Abstract
We want to explore the analgesic brain effect of the moxibustion at heat-sensitized Yaoyangguan (GV3) in patients with lumbar disc herniation (LDH) and myofascial pain syndrome (MPS). In an assessor-blinded observational study, we will include 15 LDH and 15 MPS. They will accept same treatment of heat-sensitive moxibustion at Yaoyangguan (GV3). The resting-state functionality magnetic resonance imaging image data of brain activities before and after treatment will be analyzed by mean fractional amplitude of low-frequency fluctuation, regional homogeneity analysis and brain functional connection. We select seed of first sensory cortex, second sensory cortex, insula cortex, periaqueductal gray and anterior cingulate cortex as the regions of interest to analyse the relationship between brain functional connectivity of pain-related networks and clinical data. Our study could disclose key brain targets and central response characteristics of the analgesic brain effect and the brain functional connection of heat-sensitive moxibustion.
Keywords: lumbar disc herniation, myofascial pain syndrome, point GV3 (Yaoyangguan), resting-state functionality magnetic resonance imaging, heat-sensitive moxibustion, mean fractional amplitude of low-frequency fluctuation, regional homogeneity, pilot projects
1. INTRODUCTION
Acupoint, designated locations along nerves or organ meridians, is the response point of disease as well as the operative site. It is closely related with meridians, viscera, Qi and blood. Researches have put forward that the function of acupoint is dynamic, it would regulate its nature and strength with the different functional status of its target organs.1 Under pathological conditions, the site of the acupoint from resting to active.2 Head first observed that when visceral lesions happened, some areas of the skin become more sensitive and even referred pain.3 Team of professor Chen Rixin are dedicated to the research of heat-sensitive moxibustion (HSM). They have put forward that there are six HSM sensations, it appears alone or combination in clinically, 10% in healthy and 70% in sick people, with the disease recovery those responses gradually disappear.4
Several systematic reviews and Meta-analysis have reported that HSM, as a safe method, is effective in relieving the pain of the patient, especially in lumbar disc herniation (LDH) and myofascial pain syndrome (MPS).5.6 Although number of clinical trials have proved the effectiveness of HSM in relieving pain, few researches focus on the analgesia mechanism of heat-sensitive. “Acupoints-brain relation hypothesis” suggested that the biological basis of acupoints must depend on the brain regulation effect.7 By means of the image technology, it has demonstrated that nociceptive stimuli could activate several cortical network activities, those areas named as “pain matrix” participate the pain perception and process.8
It is believed that pain stimulation can specifically activate the brain regions matrix region, which includes the first sensory cortex (S1), second sensory cortex (S2), insula cortex (IC), anterior cingulate cortex (ACC) and periaqueductal gray (PAG).9 S1 and S2 could regulate the sensory part of pain from stimulus localization, intensity and quality discrimination, which are the significant part of lateral pain system. The latter regions of IC and ACC could effectively regulate the emotional part of pain from emotional reactions and stimulus related selective attention, which are consist of the medial pain system.10,11 Several studies showed that patients of chronic low back pain with structure and function variation in ACC.12,13 PAG is an important center of the pain regulating nerve axis, which could regulate the nociceptive input from spinal dorsal horn and affect the sensory of the pain feeling.14
Recently a variety of functional neuroimaging technology have emerged to explore brain function, while functionality magnetic resonance imaging (fMRI) is widely used in the research of acupoint for its noninvasive, radiation-free and highly sensitive spatial discrimination. Task-state fMRI can reveal structural changes in the brain involved in specific stimuli or instructions; resting-state fMRI (rfMRI) can present the spontaneous activity of each brain area and analyze the data to reflect the changes of brain motor function network connection.15,16 Study have showed that moxibustion at heat-sensitized Dubi (ST35) in patients with knee osteoarthritis (KOA) by rfMRI, the change of fractional amplitude of low-frequency fluctuation (fALFF) values and regional homogeneity (ReHo) values were statistically significant when compared with conventional moxibustion.17
Previous studies have proved the significance of the heat-sensitized acupoint in patients with pain disease. We explore the central effect mechanism further, when patients with different pain diseases receive moxibustion at same heat-sensitized acupoint. We use rfMRI systematically to investigate the central brain effect and cerebral mechanism of the moxibustion at heat-sensitized Yaoyangguan (GV3) in patients with LDH and MPS.
