |||
| Bright Red | 0.92 (0.57, 1.49) | 1.01 (0.6, 1.71) | 0.97 | ||
| Light Red | 2.28 (0.89, 5.85) | 2.39 (0.91, 6.28) | 0.08 | ||
| Unknown | 1.03 (0.41, 2.55) | 1.01 (0.40, 2.53) | 0.99 | ||
| Blood Clots, Y | 1.34 (0.85, 2.11) | 1.26 (0.77, 2.07) | 0.35 | 0.35 |
Notes: aAdjusted for age (≤ 25, 25-30, 30-35, 35-45), education level (high school or less, bachelor, master/doctor), age at menarche (continuous variable), and abortion history (0, 1-2, ≥ 3 times). Adj: adjusted; MC: menstrual cycle; OR: odds ratio; LR-test: likelihood ratio test.
Both linear and logistic models suggested that menstrual blood color indeed impact fertility outcome. Women who self-judged menstrual blood in bright red color reported the lowest pregnancy rate (64.25%), and were less likely to become pregnant (adj. FOR = 0.79; 95% CI = 0.63-0.98). Women having menstrual blood in light red color were at higher risk of miscarriage, though not significantly, with an adjusted OR of 2.39 (95% CI = 0.91, 6.28, P = 0.08). The menstrual blood clots showed no obvious impacts on the fertility outcomes (Table 4).
Table 4.
Fertility outcome by MC characteristics (n = 2109)
| Item | Achieve conception [n (%)] |
Crude FOR (95% CI) |
adj. FOR (95% CI) a |
P value (wald's test) |
P value (LR-test) |
|
|---|---|---|---|---|---|---|
| Menstrual Cycle Length | < 0.001 | |||||
| Regular | 359 (69.57) | 1 | 1 | |||
| Short | 212 (66.67) | 0.85 (0.62, 1.15) | 0.81 (0.6, 1.11) | 0.2 | ||
| Long | 483 (69.00) | 0.97 (0.75, 1.25) | 0.92 (0.71, 1.2) | 0.56 | ||
| Irregular | 340 (59.13) | 0.63 (0.49, 0.82) | 0.59 (0.45, 0.77) | < 0.001 | ||
| Menstrual Blood Color | 0.11 | |||||
| Dark Red | 503 (68.44) | 1 | 1 | |||
| Bright Red | 735 (64.25) | 0.82 (0.67, 1) | 0.79 (0.63, 0.98) | 0.04 | ||
| Light Red | 49 (65.33) | 0.86 (0.52, 1.44) | 0.87 (0.52, 1.47) | 0.61 | ||
| Unknown | 107 (69.03) | 1.05 (0.71, 1.56) | 1.13 (0.76, 1.68) | 0.55 | ||
| Blood Clots, Y | 759 (35.99) | 1.08 (0.89, 1.3) | 1.02 (0.83, 1.25) | 0.88 | 0.88 |
Notes: aAdjusted for age (≤ 25, 25-30, 30-35, 35-45), education level (high school or less, bachelor, master/doctor), age at menarche (continuous variable), and abortion history (0, 1-2, ≥ 3 times). Adj: adjusted; MC: menstrual cycle; FOR: fecundability odds ratio; LR-test: likelihood ratio test.
4. DISCUSSION
The present study indicated that MC length pattern and menstrual blood color are assoCIated with fertility outcomes among Chinese rural women with statistical significance. Women with irregular MC length pattern or bright red color of menstrual blood had lower PRs and FORs. Short or long cycles were also assoCIated with a slight decline in the possibility of conception. Women with light red blood color had higher risk of miscarriage. Menstrual blood clots have no apparent relationship with fertility outcomes.
