This cohort study assesses the association between implementation of the Healthy, Hunger-Free Kids Act of 2010 and changes in body mass index among youths aged 5 to 18 years in the US.
Key Points
Question
Was the Healthy, Hunger-Free Kids Act of 2010 (HHFKA), which mandated improvements in the nutritional quality of school meals and snacks, associated with changes in body mass index (BMI) among youths in the US?
Findings
In this cohort study of 14 121 youths aged 5 to 18 years contributing 26 205 BMI measurements, there was a significant decrease in the annual change in BMI z score in the period following implementation of the HHFKA compared with the period prior to implementation.
Meaning
The study’s findings suggest that implementation of the HHFKA was associated with a reduced youth BMI and additional policies may be warranted to improve school meal quality.
Abstract
Importance
The prevalence of obesity among youths 2 to 19 years of age in the US from 2017 to 2018 was 19.3%; previous studies suggested that school lunch consumption was associated with increased obesity. The Healthy, Hunger-Free Kids Act of 2010 (HHFKA) strengthened nutritional standards of school-based meals.
Objective
To evaluate the association between the HHFKA and youth body mass index (BMI).
Design, Setting, and Participants
This cohort study was conducted using data from the Environmental Influences on Child Health Outcomes program, a nationwide consortium of child cohort studies, between January 2005 and March 2020. Cohorts in the US of youths aged 5 to 18 years with reported height and weight measurements were included.
Exposures
Full implementation of the HHFKA.
Main Outcomes and Measures
The main outcome was annual BMI z-score (BMIz) trends before (January 2005 to August 2016) and after (September 2016 to March 2020) implementation of the HHFKA, adjusted for self-reported race, ethnicity, maternal education, and cohort group. An interrupted time-series analysis design was used to fit generalized estimating equation regression models.
Results
A total of 14 121 school-aged youths (7237 [51.3%] male; mean [SD] age at first measurement, 8.8 [3.6] years) contributing 26 205 BMI measurements were included in the study. Overall, a significant decrease was observed in the annual BMIz in the period following implementation of the HHFKA compared with prior to implementation (−0.041; 95% CI, −0.066 to −0.016). In interaction models to evaluate subgroup associations, similar trends were observed among youths 12 to 18 years of age (−0.045; 95% CI, −0.071 to −0.018) and among youths living in households with a lower annual income (−0.038; 95% CI, −0.063 to −0.013).
Conclusions and Relevance
In this cohort study, HHFKA implementation was associated with a significant decrease in BMIz among school-aged youths in the US. The findings suggest that school meal programs represent a key opportunity for interventions to combat the childhood obesity epidemic given the high rates of program participation and the proportion of total calories consumed through school-based meals.
Introduction
The prevalence of obesity among youths 2 to 19 years of age in the US from 2017 to 2018 was 19.3%; improving child and adolescent nutritional intake is a key component of combatting the obesity epidemic.1 Previous studies have shown associations between school meal consumption and obesity; a study of sixth-grade children between 2004 and 2009 showed that consuming compared with not consuming school-provided meals was independently associated with childhood obesity (odds ratio, 1.29; 95% CI, 1.02-1.64).2 In addition, students living in states with school meal nutritional standards that were stricter than the US Department of Agriculture (USDA) guidelines vs those that met the USDA guidelines had body mass index (BMI) percentiles that were 11% lower (95% CI, −17.7% to −4.3%).3
The National School Lunch Program and the School Breakfast Program provide meals at low or no cost to more than 30 million children, providing an estimated 50% of students’ caloric intake each school day.4,5,6 The Healthy, Hunger-Free Kids Act of 2010 (HHFKA), which applied to school breakfasts, lunches, and snacks sold at school vending machines and stores, strengthened nutritional standards to include more whole grains, fruits, vegetables, and low-fat dairy products with less sodium and fat than prior requirements.7,8 The HHFKA brought school meals into alignment with the 2010 Dietary Guidelines for Americans and required school districts to develop policies that included other school-based wellness activities.9
The phased implementation of the HHFKA began with the 2012 to 2013 school year, with additional provisions implemented during subsequent school years.10 The USDA reported that following the 2015 to 2016 school year, 93% of school districts were in compliance with the law.11 Evidence suggests that the HHFKA-mandated nutritional standards improved the nutritional quality of school meals, with no evidence of increased cost or decreased participation in the program.12,13,14,15
To date, evaluations of the association of the HHFKA with childhood obesity have been limited but suggest an association with decreased childhood BMI in particular populations. Using the National Survey of Children’s Health, Kenney et al9 showed that while there was no association between HHFKA implementation and childhood obesity overall across the US, obesity risk significantly declined among children 10 to 18 years of age who were living in poverty. Similarly, using 2 nationally representative cohorts of kindergarten students followed through fifth grade, Richardson et al16 found that HHFKA implementation was associated with a reduction in disparities in BMI trajectories between children from families with low income who participated in the National School Lunch Program and the School Breakfast Program and families with higher income who did not participate. Sanchez-Vaznaugh et al17 showed an improvement in overweight and obesity trends in fifth-grade students at public schools in California following implementation of a statewide school nutrition program, with further improvement after the addition of the HHFKA.
Some gaps remain in the understanding of the association between the HHFKA and youth BMI. Evaluations to date have shown associations between the HHFKA and BMI only among children from households with low income.9,16 It is also possible that sex-, age-, or geographic region–based differences in youths’ interest and autonomy in obtaining food outside the school meal program may contribute to differences in the association between the HHFKA and BMI among certain subgroups. In addition, USDA efforts to improve school nutritional standards are ongoing; in February 2022, further clarity on school diet guidelines was issued.18 Evidence of the association between school nutrition guidelines and overweight and obesity among youths is crucial to build evidence and resource support for such policies.
Data from the National Institutes of Health’s Environmental Influences on Child Health Outcomes (ECHO) program offer an opportunity to assess BMI over time. In this study, we evaluated the association between the HHFKA and youth BMI using data from youths enrolled in participating ECHO cohorts, with the hypothesis that improvement in school meal quality would be associated with reduced BMI over time among all school-aged youths.
Methods
Study Participants
This cohort study was conducted using data from the ECHO program, a nationwide consortium of child cohort studies that aims to leverage its demographic and geographic heterogeneity and large sample size to answer important research questions about child health and development.19 Youths were included if they had 1 or more height and weight measurements between January 2005 and March 2020 and were 5 to 18 years of age at the time of measurement. We did not include measurements obtained after March 2020 because of the widespread school shutdowns and changes in availability and use of school meals due to the COVID-19 pandemic. The study protocol was approved by the local (or single ECHO) institutional review board of each participating cohort. Written informed consent from parents or guardians was obtained, along with youth assent as appropriate, for participation in both cohort-specific as well as ECHO-wide cohort data collection protocols. All methods were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.20
Exposure
School district–level information from the year of full implementation of HHFKA requirements was not available from the USDA. Therefore, our analysis assumed that the 2016 to 2017 school year was the first school year with full implementation of the HHFKA, starting in September 2016. This aligns with the planned phases of HHFKA implementation, and the USDA reported that 93% of school districts were in compliance by the end of the 2015 to 2016 school year.11 In this analysis, the HHFKA preimplementation period was January 2005 to August 2016 and the postimplementation period was September 2016 to March 2020.
Covariates
We examined sociodemographic characteristics of youths who contributed data to the periods before and after HHFKA implementation, and we graphically explored potential changes in the composition of the analytic sample over the study period. All sociodemographic characteristics were self-reported by adolescents (age 12-18 years) or were parent or guardian reported for children (age 5-11 years). Sex was dichotomized as female or male. Race was categorized as African American or Black, White, or other or unknown (American Indian or Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, multiple races, other races, and did not know). Ethnicity was categorized as Hispanic, non-Hispanic, or did not know. Maternal educational level was categorized as less than a high school degree; a high school degree, General Educational Development, or equivalent; some college, no degree, and above; or missing data. Annual household income was categorized as less than $30 000, $30 000 to $49 999, $50 000 to $74 999, or $75 000 or more. Enrollment cohorts were grouped by similar enrollment criteria and outcomes of interest into 6 cohort groups, namely general population birth cohorts, general population youth cohorts, early-term cohorts, ethnic minority cohorts, enriched for neurocognitive impairment, and enriched for airways-associated impairment. Youth race, youth ethnicity, maternal educational level, and cohort group were included as confounding variables in the main model as these reflected observed changes in the analytic sample over the study period. The mean or mode of imputed values among 5 iterations was used to calculate the imputed value for each missing covariate at each time point.
Outcome
The weight and height of youths meeting the inclusion criteria were used to calculate BMI (calculated as weight in kilograms divided by height in meters squared). Measurements were conducted by research staff (79%) or gathered from youth self-report (adolescents) or parent- or guardian-report (children) (21%). The BMI z-score (BMIz) measurements were compiled at the youth-month level during the period of interest and were used as the primary outcome. In the few instances when a youth had more than 1 BMI reported within the same month, the first measurement in the month was used.
Statistical Analysis
Data for BMIz were compiled at the youth level for each month from January 2005 through March 2020. We then scaled time to the annual level for ease of interpretability. An interrupted time-series analysis design was used to fit generalized estimating equation models to test whether the rate of annual BMIz change was altered after implementation of the HHFKA. We included the aforementioned covariates, imposed a first-order autoregressive covariance structure, did not include a lag term, and clustered on participant. The model included terms for year and postintervention period and an interaction term between the 2, which calculated the annual change in BMIz following HHFKA implementation compared with the annual change in BMIz prior to the intervention.
Because of differences in sociodemographic profiles of youths contributing data to the preintervention period compared with the postintervention period, we adjusted for the following individual-level covariates: self-reported race, Hispanic ethnicity, cohort group, and maternal educational level. Three-way interaction terms (along with the corresponding covariate as a main effect term) were then included in separate models to assess effect measure modification by sex (female vs male), age group (5-11 years vs 12-18 years), annual household income (<$50 000 vs≥$50 000), baseline BMI category (underweight or normal weight vs overweight or obese), and US census region of the cohort enrollment site.21 The goal of these analyses was to explore differences in the impact of the HHFKA among subgroups that may have differences in their ability to obtain food outside the school meal program or that are known to be at higher risk for excess weight gain.
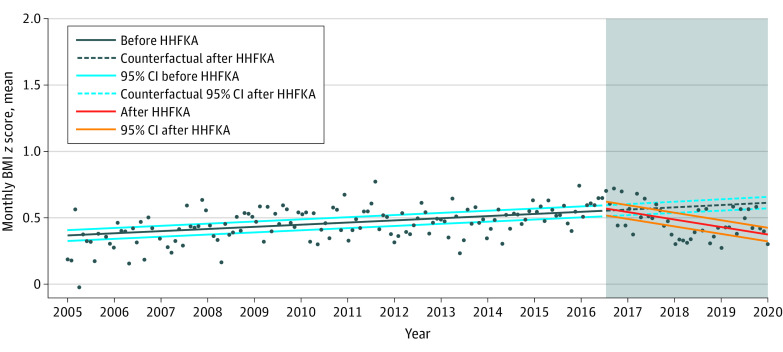
To visually compare the changes before and after HHFKA implementation, a counterfactual BMIz trend was modeled by fitting an estimated linear regression model for the postimplementation period following the calculation of the preintervention trend line (Figure).22 For ease of visualization, this exploration was done after aggregating all BMIz and covariate data to the monthly level. The counterfactual trend represents the expected trend in BMIz data if the HHFKA had not been implemented.
Figure. Mean Monthly Body Mass Index (BMI) z Scores Before and After Implementation of the Healthy, Hunger-Free Kids Act of 2010 (HHFKA).
Shading indicates the postimplementation period.
We performed 2 sensitivity analyses. We conducted a sensitivity analysis in the subset of youths contributing at least 1 data point both before and after the implementation year to test the robustness of our results to changes in sample composition over time. Second, we recognized that a limitation of the BMIz is that the calculated z-scores and percentiles for youths with extreme obesity (>97th percentile) do not accurately characterize the BMI trajectory.23,24 Therefore, we repeated the entire analysis using BMI as a percentage of the age- and sex-specific 95th percentile values provided by the Centers for Disease Control and Prevention (data shown in the eTable in Supplement 1).25
All analyses were performed using R, version 4.1.0 (R Project for Statistical Computing). Imputation was performed for missing covariate data using the Multivariate Imputation by Chained Equations package in R. The Centers for Disease Control and Prevention macro in SAS, version 9.4 (SAS Institute Inc) was used to calculate sex-specific BMIz.25
Results
A total of 14 121 youths from 50 cohorts contributing 26 205 measurements were included in the overall analytic sample (Table 1). Approximately half of the youths (6884 [48.8%]) were female, and 7237 [51.3%] were male. A total of 2833 (20.1%) were African American or Black; 159 (1.1%), American Indian or Alaska Native; 232 (1.6%), Asian; 15 (0.1%) Native Hawaiian or Other Pacific Islander; 8772 (62.1%), White; 1244 (8.8%), multiple races; 61 (0.4%), and other race; 805 (5.7%) did not know their race. For ethnicity, 2833 (20.1%) were Hispanic, 11 111 (78.7%) were non-Hispanic, and 177 (1.3%) did not know their ethnicity. The majority of youths (9862 [69.8%]) reported maternal educational level of some college or more. Enrollment sites were located primarily in the West (5213 [36.9%]) followed by the Northeast (4007 [28.4%]). The analysis included youths aged 5 to 18 years. The mean (SD) age at first BMI measurement was 8.8 (3.6). A total of 8741 (61.9%) youths in the analytic data set contributed at least 1 BMIz value both prior to and following the 2016 implementation year. The mean (SD) BMIz for all participant measurements was 0.46 (1.16), with 1.87 BMI measurements per youth. The majority (17 074 [65.2%]) of height and weight measurements were in the normal weight (18.5 to <25.0) BMI category.
Table 1. Sociodemographic Characteristics of the Analytic Sample.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Complete analytic sample | January 2005 to August 2016 | September 2016 to March 2020 | |
| By participant | |||
| Total, No. | 14 121 | 8939 | 6900 |
| >1 Measurement, No. | 5228 | 3011 | 1726 |
| Sex | |||
| Female | 6884 (48.8) | 4414 (49.4) | 3311 (48.0) |
| Male | 7237 (51.2) | 4525 (50.6) | 3589 (52.0) |
| Race | |||
| African American or Black | 2833 (20.1) | 1854 (20.7) | 1439 (20.9) |
| AI/AN | 159 (1.1) | 38 (0.4) | 127 (1.8) |
| Asian | 232 (1.6) | 153 (1.7) | 94 (1.4) |
| NH/PI | 15 (0.1) | 11 (0.1) | 5 (0.1) |
| White | 8772 (62.1) | 5380 (60.2) | 4386 (63.6) |
| Multiple | 1244 (8.8) | 752 (8.4) | 671 (9.7) |
| Othera | 61 (0.4) | 23 (0.3) | 42 (0.6) |
| Did not know | 805 (5.7) | 728 (8.1) | 136 (2.0) |
| Ethnicity | |||
| Hispanic | 2833 (20.1) | 2204 (24.7) | 875 (12.7) |
| Non-Hispanic | 11 111 (78.7) | 6596 (73.8) | 5983 (86.7) |
| Did not know | 177 (1.3) | 139 (1.6) | 42 (0.6) |
| Maternal educational level | |||
| Less than high school | 1261 (8.9) | 1033 (11.6) | 387 (5.6) |
| High school degree, GED, or equivalent | 2165 (15.3) | 1556 (17.4) | 922 (13.4) |
| Some college, no degree, and above | 9862 (69.8) | 5658 (63.3) | 5431 (78.7) |
| Missing | 833 (5.9) | 692 (7.7) | 160 (2.3) |
| Household income | |||
| <$30 000 | 2809 (19.9) | 1991 (22.3) | 1167 (16.9) |
| $30 000-$49 999 | 1447 (10.2) | 954 (10.7) | 697 (10.1) |
| $50 000-$74 999 | 1190 (8.4) | 657 (7.3) | 790 (11.4) |
| $75 000 or more | 4119 (29.2) | 2173 (24.3) | 2682 (38.9) |
| Missing | 4556 (32.3) | 3164 (35.4) | 1564 (22.7) |
| US census region of enrollment | |||
| Midwest | 2559 (18.1) | 1781 (19.9) | 1069 (15.5) |
| Northeast | 4007 (28.4) | 2958 (33.1) | 1630 (23.6) |
| South | 2342 (16.6) | 1028 (11.5) | 1608 (23.3) |
| West | 5213 (36.9) | 3172 (35.5) | 2593 (37.6) |
| By BMI measurement | |||
| Total, No. | 26 205 | 17 173 | 9032 |
| Age at first measurement, mean (SD) | 8.8 (3.6) | 9.5 (3.7) | 7.6 (2.8) |
| Age group, y | |||
| 5-11 | 18 938 (72.3) | 11 451 (66.7) | 7487 (82.9%) |
| 12-18 | 7267 (27.7) | 5722 (33.3) | 1545 (17.1) |
| Baseline BMIb | |||
| Underweight | 1000 (3.8) | 629 (3.7) | 371 (4.1) |
| Normal weight | 17 074 (65.2) | 11 157 (65.0) | 5917 (65.5) |
| Overweight | 3963 (15.1) | 2655 (15.5) | 1308 (14.5) |
| Obesity | 4168 (15.9) | 2732 (15.9) | 1436 (15.9) |
| BMI z-score, mean (SD) | |||
| All measurements | 0.46 (1.16) | 0.47 (1.15) | 0.45 (1.17) |
| >1 Measurement | 0.50 (1.14) | 0.50 (1.12) | 0.45 (1.18) |
Abbreviations: AI/AN, American Indian or Alaska Native; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); GED, General Educational Development; NH/PI, Native Hawaiian or Other Pacific Islander.
“Other” as self-identified by the participant or caregiver.
A BMI of less than 18.5 indicated underweight; 18.5 to less than 25.0, normal weight; 25.0 to less than 30.0, overweight; and 30.0 or more, obesity.
Compared with the HHFKA preintervention period (n = 8939), the postintervention period (n = 6900) had a slightly larger proportion of individuals reporting White race (4386 [63.6%] vs 5380 [60.2%]) and a smaller proportion reporting Hispanic ethnicity (875 [12.7%] vs 2204 [24.7%]) (Table 1). The proportion of youths with mothers reporting at least some college education was higher in the postintervention period (5431 [78.7%] vs 5658 [63.3%]). A larger proportion of enrollment sites were in the South region of the US in the postintervention period (1608 [23.3%] vs 1028 [11.5%]) and a smaller proportion in the Northeast (1630 [23.6%] vs 2958 [33.1%]).
In the overall sample, a significant decrease was observed in the annual change in BMIz in the period following the HHFKA intervention compared with the preintervention period (−0.041; 95% CI, −0.066 to −0.016) (Figure and Table 2). Specifically, in the preintervention period, no significant change was found in the annual change in BMIz (0.004; 95% CI, −0.002 to 0.010), but in the postintervention period, a significant decrease occurred in annual BMIz (−0.036; 95% CI, −0.060 to −0.012).
Table 2. Change in BMI z-Score Following Implementation of the Healthy, Hunger-Free Kids Act of 2010 Overall and in Subgroupsa.
| Characteristic | Annual change in BMI z score (95% CI) | ||
|---|---|---|---|
| Preintervention period | Postintervention period | Postintervention period vs preintervention period | |
| Overall (N = 14 121) | 0.004 (−0.002 to 0.010) | −0.036 (−0.060 to −0.012) | −0.041 (−0.066 to −0.016) |
| US census region (n = 14 112) | |||
| Northeast | 0.026 (0.017 to 0.035) | 0 (−0.026 to 0.025) | −0.026 (−0.051 to 0) |
| Midwest | 0.003 (−0.006 to 0.012) | −0.007 (−0.033 to 0.018) | −0.010 (−0.036 to 0.016) |
| South | −0.003 (−0.027 to 0.021) | 0.006 (−0.023 to −0.035) | 0.009 (−0.021 to 0.038) |
| West | −0.037 (−0.056 to −0.018) | −0.046 (−0.071 to −0.020) | −0.009 (−0.037 to 0.019) |
| Age group (n = 14 121), y | |||
| 5-11 | −0.0003 (−0.008 to 0.007) | −0.034 (−0.059 to −0.010) | −0.034 (−0.059 to −0.009) |
| 12-18 | 0.016 (0.005 to 0.027) | −0.029 (−0.055 to −0.003) | −0.045 (−0.071 to −0.018) |
| Sex (n = 14 121) | |||
| Female | 0.015 (0.007 to 0.023) | −0.031 (−0.055 to 0.006) | −0.046 (−0.070 to −0.020) |
| Male | −0.005 (−0.013 to 0.003) | −0.042 (−0.066 to −0.018) | −0.037 (−0.062 to −0.012) |
| Median annual household income (n = 9565) | |||
| <$50 000 | 0.007 (−0.002 to 0.017) | −0.031 (−0.056 to −0.006) | −0.038 (−0.063 to −0.013) |
| ≥$50 000 | −0.0042 (−0.037 to 0.012) | −0.037 (−0.061 to −0.013) | −0.041 (−0.066 to −0.016) |
| Baseline BMI category (n = 14 121)b | |||
| Underweight or normal | −0.007 (−0.012 to −0.002) | −0.010 (−0.026 to 0.006) | −0.003 (−0.02 to 0.013) |
| Overweight or obesity | 0.009 (0.004 to 0.014) | 0.002 (−0.014 to 0.018) | −0.008 (−0.024 to 0.009) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
All models were adjusted for self-reported race, Hispanic ethnicity, cohort group, and maternal educational level. Each subgroup model was also adjusted for the corresponding covariate as a main effect in addition to including the appropriate interaction terms.
A BMI of less than 18.5 indicated underweight; 18.5 to less than 25.0, normal weight; 25.0 to less than 30.0, overweight; and 30.0 or more, obesity.
In the region subgroup model, we did not observe a significant decrease in BMIz in any specific region. In the age subgroup model, a significant difference was observed in the annual BMIz among children aged 5 to 11 years (−0.034; 95% CI, −0.059 to −0.009) as well as adolescents aged 12 to 18 years (−0.045; 95% CI, −0.071 to −0.018); this represents a reversal of the HHFKA preintervention trend among adolescents aged 12 to 18 years who had a significant increase in annual BMIz in that period (0.016; 95% CI, 0.005-0.027). In the sex subgroup model, a significant decrease in BMIz was found among females (−0.046; 95% CI, −0.071 to −0.020) and males (−0.037; 95% CI, −0.062 to −0.012), and there was a change from the preintervention increase in BMIz among females (0.015; 95% CI, 0.007-0.023). In the income subgroup model, a significant decrease in BMIz was detected in youths from families with lower income (−0.038; 95% CI, −0.063 to −0.013) and those from families with higher income (−0.041; 95% CI, −0.066 to −0.016). In the baseline BMI category subgroup model, there was no significant change in annual BMIz in the postintervention period compared with the preintervention period.
The Figure shows the estimated trend in BMIz if the HHFKA had never been implemented, that is, if the pre-HHFKA trend in BMIz had held constant after 2016. The flat trend in BMIz in the preintervention period is also reflected in the estimated counterfactual trend in the postintervention period (Figure). In contrast, the observed data in the postintervention period showed an annual decrease in BMIz.
The sensitivity analysis limited to youths contributing at least 1 BMIz measurement prior to and after the HHFKA intervention yielded similar results as the main analysis (−0.038; 95% CI, −0.085 to 0.010). The analysis using the BMI percentage as the outcome also had a similar result and interpretation as the main analysis (−0.598; 95% CI, −0.984 to −0.212), in which the increased magnitude of effect was consistent with the order-of-magnitude difference in the mean and distribution of the BMI percentage variable compared with the BMIz (eTable in Supplement 1).
Discussion
Our study suggests that the HHFKA, the first national legislation to improve the dietary quality of school meals and snacks in over 2 decades, was associated with a significant 0.041 unit-per-year decrease in BMIz compared with pre-HHFKA trends among school-aged youths across the US. We estimated a 0.036 unit-per-year decrease in BMIz in the post-HHFKA period. This finding was in contrast to the relatively flat trend in BMIz that occurred prior to HHFKA implementation, which we estimated would have continued if the HHFKA had not been implemented. Multiple evaluations of the HHFKA have shown an improvement in the dietary quality of school meals following its implementation,12,13,14 which is consistent with our findings. Our income subgroup model also showed an annual decrease in BMIz among youths living in households with an annual income of less than $50 000; a similar pattern was observed among youths living in households at or below the federal poverty level in the National Survey of Children’s Health.9 Importantly, in contrast to our study, the overall study sample of the National Survey of Children’s Health did not show an association between the HHFKA and child obesity.9 To our knowledge, our study is one of the first to evaluate the association between the HHFKA and BMIz in a large, diverse, geographically heterogenous group of school-aged youths with repeated measures of youth BMI.
Our age subgroup model showed a decrease in annual BMIz following HHFKA implementation among adolescents aged 12 to 18 years, which was the reverse of a previously observed increase during the pre-HHFKA period. This is particularly important given the assumption that this age group likely has more autonomy in purchasing out-of-school meals or snacks and thus may not be as influenced as younger children by a school-based meal and snack intervention. Our study suggests that improving the quality of school-based meals and snacks is associated with weight change among youths and corroborates findings from previous studies suggesting that the foods provided in school-based snacks and vending machines influences the dietary behaviors of adolescents.26,27
Our analysis showed a significant 0.038 unit-per-year decrease in BMIz after HHFKA implementation among youths living in households with an annual income less than $50 000 compared with a relatively flat BMIz trend in the pre-HHFKA period. This income cutoff roughly aligns with the income eligibility for free and reduced-price meals in the 2016 to 2017 school year.28 Our findings corroborate those of 2 other studies,16,17 which reported that the HHFKA was associated with reducing excess weight gain among children from low-income households, who have been shown to be at higher risk for obesity and its sequelae.
Limitations
This study has several limitations. First, our analysis included youths from several different cohort studies over the period that had different measurement and visit structures. We attempted to account for this by including core sociodemographic covariates as adjustment terms in our model, but some residual confounding may have remained. Second, there may be factors influencing youth BMI over time that were not included in our model. While we are not aware of any other policy changes broadly affecting youths with obesity at the time of HHFKA implementation, there may have been smaller programs that affected our results. Third, youths who are home schooled or attend private schools would not have been affected by the HHFKA legislation. While we did not have the granularity of data needed to specify this, we recommend that future studies exclude these youths from similar analyses. Fourth, we recognize that BMI is not purely a measure of adiposity but also comprises lean muscle mass. We did not include information on physical activity in the calculation and interpretation of BMI as we did not have these data for all participants.
Conclusions
This study found that HHFKA implementation was associated with significant decreases in child and adolescent BMIz. Increasing trends in BMIz in the pre-HHFKA period were attenuated or even reversed after HHFKA implementation in several populations; these changes could affect long-term health in these population. School meals and snacks represent a key opportunity for interventions to combat the childhood obesity epidemic given the high rates of participation in school meal programs and the significant proportion of caloric intake that youths receive at school. We recommend further evaluations quantifying the association of the HHFKA with BMI and childhood obesity risk as well as efforts by policy makers to further improve the nutritional quality of school meals.
eTable. Change in Body Mass Index as a Percentage of the 95th Percentile Following Implementation of the Healthy, Hunger-Free Kids Act of 2010
Data Sharing Statement
References
- 1.Fryar C, Carroll M, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years in the United States, 1963–1965 through 2017–2018. Health E-Stats. US Centers for Disease Control and Prevention; National Center for Health Statistics . Accessed March 31, 2022. https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf [Google Scholar]
- 2.Eagle TF, Gurm R, Goldberg CS, et al. Health status and behavior among middle-school children in a Midwest community: what are the underpinnings of childhood obesity? Am Heart J. 2010;160(6):1185-1189. doi: 10.1016/j.ahj.2010.09.019 [DOI] [PubMed] [Google Scholar]
- 3.Taber DR, Chriqui JF, Powell L, Chaloupka FJ. Association between state laws governing school meal nutrition content and student weight status: implications for new USDA school meal standards. JAMA Pediatr. 2013;167(6):513-519. doi: 10.1001/jamapediatrics.2013.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merlo C, Brener N, Kann L, McManus T, Harris D, Mugavero K. School-level practices to increase availability of fruits, vegetables, and whole grains, and reduce sodium in school meals—United States, 2000, 2006, and 2014. MMWR Morb Mortal Wkly Rep. 2015;64(33):905-908. doi: 10.15585/mmwr.mm6433a3 [DOI] [PubMed] [Google Scholar]
- 5.US Department of Agriculture . National School Lunch Program fact sheet. Accessed March 31, 2022. https://www.fns.usda.gov/nslp/nslp-fact-sheet
- 6.Cullen KW, Chen TA. The contribution of the USDA school breakfast and lunch program meals to student daily dietary intake. Prev Med Rep. 2016;5:82-85. doi: 10.1016/j.pmedr.2016.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine . Nutrition Standards and Meal Requirements for National School Lunch and Breakfast Programs: Phase I. Proposed Approach for Recommending Revisions. The National Academies Press; 2008. [PubMed] [Google Scholar]
- 8.Healthy Meals for Healthy Americans Act of . 1994. S 1614, 103rd Congress (1993-1994). Accessed March 15, 2022. https://www.congress.gov/bill/103rd-congress/senate-bill/1614
- 9.Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact of the Healthy, Hunger-Free Kids Act on obesity trends. Health Aff (Millwood). 2020;39(7):1122-1129. doi: 10.1377/hlthaff.2020.00133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Department of Agriculture . Food and Nutrition Service. Strategies for successful implementation of the Healthy, Hunger-Free Kids Act. Accessed March 31, 2022. https://www.jumpinforhealthykids.org/userfiles/file/news/HHFKA-FruitsVegetables.pdf
- 11.US Department of Agriculture . Fact sheet: Healthy, Hunger-Free Kids Act school meals implementation. Accessed March 31, 2022. https://www.usda.gov/media/press-releases/2014/05/20/fact-sheet-healthy-hunger-free-kids-act-school-meals-implementation
- 12.Gearan EC, Fox MK. Updated nutrition standards have significantly improved the nutritional quality of school lunches and breakfasts. J Acad Nutr Diet. 2020;120(3):363-370. doi: 10.1016/j.jand.2019.10.022 [DOI] [PubMed] [Google Scholar]
- 13.Mozer L, Johnson DB, Podrabsky M, Rocha A. School lunch entrées before and after implementation of the Healthy, Hunger-Free Kids Act of 2010. J Acad Nutr Diet. 2019;119(3):490-499. doi: 10.1016/j.jand.2018.09.009 [DOI] [PubMed] [Google Scholar]
- 14.Cohen J, Schwartz MB. Documented success and future potential of the Healthy, Hunger-Free Kids Act. J Acad Nutr Diet. 2020;120(3):359-362. doi: 10.1016/j.jand.2019.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaudrin N, Lloyd K, