Abstract
Background.
Novel strategies are needed to curb the opioid overdose epidemic. Smart home sensors have been successfully deployed as digital biomarkers to monitor health conditions, yet they have not been used to assess symptoms important to opioid use and overdose risks.
Objectives.
This study piloted smart home sensors and investigated their ability to accurately detect clinically pertinent symptoms indicative of opioid withdrawal or respiratory depression in adults prescribed methadone.
Methods.
Participants (N=4, 3 completed) were adults with opioid use disorder exhibiting moderate levels of pain intensity, withdrawal symptoms and sleep disturbance. Participants were invited to two 8-hour nighttime sleep opportunities to be recorded in a sleep research laboratory, using observed polysomnography and ambient smart home sensors attached to lab bedroom walls. Measures of feasibility included completeness of data captured. Accuracy was determined by comparing polysomnographic data of sleep/wake and respiratory status assessments with time and event sensor data.
Results.
Smart home sensors captured overnight data on 48 out of 64 hours (75% completeness). Sensors detected sleep/wake patterns in alignment with observed sleep episodes captured by polysomnography 89.4% of the time. Apnea events (n=118) were only detected with smart home sensors in two episodes where oxygen desaturations were less severe (> 80%).
Conclusion.
Smart home technology could serve as a less invasive substitute for biological monitoring for adults with pain, sleep disturbances, and opioid withdrawal symptoms. Supplemental sensors should be added to detect apnea events. Such innovations could provide a step forward in assessing overnight symptoms important to populations taking opioids.
Keywords: Machine Learning, Opioid-Related Disorders, Pain, Polysomnography, Sleep
Insufficient pain relief has been linked to illicit substance use, despondency, and suicide (Petrosky et al., 2018; Weiss et al., 2014). Pain is the most common reason United States (U.S.) adults report misuse of prescription opioids, or taking opioids for reasons other than which they were prescribed (Han et al., 2017). Studies have found as many as 26% of people with chronic pain display patterns of misuse that can be a precursor to a substance use disorder (Volkow et al., 2018). Particularly among adults with opioid use disorders (OUD), comorbid chronic pain is highly prevalent with rates reported from 60–74% (John & Wu, 2020; Speed et al., 2018). As people with OUD attempt to self-manage symptoms of pain, mood, sleep, and opioid withdrawal with sedating substances (Cicero & Ellis, 2017), they increase the risk of unintended respiratory depression and/or overdose deaths.
Therefore, innovations are needed to increase understanding of how people with OUD are managing symptoms around the clock, especially at night when respiratory rates slow and sleep apneas may also be occurring (Finlay et al., 2020). Treatment with medications for opioid use disorder (MOUD) are increasingly recognized as key strategies to reduce overdose deaths (Substance Abuse and Mental Health Services Administration, 2018). However, MOUD medications such as methadone, a μ-opioid full agonist with excellent ability to curb opioid withdrawal, has also been linked to episodes of severe respiratory depression (Fox et al., 2018). Additionally, MOUD treatment outcomes are often suboptimal due to withdrawal symptoms such as sleep disturbances (Dunn et al., 2018), pain (St. Marie & Broglio, 2020), and subsequent difficulty retaining patients in treatment beyond the first 30 days (Morgan et al., 2017; Wolf & Gold, 2020). There is a need for robust in-home data to fill the information void that exists regarding how symptoms are managed between clinical office visits for people prescribed opioids and to capture adverse effects that may be occurring overnight.
Smart home technology provides an opportunity for unobtrusive and continuous monitoring of daily activities (Cook et al., 2018). Using ambient sensors in the home (no cameras, no microphones), information can be gleaned that cannot be easily captured in traditional clinical laboratory settings. Prior work using sensor-based monitoring for older adults with chronic conditions has allowed the capture of around-the-clock sensor data to track movements that can identify behaviors indicative of changes in health status such as alterations in daily routines (Sprint et al., 2016b), sleep (Williams & Cook, 2017), and socialization (Skubic et al., 2015). Machine learning (ML) models sort and computationally analyze massive amounts of smart home sensor data to assist clinicians in making sense of the data. Our team uses a ‘clinician-in-the-loop’ approach, described in detail elsewhere, to convert raw sensor data into meaningful clinically-relevant information (Fritz & Dermody, 2019) ML models are not new to health care; they are used in medical imaging (Odaibo et al., 2019), neurology (Rajpurkar et al., 2017), cardiology (Rajpurkar et al., 2017), and more. Smart home sensors have primarily been used in research to advance capabilities for facilitating aging-in-place goals. Using ambient sensors and continuous monitoring, smart homes are capable of detecting eleven activities of daily living performed naturally by older adults in their homes with 92% accuracy, thus, they are highly reliable (Aminikhanghahi & Cook, 2019). These activities include bathing, bed-toilet transitions, personal hygiene, cooking, eating, washing dishes, sleeping, relaxing, working, and leaving and entering the home. In addition, smart home researchers have shown capability to detect falls, insomnia, onset of a urinary tract infection, onset of side effects from cancer treatment, exacerbations of congestive heart failure, cognitive changes, and more (Sprint et al. 2016a).
Although existing sensor platforms support remote monitoring of sleep and respiration (Sharkey et al., 2009), smart home sensors are less invasive, do not require a person to attach devices that may disrupt sleep, and require no interaction on the part of the observed person. Our team’s prior work has successfully designed, installed, and tested smart environments using ML in more than 140 homes of community-dwelling older adults. We have focused on mechanistic explorations of disease and symptom management in naturalistic settings for older adults experiencing cognitive decline due to Alzheimer’s disease and related dementias Aramendi et al., 2018a, 2018b; Seelye et al, 2013). From these studies and others examining daily living patterns, we have perfected the use of sensor-based data and ML to collect, examine, and validate, large samples of data with relatively few participants to discover important information about human behavior patterns. Prior research by our team has determined that smart home sensors can detect pain-related behaviors in older adults using a small amount of sensor data (Fritz et al., 2020). Despite that accuracy of activity recognition has been found to reach 99.3% with smart home sensors (Dahmen & Cook, 2021), sensor-based detection of symptoms is not yet broadly used outside of the research setting. Thus, we aimed to test the feasibility and accuracy of using smart home sensor data to effectively identify symptoms important to MOUD populations, particularly those people with co-existing pain symptoms that are known to disrupt sleep (Husak & Bair, 2020).
