Abstract
Introduction
As minimal invasive techniques for depressed calcaneal fracture treatment have become more common, great progress has been achieved with various surgical methods. While these techniques are still currently utilized, new methods have been developed. This study aimed to report the radiologic and clinical outcomes of depressed calcaneal fracture treatment with the “push-out molding” technique and to propose its clinical utility.
Materials and methods
From March 2009 to October 2020, a retrospective study was conducted with 52 patients, who received the “push-out molding” technique to treat depressed intra-articular calcaneal fractures (Sanders type II, III, IV). Exclusion criteria were as follows: patients with bilateral calcaneal fractures, open fractures, and a follow-up period <12 months. Radiologic parameters were assessed at following periods: preoperative, postoperative, 3-month follow-up, and last follow-up. Limitation of range of motion (ROM), subjective satisfaction, and complications were assessed at the last follow-up period. Repeated measures ANOVA was used to analyze values at preoperative, postoperative, 3-month, and last follow-up periods.
Results
Significant differences in the talo-calcaneal angle (p < 0.001), Böhler’s angle (p=<0.001), Gissane’s angle (p = 0.023), distance from the lower cortical border of calcaneus to the anterior (p=<0.001) and posterior (p=<0.001) points of posterior articular surface, calcaneal length (p = 0.019), and talo-calcaneal height (p=<0.001). Postoperatively, the posterior articular surface was well maintained, while 21.2% retained a ROM limitation by 20° or higher. Subjective satisfaction was as follows: excellent (42.3%), good (48.1%), fair (9.6%), and poor (0%).
Conclusion
The “push-out molding” is a simple technique with the advantage of not requiring much force to treat depressed calcaneal fractures. It can be used as a beneficial surgical technique with minimal damage to the soft tissue, owing to the reduction from the depressed interior part and less severe ROM limitation.
Keywords: Calcaneal fracture, Reduction, Push-out molding technique, Minimal invasive operation
1. Introduction
Calcaneal fractures are the most common type of fractures, accounting for about 60% of the fractures of the tarsal bones, of which approximately 70% corresponds to intraarticular fractures [1]. Intra-articular fractures of the calcaneus can lead to stiffness of the subtalar joint, post-traumatic arthritis, and biomechanical changes in the ankle joint due to depression or deformation of the calcaneus. Moreover, it has socioeconomic impacts, including difficulty in returning to work for several years, and poor quality of lives (QOLs) [[2], [3], [4]]. While current radiologic examinations, surgical techniques, and the development of internal fixators have improved clinical outcomes of calcaneal fractures, new techniques are still being introduced [5–11].
Extensile lateral approach and internal fixation with plate and screws are still commonly used as surgical treatments for intra-articular calcaneus fractures. This method has the advantage of being easy to secure the visibility of the posterior articular surface of calcaneus and allowing anatomical reduction of lateral surface of the calcaneus. However, there are risks of complications, such as infection in the surgical window, skin necrosis, scar adhesion, adjacent sural nerve injury, etc. [12] To reduce these complications, the use of minimal invasive techniques is increasing. However, disadvantages of these techniques, such as wound infection, impingement, tendinitis, etc., have also been reported [[5], [6], [7], [8], [9], [10], [11]].
To reduce the complications of conventional extensile approach and plate fixation, we have continued to reduce calcaneus fractures with a minimal invasive technique using a small Ollier incision. In addition to anatomical restoration of the subtalar articular surface and Böhler's angle [7], we hypothesized that it was important to restore the alignment and height of the calcaneus body, and to carry out reduction, and the “push-out molding” technique was used. This study aimed to introduce the “push-out molding” technique and its clinical usefulness by retrospectively analyzing the radiologic and clinical outcomes of patients with intra-articular calcaneus fractures, who had been treated with this method.
2. Patients and methods
2.1. Patients and study design
This study was approved by the Institutional review board of Sanggye Paik Hospital (IRB no. 2021-10-012). From March 2009 to October 2020, among the patients who were treated at our hospital for intra-articular calcaneus fractures corresponding to Sanders type II, type III, and type IV fractures, a total of 52 patients, who could be observed for more than 12 months, were analyzed retrospectively. The following patients were excluded: those with bilateral calcaneus fractures, open fracture, multiple fractures, or tongue-shaped fractures. Minimal invasive open reduction using the “push-out molding” technique was performed with internal fixation using only Kirschner wires (K-wires) or cannulated screws, in all 52 patients. The surgery was performed by a single surgeon (the corresponding author) in all the patients.