2. METHODS
2.1. Objectives
(a) Whether there is any difference in the central effect mechanism, when patients with different pain diseases receive moxibustion at same heat-sensitized acupoint.
(b) Identify the key brain targets and central response characteristics of the analgesic brain effect when people receive the HSM.
2.2. Study design and setting
The observational study will be conducted at the Affiliated Hospital of Jiangxi University of TCM in Nanchang, with inpatient from acupuncture and moxibustion department and orthopedics department. The study will be sequentially performed in five period, the flowchart presented in Figure 1.
Figure 1. Flowchart of the participants.
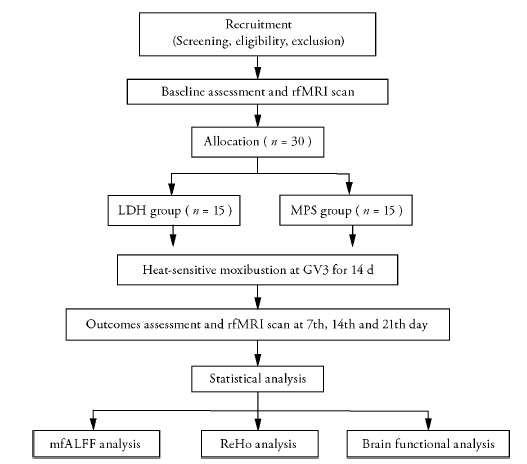
rfMRI: resting-state functionality magnetic resonance imaging; LDH: lumbar disc herniation; MPS: myofascial pain syndrome; GV3: Yaoyangguan (GV3); mfALFF: mean fractional amplitude of low-frequency fluctuation; ReHo: regional homogeneity.
2.3. Ethics approval and consent to participate
The trial follows the principal ethical guidelines of Helsinki Declaration and has received approval from the Independence Ethics Committee of the Affiliated Hospital of Jiangxi University of TCM (ethic approval number: JZFYKYLL20200525013). Each enrolled participant will provide written informed consent and be asked to sign for it before participating. Our study has been registered in the Chinese Clinical Trial Registry (ChiCTR2000035027). The trial was approved by the research ethics committee. The results of the study will be published in a peer-reviewed academic journal and will also be disseminated electronically through conference presentations.
2.4. Participants
Eligible participants met diagnostic criteria of MPS (Simons 1990 clinical criteria) 18 or LDH (1995, Guiding principles of clinical research on the treatment of lumbar intervertebral disc herniation with new Chinese medicine) will be recruited.19
2.5. Eligibility criteria
(a) Patients aged 16-60 years, male or female; (b) Right-handed; (c) With normal consciousness, coordinated behavior, they can correctly express the moxibustion sensation; (d) Acupoint heat-sensitization phenomenon exists in the region of Yaoyangguan (GV3). The location of Yaoyangguan (GV3) is on the lower back which is below the 4th lumbar spine. The following patients sensation will suggest the acupoint heat-sensitization: heat penetration means the heat sensation conducting from the moxa local skin surface into deep tissue, or even into the lumbar vertebra or abdomen; heat expansion means the heat sensation spreading the surrounding little by little around the moxa point; heat transmission means the heat sensation transferring along some pathway or direction, even to the back or thigh; local not or slightly but far heat, surface not or slightly but deep heat and non-heat-sensitive sensations. Some patients may exist more than one heat-sensitive sensation; (e) Modified Japanese Orthopaedic Association low back pain score (M-JOA) > 10; (f) Sign the informed consent by the patient himself or voluntarily.
2.6. Exclusion criteria
(a) Single nerve palsy or cauda equina paralysis manifested as muscle paralysis or rectal and bladder symptoms; (b) lumbar spinal stenosis and space occupying lesions caused by other reasons, or lumbar tumor, infection, tuberculosis, etc.; (c) combined with serious life-threatening primary diseases referred to cardio cerebrovascular system, liver, kidney and hematopoietic system, as well as psychosis; (d) pregnant or lactating women; (e) fainting during moxibustion or repelling moxibustion; (f) patients who are prohibited by magnetic resonance testing.
2.7. Sample size
It is not applicable to calculate the sample size for lacking of similar research. Professor Thirion and José M. Soares suggested that an optimal sample size of 16-32 could provide adequate reliability for fMRI investigations.20.21 So we plan to include 30 participants in our study.
2.8. Allocation
Eligible patients will be allocated into two parallel groups after baseline assessment: LDH group and MPS group. Therapists get professional training to ensure each participants receive the same treatment. Assessors who did not participate in the treatment and who are blinded to the allocation results will perform the outcome assessment.
2.9. Participant timeline
Our study will be carried out sequentially as follows: enrollment period of 6 months to set up the research group and form the operation manual, establish information acquisition database framework to select eligible patients to participate the research; a run-in period of one week prior to allocation, which give the patient enough time to familiar with the process of the research; a treatment period of 14 d (7 sessions per week); assessment period with five phrase (1st day before and after treatment, the 7th day during treatment, the 14th day and 21th after treatment). The schematic diagram is shown in Figure 2.
Figure 2. Study schedule for data collection.
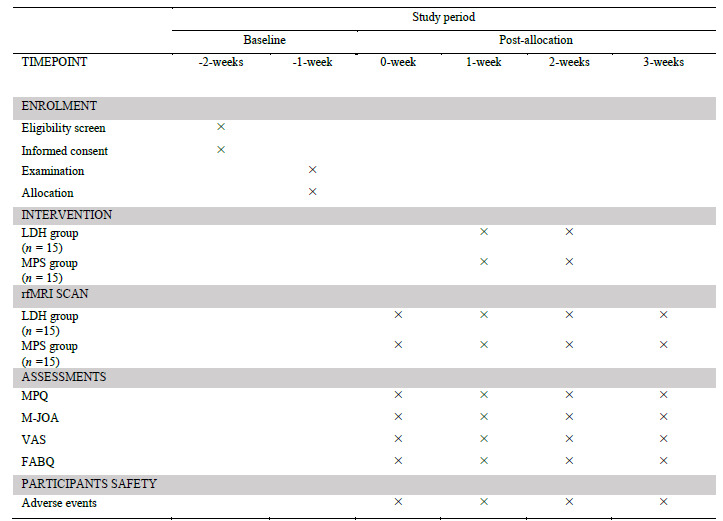
LDH: lumbar disc herniation; MPS: myofascial pain syndrome; rfMRI: resting-state functionality magnetic resonance imaging; MPQ: mcGill pain questionnaire; M-JOA: modified Japanese orthopaedic association scale; VAS: visual visual analog scale; FABQ: fear-avoidance beliefs questionnaire.
2.10. Intervention
(a) Environment: in a quiet, sealing, opacity room and temperature between 24 ℃ to 30 ℃; (b) position: the patient lies on the bed in prone position and fully expose the moxibustion site; (c) material: we choose the moxa stick manufactured by Henan Nanyang Hanfang Aiye Co., Ltd., China. The specification parameter is 12 cm (length) × 3 cm (diameter); (d) therapists: those who have received professional training with clinical experience more than 5 years in acupuncture and moxibustion are qualified; (e) method: clinical studies showed that Yaoyangguan (GV3) is high frequency point for MPS and LDH with great therapeutic effect.22 Therapist hold the ignite moxasticks over the region of Yaoyangguan (GV3) about distance of 3cm to search acupoint heat-sensitive phenomenon. The specific operation should refer to the book of Heat-sensitive moxibustion practical reader.23 (f) course: patients receive the treatment once a day for 15 min, a total of 14 sessions.