The primary objective of this study was to gather evidence supporting the deployment of smart home sensors as digital biomarkers for remote monitoring of opioid withdrawal and overnight respiratory status. We operationalized signs indicative of “opioid withdrawal” using symptoms identified on commonly used withdrawal scales that we expected could be detected using ambient sensors among adults receiving methadone treatment for OUD, namely restless leg movements and trouble getting to sleep and staying asleep. Based on our prior work, we expected that sleep and leg movement could be detected with sensor data (Aminikhanghahi & Cook, 2019). We operationalized “respiratory depression” as apnea events and peripheral arterial oxygen saturation (SaO2 pulse oximetry readings) less than 90%. that are commonly analyzed with polysomnography and clinically relevant as potential indicators of opioid overdose. We expected that ambient sensors could pick up changes in respiratory status if they were accompanied by changes in body movement (e.g., transitioning from restless to still). Our specific aims were to determine 1) whether smart home sensors could consistently detect changes in sleep and restless leg movement captured simultaneously with observed overnight polysomnography (PSG); and 2) and whether observed PSG recordings of respiratory depression could be simultaneously detected in smart home sensor data. To our knowledge, the present study is the first to examine whether smart home technology can be used as a novel approach to detect sleep/wake cycles and evidence of activity or behaviors significant to populations receiving MOUD treatment. If feasible and accurate, smart home sensors could unobtrusively capture important clinical information in natural home environments for people receiving methadone or other opioids. In-home technology could provide new insights on treatment effects and, potentially, provide information to better manage pain, opioid withdrawal symptoms, and prevent overdose deaths.
Methods
Design and Sample
The present IRB-approved observational pilot study included four participants recruited between September 2019 and January 2020 from two urban outpatient Opioid Treatment Programs (OTPs) in the northwestern U.S. who spent two consecutive nights in an observed sleep lab. They were recruited from a sub-sample of a larger study exploring hyperbaric oxygen therapy to reduce opioid withdrawal symptoms (Wilson et al., 2022). Eligibility criteria included being in the first 90 days of methadone-based MOUD treatment, ability to read, write and speak English, and greater than 18 years of age. Participants were screened to meet a minimum threshold of sleep, pain, and opioid withdrawal symptoms: at least “moderate” withdrawal symptoms on the Adjective Rating Scale for Withdrawal (ARSW), a score of at least 4 on a 0–10 Numeric Pain Intensity Scale and reported sleep burden above 50 (as reflected in a “T-score”) on the Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance (SD) and Sleep-Related Impairment (SRI) items. Ineligible were those who were pregnant, had a medical or psychiatric condition that would compromise safe study participation, or had a previous diagnosis of a sleep disorder or respiratory condition. A convenience sample allowed for inviting four of the eight participants who had already provided written informed consent to the parent study to participate in the smart home sensor data collection after learning about the opportunity. All agreed to participate and signed an additional consent to be monitored with sensors while in the sleep lab.
Procedures
After informed consent, participants (2 male, 2 female) were each given an identifier (P1, P2, P3, P4). Participants were scheduled for two consecutive in-laboratory overnight sleep phases to capture cardiorespiratory PSG and sensor data. PSG and sensor data were collected simultaneously to be compared later for cross-validation. Participants arrived at the sleep lab at 17:00 and completed demographic and health questionnaires to describe the sample using a secure online format. Paper and pencil surveys were used for additional data collection just before bedtime at 20:00 and upon being awakened at 06:00 in the morning. After being offered a small snack, at 21:00 participants prepared for eight hours of overnight monitoring using the sleep lab’s cardiorespiratory and PSG equipment. Participants received gift cards totaling $150 to compensate for time and travel.
Measures
Demographics and Health Characteristics
Socio-demographic and health history variables captured for the parent study included age, gender, race/ethnicity, education level, disease and mental health diagnoses, and medications. The following health characteristic data were collected for population descriptive purposes for the present study.
Clinical Opiate Withdrawal Scale (COWS)
Opioid withdrawal assessment using the COWS was administered by a trained research assistant before and after each night of sleep. The COWS is an 11-item scale designed to be administered by a clinician to rate common signs and symptoms of opioid withdrawal over time (Wesson & Ling, 2003). Acceptable internal reliability has been demonstrated (Cronbach’s alpha = .78) and concurrent validity established by correlations with the Clinical Institute Narcotic Assessment (CINA) (r = .85) (Tompkins et al., 2009). Signs such as observed restlessness and tremors were captured with the COWS.
Adjective Rating Scale of Withdrawal (ARSW)
Opioid withdrawal self-assessment was determined using the ARSW using a paper and pencil survey before and after each night of sleep. The ARSW is a 16-item scale designed to be self-administered to rate common signs and symptoms of opioid withdrawal with reliability as a single point in time assessment; symptoms such as muscle cramps, runny nose, “trouble getting to sleep,” and “fitful sleep” are rated on a 9-point scale from none to severe with a maximum summed score of 144 (Barbosa-Leiker et al., 2014). The primary difference from the COWS is that the ARSW is self-reported versus observed symptoms.
Numeric Rating Scale (NRS)
Pain intensity was measured using a 0–10 self-report scale to measure pain “right now” with 0 = “no pain” and 10 = “worst pain ever” before and after each night of sleep at 20:00 and 06:00. The NRS is strongly associated with other pain intensity measures and has been broadly validated across many patient populations; scores of 4–6 are generally considered to represent moderate pain and 7–10 severe pain (Karcioglu et al., 2018).
Sleep Quality
Sleep quality was assessed using the 8-item PROMIS Sleep Disturbance and Sleep-Related Impairment scales that have shown internal reliability > .9 for all items and scores with acceptable convergent validity (Yu et al., 2011). Items ask about trouble falling asleep, staying asleep, and next day effects of poor sleep.
