Abstract
The purpose of this exploratory, non-experimental mixed methods study was to analyze the habits and routines of adults in early recovery (>3 months) from substance use disorder (SUD). Participants (N = 14) were recruited from an intensive outpatient treatment (IOP) program for substance use disorders. Data collection consisted of a demographic survey, a researcher developed Daily Occupational Questionnaire (DOQ), and follow-up semi-structured interviews with 5 randomly selected participants. Quantitative results indicate rest as the most frequently engaged in activity on the most busy (31.0%) and least busy day (36.6%). There was no significant difference, t(13) = 0.117, P = .909, between newly established activities on the most busy and least busy day. Qualitative themes included 1. The most difficult time of day is often related to patterns of unused time. 2. When there is a lack of structure or unoccupied time, they return to their previously established positive supports. 3. There is a need for consistency and structure for developing anticipated/perceived routines. Implications for all healthcare and clinical providers working with this population, as well as research suggestions, are outlined.
Keywords: Habits, routines, time configuration, early recovery, substance use, addiction, occupational therapy
Introduction
Among people aged 12 or older, over 41.1 million people needed substance use treatment in 2020.1 Statistics indicate that 40% to 60% of people with addiction will experience a relapse.2 Drug relapse statistics show that 85% of individuals with substance use disorders (SUD) relapse within the first year of recovery.3 Researchers estimated that more than two-thirds of individuals in recovery relapse in the first weeks or months of starting treatment3; therefore, the first year is crucial for addressing risk factors for relapse.4 The increasing risk of overdose and death from opioid use further exacerbates the need to address this critical time frame.5 Research has found that individuals who are in recovery have up to 16 to 18 hours of new, unoccupied free time as they no longer require time spent for obtaining, using, and recovering from the effects of substances.6,7 A common obstacle during early recovery is finding new meaningful activities in which to fill these new hours.8 Therefore, the structuring and/or restructuring of these hours is a crucial part of the recovery process and one that therapists and counselors should target when working with individuals with SUD.8,9 The restructuring of time is important because of the potential unease that can prevail after abstaining from drugs and needing to create new or renewed patterns of habits and routines.10 Although occupational therapists have intervened in the area of addiction for over 70 years, there is little research, with low levels of evidence, supporting occupational therapy assessment and intervention.11 The current study answers Rojo et al’s11 call for research in adding to the body of knowledge related to the experiences of those in early recovery as well as promoting the profession of occupational therapy in the field of addiction treatment.
Early recovery and recovery capital
Recovery is generally defined as a process of gaining holistic balance when an individual faces illness, crisis, or trauma.12 This unique healing process may include acceptance of the illness and its related challenges (ie, stigma attached to diagnosis and treatment) while reconstructing attitudes, beliefs, life roles, and personal goals immersed in psychological symptoms and life stressors.12,13 Recovery does not “cure” people from the illness, crisis or trauma, and the recovery process takes on a different meaning for each individual.14-16 Substance Abuse and Mental Health Services Administration17 has a working definition of recovery from mental illness and SUD in which it is defined as “a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential” (Overview section, para. 1).
Elison et al18 highlight that there are many definitions of recovery within the literature, including definitions constructed by those with SUD and definitions constructed by professionals. These definitions include long term management of substance use and/or decreased risk of substance use as issue or concern.19-21 Other definitions include transformation of one’s self identity22,23 or increased spirituality.24,25 The Diagnostic and Statistical Manual of Mental Disorders, fifth Edition, text revision (DSM-5-TR) defines substance use as a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues to use the substance despite significant substance related problems. It further defines early remission as a period when none of the criteria for SUD have been met for at least 3 months but for less than 12 months, after full criteria were previously met.7 Sustained remission is defined as a period of when none of the criteria have been met during a period of 12 months or longer.
Research indicates there are many potential challenges to sustaining recovery, including, but not limited to, stigma, anhedonia, sleep disturbances, mental health comorbidities, and negative social support.26-31 While there are potential challenges to sustaining recovery, research has shown that recovery capital aids in recovery. Recovery capital is defined as both internal and external resources an individual may use to initiate and subsequently maintain recovery.32,33 Recovery capital has also been shown to help support clinicians and therapists when providing treatment to clients with SUD through assessment of resources that either facilitate or hinder the recovery process.34 Research has indicated that those individuals with higher levels of recovery capital also have higher rates of recovery.33 These recovery capital resources may include social support, religiosity, life meaning, and affiliation with 12-step recovery programs.33 Similarly, Davidson35 stated that recovery capital includes social, emotional, and informational resources, including, but not limited to, activities in the community setting, education, housing, self-care tools, and peer support. In an article about personal recovery experience from chronic mental illness (that of schizophrenia), Leete36 expressed that temporally structured activities gave her something to look forward to, provided her with motivation, and allowed her hours to pass by remedially and productively.
How do individuals in early recovery structure their time?: Retrospective analysis
While the research indicates the aforementioned activities and supports as potential facilitators of recovery, the literature review revealed that there has been little research done on individuals who are currently in early remission, as opposed to individuals who are currently in sustained remission and are recounting how they structured their time in early remission.8,26,37,38 The literature review for this study yielded 5 instrumental research studies that provided insight into how those in early recovery structure their time, while also providing justification for current study.
Hood37 explored the experiences of 3 women in recovery from alcohol use disorder through semi structured focus groups. Qualitative analysis of the data included the specific function of leisure activities during their substance use recovery process. Among other themes, the women reported the need to find purpose and meaning to help support recovery. In terms of leisure participation, the women identified such activity as a tool for organizing their lives. Leisure participation, which can be defined as “planning and participating in leisure activities; maintaining a balance of leisure activities with other occupations; obtaining, using and maintaining equipment and supplies” (p. 34),9 reportedly helped them to keep occupied through structure. However, the results indicated that the women had difficulty in identifying the leisure activities in which they liked to engage, which is a key clinical implication of the research and lends itself to the need to engage in leisure exploration interventions for some individuals. Leisure exploration is defined as “identifying interests, skills, opportunities, and leisure activities” (p. 34).9 Limitations of the research include lack of generalizability due to qualitative methodology as well as the focus of women. Though the findings of this article are significant, the participants were interviewed when they were no longer in early remission; they were 4 to 10 years in sustained remission.
Harris et al.38 investigated the experiences of women in recovery (n = 27) who had histories of physical or sexual abuse with co-occurring mental health and SUD. Fourteen of the 27 women were considered abstinent, while 13 of the 27 women had a significant relapse. All participants had at least 2 years of recovery at time of participation in the semi structured interviews. Qualitative data analysis yielded 7 themes, which included both facilitators and barriers to recovery. One of the barriers that was discussed was destructive habits and routines. Among other clinical suggestions, the authors encourage clinicians to help women in recovery to construct strategies to cope with feelings of boredom.