2.11. rfMRI
rfMRI is performed by 3.0TSigna scanner (Sign HDx 3.0T, General Electric Company, Wauwatosa, WI, USA) at the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, China. Each participant will receive 5 MRI sessions (one structural image before treatment, 4 functional images after treatment on the 1st, 7, 14, 21th). Before scanning, patients should be familiar with the surroundings, and they are asked to wear blinder and earplugs to reduce audio-visual interference. They are introduced to close their eyes and think of nothing without falling asleep. Head motion is minimized using foam pads and a headband. At the beginning of each session, an 8 min 3D-T1 weighted structural image is required to use gradient echo sequence to scan the whole brain, which is acquired with TR/TE/FA = 12 ms/4.2 ms/15°, a field of view (FOV) of 240 × 240 mm2 with 249 slices with 1.2 mm slice thickness, interval of 1.0 mm, a matrix size of 64 × 64 mm and resolution of 1 mm. The 7 min 10 s functional images are required to use echo-planar imaging (EPI) sequence, which is equipped with TR/TE/FA = 2000 ms/40 ms/90°, 33 slices with 5 mm thickness, interval of 1.0 mm, 4 × 4 × 4 mm voxel size, FOV of 240 × 240 mm2, a matrix size of 64 × 64 mm.
2.12. Outcomes
McGill Pain Questionnaire (MPQ) is used to assess pain severity and its characteristics of MPS, and Modified Japanese Orthopaedic Association scale (M-JOA), visual analog scale (VAS) are designed to measure intensity scores of LDH.24.25 Fear-Avoidance Beliefs Ques-tionnaire (FABQ) is used to assess the pain affects to the physical activity and working.26 The outcome measured above will be assessed before treatment, 7, 14, and 21 d. Therapeutic effect was assessed by comparing baseline and final conditions reported by the patient. Adverse effects during treatment will be recorded on the trial. Once it happens, stop the research immediately and take relevant measures to ensure the safety of the participants.
2.13. Adverse events
We define adverse events as unfavorable or unintended signs, symptoms or disease occurring after treatment. Such as blister, scald, swelling, dry cough and so on. In every visit, adverse events will be reported by participants and examined by the practitioner.
2.14. Data acquisition and preprocessing
The process will be conducted by DPARSFA2.2 (Data Processing Assistant for rfMRI) and REST V1.8. Before the data analysis, we should adjust the data form from DICOM images to NIFTI in order to facilitate data processing and matching corresponding software functions. We will respectively move the structural image and functional images into the T1Raw file and FunRaw file. Data preprocessing includes removing first time point, slice timing, realignment, image registration, T1 segmentation, normalization to the MNI space, smoothing, linear detrending and bandpass temporal filtering (0.01-0.08 Hz).
2.15. Data analyses
Demographic and clinical data (e.g., MPQ, M-JOA, VAS and FABQ) will be analyzed by SPSS 24.0 (IBM Corp., Armonk, NY, USA). The level of significance was set as P < 0.05. We select seed of S1, S2, IC, ACC and PAG as the regions of interest (ROI) to analyze the relationship between brain functional connectivity of pain-related networks and clinical data. Mean fractional amplitude of low-frequency fluctuation (mfALFF) analysis and ReHo analysis will be performed by Statistical Parametric Mapping SPM8 (https://www.fil.ion.ucl.ac.uk/spm/software/spm8/) and REST 1.827 (http://www.restfmri. net/ forum/ REST_V1.8). Paired t-test will be used to assess the difference in mfALFF and ReHo between the patients with LDH and MPS. Significant differences are set at the threshold of voxel-wise P < 0.05 (corrected), with a cluster size ≥ 85 voxels. In addition, pearson correlation coefficients will be used to estimate the connection between the seed region and all of the voxels within the whole brain separately based on different patients and conditions. The standardized ReHo Z-maps apply to subsequent group-level analysis. Significant differences are set at the threshold of voxel-wise P < 0.01 (corrected), cluster size > 2295 mm3. Intragroup standardized values of mfALFF and ReHo maps will be constructed by computing a paired t-test between baseline and after HSM mfALFF and ReHo values (AlphaSim correction at P < 0.05, edge connected cluster connectivity criterion, rmm = 5, continuous voxel ≥ 85).
