Abstract
We Prevent is a virtual counseling intervention designed to improve communication as a mechanism for reducing HIV risk among young sexual minority men (SMM) in relationships. We evaluated the feasibility, acceptability, and preliminary efficacy of We Prevent in comparison to standard Counseling, Testing, and Referral among a national sample of 318 SMM ages 15–24 in a pilot randomized control trial. We found significant differences in condomless sex with outside partners; however, there were no differences in other sexual behaviors, sexual agreements, intimate partner violence (IPV), or communication between the conditions across the 9-month follow-ups. Stratified analyses found non-significant trends suggestive that We Prevent may reduce condomless sex for those ages 15–17 and for relationships over 1-year and may reduce IPV in relationships over 1-year. Though study retention was adequate, session attendance was low. Exit interviews participants reported benefits of We Prevent and provided insights into how to increase uptake.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-023-03994-5.
Keywords: Adolescents, HIV testing, Virtual counseling, Pilot randomized controlled trial
Introduction
In the United States (US), young sexual minority men (SMM) ages 13–24 account for a disproportionate number of new HIV infections [1]. Modeling studies have estimated that one- to two-thirds of new HIV infections among SMM occur in the context of a primary partnership, and this may be as high as 84% of all new infections among young SMM [2, 3]. As a result, there have been many promising digital health interventions developed to focus on addressing the HIV prevention needs of young SMM [4–9], including younger SMM ages 14–17 [10]. Simultaneously, the understanding of the role of primary partnerships in shaping HIV transmission risk precipitated a growth in dyadic interventions, recognizing that HIV transmission often occurs in the context of a relationship, and therefore the characteristics of relationships may be important drivers of HIV risk for male couples [11–17]. Many of the existing couples-based interventions have adapted or integrated Couples HIV testing and counseling (CHTC) (in which couples receive HIV testing and counseling together, and build a prevention plan based on their joint sero-status) with relationship education or counseling [11–14] and most of these studies have investigated the efficacy of dyadic interventions for adult male couples [11, 12, 15–17]. CHTC and other interventions that address relationship dynamics through communication skills building have shown promise in reducing HIV transmission risk behaviors among young male couples 18–29 years of age, who may have more specific needs related to their personal and identity development stages [13, 14].
Despite mounting evidence that dyadic approaches are generally efficacious in promoting safer sex behaviors and engagement in HIV prevention in adult populations of male couples [18–20], few dyadic HIV prevention interventions exist for young SMM in relationships [21]. Existing digital health interventions focused on HIV prevention with young SMM have not had a specific focus on relationship dynamics such as communication skills with young SMM relationships [4–10]. To address the intervention gap for partnered SMM in relationships, and based on the recent promise of couples-based interventions for young male couples 18–29 years of age [13, 14], we developed We Prevent, a couples-based intervention which combined CHTC with relationship education delivered virtually in a single session for younger SMM (ages 15–19) in relationships [22]. The original intent was to deliver the intervention to young male couples together, so that the couple would receive CHTC and relationship education at the same time—similar to the CDC-endorsed CHTC service [12]. However, in qualitative formative research, younger SMM consistently reported not yet having the skills or confidence necessary to engage in HIV testing with their partner, and difficulties arose with the logistics of coordinating attendance at the sessions for both partners [23]. Young SMM reported a strong preference for an individual intervention, in which they could learn the salient information and skills, and subsequently use them in their relationships, rather than having to learn them with their partner present [23]. This also allowed a forum for them to ask questions without their partner present. Based on these formative findings, and through iterative conversations with the investigators of the Adolescent Medicine Trials Network for HIV and AIDS Interventions (ATN), We Prevent was subsequently redesigned to provide the option for young SMM to participate in the intervention on their own or with their partner. As such, the We Prevent intervention included the option of CHTC with relationship skills-building content (dyadic) or standard Counseling, Testing, and Referral (CTR) along with relationship skills-building content (individual). For both options, relationship skills-building content included communication strategies and sexual boundary setting. Prior to launching the pilot randomized control trial (RCT), the eligibility criteria was expanded to be inclusive of young transgender men who were in partnerships with cisgender men—to recognize the risk of HIV transmission in this group—and expanded the age to 15–24 to mirror other ATN projects and facilitate cross-study data analyses [24, 25].
This paper describes subsequent adaptions taken to design We Prevent to meet the unique developmental needs of younger SMM and to determine the feasibility, acceptability, and preliminary efficacy of We Prevent compared to standard CTR in a pilot randomized controlled trial. We hypothesized that younger SMM who participate in We Prevent would demonstrate greater reductions in sexual risk of HIV transmission (e.g., condomless sex) and increases in sexual agreement formation, PrEP use, and relationship communication skills than those in the control condition. Additionally, we hypothesized that younger SMM who participated in We Prevent might report reductions in intimate partner violence (IPV) compared to those in the control condition, because of intervention content specifically focused on boundary-setting in intimate relationships.
Methods
Study Design and Randomization
We used a parallel RCT design in which participants were randomized on a 1:1 ratio to either the intervention arm (We Prevent—which they had the option of receiving the intervention individually or dyadically) or the control arm (CTR—individual HIV counseling and testing). We randomized participants individually using a simple random allocation generator and did not stratify based on any demographic or behavioral factors. Participants were randomized after they completed a baseline survey. To avoid contamination, separate study counselors facilitated the intervention and control arms. No masking was conducted in this study.
Participant Eligibility and Recruitment
Participants were young SMM in relationships recruited nationally. Individuals were eligible to participate if they: (1) were between the ages of 15 and 24; (2) identified as a cisgender or transgender man with the intention to have sex with a cisgender man; (3) identified as being in an emotional and/or sexual relationship with a cisgender male; (4) self-reported engaging in any sex (oral, anal, or vaginal) in their lifetime; (5) met the age of sexual consent in their state of residence; (6) had access to a personal device with internet access in a safe and confidential location; (7) self-reported an HIV-negative or unknown serostatus; and (8) were able to speak and read English.
Enrollment for the pilot trial began in December 2019 and ended in September 2020. Participants were recruited through geo-social network applications (i.e., Facebook, Instagram, and Jack’d) and referrals from the Annual American Men’s Internet Survey (AMIS) [26]. Participants who clicked on the advertisement or were referred from AMIS were directed to the study webpage that provided basic information with a study screener and consent form. A study staff member then verified their responses (e.g., IP addresses, potential duplicates, age of sexual consent laws). Those who were interested, screened eligible, gave informed consent, and were verified to be eligible by a staff member were then directed to the Study Management and Retention Toolkit (SMART) registration page where they entered their contact information and received instructions on how to download the study-specific SMART app where all study activities occur (e.g., schedule session, complete surveys).
Following a baseline survey and randomization, participants in the control condition were sent a message inviting them to schedule their session with their counselor. Those who scheduled their control condition session were then mailed an at-home HIV self-testing kit. The procedures were similar for those randomized to the We Prevent intervention condition; however, participants in the intervention condition were first sent a sent a short survey to indicate whether they wanted to participate individually or with their partner. Participants who elected to complete the study with the partner were asked to provide their partners contact information. The partner was consented for the study and completed a brief survey prior to their intervention session. They then received the same messaging about scheduling their intervention condition session and mailed an at-home HIV self-testing kit if they scheduled their session. Both intervention and control condition sessions were both delivered via a HIPAA-compliant Zoom platform. To evaluate the intervention, individuals completed self-report follow-up surveys at 3-, 6-, and 9-months post-randomization. At baseline and 6-months participants were offered the option to complete at-home STI testing kits that screened for chlamydia, gonorrhea, and syphilis. We invited a subsample of participants to participate in a semi-structured interview to examine their experiences with the trial after completing their final follow-up survey. Specifically, we purposefully sampled participants who did all the study activities, those who did not complete their session but did their follow-up surveys, and a subset of participants who did not complete their session or their follow-up surveys. Participants were compensated $40 for completing each survey ($160 total). Those who completed all follow-up surveys were provided with an additional $40 as an incentive for completing all follow-up assessments, and those who completed the exit interview received $20. All study procedures were approved by the University of North Carolina at Chapel Hill institutional review board (IRB# 18-0200) with a waiver of parental permission for participants under 18 years of age.
Intervention Description
The primary goal of We Prevent was to increase young men’s communication related to HIV risk reduction in their current and future relationships. Most content was designed through an iterative process that included obtaining feedback from young SMM and experts to ensure cultural relevance and developmental sensitivity. In addition to the formative research previously described and input from the ATN youth advisory board [23, 24], we conducted a pre-test of the intervention condition in which we aimed to recruit 20 younger SMM couples to participate in sessions together. However, there were challenges recruiting and engaging couples in the dyadic-level intervention such that none of the pre-test participants engaged in the session; therefore, in this pilot RCT study, participants who were randomized to the We Prevent intervention had the option to complete the session with their partner or individually.
We Prevent and the control condition both consisted of a single face-to-face session with a counselor delivered via Zoom that lasted approximately 45 min (approximately the same time in each arm). For both conditions, the session included basic elements of standard CTR (or CHTC depending on choice of individual or dyadic delivery in the We Prevent condition): assessing risk, discussing HIV and STI prevention methods, and explaining OraQuick home HIV test results. In the We Prevent condition, the counselor engaged the participant in a discussion of general relationship communication strategies and specific communication strategies regarding sex, sexual health, and sexual agreements while waiting for the HIV test results. The We Prevent condition included two additional communication-related components focused on understanding the strengths and challenges of their current relationship and how to apply communication strategies to their current and future relationships. Details about the We Prevent intervention content has been published previously [22].
In the event of a preliminary HIV-positive test result, the protocol included counseling on linkage to care. Specifically, the counselor would arrange a time within 1 week of the session to conduct a follow-up session. During this follow-up session, those who had a preliminary positive test result would be directly linked to medical care in their local area. Study staff were instructed to follow up with the participant on the next business day to ensure they contacted a local healthcare provider. The participant would be contacted at least three times to (1) confirm an appointment was scheduled, (2) confirm the appointment was attended, and (3) report confirmatory results.
To minimize contamination bias, one counselor conducted all intervention condition sessions (MR), and a different counselor conducted all control condition sessions (CW). Both counselors identified as sexual and/or gender minority young adults and were certified in CTR and received ongoing clinical supervision (LD). The intervention counselor received additional training, including motivational interviewing techniques and a 2-day training in Couples HIV testing and counseling.
Measures
Study feasibility Measures included the percentage of individuals who completed the screener, were eligible, completed the baseline, and were retained for the follow-up assessments.
Sociodemographic characteristics Participants self-reported their age, race, ethnicity, geographic region, gender identity, sexual identity, whether they were food insecure in the past 3 months, and whether they experienced unstable housing in the past month. Due to small numbers of people of color, race/ethnicity was categorized white/non-Hispanic, Black/non-Hispanic, Latino(x)/Hispanic, and Multiracial/other (which included Asian, Native American/Alaskan Native, Native Hawaiian/other Pacific Islander, and other). Most participants identified as cisgender gay men; therefore, we recoded gender identity into dichotomous variable (cisgender man or transgender man/nonbinary). Similarly, we recoded sexual identity as those who only selected gay, bisexual, or other (which included queer, asexual, pansexual, and other sexual identities).
Current relationship characteristics Participants reported their relationship length (i.e., 3 months or less, 4–11 months, 1 year or more). Participants were asked about the presence and type of sexual agreements with the current partner. Specifically, presence of agreement was asked with one item: “Do you and your partner currently have an agreement about whether or not you can have sex with people besides each other?” with response options: “Yes,” “No,” or “I don’t know.” Type of sexual agreement was assessed with one item: “Of the following which do you think best describes your relationship with your partner?” with response options: “Both of us cannot have any sex with outside partners,” We can have sex with outside partners, without any conditions or restrictions,” “We can have sex with outside partners, but with some conditions or restrictions,” or “I don’t know.” Participants were classified as being in monogamous agreement if they reported that they had an agreement and indicated that “Both of us cannot have any sex with outside partners.” Participants were classified as being in an open agreement if they reported they had an agreement and indicated “We can have sex with outside partners, without any conditions or restrictions,” or We can have sex with outside partners, but with some conditions or restrictions.”
Efficacy Outcomes
HIV transmission risk behaviors Participants were asked a series of questions about their sexual behaviors in the past 90 days at baseline, 3-, 6- and 9-month follow ups. Specifically, participants reported the number of times that they had engaged in different sexual behaviors with or without a condom (e.g., anal insertive, anal receptive) with their main partner or any outside partners as well as their partners’ HIV status. Participants who reported that they were aware of PrEP self-reported whether they were currently on PrEP (Yes/No). Five dichotomous variables were created: (1) any condomless anal or vaginal sex with any partner (Yes/No) (2) any condomless anal or vaginal sex with a main partner, (3) any condomless anal or vaginal sex with an outside partner, (4) any condomless anal or vaginal sex with a main partner while not on PrEP, (5) any condomless anal or vaginal sex while not on PrEP with a sero-different or unknown status partner (Yes/No).
Sexual agreement formation Participants were asked to self-report whether they had a sexual agreement with their partner at the baseline, 3-, 6-, and 9-month follow-up assessments (i.e., Do you and your current boyfriend/partner currently have an agreement about whether or not you can have sex with people besides each other?). We coded whether a participant reported having any sexual agreement (Yes/No) and if they formed a sexual agreement if they started a new relationship during the follow-up period (Yes/No).
HIV-related communication Participants who reported being in a relationship at each study visit completed the 9-item Couples Efficacy to Reduce HIV Threat scale in which participants rated the extent to which they perceived that they could communicate with their partner about different HIV prevention strategies (e.g., “using condoms when we have sex with each other,” “limiting the number of other sex partners,” “talking/communicating about PrEP”) [27]. Participants responded to each item on 5-point Likert scale ranging from (1) strongly disagree to (5) strongly agree. The items were mean centered such that higher scores indicate that participants perceive that they can effectively communicate with their partner about HIV prevention strategies (sample α = 0.84).
Intimate partner violence (IPV) Participants who reported being in a relationship at each study visit were asked about IPV at any time in their current partnership using the abbreviated IPV-GBM Scale, adapted from the Conflict Tactics Scale, to assess IPV victimization among SMM [28]. Experiences of IPV were measured with a 6-item scale that included items of physical, emotional, monitoring/controlling, and sexual IPV (example item: Have arguments in your relationship with [Name of current boyfriend/partner] escalated into any of the following: destruction of property, grabbing, restraining, pushing, kicking, slapping, punching, threats of violence or other acts of physical intimidation?). Response options included “yes,” “no,” or “don’t know.” Each item was summed and then dichotomized to indicate whether participants reported experiencing any form of IPV. If participants endorsed IPV in any of the surveys, they were shown information on national level resources they could contact for further information or assistance.