Best et al.26 investigated the factors related to abstinence. Participants of the study included former heroin users (n = 107) with a minimum of 10 years abstinent from substance use. Results indicated that most expressed dissatisfaction with lifestyle associated with the substance use (“tired of lifestyle”) as factor related to abstinence. Results also included the utilization of social supports, as well as practical factors, including employment as factors in supporting abstinence along with religious and spiritual activities. A major limitation of this research is that a majority of participants were working in the field of addiction when they were retrospectively accounting for what contributed to abstinence.
Finally, Rodriguez and Smith8 examined young men’s experiences in early recovery through use of an interpretative phenomenological analysis. Participants (n = 4) engaged in semi structured interviews that explored the experiences of early recovery in Narcotics Anonymous (NA). There were several significant conclusions drawn from the results. Within the context of this study, it seems clear that certain habits/routines or strategies for creating healthy habits/routines may help to sustain recovery from SUD and prevent relapse. Specifically, writing, prayer, and consistent attendance of meetings to structure time proved to be helpful for these participants. Participants reported that their attendance at NA meetings provided them opportunities to develop social support and self-care routines. This study, unlike others, captures a more holistic experience of individuals in early recovery. However, the participants were all members of NA, so the results may not be transferable to the general treatment population.
Rationale for exploration of habits and routines in early remission
It has been shown that individuals with SUD often have maladaptive habits and routines associated with their addiction.39 Habits are defined as “specific, automatic behaviors performed repeatedly, relatively automatically, and with little variation.”9,40 (p. 214) Habits can be healthy or unhealthy, efficient or inefficient, and supportive or harmful.9,41 Routines are defined as patterns of behavior that are observable, regular, and repetitive and that provide structure for daily life. Routines require momentary time commitment and are embedded in cultural and ecological contexts.9,42,43
While research has been conducted in terms of how individuals structured their early recovery, participants in this study recounted their experiences after securing a period of abstinence. Existing literature provides little insight on what activities these individuals are actually engaging in during early recovery, as opposed to a retrospective review of what activities were utilized to support recovery.8,26,37,38 Providing insight and perspective on events in the past have the potential for recall bias and affect overestimation.44
Given the high rates of relapse in the first year of recovery, research that involves individuals in early recovery is warranted. However, there is a paucity of research that investigates what individuals are doing on a daily basis, over a period of time, in early recovery. Occupational therapists, counselors and other healthcare providers are in need of research that explores what individuals in early recovery are doing, via habit and routine exploration, in order to provide client centered intervention. Therefore, the objectives of this mixed methodology, concurrent type of research were (1) to quantitatively identify the habits and routines of adults currently in early recovery (ie, less than 1 year of sobriety) from SUD, and (2) to use semi-structured interviews to qualitatively explore the experiences, habits and routines of those in early recovery. Mixed methodology is a common methodological approach when there is little evidence in support of a specific condition.45
Methods
This research was approved by the Kean University Institutional Review Board, after approval was provided by the director of the IOP in which the participants were recruited. The outpatient program is an abstinence-based program that encourages individuals to refrain from drug use; however, in the event that an individual relapses, they are allowed to remain in the program unless it is determined that the participant needs a higher level of care.
All data collection (both quantitative and qualitative) occurred over the course of 1 month on 3 separate occasions. The researchers collaborated with the program’s clinical director to establish a specific date and time to come to a group meeting at the facility. After the date was established, the researchers emailed a recruitment flyer to the program director and asked that it was posted throughout the facility at least 1 week before the identified date of the group meeting. On the first occasion of 3, the date of which was outlined in the recruitment flyer, the researchers presented the study, described the inclusion criteria for participation, explained the purpose of the research, participant commitment, potential risks and benefits, and answered any questions potential subjects had about the research. This procedure was repeated a second time on a second occasion to increase the number of interested/consented participants in the study. On these 2 occasions, if a participant consented, they completed the corresponding outcome measures for the quantitative data collection.
Out of the 14 participants who consented, 11 individuals indicated their interest/willingness to engage in the qualitative aspect of the research study. Before the third occasion, 5 participants of the 11 were randomly selected to participate in a qualitative interview session. The participants who choose to be considered were assigned an identification number. The researchers used an internet-based random number generator to assign a random order to the identification numbers. The chosen participants were those whose identification numbers were first 5 on the random order list. In the event that 1 of the first 5 selected participants was unavailable for the qualitative portion of the study or no longer wished to continue with the study, the researchers moved down the list of identification numbers in the order generated by the random number generator. The interviews were scheduled through the clinical director. Each of the qualitative interviews was conducted in a one-on-one setting between 1 researcher and 1 participant.
The inclusion criteria for this study were as follows: over 18 years old, receiving treatment at the IOP, in early remission (ie, in treatment for less than 1 year for the current treatment episode), and proficient English literacy skills. No explicit incentive was provided for participation in the research study. However, the participants did review the potential benefits of participating on the consent form to help determine willingness to participate, one of which was to add to the body of knowledge related to treatment of adults with SUD.
Instruments and materials
The occupational therapy theoretical framework used to guide this research study is the Model of Human Occupation (MOHO47), a broad conceptual model of practice that considers differences in individuals’ motivations to engage in activities within temporal patterns and environments. The MOHO considers the interrelationships between 3 components, that of the volition subsystem, the habituation subsystem and that of performance capacity. Volition is related to the inherent drive and motivation for engagement in activities, while the habituation subsystem relates to the patterns of time spent in the desired activities. Finally, performance capacity is related to the musculoskeletal, neurologic, cardiopulmonary and other body systems that are used when engaging in activities.
Upon receipt of signed written consent, researchers administered a demographic survey and DOQ. The demographic survey identified the participants’ age, gender, ethnicity and amount of time in remission for their current treatment episode. The Daily Occupational Questionnaire (DOQ) was used to collect data on participants’ typical daily activities for one’s self identified “most busy” and “least busy” days. The DOQ was developed for the research study based upon the need to explore time use during the specified time frames. This questionnaire was specifically developed based upon the Occupational Questionnaire (OQ).46 Grounded in the Model of Human Occupation, an occupation based theoretical model of assessment and intervention as outlined above, the Occupational Questionnaire (OQ) was originally developed to measure volition subsystems and activity patterns with the geriatric population.46 The DOQ was structured in similar terms in that the participant was self-recording the activities in which he or she engaged in on a daily basis, over the course of a self-identified “ least busy” day and a “most busy” day.
When completing the DOQ, the participants listed activities for each hour between the hours of 12:00 AM and 11:00 PM for their identified “least busy day” and their identified “most busy day.” The instructions and structure of the DOQ prompted the participants to list the most important activity for each hour between the hours 12:00 AM and 11:00 PM. The participants then responded to 3 questions related to each activity.
Question one asked whether or not the subjects considered these activities as work, daily living tasks, rest, recreation/social or other.46 Work included paid or volunteer pursuits; daily living tasks were self-care and household activities such as cooking, cleaning, showering and laundry; recreational/social included activities such as swimming and playing basketball with friends; rest was sleep, relaxation and down time. If the participant did not think that the activity fit into any of those categories, they could select “other” and write how they categorized the activity.
Question 2 asked participants to indicate whether or not the activity was something that they started during the recovery process, as this data relates to the objectives of the research study. This variable, novelty, was whether or not the activity was new for participants since recovery had started. This was measured by a yes or no response.