2.2. Operative technique and postoperative care
The “push-out molding” technique for treatment of intra-articular calcaneus fractures was performed as follows. Most patients underwent lower extremity regional anesthesia using spinal or epidural anesthesia, while those, who were not indicated for lower extremity regional anesthesia due to a specific underlying disease or spinal surgery, underwent general anesthesia. Patients were placed in the lateral position with a thigh tourniquet inflated to 300 mmHg pressure. After confirming the sinus tarsi and upper end of calcaneus using fluoroscopy, a curvilinear incision was made along the wrinkles of the skin, shorter than 3 cm from the lateral process of talus towards the dorsoanterior direction (Fig. 1). Subsequently, an anterior part of the posterior joint capsule was incised to expose the posterior facet. A depressed posterior facet was lifted and was reduced by insertion and lever, using a freer, or a small, curved curette. The degree of reduction was confirmed by fluoroscopy and by visual inspection. After securing a space in the gap between the bony fragment of the depressed posterior joint surface, the larger curette was inserted carefully through the space, without damaging the joint cartilage. The thick cortex at posteroinferior side of the posterior tuberosity was pushed out with the back side of curette to restore the length and height of the calcaneus. To correct the varus of calcaneus fracture, the end of curette was lifted in the valgus direction. At that time, the lateral wall of the calcaneus, which was protruded due to depression of the calcaneus, was naturally reduced (Fig. 2). A bony defect mostly occurred under the bony fragment of the reduced posterior joint surface due to depression. However, to prevent the delayed depression, allo-bone (Allowash®, cancellous bone cubes) transplantation was performed through a space in which the curette was inserted and fixed with a cannulated screw. Moreover, if the bone fragment of articular surface was small, a K-wire was used to fix it (Fig. 3). After fixation, evaluation of the restoration and position of the fixators was confirmed by fluoroscopic anteroposterior and lateral images of the foot and ankle. Wound closure was performed, and the short leg splint was applied. Sutures were removed after 10–14 days and after short leg cast was applied, while ankle and intrinsic muscle exercises were performed until then. Short leg cast was maintained for 1 month, and the active and passive exercises were performed for the ankle joint. Weight bearing was not allowed for at least 2 months until bone union occurred after surgery, which was followed by gradual weight bearing.
Fig. 1.
Intraoperative photograph; (a) Incision site of the “push-out molding” technique, (b) Reduction by pushing out the posterior tubercle with the curette.
Fig. 2.
Curette was inserted through the space in the gap between the bony fragment and reduction was carried out by pushing out with curette.
Fig. 3.
Allo-bone graft transplantation was performed after reduction at the defective side of the calcaneus body, to prevent delayed collapse and to carry out internal fixation with cannulated screws.
2.3. Outcome evaluation
Radiologic parameters, including talo-calcaneal angle, Böhler’s angle, Gissane’s angle, the distance from inferior cortex of the calcaneus to anterior and posterior points of the depressed posterior articular surface (anterior and posterior heights), length, and talo-calcaneal height, were assessed at preoperative, postoperative, 3-month and the last follow-up periods (Fig. 4).
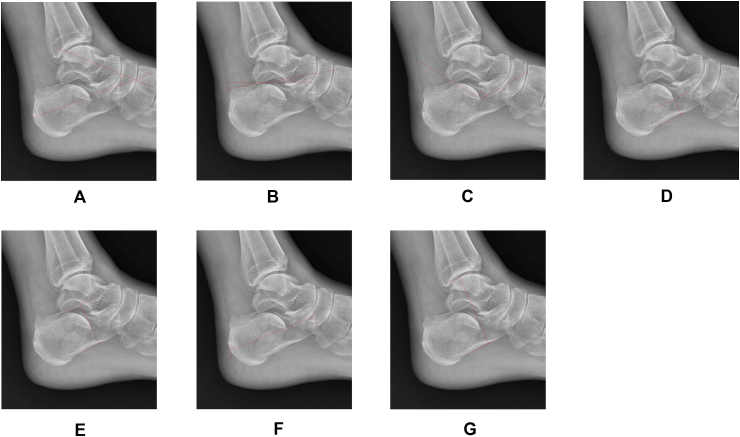
Fig. 4.
Radiologic parameters; (a) Talo-calcaneal angle, (b) Böhler’s angle, (c) Gissane’s angle, (d) Anterior height of the posterior articular surface, (e) Posterior height of the posterior articular surface, (f) Length, (g) Talo-calcaneal height.
At the final follow-up evaluation, a clinical assessment was performed, including assessment of the limitation of range of motion (ROM), subjective satisfaction, and complications with medical records.
2.4. Statistical analysis
The statistical analysis was performed using SPSS ver. 25.0 (IBM Corp., Armonk, NY, SA). Radiologic parameters at each time point were compared using repeated measures ANOVA. Mann-Whitney test was used to compare patient groups according to clinical outcomes, ROM limitation status, and subjective satisfaction. Statistical significance was set at p < 0.05.
3. Results
All demographic data were described in Table 1. The mean age at the time of surgery was 63.1 years. Of all patients, 78.8% were men and 21.2% were women. The right side was involved in 25 patients (48.1%), while the left side was involved in 27 patients (51.9%). The mean body mass index was 23.6. The mean time from the initial examination to the surgery was 3.5. Among 18 patients with type II fractures, 14 had type IIA, 3 had type IIB, and 1 had type IIC fractures. Moreover, among 29 patients with type III fractures, 15 had type IIIAB, 12 had type IIIAC, 2 had type IIIBC fractures. Five patients had type IV fractures.
Table 1.
Demographic data of included patients.
| Variables | Included patients (n = 52) |
|---|---|
| Age (years) | 63.1 ± 13.0 |
| Gender (male:female) | 41:11 (78.8%:21.2%) |
| Affected side (right/left) | 25:27 (48.1%:51.9%) |
| BMI (kg/m2) | 23.6 ± 3.4 |
| Time to surgery (days) | 3.5 ± 3.5 |
Data were presented as mean ± standard deviation or absolute number (percentage).
The talo-calcaneal angle was measured as 35.2° at preoperative, 39.4° at postoperative, 38.1° at 3-month follow-up, and 36.6° at the last follow-up periods. Among the preoperative, postoperative, 3-month, and the last follow-up periods, statistically significant differences were observed (p=<0.001, p = 0.025, p = 0.008). The Böhler’s angle was measured as 8.5° at preoperative, 23.6° at postoperative, 20.5° at 3-month follow-up, and 21.6° at the last follow-up periods. There were significant differences between the preoperative and postoperative periods and between the postoperative and 3-month follow-up periods (p=<0.001, p = 0.019, respectively), while no significant difference was found between 3-month and the last follow-up periods. The Gissane’s angle was measured as 111.5° at preoperative, 106.5° at postoperative, 112.5° at 3-month follow-up, and 109.1° at the last follow-up periods. There was a significant difference between the postoperative and 3-month follow-up periods (p=<0.001), while there were no significant differences among the other periods. Anterior height of posterior articular surface was measured as 18.8 mm at preoperative, 23.4 mm at postoperative, 23.2 mm at 3-month follow-up, and 23.2 mm at the last follow-up periods. There was a significant difference between the preoperative and postoperative periods (p=<0.001), while there were no significant differences among the other periods. Posterior height of posterior articular surface was measured as 38.4 mm at preoperative, 45.1 mm at postoperative, 44.5 mm at 3-month follow-up, and 44.3 mm at the last follow-up periods. There was a significant difference between the preoperative and postoperative periods (p=<0.001), while there were no significant differences among the other periods. The length of calcaneus was measured as 21.5 mm at preoperative, 23.0 mm at postoperative, 22.0 mm at 3-month follow-up, and 21.9 mm at the last follow-up periods. There were significant differences between the preoperative and postoperative and between the postoperative and 3-month follow-up periods (p = 0.046, p = 0.013, respectively), while there was no significant difference between the other periods. Talo-calcaneal height was measured as 65.4 mm at preoperative, 68.7 mm at postoperative, 66.3 mm at 3-month follow-up, and 66.5 mm at the last follow-up periods. There were significant differences between the preoperative and postoperative and between the postoperative and 3-month follow up periods (p=<0.001, p=<0.001, respectively), while there was no significant difference between the other periods (Table 2).
Table 2.
Radiologic measurements at the preoperative, postoperative, 3-month follow-up, and the last follow-up periods.
| Variables | Included patients (n = 52) | P – value |
|---|---|---|
| Talo-calcaneal angle (°) | <0.001 | |
| Preoperative | 35.2 ± 1.1 | *Pre vs Post: <0.001 |
| Postoperative | 39.4 ± 0.9 | *Post vs 3-month: 0.025 |
| 3-month follow-up | 38.1 ± 0.8 | *3-month vs Last: 0.008 |
| Last follow-up | 36.6 ± 0.9 | |
| Böhler angle (°) | <0.001 | |
| Preoperative | 8.5 ± 13.7 | *Pre vs Post: <0.001 |
| Postoperative | 23.6 ± 8.2 | *Post vs 3-month: 0.019 |
| 3-month follow-up | 20.5 ± 8.2 | *3-month vs Last: 0.523 |
| Last follow-up | 21.6 ± 9.2 | |
| Gissane angle (°) | 0.023 | |
| Preoperative | 111.5 ± 14.7 | *Pre vs Post: 0.190 |
| Postoperative | 106.5 ± 11.5 | *Post vs 3-month: <0.001 |
| 3-month follow-up | 112.5 ± 9.3 | *3-month vs Last: 0.008 |
| Last follow-up | 109.1 ± 10.3 | |
| Anterior height of posterior facet (mm) | <0.001 | |
| Preoperative | 18.7 ± 5.0 | *Pre vs Post: <0.001 |
| Postoperative | 23.4 ± 2.2 | *Post vs 3-month: 1.000 |
| 3-month follow-up | 23.2 ± 2.3 | *3-month vs Last: 1.000 |
| Last follow-up | 23.2 ± 2.4 | |
| Posterior height of posterior facet (mm) | <0.001 | |
| Preoperative | 38.4 ± 5.5 | *Pre vs Post: <0.001 |
| Postoperative | 45.1 ± 4.1 | *Post vs 3-month: 0.424 |
| 3-month follow-up | 44.5 ± 4.7 | *3-month vs Last: 1.000 |
| Last follow-up | 44.3 ± 4.8 | |
| Length (mm) | 0.019 | |
| Preoperative | 21.5 ± 4.6 | *Pre vs Post: 0.046 |
| Postoperative | 23.0 ± 4.0 | *Post vs 3-month: 0.013 |
| 3-month follow-up | 22.0 ± 4.4 | *3-month vs Last: 1.000 |
| Last follow-up | 21.9 ± 4.6 | |
| Talo-calcaneal height (mm) | <0.001 | |
| Preoperative | 65.4 ± 5.3 | *Pre vs Post: <0.001 |
| Postoperative | 68.7 ± 6.1 | *Post vs 3-month: <0.001 |
| 3-month follow-up | 66.3 ± 5.8 | *3-month vs Last: 1.000 |
| Last follow-up | 66.5 ± 6.7 |
Data were presented as mean ± standard deviation for each group. P-values were calculated by one-way repeated measures ANOVA test. *Post-hoc analysis was performed by Bonferroni method. Statistical significant threshold was defined as p < 0.05. Last = Last follow-up, N = Number; Post = Postoperative; Pre = Preoperative.
The clinical results at the last follow-up period showed 11 patients (21.2%) with an ROM limitation of 20° or higher, while there was no significant difference in the outcomes of the radiologic parameters between patients with and without ROM limitation. Regarding subjective satisfaction, 22 patients (42.3%) showed excellent, 25 (48.1%) showed good, 5 (9.6%) showed fair, while no patient showed poor satisfaction. There was no significant difference in the outcomes of the radiologic parameters between the satisfied group (excellent and good) and unsatisfied group (fair and poor) (Table 3). No patient showed complications, such as postoperative infection, tendon impingement, tendinitis, neuritis, or nonunion.
Table 3.
Clinical outcomes at the last follow-up.
| Clinical outcomes | All patients (n = 52) |
|---|---|
| ROM limitation | 11 (21.2%) |
| Type I | 0/1 (0%) |
| Type II | 3/17 (17.6%) |
| Type III | 7/29 (24.1%) |
| Type IV | 1/5 (20%) |
| Satisfaction | |
| Excellent | 22 (42.3%) |
| Type I | 0/1 (0%) |
| Type II | 4/17 (23.5%) |
| Type III | 16/29 (55.2%) |
| Type IV | 2/5 (40%) |
| Good | 25 (48.1%) |
| Type I | 1/1 (100%) |
| Type II | 11/17 (64.7%) |
| Type III | 11/29 (37.9%) |
| Type IV | 2/5 (40%) |
| Fair | 5 (9.6%) |
| Type I | 0/1 (0%) |
| Type II | 2/17 (11.8%) |
| Type III | 2/29 (7.9%) |
| Type IV | 1/5 (20%) |
| Poor | 0 (0%) |
| Type I | 0/1 (0%) |
| Type II | 0/17 (0%) |
| Type III | 0/29 (0%) |
| Type IV | 0/5 (0%) |
ROM = Range of motion.
4. Discussion
Lateral extensile approach and plate fixation is considered as the gold standard treatment for intra-articular calcaneus fractures because of its advantage of visualization of fracture site and joint. However, there are risks of complications, such as postoperative skin necrosis and infection, nerve damage, etc. Percutaneous leverage techniques is used to decrease such complications and improve the function signficantly. Baca et al. [13] reported modified percutaneous technique can give good results with a fast, even in contraindication of open reduction. However, wound-related complications (3.02%), need for revision surgery (4.54%) were reported. Minimal invasive approach is also devised to prevent such complications and to secure the field of fracture site [6–11]. “Push-out molding” technique was devised not only to prevent complications but also easily reduce the fracture.
Surgical treatment with minimal invasive technique has also been reported to cause complications, such as postoperative infection, tendon impingement, neuritis, etc. Zhang et al. [7] reported that 12.5% of wound complications, 4.2% of sural nerve injuries, and 4.2% of medial plantar nerve injuries occurred after open reduction using the sinus tarsi approach, while 2.9% of wound complications, 1.5% of sural nerve injuries, and 5.8% of medial plantar nerve injuries occurred after using the minimal invasive longitudinal approach. Kikuchi et al. [8] reported that 13.6% of wound complications occurred after using the limited sinus tarsi approach. Ebraheim et al. [14] reported that 8.5% of wound complications, 3.8% of peroneal tendinitis, 1.8% of tarsal tunnel syndrome, 1.8% of postoperative compartment syndrome, 0.9% of sural neuritis, 0.9% of calcaneofibular impingement occurred after using the sinus tarsi approach. Use of intramedullary locking device (ILD) as minimal invasive technique to treat displaced intraarticular fracture was developed for reducing complications. Bernasconi et al. [15] reported treating displaced intraarticular calcaneal fracture with ILD leads to satisfactory clinical outcomes. However, complication rates ranged between 5 and 30%, with wound infection, nerve entrapment symptoms, metalware irritation, and CRPS.ILD produced favorable clinical outcomes, but complications are still a problem. The “push-out molding” technique is a good surgical method to prevent complications, since no patient has been reported with wound infection, neuritis, or impingement syndrome after surgery (Table 4) [9,11,14,18]. To perform this minimal invasive technique, we used a very short incision and a part of Ollier approach (approximately 3 cm from the lateral process of talus towards the dorsolateral direction, which did not encounter with the peroneal tendon or nerve and incised relatively loose, wrinkled skin and joint capsule, creating a soft tissue window in front of the posterior articular surface to reduce fracture through the anterior aspect of the posterior articular surface). This approach provided a sufficient field of view for anatomical reduction of the depressed bone fragment and reduces damage to the soft tissue, joint ligaments, tendons, and nerves. It is considered to be advantageous for ROM restoration after surgery, because the joint capsule and ligaments are preserved, and less adhesion of the soft tissue occurs. In this study, there were only 11 significant ROM limitations, despite the inclusion of Sander type III and IV fractures.
Table 4.
Comparison of clinical outcomes between the “push-out molding technique” and other reports.
| Variables | Push-out molding technique | Other reports |
|---|---|---|
| Subjective satisfaction | ||
| Excellent (%) | 42.3 (22 cases) | 16.7–55.1 |
| Good (%) | 48.1 (25 cases) | 24.6–50.0 |
| Fair (%) | 9.6 (5 casses) | 9.7–33.3 |
| Poor (%) | 0 | 0–11 |
| Postoperative complications | ||
| Superficial infection (%) | 0 | 0–15.6 |
| Deep infection (%) | 0 | 0–1.3 |
| Impingement (%) | 0 | 0–0.9 |
| Neuritis (%) | 0 | 0–7.8 |
| Tendinitis (%) | 0 | 0–5.6 |
The clinical results of the minimal invasive approach have been reported to be similar to those of the lateral extensile approach. Weber et al. [11] reported 37.5% of excellent, 45.8% of good, 12.5% of fair, and 4.1% of poor patient satisfaction. Zhang et al. [7] reported 52.8% of excellent, 34.7% of good, 9.7% of fair, 2.8% of poor patient satisfaction after using the sinus tarsi approach. In our study, 42.3% of excellent, 48.1% of good, 9.6% of fair, and 0% of poor patient satisfaction was reported. Compared with other studies, the clinical outcomes in patients treated with the “push-out molding” technique were excellent, because of the aforementioned advantages of this method as well as the easy reduction of shape of the calcaneus with less manipulation (Table 4) [[14], [16], [17], [18], [19]].
As the proportion of the cancellous bone in calcaneus is high, bony defects along with delayed collapse may occur even after operation [16]. During the “push-out molding” technique, lifting the anterior depression of the posterior facet fragment and pushing out the posterior tuberosity can cause bony defects at the cancellous portion, which can lead to delayed collapse. To prevent this collapse, allo-bone graft transplantation was performed. Crosby et al. [20] reported that the degree of injury and maintenance of the posterior articular surface of the calcaneus were important determinants of the clinical results of the treatment of calcaneus fractures. Our “push-out molding” technique confirmed that the anterior and posterior heights of the posterior articular surface were well maintained after surgery, with excellent clinical results.
A limitation of this study was that radiologic evaluation conducted at 3-month and last follow-up periods occurred under weight bearing status, while evaluation conducted at the preoperative and postoperative periods were under non-weight bearing status. Therefore, errors in the radiologic analysis could exist. In future, an additional analysis will be needed by performing the radiologic evaluation under same conditions. Furthermore, no other treatment was used besides this “push-out molding” technique. Therefore, comparisons of this technique with other treatments performed by the same operator as well as the clinical results of this study with those of previous reports were not possible.
5. Conclusion
The “push-out molding” technique does not require much force to treat depressed calcaneus fractures, as it uses minimal incision and pushes out from inside of the body of calcaneus to reduce fracture. Additionally, as reduction is well maintained, clinical satisfaction is high, and there are fewer complications, “push-out molding” is considered a useful surgical method.
Declarations
Author contribution statement
Young Jin Choi, MD: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Su-Young Bae, MD, Ph.D.: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
The authors do not have permission to share data.
Declaration of interest’s statement
The authors declare no competing interests.
Additional information
No additional information is available for this paper.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Inje University Sanggye Paik Hospital (IRB no. 2021-10-012) Written informed consent was obtained from the patients for publication of this study and any accompanying images.
Acknowledgements
None.
References
- 1.Talarico L.M., Vito G.R., Zyryanov S.Y. Management of displaced intraarticular calcaneal fractures by using external ring fixation, minimally invasive open reduction, and early weightbearing. J. Foot Ankle Surg. 2004;43:43–50. doi: 10.1053/j.jfas.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Dhillon M.S., Bali K., Prabhakar S. Controversies in calcaneus fracture management: a systematic review of the literature. Musculoskelet. Surg. 2011;95:171–181. doi: 10.1007/s12306-011-0114-y. [DOI] [PubMed] [Google Scholar]
- 3.Tufescu T.V., Buckley R. Age, gender, work capability, and worker's compensation in patients with displaced intraarticular calcaneal fractures. J. Orthop. Trauma. 2001;15:275–279. doi: 10.1097/00005131-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Sanders R. Displaced intra-articular fractures of the calcaneus. J. Bone Joint Surg. Am. 2000;82:225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Swanson S.A., Clare M.P., Sanders R.W. Management of intra-articular fractures of the calcaneus. Foot Ankle Clin. 2008;13:659–678. doi: 10.1016/j.fcl.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Giannini S., Cadossi M., Mosca M., Tedesco G., Sambri A., Terrando S., et al. Minimally-invasive treatment of calcaneal fractures: A review of the literature and our experience. Injury. 2016;47(Suppl 4):S138–S146. doi: 10.1016/j.injury.2016.07.050. [DOI] [PubMed] [Google Scholar]
- 7.Zhang T., Su Y., Chen W., Zhang Q., Wu Z., Zhang Y. Displaced intra-articular calcaneal fractures treated in a minimally invasive fashion: longitudinal approach versus sinus tarsi approach. J. Bone Joint Surg. Am. 2014;96:302–309. doi: 10.2106/JBJS.L.01215. [DOI] [PubMed] [Google Scholar]
- 8.Kikuchi C., Charlton T.P., Thordarson D.B. Limited sinus tarsi approach for intra-articular calcaneus fractures. Foot Ankle Int. 2013;34:1689–1694. doi: 10.1177/1071100713510267. [DOI] [PubMed] [Google Scholar]
- 9.Battaglia A., Catania P., Gumina S., Carbone S. Early minimally invasive percutaneous fixation of displaced intra-articular calcaneal fractures with a percutaneous angle stable device. J. Foot Ankle Surg. 2015;54:51–56. doi: 10.1053/j.jfas.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Kapil Mani K.C., Acharya P., Dirgha Raj R.C., Pangeni B.R., Sigdel A., Marahatta S.B. A modified minimally invasive technique for intra-articular displaced calcaneal fractures fixed by transverse and axial screws. Eur. J. Orthop. Surg. Traumatol. 2017;27:997–1004. doi: 10.1007/s00590-017-1969-x. [DOI] [PubMed] [Google Scholar]
- 11.Weber M., Lehmann O., Sägesser D., Krause F. Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J. Bone Joint Surg Br. 2008;90:1608–1616. doi: 10.1302/0301-620X.90B12.20638. [DOI] [PubMed] [Google Scholar]
- 12.Maskill J.D., Bohay D.R., Anderson J.G. Calcaneus fractures: a review article. Foot Ankle. Clin. 2005;10:463–489. doi: 10.1016/j.fcl.2005.03.002. vi. [DOI] [PubMed] [Google Scholar]
- 13.Baca E, Koluman A. Eklem Hastalik Cerrahisi. Modified percutaneous fixation for displaced intra-articular calcaneal fractures. 19;30:168-174. doi: 10.5606/ehc.2019.66386. [DOI] [PubMed]
- 14.Ebraheim N.A., Elgafy H., Sabry F.F., Freih M., Abou-Chakra I.S. Sinus tarsi approach with trans-articular fixation for displaced intra-articular fractures of the calcaneus. Foot Ankle. Int. 2000;21:105–113. doi: 10.1177/107110070002100203. [DOI] [PubMed] [Google Scholar]
- 15.Bernasconi A., Iorio P., Ghani Y., et al. Use of intramedullary locking nail for displaced intraarticular fractures of the calcaneus: what is the evidence? Arch. Orthop. Trauma Surg. 2022;142:1911–1922. doi: 10.1007/s00402-021-03944-7. [DOI] [PubMed] [Google Scholar]
- 16.Kim K.W., Cho S.G., Lee D.Y. Treatment of displaced intra-articular calcaneal fracture using ollier approach. J. Kor. Foot Ankle. Soc. 2008;12:174–179. [Google Scholar]
- 17.Wiley W.B., Norberg J.D., Klonk C.J., Alexander I.J. "Smile" incision: an approach for open reduction and internal fixation of calcaneal fractures. Foot Ankle. Int. 2005;26:590–592. doi: 10.1177/107110070502600802. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y.M., Cho B.K., Shon H.C., et al. The operative treatment using mini-open sinus tarsi approach for displaced intraarticular calcaneal fractures. J. Kor. Foot Ankle. Soc. 2012;16:247–256. [Google Scholar]
- 19.Mostafa M.F., El-Adl G., Hassanin E.Y., Abdellatif M.S. Surgical treatment of displaced intra-articular calcaneal fracture using a single small lateral approach. Strateg. Trauma Limb. Reconstr. 2010;5:87–95. doi: 10.1007/s11751-010-0082-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crosby L.A., Fitzgibbons T. Computerized tomography scanning of acute intra-articular fractures of the calcaneus. A new classification system. J. Bone Joint Surg. Am. 1990;72:852–859. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.