Intervention acceptability Satisfaction with the counseling session was assessed at the 3-month follow-up visit with the following items: “Overall, I am very satisfied with We Prevent” and “I would recommend We Prevent to my friends.” Each item was rated on a 7-point Likert scale ranging from (1) strongly disagree to (7) strongly agree. We recoded these two items to compare those who endorsed strongly agree or agree with those who did not.
A subset of 16 participants who were randomized to the We Prevent condition were invited to complete an exit interview via Zoom after their 9-month follow-up survey window closed. We purposefully sampled participants who did and did not complete the We Prevent intervention or other study activities. Participants were asked their impression of each of the study components, including what they liked, disliked, and areas for improvement. The interview was completed by a member of the team who did not facilitate the We Prevent intervention sessions. All interviews were audio-recorded and transcribed verbatim.
Analysis Plan
Primary statistical analyses Baseline data are described overall and by study arm using counts and percentages for categorical data and medians and interquartile ranges (IQRs) for continuous data. We also examined differences in HIV communication by study arm using the lowest quintile at baseline to see if the We Prevent intervention may have had an impact among those with lower HIV communication scores. Given the potential for randomization failures, we decided a priori to present both unadjusted and confounder-adjusted results. In addition to the measures described, we also report the percentage of participants enrolled prior to and during the onset of the COVID-19 pandemic (April 2020).
Outcome data are presented by study arm in an intent-to-treat (ITT) analysis for study visits 3-, 6-, and 9-months. The ITT analysis examines the primary outcomes for all participants as randomized. Dichotomous outcomes are presented using counts and percentages, with Chi-square or Fisher’s Exact tests to evaluate statistical differences by study arm. The HIV communication scale was assessed for normality and is presented by study arm using median IQRs and the lowest quintile as the scale was not normally distributed. Wilcoxon Two-Sample Tests of medians were used to evaluate statistical differences by study arm.
This pilot RCT was designed to assess the feasibility, acceptability, and preliminary efficacy of the We Prevent intervention. Given the large percentage of participants who did not take part in the intervention, the per-protocol (PP) analysis considers primary outcomes for only those who took part in the intervention versus control arm activities. Conducting both ITT and PP analyses allows us to assess the We Prevent intervention’s impact on outcomes (ITT) and whether this impact was consistent across specific groups of participants (PP), information which is vital for the future tailoring of the intervention.
Post-hoc sub-group analyses To understand whether the We Prevent intervention had differential efficacy for participants from certain demographic groups, we explored differences in outcomes by study arm within subgroups for: age (15–17 vs. ≥ 18 years), gender (transgender man/nonbinary vs. cisgender male), and relationship length (< 1 year vs. ≥ 1 year). These analyses employed the same methods as the primary statistical analyses.
Intervention acceptability analyses We calculated frequencies and percentages of intervention satisfaction items for those who were randomized to the We Prevent intervention.
All qualitative exit interviews were transcribed verbatim, double-checked for accuracy, and de-identified. We used an established rapid deductive-inductive qualitative analytic approach designed for intervention development and evaluation [29, 30]. First, a template was developed deductively from the topics in the interview guide. The member of research team (CW) who conducted the interviews used the template and generated summaries for each participant. The first author (KG) then independently read all the transcripts using the template and both team members then made refinements to the template to establish consistency of summaries. Next, KG compiled the summaries into matrices by the three groups (i.e., those who did everything, those who did not do the session but completed all the follow-up surveys, and those who did not do their session or any follow-up surveys). Themes among those who did not complete the session but did their follow-up surveys and those who did not complete the session or do their follow-up surveys were found to be consistent. The findings were then summarized and organized by themes by each group with exemplary quotes.
Results
Study Feasibility
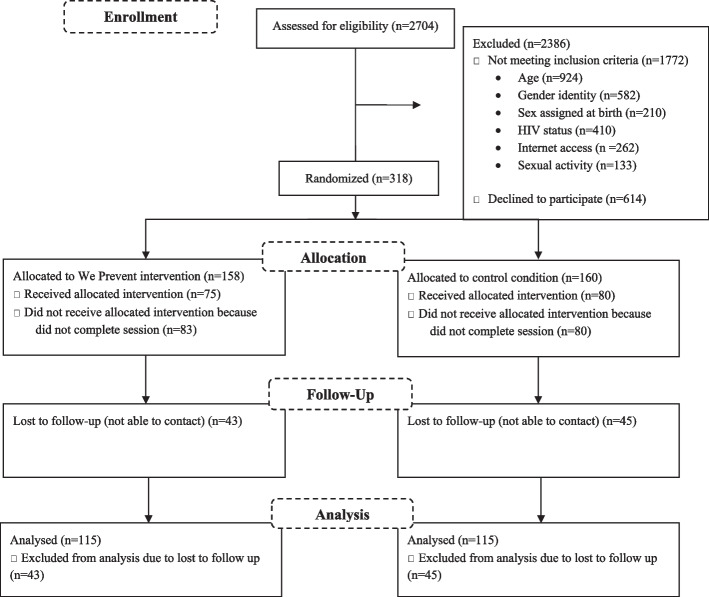
A total of 2704 potential participants completed the eligibility screener over a 10-month recruitment period, and 932 (34%) of these met initial eligibility criteria (Fig. 1). Of those, 321 (12%) completed the baseline survey. Three participants were excluded due to not meeting eligibility criteria due to gender identity. The final analytic sample was 318 participants, 158 of which were randomized to the intervention arm and 160 to the control arm. Approximately one-quarter of the sample opted to complete the at-home STI testing at baseline (n = 77) and 12.6% completed the at-home STI testing at 6-month follow-up (n = 40). Three participants tested positive for chlamydia and 4 for gonorrhea. Study staff members followed up with participants to share the STI results and provided them with referrals for treatment in their geographical locale. None of the participants who completed an HIV self-test during their session had a positive test result. Overall retention was 75.8% at 3-months, 72.3% at 6-months, and 72.6% at 9-months.
Fig. 1.
Flow chart
Participant Characteristics
Participants ranged in age from 15 to 24 (median = 21.0, IQR = 3.0) with 13.8% between the ages of 15 and 17 (n = 44), 33.0% between the ages of 18 and 20 (n = 105), and 53.1% between the ages of 21 and 24 (n = 169). As shown in Table 1, 42% identified as person of color, and most identified as cisgender male (75%) and gay (72%). Participants varied in terms of relationship length: 30% had been in the relationship for less than 3 months, 27% for 4–11 months, and 43% for 1 year or more. Most participants remained with their baseline main partner through the study period (82% at 3 months, 77% at 6 months, and 71% at 9 months). Baseline characteristics, including whether participant enrolled prior to or after the beginning of the COVID-19 pandemic, were balanced by study arm.
Table 1.
Distribution of baseline variables by study arm (N = 318)
| Total (N = 318) | Intervention (N = 158) | Control (N = 160) | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Sociodemographic characteristics | ||||||
| Age (median, IQR) | 21.0 | 3.0 | 21.0 | 4.0 | 21.0 | 3.0 |
| Race/ethnicity | ||||||
| Black, non-Hispanic | 24 | 8% | 13 | 8% | 11 | 7% |
| Latino/x or Hispanic | 50 | 16% | 23 | 15% | 27 | 17% |
| Multiracial/other | 60 | 19% | 27 | 17% | 33 | 21% |
| White, non-Hispanic | 184 | 58% | 95 | 60% | 89 | 56% |
| Gender identity | ||||||
| Cisgender male | 237 | 75% | 112 | 71% | 125 | 78% |
| Trans man/nonbinary | 81 | 25% | 46 | 29% | 35 | 22% |
| Sexual identity | ||||||
| Bisexual | 57 | 18% | 31 | 20% | 26 | 16% |
| Gay | 229 | 72% | 111 | 70% | 118 | 74% |
| Other sexual identity | 32 | 10% | 16 | 10% | 16 | 10% |
| Food insecure, past 3 months | ||||||
| No | 228 | 72% | 112 | 71% | 116 | 73% |
| Yes | 90 | 28% | 46 | 29% | 44 | 28% |
| Unstable housing, past month | ||||||
| No | 295 | 93% | 144 | 91% | 151 | 94% |
| Yes | 23 | 7% | 14 | 9% | 9 | 6% |
| Geographic region | ||||||
| South | 120 | 38% | 64 | 41% | 56 | 35% |
| West | 64 | 20% | 33 | 21% | 31 | 19% |
| Midwest | 72 | 23% | 39 | 25% | 33 | 21% |
| Northeast | 60 | 19% | 21 | 13% | 39 | 24% |
| Pacific | 2 | 1% | 1 | 1% | 1 | 1% |
| Current relationship characteristics | ||||||
| Relationship length | ||||||
| 3 months or less | 95 | 30% | 44 | 28% | 51 | 32% |
| 4–11 months | 85 | 27% | 44 | 28% | 41 | 26% |
| 1 year or more | 134 | 43% | 68 | 44% | 66 | 42% |
| Sexual agreement | ||||||
| No | 87 | 27% | 36 | 23% | 51 | 32% |
| Yes | 206 | 65% | 109 | 69% | 97 | 61% |
| Decline to answer | 25 | 8% | 13 | 8% | 12 | 8% |
| Type of sexual agreement | ||||||
| Monogamous | 169 | 54% | 77 | 49% | 92 | 59% |
| Open | 110 | 35% | 60 | 38% | 50 | 32% |
| Don’t know | 35 | 11% | 20 | 13% | 15 | 10% |
| IPV with main partner | ||||||
| No | 254 | 80% | 124 | 78% | 130 | 81% |
| Yes | 64 | 20% | 34 | 22% | 30 | 19% |
| HIV transmission risk, past 3 months | ||||||
| Ever had condomless sex with primary partner | ||||||
| No | 66 | 21% | 35 | 22% | 31 | 20% |
| Yes | 247 | 79% | 121 | 78% | 126 | 80% |
| Refuse to answer | 5 | 1% | ||||
| Condomless anal or vaginal sex with any partner | ||||||
| No | 100 | 31% | 52 | 33% | 48 | 30% |
| Yes | 218 | 69% | 106 | 67% | 112 | 70% |
| Condomless anal or vaginal sex with main partner | ||||||
| No | 122 | 38% | 60 | 38% | 62 | 39% |
| Yes | 196 | 62% | 98 | 62% | 98 | 61% |
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 266 | 84% | 137 | 87% | 129 | 81% |
| Yes | 52 | 16% | 21 | 13% | 31 | 19% |
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 139 | 44% | 65 | 41% | 74 | 46% |
| Yes | 178 | 56% | 92 | 59% | 86 | 54% |
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 306 | 98% | 155 | 99% | 151 | 96% |
| Yes | 7 | 2% | 1 | 1% | 6 | 4% |
| Currently on PrEP | ||||||
| No | 4 | 16% | 1 | 13% | 3 | 18% |
| Yes | 21 | 84% | 7 | 88% | 14 | 82% |
| Ever had an HIV test | ||||||
| No | 106 | 33% | 51 | 32% | 55 | 34% |
| Yes | 212 | 67% | 107 | 68% | 105 | 66% |
| Frequency of HIV testing | ||||||
| Never | 106 | 33% | 51 | 32% | 55 | 34% |
| Every 3 months | 46 | 15% | 25 | 16% | 21 | 13% |
| Every 6 months | 40 | 13% | 20 | 13% | 20 | 13% |
| Every year | 29 | 9% | 14 | 9% | 15 | 9% |
| Every time there is a potential exposure | 35 | 9.1% | 20 | 11% | 15 | 9% |
| Don’t test regularly | 61 | 19% | 27 | 19% | 34 | 21% |
| Prior HIV self-test experience | 103 | 32% | 50 | 32% | 53 | 33% |
| HIV communication (score 1–5; median, IQR) | 4.5 | 1.0 | 4.4 | 0.9 | 4.5 | 1.1 |
| Enrollment During COVID-19 | ||||||
| Prior to COVID-19 (December 2019–March 2020) | 146 | 46% | 74 | 47% | 72 | 45% |
| During COVID-19 (April 2020–September 2021) | 172 | 54% | 84 | 53% | 88 | 55% |
Intervention Preliminary Efficacy
Table 2 presents ITT analyses among the full sample and those who were in each relationship at each follow-up period. There was a significant difference between the intervention and control condition at 9-months among the full sample in reductions in condomless anal or vaginal sex with an outside partner ( =5.06; p = 0.025), as well as among those who stayed in a relationship ( = 4.28; p = 0.039). Condomless anal or vaginal sex with any outside partner decreased significantly in the intervention arm from 10% at 3 months to 3% at 9 months ( = 3.25; p = 0.0477). There were no other statistically significant differences in other sexual behavior, sexual agreements, PrEP use, IPV, or HIV communication by study arm at any of the follow-up time points. The PP analyses among the full sample and those who were in a relationship at each follow-up period are presented in Supplementary Table 1. Although there were no statistically significant differences in the PP analyses, there were meaningful differences in reductions in condomless anal or vaginal sex with outside partners among the full sample at 9-months ( = 2.92; p = 0.088).
Table 2.
Outcomes over time: intention-to-treat (ITT) analysis
| Among participants regardless of relationship status | ||||||
|---|---|---|---|---|---|---|
| Among participants regardless of relationship status | ||||||
| 3 months (N = 241) | ||||||
| Intervention (n = 120) | Control (n = 121) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex with any partner | ||||||
| No | 64 | 53% | 61 | 50% | 0.2058 | 0.65 |
| Yes | 56 | 47% | 60 | 50% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 66 | 55% | 66 | 55% | 0.0050 | 0.944 |
| Yes | 54 | 45% | 55 | 45% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 108 | 90% | 109 | 90% | 0.0005 | 0.983 |
| Yes | 12 | 10% | 12 | 10% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 58 | 53% | 60 | 54% | 0.0029 | 0.957 |
| Yes | 51 | 47% | 52 | 46% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 106 | 98% | 112 | 99% | 0.6149 | |
| Yes | 2 | 2% | 1 | 1% | ||
| Current PrEP use | ||||||
| No | 2 | 25% | 3 | 33% | 1 | |
| Yes | 6 | 75% | 6 | 67% | ||
| Sexual agreement | ||||||
| No/don’t know | 19 | 35% | 15 | 28% | 0.5346 | |
| Yes | 35 | 65% | 39 | 72% | ||
| Sexual agreement formation* | ||||||
| No | 9 | 64% | 10 | 38% | 0.1856 | |
| Yes | 5 | 36% | 16 | 62% | ||
| Among participants regardless of relationship status | ||||||
|---|---|---|---|---|---|---|
| Among participants regardless of relationship status | ||||||
| 6 months (N = 230) | ||||||
| Intervention (n = 116) | Control (n = 114) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex with any partner | ||||||
| No | 69 | 59% | 60 | 53% | 1.0957 | 0.295 |
| Yes | 47 | 41% | 54 | 47% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 72 | 62% | 67 | 59% | 0.2614 | 0.6092 |
| Yes | 44 | 38% | 47 | 41% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 108 | 93% | 102 | 89% | 0.9541 | 0.329 |
| Yes | 8 | 7% | 12 | 11% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 63 | 60% | 64 | 59% | 0.0121 | 0.912 |
| Yes | 42 | 40% | 44 | 41% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 105 | 100% | 106 | 98% | 0.498 | |
| Yes | 0 | 0% | 2 | 2% | ||
| Current PrEP use | ||||||
| No | 1 | 14% | 1 | 10% | 1 | |
| Yes | 6 | 86% | 9 | 90% | ||
| Sexual agreement | ||||||
| No/don’t know | 10 | 45% | 5 | 25% | 0.2087 | |
| Yes | 12 | 55% | 15 | 75% | ||
| Sexual agreement formation* | ||||||
| No | 8 | 57% | 9 | 47% | 0.7283 | |
| Yes | 6 | 43% | 10 | 53% | ||
| Among participants regardless of relationship status | ||||||
|---|---|---|---|---|---|---|
| Among participants regardless of relationship status | ||||||
| 9 months (N = 231) | ||||||
| Intervention (n = 115) | Control (n = 116) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex with any partner | ||||||
| No | 74 | 64% | 64 | 55% | 0.0202 | 0.155 |
| Yes | 41 | 36% | 52 | 45% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 76 | 66% | 69 | 59% | 1.0778 | 0.299 |
| Yes | 39 | 34% | 47 | 41% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 111 | 97% | 103 | 89% | 5.0595 | 0.025 |
| Yes | 4 | 3% | 13 | 11% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 64 | 63% | 65 | 61% | 0.0922 | 0.761 |
| Yes | 37 | 37% | 41 | 39% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 101 | 99% | 107 | 100% | 0.488 | |
| Yes | 1 | 1% | 0 | 0% | ||
| Current PrEP use | ||||||
| No | 1 | 9% | 0 | 0% | 0.44 | |
| Yes | 10 | 91% | 14 | 100% | ||
| Sexual agreement | ||||||
| No/don’t know | 5 | 19% | 6 | 24% | 0.7396 | |
| Yes | 22 | 81% | 19 | 76% | ||
| Sexual agreement formation* | ||||||
| No | 3 | 30% | 7 | 32% | > 0.999 | |
| Yes | 7 | 70% | 15 | 68% | ||
| Among participants who stayed in a relationship | ||||||
|---|---|---|---|---|---|---|
| 3 months (N = 198) | ||||||
| Intervention (n = 97) | Control (n = 101) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex, any partner | ||||||
| No | 41 | 42% | 41 | 41% | 0.0571 | 0.811 |
| Yes | 56 | 58% | 60 | 59% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 43 | 44% | 46 | 46% | 0.0295 | 0.864 |
| Yes | 54 | 56% | 55 | 54% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 85 | 88% | 89 | 88% | 0.0112 | 0.916 |
| Yes | 12 | 12% | 12 | 12% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 44 | 46% | 48 | 48% | 0.0555 | 0.814 |
| Yes | 51 | 54% | 52 | 52% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 92 | 98% | 100 | 99% | 0.61 | |
| Yes | 2 | 2% | 1 | 1% | ||
| Current PrEP use | ||||||
| No | 1 | 25% | 2 | 33% | 1 | |
| Yes | 3 | 75% | 4 | 67% | ||
| IPV | ||||||
| No | 77 | 82% | 87 | 86% | 0.6496 | 0.42 |
| Yes | 17 | 18% | 14 | 14% | ||
| Among participants who stayed in a relationship | ||||||
|---|---|---|---|---|---|---|
| 6 months (N = 177) | ||||||
| Intervention (n = 89) | Control (n = 88) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex, any partner | ||||||
| No | 42 | 47% | 34 | 39% | 1.3216 | 0.25 |
| Yes | 47 | 53% | 54 | 61% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 45 | 51% | 41 | 47% | 0.2793 | 0.597 |
| Yes | 44 | 49% | 47 | 53% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 81 | 91% | 76 | 86% | 0.9536 | 0.329 |
| Yes | 8 | 9% | 12 | 14% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 46 | 52% | 44 | 50% | 0.091 | 0.763 |
| Yes | 42 | 48% | 44 | 50% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 88 | 100% | 86 | 98% | 0.497 | |
| Yes | 0 | 0% | 2 | 2% | ||
| Current PrEP use | ||||||
| No | 1 | 25% | 1 | 17% | 1 | |
| Yes | 3 | 75% | 5 | 83% | ||
| IPV | ||||||
| No | 76 | 86% | 79 | 91% | 0.8524 | 0.356 |
| Yes | 12 | 14% | 8 | 9% | ||
| Among participants who stayed in a relationship | ||||||
|---|---|---|---|---|---|---|
| 9 months (N = 163) | ||||||
| Intervention (n = 77) | Control (n = 86) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex, any partner | ||||||
| No | 36 | 47% | 34 | 40% | 0.8639 | 0.353 |
| Yes | 41 | 53% | 52 | 60% | ||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 38 | 49% | 39 | 45% | 0.2610 | 0.609 |
| Yes | 39 | 51% | 47 | 55% | ||
| Condomless anal or vaginal sex with any outside partner | ||||||
| No | 73 | 95% | 73 | 85% | 4.2808 | 0.039 |
| Yes | 4 | 5% | 13 | 15% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 38 | 51% | 42 | 51% | 0.0001 | 0.994 |
| Yes | 37 | 49% | 41 | 49% | ||
| Condomless anal or vaginal sex with any outside partner of sero-different or unknown status, no PrEP | ||||||
| No | 75 | 99% | 84 | 100% | 0.475 | |
| Yes | 1 | 1% | 0 | 0% | ||
| Current PrEP use | ||||||
| No | 1 | 20% | 0 | 0% | 0.357 | |
| Yes | 4 | 80% | 9 | 100% | ||
| IPV | ||||||
| No | 67 | 89% | 71 | 85% | 0.7995 | 0.371 |
| Yes | 8 | 11% | 13 | 15% | ||
| Z test statistic | ||||||
|---|---|---|---|---|---|---|
| HIV communication (score 1–5, median, IQR) | 4.6 | 1 | 4.6 | 0.9 | − 0.086 | 0.932 |
| Change in HIV communication score vs baseline score among those in lowest quintile (≤ 4.0) at baseline | 0 | 1 | 0.5 | 0.9 | 3.1805 | 0.0745 |
| Z test statistic | ||||||
|---|---|---|---|---|---|---|
| HIV communication (score 1–5, median, IQR) | 4.9 | 0.9 | 4.5 | 0.8 | − 1.348 | 0.179 |
| Change in HIV communication score vs baseline score among those in lowest quintile (≤ 4.0) at baseline | 0.4 | 1.1 | 0.5 | 0.9 | 0.2629 | 0.6081 |
| Z test statistic | ||||||
|---|---|---|---|---|---|---|
| HIV communication (score 1–5, median, IQR) | 5 | 0.6 | 4.8 | 0.8 | 0.9775 | 0.33 |
| Change in HIV communication score vs baseline score among those in lowest quintile (≤ 4.0) at baseline | 0.4 | 1.2 | 0.5 | 0.8 | 0.4179 | 0.8252 |
Note: *‘No’ or ‘decline to answer’ to having a relationship agreement at baseline; Kruskal–Wallis tests were used for continuous variable, Chi-square testes were used for categorical variables; and Fisher’s exact tests do not produce test statistics.
There were not statistically significant results; however, there were meaningful differences between groups in the post-hoc sub-group analyses (see Table 3). In ITT analyses, participants ages 15–17 reported lower levels condomless sex with their main partner in the intervention condition (6% versus 36% in the control condition) at 3-months (p = 0.05) and reported lower levels of condomless sex with their main partner without PrEP in the intervention condition (7% versus 38% in the control condition) at 3-month follow-up (p = 0.08). Participants in relationships of at least 1 year were less likely to report IPV in the intervention condition (5% versus 21% in the control condition) at 9-month follow-up ( = 4.02; p = 0.04). In PP analyses, participants in relationships for at least 1 year were less likely to report condomless sex with their main partner in the intervention (39% versus 67% in the control condition at 6-months ( =4.36; p = 0.04) and less likely to report condomless sex with their main partner without PrEP in the intervention condition (44% versus 69% in the control condition) at 6-month follow-up ( = 3.42; p = 0.06).
Table 3.
Post-hoc sub-group analysis results
| Intention-to-treat analysis | ||||||
|---|---|---|---|---|---|---|
| STRATA: AGE 15–17 (all participants regardless of relationship status | 3 months | |||||
| Intervention (n = 17) | Control (n = 14) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 16 | 94% | 9 | 64% | 0.05438 | |
| Yes | 1 | 6% | 5 | 36% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 13 | 93% | 8 | 62% | 0.0768 | |
| Yes | 1 | 7% | 5 | 38% | ||
| STRATA: ≥ 1 year relationship length (participants with a partner) | 9 months | |||||
|---|---|---|---|---|---|---|
| Intervention (n = 37) | Control (n = 43) | p value | ||||
| N | % | N | % | |||
| IPV | ||||||
| No | 35 | 95% | 34 | 79% | 4.042 | 0.0444 |
| Yes | 2 | 5% | 9 | 21% | ||
| Per-protocol analysis | ||||||
|---|---|---|---|---|---|---|
| STRATA: ≥ 1 year relationship length (participants with a partner) | 6 months | |||||
| Intervention (n = 25) | Control (n = 29) | test statistic | p value | |||
| N | % | N | % | |||
| Condomless anal or vaginal sex with main partner | ||||||
| No | 17 | 61% | 10 | 33% | 4.364 | 0.0425 |
| Yes | 11 | 39% | 20 | 67% | ||
| Condomless anal or vaginal sex with main partner, no PrEP | ||||||
| No | 14 | 56% | 9 | 31% | 3.422 | 0.0643 |
| Yes | 11 | 44% | 20 | 69% | ||
Note: Kruskal–Wallis tests were used for continuous variable, Chi-square testes were used for categorical variables; and Fisher’s exact tests do not produce test statistics.
Intervention Feasibility and Acceptability
Regarding intervention feasibility, there was low engagement in the intervention activities such that 48% (n = 75) of participants completed their We Prevent intervention session and 50% (n = 80) completed the CTR control condition session. Only two of the intervention participants opted to receive the We Prevent intervention with their partner. We found no meaningful or statistical differences in study activities completion among those recruited before or during the COVID-19 pandemic. Supplementary Table 2 presents the distribution of baseline variables by session uptake regardless of study condition. A greater proportion of participants who completed a session reported having an HIV test in their lifetime ( = 6.44; p = 0.01) and had used an HIV self-test prior to the study ( = 2.41; p = 0.02). There were no other statistically significant differences by session uptake. Acceptability of the We Prevent intervention was high among those who completed it. In total, 93% of participants who completed the We Prevent intervention reported that they “strongly agree or agreed” that they were very satisfied with We Prevent, and 82% reported that they would recommend We Prevent to their friends.
In qualitative interviews with participants who completed the We Prevention intervention (n = 5), participants described the intervention content as novel and generally had positive experiences. For example, one participant appreciated having a neutral third party to discuss their relationship with: “It felt good, especially at the time I was having some issues. I could have gone to my friends with that but that kind of sets a wedge in the relationship and they might view [my partner] negatively—Latinx Multiracial, cisgender man, age 23.” Participants described their appreciation of learning about communication strategies, boundary setting, and sexual consent in their relationships. For example, one participant noted: “I learned that setting those boundaries about sex is important. Setting those boundaries and clear communication is so important—Multiracial, cisgender man, age 20.” However, participants who completed the We Prevent intervention session also noted additional content that would be useful, which included communication strategies with strangers such as sex partners on dating apps and the inclusion of other aspects of sexual health such as pregnancy concerns. Although many participants appreciated having virtual sessions especially with COVID-19 restrictions, others expressed a desire for in-person relationship-focused counseling at local venues.
In interviews with participants who did not complete the We Prevent intervention but completed the follow-up surveys (n = 5) and those who did not complete the We Prevent intervention or the follow-up surveys (n = 6), participants identified a variety of issues impeding intervention participation and study retention. Across both groups, several participants were involved in similar online research studies that also included home HIV testing, which created confusion about study-specific requirements and activities. Those who did not complete their follow-up surveys reported believing they could not return for follow up study activities if they missed any, indicating that communication from the study team may have been unclear. Similarly, participants across both groups explained how they did not know what to expect from the We Prevent intervention or described how they were generally distrustful of researchers and stated that they would have appreciated more personal contact with the study team or counselors. One participant stated: “I do think a phone call or like a ‘How to’ video would have been potentially helpful or like a ‘Here’s what to expect’ links that I could browse or peruse before I did anything else—White, transgender man, age 21.” Another participant noted how a picture with information about the potential counselor would have made them feel more trusting and comfortable to participate in the counseling session.
Eight of the participants who did not complete the We Prevention intervention described how COVID-19 impacted their engagement in the study. For example, three participants explained how that had to move home from college after enrolling in the study and their subsequent concerns about privacy if they were to try to complete the session. For example, one participant stated: “I ended up moving out of our school housing and in with my parents and I think I remember it just like, wanting to do this session and feeling awkward about having like this HIV test kit coming to my parents’ house because, of course, then they’re going to be like, ‘Well, why do you need to be HIV tested, you know, like, what’s going on? What are you doing?”—White, cisgender man, age 24. Others described how the COVID-19 pandemic had created so much stress and mental health challenges that the study was less relevant to their lives as they had stopped being sexually active.
Discussion
This study sought to evaluate the feasibility, acceptability, and preliminary efficacy of We Prevent, a virtual HIV testing and counseling intervention intended to improve relationship skills and reduce sexual HIV transmission risk among younger SMM in relationships with cisgender male partners. Preliminary efficacy results indicated that We Prevent resulted in significant reductions in condomless sex at 9-months compared to standard CTR; however, We Prevent did not have an impact on condomless sex while not on PrEP, sexual agreement formation, HIV communication skills, or IPV in this sample. In post hoc stratified analyses, there were some trends suggesting that We Prevent may reduce HIV transmission risk among younger men and those in longer relationships. Additionally, We Prevent may hold promise in reducing IPV among young men in longer relationships. As such, our study offers important insights into how relationship-focused interventions may be better modified, delivered, and evaluated for younger SMM in relationships.
Only two participants randomized to the We Prevent intervention opted to complete the session with their partner. This finding confirmed our formative work suggesting that younger SMM in relationships may not be interested in or able to complete couples-based HIV interventions with their partners [23]. Young men may not yet have the confidence or relationship skills necessary to actively engage in dyadic interventions—yet We Prevent may, in fact, serve as a stepping-stone to building those skills and allow them to participate in dyadic interventions in the future. Notably, exit interview participants found the content novel and benefitted from the relationship skills component. Thus, the additional relationship skills content may be a developmentally appropriate and culturally relevant addition to standard CTR implemented in community settings. Additionally, We Prevent may be a promising feature for existing digital health interventions focused on the HIV prevention needs of young SMM [4–9].
Notably, there was no evidence that We Prevent created changes in PrEP use or sexual agreement formation among participants. We Prevent content did not specifically focus on PrEP but rather focused on communication skills; therefore, content that explicitly focuses on PrEP may be an important addition. Regarding sexual agreement formation, a recent trial of a virtually delivered HIV counseling intervention for adult male couples found that couples in the intervention arm—who received CHTC and relationship education—were more likely to create and adhere to sexual agreements [31]. While this result was for adult male couples, who may have more experiences of relationships than young SMM, it does suggest that when both members of the dyad are present that there can be impactful conversations around sexual agreements. Therefore, We Prevent may be more successful in creating gains in sexual agreement formation among participants who opt to participate with their partner—as this gives them an opportunity to talk through agreement options with a counselor present.
Both recruitment and retention rates demonstrated adequate feasibility of studying We Prevent and similar studies of young male couples and other digital health interventions designed for young SMM [4–9]; however, actual participation in sessions across both study arms was low. The low engagement may indicate that many young SMM in relationships may want access to HIV home tests but may not be interested in or able to participate in virtual HIV counseling sessions. Similar results were found in a recent pilot RCT of telehealth-delivered HIV testing for transgender and nonbinary youth in the US, who reported discomfort about not knowing the counselor or the perception that they would have to appear on camera as a barrier to intervention participation [32]. Although the quantitative findings demonstrated no differences in engagement in study activities due to the COVID-19 pandemic, our qualitative exit interviews suggested that the pandemic created conditions that might have made it even more challenging for participants to conduct the virtual sessions. The supplementary quantitative analyses illustrated that participants with prior HIV testing and HIV self-testing experiences were more likely to engage in the sessions. Qualitative findings also suggested that in-person sessions may be more acceptable to some as participants reported wanting more frequent and personal interactions with study staff, privacy concerns around completing counseling sessions at home, and a lack of understanding regarding the logistics of the counseling session and/or study activities. We Prevent may be delivered in a youth-friendly clinic, rather than virtually, to reduce discomfort that some participants reported in accessing the intervention, especially among those without HIV testing experiences. It is also possible that a subset of younger SMM simply prefer to take HIV home tests without counseling of any kind. Thus, future research is warranted to improve the feasibility of the We Prevent intervention.
Results from post-hoc stratified analyses indicate that We Prevent may have greater efficacy than standard CTR for some subgroups of younger SMM. While these findings should be interpreted cautiously due to the small sample sizes within strata—and the trial was not powered for these analyses—they signal that implementation of relationship-focused HIV prevention interventions may be best directed at younger SMM ages 15–17 and those in a relationship for longer than 1 year. Younger SMM might not have the relationship experiences or communication skills that older SMM do have, and therefore may benefit more from access to relationship-centered education. Conversely, those in longer relationships (e.g., longer than 1 year) may have more relationship context within which to understand and apply the education and skills they receive.
Finally, our results suggest that virtual counseling sessions by a university-based research team may not be the optimal avenue through which We Prevent and similarly conceived HIV prevention interventions for younger SMM should be delivered. While the virtual format allowed the study to proceed uninterrupted during the onset of COVID-19, qualitative findings suggested that communications with the study team were unclear and that the subsample of participants who did complete counseling sessions wanted more frequent contact with counselors. Additionally, participants reported engaging in similar online studies that made it challenging for them to remember study-specific activities. We did not inquire about participation in other studies during the follow-up surveys, which is an important avenue for future research to understand the impact of engaging in different studies has on study outcomes. As such, caution should be taken when interpreting the study findings given low the session completion and participants’ engagement in other HIV prevention studies. We did not require at-home STI testing procedures as part of study participation, which may contribute to the low uptake at baseline and 6-month follow-up. Local venues including healthcare centers and community-based organizations may be able to better tailor and customize intervention components, including at-home HIV and other STI testing based on participant characteristics (e.g., age, relationship length) and needs (e.g., for virtual or in person counseling, for access to HIV and other STI home testing without counseling) than research institutions.
Limitations
Several limitations likely influence the findings drawn from this study. First, as this was a pilot study, we did not recruit a large enough sample to achieve sufficient statistical power for efficacy analyses. This may partially explain the small number of statistically significant results. Although we were able to recruit a national sample of younger SMM at the peak of the COVID-19 pandemic, the racial/ethnic makeup of the sample does not reflect that of overall HIV incidence among this population [1]. The underrepresentation of Black and Latino/x participants, the fact that no study participants tested positive for HIV, and qualitative findings that participants were simultaneously enrolled in other HIV prevention interventions suggest that our sample may have lower overall risk for HIV than the general population of younger SMM most in need of prevention services. Although there were no statistically significant differences in our outcomes between study arms, those randomized to control condition reported slightly higher levels of condomless sex with outside partners compared to those in the We Prevent intervention, which could potentially bias our results from the null. Finally, we had separate study counselors facilitate the intervention and control arms to avoid contamination. However, we were unable to statistically control for counselor characteristics because there was only one counselor per condition; therefore, it is plausible that counselor characteristics could have impacted the findings.
Conclusion
Despite these limitations, We Prevent may be a feasible and acceptable addition to standard CTR for some SMM youth. Results indicated that the intervention was acceptable and may positively impact reductions in condomless sex and relationship outcomes among subsets of young SMM, but additional research is needed to adapt the intervention to the specific needs of sub-groups of SMM. Further, to our knowledge, this is among the first relationship-focused interventions to have attempted to engage SMM as young as 15 years old [13, 14]. Interventions for younger men (e.g., 15–17) that focus on relationship and sexual communication and boundary setting may be critical to the development and maintenance of behavioral skills across the life course [33]. Overall, the results of this pilot study warrant further implementation in community settings to better understand the acceptability, feasibility, and effectiveness of We Prevent. Future research is needed to examine whether the addition of We Prevent content to standard CTR has the potential to reduce HIV transmission risk and IPV among young SMM with minimal organizational burden.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank the young men who participated in this study; Wesley King for contributions to the manuscript, and staff members: Rachel Valencia, Ramona Rai, Elizabeth Adam, Oksana Kutsa, and Kristina Countryman for their contributions to this study. The authors are also grateful to Dr. Sonia Lee for her support of this project. This study was funded by a Grant from the National Institutes of Health (U19HD89881).