Question 3 asked the participants to place a check for the top 3 activities that were important to their routine. The third variable, activity importance, qualified whether the activity was one of the top 3 most important activities to an individual’s routine. Activity importance was measured by the presence or absence of a check mark. The researchers created this questionnaire for the current research, so no reliability, validity or norms were established. Specifically, no face, construct or expert validity testing was completed to help determine if the categories used in the questionnaire were applicable for the SUD population in light of the original use with the geriatric population. However, the theoretical basis of the original Occupational Questionnaire, that of MOHO, does propose applicability across practice settings and populations with the additional consideration that substance use is in part characterized by how someone structures their time in terms of importance levels.47
The researchers also conducted interviews with 5 randomly selected participants as outlined above, as per the mixed methods approach to data collection and analysis. During these qualitative interviews, the participants were asked to explain their responses on the DOQ. They were also asked additional questions about their responses on the DOQ to expand upon what they experienced related to structuring their time in early recovery (in both least busy and most busy day) and how they experienced those periods of time. The interview questions aimed to explore what, if any, times of day are most difficult for the participant, what activities are new to their daily routine, and how these activities have impacted their routine (ie, helpful or not). The interviews continued until there was adequate saturation of data. Interviews did not last longer than 40 minutes. The following grand tour interview questions were generated by the researchers based on the Daily Occupational Questionnaire:
What activities that are not currently part of your routine would you like to start doing?
How do you think this activity would help you in your recovery?
Since being in recovery, what is the biggest difference in your daily routine?
How do you think this difference has impacted your recovery?
What time of day or night is most difficult for you? What specific time frame is most difficult for you?
What about this time of the day/time frame is difficult for you?
Additional follow-up questions were asked depending the need for further clarification based on initial responses to the above interview questions.45
Data analysis
The quantitative data was analyzed through the use of descriptive statistics, including frequencies and percentages. These frequencies were used to compare the most frequently selected categories, the general trends in new activities, the activities that were most frequently marked as important, and comparisons between the most busy and least busy day. The descriptive statistics were inputted into a Microsoft Excel spreadsheet for ease in classification and organization. The data was then inputted into Statistical Package for the Social Sciences for further analysis. Inferential statistics (independent samples T-test) were conducted to determine the difference in the mean number of new activities in the most busy and least busy days to determine if the participants are filling their free time with new activities.48 The set alpha level was P < .05.
Methods for the qualitative analysis were as follows. The initial data analysis consisted of sorting the transcripts into previously established codes. An a priori coding system was used as described by Schwandt.49 The codes were predetermined before the data collection occurred, based upon the review of literature and research objectives. The following codes were used for transcription analysis: habits, routines, time of day/difficult, biggest difference between least busy and busiest day, desired future occupations, experience of work, experience of daily living task, experience of rest, experience of social/recreation (leisure), and other. Each researcher reviewed the transcription of the interview and categorized the transcription using the a priori codes. Additional codes were added dependent upon the content within the interviews to avoid limiting analysis.49 Each coded transcription was checked by one other researcher (an independent analyst). The researchers then engaged in an in-depth process of peer debriefing,50 during which each researcher explored emerging themes from his/her respective transcript, and all researchers discussed similarities to maintain objectivity in theme statements.
Triangulation was achieved in several ways. First, each participant who was selected for an interview completed the DOQ; second, each analysis was reviewed by an independent analyst to ensure that the analysis was both accurate and thorough; and third, the participants were given the opportunity to participate in a member check for their interview transcription. Member checking is a validation tool in qualitative research in that it provides opportunity for the participants to review the data for accuracy.51 Throughout the transcription process, the observer comments were included where there was an opportunity for additional questions or coding categories. Additionally, the researchers engaged in a continuous process of memoing; these memos served the purpose of establishing the researchers’ potential thoughts and biases before data collection, elaborating on the predetermined codes, explaining any developing or emerging patterns, and describing any phenomena related to the setting. After all transcriptions were analyzed and sorted into codes, all researchers collaborated to determine similarities between codes and to create emerging theme statements.
Results
Over the course of 2 data collection sessions, a total of 14 individuals consented to participate in the study. Out of the 14 participants, 11 individuals consented to consideration for an interview. Per protocol, 5 participants were randomly selected among the 11 who consented, and all interviews were conducted approximately 1 month after initial quantitative data collection.
Out of the 14 participants, 8 were male (57.1%) and 6 were female (42.9%). Participants’ ages ranged from 22 to 68 years old, with a mean age of 43.78 years old. Time in recovery ranged from 1 to 12 weeks, with an average of 6.39 weeks.
Habits and routines
Over the course of 1 day, there were 336 possible activity responses (ie, each of the 14 participants indicated an activity for all 24 hours of the day) on the DOQ. During the most busy day, for all participants, work was selected a total of 53 times (15.8%). Of those 53 times, work was new 9 times (17.0%) and important 50 times (94.3%). Daily living tasks were indicated 73 times (21.7%). Of that, daily living tasks were new 11 times (15.1%) and important 46 times (63.0%). The recreation/social category was selected 40 times (11.9%) in total. Of that, recreation/social was new 11 times (28.0%) and important 16 times (40.0%). Rest was the most frequently selected activity category on the most busy day (104, 31.0%). Of that, it was new 47 times (45.2%) and important 88 times (84.6%). The other category was indicated 33 times (10.0%) and of that was new 28 times (84.8%) and important 26 times (78.8%). Several participants did not select a category; no response was indicated 33 times in total (10.0%). Of that, the particular activity was new one time (3.0%) and important 3 times (9.1%). See Table 1 for a summary of activities on the most busy day.
Table 1.
Summary of activities on most busy day.
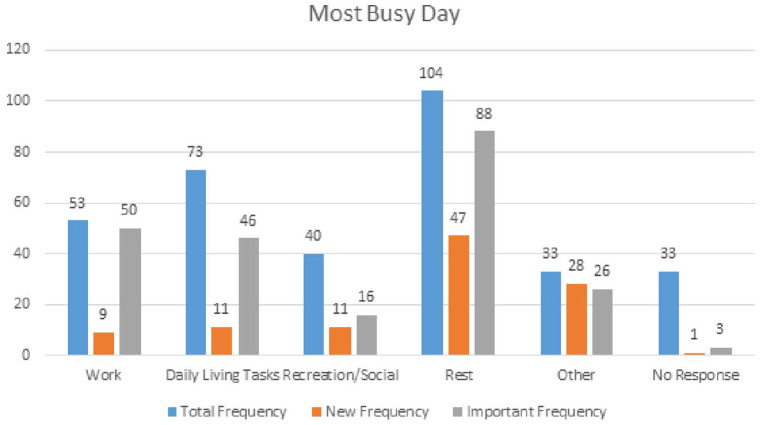
|
y-axis total frequency for each category (work, daily living skills, recreation, rest, other, no response) is out of a possible 336, as n = 14 over a 24-hour period.