PSG Data Collection
Sleep data were collected using standard electrode montage and respiratory equipment for PSG gathered in 30-second epochs (Finlay et al., 2020). All participants fell asleep between 21:41 and 22:18 (mean 22:01), were woken at 06:00, and left the lab by 07:00. Records were scored for sleep stage, respiratory events, and periodic leg movements (PLMs: scored as a series of at least four muscle contractions in the anterior tibial muscle during sleep) by a trained PSG technologist using established criteria from the American Academy of Sleep Medicine (Berry et al., 2012). Such criteria have been determined to be sufficiently reliable for overall sleep scoring (Cohen’s kappa 0.76) (Lee at al., 2022).
Ambient Sensor Data Collection
We placed three ambient sensors in the sleep lab room where the participant stayed overnight (Figure 1) (Cook et al., 2012). One passive infrared (PIR) sensor was placed on the ceiling above the bed to sense the area over the bed. The other PIR sensor was placed on a wall where it was unobstructed by furniture. It sensed all motion occurring anywhere in the room. The door use sensor was placed on the sleep lab bedroom door. Each sensor had a unique purpose. The sensor over the bed sensed when the participant was in bed and moving (whole body or limbs only). The sensor detecting motion anywhere in the room allowed tracking of participant moving around the room as well as staff movements anywhere in the room. The door use sensor allowed tracking of anyone entering or exiting the room; for example, night-time bathroom use or staff entering/exiting to assist the participant.
Figure 1.

(left) The CASAS Smart Home in a Box (SHiB) contains (middle) passive infrared (PIR) motion detectors coupled with ambient light sensors and (right) magnetic door use detectors coupled with ambient temperature sensors. When there is a change in state, sensors indicate the new state in a text message sent to a central Raspberry Pi. This machine tags the message with the corresponding date, time, and sensor identifier.
Data analysis
A qualitative and quantitative descriptive approach was used to summarize and compare data. Demographic and health survey data were calculated in means and ranges to describe the sample characteristics. PSG records were analyzed for total time in bed (TIB) and total sleep time (TST). Time spent in rapid eye movement (REM) sleep as well non-REM sleep stages (N1, N2, N3) were also calculated. Other commonly reported sleep variables were captured including sleep efficiency (SE) (a ratio of TST over TIB), sleep latency (SL) (the time it takes to fall asleep once in bed), and wake after sleep onset (WASO) periods of wakefulness during the night. PSG data were also analyzed for respiratory events quantified with the apnea-hypopnea index (AHI), a value derived from the number of apnea or hypopnea events per hour of total sleep time. Respiratory events consist of two distinct classes: (1) hypopneas, events characterized by a 30% reduction in airflow for at least 10 seconds, and (2) apneas, events characterized by a 90% reduction of airflow for at least 10 seconds. Apneas were further classified into three subtypes: (1) obstructive apneas, which have sustained respiratory effort throughout the event usually caused by a blocked airway, (2) central apneas, characterized by a cessation of respiratory effort throughout the event, which generally have neurological roots, and (3) mixed apneas, characterized by a cessation of airflow in the first half of the event and a restoration of airflow at the end (Berry et al., 2012).
Due to the pilot nature of using smart home sensors in this population, feasibility of procedures was assessed using participant recruitment and retention data and adherence to protocol (measured in days of attendance and data collection completion during the sleep lab portion of the sub-study). To address our specific aims, we assessed for accuracy with time and event comparisons of polysomnographic data to sensor data. PSG and ambient sensor data were compiled on one single spreadsheet. All data had timestamps. A Python script was written to retrieve and organize each data type in chronological order. A rule was instituted to adjust any simultaneous data points (i.e., same time stamp for a PSG data point and a sensor data point), automatically offsetting them by one second. PSG and sensor data were reviewed by a nurse experienced in interpreting sensor data to assign clinical relevance to sensor data segments. Meaning, the nurse focused on reviewing the ambient sensor data to identify and mark sleep/wake data segments (i.e., marking sleep/wake start and stop times). Three categories of wake/sleep were identified using sensor data: wake, fitful sleep, sleep. Wake cycles were identified as a segment of sensor data showing continuous movement (sensor readings occurring moment-by-moment within seconds of each other) lasting 10 minutes or longer or showing use of the door. Fitful sleep cycles were identified as a segment of sensor data where multiple sensor readings occurred sequentially within seconds of each other followed by a brief period of sensor-quietness followed by another segment of multiple sensor readings (i.e., the sensors were intermittently sensing movement). Sleep cycles were associated with gaps in the time window of sensor events indicating the sensors did not sense any movement.
The nurse then re-reviewed the sensor data focusing on the associated PSG data to determine if markings for the sensor data matched the PSG sleep cycle during the same time periods. Segments of sensor data showing wake or sleep cycles that were not aligned with PSG wake or sleep cycles were highlighted and later reviewed for coherency with the PSG technician. Consensus between the nurse and PSG technician was reached for each instance where the start or stop times of a sleep cycle for each set of data (sensor, PSG) were not aligned. The nurse and technician manually compared sensor and PSG data (using the Excel spreadsheet containing each type of data in chronological order) and quantified the number of sleep changes (e.g., arousals, apnea events) as well as the level of alignment (%) across PSG and sensor data for both nights.
Results
Participant Characteristics
Participant demographics and health characteristics are summarized in Table 1. Two subjects had a chronic back pain diagnosis. All subjects reported a previous mental health disorder including major depression, bipolar disorder, and anxiety. All reported multiple past substances used, including tobacco, marijuana, methamphetamine, and benzodiazepines. On average, participants displayed mild opioid withdrawal symptoms and moderate pain intensity before sleep. Withdrawal symptom scores increased slightly into the “moderate” range after awakening, while pain worsened, falling into a “severe” range.
Table 1.
Participant characteristics (N = 4)
| Measure | Mean | Range |
|---|---|---|
|
| ||
| Age (in years) | 40.6 | 31–60 |
| Body Mass Index (BMI) | 28.1 | 21–38 |
| Daily methadone dose (in milligrams) | 58.8 | 40–85 |
| Clinical Opiate Withdrawal Scale (COWS) first evening | 11.8 | 6–19 |
| Clinical Opiate Withdrawal Scale (COWS) first morning | 14.3 | 5–28 |
| Numeric Pain Intensity Scale first evening | 5.0 | 2–7 |
| Numeric Pain Intensity Scale first morning | 7.3 | 7–8 |
| Adjective Rating Scale for Withdrawal first evening | 66.4 | 63–114 |
| Adjective Rating Scale for Withdrawal first morning | 87.0 | 41–122 |
| Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance baseline | 61.6 | 54–69 |
| Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep-Related Impairment baseline | 66.0 | 61–75 |
Procedures Feasibility
All four participants who consented for the sleep study completed the first night of overnight data collection. One female dropped out of the study before the second night due to gastrointestinal symptoms. An additional eight hours of overnight data were lost to equipment failure; the device receiving the sensor information was mistakenly unplugged. Smart home sensors reliably captured overnight data on 48 hours of a potential 64 hours (75%) from four participants.
PSG Sleep and Respiratory Data
Participant sleep information is summarized in Table 2. Participants’ average apnea-hypopnea index (AHI) was 19.28 (range 2.77–35.01) events per hour, placing subjects within criteria for moderate sleep apnea on average (Berry et al., 2012). One subject scored in the mild range (AHI of 0–5/hour) two subjects scored in moderate range (AHI 15–30/hour) and one subject in the severe range (AHI>30/hour). The distribution of respiratory events is summarized in Table 3. The most common disturbance was central sleep apneas, followed by hypopneas, and obstructive and mixed apneas. The average peripheral arterial oxygen saturation (SaO2) nadir was 78.5% (range 51%–90%). That value was skewed, however, by one person with a particularly low value. With that participant removed, the average peripheral arterial oxygen saturation (SaO2) nadir was 87.7% (range 67%–90%). In both cases, the mean SaO2 nadir fell below the recommended cut off for supplemental oxygen (Kushida et al., 2008).
Table 2.
Participant sleep information (N=4)
| Measure | Mean | Range |
|---|---|---|
|
| ||
| Time in bed (TIB, in hours) | 8.3 | 7.7 – 8.7 |
| Total sleep time (TST, in hours) | 7.2 | 6.7 – 7.9 |
| Sleep efficiency (SE, in minutes as ratio of TST/TIB) | 86.7 | 80.8 – 94.4 |
| Sleep latency (time to fall asleep, in minutes) | 5.9 | .5 – 18.5 |
| Wake after sleep onset (WASO, in minutes) | 60.5 | 24 – 82.5 |
| Stage N1 sleep (in minutes) | 20.3 | 8 – 49.5 |
| Stage N3 sleep (in minutes) | 130.5 | 1 – 146 |
| Rapid Eye Movement (REM) sleep (in minutes) | 76.6 | 5.5 – 209.5 |
| Periodic limb movement series (PLM) | 7.0 | 1 – 17 |
Table 3.
Events included in the AHI* displayed by a mean percentage of total events (N=4)
| Measure | Mean percentage (%) | Range (%) |
|---|---|---|
|
| ||
| Central sleep apneas | 77.4 | 20–97 |
| Hypopneas | 14.1 | 3–80 |
| Obstructive apneas | 6.1 | 0–24.1 |
| Mixed apneas | 2.3 | 0–16 |
AHI*= Apnea-Hypopnea Index. The number of Apnea (central, obstructive, and mixed) and Hypopnea events per hour of total sleep time.
Sensor Sleep Data
For P1, we collected 758 unique sensor readings; for P2: 2,218; for P3: 1,385; for P4: 2,624. P1 had only one night of sleep versus two nights for P2-P4. Ambient sensor data were examined to identify sleep/wake data segments before comparing discoveries with the PSG data. Three categories of wake/sleep were identified using sensor data: wake, fitful sleep, sleep. Wake cycles were associated with a segment of PIR sensor events occurring continuously within seconds of each other and lasting 10 minutes or longer, or showing door use sensor events. Fitful sleep cycles were associated with a segment of sensor data where multiple PIR sensor events occurred sequentially within seconds of each other and were followed by a brief time period of sensor-quietness, followed by another set of PIR sensor events (an ON state). This cycle could repeat multiple times across several minutes, or hours. Sleep cycles were associated with gaps in the time window of sensor events. Meaning, PIR sensors did not sense any movement and therefore did not send an ‘ON’ message. Table 4 illustrates sensor data representing wake, then sleep, and then a fitful sleep cycle for P1 on the first night of sleep lab monitoring alongside of PSG sleep stage data.
Table 4.
Comparison of sensor-based sleep/wake cycles and polysomnography sleep stages
| Date | Time | Sensor ID | State | Categories | Sleep Stage | Agree |
|---|---|---|---|---|---|---|
|
| ||||||
| 2019-11-11 | 21:41:33 | BedroomArea | OFF | Sleep | N1 | Y |
| ... | ||||||
| 2019-11-11 | 22:11:22 | REM | Y | |||
| 2019-11-11 | 22:11:45 | BedroomBed | ON | Awake | Wake | Y |
| 2019-11-11 | 22:11:46 | BedroomBed | ON | Awake | Wake | Y |
| 2019-11-11 | 22:11:48 | BedroomBed | ON | Awake | Wake | Y |
| ... | ||||||
| 2019-11-11 | 22:16:57 | BedroomDoor | ON | Awake | Wake | Y |
| 2019-11-11 | 22:17:05 | BedroomBed | ON | Awake | Wake | Y |
| ... | ||||||
| 2019-11-11 | 22:18:10 | BedroomBed | ON | Awake | Wake | Y |
| 2019-11-11 | 22:18:11 | BedroomBed | OFF | Sleep | Wake | N |
| ... | ||||||
| 2019-11-11 | 23:02:00 | BedroomArea | ON | Sleep | N1 | Y |
| 2019-11-11 | 23:03:00 | BedroomArea | OFF | Fitful | Wake | Y |
| 2019-11-11 | 23:03:42 | BedroomArea | ON | Fitful | Wake | Y |
Note: Ellipses signify uneventful time periods that were removed. Data shown is from one participant in first two hours of sleep opportunity. Smart home sensors generate text readings whenever they internally detect a change in state. Passive infrared sensors sample their state every 0.25 seconds. They generate an “ON” message when heat-based movement is detected and an “OFF” message when movement stops.
PSG and Ambient Sensor Data Comparison
Sleep
PSG and sensor data for sleep versus wake cycles were aligned (in agreement) 89.4% (range 82.3%–98.1%) across all epochs (Figure 2). Data were determined to be aligned if the PSG data indicated a participant was asleep (stage N1-N3 or REM) and the ambient sensors were simultaneously quiet. Similarly, for wake times, when the sensor data indicated a light was on or in the bathroom or the participant was moving around in bed (sensors showed ON), the PSG data also indicated a wake stage. Across all four participants, 51 transitions between sleep and wake were identified. For each of these transitions, PSG and sensor data timestamps were within seconds of each other. Meaning, both data sets’ transition segments were aligned for time and for sleep cycle (asleep versus awake). The number of transitions per participant were: P1=18, P2=11, P3=4, P4=18. All transitions for all participants were first reviewed and marked on the compiled spreadsheet by the nurse and the polysomnographic technician individually and then together. Greater disagreement appeared between ambient sensor and PSG data for sleep cycles than wake cycles. There was 100% agreement for wake times (i.e., before participant fell asleep, after 06:00 the next morning, during bathroom use, and other general wake times during the night).
Figure 2.
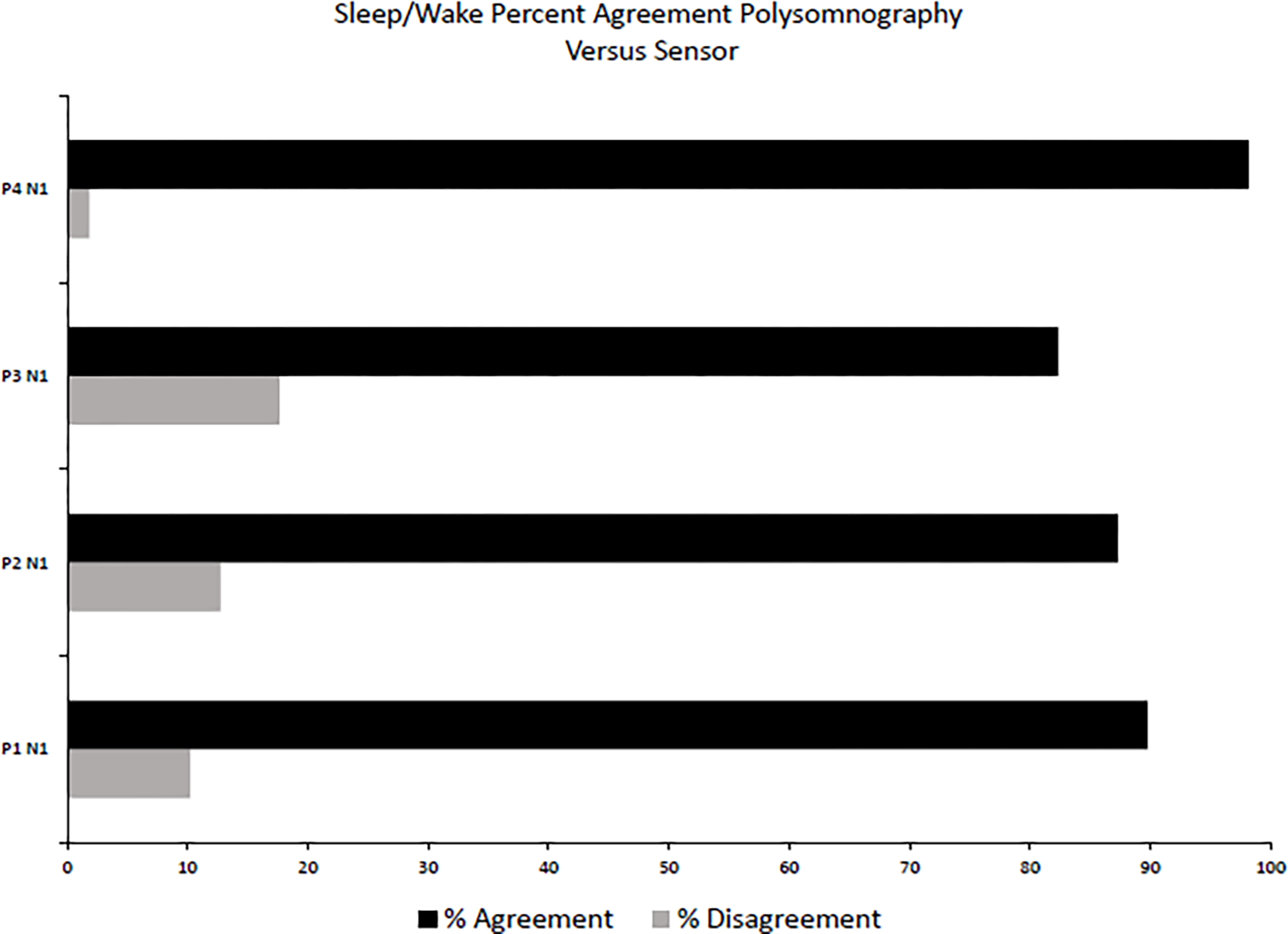
Percent of polysomnography 30 second epochs scored for sleep/wake and ambient sensor events that agree and disagree with each other for participants #P1-P4
Agreement between PSG and sensor detection of episodes of fitful sleep were also calculated. Fitful sleep was defined as intermittent wake times or arousals after initially falling asleep. All four participants experienced fitful sleep that was evidenced in awakenings throughout the night and captured as WASO values with PSG. In the sensor data, initial sleep was identified by a gap in the data (no “ON” motion sensor readings for at least 2 minutes) following a long string of motion readings. PSG data contained a high wakefulness after sleep onset (WASO) value (60.50 minutes, range 24–82.5 minutes) at times that overlapped with sensor detection of fitful sleep, indicating the participants were moving for almost an hour after initially falling asleep.
Respiration
Of the 118 apnea episodes analyzed, ambient sensors were not activated in 116/118 episodes resulting in 1.7% agreement. The participants were motionless during these 116 episodes, thus the apnea episode could not be differentiated from a sleep cycle without relying on PSG (i.e., pulse oximetry SaO2 data). In two apnea episodes (associated with less severe oxygen desaturation; > 80%), sensor readings were present, meaning body extremity movement was detected during the episode. Because the ambient sensors are tuned to detect larger movements, they did not generate readings corresponding to the rise and fall of the chest, so gasping and oxygen re-saturation after desaturation was only detected by PSG in all episodes. When re-saturation triggered arm and leg movements, the ambient sensors consistently detected this. The causal relationship between hypopnea and ambient sensor readings could not be confirmed. P1 experienced the most apnea and hypopnea episodes yet exhibited the least overall movement.
Movement Data
When compared to leg movements detected in PSG data, ambient sensors inconsistently detected PLMs noted in the PSG data and these could not be distinguished from other body movements, therefore, calculating a valid agreement between PLM and sensor data was not possible. In one participant, strong coughing episodes were picked up as movement by the ambient sensors. Simultaneous to reported times of robust coughing in sleep lab record (e.g., “strong coughing”), sensor data were recorded showing the participant moving while remaining in bed. Based on documentation in the sleep lab record, these coughing episodes were strong coughs, likely causing some full body movement, which was sensed. In other cases where coughing reportedly required less effort, such as clearing the throat or chest rise and fall movement associated with respiratory effort, ambient sensors did not report any readings of sensed movement. The magnetic door sensors accurately detected trips to the bathroom and staff entering and exiting the room.
Discussion
In this pilot sample of adults receiving methadone for OUD, data collection was sufficient for determining that smart home ambient sensors could accurately pick up when participants were awake, asleep, and transitioning between sleep and wake. The sensors were able to measure sleep/wake activity in our MOUD population with epoch-by-epoch sleep versus wake agreement at 89.4%. This is comparable to epoch-by-epoch agreement measures in clinical population comparing commercially available wearable devices to PSG (78–88%) (Cook, Prairie, & Plante, 2017). Additionally, sensors showed the ability to detect fitful sleep episodes, a clinically-relevant data point to objectively assess how well medications are managing pain, opioid withdrawal, and related symptoms occurring during sleep. Unlike PSG monitoring, the ambient sensors were not able to accurately specify leg movement or apnea events. Yet, ambient sensors do not require attachment of electrodes, wires, belts, and direct observation by trained personnel, thus offering a less invasive system to capture clinically relevant data.
Notably, the participants displayed moderate opioid withdrawal symptoms and worsening pain, falling into a “severe” range of pain after awakening. Although we did not capture these measurements during the PSG overnight sessions, conceivably, they were responsible for the fitful sleep and multiple awakenings. The burden of withdrawal symptoms has been recognized as an important detractor to OUD recovery (Bell & Strang, 2020) and can also occur if opioids are abruptly stopped when used for pain (St. Marie & Broglio, 2020). The traditional COWS scale (Avery & Taylor, 2019) only captures information at one point in time, although opioid withdrawal symptoms can change throughout the day. Because poorly managed withdrawal symptoms can trigger a return to drug use, a critical need exists to develop more accurate means to determine whether MOUD therapies are performing adequately and when dose adjustments are warranted. Pre-surgery sleep has been correlated with declines in pain symptoms and morphine use post-surgery (Roehrs & Roth, 2017). It has also been identified that PSG results are correlated to risk of return to substance use in detoxified patients with opiate-misuse (Rady et al 2020). More attention seems warranted to examine the usefulness of sleep assessment in the context of opioid use outcomes, particularly when pain co-exists.
The MOUD population is likely to experience sleep respiratory issues. Because ambient sensors did not sense all apnea and hypopnea episodes in our sample, supplemental sensors, such as finger probes that measure overnight oxygenation, could be added to provide additional insights. In this study, sleep efficiency was comparable but N1 and N3 sleep were reduced compared to similarly-aged healthy adults (Mitterling et al., 2015). Time to fall asleep (sleep latency) was normal, yet WASO exceeded the threshold associated with clinical insomnia (AASM, 2014). Participants displayed few obstructive sleep apnea events, suggesting that opioids were a more likely reason for respiratory disturbances than obstructed airway.
Clinical and Research Implications
A barrier to advancing research using pervasive computing and machine learning technologies is the time needed to interpret large real-world datasets and provide associated ground truth, such as activity labels and clinician-verified health events or assessments. However, prior studies indicate that a small amount of sensor data with ground truth labels can be used to train machine learning models to accurately recognize behavior changes related to sleep (Fellger et al., 2020), physical and cognitive function (Aramendi et al., 2018a), and pain (Fritz et al., 2020). Thus, we hypothesized that even small sets of smart home sensor data could help identify OUD symptoms that are known to disrupt sleep (Husak & Bair, 2020). Fitful sleep is clinically recognized as an opioid withdrawal symptom on the COWS, yet is a symptom generally only assessed by self-report in MOUD populations. Our present analysis suggests that smart home sensor data can provide sufficient information for remote assessments of fitful sleep, time to fall asleep, and overall sleep quantity. Therefore, sensors deployed in home settings could, potentially, further both research and objective clinical knowledge regarding responses to MOUD treatment. This information could be particularly useful when people with OUD are initiating treatment, changing dosages, or upon discharge from acute inpatient settings after detoxification when overdose risk is heightened (Bell & Strang, 2020). Still needed are innovations that can provide alert systems for real-time OUD interventions if at-home monitoring is used and machine learning models specific to MOUD populations to reduce time burdens of manual sensor data analysis.
A strength of our study was the ability to capture detailed observations accompanying PSG recordings during monitored hours in the sleep lab. Study limitations include the small sample size and the inability to clarify participant experiences further due to the retrospective analysis. Because we did not receive IRB approval for the sensor sub-study until four participants had already completed their time in the parent study, recruitment was limited to the pool of four people available to participate. All agreed, adding evidence to the acceptability of the procedures. All participants reported high satisfaction with the in-lab experience as detailed in the parent study and the sole dropout on the second study day was due to personal illness (Wilson et. al, 2022). Our data on pain and withdrawal symptoms were captured before and after sleep opportunities so we could not verify conclusively whether symptoms occurring overnight were due to conditions other than opioid withdrawal, such as pain or insomnia. Yet, the population receiving methadone-based MOUD is often difficult to study due to challenges in living situations and complex health status. The inquiry presented here allowed for robust data collection with detailed observations that are rarely possible with populations in MOUD treatment. Although we focused on overnight sleep symptoms and respiratory depression for the sake of this study, pain, anxiety or other symptoms common in the OUD population could also be explored in the future. Future studies can also test how novel in-home data collection strategies can influence treatment options (e.g., MOUD dose adjustments), and how this in turn affects overall OUD outcomes and quality of life. Smart home sensor data can be used to apply behavior change theories in future development and testing. This might lead to more sustained desired changes among OUD or pain populations.
