Abstract
Objectives
The quality of health care is individually and subjectively reflected through patients' level of satisfaction, as well as the optimality and effectiveness of the provided postoperative pain management. The provision of postanesthesia care unit (PACU) service in hospitals has led to overall positive outcomes, in addition to the enhancement of patients' satisfaction with the provided pain management service. This study assessed patients’ level of satisfaction with PACU service at a university hospital and discussed different factors that might have contributed to the level of satisfaction.
Methods
A prospective cross-sectional study was carried out among patients after being discharged from PACU. The study took place at King Fahad Hospital of the University in Al Khobar, KSA between November 2021 and February 2022. The data were collected using a three-section predesigned questionnaire.
Results
Two hundred patients were included in this study. Nearly all patients (95.5%) were satisfied with the provided pain management service. Almost all patients (99.5%) indicated that the PACU staff was courteous and professional during the entire pain management service. More patients complained about pain before using analgesia and this difference was statistically significant (Z = 8.642; p < 0.001). The satisfaction rate was significantly higher in the older age group (>45 years) (Z = 2.114; p = 0.035), in patients with American Society of Anesthesiology (ASA) 3 physical status (H = 13.130; p = 0.001), and those with a previous surgical history (Z = 2.139; p = 0.032).
Conclusion
This study concluded that the level of patients' satisfaction with PACU service was high, and established a statistically significant association with age, ASA score, and previous surgical history. Healthcare providers should consider patient education and effective communication to increase patients’ satisfaction level and improve the overall quality of care.
Keywords: Analgesia, Anesthesia, Patient satisfaction, Postanesthesia care unit, Preoperative education
Abbreviations: PACU, Postanesthesia care unit; KFHU, King Fahad Hospital of the University; ASA, American Society of Anesthesiology; ICU, Intensive care unit; GA, General anesthesia; BMI, Body Mass Index; SPSS, Statistical Packages for Software Sciences; IV, Intravenous; OR, Operating room; SCRELC, Standing Committee for Research Ethics on Living Creatures; IRB, Institutional Review Board (IRB)
الملخص
أهداف البحث
تنعكس جودة الرعاية الصحية بشكل فردي وذاتي من خلال مستوى رضا المرضى ، فضلا عن الأمثلية وفاعلية تدبير الألم بعد الجراحة المقدمة. أدى توفير خدمة وحدة رعاية ما بعد التخدير في المستشفيات إلى نتائج إيجابية عامة ، بالإضافة إلى تعزيز رضا المرضى عن خدمة تدبير الألم المقدمة. تهدف هذه الدراسة إلى تقييم مستوى رضا المرضى عن هذه الخدمة في المستشفى الجامعي ومناقشة العوامل المختلفة التي قد تكون ساهمت في هذا المستوى من الرضا.
طريقة البحث
تم إجراء دراسة مقطعية مستقبلية بين المرضى بعد خروجهم من وحدة رعاية ما بعد التخدير. أجريت الدراسة في مستشفى الملك فهد الجامعي في الخبر بالمملكة العربية السعودية بين نوفمبر 2021 وفبراير 2022. تم جمع البيانات باستخدام استبانة مكونه مسبقا من ثلاثة أقسام.
النتائج
تم تضمين نتائج 200 مريض في هذه الدراسة. كان جميع المرضى تقريبا (95.5٪) راضين عن خدمة تدبير الألم المقدمة. أشار جميع المرضى تقريبا (99.5٪) إلى أن طاقم وحدة رعاية ما بعد التخدير كانوا مهذبين ومهنيين خلال خدمة تدبير الألم بأكملها. اشتكى المزيد من المرضى من الألم قبل استخدام المسكن وكان هذا الاختلاف ذا دلالة إحصائية. كان معدل الرضا أعلى بشكل ملحوظ بين الفئة العمرية الأكبر سنا (> 45 عاما) وللمرضى في التصنيف الثالث من تصنيف الحالة الجسدية للجمعية الأمريكية لأطباء التخدير ومن لديهم تاريخ جراحي سابق.
الاستنتاجات
اختتمت الدراسة الحالية بمعدل رضا مرتفع بين المرضى تجاه خدمة وحدة رعاية ما بعد التخدير وأثبتت ارتباطا ذا دلالة إحصائية بالعمر ودرجة التصنيف في مقياس الحالة الجسدية للجمعية الأمريكية لأطباء التخدير والتاريخ الجراحي السابق. يجب على مقدمي الرعاية الصحية النظر في تثقيف المريض والتواصل الفعال لزيادة مستوى رضا المريض وتحسين الجودة الشاملة للرعاية.
الكلمات المفتاحية: تخدير, تسكين الألم, رضا المرضى, وحدة رعاية ما بعد التخدير, التعليم قبل الجراحة, تدبير الألم
Introduction
Pain in all its forms is a major problem that holds serious consequences suffered by postoperative patients during the length of recovery. Despite the advancement of medical protocols and analgesic variations and combinations, inadequately treated pain that persists is a hindering obstacle facing patients in the postoperative period. The cascade by which such pain influences patients’ lives is not merely physical but also extends to affect the quality of life lived with such pain, the lengthy recovery demanded by that pain, the byproduct of health care costs, and the overall satisfaction of pain management services.1, 2, 3
That being said, the quality of health care is individually and subjectively reflected through patients’ level of satisfaction, as well as the optimality and effectiveness of the provided postoperative pain management.4,3 Regardless of all of the clinical challenges in the postoperative period, the postanesthesia care unit (PACU) aims to handle patients in the fragile period following surgery and anesthesia and manage them accordingly. The provision of PACU service in hospitals has led to overall positive clinical and physiological outcomes, as well as enhanced satisfaction of the provided pain management service.5
Therefore, the purpose of this study was to evaluate patients’ level of satisfaction with PACU service and discuss different factors that might have contributed to the level of satisfaction.
Materials and Methods
Study setting, population and design
This was a prospective cross-sectional study that explored the influence of PACU service on patients’ level of satisfaction at King Fahad Hospital of the University (KFHU) in Al Khobar, KSA. The study was performed on postoperative patients after they were discharged from PACU service during the period from November 2021 to February 2022. The participants were interviewed by medical students after they were discharged from the PACU and provided postoperative analgesia. The patients provided written informed consent at the time of the interview.
Inclusion and exclusion criteria
The inclusion criteria were elective surgeries, general anesthesia, age >18 years, and American Society of Anesthesia (ASA) score 1–3. The exclusion criteria were: patients who had emergency surgeries, local/regional anesthesia, and postoperative intensive care unit admission.
Sampling and sample size
According to the number of patients who undergo elective surgeries per month in the hospital and the specified data collection period of 3 months, the total number of patients in the study was 450. Additionally, based on assumption of confidence interval of 95%, ±3% margin of error, and a P value of 0.05, the calculated sample size was 208 patients. Using the convenience sampling technique, a total of 200 postoperative patients, who matched the preset inclusion and exclusion criteria, were interviewed.
Data collection tool
A three-section questionnaire was administered to our selected sample, which has been previously tested and validated by a study by Farooq et al.6 The first section consisted of a total of six questions about demographical and identification data along with ASA score. The second section consisted of 10 questions regarding previous operations, current operation specifications, and postoperative analgesia and pain rating. The third section consisted of 10 questions in the form of 5-point Likert scale questions with Yes/No questions evaluating quality and experience in the postoperative period.
Data analysis
The satisfaction of patients with PACU service was measured using 10-item questionnaires adopted from the study of Farooq et al.6 To achieve better precision of satisfaction, we re-scaled the 5-Likert scale categories from lowest to highest and recoded “Yes” or “No” to 1 and 0. The total satisfaction score was calculated by adding all 10 items. Based on the participants’ responses, the satisfaction score ranged from 4 to 34 points; the higher the score, the higher satisfaction with the PACU service. By using 60% as a cutoff point to determine the level of satisfaction, patients were classified as dissatisfied if the score was ≤60% and satisfied if the score was >60%.
Categorical variables were measured as frequency and proportion (%), whereas continuous variables are expressed as the mean and standard deviation. The difference in satisfaction score according to the sociodemographic characteristics of participants was determined using the Mann Whitney Z-test and Kruskal–Wallis H test. A p-value of <0.05 was considered statistically significant. The overall distribution of data was analyzed using the Shapiro–Wilk test. The satisfaction score followed the abnormal distribution; thus, non-parametric tests were applied. The comparison between pain before and after using analgesia was conducted using the Wilcoxon signed-rank test. All data analyses were performed using Statistical Packages for Software Sciences version 26 (IBM Corporation, Armonk, NY, USA).
Results
A total of 200 patients were enrolled in this study. The most common age group was 46–60 years old (28%) with more than half being females (51.5%) and mostly Saudi nationality (84%). Regarding body mass index (BMI), approximately 34.5% were overweight and 33.5% were obese. With respect to education, 44% had college degrees. With regards to ASA physical status, 57% were classified as ASA category 2. Table 1 describes the sociodemographic characteristics of the 200 patients involved.
Table 1.
Participants’ sociodemographic characteristics.
| Study variables | N (%) |
|---|---|
| Age group in years | |
| 18–25 years | 24 (12.0%) |
| 26–35 years | 46 (23.0%) |
| 36–45 years | 46 (23.0%) |
| 46–60 years | 56 (28.0%) |
| >60 years | 28 (14.0%) |
| Sex | |
| Female | 103 (51.5%) |
| Male | 97 (48.5%) |
| BMI | |
| Underweight (<18.5 kg/m2) | 10 (5.0%) |
| Normal (18.5–24.9 kg/m2) | 54 (27.0%) |
| Overweight (25–29.9 kg/m2) | 69 (34.5%) |
| Obese (≥30 kg/m2) | 67 (33.5%) |
| Nationality | |
| Saudi | 168 (84.0%) |
| Non-Saudi | 32 (16.0%) |
| Level of education | |
| Uneducated | 14 (7.0%) |
| School educated | 85 (42.5%) |
| College educated | 88 (44.0%) |
| Postgraduate educated | 13 (16.5%) |
| ASA physical status | |
| ASA 1 | 53 (26.5%) |
| ASA 2 | 114 (57.0%) |
| ASA 3 | 33 (16.5%) |
The prevalence of patients with a previous surgical history was 67%, of whom 76.1% had previous management modalities. Of those with previous management modalities, the majority (58.8%) were strongly satisfied with the services received. A great proportion of the patients (62%) experienced pain preoperatively, whereas approximately 80% received preoperative information on postoperative pain management. The most common type of surgery was general surgery (42%); 43.5% had a surgery duration of 1–2 h. The main type of postoperative analgesia administered was intravenous (93.5%). Table 2 shows the surgical history of the included patients along with the postoperative pain management.