During the least busy day, for all participants, work was selected a total of 9 times (2.7%). Of those 9 times, work was new 9 times (1%) and important 9 times (1%). Daily living tasks were indicated 85 times (25.3%). Of that, daily living tasks were new 14 times (16.5%) and important 52 times (61.2%). The recreation/social category was selected 57 times (16.17%) in total. Of that, recreation/social was new 0 times (0%) and important 16 times (28.1%). Rest was the most frequently selected activity category on the least busy day (123, 36.6%). Of that, it was new 50 times (40.7%) and important 82 times (66.7%). The other category was indicated 20 times (6.0%) and of that was new 20 times (1%) and important 20 times (1%). Several participants did not select a category; no response was indicated 42 times in total (12.5%). Of that, the particular activity was new 1 time (2.4%) and important 2 times (4.8%). See Table 2 for a summary of activities on the least busy day.
Table 2.
Summary of activities on least busy day.
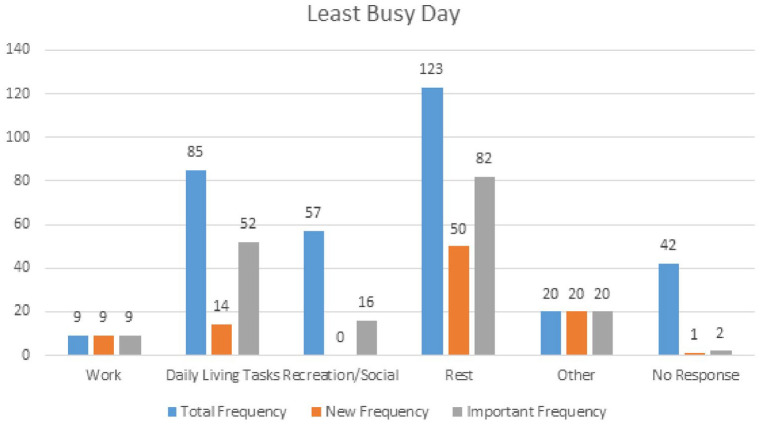
|
y-axis total frequency for each category (work, daily living skills, recreation, rest, other, no response) is out of a possible 336, as n = 14 over a 24-hour period.
Analysis also considered how many new activities were taking place on the most busy and least busy days. On the most busy day, new activities made up a total of 31.8% of all activities. On the least busy day, new activities made up a total of 28.0% of all activities. Finally, a paired t-test was conducted to determine whether or not there was a significant difference in the number of new activities on the most busy (M = 6.93, SD = 9.24) and least busy days (M = 6.71, SD = 10.28). Through this analysis, it was concluded that there was no significant difference, t(13) = 0.117, P = .909.
Theme statements
Of the 5 participants randomly selected for the semi-structured interviews (out of the 11 who consented), 3 were male and 2 were female. The age range among participants was from 22 to 65, and the mean age was 40.2 years old. The average time in recovery was 5.4 weeks.
Three major themes emerged from the analysis of the follow-up interviews. 1. The most difficult time of day is often related to patterns of unused time. 2. When there is a lack of structure or unoccupied time, they return to their previously established positive supports. 3. There is a need for consistency and structure for developing anticipated/perceived routines.
The most difficult time of day is often related to patterns of unused time
When the participants were asked what part of their day is particularly difficult for them in terms of recovery, their responses indicated that the specific time of day was not particularly significant, but rather that blocks of unused time, regardless of time of day, were most difficult. Participant 4 is currently finishing up school and noted that they will have more free time. They stated, “Now having this free time is going to make me nervous and that is a bit of a concern. But that is why I need to implement other activities and other things.” For Participant 4, time moves slowly in the absence of required structured activity, and it is the repetition of this slow-moving time that proves to be difficult. Participant 4 stated, “I feel like, late at night gets rough because that is when everything is slowing down and I’m in my head. Down time is definitely rough for me, but it can also be during the day.”
Participant 3 stressed the difficulty of repetitive unused time and noted that it helpful when there is something that is recurring (ie, IOP group) each week to rely on in order to fill up time. This participant reports concern about the larger periods of time that will need to be filled after discontinuing with the IOP program.
Having free time and kind of getting bored and when I’m bored, is when I start thinking about using. I try to fill my free time with whatever I have to keep busy. Which sometimes is difficult but being here three times, a week help me a lot because I don’t have to think about those three days and I only have Tuesdays and Fridays to think about. So once I am out of here I have to go and look for other ways to fill the three nights.
Additionally, these times of difficulty were correlated with their previous routines and patterns of substance use. Participant 2 stated that their most difficult time of day was not specific to either night time or day time hours, but rather that it was associated with previous patterns of his drug use. For Participant 2, the social, physical, and cultural environments of their apartment complex contribute to the level of difficulty; when they are at home, they are surrounded by reminders of people they used to sell drugs to and can see opened bags of drugs on the floor. Participant 4 also stated, “I broke up with my girl about a year ago. But, so I’m used to having someone in the house. And sometimes when I come home, and I’m there by myself, I’ll call over a female friend and we’ll use.”
Participants 3, 5, and 1 agree that their previous times of drug use are the times that are particularly difficult for them during recovery. Participant 3 stated, “I used to come from work, go get my drugs and use until I pass out. I would usually do that between 6 and 10 pm and have to try and turn around and get other things to do.” Participant 5 expressed that their previous substance use occurred frequently throughout the day. In recovery, Participant 5 experiences difficulty, “All the time. I want to use all the time.” Prior to beginning his new job, Participant 5 stated that they relied on Netflix to fill the times of day that they felt bored. Participant 5 reported, “You know it was something to do. I was in a big pit, you know. It was a binge for me.” Participant 1 articulated that currently, the most difficult time period is night, but the specific time was not noted. This is due to the fact that during their previous episode, night time was when they would spend most of their time drinking, which now affects their ability to fall asleep. Participant 1 expressed that alcohol contributed to the ability to fall asleep more easily.
Lack of structure or unoccupied time results in the return to previously established positive supports
The participants shared that when they experience unoccupied time, they turn to their previously established supports (ie, family, significant others, religion, helping others, etc.) to occupy their time. However, these supports are not consistently embedded into their routines. Participant 2 reported that they like to fill his time in the pursuit of helping others. They stated that being bored is a trigger for drug use and noted that their strategy for avoiding boredom is by keeping busy, “If I’m not doing anything work related or helping anybody, what do I do? I go – I’m not going to no gym or school, I go to New York, walk, go buy me shoes. . .” For this participant, the presence of unoccupied time leads to returning to past activities. Participant 1 expressed the same sentiment in their interview. Before Participant 1’s last treatment episode, they constantly participated in gardening outdoors and occasionally indoors as well. Participant 1 stated, “As I was growing up, my mom always had a garden so I was always exposed to that.” Participant 1 enjoyed planting fruits, vegetables, etc. as long as it involved being outside in the warm weather. Once Participant 1 started using, they stopped participating in this activity and has never resumed doing it due to the cold weather. However, Participant 1 hopes to start incorporating the activity back into their daily life once the warmer weather returns.
