Abstract
OBJECTIVE:
To assess the effectiveness and safety of acupuncture for post‐stroke fatigue (PSF).
METHODS:
Eight online databases were searched to collect relevant trials of acupuncture for PSF published before April 2021. Meta-analysis was performed by using RevMan 5.4 software. The Grading of Recommendations, Assessment, Development and Evaluation system was used to assess the certainty of evidence.
RESULTS:
Four randomized controlled trials involving 289 PSF patients were identified and included in the systematic review. The results of the Meta-analysis revealed that acupuncture group was significantly better than routine treatment group in improving the effective rate [risk ratio (RR) = 1.15, 95%CI (1.01, 1.33), P = 0.04], reducing the FSS score [mean difference (MD) = -4.71, 95% CI (-6.22, -3.20), P < 0.000 01] and FMA score [MD = 15.60, 95% CI (11.96, 19.23), P < 0.000 01]. Side effects of acupuncture were mild and rarely reported. The certainty of evidence of the outcomes based on the four trials was assessed as low.
CONCLUSIONS:
The existing evidence suggests acupuncture as an adjunct to routine treatment may benefit in managing fatigue in stroke patients. However, high-quality RCTs are needed to further confirm these findings.
Keywords: acupuncture, stroke, fatigue, systematic review, Meta-analysis
1. INTRODUCTION
Post-stroke fatigue (PSF) is one of the most serious sequelae of stroke. It is characterized by fatigue and a lack of energy feeling physically and mentally, and this condition cannot be relieved by rest.1 According to statistics, the prevalence of PSF in stroke survivors ranges from 25% to 85%.2 Persistent fatigue symptoms may limit the rehabilitation process and have a negative impact on the patient's mental health and quality of life.3,4 Fatigue can also increase the disability rate and even mortality of patients.5 In addition, a recent Meta-analysis showed that the fatigue of stroke survivors increased over time.6 Therefore, early detection and treatment of fatigue may have a positive impact on stroke recovery.
At present, the pathogenesis of PSF is still unclear, and its fatigue is thought to be related to biological, psychosocial and behavioral factors.7 Since PSF may be related to a variety of causative factors, there are many potential pharmacological intervention options, such as antidepressants and conscious stimulants.8,9 However, recent studies have shown that there is insufficient evidence to support the effectiveness of pharmacological treatments and the overall effect of drugs is far from satisfactory.9,⇓-11 Therefore, some researchers have begun to turn their attention to non-pharmacological interventions.12
Acupuncture, as one of the oldest non-pharmacological therapy, involves inserting thin needles into specific acupoints at a specific angle to treat diseases.13 In China, acupuncture has been widely used in the management of stroke and related symptoms for a long time, and it has gradually been recognized worldwide.14,15 In addition, acupuncture has been recommended by the World Health Organization (WHO) as a complementary and alternative treatment for stroke management.16 In many published clinical trials on the treatment of PSF with acupuncture, most studies have shown that acupuncture is a beneficial intervention for PSF, and safety issues rarely occur.17 However, no systematic review has been conducted to collect evidence on the efficacy of acupuncture for PSF. Therefore, the current study was conducted to evaluate the effectiveness and safety of using acupuncture to manage PSF.
2. METHODS
The protocol for this study was registered in the PROSPERO (https://www.crd.york.ac.uk/PROSPERO/;registrationnumberCRD42020197221).
2.1. Study identification
The following databases were searched from their inception to April 2021: Embase, PubMed, Web of Science, Cochrane Library, WanFang, China National Knowledge Infrastructure Database, China Science and Technology Journal Database and the Chinese SinoMed Database. The database search was carried out using a combination of MeSH terms and free words, and the search terms include disease name (post-stroke fatigue) and intervention method (acupuncture). References of all included trials were also scanned to identify additional eligible trials. The detailed search strategies in each database are shown in Appendix 1.
2.2. Inclusion/exclusion criteria
We used the following items as eligibility criteria: (a) RCTs assessing acupuncture for PSF were included; (b) participants need to meet the diagnosis of stroke and fatigue at the same time, and there were no restrictions on the pathological types of stroke, including hemorrhagic stroke, ischemic stroke or mixed stroke; (c) in addition to the routine treatment of stroke (including western medicine basic treatment and rehabilitation treatment), the intervention of experimental group only included acupuncture, and the acupuncture here only includes manual acupuncture and electro-acupuncture, regardless of different acupoints or treatment duration; (d) in addition to the routine treatment of stroke, studies that employed sham acupuncture, no treatment or medicine as control group intervention were considered eligible; (e) the included trials measured at least one of the following indicators: clinical efficacy (Proportion of patients with improved fatigue symptoms), Fatigue Severity Scale (FSS), Fugl-Meyer Assessment (FMA), and adverse events. Exclusion criteria: (f) Non-RCTs; (g) duplicates; (h) literature reviews; (i) animal experiments.
2.3. Study selection and data extraction
We input all retrieved articles into EndNote 9 software and use the software to eliminate duplicate records. Two investigators independently screened eligible studies by browsing the title, abstract and full text, and extracted relevant data from the included trials, including the study author, publication date, sample size, mean age, intervention, acupuncture session, acupoints, outcomes and adverse events. If there is a difference in study selection or data extraction process, a third investigator would be asked to judge.
2.4. Study quality assessment
Two investigators independently assessed the quality of the included studies by using the Cochrane Risk of Bias tool version 2 (ROB 2.0), which included the following domains: (a) randomization process; (b) deviations from intended interventions; (c) missing outcome data; (d) measurement of the outcome; (e) selection of the reported result.18 Discrepancies were resolved through negotiation.
2.5. Data synthesis and analysis
Meta-analysis was performed using Review Manager 5.4. Risk ratio (RR) was used to measure dichotomous variables, and mean difference (MD) or standardized mean difference (SMD) was used to measure continuous variables. When results were measured on the same scale, the outcomes were reported as MD; otherwise, the results were reported as SMD. Heterogeneity was evaluated by I2 value and χ2 test. When I2 ≤ 50% and P ≥ 0.10, the fixed effect model was used; Otherwise, the random effects model was used to make a more conservative assessment of the intervention effect, and sensitivity analysis was performed to explore the robustness of the results. If the number of included trials was insufficient (fewer than 10 studies), we did not assess publication bias.
2.6. Certainty of evidence
The GRADE system was adopted to assess the certainty of evidence for the results, and each outcome indicator was divided into four categories: high, medium, low, and very low.19
3. RESULTS
3.1. Literature search
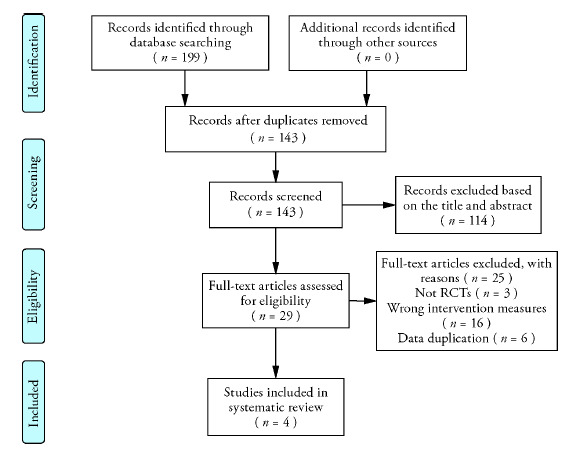
A total of 199 studies were found after primary search. It remained 143 studies after we excluded 56 duplicates. Then, after reading the title, abstract and full text, 139 studies were eliminated. Finally, 4 RCTs20-23 were included in this systematic review. The process of eligible RCT selection is presented in Figure 1.
Figure 1. Study selection process.
3.2. Study characteristics
We included a total of 4 trials from different research teams. Among them, the outcome indicators of one study21 were derived from two RCTs.21,24 Because these two RCTs were based on the same study, we integrated the outcome evaluation indicators of the two RCTs into the same one. A total of 289 PSF patients were involved in these four studies (145 in the acupuncture group, and 144 in the control group). All studies were conducted in China and published in Chinese. The sample sizes of the 4 RCTs ranged from 60 to 99. Characteristics of included 4 RCTs were summarized in Table 1.
Table1.