Table 2.
Surgical history and postoperative pain management.
| Variables | N (%) |
|---|---|
| Previous surgical history | |
| Yes | 134 (67.0%) |
| No | 66 (33.0%) |
| Previous management modality (n = 134) | |
| Yes | 102 (76.1%) |
| No | 32 (23.9%) |
| If previous question is Yes, what was the level of satisfaction (n = 102) | |
| Strongly dissatisfied | 5 (4.9%) |
| Dissatisfied | 2 (2.0%) |
| Neutral | 15 (14.7%) |
| Satisfied | 20 (19.6%) |
| Strongly satisfied | 60 (58.8%) |
| Preoperative pain | |
| Yes | 124 (62.0%) |
| No | 76 (38.0%) |
| Preoperative information of postoperative pain management was provided | |
| Yes | 160 (80.0%) |
| No | 40 (20.0%) |
| Type of surgery | |
| General surgery | 84 (42.0%) |
| Gynecology | 21 (10.5%) |
| Urology | 28 (14.0%) |
| Neurosurgery | 5 (2.5%) |
| Orthopedic | 30 (15.0%) |
| Other | 32 (16.0%) |
| Duration of surgery | |
| <1 h | 30 (15.0%) |
| 1–2 h | 87 (43.5%) |
| >2 h | 83 (41.5%) |
| Type of postoperative analgesia | |
| Intravenous | 187 (93.5%) |
| Patient control analgesia | 9 (4.5%) |
| Epidural | 4 (2.0%) |
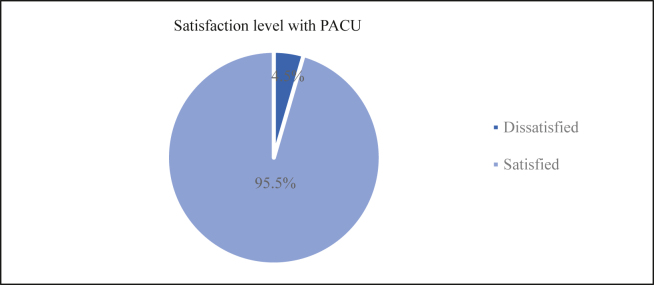
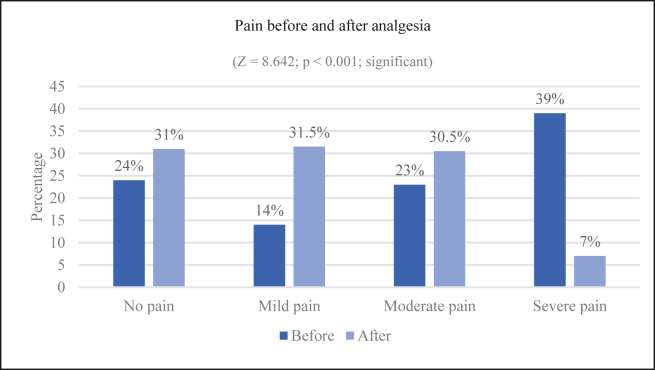
Regarding the assessment of satisfaction with the PACU, 28% of the patients expressed that they were expecting severe pain postoperatively; however, this expectation increased to 39% in the actual experience of severe pain. A great proportion of patients reported that the PACU staff responded within 30 min after complaining of pain. Nearly two-thirds of the patients (62%) rated the PACU as excellent after receiving management and most of them (86%) rated PACU staff as excellent for being attentive and sensitive. Overall experience with the pain management services provided by the PACU was also excellent among 73.5% of the patients. The proportion of patients who would use the same analgesia modality and recommend it to family/friends was 86.5% and 84.5%, respectively. Almost all patients indicated that the PACU team was courteous and professional with the entire pain management service. In addition, 42% of the patients were aware that a team of specialist pain doctors looked after pain relief. According to our criteria, the overall mean satisfaction score was 27.4 (standard deviation 3.30) of 34 points. Table 3 shows the satisfaction level with respect to PACU assessment. Nearly all patients (95.5%) were satisfied with the pain management services provided by the PACU, whereas only 4.5% were dissatisfied (Figure 1). Moreover, more patients complained about pain before using analgesia and this difference was statistically significant (Z = 8.642; p < 0.001) (Figure 2).
Table 3.
Assessment of satisfaction with PACU.
| Statement | N (%) |
|---|---|
| What type of pain did you expect in the postoperative period? | |
| No pain | 36 (18.0%) |
| Mild pain | 40 (20.0%) |
| Moderate pain | 55 (27.5%) |
| Less than severe | 13 (6.5%) |
| Severe pain | 56 (28.0%) |
| What type of pain did you experience in the postoperative period? | |
| No pain | 48 (24.0%) |
| Mild pain | 28 (14.0%) |
| Moderate pain | 46 (23.0%) |
| Less than severe | 0 |
| Severe pain | 78 (39.0%) |
| When you were in pain, did the PACU respond? | |
| Within 30 min | 176 (88.0%) |
| Within 1 h | 6 (3.0%) |
| Within 2 h | 2 (1.0%) |
| After 2 h | 4 (2.0%) |
| Never | 12 (6.0%) |
| What was the quality of pain relief after PACU management? | |
| Excellent | 124 (62.0%) |
| Very good | 42 (21.0%) |
| Good | 27 (13.5%) |
| Fair | 5 (2.5%) |
| Poor | 2 (1.0%) |
| How would you rate the attentiveness sensitivity of the PACU staff? | |
| Excellent | 172 (86.0%) |
| Very good | 22 (11.0%) |
| Good | 4 (2.0%) |
| Fair | 1 (0.50%) |
| Poor | 1 (0.50%) |
| How was your overall experience with your pain management service? | |
| Excellent | 147 (73.5%) |
| Very good | 31 (15.5%) |
| Good | 19 (9.5%) |
| Fair | 3 (1.5%) |
| Would you use the same analgesia modality again if required? | |
| Yes | 173 (86.5%) |
| No | 27 (13.5%) |
| Would you recommend the same modality to your family/friends? | |
| Yes | 169 (84.5%) |
| No | 31 (15.5%) |
| Was the PACU team courteous and professional during your entire interaction? | |
| Yes | 199 (99.5%) |
| No | 1 (0.50%) |
| Are you aware that a team of specialist pain doctors looked after your pain relief that is a part of the anesthesia department? | |
| Yes | 84 (42.0%) |
| No | 116 (58.0%) |
| Total satisfaction score (mean ± standard deviation) | 27.4 ± 3.30 |
Figure 1.
Level of satisfaction with PACU.
Figure 2.
Comparison of pain before and after using analgesia.
Additionally, the satisfaction rate was significantly higher among the older age group (>45 years) (Z = 2.114; p = 0.035), patients with ASA 3 physical status (H = 13.130; p = 0.001), and those with a previous surgical history (Z = 2.139; p = 0.032), whereas the satisfaction rate between sex, BMI, nationality, level of education, previous surgical history, previous management modality, preoperative pain, preoperative information of postoperative pain management provided, and duration of surgery was not significantly different across the groups (p > 0.05). Table 4 shows the association between satisfaction level toward PACU and different factors.
Table 4.
Association between participants sociodemographic characteristics and satisfaction with PACU.
| Factor | Satisfaction Score (34) Mean ± standard deviation |
Z/H-test | p-value |
|---|---|---|---|
| Age group in yearsa | |||
| ≤45 years | 26.9 ± 3.26 | Z = 2.114 | 0.035c |
| >45 years | 27.9 ± 3.29 | ||
| Sexa | |||
| Female | 27.3 ± 3.16 | Z = 0.550 | 0.583 |
| Male | 27.5 ± 3.46 | ||
| BMI levelb | |||
| Normal or underweight | 27.0 ± 3.53 | H = 3.853 | 0.146 |
| Overweight | 27.1 ± 3.07 | ||
| Obese | 28.0 ± 3.28 | ||
| Nationalitya | |||
| Saudi | 27.3 ± 3.37 | Z = 0.351 | 0.725 |
| Non-Saudi | 26.7 ± 2.96 | ||
| Level of educationa | |||
| School level or uneducated | 27.5 ± 3.31 | Z = 0.381 | 0.703 |
| College degree or higher | 27.3 ± 3.32 | ||
| ASA physical statusb | |||
| ASA 1 | 26.4 ± 2.86 | H = 13.130 | 0.001c |
| ASA 2 | 27.5 ± 3.29 | ||
| ASA 3 | 28.7 ± 3.59 | ||
| Previous surgical historya | |||
| Yes | 27.7 ± 3.27 | Z = 2.139 | 0.032c |
| No | 26.7 ± 3.29 | ||
| Previous management modalitya | |||
| Yes | 27.6 ± 3.29 | Z = 0.506 | 0.613 |
| No | 28.1 ± 3.23 | ||
| Preoperative paina | |||
| Yes | 27.1 ± 3.19 | Z = 1.725 | 0.085 |
| No | 27.8 ± 3.46 | ||
| Preoperative information of postoperative pain management was provideda | |||
| Yes | 27.4 ± 3.25 | Z = 0.328 | 0.743 |
| No | 27.1 ± 3.54 | ||
| Duration of surgeryb | |||
| <1 h | 28.4 ± 3.38 | H = 4.345 | 0.114 |
| 1–2 h | 27.1 ± 3.32 | ||
| >2 h | 27.3 ± 3.23 | ||
The p-value has been calculated using Mann–Whitney Z test.
The p-value has been calculated using Kruskal–Wallis H test.
Significant at p < 0.05 level.
Discussion
Patient satisfaction is an indicator of the quality of care, and it is an important assessment measure to enhance the health care services especially in acute settings.7,8 There are many factors that might play a role in patients' level of satisfaction including accessibility and convenience of the services, interpersonal relationships, health care practitioners' competence, patients' preferences and expectations, and the structure of the institution.8 Since the high standards of care are the focus of interest in our institution, this study aimed to identify patients’ level of satisfaction toward PACU services and to address the different contributing influencing factors.
In this study, the level of satisfaction with postoperative pain management services provided by PACU was 95.5%, whereas only 4.5% were dissatisfied. The low rate of dissatisfaction was consistent with other studies that were conducted internationally.8,9 Mayles et al.8 reported a 3.2% rate of dissatisfaction with anesthesia services postoperatively in Melbourne, Australia. Similarly, Tong et al.9 showed that only 1.1% of 2730 respondents rated the anesthesia care in Toronto hospital in Canada as poor, and this was mainly attributed to anesthesia related postoperative symptoms. Nevertheless, the rates of patients’ satisfaction/dissatisfaction were variable among the studies that were conducted nationally.7,10,11 Baroudi et al.10 conducted a multicenter study, which included 803 responses showing that only 21.56% of the participants were dissatisfied with the anesthesia services. Additionally, Alshehri et al.7 reported that 91.2% of patients had a high level of satisfaction with anesthesia care, whereas Alsaif et al.11 showed moderate overall satisfaction level of 56.5%.
Generally, the explanation behind the low rate of reported dissatisfaction and higher level of satisfaction with health care services in most studies might be attributed to the biased patients' responses to please the staff and avoid the consequences of negative appraisal of the provided care.8,9 Moreover, it has been recognized that most patients do not know what to expect from the health care services in order to rate them properly, and in most situations, they rate one aspect of the provided services.9 According to a meta-analysis, patients tend to report favorable responses in surveys focused on specific episodes compared to views related to health care in general because they may have optimistic bias assuming that their own experience is better than others.12,13 Hence, this might result in underrepresentation of the true picture of the actual satisfaction/dissatisfaction with the PACU service.1,8,14 However, adequate communication with the responsible staff, caring attitude toward the patients, and preoperative patients' education were found in several studies to increase the rate of satisfaction and enhance patients’ recovery postoperatively.6,8,15,16 This might explain the high rate of satisfaction in our study since almost all of the participants (99.5%) indicated that the team was courteous and professional during the entire interaction in the pain management service. Also, the majority of patients estimated a staff response to their pain to be within 30 min, and rated the PACU staff attentiveness and sensitivity as excellent (88% and 86%, respectively).
Furthermore, the current study showed a significant association between patients' satisfaction with PACU service and age, ASA physical status, and previous surgical history. Even though postoperative patient satisfaction has always been associated with lower pain intensity, there is opposing evidence that high satisfaction level is achieved despite having high pain intensity. This helps to prove that multiple factors exist and affect patients’ satisfaction toward postoperative pain management services.1,4,8,17, 18, 19
Regarding age groups, our results indicate that satisfaction rate was significantly higher among older age group (age >45) (Z = 2.114; p = 0.035). This finding supports the outcomes of previous research, where the satisfaction rate was also significantly higher among older age-group patients.8 Additionally, another two studies revealed that older patients report less pain intensity.17,18 This raises another question of whether the pain threshold in these patients is truly high, or if it is the result of patients’ aging processes and co-morbidities.17,18 Even though the literature suggests that pain perception is lower in old age, a meta-analysis concluded that there is insufficient evidence on age-related pain sensitivity response changes among healthy individuals.20 Therefore, there is a need for further studies to compare between pain sensitivity response and threshold in relation to age. Another study explained that the high satisfaction level in old age-group patients might be attributed to the fact of being through the process of previous surgeries and experiencing postoperative pain management previously.4
Having a previous surgical history was statistically significant (Z = 2.139; p = 0.032) in the current study. Patients with previous surgical experience were more satisfied with the PACU service due to patients being more adaptive, having more knowledge, and being less stressed about the upcoming surgery. Based on a cross-sectional study about pain experience and satisfaction, a significant relationship between previous surgical history and pain management satisfaction was established (p < 0.025) by having a higher satisfaction level in patients with previous surgical experience.4 In addition to prior surgical experience and knowledge, the study suggested that postoperative pain expectations of previous surgeries, and the relative change between preoperative and postoperative pain are all causes of high satisfaction level among these patients.4 Therefore, by filling knowledge gaps, comforting patients, and well communication might lead to a better outcome, and subsequently, higher satisfaction.4 Nevertheless, another study conducted on patients who underwent lumbar spine stenosis surgery showed opposite findings.20 The study demonstrated that patients with no previous surgical history of the same procedure showed more satisfaction level despite having good or bad outcomes.21 This suggests that the type of surgery, degree of invasiveness, and postoperative complications might affect satisfaction in those with previous surgical history.
In addition, another statistically significant factor of patient satisfaction rate with PACU was ASA physical status score (H = 13.130; p = 0.001). The ASA score is a helpful classification for anesthesiologists to determine if the patient is a good candidate for anesthesia by assessing the physiological status of the patient.22 However, the ASA has some limitations in estimating the direct operative risk as it does not account for other factors affecting operative risks.22 In our study, patients with an ASA 3 score had a significantly higher satisfaction level compared to ASA 1 and 2 scores (p = 0.001). This finding is similar to a study that included 10,811 patients.8 In that study, patients with ASA 3, 4, and 5 had a very low dissatisfaction rate (2.6%).8 However, when perioperative risk was adjusted, the physical status of patients was no longer associated with patient dissatisfaction.8 These results show that even with a higher risk of complication, patients are still highly satisfied with the care provided by the anesthesia team.
Moreover, pain relief before and after the analgesia showed a statically significant difference (Z = 8.642; p < 0.001). The majority of patients reported that they would use the same analgesia modality and recommend it to family/friends (86.5% and 84.5%, respectively). These again emphasize the effectiveness of administered analgesics and the high rate of satisfaction with the provided PACU service. Additionally, it has been postulated that patients' expectations about postoperative pain impact their later experience with the actual postoperative pain.6,23 Based on the findings from a meta-analysis, patients' expectations about acute intervention can be relieved by verbal suggestion, which in turn, highlights the importance of verbal communication while administering analgesic treatments.24 However, the results of the current study demonstrated an increase in the rate of “severe expected pain” postoperatively compared to the actually perceived pain from 28% to 39%. Even though patients' preoperative education and communication showed insignificant results with patients' satisfaction with PACU (Z = 0.328; p = 0.743), about 80% of the participants disclosed that they were provided preoperative information about postoperative pain management and 73.5% rated their overall experience with the PACU services as excellent. This might be explained by the fact that satisfaction level is not associated with the severity of pain but rather is associated with staff/patient communication regarding pain management priorities.25 This highlights the importance of pre-operative patients’ education and engaging patients in their management plan, which can be achieved through proper communication with patients to reach the highest possible level of satisfaction.4,18,19
Although in our study, sex (Z = 0.550; p = 0.583) and educational level (Z = 0.381; p = 0.703) were not significant, other studies found the opposite. A study done in 4853 patients, of whom 42.9% were males, revealed a higher satisfaction rate in males than in females about the provided care, which might be due to females having a significantly higher rate of nausea and vomiting postoperatively as reported by a previous study.26 The adverse effects of nausea and vomiting in females could be due to the fact that females are more prone to having postanesthesia side effects after discharge.27 In addition, due to cultural expectations and stereotyping of men regarding emotions, they tend to express their emotions less than women.28 Moreover, even though our results did not indicate a significant correlation between patients’ satisfaction with PACU and educational level, another study suggested that it is one of the dissatisfaction causes of postoperative pain management.4 The study discussed that patients with higher educational level are more likely to be dissatisfied compared to illiterate patients or those with a lower educational level. This might be due to the high expectations and demanding nature of the educated patient.4
Finally, more than half of the included patients (58%) in this study were not aware of the role of anesthesia physicians in alleviating their pain. This lack of knowledge about the varying roles of the anesthesia team was similar to the findings of other studies.29, 30, 31, 32 Baa et al.29 conducted a study in Riyadh, KSA, which revealed that 55.3% of the participants were ignorant about the role of anesthesia physicians in general. Also, Marulasiddappa and Nethra30 demonstrated that about 57% of patients in Karnataka, India were not familiar with anesthesia physicians' roles in the operating room (OR), and only 2% were aware about the roles of anesthesia physicians outside the OR. Likewise, Garcia-Marcinkiewicz et al.31 performed a study in Minnesota in the United States, which concluded that the roles of anesthesiologists within and outside the OR were not well known, and only 20% of 475 participants knew the role of anesthesiologists in the pain management clinic. The main reason behind this unawareness about the job of anesthesia physicians might be attributed to the limited patient–physician interactions.32 Therefore, this underlines the need of increasing public awareness about the different roles of anesthesia team by highlighting their responsibilities in managing the patients in variable settings via using different media channels. In addition, the anesthesia team should also emphasize and establish the importance of their roles by introducing themselves during the rounds and preoperative assessment of the patients because familiarity of the patients with their team can enhance patients’ experience and knowledge in making informed decisions, and consequently, improve the quality of health care system.