Funding
This study was supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant No. U19HD089881).
Declarations
Conflict of interest
Each of the authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CDC, Estimated HIV incidence and prevalence in the United States 2015–2019. HIV Surveillance Supplemental Report, vol 26. 2021.
- 2.Sullivan PS, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 3.Goodreau SM, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gannon B, et al. A mobile sexual health app on empowerment, education, and prevention for young adult men (MyPEEPS mobile): acceptability and usability evaluation. JMIR Form Res. 2020;4(4):e17901. doi: 10.2196/17901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mustanski B, et al. Biomedical and behavioral outcomes of Keep It Up!: an eHealth HIV prevention program RCT. Am J Prev Med. 2018;55(2):151–158. doi: 10.1016/j.amepre.2018.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauermeister JA, et al. Acceptability and preliminary efficacy of an online HIV prevention intervention for single young men who have sex with men seeking partners online: the myDEx Project. AIDS Behav. 2019;23(11):3064–3077. doi: 10.1007/s10461-019-02426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mustanski B, et al. (2015) Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: the Queer Sex Ed intervention. J Sex Res. 2015;52(2):220–30. [DOI] [PubMed]
- 8.Bauermeister JA, et al. Acceptability and preliminary efficacy of a tailored online HIV/STI testing intervention for young men who have sex with men: the Get Connected! program. AIDS Behav. 2015;19(10):1860–1874. doi: 10.1007/s10461-015-1009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ybarra ML, et al. The effect of a text messaging based HIV prevention program on sexual minority male youths: a national evaluation of information, motivation and behavioral skills in a randomized controlled trial of Guy2Guy. AIDS Behav. 2018;22(10):3335–3344. doi: 10.1007/s10461-018-2118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson KM, et al. The young men and media study: a pilot randomized controlled trial of a community-informed, online HIV prevention intervention for 14–17-year-old sexual minority males. AIDS Behav. 2022;26(2):569–583. doi: 10.1007/s10461-021-03412-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stephenson R, et al. Home-based HIV testing and counseling for male couples (Project Nexus): a protocol for a randomized controlled trial. JMIR Res Protoc. 2017;6(5):e7341. doi: 10.2196/resprot.7341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan PS, et al. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework. SpringerPlus. 2014;3(1):1–13. doi: 10.1186/2193-1801-3-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starks TJ, et al. A pilot randomized trial of intervention components addressing drug use in couples HIV testing and counseling (CHTC) with male couples. AIDS Behav. 2019;23(9):2407–2420. doi: 10.1007/s10461-019-02455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newcomb ME, et al. Integrating HIV prevention and relationship education for young same-sex male couples: a pilot trial of the 2GETHER intervention. AIDS Behav. 2017;21(8):2464–2478. doi: 10.1007/s10461-017-1674-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez O, et al. Adaptation of a couple-based HIV/STI prevention intervention for Latino men who have sex with men in New York City. Am J Mens Health. 2017;11(2):181–195. doi: 10.1177/1557988315579195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu E, et al. Feasibility and promise of a couple-based HIV/STI preventive intervention for methamphetamine-using, black men who have sex with men. AIDS Behav. 2011;15(8):1745–1754. doi: 10.1007/s10461-011-9997-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitchell JW, et al. Feasibility and acceptability of an electronic health HIV prevention toolkit intervention with concordant HIV-negative, same-sex male couples on sexual agreement outcomes: pilot randomized controlled trial. JMIR Form Res. 2020;4(2):e16807. doi: 10.2196/16807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS Behav. 2010;14(1):1–10. doi: 10.1007/s10461-008-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crepaz N, et al. Are couple-based interventions more effective than interventions delivered to individuals in promoting HIV protective behaviors? A meta-analysis. AIDS Care. 2015;27(11):1361–1366. doi: 10.1080/09540121.2015.1112353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.LaCroix JM, et al. Behavioural interventions to reduce sexual risk for HIV in heterosexual couples: a meta-analysis. Sex Transm Infect. 2013;89(8):620–627. doi: 10.1136/sextrans-2013-051135. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell JW. The use of technology to advance HIV prevention for couples. Curr HIV/AIDS Rep. 2015;12(4):516–522. doi: 10.1007/s11904-015-0290-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gamarel KE, et al. The development and testing of a relationship skills intervention to improve HIV prevention uptake among young gay, bisexual, and other men who have sex with men and their primary partners (We Prevent): protocol for a randomized controlled trial. JMIR Res Protoc. 2019;8(1):e10370. doi: 10.2196/10370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gamarel KE, et al. Perspectives from young partnered gay, bisexual, and other men who have sex with men on the adaptation of couples HIV testing and counseling (CHTC) AIDS Behav. 2021;25(3):836–846. doi: 10.1007/s10461-020-03037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hightow-Weidman LB, et al. University of North Carolina/Emory Center for Innovative Technology (iTech) for addressing the HIV epidemic among adolescents and young adults in the United States: protocol and rationale for center development. JMIR Res Protoc. 2018;7(8):e10365. doi: 10.2196/10365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Starks TJ, et al. Adolescent male couples-based HIV testing intervention (We Test): protocol for a type 1, hybrid implementation-effectiveness trial. JMIR Res Protoc. 2019;8(6):e11186. doi: 10.2196/11186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiatrek S, et al. The Annual American Men’s Internet Survey of behaviors of men who have sex with men in the United States: key indicators report 2018. JMIR Public Health Surveill. 2021;7(3):e21812. doi: 10.2196/21812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salazar LF, et al. Development and validation of HIV-related dyadic measures for men who have sex with men. J Sex Res. 2013;50(2):164–177. doi: 10.1080/00224499.2011.636845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stephenson R, Finneran C. The IPV-GBM scale: a new scale to measure intimate partner violence among gay and bisexual men. PLoS ONE. 2013;8(6):e62592. doi: 10.1371/journal.pone.0062592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewinski AA, et al. Applied rapid qualitative analysis to develop a contextually appropriate intervention and increase the likelihood of uptake. Med Care. 2021;59(6 Suppl 3):S242. doi: 10.1097/MLR.0000000000001553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res. 2019;280:112516. doi: 10.1016/j.psychres.2019.112516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stephenson R, et al. Efficacy of a telehealth delivered Couples’ HIV Counseling and Testing (CHTC) Intervention to improve formation and adherence to safer sexual agreements among male couples in the US: results from a randomized control trial. AIDS Behav. 2022 doi: 10.1007/s10461-022-03619-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephenson R, et al. Project Moxie: results of a feasibility study of a telehealth intervention to increase HIV testing among binary and nonbinary transgender youth. AIDS Behav. 2020;24(5):1517–1530. doi: 10.1007/s10461-019-02741-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Viner RM, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–1652. doi: 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.