Characteristics of included studies
| Study | Participants | Interventions | Acupuncture session | Outcomes | ||
|---|---|---|---|---|---|---|
| Number (male/female) | Age (Mean±SD) |
Interventions Group | Control Group | |||
| Yin HN et al 201620 | T: 16 /14 C: 17 /13 |
T:61.16±8.2 C:62.23±8.0 |
MA (GV20, EX-HN1) +C | Routine treatment (rehabilitation) | Once a day, five times per week for 4 weeks, 30 min | CE, FSS |
| Huang Z et al 201821 | T: 27 /8 C: 20 /15 |
T:60.57±10.77 C:60.29±10.11 |
MA (CV12, CV10, CV6, CV4, ST24, ST26) +C | Routine treatment (western medicine basic treatment + rehabilitation) | Once a day, six times per week for 2 weeks, 30 min | CE, FSS, FMA |
| Bei JH et al 201922 | T: 28 /22 C: 26 /23 |
T: 58.46 ±7.48 C: 58.06 ±7.45 |
MA (GV20, GV24, CV4, CV6, ST36, SP6, LR3) +C | Routine treatment (western medicine basic treatment + rehabilitation) | Once a day, five times per week for 4 weeks | FSS, FMA |
| Gao L 201923 | T: 18 /12 C: 21 /9 |
T: 58.17±12.00 C: 58.80±11.99 |
MA (GV4, GV14, GV16, GV20, EX-B2, LI15, LI11, LI4, TE5, LU5, ST36, SP6, BL40, GB39) +C | Routine treatment (western medicine basic treatment + rehabilitation) | Once a day for 8 weeks | CE, FSS |
Notes: T: therapy group; C: control group; CE: clinical efficacy; FMA: Fugl-Meyer Assessment; FSS: Fatigue Severity Scale; MA: manual acupuncture; NR: not reported.
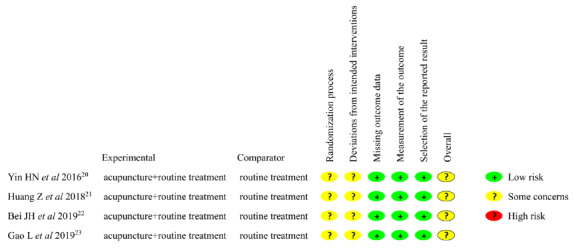
3.3. Risk of bias
The ROB assessment is shown in Figure 2. Although all studies used random number tables for random grouping, none of the studies mentioned the specific details of allocation concealment. In addition, due to the nature of acupuncture manipulations, blinding to participants is not suitable for acupuncture therapy. This makes all included studies have a certain risk of bias.
Figure 2. Risk of bias assessment.
3.4. Efficacy and safety of acupuncture
3.4.1. Clinical efficacy
Three trials evaluated the effective rate of acupuncture for PSF. No heterogeneity was noted (P = 0.72, I2 = 0%), and the fixed-effects model demonstrated that acupuncture group was significantly higher than the routine treatment group [RR = 1.15, 95% CI (1.01, 1.33), P = 0.04] in improving effective rate (Figure 3A).
Figure 3. Meta-analysis results of the efficacy of acupuncture versus control group.
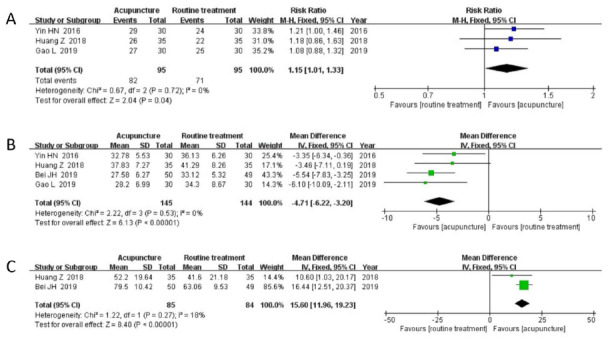
A: forest plot of acupuncture on the effective rate; B: forest plot of acupuncture on FSS; C: forest plot of acupuncture on FMA. FSS: Fatigue Severity Scale; FMA: Fugl-Meyer Assessment.
3.4.2. FSS
Four trials assessed the severity of fatigue in stroke patients by using the FSS scores. The four RCTs showed no heterogeneity (P = 0.53, I2 = 0%), and the fixed-effects model revealed that acupuncture group could further improve fatigue symptoms compared with the routine treatment group [MD = -4.71, 95% CI (-6.22, -3.20), P < 0.000 01] (Figure 3B).
