Abstract
Introduction
Situational judgment tests have been adopted by medical schools to assess decision-making and ethical characteristics of applicants. These tests are hypothesized to positively affect diversity in admissions by serving as a noncognitive metric of evaluation. The purpose of this study was to evaluate the performance of the Computer-based Assessment for Sampling Personal Characteristics (CASPer) scores in relation to admissions interview evaluations.
Methods
This was a cohort study of applicants interviewing at a public school of medicine in the southeastern United States in 2018 and 2019. Applicants took the CASPer test prior to their interview day. In-person interviews consisted of a traditional interview and multiple-mini-interview (MMI) stations. Between subjects, analyses were used to compare scores from traditional interviews, MMIs, and CASPer across race, ethnicity, and gender.
Results
1,237 applicants were interviewed (2018: n = 608; 2019: n = 629). Fifty-seven percent identified as female. Self-identified race/ethnicity included 758 White, 118 Black or African-American, 296 Asian, 20 Native American or Alaskan Native, 1 Native Hawaiian or Other Pacific Islander, and 44 No response; 87 applicants identified as Hispanic. Black or African-American, Native American or Alaskan Native, and Hispanic applicants had significantly lower CASPer scores than other applicants. Statistically significant differences in CASPer percentiles were identified for gender and race; however, between subjects, comparisons were not significant.
Conclusions
The CASPer test showed disparate scores across racial and ethnic groups in this cohort study and may not contribute to minimizing bias in medical school admissions.
Introduction
Underrepresentation in US medical school from individuals identifying as Black or African-Americans, Hispanic, and American Indian or Alaska Native persists [1]. Underrepresented in medicine (UIM) physician role models lead to better outcomes for underrepresented minority patients [2]. Additionally, UIM students are nearly two times more likely to have plans to practice in underserved areas compared to their White and Asian counterparts [3]. There has been a steady decline in the numbers of African-American men entering medical school since 1978 [3–6]. Speculation about metrics such as grade point average (GPA) and Medical College Admission Test (MCAT) to select candidates for medical school may contribute to this decline [7].
Studies indicate that UIM individuals have lower GPA and MCAT scores [8,9]. Since GPA and MCAT scores are used to screen applicants for interviewing, overreliance on academic performance measures alone fails to capture noncognitive characteristics important for physicians [7]. Also, a meta-analysis reported the MCAT had minimal predictive value on future academic performance [10]. Structural racism and disparate educational opportunity play a role in MCAT performance of underrepresented applicants [11]. Consequently, overreliance on GPA and MCAT has the potential to lead to continued bias in admissions decisions.
Medical schools report balancing individual experience and attributes in conjunction with traditional metrics [12–14]. However, GPA and MCAT scores are heavily weighted in this screening process. Situational judgment tests add an alternative metric, assessing decision-making on predetermined scenarios [15]. Respondents judge the appropriateness of response choices by stating what they should or would do. Situational judgment tests in business demonstrated job performance predictive validity [16]. These tests have been used in hiring decisions and only recently have been used for medical school admissions [17].
The Computer-based Assessment for Sampling Personal Characteristics (CASPer) is a 12-section, online video-stem based situational judgment test of non-academic competencies. The test is structured to provide a scenario covering topics such as collaboration, communication, empathy, equity, ethics, motivation, problem solving, professionalism, resilience, and self-awareness. After each scenario, three follow up questions are presented that must be answered within five minutes using an open-ended response format.
Situational judgment tests are being used more by medical schools for holistic admissions processes. In fact, a review of the CASPer website indicates that 16 US medical schools and 6 osteopathic medical schools require students complete CASPer. The schools listed are geographically dispersed throughout the country.
The Office of Admissions for the University of North Carolina School of Medicine (UNCSOM) explored CASPer as an additional metric to use in admissions processes. Before integrating CASPer into the admissions process, we explored associations CASPer percentile scores had with our MMI and traditional interview scores. Our research questions included the following: (1) What is the difference in CASPer percentile by gender and race/ethnicity? (2) What is the association between CASPer percentile with MMI and traditional interview scores?
Material and methods
This cohort study included applicants to UNCSOM during the 2018 and 2019 admissions cycles. Demographic data extracted from the American Medical College Application Service (AMCAS) application included gender identification and race/ethnicity. The UNC Institutional Review Board reviewed this study and determined it met criteria for exempt status (IRB No. 18–3453) and met criteria under 45CFR46.116(f) to waive consent.
All applicants were required to take CASPer prior to their interview. Because we were still exploring the results, the UNCSOM did not formally use the CASPer percentile scores in admissions decisions. The test is taken by applicants on preset dates and times, requiring Internet access [15]. CASPer is comprised of up to 12 scenarios; each item comes with three questions students must provide a response. The test itself takes up to 120 minutes. CASPer is scored on a 9-point Likert scale (1 = unsatisfactory to 9 = superb). Each section is scored by a unique rater, thereby resulting in a score comprised of multiple raters. Responses are scored relative to other responses to the same scenario. Psychometric results of CASPer indicate overall test reliability (G = .72-.83) and inter-rater reliability (G = .82-.95) [18]. Students are informed about what quartile they achieved, but do not receive a specific percentile score. Only the medical school receives their percentile score.
On the interview day, applicants experience a 30-minute traditional interview with a faculty interviewer who had access to the applicant’s AMCAS materials prior to the interview. Seven interpersonal and intrapersonal competencies were assessed by multiple mini-interviews (MMI) questions within two group stations (12–14 minutes) and two one-on-one stations (8 minutes each). A final station (8 minutes) allowed applicants to interact with a simulated patient as an introduction to our curriculum. Evaluators for the MMI stations were blinded to the applicant’s AMCAS materials.
Applicant evaluations were scored 1–5 (low to high) for both traditional interview score and for each MMI station. Reliability across MMI stations resulted in Cronbach alpha = .66. Traditional interviewers assigned a score based on holistic review of the application and interview. MMI station interviewers were provided with a station-specific rubric for scoring, and an overall average MMI score was calculated.
To answer our first research question, CASPer percentile scores were compared by gender and UIM status. We generated a bivariate categorization of UIM using white and Asian as non-UIM and all others plus Hispanic as UIM. If significant differences were identified using the bivariate UIM categorization, analysis of variance (ANOVA) was conducted with racial groups of more than 100 individuals.
To answer the second research question, CASPer percentile, MMI and traditional interview scores were analyzed. Differences in scores were analyzed based on gender and UIM. Magnitude of factor differences was indicated by calculating Cohen’s d, where Cohen’s d = 0.2 is considered a “small” effect size, 0.5 “medium”, and 0.8 “large” [19]. Regression analyses were conducted using MMI scores as the criterion variable and CASPer, gender, and UIM as predictors. All analyses were conducted using IBM SPSS v. 28 (Armonk, NY). Data is available as a Supporting Information file.
Results
There were 1,237 applicants interviewed during 2018 (n = 608) and 2019 (n = 629) admissions cycles. The average age of applicants was 24 years old. Fifty-seven percent identified as female. Demographic information is detailed in Table 1.
Table 1. Demographic information for applicants.
| Age | 24.02 (Range 20–41) |
| Gender | |
| Female | 699 (56.5%) |
| Male | 538 (43.5%) |
| Underrepresented in Medicine* | 213 (17.2%) |
| Race | |
| Asian | 296 (23.9%) |
| Black or African-American | 118 (9.5%) |
| Native Hawaiian or Other Pacific Islander | 1 (.1%) |
| Native American or Alaskan Native | 20 (1.6%) |
| White | 758 (61.3%) |
| Unanswered | 44 (3.6%) |
| Hispanic | 87 (7.0%) |
Percents are of the population sampled.
*Underrepresented in medicine was defined as Black or African-American, Native Hawaiian or Other Pacific Islander, Hispanic, and Native American or Alaskan Native.
To address our first research question, we used t-tests for bivariate comparisons. Table 2 summarizes the comparisons by gender, race, and ethnicity. In comparing gender, females scored higher for MMI (t = 3.77, p = .001, d = .21) and traditional interviews (t = 3.28, p = .001, d = .19). For CASPer percentile scores, UIM (t = -6.35, p = .001, d = .49) and Hispanic applicants (t = -3.28, p = .001, d = .38) scored lower. Given the significant differences of candidates identifying as UIM, we analyzed difference of candidates identifying as Asian, Black/African American, and White to obtain more specific results.
Table 2. Comparisons of MMI Score, Traditional Interview Score and CASPer Percentile.
| Mean | Std. Dev. | Mean | Std. Dev. | t | p | Cohen’s d | |
|---|---|---|---|---|---|---|---|
| Gender | Female (n = 698) | Male (n = 537) | |||||
| MMI Average | 3.76 | .48 | 3.66 | .48 | 3.77 | .000 | .21 |
| Traditional Interview | 4.21 | .80 | 4.05 | .86 | 3.28 | .001 | .19 |
| CASPer Percentile | 61.05 | 26.76 | 58.50 | 27.97 | 1.59 | .111 | .09 |
| UIM | Yes (n = 212) | No (n = 1023) | |||||
| MMI Average | 3.74 | .50 | 3.71 | .48 | .84 | .402 | .07 |
| Traditional Interview | 4.11 | .83 | 4.15 | .83 | -.61 | .543 | .04 |
| CASPer Percentile | 48.92 | 27.51 | 62.18 | 26.73 | -6.35 | .000 | .49 |
| Hispanic | Yes (n = 87) | No (n = 1129) | |||||
| MMI Average | 3.63 | .50 | 3.72 | .48 | -1.68 | .093 | .19 |
| Traditional Interview | 4.01 | .83 | 4.15 | .83 | -1.51 | .131 | .17 |
| CASPer Percentile | 50.25 | 25.87 | 60.51 | 27.26 | -3.28 | .001 | .38 |
p significant < .05.
The mean CASPer percentile score for Asian was 63.04 (n = 282, SD: 27.77, 95% CI:59.78–66.29), Black/African American was 47.86 (n = 112, SD: 28.74, 95% CI: 42.48–53.24), and White was 60.95 (n = 728, SD: 26.32, 95% CI: 59.04–62.87). The between groups model was significant for race (F2,1116 = 12.42, p < .001, h2 = .02). Post hoc analysis indicated Black/African American candidates had significantly lower CASPer percentile scores than Asian and White candidates (p < .001).
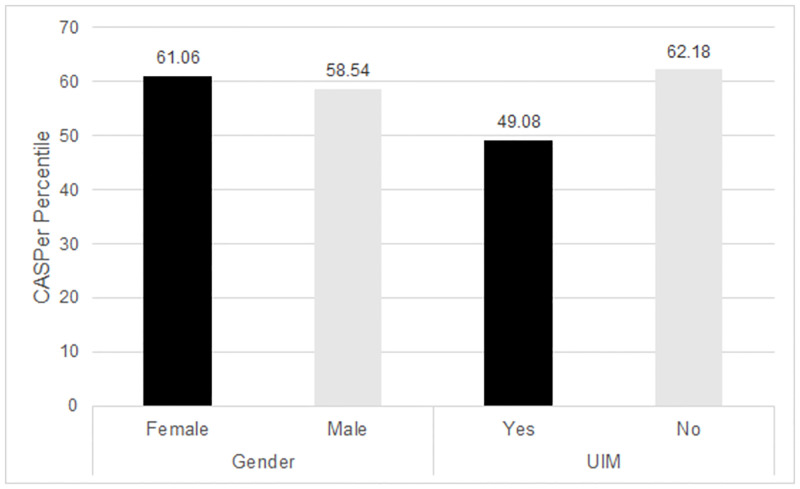
The between groups model for gender was also significant (F2,1116 = 12.42, p < .001, h2 = 0) for females scoring higher than males. The interaction of race and gender was not statistically significant. (Fig 1).
Fig 1. Differences in CASPer Percentile by Gender, SES Indicator, and UIM Status.
A between subjects ANOVA indicated there were significant differences between CASPer percentile scores by each variable (Gender: F2,1116 = 12.42, p < .001, h2 = 0, UIM: F2,1116 = 12.42, p < .001, h2 = .02). Interactions between variables did not result in statistically significant differences.
To address question two, a linear regression model explored an association with MMI score using CASPer percentile, gender, and race. All three predictors were significantly associated with MMI score (Constant: 3.68; CASPer: β = .16, t = 5.55, p < .001; Gender: β = -.10, t = -3.50, p < .001; Race: β = .07, t = 2.311, p = .02). However, these variables identified a weak correlation (r = .20), explaining approximately 4 percent of the variance in MMI scores.
Discussion
Situational judgment tests contribute noncognitive data to consider as part of the medical school admissions process [20]. Based on our pool of candidates, CASPer scores varied significantly, with lower scores seen in those identifying as Black or African-American, American Indian or Alaskan Native, Native Hawaiian or Other Pacific Islander, or Hispanic ethnicity.
Our findings different from the New York Medical College School of Medicine study [15], which may be a reflection of the differences in the candidate pools. Specifically, in their comparison of White and African-American applicants, the White applicants scored higher on CASPer, but not significantly. As part of their study they used these results to simulate potential for an interview offer for medical school. With the inclusion of CASPer in the simulation, results suggested an increase in African-Americans being invited to interview.
Our results suggest UIM students may be further disadvantaged if CASPer was weighted in applicant screening. The UNCSOM candidate pool is from the southeastern US; perhaps social and cultural differences played a role in individual performance. Previous studies note differences based on race and ethnicity [21] as a result of response instructions for the test. This may be the result of the scoring process as well, since raters compare scenario responses as they grade. The CASPer test was also developed in Canada [22,23], but little research has been published using the instrument in the United States. Our results should be an example to other schools to regularly analyze results of instruments being used to ensure they are not inadvertently disadvantaging a particular population.
There is evidence of increased use of CASPer in medical school admissions. Additionally, a scan of the CASPer website indicates 22 US medical schools and osteopathic schools use the exam. Although medical schools are using the exam, there continues to be little agreement on what is actually being measured or how to integrate the information effectively in holistic review [24]. Altus Assessments has recommended using quartile performance to rate candidates [25], suggesting that acceptable scores range from the 33rd to 75th percentile. However, with such a broad range of scores one must question what these results actually mean and how do they pertain to future medical student performance.
When CASPer was analyzed by gender, there was not a significant difference in how females performed compared to males. These findings are consistent with work by Whetzel and colleagues [21]. However, females did significantly better on MMIs and the traditional interview, consistent with other studies demonstrating stronger female communication ratings [26,27]. Yet given a study demonstrating a correlation of situational judgment test items to interpersonal communication skills [24], one would expect females to have outperformed males on CASPer.
Based on two years of data from UNCSOM, MMI and traditional scores did not show differences across racial groups [26]. Since UNCSOM was piloting CASPer, the results of the test were not part of the formal deliberations by the admissions committee. If we continue using CASPer, applying methods outlined by Aguinis and Smith [28] may clarify an appropriate cut score for CASPer. They calculated relationships between desired performance levels, expected adverse impact, and probabilities of false positives and false negatives to determine a cut score. Alternatively, weighting interview metrics using a Pareto optimization approach could allow for institutional flexibility in predictive measures as well as diversity goals [29].
This study was conducted at a single institution in the southeastern US, presenting a limitation. Future studies should be conducted with other medical schools using CASPer to explore whether differences appear. As with any assessment, requiring applicants to complete CASPer may have contributed to performance on the examination. This is a question that should be further explored in future research.
Conclusions
Using a variety of methods in the admissions process appears to be the best approach to ensure diversity and inclusion in medical student classes. Overreliance on MCAT scores or GPAs inadvertently disadvantages underrepresented minorities. Although well intended, the CASPer was not found to level the playing field as we thought it might. Based on these data, using a combined approach of rating academic performance, preparation for medical school, life experience, interviews, and MMIs along with appropriately trained interviewers and committee members may be sufficient for holistic admissions that favors a diverse medical school class.
Supporting information
(XLSX)
Data Availability
The data has been uploaded as a Supporting information file.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Lett LA, Murdock HM, Orji WU, Aysola J, Sebro R. Trends in racial/ethnic representation among US medical students. JAMA Netw Open. 2019; 2(9):e1910490. doi: 10.1001/jamanetworkopen.2019.10490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alsan M, Garrick O, Graziani GC. Does diversity matter for health? Experimental evidence from Oakland. NBER Working Paper 24787. June 2018. Revised August 2019. https://www.nber.org/system/files/working_papers/w24787/w24787.pdf. Accessed May 12, 2021.
- 3.Association of American Medical Colleges. Diversity in Medicine: Facts and Figures 2019. https://www.aamc.org/data-reports/workforce/report/diversity-medicine-facts-and-figures-2019. Retrieved May 12, 2021.
- 4.Carnevale AP, Strohl J. How increasing college access is increasing inequality, and what to do about it. In: Kahlenberg RD, ed. Rewarding Strivers: Helping Low-Income Students Succeed in College. New York, NY: Century Foundation; 2010. [Google Scholar]
- 5.Thomas BR, Dockter N. Affirmative action and holistic review in medical school admissions: Where we have been and where we are going. Acad Med. 2019; 94:473–476. doi: 10.1097/ACM.0000000000002482 [DOI] [PubMed] [Google Scholar]
- 6.Poole KG Jr, Jordan BL, Bostwick JM. Mission drift: Are medical school admissions committees missing the mark on diversity? Acad Med. 2020; 95(3):357–60. doi: 10.1097/ACM.0000000000003006 [DOI] [PubMed] [Google Scholar]
- 7.Ballejos MP, Rhyne RL, Parkes J. Increasing the relative weight of noncognitive admission criteria improves underrepresented minority admission rates ot medical school. Teach Learn Med. 2015; 27(2):155–162. doi: 10.1080/10401334.2015.1011649 [DOI] [PubMed] [Google Scholar]
- 8.Heller CA, Rúa SH, Mazumdar M, Moon JE, Bardes C, Gotto AM Jr. Diversity efforts, admissions, and national rankings: Can we align priorities? Teach Learn Med. 2014; 26(3):304–11. doi: 10.1080/10401334.2014.910465 [DOI] [PubMed] [Google Scholar]
- 9.Ramsbotton-Lucier M, Johnson MM, Elam CL. Age and gender differences in students’ preadmission qualifications and medical school performances. Acad Med. 1995; 70(3):236–9. doi: 10.1097/00001888-199503000-00016 [DOI] [PubMed] [Google Scholar]
- 10.Donnon T, Paolucci EO, Violato C. The predictive validity of the MCAT for medical school performance and medical board licensing examinations: A meta-analysis of the published research. Acad Med. 2007; 82:100–6. doi: 10.1097/01.ACM.0000249878.25186.b7 [DOI] [PubMed] [Google Scholar]
- 11.Lucey CR, Saguil A. The consequences of structural racism on MCAT scores and medical school admissions: The past is prologue. Acad Med. 2020; 95(3):351–6. doi: 10.1097/ACM.0000000000002939 [DOI] [PubMed] [Google Scholar]
- 12.Grbic D, Morrison E, Sondheimer HM, Conrad SS, Milem JF. The association between a holistic review in admissions workshop and the diversity of accepted applicants and students matriculating to medical school. Acad Med. 2019; 94:396–403. doi: 10.1097/ACM.0000000000002446 [DOI] [PubMed] [Google Scholar]
- 13.Milem JF, O’Brien CL, Bryan WP. The matriculated student: Assessing the impact of holistic review. In: Roadmap to Excellence: Key Concepts for Evaluating the Impact of Medical School Holistic Admissions. Washington, DC: Association of American Medical Colleges; 2013. [Google Scholar]
- 14.Association of American Medical Colleges. Holistic Review. https://www.aamc.org/services/member-capacity-building/holistic-review. Accessed May 28, 2021.
