Abstract
Lack of sleep can affect the health and performance of firefighters. This systematic review and meta-analysis estimated the global prevalence of sleep disorders and poor sleep quality among firefighters and reported associated factors. Four academic databases (Scopus, PubMed, Web of Science, and Embase) were systematically searched from January 1, 2000 to January 24, 2022. These databases were selected as they are known to index studies in this field. The search algorithm included two groups of keywords and all possible combinations of these words. The first group included keywords related to sleep and the second group keywords related to the firefighting profession. The relevant Joanna Briggs Institute checklist was used to evaluate study quality. Data from eligible studies were included in a meta-analysis. In total, 47 articles informed this review. The pooled prevalence of sleep disorders and poor sleep quality in firefighters were determined as 30.49% (95% CI [25.90, 35.06]) and 51.43% (95% CI [42.76, 60.10]), respectively. The results of a subgroup analysis showed that individuals in low- and middle-income countries (LMICs) had a higher prevalence of sleep disorders than those in high-income countries (HICs) but HICs had a higher prevalence of poor sleep quality than LMICs. Various factors, including shift work, mental health, injuries and pain, and body mass index were associated with sleep health. The findings of this review highlight the need for sleep health promotion programs in firefighters.
Keywords: Global prevalence, Sleep disorders, Poor sleep quality, Firefighters, Systematic review, Meta-analysis
Highlights
-
•
The prevalence of sleep disorders in firefighters was determined as 30.49%.
-
•
The prevalence of poor sleep quality in firefighters was determined as 51.43%.
-
•
Individuals in low- and middle-income countries had a higher prevalence of sleep disorders.
-
•
Individuals in high-income countries had a higher prevalence of poor sleep quality.
1. Introduction
Sleep disorders defined as conditions that impairs a person's sleep and prevents their restful sleep [1]. Based on the international classification of sleep disorders (ICSD), types of sleep disorders include insomnia, sleep-related breathing disorders, central disorders of hypersomnolence, circadian rhythm sleep-wake disorders, parasomnias, sleep-related movement disorders, and other sleep disorders [2]. Sleep quality is described as the person's satisfaction across all aspects of the sleep experience which in turn consists of four attributes, these being sleep efficiency, sleep latency, sleep duration, and wake after sleep onset [3]. Sleep disorders can create poor sleep quality [4].
Sleep disorders and poor sleep quality can be associated with serious impacts on an individual's physical and mental performance and productivity. Also, it can disrupt their healthy social relationships [5,6]. Research suggests that sleep deprivation weakens the immune system, decreases hypothalamus, pituitary, and adrenal function, and increases blood pressure [7]. Furthermore, Petrov et al. have highlighted the potential negative impacts of sleep disorders and sleep quality on mental health [8]. In the workplace, workers with sleep disorders have been reported to have significantly more workplace absences, which in turn, increases costs to their employer and society in general [9]. These workers are claimed to possess less self-confidence and lower job satisfaction [10]. Concerningly, research in industrial occupations suggest that sleep disorders and poor sleep quality can increase the risk of workplace accidents [11].
Firefighting is an example of an occupation where personnel work in shifts [12]. As such it is not surprising that it is one of the occupations with a high reported incidence of sleep disorders. The percentage of firefighters reporting sleep disorders ranges from 37% [13] to as high as 70% [14] with multiple percentages reported within this range [[15], [16], [17], [18], [19], [20], [21]]. Factors associated with sleep disorders in firefighters were found to include the aforementioned shift work, but also musculoskeletal disorders, higher body mass index, depression, stress, psychosomatic disorders and post-traumatic stress [13,15,[17], [18], [19], [20], [21]].
The prevalence of sleep disorders and poor sleep quality among firefighters have been found to range widely across various studies with no clear agreement on their prevalence. Furthermore, there is a sparsity of discussion regarding the factors identified as affecting sleep disorders and sleep quality. Therefore, the aims of this systematic review study and meta-analysis were to determine the global prevalence of, and the factors associated with, sleep disorders and poor sleep quality among firefighters. It was hypothesized that the prevalence of sleep disorders and poor sleep quality were higher in firefighters, particularly in those working in low-income countries.
2. Materials and methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22]. The methodology to be followed was reviewed and approved by the Medical Ethics Committee of Kashan University of Medical Sciences (IR.KAUMS.NUHEPM.REC.1400.044).
2.1. Search strategy
Searches of four academic databases (Scopus, PubMed, Web of Science, and Embase) were systematically carried out from January 1, 2000 to January 24, 2022. The search algorithm included two groups of keywords and all possible combinations of these words. The search operator of “AND” was used to combined these two groups of keywords into the search term string. The first group of keywords comprised of terms relating to sleep being. These key words included sleep problem, sleep disorder, sleep disturb, sleep debt, sleep deficien, sleep restrict, sleep depriv, sleep disrupt, sleep paralysis, sleep dysfunction, sleep quality, dyssomnia, parasomnia, restless legs syndrome, RLS, Willis Ekbom disease, periodic limb movement disorder, circadian disorders, narcolepsy, paroxysmal, narcoleptic syndrome, gelineau syndrome, hypersomnia, sleep-wake disorder, shift work sleep disorder, sleep behavior disorder, insomnia, sleep bruxism, sleep apnea, sleep loss, sleep latency, somnolence, sleep apnea syndromes, sleep wake disorders, sleep paralysis, dyssomnias, parasomnias, nocturnal myoclonus syndrome, sleep disorders, circadian rhythm, narcolepsy, disorders of excessive somnolence, sleep initiation and maintenance disorders, sleep latency, sleepiness, and sleep quality. The second group of keywords consisted of terms specific to firefighters. These keywords included firefight, fireman, fire guard, fire, fire service, and firefighter’.
2.2. Eligibility criteria
The following inclusion criteria were applied: a) study reported on a sleep disorder; and b) the study included firefighter populations. No filters for year of publication, age, or sex/gender, were applied. In addition, the following exclusion criteria were applied: a) the article was a review with/without meta-analysis, editorial letter, conference paper, case, or interventional or trial study; b) the article was published in a language other than English, c) the study did not report their inclusion criteria, d) the study did not report prevalence rates, or (e) the study was of poor quality based on the findings of the quality assessment.
2.3. Study selection
All papers identified through the searching of the various databases were entered into Endnote and duplicates were removed. Titles and abstracts of the collated papers were then screened by two reviewers (A.KH and S.Y) independently. Following this step, studies not of relevance to this review were removed. The remaining studies were then subjected to the inclusion and exclusion criteria by two reviewers (A.KH and S.Y). Studies meeting the inclusion criteria but failing to meet the exclusion criteria were retained to inform this review.
2.4. Quality assessment
The Joanna Briggs Institute (JBI) checklist for prevalence studies was used to evaluate the quality of the studies [23] with the evaluation performed by two researchers (A.KH and S.Y). This instrument has nine questions with four response options, including yes, no, unclear, and not applicable. The JBI tool evaluates prevalence studies based on criteria including the appropriateness of sample frame, appropriateness of sampling way, adequacy of sample size, description of study subjects and the setting, sufficiency of data analysis, the validity of used methods, reliability of measurement ways, appropriateness of statistical analysis, and adequacy of response rate. In this study, the number of positive responses were computed, and articles were categorized into three groups, including low quality (scores 1 and 2 out of 9), moderate quality (scores 3–6 out of 9), and high quality (scores 7–9).
2.5. Data extraction
After selecting papers, the required information was extracted by researchers. This information included first author, publication year, country, sample size, gender, study type, job type, age of participants, work experience, prevalence, sleep assessment tool, and related main factors.
2.6. Data analysis
The level of agreement between the two reviewers was computed using Cohen's kappa [24]. The kappa coefficients related to the first and second steps were 0.89 and 0.93, which shows a good agreement between the two reviewers. In most cases, the prevalence estimates in each study were exactly computed, but occasionally estimates were extracted from graphs or calculated using medians. Standard errors of the differences were estimated by available data whenever possible. For heterogeneity, all pooled estimates were evaluated using the Q test and I2 statistics [25]. For the primary outcome, subgroup heterogeneity and a sensitivity analysis were explored. A post hoc sensitivity analysis was also conducted. Q test and I2 statistics were applied to test for meaningful heterogeneity reduction in partitioned subgroups (country classification, study data, sample size, type of sleep assessment tools, and gender). Countries were classified into countries with low and middle income (LMIC) to high income (HIC) based on the world bank categories [26]. Study date and sample size were also divided based on the median value. Types of sleep assessment tools were categorized into four types: Type 1: The Pittsburgh sleep quality index-Epworth sleepiness scale- Epworth daytime sleepiness score; Type 2: insomnia severity index-Athens insomnia scale; Type 3: use of type 1 and type 2; Type 4: other. Genders included male and female. Publication bias was evaluated using visual inspection of the funnel plot and computation of the Begg's linear regression test [27]. Data analyses were performed using STATA 14.2.
3. Results
3.1. Study selection results and basic characteristics
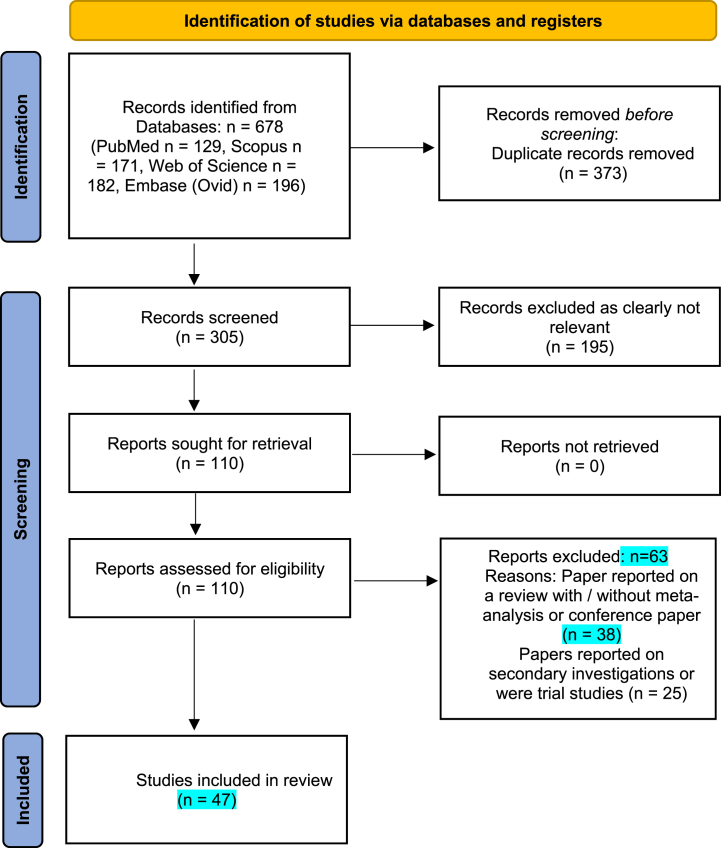
From the initial search, 678 papers were found. Following the removal of 373 duplicate studies, 305 studies remained to be screened by title and abstract. Finally, by eliminating 195 papers that were clearly not relevant to this study (for example ‘The sleep architecture of Australian volunteer firefighters during a multi-day simulated wildfire suppression: impact of sleep restriction and temperature’ [28]), 110 studies were submitted for consideration against the eligibility criteria. Overall, 62 papers were excluded with their reasons recorded (see Fig. 1) leaving 47 papers to inform the meta-analysis. Of these 47 papers, 34 papers reported on the prevalence of sleep disorders, 13 papers on the prevalence of poor sleep quality, and 4 papers on both sleep disorder and poor sleep quality prevalence (Fig. 1). The results from the relevant 47 studies were entered into the meta-analysis (Table 1).
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Table 1.
Characteristics of the studies included in the meta-analysis.
| First author (Year) | Country | Gender | Sample size | Study Type | Job Type | Age of participants | Work experience | Sleep information | Prevalence (%) | Main factor related | Sleep assessment tool | Quality | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smith et al. (2019) [69] | United States | Male-female | 652 | Retrospective Cohort | Career | 38.4 | 13.4 | Sleep disorder | 48.6 | Alcohol misuse, distress tolerance | Pittsburgh sleep quality index | High | ||||
| Angelique Savall et al. (2021) [29] | France | Male -female | 193 | Cross-sectional | Career/Volunteer | 39.1 | NR | Sleep disorder | 16.1 | NR | Pittsburgh sleep quality index, Epworth sleepiness scale and insomnia severity index | High | ||||
| Poor sleep quality | 26.9 | |||||||||||||||
| Wolińska et al. (2017) [70] | Poland | Male | 23 | Cross-sectional | Career | 33 | NR | Sleep disorder | 14.12 | Amount of work hours, coffee drinking | Epworth sleepiness scale- Athens insomnia scale | Moderate | ||||
| Víviam Vargas de Barros (2013) [21] | Brazil | Male-female | 303 | Cross-sectional | Career | 33 | 10 | Sleep disorder | 51.2 | Psychological distress, psychosomatic disturbances | General health questionnaire and sleep disturbances subscale | High | ||||
| Psarros et al. (2018) [71] | Greece | Male | 102 | Cross-sectional | Career | 40 | NR | Sleep disorder | 23.5 | PTSD | Athens insomnia scale | Moderate | ||||
| Reinberg et al. (2013) [72] | France | Male | 30 | Cohort | Career | 37.1 | 17.53 | Sleep disorder | 60 | Shift work | Self-assessments | High | ||||
| Vincent et al. (2020) [73] | Australia | Male -female | 60 | Cross-sectional | Career | 38.4 | 9.5 | Sleep disorder | 7.5 | Frequency of calls | Pittsburgh sleep quality index | Moderate | ||||
| Yun et al. (2015) [51] | South Korea | Female | 515 | Cross-sectional | Career | 38.3 | 10.49 | Sleep disorder | 20.4 | PTSD, stress, depressive symptoms, Chronotype | Pittsburgh sleep quality index | High | ||||
| Shi et al. (2021) [74] | United States | Male -female | 268 | Cross-sectional | Career | 42.95 | 19.91 | Sleep disorder | 42 | Depression, years of professional experiences | Epworth sleepiness scale | Moderate | ||||
| Wagner et al. (2018) [75] | Australia | Male -female | 160 | Case-control | Career | 36.8 | NR | Sleep disorder | 10.5 | NR | Pittsburgh sleep quality index | Moderate | ||||
| Webber et al. (2011) [50] | United States | Male | 10,342 | Retrospective Cohort | Career | 44.2 | NR | Sleep disorder | 36.5 | BMI | Berlin questionnaire | High | ||||
| Wróbel-Knybel et al. (2021) [76] | Poland | Male -female | 831 | Cross-sectional | Career | 35.25 | NR | Sleep disorder | 8.7 | PTSD, stress | Sleep paralysis experience and phenomenology questionnaire | High | ||||
| Wolkow et al. (2019) [20] | United States | Male -female | 6933 | Cross-sectional | Career | 40.4 | NR | Sleep disorder | 6.6 | Burnout | Athens insomnia scale, Berlin questionnaire, and symptoms and treatment questionnaire | High | ||||
| Khumtong and Taneepanichskul1 (2019) [18] | Thailand | Male | 1215 | Cross-sectional | Career | 39.2 | 11.5 | Poor sleep quality | 49.1 | PTSD | Pittsburgh sleep quality index | High | ||||
| Korre et al. (2016) [77] | United States | Male | 400 | Cross-sectional | Career | 47 | NR | Sleep disorder | 20.86 | BMI | Berlin questionnaire | High | ||||
| Kim and Ahn (2021) [78] | South Korea | Male | 297 | Case-control | Career | 38.9 | NR | Sleep disorder | 41.75 | NR | Insomnia severity index | High | ||||
| Park et al. (2019) [79] | South Korea | Male | 287 | Cross-sectional | Career | 40.1 | NR | Sleep disorder | 31.1 | NR | Athens insomnia scale | High | ||||
| Hom et al. (2017) [80] | United States | Male -female | 929 | Cross-sectional | Career | 38.93 | 12.6 | Sleep disorder | 51.9 | NR | Insomnia severity index | High | ||||
| Abbasi et al. (2020) [60] | Iran | Male | 118 | Cross-sectional | Career | 33.30 | 8.35 | Sleep disorder | 50.8 | Musculoskeletal disorders | Insomnia severity index | High | ||||
| Angehrn et al. (2020) [49] | Canada | Male - female | 760 | Cross-sectional | career/volunteer | 18–64 (range) | NR | Sleep disorder | 49 | PTSD, depression, anxiety, social anxiety disorder, panic disorder, alcohol use disorder | Insomnia severity index | High | ||||
| Barger et al. (2015) [16] | United states | Male - female | 6933 | Cross-sectional | Career | 40.40 | 13.7 | Sleep disorder | 37.2 | NR | Sleep disorders screening questionnaires | High | ||||
| Sullivan et al. (2017) [81] | United states | Male - female | 431 | Cohort | Career | 42.70 | 15.65 | Sleep disorder | 41.5 | NR | Sleep disorders screening questionnaires | High | ||||
| Haddock et al. (2013) [81] | United states | Male | 458 | Cohort | Career | 38.2 | 13.8 | Sleep disorder | 18.1 | 48-h work shifts, non-private department sleep areas, working a second job outside the fire service | Epworth sleepiness score | High | ||||
| Hom et al. (2016) [17] | United states | Male-female | 880 | Cross-sectional | Career/volunteer | 18 to 82 (range) | NR | Sleep disorder | 52.7 | NR | Insomnia severity index | High | ||||
| Jang et al. (2020) [44] | South Korea | Male-female | 9738 | Cross-sectional | Career | <40 to >50 | NR | Sleep disorder | 41.8 | Type of job, the frequency of emergency and off-duty work | Insomnia severity index | High | ||||
| Kim et al. (2021) [82] | South Korea | Male-female | 51149 | Cross-sectional | Career | 40.70 | 11.70 | Sleep disorder | 16.1 | PTSD, AUDs, depression | Berlin questionnaire | High | ||||
| Kwak et al. (2020) [45] | South Korea | Male-female | 352 | Prospective before–after | Career | 40.1 | NR | Sleep disorder | 47.16 | NR | Insomnia severity index | High | ||||
| Lim et al. (2020) [83] | South Korea | Male-female | 325 | Cross-sectional | Career | 41.13 | NR | Sleep disorder | 8.48 | Shift work | Pittsburgh sleep quality index, insomnia severity index and Epworth sleepiness scale | High | ||||
| Poor sleep quality | 50.15 | |||||||||||||||
| Lim et al. (2020) [84] | South Korea | Male-female | 602 | Cross-sectional | Career | 30.72 | NR | Sleep disorder | 4 | Caffeine intake, shift work, circadian rhythm type, depression, anxiety, stress and social support | Pittsburgh sleep quality index and insomnia severity index | High | ||||
| Poor sleep quality | 42.4 | |||||||||||||||
| Lim et al. (2020) [85] | South Korea | Male-female | 9788 | Cross-sectional | Career | 39.58 | NR | Sleep disorder | 9.1 | levels of feeling of job loading, levels of physical strength utilization rate, frequency levels of occupational activities, high-intensity leisure-time physical activities |
Insomnia severity index | High | ||||
| Lusa et al. (2002) [65] | Finland | Male | 543 | Cross-sectional | Career | <35 to >54 | NR | Sleep disorder | 61 | Duration of working, alcohol consumption, smoking | Three-levels variable based on two questions | High | ||||
| Lusa et al. (2015) [62] | Finland | Male | 360 | Cohort | Career | 35.7 | NR | Sleep disorder | 41.94 | NR | A self-administered questionnaire (two questions) | High | ||||
| Choi et al. (2020) [86] | South Korea | Male-female | 60 | Cross-sectional | Career | 42.80 | NR | Sleep disorder | 31.65 | Depressive mood and anxiety symptoms | Insomnia severity index and Epworth sleepiness scale | High | ||||
| Cramm et al. (2021) [87] | Canada | Male-female | 1217 | Cross-sectional | Career/volunteer | 18 to 60 < | >4 to 16 < | Sleep disorder | 21.3 | NR | Insomnia severity index and five-point scale of sleep quality | High | ||||
| Poor sleep quality | 69.2 | |||||||||||||||
| Vasconcelos et al. (2021) [88] | Brazil | Male-female | 493 | Cohort | Career | 24.3 | NR | Sleep disorder | 22.1 | NR | Single question on sleep problems | Moderate | ||||
| Stout et al. (2021) [89] | United States | Male -female | 45 | Cross-sectional | Career | 37.4 | NR | Poor sleep quality | 83.95 | Shift work | Pittsburgh sleep quality index and actigraphy | High | ||||
| Mehrdad et al. (2013) [14] | Iran | Male | 379 | Cross-sectional | Career | 33.01 | 9.74 | Poor sleep quality | 69.9 | Having another job, smoking, years of job experience | Pittsburgh sleep quality index | High | ||||
| Hernandez et al. (2017) [90] | United States | Male | 79 | Cross-sectional | Career | NR | NR | Poor sleep quality | 59.5 | NR | Pittsburg sleep quality index | High | ||||
| Demiralp and Özel (2021) [53] | Turkey | Male | 43 | Cross-sectional | Career | NR | NR | Poor sleep quality | 8 | Shift work | Pittsburgh sleep quality index | High | ||||
| Abbasi et al. (2018) [15] | Iran | Male | 118 | Cross sectional study | Career | 33.30 | 8.35 | Poor sleep quality | 59.3 | Musculoskeletal disorders, shift work, BMI, job stress | Pittsburgh sleep quality index | Moderate | ||||
| Oh et al. (2018) [91] | South Korea | Male - female | 120 | Cross-sectional | Career | 38.00 | NR | Poor sleep quality | 52.69 | Alcohol consumption, depression, anxiety, experience of traumatic events | Pittsburgh sleep quality index | Moderate | ||||
| Billings et al. (2016) [43] | United states | Male | 109 | Cross-sectional | Career | 38.0 | 12.70 | Poor sleep quality | 73.4 | Shift work, personal average number of night interruptions at work, working a second job | Pittsburgh sleep quality index | High | ||||
| Carey et al. (2011) [92] | United states | Male-female | 112 | Cross-sectional | Career | 43.6 | 15.5 | Poor sleep quality | 59 | Depression, physical/mental well-being, drinking behaviors (hazardous drinking and caffeine overuse), and age. | Pittsburgh sleep quality index and Epworth sleepiness scale | High | ||||
| Jeong et al. (2019) [93] | South Korea | Male-female | 359 | Cross-sectional | Career | <40 to >50 | NR | Poor sleep quality | 55.4 (Control group) 72.8% (day work) 92.9% (night work) 78.2% (rest day) |
Shift work | Actigraphy and sleep diary | High | ||||
| Kim et al. (2020) [94] | South Korea | Male-female | 1022 | Cohort | Career | 41.77 | NR | Poor sleep quality | 52.45 | NR | Pittsburgh sleep quality index | High | ||||
| Lim et al. (2014) [13] | South Korea | Male | 657 | Cross-sectional | Career | <29 to >50 | <10 to >20 | Poor sleep quality | 48.7 | Shift work, musculoskeletal disorders, depression | Pittsburg sleep quality index | High | ||||
| Marconato and Monteiro (2015) [95] | Brazil | Male | 71 | Cross-sectional | Career | 36.4 | NR | Poor sleep quality | 17.8 | NR | – | Moderate | ||||
NR = Not Reported; PTSD: post-traumatic stress disorder; AUDs: alcohol use disorders; BMI: body mass index.
In total, 28 studies included both male and female participants, while 19 studies included only male participants, and one study only female participants. The majority of the research was carried out in the USA (n = 15 studies) and in South Korea (n = 14 studies). Other countries included Brazil and Iran (n = 3 studies respectively), Australia, Canada, Finland, France, and Poland (n = 2 studies respectively), and Greece, Thailand, and Turkey (n = 1 study respectively).
3.2. Quality assessment
The JBI checklist was used to assess the quality of articles. The results indicated that almost 80% of the included studies were of a high quality, being scores of 7/9 or higher. This suggests that the volume of evidence presented in this review was of high quality.
3.3. Global prevalence of sleep disorders in firefighters
3.3.1. Results of meta-analysis
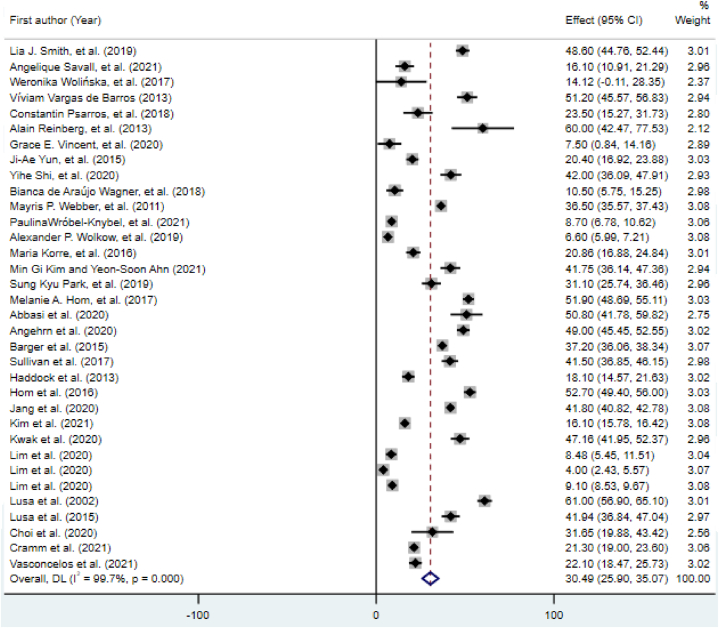
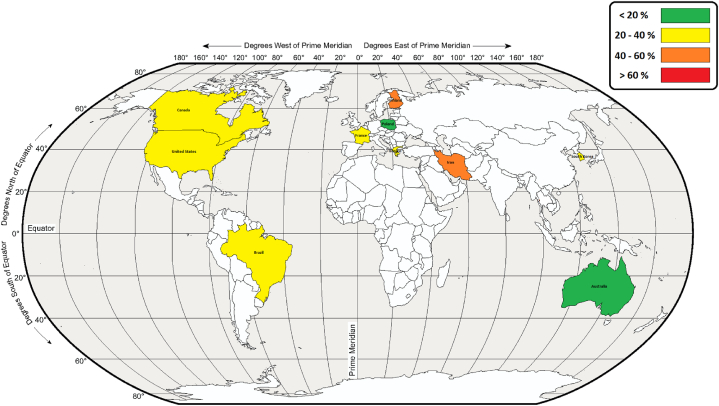
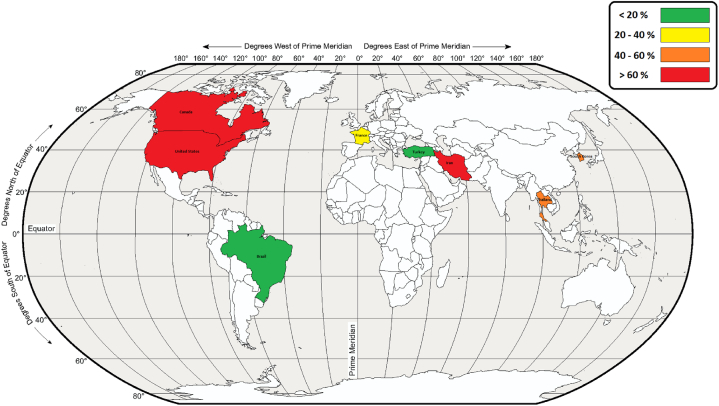
Based on the meta-analysis results, the pooled prevalence of sleep disorders in firefighters was 30.49% (95% CI [25.90, 35.06]; Fig. 2). Fig. 3 shows the global map of prevalence of sleep disorders in various countries. Computation of the Egger's test (t = 2.47, 95% CI [1.53, 16.03], p = 0.019) identified a publication bias.
Fig. 2.
Forest plot of the prevalence of sleep disorders.
Fig. 3.
The global map of prevalence of sleep disorders in various countries.
3.3.2. Results of subgroup analyses
The findings of the subgroup analyses are presented in Table 2. Individuals in LMICs had a higher prevalence of sleep disorders than those in HICs (41.17%, 95% CI [19.15, 63.19] vs. 29.48%, 95% CI [24.70, 34.25]). A significant heterogeneity was seen among the studies, according to the Q test (p < 0.001) and I2 statistics. The sleep disorder prevalence in firefighters is shown in Fig. 2 as a random effects model where the grey box shows the prevalence and the length of the line at which the grey box lies the 95% confidence interval for each study. The diamond sign shows the pooled prevalence globally for all studies.
Table 2.
Subgroup analysis and univariate meta-regression results for the prevalence of sleep disorders.
| Subgroups | Subgroup analysis |
|||||
|---|---|---|---|---|---|---|
| Categories (No. of studies) | Pooled prevalence percentage (95% CIs) | I2 (%) | Q statistic (d.f.) | P-value of heterogeneity | Begg's test z (p) | |
| Country classification (income level) | HICs (n = 31) | 29.48 (24.70–34.25) | 99.7 | 10052.4 (30) | <0.001 | 0.07 (0.946) |
| LMICs (n = 3) | 41.17 (19.15–63.19) | 97.8 | 89.67 (2) | <0.001 | 0.0 (1) | |
| Study date | Before median of 2019 (n = 16) | 36.79 (31.57–42.02) | 98.1 | 776.38 (15) | <0.001 | 1.04 (0.3) |
| Equals median or later (n = 17) | 26.16 (20.90–31.41) | 99.7 | 4927.15 (16) | <0.001 | 0.75 (0.450) | |
| Sample size | Below median: n < 352 (n = 13) | 29.50 (19.84–39.16) | 96.9 | 387.5 (12) | <0.001 | 1.04 (0.3) |
| Median or greater: n = ≥352 (n = 21) | 31.15 (25.44–36.87) | 99.8 | 9814.7 (20) | <0.001 | 0.42 (0.673) | |
| Gender | Female (n = 1) | 20.40 (16.92–23.88) | N/A | N/A | N/A | N/A |
| Male (n = 11) | 36.02 (28.48–43.55) | 97.1 | 346.22 (10) | <0.001 | 0.31 (0.755) | |
| Male- female (n = 22) | 28.31 (23.00–33.63) | 99.7 | 7850.93 (21) | <0.001 | 0.39 (0.693) | |
| Type of sleep assessment tool | Type 1 (7) | 21.94 (9.507–34.374) | 99.1 | 654.00 (6) | 0.001 | 0.15 (0.881) |
| Type 2 (11) | 38.166 (25.110–51.223) | 99.8 | 4545.24 (10) | <0.001 | −1.17 (0.243) | |
| Type 3 (5) | 12.971 (6.513–19.428) | 90.7 | 42.90 (4) | <0.001 | 0.98 (0.327) | |
| Type 4 (11) | 35.395 (26.729–44.061) | 99.7 | 3474.99 (10) | <0.001 | 0.23 (0.815) | |
LMIC = low- and middle-income countries: HIC = high-income countries.
3.3.3. Results of meta-regression
To study the effects of potential parameters on the heterogeneity of sleep disorder prevalence in firefighters, meta-regression was applied for age, the sample size, and year of survey. Univariate meta-regression analysis revealed that mean age (slope = 0.32, p = 0.725), sample size (slope = −0.0001, p = 0.713), and survey year (slope = −1.90, p = 0.153) were not associated with sleep disorder prevalence. According to findings, with the increase in the age of participants the prevalence of sleep disorder in firefighters increases, although not significantly (p = 0.725). Similarly, findings showed that with the increase in the sample size the prevalence of sleep disorder in the firefighters also increased, again not significantly (p = 0.713). Furthermore, with the furthering of the years of the surveys, the prevalence of sleep disorder in firefighters also increased, again not significantly (p = 0.153).
3.4. Global prevalence of poor sleep quality in firefighters
3.4.1. Results of meta-analysis
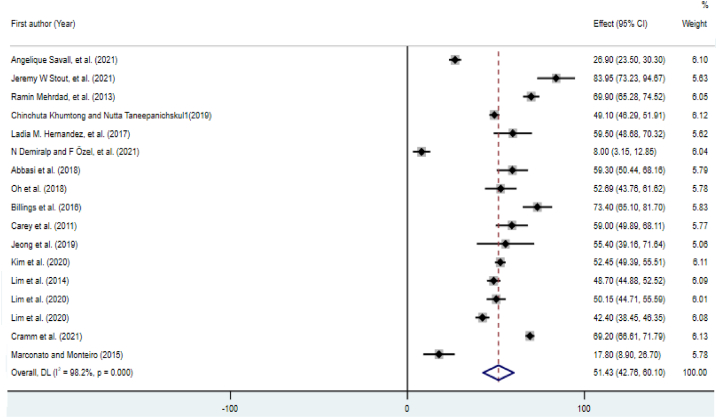
According to the data from 18 studies, the pooled prevalence of poor sleep quality was 51.43% (95% CI [42.76, 60.10]; Fig. 4). Fig. 5 shows the global prevalence of poor sleep quality in various countries. The Begg's test (z = 0.54, p = 0.592) did not identify a publication bias.
Fig. 4.
Forest plot of the prevalence of poor sleep quality.
Fig. 5.
The global map of prevalence of poor sleep quality in various countries.
3.4.2. Results of subgroup analyses
In the subgroup analyses (Table 3), HICs had a higher prevalence of poor sleep quality than LMICs (55.83%, 95% CI [46.61–65.04] vs. 40.85% 95% CI [18.52, 63.19]). A significant heterogeneity was seen among the studies, according to Q test (p < 0.001) and I2 statistics.
Table 3.
Subgroup analysis and meta-regression results for the prevalence of poor sleep quality.
| Subgroups | Subgroup analysis |
|||||
|---|---|---|---|---|---|---|
| Categories (No. of studies) | Pooled prevalence percentage (95% CIs) | I2 (%) | Q statistic (d.f.) | P-value of heterogeneity | Begg's test z (p) | |
| Country classification (income level) | HICs (n = 12) | 55.83 (46.61–65.04) | 97.6 | 467.36 (11) | <0.001 | 1.03 (0.304) |
| LMICs (n = 5) | 40.85 (18.52–63.19) | 99.0 | 388.93 (4) | <0.001 | 0.73 (0.462) | |
| Study date | Before median of 2019 (n = 7) | 52.49 (40.89–64.09) | 95.0 | 119.97 (6) | <0.001 | 0.00 (1) |
| Equals median or later (n = 10) | 50.75 (38.69–62.82) | 98.8 | 759.42 (9) | <0.001 | 0.18 (0.858) | |
| Sample size | Below median: n < 352 (n = 11) | 49.38 (35.22–63.54) | 97.7 | 438.97 (10) | <0.001 | −0.54 (0.586) |
| Median or greater: n = ≥352 (n = 6) | 55.28 (46.23–64.33) | 97.7 | 222.21 (5) | <0.001 | −1.32 (0.188) | |
| Gender | Male (n = 8) | 48.13 (33.43–62.84) | 98.4 | 438.09 (7) | <0.001 | 0.12 (0.902) |
| Male- female (n = 9) | 54.38 (42.85–65.92) | 98.2 | 437.45 (8) | <0.001 | 0.73 (0.466) | |
| Type of sleep assessment tool | Type 1 (12) | 52.608 (42.288–62.929) | 97.8 | 492.51 (11) | <0.001 | 0.41 (0.681) |
| Type 2 (3) | 46.186 (19.455–72.918) | 99.5 | 399.88 (2) | <0.001 | −0.52 (0.602) | |
| Type 3 (1) | 50.150 (44.714–55.586) | N/A | N/A | N/A | N/A | |
| Type 4 (1) | 51.429 (42.762–60.095) | N/A | N/A | N/A | N/A | |
LMIC = low- and middle-income countries: HIC = high-income countries.
3.4.3. Results of meta-regression
Univariate meta-regression analysis showed that mean age (slope = −0.657, p = 0.671), sample size (slope = −0.004, p = 0.172), and survey year (slope = 0.198, p = 0.922) were not associated with the percentage of poor sleepers.
3.4.4. Factors affecting sleep disorders and poor sleep quality in firefighters
To add further context to this paper, the main determinants of sleep disorders and poor sleep quality were reviewed systematically. Some papers (16 papers) investigated the association between sleep disorders/poor sleep quality and medical condition, such as musculoskeletal disorders or mental health, response to traumatic events, distress, and depression. Other papers (17 papers) investigated the association between sleep disorders/poor sleep quality and chronotype, shift work, and other career aspects. The evidence suggests that shift work may be associated with sleep problems and poor sleep quality in firefighters, especially if firefighters are working “out-of-phase” with regard to chronotype.
4. Discussion
Of the initial 678 papers identified in this systematic review, 47 studies from 12 countries spanning 5 continents (North America, South America, Asia, Australia/Oceania, and Europe) were retained. All 47 studies were included in the final meta-analysis, with 34 studies presenting on the prevalence of sleep disorders and 13 studies on the prevalence of sleep quality (4 studies presenting on both sleep disorder and poor sleep quality prevalence). This systematic review and meta-analysis is the first known review that presents a quantitative estimation of subjective sleep disorders and poor sleep quality among firefighters globally.
Sleep disorders are common but stay mainly undiagnosed and untreated in the general population, as well as in firefighters [16,29]. Furthermore, sleep disorders among firefighters are considered to be greater than that found in the general population [21,30]. However, the quantitative synthesis performed in the current study shows that the global pooled prevalence of sleep disorders was 30.49% (95% CI [25.90, 35.06]). These data are lower than those found in some populations but higher than those in others. In health care personnel. For example, the percentage of sleep disturbances in Italian nurses facing COVID-19 has been reported at 71.4% [31] and in Pakistani nurses at 74.9% [32]. Conversely, the percentage of sleep disorders among female and male Egyptian public officials were found to be lower at 26.2% and 14.5% [33]. Similar to the results of this study, a comprehensive study by Barger et al. (2015) about sleep disorder screening program in firefighters found that 37.2% of firefighters reported symptoms in accordance with at least one sleep disorder. In that study the most prevalent sleep disorders were obstructive sleep apnea (OSA), followed by shift work disorder, insomnia, and restless legs syndrome [16].
Considering the above findings of differences in prevalence, the pooled prevalence of sleep disorders in this review was found to be considerably higher in LMICs (41.17%) than in HICs (29.48%). An explanation for these results can follow that key cultural, demographic, geographical, and health factors may tend towards lower population risk in HICs [34]. This supposition is supported by previous global reviews which found higher rates of sleep disorders in LMICs [[34], [35], [36]]. Support for the findings of this review can be drawn from a cross-sectional survey conducted of 16,680 residents who were 65 years old or older in catchment areas of Cuba, the Dominican Republic, Peru, Venezuela, Mexico, China, India, and Puerto Rico. The prevalence of sleep complaints in that study ranged from 9.1% (China) to 37.7% (India) [35]. The higher rates of sleep disorders in LMICs can be due to a number of reasons ranging from the number firefighter facilities to the number of firefighter personnel and the number of fire incidents attended. In HICs, the firefighting facilities and available equipment are present in greater numbers than in LMICs, reducing the number of fires attended by individual firefighters [37]. This exposure to fire incidence attendance is further reduced by the generally higher number of personnel in HIC. As such, the higher pooled prevalence in LMICs highlights the importance of considering sleep disorders as a public health concern, especially in LMICs who already face challenges imparted by communicable and nutritional deficiency diseases. These LMIC impacts are seen in other occupations as well. For example, a scoping review of healthcare employees during the COVID-19 pandemic in LMICs reported that insomnia and poor sleep quality were common in healthcare employees [38]. The differences in prevalence between income country categories, highlights the importance of considering the research in the context of the countries the findings were drawn from and highlights the strengths of this review in which studies were drawn from 5 continents.
In regard to sleep quality, the data reported in this review identified that firefighters presented with a concerning level of poor sleep quality with more than half (51.43%) making a complaint in this regard. This reported prevalence of poor sleep quality is higher than the prevalence observed in frontline health professionals (18.4%) [39] and in workers who came back to work during the COVID-19 pandemic (14.9%) [40], but lower than that reported in the nursing staff (61%) [41]. Furthermore, in contrast to the prevalence findings for sleep disorders, the pooled prevalence of poor sleep quality was largely higher in HICs (55.83%) than in LMICs (40.85%). These findings may have been due to several factors such as higher levels of substance use, psychological stress, and access to and consumption of caffeinated beverages, all of which can affect sleep quality [34,42].
Several studies [[43], [44], [45]] have reported that work seniority was correlated with higher sleep quality, the results indicating that adaptive mechanisms and strategies might intervene. However, shift work was found to lead to poorer sleep outcomes [[43], [44], [45]]. Polysomnographic surveys have shown the existence of a relationship of dose-response between shift work duration and the frequency of changing sleep patterns [46,47]. These findings are supported by the work of Lim et al. [13] who identified a significant relationship between sleep disorders and musculoskeletal disorders, depression, and shift work. As such, the evidence in relation to sleep quality and seniority and shift work is of note given that firefighters present as a population at increased risk of sleep disorders. These findings inform the importance of, and potential approaches to, sleep health promotion programs in firefighters. These programs can be included in already successful healthy lifestyle studies being conducted with firefighters [48] and can be especially helpful for firefighters at the beginning of their occupation and for those on evening/night shift.
Chronic exposure to routine stressors encountered in the firefighters’ general work environment was observed to be largely associated with poor sleep quality and sleep disorders [20,49,50]. This chronicity is of concern, given associations between poor sleep quality and mental health. For example, De Barros et al. in a study on 303 firefighters, reported that sleep disturbances were significantly associated with psychological distress and psychosomatic disturbances [21]. Likewise, Khumtong et al. found that poor sleep quality were associated with post-traumatic stress symptoms (PTSD) [18]. This report, in agreement with findings presented by other authors [15,51], suggests that stress associated with routine and ongoing operations can be more detrimental to the health of the firefighters than exposure to a single stressful event: A finding that may be of benefit to health promotion program content.
There are some data indicating that good sleep quality can protect the human body from a variety of metabolic and nutritional disorders [52]. Demiralp and Özel reported that poor sleepers in Turkish firefighters presented with a higher prevalence of metabolic syndrome (MetS) than mine industry workers [53]. Research confirms that sleep deprivation has a causal association with weight gain. Insomnia, for example, can lead to obesity through fatigue and subsequent decreased physical activity [54]. At a higher order level, brain activity (frontal cortex) has been noted to increase in response to food stimuli in people with chronic sleep deprivation [55]. Thus, it is not surprising that higher BMIs are associated with poorer sleep quality among firefighters [15,29,[56], [57], [58]], and, given that BMI is associated with MetS, that MetS prevalence in firefighters with poor sleep quality is high [53].
Musculoskeletal disorders (MSDs) are a notable concern for firefighters [59]. As such, findings that report connections between MSDs and sleep disorders in firefighters are of note [15,[60], [61], [62]]. While the associations between MSDs and sleep disorders were only found in relation to sleep quality and low back pain, sleep disorders can worsen pain and inflammatory processes through a reduction in endogenous pain inhibitors which occurs as insomnia severity increases [63]. Hence the findings by Salazar et al. [64] who reported that people with pain-related sleep disorders are remarkably more disabled. Considering the findings of relationships between MSDs, pain and sleep, there is also a complicated mutual relationship between mental health parameters (stress and depression) and occupational MSDs [15,65]. Research by Kim et al. [66], as an example, found that both occupational stress and MSDs were prevalent in firefighters. The co-existence of these factors, being MSDs, pain, occupational stress and depression, and sleep pattern can act in synergy to impact on firefighter wellness. Therefore, health and wellbeing interventions that target any of these factors may be of benefit to firefighters sleep quality and improve life quality [67,68]. As a limitation to this review, most of the studies were conducted in developed countries whereas sleep disorders and associated concerns may be greater in developing countries with low or medium incomes, Africa in particularly. Further limitations include the limited number of cohort studies compared to cross sectional studies.
5. Conclusion
The findings of this systematic review with meta-analysis, which consisted of generally high quality (80%+) research papers from across 5 continents, identified that the global prevalence of poor sleep quality in firefighters was high with sleep disorders considerably higher in LMICs than in HICs but poor sleep quality considerably higher in HICs than in LMICs. Sleep disorders and poor sleep quality are a notable and relevant concern among firefighters and can cause considerable damage to both their health and physical wellbeing. As such, it is recommended that sleep health promotion programs are provided to firefighters and should be implemented at the beginning of their occupation and reinforced for those on evening/night shift. Likewise, reducing MSDs, pain management and optimizing mental health may feed into, and be an outcome of, sleep health promotion programs. Thus, the volume of evidence in this review suggests that the sleep health (and subsequent health and wellbeing) of firefighters should be addressed from both a public and occupational health perspective (e.g., BMI, mental health, shift work planning, etc.) and an occupational medicine perspective (e.g., reducing MSDs and pain).
Ethics approval and consent to participate
The methodology to be followed was reviewed and approved by the Medical Ethics Committee of Kashan University of Medical Sciences (IR.KAUMS.NUHEPM.REC.1400.044).
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
Amir Hossein Khoshakhlagh was supported by Kashan University of Medical Sciences [IR.KAUMS.NUHEPM.REC.1400.044].
Data availability statement
Data will be made available on request.
Declaration of interest’s statement
The authors declare no conflict of interest.
Acknowledgment
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e13250.
Contributor Information
Amir Hossein Khoshakhlagh, Email: ah.khoshakhlagh@gmail.com.
Saleh Al Sulaie, Email: smsulaie@uqu.edu.sa.
Saeid Yazdanirad, Email: saeedyazdanirad@gmail.com.
Robin Marc Orr, Email: rorr@bond.edu.au.
Hossein Dehdarirad, Email: dehdari.hossein@gmail.com.
Alireza Milajerdi, Email: miljerdi.a@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Hombali A., et al. Prevalence and correlates of sleep disorder symptoms in psychiatric disorders. Psychiatr. Res. 2019;279:116–122. doi: 10.1016/j.psychres.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Sateia M.J. International classification of sleep disorders. Chest. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 3.Nelson K.L., Davis J.E., Corbett C.F. Nursing Forum. Wiley Online Library; 2022. Sleep quality: an evolutionary concept analysis. [DOI] [PubMed] [Google Scholar]
- 4.Khalladi K., et al. Inter-relationship between sleep quality, insomnia and sleep disorders in professional soccer players. BMJ Open Sport Exerc. Med. 2019;5(1):e000498. doi: 10.1136/bmjsem-2018-000498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wells M.E., Vaughn B.V. Poor sleep challenging the health of a nation. Neurodiagn. J. 2012;52(3):233–249. [PubMed] [Google Scholar]
- 6.Swanson L.M., et al. Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J. Sleep Res. 2011;20(3):487–494. doi: 10.1111/j.1365-2869.2010.00890.x. [DOI] [PubMed] [Google Scholar]
- 7.Han K.S., Kim L., Shim I. Stress and sleep disorder. Exp. Neurobiol. 2012;21(4):141. doi: 10.5607/en.2012.21.4.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petrov M.E., Lichstein K.L., Baldwin C.M. Prevalence of sleep disorders by sex and ethnicity among older adolescents and emerging adults: relations to daytime functioning, working memory and mental health. J. Adolesc. 2014;37(5):587–597. doi: 10.1016/j.adolescence.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Rosekind M.R., et al. The cost of poor sleep: workplace productivity loss and associated costs. J. Occup. Environ. Med. 2010:91–98. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- 10.Afonso P., Fonseca M., Teodoro T. Journal of Public Health; Oxford, England): 2021. Evaluation of Anxiety, Depression and Sleep Quality in Full-Time Teleworkers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uehli K., et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med. Rev. 2014;18(1):61–73. doi: 10.1016/j.smrv.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Orr R.M., Bennett J.R. NSCA's Essentials of Tactical Strength and Conditioning. Human Kinetics; 2017. Wellness interventions in tactical populations; pp. 551–562. [Google Scholar]
- 13.Lim D.-K., et al. Factors related to sleep disorders among male firefighters. Ann. Occup. Environ. Med. 2014;26(1):1–8. doi: 10.1186/2052-4374-26-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehrdad R., Haghighi K.S., Esfahani A.H.N. Sleep quality of professional firefighters. Int. J. Prev. Med. 2013;4(9):1095. [PMC free article] [PubMed] [Google Scholar]
- 15.Abbasi M., et al. Sleep and Hypnosis; 2018. Factors Affecting Sleep Quality in Firefighters. [Google Scholar]
- 16.Barger L.K., et al. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J. Clin. Sleep Med. 2015;11(3):233–240. doi: 10.5664/jcsm.4534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hom M.A., et al. The association between sleep disturbances and depression among firefighters: emotion dysregulation as an explanatory factor. J. Clin. Sleep Med. 2016;12(2):235–245. doi: 10.5664/jcsm.5492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khumtong C., Taneepanichskul N. Posttraumatic stress disorder and sleep quality among urban firefighters in Thailand. Nat. Sci. Sleep. 2019;11:123. doi: 10.2147/NSS.S207764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pagnin D., et al. The relation between burnout and sleep disorders in medical students. Acad. Psychiatr. 2014;38(4):438–444. doi: 10.1007/s40596-014-0093-z. [DOI] [PubMed] [Google Scholar]
- 20.Wolkow A.P., et al. Associations between sleep disturbances, mental health outcomes and burnout in firefighters, and the mediating role of sleep during overnight work: a cross-sectional study. J. Sleep Res. 2019;28(6) doi: 10.1111/jsr.12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vargas de Barros V., et al. Mental health conditions, individual and job characteristics and sleep disturbances among firefighters. J. Health Psychol. 2013;18(3):350–358. doi: 10.1177/1359105312443402. [DOI] [PubMed] [Google Scholar]
- 22.Page Matthew J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;(n71):372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma L.-L., et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil. Med. Res. 2020;7(1):1–11. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pérez J., et al. Systematic literature reviews in software engineering—enhancement of the study selection process using Cohen's kappa statistic. J. Syst. Software. 2020;168 [Google Scholar]
- 25.Ruppar T. Meta-analysis: how to quantify and explain heterogeneity? Eur. J. Cardiovasc. Nurs. 2020;19(7):646–652. doi: 10.1177/1474515120944014. [DOI] [PubMed] [Google Scholar]
- 26.Yu W., et al. Mapping access to basic hygiene services in low-and middle-income countries: a cross-sectional case study of geospatial disparities. Appl. Geogr. 2021;135 [Google Scholar]
- 27.Lin L., et al. Empirical comparison of publication bias tests in meta-analysis. J. Gen. Intern. Med. 2018;33(8):1260–1267. doi: 10.1007/s11606-018-4425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cvirn M.A., et al. The sleep architecture of Australian volunteer firefighters during a multi-day simulated wildfire suppression: impact of sleep restriction and temperature. Accid. Anal. Prev. 2017;99:389–394. doi: 10.1016/j.aap.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Savall A., et al. Sleep quality and sleep disturbances among volunteer and professional French firefighters: FIRESLEEP study. Sleep Med. 2021;80:228–235. doi: 10.1016/j.sleep.2021.01.041. [DOI] [PubMed] [Google Scholar]
- 30.Szubert Z., Sobala W. Health reason for firefighters to leave their job. Med. Pr. 2002;53(4):291–298. [PubMed] [Google Scholar]
- 31.Simonetti V., et al. Anxiety, sleep disorders and self‐efficacy among nurses during COVID‐19 pandemic: a large cross‐sectional study. J. Clin. Nurs. 2021;30(9–10):1360–1371. doi: 10.1111/jocn.15685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arif I., et al. Sleep disorders among rotating shift and day-working nurses in public and private sector hospitals of peshawar. J. Dow Univer. Heal. Sci.(JDUHS) 2020;14(3):107–113. [Google Scholar]
- 33.Eshak E.S. The prevalence and determining factors of sleep disorders vary by gender in the Egyptian public officials: a large cross-sectional study. Bull. Natl. Res. Cent. 2022;46(1):1–10. [Google Scholar]
- 34.Simonelli G., et al. Sleep health epidemiology in low and middle-income countries: a systematic review and meta-analysis of the prevalence of poor sleep quality and sleep duration. Sleep Health. 2018;4(3):239–250. doi: 10.1016/j.sleh.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Mazzotti D.R., et al. Prevalence and correlates for sleep complaints in older adults in low and middle income countries: a 10/66 Dementia Research Group study. Sleep Med. 2012;13(6):697–702. doi: 10.1016/j.sleep.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Manzar M.D., et al. Prevalence of poor sleep quality in the Ethiopian population: a systematic review and meta-analysis. Sleep Breath. 2020;24(2):709–716. doi: 10.1007/s11325-019-01871-x. [DOI] [PubMed] [Google Scholar]
- 37.Valentine N.N., Bolaji W.A. Fire disaster preparedness among residents in a high income community. Int. J. Disas. Manag. 2021;4(2):23–32. [Google Scholar]
- 38.Moitra M., et al. Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for LMICs. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.602614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou Y., et al. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front. Psychiatr. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang Y., et al. Prevalence and associated factors of poor sleep quality among Chinese returning workers during the COVID-19 pandemic. Sleep Med. 2020;73:47–52. doi: 10.1016/j.sleep.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zeng L.-N., et al. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behav. Sleep Med. 2020;18(6):746–759. doi: 10.1080/15402002.2019.1677233. [DOI] [PubMed] [Google Scholar]
- 42.Lemma S., et al. The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and khat use among Ethiopian college students. Sleep Dis. 2012;2012 doi: 10.1155/2012/583510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Billings J., Focht W. Firefighter shift schedules affect sleep quality. J. Occup. Environ. Med. 2016;58(3):294–298. doi: 10.1097/JOM.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 44.Jang T.W., et al. The relationship between the pattern of shift work and sleep disturbances in Korean firefighters. Int. Arch. Occup. Environ. Health. 2020;93(3):391–398. doi: 10.1007/s00420-019-01496-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwak K., et al. Association between shift work and neurocognitive function among firefighters in South Korea: a prospective before–after study. Int. J. Environ. Res. Publ. Health. 2020;17(13):1–15. doi: 10.3390/ijerph17134647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nalan K. Effect of sleep quality on psychiatric symptoms and life quality in newspaper couriers. Nöro Psikiyatri Arşivi. 2016;53(2):102. doi: 10.5152/npa.2015.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Monk T.H., et al. Polysomnographic sleep and circadian temperature rhythms as a function of prior shift work exposure in retired seniors. Healthy Aging & Clin. Care Elder. 2013;2013(5):9. doi: 10.4137/HACCE.S11528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elliot D.L., et al. The PHLAME (Promoting Healthy Lifestyles: alternative Models' Effects) firefighter study: outcomes of two models of behavior change. J. Occup. Environ. Med. 2007:204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 49.Angehrn A., et al. Sleep quality and mental disorder symptoms among Canadian public safety personnel. Int. J. Environ. Res. Publ. Health. 2020;17(8):14. doi: 10.3390/ijerph17082708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Webber M.P., et al. Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center-exposed rescue/recovery workers. Sleep Breath. 2011;15(3):283–294. doi: 10.1007/s11325-010-0379-7. [DOI] [PubMed] [Google Scholar]
- 51.Yun J.-A., et al. The relationship between chronotype and sleep quality in Korean firefighters. Clin. Psychopharm. Neurosci. 2015;13(2):201. doi: 10.9758/cpn.2015.13.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vorona R.D., et al. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch. Intern. Med. 2005;165(1):25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 53.Demiralp N., Özel F. Evaluation of metabolic syndrome and sleep quality in shift workers. Occup. Med. 2021;71(9):453–459. doi: 10.1093/occmed/kqab140. [DOI] [PubMed] [Google Scholar]
- 54.Keith S.W., et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int. J. Obes. 2006;30(11):1585–1594. doi: 10.1038/sj.ijo.0803326. [DOI] [PubMed] [Google Scholar]
- 55.Crispim C.A., et al. Relationship between food intake and sleep pattern in healthy individuals. J. Clin. Sleep Med. 2011;7(6):659–664. doi: 10.5664/jcsm.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaipust C.M., et al. Sleep, obesity, and injury among US male career firefighters. J. Occup. Environ. Med. 2019;61(4):e150–e154. doi: 10.1097/JOM.0000000000001559. [DOI] [PubMed] [Google Scholar]
- 57.Kleiser C., et al. Potential determinants of obesity among children and adolescents in Germany: results from the cross-sectional KiGGS Study. BMC Publ. Health. 2009;9(1):1–14. doi: 10.1186/1471-2458-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seegers V., et al. Short sleep duration and body mass index: a prospective longitudinal study in preadolescence. Am. J. Epidemiol. 2011;173(6):621–629. doi: 10.1093/aje/kwq389. [DOI] [PubMed] [Google Scholar]
- 59.Orr R.M., et al. A profile of injuries sustained by firefighters: a critical review. Int. J. Environ. Res. Publ. Health. 2019;16(20):3931. doi: 10.3390/ijerph16203931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abbasi M., et al. Prevalence of musculoskeletal disorders in firefighters and its association with insomnia. Pol. Pract. Health Saf. 2020;18(1):34–40. [Google Scholar]
- 61.Alsaadi S.M., et al. Detecting insomnia in patients with low back pain: accuracy of four self-report sleep measures. BMC Muscoskel. Disord. 2013;14(1):1–9. doi: 10.1186/1471-2474-14-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lusa S., et al. Sleep disturbances predict long-term changes in low back pain among Finnish firefighters: 13-year follow-up study. Int. Arch. Occup. Environ. Health. 2015;88(3):369–379. doi: 10.1007/s00420-014-0968-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tang N.K., et al. Deciphering the temporal link between pain and sleep in a heterogeneous chronic pain patient sample: a multilevel daily process study. Sleep. 2012;35(5):675–687. doi: 10.5665/sleep.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salazar A., et al. Preventing chronic disease; Spain: 2014. Peer Reviewed: Association of Painful Musculoskeletal Conditions and Migraine Headache with Mental and Sleep Disorders Among Adults with Disabilities; p. 11. 2007–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lusa S., et al. Perceived physical work capacity, stress, sleep disturbance and occupational accidents among firefighters working during a strike. Work. Stress. 2002;16(3):264–274. [Google Scholar]
- 66.Kim M.G., et al. Relationship between occupational stress and work-related musculoskeletal disorders in Korean male firefighters. Ann. Occup. Environ. Med. 2013;25(1):1–7. doi: 10.1186/2052-4374-25-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chang J.-H., et al. Association between sleep duration and sleep quality, and metabolic syndrome in Taiwanese police officers. Int. J. Occup. Med. Environ. Health. 2015;28(6):1011. doi: 10.13075/ijomeh.1896.00359. [DOI] [PubMed] [Google Scholar]
- 68.Garbarino S., et al. Sleep quality among police officers: implications and insights from a systematic review and meta-analysis of the literature. Int. J. Environ. Res. Publ. Health. 2019;16(5):885. doi: 10.3390/ijerph16050885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith L.J., et al. Sleep disturbance among firefighters: understanding associations with alcohol use and distress tolerance. Cognit. Ther. Res. 2019;43(1):66–77. [Google Scholar]
- 70.Wolińska W., et al. Occurrence of insomnia and daytime somnolence among professional drivers. Fam. Med. Prim. Care Rev. 2017;(3):277–282. [Google Scholar]
- 71.Psarros C., et al. Personality characteristics and individual factors associated with PTSD in firefighters one month after extended wildfires. Nord. J. Psychiatr. 2018;72(1):17–23. doi: 10.1080/08039488.2017.1368703. [DOI] [PubMed] [Google Scholar]
- 72.Reinberg A., et al. Circadian time organization of professional firemen: desynchronization—tau differing from 24.0 hours—documented by longitudinal self-assessment of 16 variables. Chronobiol. Int. 2013;30(8):1050–1065. doi: 10.3109/07420528.2013.800087. [DOI] [PubMed] [Google Scholar]
- 73.Vincent G.E., et al. Impacts of Australian firefighters' on-call work arrangements on the sleep of partners. Clocks Sleep. 2020;2(1):39–51. doi: 10.3390/clockssleep2010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shi Y., et al. Daytime sleepiness among Midwestern firefighters. Arch. Environ. Occup. Health. 2021;76(7):433–440. doi: 10.1080/19338244.2020.1841718. [DOI] [PubMed] [Google Scholar]
- 75.Wagner B.d.A., Moreira Filho P.F. Painful temporomandibular disorder, sleep bruxism, anxiety symptoms and subjective sleep quality among military firefighters with frequent episodic tension-type headache. A controlled study. Arq. Neuro. Psiquiatr. 2018;76:387–392. doi: 10.1590/0004-282X20180043. [DOI] [PubMed] [Google Scholar]
- 76.Wróbel-Knybel P., et al. Sleep paralysis among professional firefighters and a possible association with PTSD—online survey-based study. Int. J. Environ. Res. Publ. Health. 2021;18(18):9442. doi: 10.3390/ijerph18189442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Korre M., et al. Effect of body mass index on left ventricular mass in career male firefighters. Am. J. Cardiol. 2016;118(11):1769–1773. doi: 10.1016/j.amjcard.2016.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim M.G., Ahn Y.-S. Associations between lower back pain and job types in South Korean male firefighters. Int. J. Occup. Saf. Ergon. 2021;27(2):570–577. doi: 10.1080/10803548.2019.1608061. [DOI] [PubMed] [Google Scholar]
- 79.Park S.K., et al. Emotional labor and job types of male firefighters in Daegu Metropolitan City. Ann. Occup. Environ. Med. 2019;31(1) doi: 10.35371/aoem.2019.31.e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hom M.A., et al. Examining physical and sexual abuse histories as correlates of suicide risk among firefighters. J. Trauma Stress. 2017;30(6):672–681. doi: 10.1002/jts.22230. [DOI] [PubMed] [Google Scholar]
- 81.Sullivan J.P., et al. Randomized, prospective study of the impact of a sleep health program on firefighter injury and disability. Sleep. 2017;40(1):zsw001. doi: 10.1093/sleep/zsw001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim J.I., et al. The mediation effect of depression and alcohol use disorders on the association between post-traumatic stress disorder and obstructive sleep apnea risk in 51,149 Korean firefighters: PTSD and OSA in Korean firefighters. J. Affect. Disord. 2021;292:189–196. doi: 10.1016/j.jad.2021.05.077. [DOI] [PubMed] [Google Scholar]
- 83.Lim G.-Y., et al. Comparison of cortisol level by shift cycle in Korean firefighters. Int. J. Environ. Res. Publ. Health. 2020;17(13):4760. doi: 10.3390/ijerph17134760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lim M., et al. Psychosocial factors affecting sleep quality of pre-employed firefighters: a cross-sectional study. Ann. Occup. Environ. Med. 2020;32 doi: 10.35371/aoem.2020.32.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lim M., et al. Effects of occupational and leisure-time physical activities on insomnia in Korean firefighters. Int. J. Environ. Res. Publ. Health. 2020;17(15):5397. doi: 10.3390/ijerph17155397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Choi S.J., et al. Insomnia symptoms and mood disturbances in shift workers with different chronotypes and working schedules. J. Clin. Neurol. 2020;16(1):108–115. doi: 10.3988/jcn.2020.16.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cramm H., et al. Mental health of Canadian firefighters: the impact of sleep. Int. J. Environ. Res. Publ. Health. 2021;18(24) doi: 10.3390/ijerph182413256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vasconcelos A.G., et al. Work-related factors in the etiology of symptoms of post-traumatic stress among first responders: the Brazilian Firefighters Longitudinal Health Study (FLoHS) Cad. Saúde Pública. 2021;37:e00135920. doi: 10.1590/0102-311X00135920. [DOI] [PubMed] [Google Scholar]
- 89.Stout J.W., et al. Sleep disturbance and cognitive functioning among firefighters. J. Health Psychol. 2021;26(12):2248–2259. doi: 10.1177/1359105320909861. [DOI] [PubMed] [Google Scholar]
- 90.Hernandez L.M., et al. Inadequate sleep quality on‐and off‐duty among central Texas male firefighters. Faseb. J. 2017;31:lb445. lb445. [Google Scholar]
- 91.Oh J., et al. Factors affecting sleep quality of firefighters. Kor. J. Psych. Med. 2018;26(1):19–25. [Google Scholar]
- 92.Carey M.G., et al. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J. Occup. Environ. Med. Am. Coll. Occup. Environ. Med. 2011;53(8):928. doi: 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jeong K.S., et al. Sleep assessment during shift work in Korean firefighters: a cross-sectional study. Saf. Health Work. 2019;10(3):254–259. doi: 10.1016/j.shaw.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim Y.T., et al. Cohort profile: firefighter research on the enhancement of safety and health (FRESH), a prospective cohort study on Korean firefighters. Yonsei Med. J. 2020;61(1):103–109. doi: 10.3349/ymj.2020.61.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Marconato R.S., Monteiro M.I. Pain, health perception and sleep: impact on the quality of life of firefighters/rescue professionals. Rev. Latino-Am. Enferm. 2015;23:991–999. doi: 10.1590/0104-1169.0563.2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Data will be made available on request.