Two of the participants reported that their families were a significant source of support for them. However, as previously stated, visits with family members are not a consistent part of their routines. Participant 3 stated, “On Fridays if I have time I go for meetings and if not, I go visit with my family, like my parents and my sisters so that kind of fill my time.” In parallel, Participant 4 expressed that they spend time with her sister, stating, “I love spending time with her and she obviously knows about everything going on in my life. I don’t have to hide anything from her and I just feel comfortable around her.”
Finally, Participant 5 noted the impact of religion and spirituality during their recovery. Specifically, Participant 5 has intensified religion practices during their time in early recovery. Participant 5 stated, “I have been religious all my life. It just has intensified. I need Jesus more. I go deeper with him. And you know and just no matter how bad I am he still loves me. So thank God. He’s great.” In addition, Participant 5 also returns to the support of their girlfriend during recovery. “I hang out with my girlfriend more. We are spending more and more time together and I’m happy with it. She supports me in every way.” In general, the previously established supports seem to be chosen because of the participants’ anticipation of positive feelings/outcomes related to these activities.
There is a perceived need for consistency and structure in developing anticipated/future routines
Throughout the interviews, all 5 participants indicated the value of repetition, consistency, and structure in creating new routines to fill up their unused time. Participant 4 expressed the need for consistency in their schedule, stating, “My schedule during the week is very structured which helps me. Structure and consistency is key for me.” Participant 1 indicated the importance of a daily routine to start their day. Participant 4 stated, “Well, I get up earlier now, I actually make the bed, which I normally did not because I was always in the bed. On a nice day I open the window and go outside and you know just feel more alive.”
Three of the participants reported that they would like to start participating in new activities, but are not currently. Participant 2 in particular indicated that they want to start going to the gym. When asked why they were not currently going, Participant 2 stated, “My time. My schedule is crazy. So when you’re going to the gym you have to go like – if you go in the morning, you go in the morning. If you go in the afternoon, you go every afternoon.” Participant 2 believes it is impossible to develop a new routine in the absence of a consistent pattern. Participant 3 reported that they wanted to return to the gym, start playing golf, and fill their weekends with typical leisure activities (ie, basketball and spending time with friends). Participant 1 similarly reported that they wanted to get back to gardening. However, at the time of the study, neither participant had established routines. In this stage of recovery, the participants prioritized the management of current free time over adding new activities.
The participants expressed how they felt these desired new routines would have positive effects on how they feel. Participant 5 stated that they wanted to start working out more. Participant 5 reported that working out would help them have, “more energy and more motivation and more focus and more concentration and feeling better all around.” In addition, Participant 5 expressed that marrying their partner would have a positive impact. Participant 5 stated, “I want to get married. It would make life so much better. In every way it would. I truly believe that. She is just so good.” Similarly, Participant 3 stated that participating in certain activities would have a positive impact on their life. Participant 3 reported, “going to the gym and eating better will hopefully help me sleep better.”
Participant 4 stated that they believe incorporating healthier choices into their routine will help them through recovery. Participant 4 expressed that, “I feel like the more healthier things I do, it is going to bring me further from the drug because that was essentially destroying myself.” Similarly, Participant 2 stated that they wanted to go back to school to get a Master’s degree, to become a licensed clinical drug and alcohol counselor (LCADC), and to continue giving back to the community through their work in a substance use treatment program. Each of these activities contributes to their feelings of self-concept and worth. Participant 2 stated, “I always liked to help people. A lot of addicts are like that. They feel like they have to give back. I don’t know, maybe because all the wrong I had done. I feel like I have to give back.” Based on the participant responses, it appears that they are currently in the planning stage, rather than the implementation stage, of establishing their routines for the future and that they have identified future activities which they perceive to have positive impacts on their recovery.
Discussion
By virtue of the diagnosis of SUD, individuals have engaged in a great deal of time obtaining the substance(s), using the substance(s) and recovering from the(ir) effects, thereby limiting or eliminating certain occupations, or valued daily activities.7,9 Other diagnostic criteria for substance use include recurrent use resulting in failure to fulfill major role obligations at work, school or work, and reduction or giving up of important social, occupational, or recreational activities.7 Therefore, active substance use has impacted the nature, frequency and duration of daily patterns of occupational performance, which is defined as the ability to engage in a desired activity in consideration of the client, their context and desired activity.9 The transition between active addiction and being in “recovery,” or being in a treatment program, inherently affects one’s habits and routines and occupational performance. Occupational performance is defined as the engagement in a desired activity as related to the client, his/her/their abilities and his/her/their context.9 In early recovery, a large portion of one’s daily routine is potentially available for new or renewed activity engagement. A sense of physical and emotional readiness is associated with an individual’s movement from substance-related patterns of behavior into establishing recovery-based habits and routines. Within Prochaska and DiClemente’s Transtheoretical Model, an individual may progress through 5 stages.52 Within the first stage, the precontemplation stage, an individual has no intentions of changing either current or future behavior. In the second stage, the contemplation stage, the intention to attempt behavior change within the future becomes more prevalent. The third stage is the preparation stage. This stage is when an individual begins to develop a plan of action for the immediate future but are not currently taking such measures. In the fourth stage, action, individuals address specific actions and lifestyle changes to overcome their problems. Finally, in the maintenance stage, individuals focus on preventing relapse, but they do not take action as frequently as they do in the action stage.52
Based on the findings of this research, it appears that the participants are in the preparation stage, rather than the action stage. On both the most busy and the least busy days, less than 30% of the activities were considered new to their routine in recovery. Furthermore, the participants reported no new recreation/social activities on the least busy day, when they theoretically have more free time than on their most busy day. In other words, the participants are not currently implementing new activities into their current routines. In the interviews, the participants repeated this sentiment. Participants highlighted things that they want to do in the near future (ie, gym, work, gardening, etc.). This exemplifies the very notion of the preparation stage; the participants have identified new activities they want to do and they acknowledge how they believe these activities are going to make them feel. However, they are not currently at the stage to implement these activities into their routines.
In treatment for SUD, professionals tend to use action-orientated treatment plans that do not match the stage of the majority of clients.62 Based on the review of existing literature, many treatment programs indicate that it is important for individuals in early remission to restructure their newfound time through the routine use of recovery capital. It has been found that individuals commonly restructure time through routinely participating in leisure, work, social participation8,26,37,53-55 or spirituality practices.38,56,57 The activities the individuals reported on the DOQ align with this literature. More specifically, on the most busy day, the participants engaged in work 15.8% of the time, daily living tasks 21.7% of the time, recreation/social activity 11.9% of the time, and rest 31.0% of the time. On the least busy day, the participants engaged in work 2.7% of the time, daily living tasks 25.3% of the time, and recreation/social activity 16.7% of the time, and rest 36.6% of the time. The participants seem to be engaging in the activities that were reported in the literature review; however, the activities were not as new as the previous research suggests (ie, only 31.8% of activities were new on the most busy day and only 28.0% of activities were new on the least busy day). Based on the follow up interviews, the results suggest that the participants have returned to their previously established positive supports, which include family, leisure activities, religion, and work. This research challenges the notion that those in recovery should avoid activities that were associated with active substance use. In general, participants appeared to choose the previously established supports based on anticipation of positive feelings/outcomes related to those activities. The participants indicated that there are desired future occupations in which they are not currently engaging. The results suggest that there is a perceived need for consistency and structure in developing new habits and routines. Nemec et al.58 identified that there are several strategies for establishing new habits, including developing awareness of one’s current behaviors, identifying reasons to change and creating a plan for change with both specific and measurable goals. Additionally, the authors suggested that new habits are most effectively integrated into a routine when they are paired with existing routines and are repeated consistently.
Impact of rest and sleep in early recovery
Results of the current study indicate that participants are most frequently engaging in rest, which may include sleep, relaxation, and other down-time activities (31.0% of the time of the most busy day and 36.6% of the time on the least busy day). The participants also indicated that rest was the most frequently new and important aspect of their routine. On the most busy day, rest was new 45.2% of the time and important 84.6% of the time. On the least busy day, rest was new 40.7% of the time and important 66.7% of the time.
The DSM-5-TR outlines the impact of substance withdrawal on sleep.7 Cannabis withdrawal includes sleep difficulty. Stimulant withdrawal includes fatigue and vivid, unpleasant dreams that may contribute to poor sleep. Opioid intoxication includes drowsiness or coma. One opiate withdrawal symptom is disrupted sleep.59
Based on the results of this research, it is unclear whether the participants chose to rest (includes sleep, relaxation, down-time, or not doing anything in particular) intentionally, as a result of a lack of having other activities to participate in, or due to physiological reasons related to substance withdrawal. Previous literature does indicate the potential for feelings of boredom, as defined by feeling under-stimulated by an activity or lack of activity, to serve as a risk for SUD.60 Insufficient amounts of sleep create the inclination for the likelihood of decreased performance and productivity, substance use/misuse, and the creation of added daily stress.61 It is interesting to note that while the participants most frequently selected rest on both the most busy and least busy days of the DOQ, all 5 of the participants interviewed noted that downtime was the area of biggest stress. The participants expressed that their most difficult time of day was associated with the periods of time when there were no structured activities, or in the times when they previously used drugs/alcohol. It is possible that there is a difference between unproductive, unintentional rest and productive, intentional rest. Therefore, it is not possible to conclude whether the rest reported on the DOQ was unintentional or intentional. However, the data from the interviews suggest that unintentional rest was stressful. Both the quantitative and qualitative data suggest that rest could either have a positive or negative impact on recovery.
Limitations of research and considerations for future research
The current research study has several limitations. The participant demographics were not fully representative of the entire population of people in early recovery, as this sample is heterogenous. Specifically, the participants’ time in recovery ranged from 1 to 12 weeks, they were from 1 outpatient program, and the relatively small sample size is not sufficient to make general conclusions about this population. Qualitative findings are not meant to generalize, but rather to understand the experience of individuals with a lived experience.45 Some of the collected surveys were not entirely completed. Therefore, partial information was used for data analysis in order to ensure all responses were represented within the data analysis and to ensure that completion of the DOQ did not affect ability to participate in the follow-up interviews. Additionally, the recruitment site and program were abstinence-based, which may have acted as a confounding factor in the analysis of the data. Participants’ experiences of daily habits and routines may have been impacted if they were experiencing relapse(s). Recovery is a personal phenomenon and is defined differently by each person.18 Some of the participants indicated their time in recovery as the amount of time from the date of last use, even though the definition of early recovery used in this research was provided on the demographic survey. This creates potential discrepancy or differences in experiences related to habits, routines and activity engagement. In terms of the inferential statistics comparing the difference in number of new activities on most busy day versus new activities on least busy day, a small sample size was utilized, thereby limiting the power and validity of the results, and warranting larger samples in future research. Finally, there were minimal demographics collected at time of research, in an effort to protect this vulnerable population. However, in retrospect, more demographics, including but not limited to, marital status, employment status, income would add to the results and discussion in terms of how these demographics may or may not impact establishment or reestablishment of habits and routines in early recovery. Collecting mental and physical health diagnoses, if applicable, would permit exploration as to whether or not the diagnoses were impacting habit establishment or re-establishment, separate from the SUD.
Because the researchers created the DOQ specifically for this research, there are no established norms for reliability and validity. Future research could be conducted to establish these norms. The DOQ, its formatting, and structure also warrants overall strengthening, including improving the overall quality of the directions, creating stronger differentiations between the activity categories (ie, rest vs sleep), and changing the way questions are worded to note whether activities are new or important.
There are many ways that this research can be expanded upon in order to aid in the treatment and research processes for individuals in early recovery from SUD. First, future researchers can investigate sleep or sleep disturbances and SUD.63 Though this research does not necessarily indicate which type of rest is most important (ie, sleep vs down-time), it does provide evidence that rest is an important part of early recovery. There has been little research indicating the benefits of such rest in early recovery and/or the perceptions and experiences of rest of those in early recovery and how shapes daily routines and habits.29 Additional research could be conducted to determine whether the activity frequencies are similar or different to a sample of individuals without SUD, or whether the results look different when the participants are slightly further along in their recovery journey (ie, longer than 12 weeks in recovery). A final recommendation for future research relates to the limited demographics collected. Future research can incorporate expanded demographics in exploratory/correlational research. For example, does one’s marital or relationship status relate or impact early recovery and habit formation? Does one’s role as parent or guardian relate or impact early recovery and habit formation? Each of these recommendations for further research would strengthen the base of knowledge around early recovery to potentially decrease the risk of relapse and promote overall health, well-being, and quality of life.
Implications for clinical practice for interprofessional colleagues
As previously mentioned, the participants in this study were found to be in the preparation stage of change, as are many people in treatment programs.62 However, it is most common for treatment programs to employ action-oriented treatment plans, rather than targeting the current stage of change that the individual is in.62 Other health professionals, such as counselors and social workers, can use this information as well to help guide those individuals seeking treatment by meeting them where they are at personally, within their current treatment episode. This research can serve as a foundation for all people, including members of the treatment team, social supports, and family members/loved ones, to begin to consider the individuals’ lived experience of the preparation stage of early recovery.
As part of the interprofessional team, occupational therapists can utilize time configuration assessment as part of the evaluation stage, referring to assessment that explores how individuals structure their time on a daily, weekly, monthly and/or yearly basis.9 In addition to developing an occupational profile of a client’s interests, values, and priorities, the occupational therapist can assess past habits and routines in order to help client identify if whether or not these habits and routines will act as facilitators or barriers in pursuit of recovery and abstinence. Additionally, if clients indicate rest and sleep as a new activity in early recovery, practitioners should explore if engagement in those activities are due to feeling bored or the biological need to engage in this occupation during physiological withdrawal.7 Occupational therapy practitioners can also specifically assess the habits and routines associated with the occupation of sleep to determine if there is a need to adapt the environment or performance patterns to promote satisfaction with sleep (ie, turning off lights and turning off or limiting mobile device use).64
Conclusion
The purpose of this study was to explore the habits and routines of individuals currently in early recovery from SUD and to describe the phenomenon of time in early recovery. The results of this study suggest that the habits and routines of individuals in early recovery include work, daily living tasks, recreation and social activities, and rest. However, the majority of these activities were not new to their routine. Rather, the participants indicated that they have returned to previously established positive supports and activities, such as work, leisure, religion, and social supports. The participants also indicated that there are desired future activities which they wish to engage in, including exercise, gardening, and eating healthier, but that there is a perceived need for consistency and structure to fully develop these habits. The participants are not currently implementing these new activities into their routines, which suggests that they are more likely in the preparation stage, rather than the action stage, of the transtheoretical model.
Participants in this research were primarily in the preparation stage.62 In a meta-analysis of stages of change and psychotherapy outcomes, Krebs et al.65 (p. 1975) found that all reviewed studies “reported findings in support of stage matching treatments.” It is possible that individuals in early recovery would benefit from more time to engage in what Krebs et al.65 describe as self-liberation related to the preparation stage prior to moving into the counterconditioning that often occurs in the action phase.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contribution(s): RK, JG, MM, CC, NF, EL, JM, and GR contributed to overall conceputalization, writing of the manuscript, and data analysis. CC, NF, EL, JM, and GR also contributed to subject recruitment, data collection, and report writing. RK, JG, and MM were responsible for overall supervision of the research.
References
- 1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2020 national survey on drug use and health. HHS Publication; 2021:PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf [Google Scholar]
- 2. National Institute on Drug Abuse [NIDA]. How effective is drug addiction treatment?. 2020. Accessed January 29, 2022. https://nida.nih.gov/download/675/principles-drug-addiction-treatment-research-based-guide-third-edition.pdf?v=74dad603627bab89b93193918330c223
- 3. Sinha R. New findings on biological factors predicting addiction relapse vulnerability. Curr Psychiatry Rep. 2011;13:398-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kadam M, Sinha A, Nimkar S, Matcheswalla Y, De Sousa A. A comparative study of factors associated with relapse in alcohol dependence and opioid dependence. Indian J Psychol Med. 2017;39:627-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention [CDC]. Drug overdose deaths. 2022. Accessed January 29, 2022. https://www.cdc.gov/drugoverdose/deaths/index.html
- 6. Gutman SA. Why addiction has a chronic, relapsing course. The neurobiology of addiction. Occup Ther Ment Health. 2006;22:1-29. [Google Scholar]
- 7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-5-TR. 5th ed. American Psychiatric Association; 2022. [Google Scholar]
- 8. Rodriguez L, Smith JA. Finding your own place: an interpretative phenomenological analysis of young men’s experience of early recovery from addiction. Int J Ment Health Addict. 2014;12:477-490. [Google Scholar]
- 9. American Occupational Therapy Association. Occupational therapy practice framework: domain and process-fourth edition. Am J Occup Ther. 2020;74: 74124100101-741241001087. [DOI] [PubMed] [Google Scholar]
- 10. Werner JM. Occupation and recovery: identity, routines, and social support. AOTA: Ment Health Spec Inter Sect Quart. 2012;35:1-4. [Google Scholar]
- 11. Rojo-Mota G, Pedrero-Pérez EJ, Huertas-Hoyas E. Systematic review of occupational therapy in the treatment of addiction: models, practice, and qualitative and quantitative research. Am J Occup Ther. 2017;71:71051000301-710510003011. [DOI] [PubMed] [Google Scholar]
- 12. Swarbrick M. A wellness and recovery model for state psychiatric hospitals. Occup Ther Ment Health. 2009;25:343-351. [Google Scholar]
- 13. McGruder J. Life experience is not a disease or why medicalizing madness is counterproductive to recovery. Occup Ther Ment Health. 2002;17:59-80. [Google Scholar]
- 14. Sørensen T, Lien L. Significance of self-transcendence for rehabilitation and relapse prevention among patients with substance use disorder: A qualitative study. Religions. 2022;13:1-13. [Google Scholar]
- 15. Eakman AM, Eklund M. The relative impact of personality traits, meaningful occupation and occupational value on meaning in life and life satisfaction. J Occup Sci. 2012;19:165-177. [Google Scholar]
- 16. Kuo BCH. Culture’s consequences on coping: theories, evidence, and dimensionalities. J Cross Cult Psychol. 2011;42:1084-1100. [Google Scholar]
- 17. Substance Abuse and Mental Health Services Administration. Recovery and recovery support; 2022. Accessed January 29, 2022. https://www.samhsa.gov/find-help/recovery
- 18. Elison S, Davies G, Ward J. Initial development and psychometric properties of a new measure of substance use disorder “recovery progression”: the Recovery Progression Measure (RPM). Subst Use Misuse. 2016;51:1195-1206. [DOI] [PubMed] [Google Scholar]
- 19. Laudet AB, White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. J Subst Abuse Treat. 2010;38:51-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Neale J, Finch E, Marsden J, et al. How should we measure addiction recovery? Analysis of service provider perspectives using online Delphi groups. Drugs Educ Prev Policy. 2014;21:310-323. [Google Scholar]
- 21. Neale J, Tompkins C, Wheeler C, et al. “You’re all going to hate the word ‘recovery’ by the end of this”: service users’ views of measuring addiction recovery. Drugs Educ Prev Policy. 2015;22:26-34. [Google Scholar]
- 22. Buckingham SA, Frings D, Albery IP. Group membership and social identity in addiction recovery. Psychol Addict Behav. 2013;27:1132-1140. [DOI] [PubMed] [Google Scholar]
- 23. Mackintosh V, Knight T. The notion of self in the journey back from addiction. Qual Health Res. 2012;22:1094-1101. [DOI] [PubMed] [Google Scholar]
- 24. Galanter M. Spirituality and addiction: A research and clinical perspective. Am J Addict. 2006;15:286-292. [DOI] [PubMed] [Google Scholar]
- 25. Lyons GCB, Deane FP, Kelly PJ. Forgiveness and purpose in life as spiritual mechanisms of recovery from substance use disorders. Addict Res Theory. 2010; 18:528-543. [Google Scholar]
- 26. Best DW, Ghufran S, Day E, Ray R, Loaring J. Breaking the habit: a retrospective analysis of desistance factors among formerly problematic heroin users. Drug Alcohol Rev. 2008;27:619-624. [DOI] [PubMed] [Google Scholar]
- 27. Earnshaw VA, Bogart LM, Menino D, et al. Disclosure, stigma, and social support among young people receiving treatment for substance use disorders and their caregivers: A qualitative analysis. Int J Ment Health Addict. 2019;17: 1535-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huhn AS, Harris J, Meyer RE, Bixler E, Bunce S. Evidence for anhedonia in early recovery from prescription opiate addiction: affect modulated startle response suggests blunted hedonic responses to natural reward cues. Drug Alcohol Depend. 2015;156:e100. [Google Scholar]