- 15.Juster FR, Baum RC, Zou C, Risucci D, Ly A, Reiter H, et al. Addressing the diversity-validity dilemma using situational judgment tests. Acad Med. 2019; 94(8):1197–203. doi: 10.1097/ACM.0000000000002769 [DOI] [PubMed] [Google Scholar]
- 16.Webster ES, Paton LW, Crampton PES, Tiffin PA. Situational judgement test validity for selection: A systematic review and meta-analysis. Med Educ. 2020; 54:888–902. doi.org/doi: 10.1111/medu.14201 [DOI] [PubMed] [Google Scholar]
- 17.de Leng WE, Stegers-Jager KM, Husbands A, Dowell JS, Born MP, Themmen APN. Scoring method of a situational judgment test: Influence on internal consistency reliability, adverse impact and correlation with personality? Adv Health Sci Educ. 2017; 22:243–65. doi: 10.1007/s10459-016-9720-7 [DOI] [PubMed] [Google Scholar]
- 18.Dore KL, Reiter HI, Kreuger S, Norman GR. CASPer, an online pre-interview screen for personal/professional characteristics: Prediction of national licensure scores. Adv Health Sci Educ. 2017; 22:327–36. doi: 10.1007/s10459-016-9739-9 [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for Behavioral Sciences, 2nd ed. New York, NY: Routledge, 1988. [Google Scholar]
- 20.Patterson F, Knight A, Dowell J, Nicholson S, Cousans F, Cleland J. How effective are selection methods in medical education? A systematic review. Med Educ. 2016; 50:36–60. doi: 10.1111/medu.12817 [DOI] [PubMed] [Google Scholar]
- 21.Whetzel DL, McDaniel MA, Nguyen NT. Subgroup differences in situational judgment test performance: A meta-analysis. Hum Perform. 2008; 21:291–309. doi: 10.1080/08959280802137820 [DOI] [Google Scholar]
- 22.Dore KL, Reiter HI, Eva KW, et al. Extending the interview to all medical school candidates—Computer-based multiple sample evaluation of noncognitive skills (CMSENS). Acad Med. 2009;84(10):S9–12. doi: 10.1097/ACM.0b013e3181b3705a [DOI] [PubMed] [Google Scholar]
- 23.O’Connell MS, Hartman NS, McDaniel MA, Grubb WL III, Lawrence A. Incremental validity of situational judgment tests for task and contextual job performance. Internatl J Select Assess. 2007; 15(1):19–29. doi: 10.1111/j.1468-2389.2007.00364.x [DOI] [Google Scholar]
- 24.Tiffin PA, Paton LW, O’Mara D, MacCann C, Lang JWB, Lievens F. Situational judgement tests for selection: Traditional vs construct-driven approaches. Med Educ. 2020;54:105–11. doi: 10.1111/medu.14011 [DOI] [PubMed] [Google Scholar]
- 25.Altus Assessments. Frequently Asked Questions: Post-Test. https://takecasper.com/faq/#after Accessed May 12, 2021.
- 26.Langer T, Ruiz C, Tsai P, et al. Transition to multiple mini interview (MMI) interviewing for medical school admissions. Perspect Med Educ. 2020; 9:229–35. doi: 10.1007/s40037-020-00605-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vogel D, Meyer M, Harendza S. Verbal and non-verbal communication skills including empathy during history taking of undergraduate medical students. BMC Med Educ. 2018; 18:157. doi: 10.1186/s12909-018-1260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aguinis H, Smith MA. Understanding the impact of test validity and bias on selection errors and adverse impact in human resource selection. Pers Psychol. 2007; 60:165–99. doi: 10.1111/j.1744-6570.2007.00069.x [DOI] [Google Scholar]
- 29.Lievens F, Sackett PR, De Corte W. Weighting admission scores to balance predictiveness-diversity: The Pareto-optimization approach. Med Educ. 2021; ePub ahead of print. doi: 10.1111/medu.14606 [DOI] [PubMed] [Google Scholar]