3.4.3. FMA
Two trials evaluated the recovery of motor function by using the FMA score. Analysis of data from FMA showed low heterogeneity (P = 0.27, I2 = 18%), and the fixed-effects model showed that acupuncture group could further improve motor function compared with the routine treatment group [MD = 15.60, 95% CI (11.96, 19.23), P < 0.000 01] (Figure 3C).
3.4.4. Safety assessment
Two RCTs21,23 reported the safety of acupuncture. One study23 reported that 3 cases in the acupuncture group experienced subcutaneous hemorrhage, which disappeared after treatment. And one study21 reported no adverse effects related to acupuncture.
3.5. Acupuncture point
A total of 23 acupoints were involved in the included 4 trials. Among them, Baihui (GV20) has the highest frequency of use. A total of 3 studies have selected this acupoint. The top five acupoints used in frequency were Baihui (GV20), Qihai (CV6), Guanyuan (CV4), Zusanli (ST36), Sanyinjiao (SP6).
3.6. Publication bias
Since the number of RCTs included in this study was only four (fewer than 10 studies), we did not perform a publication bias analysis.
3.7. Certainty of evidence
In general, all results were ranked as having low-quality evidence. The main reason for the decline in the certainty of evidence may be related to the poor methodological quality of the included studies and the small sample size. Table 2 presents the results of the GRADE analysis.
Table 2.
GRADE quality grading evaluation.
| Quality assessment | No of patients | Quality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Experimental group | Control group | |
| Clinical efficacy (Acupuncture+Routine treatment vs Routine treatment) | |||||||||
| 3 | Randomized | Serious a | No serious inconsistency | No serious indirectness | Serious b | None | 82/95 (86.3%) | 71/95 (74.7%) | ⊕⊕◯◯ Low |
| FSS (Acupuncture+Routine treatment vs Routine treatment) | |||||||||
| 4 | Randomized | Serious a | No serious inconsistency | No serious inconsistency | Serious b | None | 145 | 144 | ⊕⊕◯◯ Low |
| FMA (Acupuncture+Routine treatment vs Routine treatment) | |||||||||
| 2 | Randomized | Serious a | No serious inconsistency | No serious inconsistency | Serious b | None | 85 | 84 | ⊕⊕◯◯ Low |
Notes: aRisk of bias: the quality of all included studies is not high; bImprecision: small sample size. GRADE: the Grading of Recommendations, Assessment, Development and Evaluation; FSS: Fatigue Severity Scale;FMA: Fugl-Meyer Assessment.
4. DISCUSSION
Stroke is a major cause of mortality and disability worldwide 3 . Due to the aging population, stroke has become an increasingly serious health concern. At the same time, those who survive a stroke often suffer from residual functional disabilities, cognitive deficits and emotional problems. Among them, fatigue is one of the most common complaints after stroke, and the management and prevention of PSF has been listed as one of the ten research priorities related to life after stroke.25,⇓-27 Although the prevalence of fatigue in stroke patients is high, the pathophysiology of fatigue is poorly understood, and there is almost no evidence-based therapy to relieve fatigue.9 Acupuncture has been used to treat stroke and its sequelae for centuries in China, and it has the advantages of reliable efficacy, easy operation, and safety.14 Although the pathogenesis of PSF is still unclear, and PSF is also considered to be a multifactorial disease with complex etiology,28 the clinical and basic research on acupuncture treatment of stroke and its sequelae have confirmed the efficacy of acupuncture. Acupuncture can promote the repair of the injured nervous system, reduce inflammation, increase cerebral blood flow, and regulate oxidative stress to improve stroke-related symptoms.14,29,⇓-31 In addition, several recent Meta-analysis have also confirmed the anti-fatigue effect of acupuncture,32,⇓-34 which may be related to the effect of acupuncture in regulating perturbed energy Metabolism, choline Metabolism, attenuating reactive oxygen species induced stress and down-regulating the levels of related inflammatory factors (CPR, IL-6, TNF-α, IFN-γ, sTNF-R1).35,⇓,⇓-38 Therefore, acupuncture is regarded as a promising intervention method for PSF.
In this systematic review, although the acupoint plans used by these 4 RCTs were different, some acupoints were still used very frequently. The five most popular acupoints were Baihui (GV20), Qihai (CV6), Guanyuan (CV4), Zusanli (ST36), Sanyinjiao (SP6). According to the theory of traditional Chinese medicine (TCM), we found that the above-mentioned acupoints have the properties of replenishing Qi and activating blood, regulating Qi, and awakening the brain.39 At the same time, TCM theory believes that the main cause of PSF is related to the deficiency of Qi and blood and poor circulation of Qi and blood.40,41 Therefore, the therapeutic effects of the above 5 acupoints are beneficial to improve the fatigue symptoms of stroke patients.