One of the main strengths of the current study was that the data collectors were unbiased personnel as they were not part of the PACU and did not participate in delivering care to the patients. Thus, the patients did not feel obliged to express positive answers. Also, it is noteworthy to mention that intensive care unit's admitted patients, and emergency surgeries were excluded; therefore, detection and reporting biases in uncooperative patients were unlikely to occur in this study. On the other hand, this study had several limitations. First, it was a cross-sectional study and involved recall bias, which might have limited the establishment of an association between different variables. Second, this study was conducted in patients under general anesthesia. This might reflect a high rate of satisfaction since patients who underwent regional anesthesia, who were awake and could recognize different aspects of the care during the operation, were not recruited. Third, the study did not include the impact of operating surgeon reassurance on the patients postoperatively, which might significantly influence patients' feelings of being cared. Additionally, the results of this study might have a significant influence on physicians' decision-making during the management of patients' symptoms, especially when considering the administration of analgesia for alleviation of pain. Therefore, further studies should incorporate the reasons for satisfaction and dissatisfaction to identify the major drawbacks in the provided services and hence optimize the quality of care. Furthermore, other aspects should be included such as preoperative stress status and postoperative anesthesia related symptoms, such as nausea/vomiting, shivering, and/or presence of drains/tubes, as these factors might alter patients' level of satisfaction. Identification of contributing factors to patients' satisfaction might influence further modes of management directed to enhance their experiences. Also, self-reported questionnaires might be used to eliminate biased responses of patients who feel obligated to answer positively during the interview. Lastly, higher numbers of patients with different anesthesia modalities might be considered to overcome the high variabilities in responses and to compare the impact of different anesthesia modalities on the level of satisfaction with services.
Conclusion
In conclusion, the current study established that patients have a high level of satisfaction with PACU service. Moreover, the study discussed different factors that may contribute to patients’ satisfaction with postoperative pain management services and found a significant association with age, ASA, and previous surgical history. This research might aid in guiding healthcare providers to explore and develop different aspects of postoperative pain management services. This could be achieved by patient education and effective communication to improve the overall quality of care and hopefully increase the level of satisfaction among these patients.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This study was in concordance with Imam Abdulrahman Bin Faisal University Standing Committee for Research Ethics on Living Creatures and has been approved by the institutional review board (No. IRB-UGS-2021-010383, Approval Date 26/10/2021).
Consent
The patients provided written informed consent at the time of interview, and were given a proper explanation of what the study entailed. All data were non-identifying and ensured patients’ confidentiality at all stages of the study. All acquired data, both included and excluded, were handled and strictly used for research purposes only.
Authors contributions
ZMA, NHA, NEA, and LHA participated in Conceptualization, Methodology, Investigation, Resources, Data Curation, and Writing - Original Draft. AMK and SMF contributed to the Conceptualization, Methodology, Writing - Review & Editing, and Supervision.
Acknowledgments
The authors would like to thank Lojain Alnosair for her contribution in data collection.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Sharma S., Thakur K., Mudgal S., Payal Y. Acute postoperative pain experiences and satisfaction with its management among patients with elective surgery: an observational study. Indian J Anaesth. 2020;64(5):403–408. doi: 10.4103/ija.IJA_33_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gan T. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–2298. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glowacki D. Effective pain management and improvements in patients' outcomes and satisfaction. Crit Care Nurse. 2015;35(3):33–43. doi: 10.4037/ccn2015440. [DOI] [PubMed] [Google Scholar]
- 4.Subramanian P., Ramasamy S., Ng K.H., Chinna K., Rosli R. Pain experience and satisfaction with postoperative pain control among surgical patients. Int J Nurs Pract. 2016;22(3):232–238. doi: 10.1111/ijn.12363. [DOI] [PubMed] [Google Scholar]
- 5.Davidson M., Litchfield K. Patient recovery and the post-anaesthesia care unit. Anaesth Intensive Care Med. 2021;22(10):607–610. [Google Scholar]
- 6.Khan R., Farooq F., Ahmed A. Assessment of patient satisfaction with acute pain management service: monitoring quality of care in clinical setting. Indian J Anaesth. 2016;60(4):248–252. doi: 10.4103/0019-5049.179450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alshehri A., Alomar Y., Mohammed G., Al-Fozan S., Al-Harbi S., Alrobai A., et al. A survey on postanesthetic patient satisfaction in a university hospital. Saudi J Anaesth. 2015;9(3):303–305. doi: 10.4103/1658-354X.158499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myles P., Williams D., Hendrata M., Anderson H., Weeks A. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84(1):6–10. doi: 10.1093/oxfordjournals.bja.a013383. [DOI] [PubMed] [Google Scholar]