Our results of MC length and fertility are consistent with previous studies. Wesselink et al 24 indicated that menstrual irregularity was associated with a slight reduction of fecundability (FOR = 0.93; 95% CI = 0.81-1.06). Kolstad et al 25 found that of women with a cycle length that differed by >10 d from the usual cycle length, fecundity was only approximately 25% of women who had no variation (odds ratio = 0.25, 95% CI = 0.09-0.68). Women with irregular cycles may have longer time to pregnancy due to higher risk of anovulation,26 and/or an underlying disorder of the hypothalamic-pituitary-ovarian axis or the uterus.27 As to longer or shorter MC length, the negative impacts on FOR were also reported in previous studies. Jensen et al. found lower fecundability after cycles of > 35 d (FOR = 0.74; 95% CI = 0.70-0.87).28 Short menstrual cycles may reflect ovarian aging29 or a narrow fertile window and are associated with higher risk of anovulation28 and lower fecundability compared with normal length cycles.9
While western physiology describes the menstrual cycle in terms of hormones which influence the ovaries and the uterus, TCM captures it in the aspects of Qi and Blood, Yin and Yang on the Uterus. If some basic elements (Qi, Blood, Yin, Yang) were in pathology status, reproductive dysfunction may be affected. One may take Qi, a vital form of energy which circulates in meridians (or channels) to nourish the body, as an example. Women with Qi deficiency may have scanty menstruation, or oligomenorrhea. The transport of Qi along the meridians, in some cases, represents the energy movement in body. In a menstrual cycle, the movement of Qi can facilitate the journey of an egg from ovary through fallopian tube to uterus at ovulation time. If Qi stagnates, the ovulation process might fail, the menstrual cycle can be in an irregular pattern, which may reduce the ability of conception.
Our results also indicated that the lighter menstrual blood color, the higher risk of low fertility rate and miscarriages. Menstrual blood color is rarely considered by western doctors, but as always, is inquired by TCM doctors. Physiologically, blood color is mainly determined by hemoglobin concentration.30 According to this hypothesis, the lighter menstrual blood color, the lower level of hemoglobin. From the TCM perspective, the lighter menstrual blood color may be a typical symptom belongs to the pattern of Qi deficiency, Blood deficiency or Yang deficiency, all of which are risk patterns of low fecundability and miscarriage.14 Menstrual blood color may also be impacted by estrogen level, and light color may indicate low estrogen. Analogue to the Haemoglobin Color Scale that was developed by WHO to screen for anemia,31 it's reasonably considerable to develop a menstrual blood color scale, as a simple and inexpensive tool to assess reproductive health.
Although no significant association between menstrual blood clots and fertility was found in this study, we believe that more attention should be paid to the menstrual blood clots. In TCM view, blood clots are caused by Blood Stasis in body, which is a common risk pattern of miscarriage.32 Pathologically, visible or frequent clots can be a signal of many medical issues, such as uterine polyps or fibroids, endometriosis, adenomyosis, hormonal imbalances.33 Therefore, more rigorous investigations on menstrual blood clots and their correlations with healthy status and fertility outcomes are needed in future studies.
While we have unraveled the important impact of MC characteristics on fertility of women, this study remained needed to be advanced in future work. First, the menstrual blood color and clots are highly time-dependent. For example, fresh menstrual blood can change its color and clotting status with prolonging time, and it is almost not possible to obtain the data of the very fresh menstrual blood in the daily life of the recruited women. This may explain why we did not observe obvious correlation between menstrual blood clots and FOR. Second, the volume of menstrual blood loss and menstrual bleed length are lacked in this study, which will be took into consideration in our next step. Last but not least, though the whole study, we only collected the MC characteristic data in a relatively short period (three months), which may increase the data variance, and therefore longer observation is required in future study.
In conclusion, the present community-based study revealed that irregular, short or long MC length pattern, and bright menstrual blood color were intimately or potentially associated with low FOR, and light red color might be a risk factor for miscarriage in the study population. Menstrual blood clots, however, had no significant correlation with fertility outcomes. Since the self-reported MC characteristics can be easily collected online (via app in smart phones), we suggested that MC characteristics, including MC lengths, blood color and clots, can be taken as indicators into consideration in women's preconception health assessment and clinical deCIsion-making process.34 Further elaborate studies are needed to testify our findings before clinical application.