To date, there is no systematic review focusing on acupuncture for PSF, and this is the first Meta-analysis to evaluate the efficacy of acupuncture for PSF. In this study, we included 4 eligible trials with a total of 289 PSF participants in this review. Compared with routine treatment, acupuncture combined with routine treatment has shown potential benefits in improving FSS, FMA and clinical efficacy. In addition, in terms of safety, one study reported no adverse events, and only one study reported subcutaneous hemorrhage after acupuncture treatment, but the symptoms were mild. Therefore, based on the findings of this review, we suggest that acupuncture might be an effective and safe adjuvant therapy for PSF. However, the GRADE system has rated the existing evidence as “low”. This weakens the reliability and influence of the evidence. Therefore, it is necessary to further explore the efficacy of acupuncture for PSF.
There were some limitations exist in the current study. Firstly, we only searched the Chinese and English databases, which may miss some potential trials published in other languages that meet the inclusion criteria. In addition, the four trials included in this study were all conducted in China. Therefore, the evidence in this review may have regional limitations. Secondly, the methodological quality of the evidence in this study is not high. None of the included trials reported the implementation of allocation concealment. Moreover, due to the particularity of acupuncture, it is not feasible to implement a blind design. Thirdly, despite our extensive search, this study was still limited by the number of included trials and the small sample size, which may lead to inaccurate research evidence.
In conclusion, based on currently limited evidence, the results of our Meta-analysis show that acupuncture as an adjunct to routine treatment may benefit in managing PSF. However, the number of RCTs included in this study is limited and the methodological quality is suboptimal, which greatly weakens the reliability and influence of the evidence. Therefore, high-quality RCTs are still needed to confirm the benefits of acupuncture for PSF.
Table 3.
Appendix 1 Search strategy in each database
| Database | Search strategy |
|---|---|
| PubMed | (Stroke [MeSH] OR Cerebrovascular Disorders [MeSH] OR Brain Ischemia [MeSH] OR Cerebral Hemorrhage [MeSh] OR Cerebral infarction [MeSH] OR Cerebrovascular Disorder [MeSH] OR Stroke [Ti/Ab] OR Cerebrovascular Disorders [Ti/Ab] OR Brain Ischemia [Ti/Ab] OR Cerebral Hemorrhage [Ti/Ab] OR Cerebral infarction [Ti/Ab] OR Cerebrovascular Disorder [Ti/Ab]) AND (Fatigue [MeSH] OR Fatigue [Ti/Ab] OR Tiredness [Ti/Ab] OR exhaustion [Ti/Ab] OR Fatigue after stroke [Ti/Ab] OR Post stroke fatigue [Ti/Ab]) AND (Acupuncture [MeSH] OR Acupuncture therapy [MeSH] OR Acupuncture [Ti/Ab] OR Electroacupuncture [Ti/Ab] OR Electro-acupuncture [Ti/Ab] OR Acupoint [Ti/Ab]) |
| Embase |
(Stroke/exp OR Cerebrovascular Disorders/exp OR Brain Ischemia/exp OR Cerebral Hemorrhage/exp OR Cerebral infarction/exp OR Cerebrovascular Disorder/exp OR Stroke:ti,ab OR Cerebrovascular Disorders:ti,ab OR Brain Ischemia:ti,ab OR Cerebral Hemorrhage:ti,ab OR Cerebral infarction:ti,ab OR Cerebrovascular Disorder:ti,ab) AND (Fatigue/exp OR Fatigue:ti,ab OR Tiredness:ti,ab OR Exhaustion:ti,ab OR Fatigue after stroke:ti,ab OR Post stroke fatigue:ti,ab) AND (Acupuncture/exp OR Acupuncture therapy/exp OR Acupuncture:ti,ab OR Electroacupuncture:ti,ab OR Electro-acupuncture:ti,ab OR Acupoint:ti,ab) |