- 9.Tong D., Chung F., Wong D. Predictive factors in global and anesthesia satisfaction in ambulatory surgical patients. Anesthesiology. 1997;87(4):856–864. doi: 10.1097/00000542-199710000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Baroudi D., Nofal W., Ahmad N. Patient satisfaction in anesthesia: a modified Iowa satisfaction in anesthesia scale. Anesth Essays Res. 2010;4(2):85–90. doi: 10.4103/0259-1162.73513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alsaif A., Alqahtani S., Alanazi F., Alrashed F., Almutairi A. Patient satisfaction and experience with anesthesia: a multicenter survey in Saudi population. Saudi J Anaesth. 2018;12(2):304–310. doi: 10.4103/sja.SJA_656_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall J., Dornan M. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27(6):637–644. doi: 10.1016/0277-9536(88)90012-3. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick R. Surveys of patient satisfaction: II--Designing a questionnaire and conducting a survey. BMJ. 1991;302(6785):1129–1132. doi: 10.1136/bmj.302.6785.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gandhi K., Baratta J., Heitz J., Schwenk E., Vaghari B., Viscusi E. Acute pain management in the postanesthesia care unit. Anesthesiol Clin. 2012;30(3):e1–e15. doi: 10.1016/j.anclin.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Lin C. Applying the American Pain Society's QA standards to evaluate the quality of pain management among surgical, oncology, and hospice inpatients in Taiwan. Pain. 2000;87(1):43–49. doi: 10.1016/S0304-3959(00)00267-0. [DOI] [PubMed] [Google Scholar]
- 16.Kol E., Alpar Ş., Erdoğan A. Preoperative education and use of analgesic before onset of pain routinely for post-thoracotomy pain control can reduce pain effect and total amount of analgesics administered postoperatively. Pain Manag Nurs. 2014;15(1):331–339. doi: 10.1016/j.pmn.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Woldehaimanot T., Eshetie T., Kerie M. Postoperative pain management among surgically treated patients in an Ethiopian hospital. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0102835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eshete M., Baeumler P., Siebeck M., Tesfaye M., Haileamlak A., Michael G., et al. Quality of postoperative pain management in Ethiopia: a prospective longitudinal study. PLoS One. 2019;14(5) doi: 10.1371/journal.pone.0215563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siu E., Quick J., Xu X., Correll D. Evaluation of the determinants of satisfaction with postoperative pain control after thoracoscopic surgery: a single-center, survey-based study. Anesth Analg. 2019;128(3):555–562. doi: 10.1213/ANE.0000000000003756. [DOI] [PubMed] [Google Scholar]
- 20.El Tumi H., Johnson M., Dantas P., Maynard M., Tashani O. Age-related changes in pain sensitivity in healthy humans: a systematic review with meta-analysis. Eur J Pain. 2017;21(6):955–964. doi: 10.1002/ejp.1011. [DOI] [PubMed] [Google Scholar]
- 21.Aalto T., Sinikallio S., Kröger H., Viinamäki H., Herno A., Leinonen V., et al. Preoperative predictors for good postoperative satisfaction and functional outcome in lumbar spinal stenosis surgery—a prospective observational study with a two-year follow-up. Scand J Surg. 2012;101(4):255–260. doi: 10.1177/145749691210100406. [DOI] [PubMed] [Google Scholar]
- 22.Doyle D., Goyal A., Garmon E. StatPearls. StatPearls Publishing; Treasure Island (FL): 2021. American society of anesthesiologists classification. [PubMed] [Google Scholar]
- 23.Fosnocht D., Heaps N., Swanson E. Patient expectations for pain relief in the ED. Am J Emerg Med. 2004;22(4):286–288. doi: 10.1016/j.ajem.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Peerdeman K., van Laarhoven A., Keij S., Vase L., Rovers M., Peters L., et al. Relieving patients' pain with expectation interventions. Pain. 2016;157(6):1179–1191. doi: 10.1097/j.pain.0000000000000540. [DOI] [PubMed] [Google Scholar]
- 25.Ward S., Gordon D. Application of the American Pain Society quality assurance standards. Pain. 1994;56(3):299–306. doi: 10.1016/0304-3959(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 26.Teunkens A., Vanhaecht K., Vermeulen K., Fieuws S., Van de Velde M., Rex S., et al. Measuring satisfaction and anesthesia related outcomes in a surgical day care centre: a three-year single-centre observational study. J Clin Anesth. 2017;43:15–23. doi: 10.1016/j.jclinane.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 27.Apfel C., Philip B., Cakmakkaya O., Shilling A., Shi Y., Leslie B., et al. Who is at risk for postdischarge nausea and vomiting after ambulatory surgery? Anesthesiology. 2012;117(3):475–486. doi: 10.1097/ALN.0b013e318267ef31. [DOI] [PubMed] [Google Scholar]
- 28.Koenig A. Comparing prescriptive and descriptive gender stereotypes about children, adults, and the elderly. Front Psychol. 2018:1086. doi: 10.3389/fpsyg.2018.01086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baaj J., Takrouri M., Hussein B., Al Ayyaf H. Saudi patients' knowledge and attitude toward anesthesia and anesthesiologists--A prospective cross-sectional interview questionnaire. Middle East J Anesthesiol. 2006;18(4):679–691. [PubMed] [Google Scholar]
- 30.Marulasiddappa V., Nethra H. A survey on awareness about the role of anesthesia and anesthesiologists among the patients undergoing surgeries in a tertiary care teaching women and children hospital. Anesth Essays Res. 2017;11(1):144–150. doi: 10.4103/0259-1162.186595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia-Marcinkiewicz A., Long T., Danielson D., Rose S. Health literacy and anesthesia: patients' knowledge of anesthesiologist roles and information desired in the preoperative visit. J Clin Anesth. 2014;26(5):375–382. doi: 10.1016/j.jclinane.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 32.Kadri I., Haider G., Memon I., Memon W. Awareness of patients regarding anesthesia;attitude towards basic types of anesthesia techniques. Prof Med J. 2018;21(4):782–787. [Google Scholar]