3. DISCUSSION
Pain is an unpleasant sensation when people receive the actual or potential tissue injury which is detected by nerve endings of nociceptive neurons.28 The negative cognition and emotion accompanied by pain bring a great burden to the life and work of patients. Statistically, chronic pain affects about a fifth of adults worldwide, about 30%-45% of people with chronic pain suffer from severe depression.29.30 Clinical trials showed that the appearance of heat-sensitive phenomenon is highly related to the disease state. Under the pathological condition, the state of acupoint become sensitive, as the disease improving, the rate of heat-sensitive phenomenon could reduce by 15%.31 The relationship between sensitized acupoints and external intervention summarizes as “small stimuli with big responses”.23
There are some studies about HSM for pain diseases. Effect of multiple brain regions with significant change is basically consistent with the somatic pain temperature conduction path after HSM, and the somatosensory system activation may be the objective basis of meridian sensation transmission phenomenon.32 The network of multiple brain regions achieves the brain functional regulation on the intervention of HSM. It regulates the emotional part of the network central control through ACC-IC medial pain system.17
We conduct the study to explore the analgesic brain effect of the moxibustion at heat-sensitized Yao-yangguan (GV3) in patients with LDH and MPS by rfMRI. The technique of rfMRI based on changes in brain function during resting states, or spontaneous neural activity. It is uncomplicated to operate with high compliance for without repeated task stimulation. Considering the characteristics of noninvasive, high spatial and temporal resolution, it is widely used in many fields of neuroscience and psychology to clarify the brain functional connections.
We select various method to analyze the data and images. The mfALFF analysis is applicable to rfMRI, it could directly reflect the brain function changes and amplitude of BOLD oscillations on the resting state without the time interference.33 ReHo analysis can effectively reflect the homogeneity between different voxel time series in a functional area. The pain sensation regulated from peripheral (spinal cord), subcortical and cortical three levels.34 When people receiving the pain signals, they are transmitted by ascending projection fibers to the various centers and received multiple integration. On the process, the ACC and IC play great role. The IC receives signals from the thalamus and involves the regulation of sensorimotor, pain and emotion from multiple angles.35 It is known as the center of the endosensory system with closely connection of emotion expression. ACC mainly accepts the signals from the medial thalamus nucleus and involves in the processing and modulation of pain information.36 The metabotropic glutamate receptor 5 (mGluR5) in the PAG maintain an appropriate sensory perception in normal conditions. While in the neuropathic pain condition, the disrupted of persistent mGluR5 activity would result in chronic pain.37
There is great significant in chronic visceral pain and sensitivity of functional connectivity to PAG localization.38 So we choose HSM as a sensory stimulus and select S1-S2-IC-ACC-PAG seed as ROI to analyze functional connections. It can assess the strength of significant connections between functional brain regions and reflect the function of brain as network structure.
We hope our study could disclose key brain targets and central response characteristics of the analgesic brain effect and the brain functional connection of HSM. It would be helpful for the clinical application of HSM in pain relieving.