| The Cochrane Library | 1. Stroke:ti,ab OR Cerebrovascular Disorders:ti,ab OR Brain Ischemia:ti,ab OR Cerebral Hemorrhage:ti,ab OR Cerebral infarction:ti,ab OR Cerebrovascular Disorder:ti,ab 2. MeSH descriptor: [Stroke] explode all trees 3. MeSH descriptor: [Cerebrovascular Disorders] explode all trees 4. MeSH descriptor: [Brain Ischemia] explode all trees 5. MeSH descriptor: [Cerebral Hemorrhage] explode all trees 6. MeSH descriptor: [Cerebral infarction] explode all trees 7. MeSH descriptor: [Cerebrovascular Disorder] explode all trees 8. #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 9. MeSH descriptor: [Fatigue] explode all trees 10. Fatigue:ti,ab OR Tiredness:ti,ab OR Exhaustion:ti,ab OR Fatigue after stroke:ti,ab OR Post stroke fatigue:ti,ab 11. #9 OR #10 12. MeSH descriptor: [Acupuncture] explode all trees 13. MeSH descriptor: [Acupuncture therapy] explode all trees 14. Acupuncture:ti,ab OR Electroacupuncture:ti,ab OR Electro-acupuncture:ti,ab OR Acupoint:ti,ab 15. #12 OR #13 OR #14 16. #8 AND #11 AND #15 |
| Web of science | 1. TS=( Stroke OR Cerebrovascular Disorders OR Brain Ischemia OR Cerebral Hemorrhage OR Cerebral infarction OR Cerebrovascular Disorder) 2. TI=(Stroke OR Cerebrovascular Disorders OR Brain Ischemia OR Cerebral Hemorrhage OR Cerebral infarction OR Cerebrovascular Disorder) 3. #1 OR #2 4. TS=(Fatigue) 5. TI=( Fatigue OR Tiredness OR Exhaustion OR Fatigue after stroke OR Post stroke fatigue) 6. #4 OR #5 7. TS =( Acupuncture OR Acupuncture therapy) 8. TI=( Acupuncture OR Electroacupuncture OR Electro-acupuncture OR Acupoint) 9. #7 OR #8 10. #3 AND #6AND #9 |
| CNKI | (SU%'中风'+'脑卒中'+'脑梗塞'+'脑出血'+'脑梗死') and (SU%'疲劳'+'疲乏') and (SU%'针刺'+'针灸'+'电针'+'针') |
| WanfangData | 主题= (中风 OR脑卒中 OR 脑梗塞 OR 脑出血OR 脑梗死) AND主题= (疲劳OR 疲乏) AND 主题= (针刺 OR 针灸 OR 电针 OR 针) |
| VIP | U=(中风 OR 脑卒中OR 脑梗塞OR 脑梗死 OR 脑出血) AND U=(疲劳 OR 疲乏) AND U=(针刺 OR 针灸 OR 电针 OR 针) |
| SinoMed | (中风[标题] OR 脑卒中[标题] OR 脑梗塞[标题]) OR 脑梗死[标题] OR 脑出血[标题]) AND (疲劳[标题]) OR 疲乏[标题]) AND (针刺[标题] OR 针灸[标题] OR 电针[标题] OR 针[标题]) |
REFERENCES
- 1. De Groot MH, Phillips SJ, Eskes GA. Fatigue associated with stroke and other neurologic conditions: implications for stroke rehabilitation. Arch Phys Med Rehabil 2003; 84: 1714-20. [DOI] [PubMed] [Google Scholar]
- 2. Cumming TB, Packer M, Kramer SF, English C. The prevalence of fatigue after stroke: a systematic review and Meta-analysis. Int J Stroke 2016; 11: 968-77. [DOI] [PubMed] [Google Scholar]
- 3. Lerdal A, Bakken LN, Kouwenhoven SE, et al. Poststroke fatigue--a review. J Pain Symptom Manage 2009; 38: 928-49. [DOI] [PubMed] [Google Scholar]
- 4. de Bruijn MA, Synhaeve NE, van Rijsbergen MW, et al. Quality of life after young ischemic stroke of mild severity is mainly influ-enced by psych-ological factors. J Stro-ke Cere-brovasc Dis 2015; 24: 2183-8. [DOI] [PubMed] [Google Scholar]
- 5. Glader EL, Stegmayr B, Asplund K. Post-stroke fatigue: a 2-year follow-up study of stro-ke patients in Swe-den. Stroke 2002; 33: 1327-33. [DOI] [PubMed] [Google Scholar]
- 6. Cumming TB, Yeo AB, Marquez J, et al. Investigating post-stro-ke fatigue: an indi-vi-dual participant data Meta-analysis. J Psy-chosom Res 2018; 113: 107-12. [DOI] [PubMed] [Google Scholar]
- 7. Wu S, Mead G, Macleod M, Chalder T. Model of unde-rstanding fatigue after stroke. Stroke 2015; 46: 893-8. [DOI] [PubMed] [Google Scholar]
- 8. Brioschi A, Gramigna S, Werth E, et al. Effect of modafinil on subjective fatigue in multiple sclerosis and stroke patients. Eur Neurol 2009; 62: 243-9. [DOI] [PubMed] [Google Scholar]
- 9. Wu S, Ku-lubaev MA, Chun HY, et al. Inter-ventions for post-stroke fatigue. Co-chrane Data-base Syst Rev 2015: CD007030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Karaiskos D, Tzave-llas E, Spengos K, Vassilopoulou S, Papar-rigopoulos T. Dulo-xetine versus citalopram and sertraline in the treatment of poststroke depression, anxiety, and fatigue. J Neuro-psy-chiatry Clin Neuro-sci 2012; 24: 349-53. [DOI] [PubMed] [Google Scholar]
- 11. Choi-Kwon S, Choi J, Kwon SU, Kang DW, Kim JS. Fluo-xetine is not effective in the tr-eatment of post-stroke fatigue: a double-blind, placebo-contr-olled stu-dy. Cerebro-vasc Dis 2007; 23: 103-8. [DOI] [PubMed] [Google Scholar]
- 12. Su Y, Yuki M, Otsuki M. Non-pharm-acological interventions for post-stroke fatigue: systematic review and network Meta-analysis. J Clin Med 2020; 9: 621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. You J, Li H, Xie D, Chen R, Chen M. Acu-puncture for chr-onic pain-related dep-ression: a systematic review and Meta-analysis. Pain Res Manag 2021; 2021: 6617075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang A, Wu HM, Tang JL, Xu L, Yang M, Liu GJ. Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev 2016: CD004131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xu M, Li D, Zhang S. Acupuncture for acute stroke. Cochrane Database Syst Rev 2018; 3: CD003317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chavez LM, Huang SS, MacDonald I, Lin JG, Lee YC, Chen YH. Mechanisms of acupuncture therapy in ischemic stroke rehabilitation: a literature review of basic studies. Int J Mol Sci 2017; 18: 2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu X, Yang FM, Dong LL, Hao CY. A clinical study on efficacy of Tiaoshen Yiqi acupuncture therapy in treating patients with post stroke fatigue. Zhong Guo Zhong Xi Yi Jie He Ji Jiu Za Zhi 2018; 25: 494-8. [Google Scholar]
- 18. Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 19. Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011; 64: 401-6. [DOI] [PubMed] [Google Scholar]
- 20. Yin HN, Guo YH, Li Q. Clinical observation of acupuncture at Baihui (GV20) and Sishencong (EX-HN1) combined with rehabilitation training on patients of post stroke fatigue. Zhong Guo Zhong Yi Ji Zheng 2016; 2016: 1746-8. [Google Scholar]
- 21. Huang Z, Zhan LC, Chen HX, Pan RH. Abdominal acupuncture combined with rehabilitation training for post-stroke fatigue: a randomized controlled trial. Zhong Yi Yao Dao Bao 2018; 24: 71-3. [Google Scholar]
- 22. Bei JH, Chen PD, Ning Y, Wang L, Yang ZX. Clinical effect of "Tiaoren Tongdu" acupuncture combined with rehabilitation training in the treatment of fatigue after cerebral infarction. Xian Dai Zhong Xi Yi Jie He Za Zhi 2019; 28: 2443-6. [Google Scholar]
- 23. Gao L. Effect of tongdu tiaoshen acupuncture on homocysteine level in patients with post-stroke fatigue and its therapeutic effect Hefei: Anhui University of Chinese Medicine, . 2019: 17-27. [Google Scholar]
- 24. Zhan LC, Pan RH, He MF, et al. Effect and inflammatory mechanism of abdominal acupuncture combined with rehabilitation training for patients with post-stroke fatigue. Zhong Xi Yi Jie He Xin Nao Xie Guan Bing Za Zhi 2017; 15: 1966-8. [Google Scholar]
- 25. Rudberg AS, Berge E, Laska AC, et al. Stroke survivors' priorities for research related to life after stroke. Top Stroke Rehabil 2021; 28: 153-8. [DOI] [PubMed] [Google Scholar]
- 26. Pollock A, St George B, Fenton M, Firkins L. Top. 10 research priorities relating to life after stroke--consensus from stroke survivors, caregivers, and health professionals. Int J Stroke 2014; 9: 313-20. [DOI] [PubMed] [Google Scholar]
- 27. Pollock A, St George B, Fenton M, Firkins L. Top ten research priorities relating to life after stroke. Lancet Neurol 2012; 11: 209. [DOI] [PubMed] [Google Scholar]
- 28. Choi-Kwon S, Kim JS. Poststroke fatigue: an emerging, critical issue in stroke medicine. Int J Stroke 2011; 6: 328-36. [DOI] [PubMed] [Google Scholar]
- 29. Su XT, Wang L, Ma SM, et al. Mechanisms of acupuncture in the regulation of oxidative stress in treating ischemic stroke. Oxid Med Cell Longev 2020; 2020: 7875396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cao BQ, Tan F, Zhan J, Lai PH. Mechanism underlying treatment of ischemic stroke using acupuncture: transmission and regulation. Neural Regen Res 2021; 16: 944-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chang QY, Lin YW, Hsieh CL. Acupuncture and neuroregen-eration in ischemic stroke. Neural Regen Res 2018; 13: 573-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yin ZH, Wang LJ, Cheng Y, et al. Acupuncture for chronic fatigue syndrome: an overview of systematic reviews. Chin J Integr Med 2021; 27: 940-6. [DOI] [PubMed] [Google Scholar]
- 33. Zhang Q, Gong J, Dong H, Xu S, Wang W, Huang G. Acupuncture for chronic fatigue syndrome: a systematic review and meta-analysis. Acupunct Med 2019; 37: 211-22. [DOI] [PubMed] [Google Scholar]
- 34. Jang A, Brown C, Lamoury G, et al. The effects of acupuncture on cancer-related fatigue: updated systematic review and Meta-analysis. Integr Cancer Ther 2020; 19: 1534735420949679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shui L, Yi RN, Wu YJ, et al. Effects of Mongolian warm acup-uncture on iNOS/NO and inflammatory cytokines in the hippo-campus of chronic fatigue rats. Front Integr Neurosci 2019; 13: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ma H, Liu X, Wu Y, Zhang N. The intervention effects of acupuncture on fatigue induced by exhaustive physical exercises: a metabolomics investigation. Evid Based Complement Alternat Med 2015; 2015: 508302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Qing P, Zhao JF, Zhao CH, Hu J, Lin YL, He KJ. Effect of acupuncture on patients with cancer-related fatigue and serum levels of CRP, IL-6, TNF-alpha and sTNF-R1. Zhong Guo Zhen Jiu 2020; 40: 505-9. [DOI] [PubMed] [Google Scholar]
- 38. Wang C, Xie WJ, Liu M, et al. Effect of manual acupuncture stimulation of "Baihui" (GV 20), etc. on serum IFN-gamma and IL-4 contents in rats with chronic fatigue syndrome. Zhen Ci Yan Jiu 2014; 39: 387-9. [PubMed] [Google Scholar]
- 39. Zhou Y, Zhou GY, Li SK, Jin JH. Clinical observation on the therapeutic effect of electroacupuncture combined with cupping on post-stroke fatigue. Zhen Ci Yan Jiu 2010; 35: 380-3. [PubMed] [Google Scholar]
- 40. Xu L, Xu XY, Hou XQ, Wang FG, Gao S, Zhang HT. Adjuvant therapy with Astragalus membranaceus for post-stroke fatigue: a systematic review. Metab Brain Dis 2020; 35: 83-93. [DOI] [PubMed] [Google Scholar]
- 41. Guo YH, Chen HX, Xie RM. Effects of Qi-supplementing dominated Chinese materia medica combined with rehabilitation training on the quality of life of ischemic post-stroke fatigue patients of Qi deficiency syndrome. Zhong Guo Zhong Xi Yi Jie He Za Zhi 2012; 32: 160-3. [PubMed] [Google Scholar]