From the present results, we propose that regulating women's menstrual cycle may be an effective but cheap and easy routine to improve fertility outcome. Indeed, “regulating menstrual cycle”, which was recommended by TCM masters in thousand years, is one of the core principles to improve fecundability in TCM.13 We believe that increasing the knowledge and awareness of MC characteristics for women in productive ages would also bring great benefits to understand their preconception health conditions.
5. ACKNOWLEDGEMENTS
The authors thank Lü Aiping for research protocol, Qi Zhengping and Kou Huixin for data collection, and Betty Chang for giving advice on the whole manuscript.
REFERENCES
- 1. Treloar AE, Boynton RE, Behn BG, Brown BW. The menstrual cycle: variation of the human menstrual cycle through reproductive life. Obstet Gynecol Surv 1968; 12: 77-126. [PubMed] [Google Scholar]
- 2. Mihm M, Gangooly S, Muttukrishna S. The normal menstrual cycle in women. Anim Reprod SCI 2011; 124: 229-36. [DOI] [PubMed] [Google Scholar]
- 3. Brodin T, Bergh T, Berglund L, Hadziosmanovic N, Holte J. Menstrual cycle length is an age-independent marker of female fertility: results from 6271 treatment cycles of in vitro fertilization. Fertil Steril 2008; 90: 1656-61. [DOI] [PubMed] [Google Scholar]
- 4. Frisch RE. Body fat, menarche, fitness and fertility. Hum Reprod 1987; 2: 521-33. [DOI] [PubMed] [Google Scholar]
- 5. Weisman CS, Misra DP, Hillemeier MM, et al. Preconception predictors of birth outcomes: prospective findings from the central Pennsylvania women’s health study. Matern Child Health J 2011; 15: 829-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosenberg MJ, Waugh MS, Higgins JE. The effect of desogestrel, gestodene, and other factors on spotting and bleeding. Contraception 1996; 53: 85-90. [DOI] [PubMed] [Google Scholar]
- 7. Maybin JA, Critchley HOD. Menstrual physiology: implications for endometrial pathology and beyond. Hum Reprod Update 2015; 21: 748-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crawford NM, Pritchard DA, Herring AH, Steiner AZ. Prospective evaluation of the impact of intermenstrual bleeding on natural fertility. Fertil Steril 2016; 105: 1294-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Small CM, Manatunga AK, Klein M, et al. Menstrual cycle characteristics: associations with fertility and spontaneous abortion. Epidemiology 2006; 17: 52-60. [DOI] [PubMed] [Google Scholar]
- 10. Zhang Q, Wang YY, Zhang Y, et al. The influence of age at menarche, menstrual cycle length and bleeding duration on time to pregnancy: a large prospective cohort study among rural Chinese women. BJOG 2017; 124: 1654-62. [DOI] [PubMed] [Google Scholar]
- 11. Manley H, Sprinks J, Breedon P. Menstrual blood-derived mesenchymal stem cells: women’s attitudes, willingness, and barriers to donation of menstrual blood. J Womens Health (Larchmt) 2019; 28: 1688-97. [DOI] [PubMed] [Google Scholar]
- 12. James AH. Heavy menstrual bleeding: work-up and management. Hematol Am Soc Hematol Educ Progrm 2016; 2016: 236-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maciocia G. Obstetrics and gynecology in Chinese medicine. Elsevier Ltd Oxford; 2011. [Google Scholar]
- 14. Lyttleton J. The treatment of infertility with Chinese Medicine. Oxford: Elsevier Ltd., 2013: 250-71. [Google Scholar]
- 15. Alfred A, Ried K. Traditional Chinese medicine: women’s experiences in the treatment of infertility. Aust Fam Physician 2011; 40: 718-22. [PubMed] [Google Scholar]
- 16. Adams J, Lui CW, Sibbritt D, et al. Women’s use of complementary and alternative medicine during pregnancy: a critical review of the literature. Birth 2009; 36: 237-45. [DOI] [PubMed] [Google Scholar]
- 17. Zhang HH, Song XY. Analysis of the global development of traditional and complementary medicine based on WHO global report on traditional and complementary medicine. Zhong Hua Zhong Yi Yao Za Zhi 2020; 35: 3090-3. [Google Scholar]
- 18. Ried K, Alfred A. Quality of life, coping strategies and support needs of women seeking Traditional Chinese Medicine for infertility and viable pregnancy in Australia: a mixed methods approach. BMC Womens Health 2013; 13: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. WU XQ, Huang DH, Qi ZP, Kou HX, Lin QL, Peng J. Design of a questionnaire for evaluating fertile women’s preconception health status. Xian Dai Yu Fang Yi Xue 2012; 39: 6130-3. [Google Scholar]
- 20. Yang Y, He Y, Li Q, et al. Preconception blood pressure and risk of preterm birth: a large historical cohort study in a Chinese rural population. Fertil Steril 2015; 104: 124-30. [DOI] [PubMed] [Google Scholar]
- 21. Ronda E, García AM, Sánchez-Paya J, Moen BE. Menstrual disorders and subfertility in Spanish hairdressers. Eur J Obstet Gynecol Reprod Biol 2009; 147: 61-4. [DOI] [PubMed] [Google Scholar]
- 22. Cho SI, Damokosh AI, Ryan LM, et al. Effects of exposure to organic solvents on menstrual cycle length. J Occup Env Med 2001; 43: 567-75. [DOI] [PubMed] [Google Scholar]
- 23. Bienstock , Fox , Wallach , et al. Johns Hopkins Manual of Gynecology and Obstetrics. J Pediatr Adolesc Gynecol 2015; 23: e51-e52. [Google Scholar]
- 24. Wesselink AK, Wise LA, Hatch EE, et al. Menstrual cycle characteristics and fecundability in a North American preconception cohort. Ann Epidemiol 2016; 26: 482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kolstad HA, Bonde JP, Hjøllund NH, et al. Menstrual cycle pattern and fertility: a prospective follow-up study of pregnancy and early embryonal loss in 295 couples who were planning their first pregnancy. Fertil Steril 1999; 71: 490-6. [DOI] [PubMed] [Google Scholar]
- 26. Harlow SD, Ephross SA. Epidemiology of menstruation and its relevance to women’s health. Epidemiol Rev 1995; 17: 265-86. [DOI] [PubMed] [Google Scholar]
- 27. Delieu JM. The Reproductive System at a Glance, 3rd ed. J Anat 2011; 219: 778. [Google Scholar]
- 28. Jensen TK, Scheike T, Keiding N, Schaumburg I, Grandjean P. Fecundability in relation to body mass and menstrual cycle patterns. Epidemiology 1999; 10: 422-8. [DOI] [PubMed] [Google Scholar]
- 29. Gizzo S, Andrisani A, Noventa M, et al. Menstrual cycle length: a surrogate measure of reproductive health capable of improving the accuracy of biochemical/sonographical ovarian reserve test in estimating the reproductive chances of women referred to ART. Reprod Biol Endocrinol 2015; 13: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. W H O. Worldwide prevalence of anemia 1993-2005: WHO global database on anemia. 2008. [Google Scholar]
- 31. Dobson M. World Health Organization haemoglobin colour scale: a practical answer to a vital need. Updat Anaesth 2002: 51-2. [Google Scholar]
- 32. Millikan M, Xu H, Trevean H. Metal analysis of Si Wu Tang in relation to its clinical application. Aust J Acupunct Chinese Med 2011; 6: 12-8. [Google Scholar]
- 33. Meade TW, Ruddock V, Stirling Y, Chakrabarti R, Miller GJ. Fibrinolytic activity, clotting factors, and long-term incidence of ischaemic heart disease in the Northwick Park Heart Study. Lancet 1993; 342: 1076-9. [DOI] [PubMed] [Google Scholar]
- 34. Robbins CL, D’Angelo D, Zapata L, et al. Preconception health indicators for public health surveillance. J Womens Health (Larchmt) 2018; 27: 430-43. [DOI] [PMC free article] [PubMed] [Google Scholar]