Conclusions
Our present analysis was intended to explore whether smart home sensor data can provide sufficient information that could assist with overnight assessments of OUD responses to treatment. Such data could assist in maximizing treatment benefits and reducing risk for a complex population. We found that smart home ambient sensors consistently picked up when participants were awake, asleep, experiencing fitful sleep, and transitioning in and out of sleep when compared with observed PSG evaluations in a sleep lab setting. This supports future research directions targeting smart home use for potential home monitoring related to sleep length and quality in the OUD population undergoing treatment. Congruent with previous research, we identify sleep and breathing issues in our sample. Apnea and desaturation episodes were present, yet not accurately detected with ambient sensors alone. Withdrawal and pain symptoms were prevalent and worsened from evening to morning. Going forward, we can examine whether insights gleaned from smart home sensors can enhance overnight assessments and, potentially, lead to improving poorly-managed opioid withdrawal symptoms, pain, and disrupted sleep within other populations prescribed opioids. Such innovations could be important in maximizing OUD recovery outcomes, symptom management, and quality of life while reducing opioid-related risks.
Highlights.
Novel solutions are needed to reduce risk among adults prescribed opioids.
Smart home sensors were tested and compared to polysomnography data.
Sensors were sufficiently reliable for unobtrusive sleep/wake pattern detection.
Acknowledgement:
The authors thank Dr. Hans Van Dongen, Professor and Director of the Sleep and Performance Research Center, Spokane WA for his collaboration and use of sleep lab facilities.
Funding:
Research reported in this publication was supported by the Rayce Rudeen Foundation and the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR016732. The content is solely the responsibility of the authors and does not necessarily represent the official views of the affiliations, funding agency, or the National Institutes of Health.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to report.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical Conduct of Research: Participants gave their written consent prior to study participation and were paid for their time. All procedures were reviewed and approved by the Washington State University Institutional Review Board.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- AASM. (2014). International Classification of Sleep Disorders. American Academy of Sleep Medicine. [Google Scholar]
- Aminikhanghahi S, & Cook DJ (2019). Enhancing activity recognition using CPD-based activity segmentation. Pervasive and Mobile Computing, 53, 75–89. doi: 10.1016/j.pmcj.2019.01.004 [DOI] [Google Scholar]
- Aramendi A, Weakley A, Goenaga A, Schmitter-Edgecombe M, & Cook D (2018a). Automatic assessment of functional health decline in older adults based on smart home data. Journal of Biomedical Informatics, 81, 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aramendi A, Weakley A, Schmitter-Edgecombe M, & Cook D, Aztiria A, Basarab A, & Barrenechea M. (2018b). Smart home-based prediction of multi-domain symptoms related to Alzheimer’s disease. Journal of Biomedical and Health Informatics, 22(6), 1720–1731. doi: 10.1109/JBHI.2018.2798062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery J, & Taylor KE (2019). Calculated decisions: Clinical opiate withdrawal scale (COWS). Emergency Medicine Practice, 21(11), CD5–CD6. [PubMed] [Google Scholar]
- Bell J, & Strang J (2020). Medication treatment of opioid use disorder. Biological Psychiatry, 87(1), 82–88. [DOI] [PubMed] [Google Scholar]
- Berry RB, Budhirajan R, Gottleib DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan S, Redline SF, Strohl KP, Davidson SL, & Tangredi MM (2012). Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. Journal of Clinical Sleep Medicine, 8(5), 597–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, & Ellis MS (2017). The prescription opioid epidemic: a review of qualitative studies on the progression from initial use to abuse. Dialogues in Clinical Neuroscience, 19(3), 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DJ, Crandall A, Thomas B, & Krishnan N (2012). CASAS: A smart home in a box. IEEE Computer, 46(7), 62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JD, Prairie ML, & Plante DT (2017). Utility of the Fitbit Flex to evaluate sleep in major depressive disorder: A comparison against polysomnography and wrist-worn actigraphy. Journal of Affective Disorders, 217, 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DJ, Sprint G, Fritz R, & Duncan GE (2018). Using smart city technology to make healthcare smarter. Proceedings of the IEEE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahmen J, & Cook DJ (2021). Indirectly-supervised anomaly detection of clinically-meaningful health events from smart home data. ACM Transactions on Intelligent Systems and Technology, 12(2), 1–18. 10.1145/3439870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn KE, Finan PH, Tompkins DA, & Strain EC (2018). Frequency and correlates of sleep disturbance in Methadone and Buprenorphine-maintained patients. Addictive Behaviors, 76, 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellger A, Sprint G, Weeks D, Crooks E, & Cook DJ (2020). Wearable device-independent next day activity and next night sleep prediction for rehabilitation populations. IEEE Journal of Translational Engineering in Health and Medicine8, 8, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay M, Wilson M, Erwin JA, Hansen DA, Layton ME, Quock RM, Van Dongen HPA (2020). Individuals receiving methadone for medication-assisted treatment of opioid use disorder show evidence of respiratory depression. Sleep, 43(S1), April 2020, A278. 10.1093/sleep/zsaa056.726 [DOI] [Google Scholar]
- Fox LM, Hoffman RS, Vlahov D, & Manini AF (2018). Risk factors for severe respiratory depression from prescription opioid overdose. Addiction, 113(1), 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz R, & Dermody G (2019). A nurse-driven method for developing artificial intelligence in “smart” homes for aging in place. Nursing Outlook, 67(2), 140–153. doi: 10.1016/j.outlook.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz R, Wilson M, Dermody D, Schmitter-Edgecombe M, & Cook DJ (2020). Automated smart home assessment to support pain management. Journal of the American Medical Informatics Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, & Jones CM (2017). Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Annals of Intern Medicine, 167(5), 293–301. 10.7326/M17-0865 [DOI] [PubMed] [Google Scholar]
- Husak AJ, & Bair MJ (2020). Chronic pain and sleep disturbances: A pragmatic review of their relationships, comorbidities, and treatments. Pain Medicine, 21(6), 1142–1152. [DOI] [PubMed] [Google Scholar]
- John WS, & Wu LT (2020). Chronic non-cancer pain among adults with substance use disorders: Prevalence, characteristics, and association with opioid overdose and healthcare utilization. Drug and Alcohol Dependence, 209, 1–9. 10.1016/j.drugalcdep.2020.107902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karcioglu O, Topacoglu H, Dikme O, & Dikme O (2018). A systematic review of the pain scales in adults: Which to use? The American Journal of Emergency Medicine, 36(4), 707–714. 10.1016/j.ajem.2018.01.008 [DOI] [PubMed] [Google Scholar]
- Kushida A, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, & Rowley JA (2008). Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. Journal of Clinical Sleep Medicine, 4(2), 157–171. [PMC free article] [PubMed] [Google Scholar]
- Lee YJ, Lee JY, Cho JH, & Choi JH (2022). Interrater reliability of sleep stage scoring: a meta-analysis. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 18(1), 193–202. 10.5664/jcsm.9538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitterling T, Hogl B, Schownwald S, Hacker H, Gabelia D, Biermayr M, & Frauscher B (2015). Sleep and respiration in 100 healthy Caucasian sleepers - A polysomnographic study according to American Academy of Sleep Medicine Standards. Sleep, 38(6), 867–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan JR, Schackman BR, Leff JA, Linas BP, & Walley AY (2017). Injectable Naltrexone, Oral Naltrexone, and Buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. Journal of Substance Abuse Treatment, 85, 90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odaibo D, Zhang Z, & Skidmore F (2019). Detection of visual signals for pneumonia in chest radiographs using weak supervision, Southeast Con IEEE, 1–5. doi: 10.1109/southeastcon42311.2019.9020631 [DOI] [Google Scholar]
- Petrosky E, Harpaz R, Fowler KA, Bohm MK, Helmick CG, Yuan K,…Betz MS. (2018). Chronic pain among suicide decedents, 2003 to 2014: Findings from the National Violent Death Reporting System. Ann Intern Med. 169, 448–455. doi: 10.7326/M18-0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rady A, Mekky J, Moulokheya T, & Elshshai A (2020). Polysomnographic correlates for the risk of relapse in detoxified opiate-misuse patients. Neuropsychiatric Disease and Treatment, 16, 3187–3196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajpurkar P, Hannun AY, Haghpanahi M (2017). Cardiologist-level arrhythmia detection with convolutional neural networks. URL: http://arxiv.org/abs/1707.01836
- Roehrs TA, & Roth T (2017). Increasing presurgery sleep reduces post surgery pain and analgesic use following joint replacement: a feasibility study. Sleep Medicine, 33, 109–113 [DOI] [PubMed] [Google Scholar]
- Seelye A, Schmitter-Edgecombe M, Cook D, & Crandall A (2013). Naturalistic assessment of everyday activities and prompting technologies in mild cognitive impairment. Journal of the International Neuropsychological Society, 43(3), 820–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey KM, Kurth ME, Corso RP, Brower KJ, Millman RP, & Stein MD (2009). Home polysomnography in methadone maintenance patients with subjective sleep complaints. The American Journal of Drug and Alcohol Abuse, 35(3), 178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skubic M, Guevara RD, & Rantz M (2015). Automated health alerts using in-home sensor data for embedded health assessment. IEEE J Transl Eng Heal Med, 3. doi: 10.1109/JTEHM.2015.2421499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprint G, Cook D, Fritz R, & Schmitter-Edgecombe M (2016a). Using smart homes to detect and analyze health events. Computer, 49(11), 29–37. Featured article. doi: 10.1109/MC.2016.338 [DOI] [Google Scholar]
- Sprint G, Cook D, Fritz R, et al. (2016b). Detecting health and behavior change by analyzing smart home sensor data. In: IEEE International Conference on Smart Computing, SMARTCOMP; 2016. doi:10.1109/SMARTCOMP.2016.7501687 [Google Scholar]
- St Marie B, & Broglio K (2020). Managing pain in the setting of opioid use disorder. Pain Management Nursing, 21(1), 26–34. doi: 10.1016/j.pmn.2019.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2018). MAT medications, counseling and related conditions. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions#medications-used-in-mat
- Tompkins DA, Bigelow GE, Harrison JA, Johnson RE, Fudala PJ, & Strain EC (2009). Concurrent validation of the Clinical Opiate Withdrawal Scale (COWS) and single-item indices against the Clinical Institute Narcotic Assessment (CINA) opioid withdrawal instrument. Drug Alcohol Dependence, 105(1–2), 154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N, Benveniste H, & McLellan AT (2018). Use and misuse of opioids in chronic pain. Annual Review of Medicine, 69, 451–465. 10.1146/annurev-med-011817-044739 [DOI] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Griffin ML, McHugh RK, Haller D, Jacobs P, … Rosen KD (2014). Reasons for opioid use among patients with dependence on prescription opioids: the role of chronic pain. Journal of Substance Abuse Treatment, 47(2), 140–145. doi: 10.1016/j.jsat.2014.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesson DR, & Ling W (2003). The Clinical Opiate Withdrawal Scale (COWS). J Psychoactive Drugs, 35(2), 253–259. doi: 10.1080/02791072.2003.10400007 [DOI] [PubMed] [Google Scholar]
- Williams JA, & Cook D (2017). Forecasting behavior in smart homes based on sleep and wake patterns. Technol Heal Care, 25(1), 89–110. doi: 10.3233/THC-16125519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson M, Bindler R, Stanek K, Layton M, & Quock R (2022). Piloting hyperbaric oxygen therapy for pain and opioid withdrawal symptoms. Pain Management Nursing. Epub ahead of print April 4, 2022. 10.1016/j.pmn.2022.03.001 [DOI] [PubMed] [Google Scholar]
- Wolf DAPS, & Gold M (2020). Treatment resistant opioid use disorder (TROUD): Definition, rationale, and recommendations. Journal of Neurological Science, 411, 116718. [DOI] [PubMed] [Google Scholar]