REFERENCES
- 1. Yu XC, Zhu B, Gao JH, et al. Scientific basis of dynamic process of acupoints. Zhong Yi Za Zhi 2007; 48: 971-73. [Google Scholar]
- 2. Zhu B. The sensitization phenomenon of acupoint and biological significances. Zhong Guo Zhen Jiu 2019; 39: 115-21. [DOI] [PubMed] [Google Scholar]
- 3. Henry H. On disturbances of sensation with especial reference to the pain of visceral disease. Brain 1893; 16: 1-133. [Google Scholar]
- 4. Xie DY. Professor Chen Rixin's views on moxibustion sensation. Zhong Guo Zhen Jiu 2016; 36: 789-92. [DOI] [PubMed] [Google Scholar]
- 5. Xu YH, Zhang ZX, Zhang XQ. Meta-analysis of therapeutic effect of heat-sensitive moxibustion on lumbar intervertebral disc herniation. Zhong Hua Zhong Yi Yao Xue Kan 2020; 38: 138-43+270. [Google Scholar]
- 6. Liu FS, Jin YL, Zhou FY, et al. Systematic review and Meta-analysis of heat-sensitive moxibustion for pain syndromes. Zhong Yi Lin Chuang Yan Jiu 2018; 10: 115-23. [Google Scholar]
- 7. Lai XS, Huang Y. A cerebral functional definition on the specificity of acupoints, needling sensation and association of acupoints based on the “acupoints-brain relation hypothesis”. Zhong Guo Zhen Jiu 2007; 10: 777-80. [PubMed] [Google Scholar]
- 8. Peyron R, Laurent B, García-Larrea L. Functional imaging of brain responses to pain: a review and Meta-analysis ( 2000). Neurophysiol Clin 2000; 30: 263-88. [DOI] [PubMed] [Google Scholar]
- 9. Dhond RP, Kettner N, Napadow V. Neuroimaging acupuncture effects in the human brain. J Altern Complement Med 2007; 13: 603-16. [DOI] [PubMed] [Google Scholar]
- 10. Mouraux A, Diukova A, Lee MC, Wise RG, Iannetti GD. A multisensory investigation of the functional significance of the "pain matrix". Neuroimage 2011; 54: 2237-49. [DOI] [PubMed] [Google Scholar]
- 11. Huang W, Pach D, Napadow V, et al. Characterizing acupuncture stimuli using brain imaging with FMRI--a systematic review and Meta-analysis of the literature. PLoS One 2012; 7: e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Caeyenberghs K, Pijnenburg M, Goossens N, Janssens L, Brumagne S. Associations between measures of structural morphometry and sensorimotor performance in individuals with nonspecific low back pain. AJNR Am J Neuroradiol 2017; 38: 183-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhao X, Xu M, Jorgenson K, Kong J. Neurochemical changes in patients with chronic low back pain detected by proton magnetic resonance spectroscopy: a systematic review. Neuroimage Clin 2016; 13: 33-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zare A, Jahanshahi A, Meriaux C, Steinbusch HW, . van Koeveringe GA. Glutamatergic cells in the periaqueductal gray matter mediate sensory inputs after bladder stimulation in freely moving rats. Int J Urol 2018; 25: 621-26. [DOI] [PubMed] [Google Scholar]
- 15. Glover GH. Overview of functional magnetic resonance imaging. Neurosurg Clin N Am 2011; 22: 133-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stewart JC, Dewanjee P, Shariff U, Cramer SC. Dorsal premotor activity and connectivity relate to action selection performance after stroke. Hum Brain Mapp 2016; 37: 1816-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xiong J. A fMRI study of heat-sensitized acupoint DuBi in the patients of knee osteoarthritis. Guangzhou: Guangzhou University of Chinese Medicine, 2014: 1-137. [Google Scholar]
- 18. Patrzck DW, Ronald M. Pain. Shenyang: Liaoning Education Press, 2000: 2. [Google Scholar]
- 19. Guidelines for clinical research on the treatment of lumbar intervertebral disc herniation with New Chinese medicine ( draft). . Zhong Guo Zhong Yi Gu Shang Ke 1995; 52-3. [Google Scholar]
- 20. Friston K. Ten ironic rules for non-statistical reviewers. Neuroimage 2012; 61: 1300-10. [DOI] [PubMed] [Google Scholar]
- 21. Oares JM, Magalhães R, Moreira PS, et al. A Hitchhiker's guide to functional magnetic resonance imaging. Front Neurosci 2016; 10: 515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pei XH, Qin Y Li ZQ, Tian YX, Zhao JX. Visual analysis of common acupoints for moxibustion in the treatment of lumbar disc herniation. Zhong Yi Yao Xian Dai Hua 2018; 20: 1860-66. [Google Scholar]
- 23. Chen RX, Chen MM, Kang MF. Heat-sensitive moxibustion practical reader. Beijing: People's Medical Publishing House, 2009; 50- 52. [Google Scholar]
- 24. Melzack R. The short-form McGill Pain Questionnaire. Pain 1987; 30: 191-7. [DOI] [PubMed] [Google Scholar]
- 25. Clinical Outcomes Committee of the Japanese Orthopaedic Asso-ciation, Subcommittee on Evaluation of Back Pain and Cervical Myelopathy; Subcommittee on Low Back Pain and Cervical Mye-lopathy Evaluation of the Clinical Outcome Committe of the Japa-nese Orthopaedic Association, Fukui M, et al. JOA back pain eval-uation questionnaire: initial report. J Orthop Sci 2007; 12: 443-50. [Google Scholar]
- 26. Pei LB, Xia JJ, Yan JL. Cross-cultural adaptation, reliability and validity of the Chinese version of the fear avoidance beliefs questionnaire. J Int Med Res 2010; 38: 1985-96. [DOI] [PubMed] [Google Scholar]
- 27. Song X, Dong Z, Long X, et al. REST: a toolkit for resting-state functional magnetic resonance imaging data processing. PLoS One 2011; 6: e25031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Classification of chronic pain. . Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the international association for the study of pain, subcommittee on taxonomy. Pain Suppl 1986; 3: S1-226. [PubMed] [Google Scholar]
- 29. Rice AS, Smith BH, Blyth FM. Pain and the global burden of disease. Pain 2016; 157: 791-6. [DOI] [PubMed] [Google Scholar]
- 30. Alschuler KN, Theisen-Goodvich ME, Haig AJ, Geisser ME. A comparison of the relationship between depression, perceived disability, and physical performance in persons with chronic pain. Eur J Pain 2008; 12: 757-64. [DOI] [PubMed] [Google Scholar]
- 31. Chen RX, Kang MF. Clinical application of acupoint thermal sensitivity. Zhong Guo Zhen Jiu 2007; 27: 199. [PubMed] [Google Scholar]
- 32. Xie HW. Heat-sensitive moxibustion therapy in DuBi acupoint with knee osteoarthritis patients functional brain imaging study. Chongqing: Chongqing Medical University, 2012: 1-46. [Google Scholar]
- 33. Hoptman MJ, Zuo XN, Butler PD, et al. Amplitude of low-frequency oscillations in schizophrenia: a resting state fMRI study. Schizophr Res 2010; 117: 13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bai L B, Qin W, Tian J, et al. Detection of dynamic brain networks modulated by acupuncture using a graph theory model. Progress in Natural Science 2009; 19: 827-35. [Google Scholar]
- 35. Mouraux A, Diukova A, Lee MC, Wise RG, Iannetti GD. A multisensory investigation of the functional significance of the "pain matrix". Neuroimage 2011; 54: 2237-49. [DOI] [PubMed] [Google Scholar]
- 36. Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther 2003; 8: 130-40. [DOI] [PubMed] [Google Scholar]
- 37. Chung G, Shim HG, Kim CY, et al. Persistent activity of metabotropic glutamate receptor 5 in the periaqueductal gray constrains emergence of chronic neuropathic pain. Curr Biol 2020; 30: 4631-42. [DOI] [PubMed] [Google Scholar]
- 38. Fenske SJ, Bierer D, Chelimsky G, et al. Sensitivity of functional connectivity to periaqueductal gray localization, with implications for identifying disease-related changes in chronic visceral pain: a MAPP research network neuroimaging study. Neuroimage Clin 2020; 28: 102443. [DOI] [PMC free article] [PubMed] [Google Scholar]