- 29. Kolla BP, Schneekloth T, Biernacka J, et al. The course of sleep disturbances in early alcohol recovery: an observational cohort study. Am J Addict. 2014;23:21-26. [DOI] [PubMed] [Google Scholar]
- 30. McGaffin BJ, Deane FP, Kelly PJ, Ciarrochi J. Flourishing, languishing and moderate mental health: Prevalence and change in mental health during recovery from drug and alcohol problems. Addict Res Theory. 2015;23:351-360. [Google Scholar]
- 31. Substance Abuse and Mental Health Services Administration. Value of peers; 2017. Accessed January 29, 2022. https://www.samhsa.gov/brss-tacs/recovery-support-tools/peers
- 32. Granfield R, Cloud W. Coming Clean: Overcoming Addiction Without Treatment. New York University Press; 1999. [Google Scholar]
- 33. Laudet AB, White WL. Recovery capital as prospective predictor of sustained recovery, life satisfaction and stress among former poly-substance users. Substance Abuse & Misuse. 2008;43:27-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hennessy EA. Recovery capital: A systematic review of the literature. Addict Res Theory. 2017;25:349-360. [Google Scholar]
- 35. Davidson L. Integrating recovery supports in recovery-oriented systems of care; 2012. Accessed June 18, 2018. www.dsgonline.com/rtp/resources.html
- 36. Leete E. How I perceive and manage my illness. Schizophr Bull (Bp). 1989;15:197-200. [DOI] [PubMed] [Google Scholar]
- 37. Hood CD. Women in recovery from alcoholism: the place of leisure. Leisure Sci. 2003;25:51-79. [Google Scholar]
- 38. Harris M, Fallot RD, Berley RW. Special section on relapse prevention: qualitative interviews on substance abuse relapse and prevention among female trauma survivors. Psychiatr Serv. 2005;56:1292-1296. [DOI] [PubMed] [Google Scholar]
- 39. Scaffa ME. Alcoholism: an occupational behavior perspective. Occup Ther Ment Health. 1991;11:99-111. [Google Scholar]
- 40. Matuska K, Barrett K. Patterns of occupations. In: Schell BAB, Gillen G, eds. Willard and Spackman’s Occupational Therapy. 13th ed. Wolters Kluwer; 2019:212-220. [Google Scholar]
- 41. Dunn W. W. Habit: What’s the brain got to do with it?. Occup Particip Health. 2000;20:6S-20S. [Google Scholar]
- 42. Fiese BH. Routines and rituals: opportunities for participation in family health. Occup Ther J Res. 2007;27:41S-49S. [Google Scholar]
- 43. Segal R. Family routines and rituals: a context for occupational therapy interventions. Am J Occup Ther. 2004;58:499-508. [DOI] [PubMed] [Google Scholar]
- 44. Colombo D, Suso-Ribera C, Fernández-álvarez J, et al. Affect recall bias: being resilient by distorting reality. Cognit Ther Res. 2020;44:906-918. [Google Scholar]
- 45. Creswell JW. Qualitative inquiry & research design: choosing among five approaches. 3rd ed. SAGE Publications, Inc; 2013. [Google Scholar]
- 46. Smith NR, Kielhofner G, Watts JH. The relationships between volition, activity pattern, and life satisfaction in the elderly. Am J Occup Ther. 1986;40:278-283. [DOI] [PubMed] [Google Scholar]
- 47. Taylor RR. Kielhofner’s Model of Human Occupation: Theory and Application. 5th ed. Lippincott Williams & Wilkins; 2017. [Google Scholar]
- 48. DePoy E, Gitlin LN. Introduction to Research: Understanding and Applying Multiple Strategies. 6th ed. Elsevier; 2020. [Google Scholar]
- 49. Schwandt TA. Dictionary of Qualitative Inquiry. 2nd ed. SAGE Publications, Inc; 2001. [Google Scholar]
- 50. Ely M, Anzul M, Friedman T, Garner D, McCormack-Steinmetz A. Doing qualitative research: circles Within circles. Routledge Falmer; 1997. [Google Scholar]
- 51. Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: A tool to enhance trustworthiness or merely a nod to validation? Qual Health Res. 2016; 26:1802-1811. [DOI] [PubMed] [Google Scholar]
- 52. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102-1104. [DOI] [PubMed] [Google Scholar]
- 53. Rebeiro KL. Occupation-as-means to mental health: a review of the literature, and a call for research. Can J Occup Ther. 1998;65:12-19. [Google Scholar]
- 54. Williams DJ, Strean WB. Physical activity as a helpful adjunct to substance abuse treatment. J Soc Work Pract Addict. 2004;4:83-100. [Google Scholar]
- 55. Marlatt K, Walker GA, D, Mindfulness-based relapse prevention for alcohol and substance use disorders. J Cogn Psychother. 2005;19:211-228. [Google Scholar]
- 56. Green LL, Fullilove MT, Fullilove RE. Stories of spiritual awakening: the nature of spirituality in recovery. J Subst Abuse Treat. 1998;15:325-331. [DOI] [PubMed] [Google Scholar]
- 57. Pardini DA, Plante TG, Sherman A, Stump JE. Religious faith and spirituality in substance abuse recovery: determining the mental health benefits. J Subst Abuse Treat. 2000;19:347-354. [DOI] [PubMed] [Google Scholar]
- 58. Nemec PB, Swarbrick MA, Merlo DM. The force of habit: creating and sustaining a wellness lifestyle. J Psychosoc Nurs. 2015;53:24-30. [DOI] [PubMed] [Google Scholar]
- 59. Beswick T, Best D, Rees S, Bearn J, Gossop M, Strang J. Major disruptions of sleep during treatment of the opiate withdrawal syndrome: differences between methadone and lofexidine detoxification treatments. Addict Biol. 2003;8:49-57. [DOI] [PubMed] [Google Scholar]
- 60. Chao TW-C. A systematic review and empirical study of the role of boredom in substance use problems. Dissertation. The New School for Social Research; 2021: 1-132. [Google Scholar]
- 61. Wells ME, Vaughn BV. Poor sleep challenging the health of a nation. Neurodiagn J. 2012;52:233-249. [PubMed] [Google Scholar]
- 62. Norcross JC, Krebs PM, Prochaska JO. Stages of change. J Clin Psychol. 2011;67:143-154. [DOI] [PubMed] [Google Scholar]
- 63. Wilkerson AK, Simmons RO, Sahlem GL, et al. Sleep and substance use disorder treatment: A preliminary study of subjective and objective assessment of sleep during an intensive outpatient program. Am J Addict. 2021;30: 477-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gardner J, Swarbrick M, Dennis S, Franklin M, Pricken M, Palmer K. Sleep habits and routines of individuals diagnosed with mental and/or substance-use disorders. Occup Ther Ment Health. 2021;37:1-20. doi: 10.1080/0164212x.2021.1877592 [DOI] [Google Scholar]
- 65. Krebs P, Norcross JC, Nicholson JM, Prochaska JO. Stages of change and psychotherapy outcomes: a review and meta-analysis. J Clin Psychol. 2018;74: 1964-1979. [DOI] [PubMed] [Google Scholar]


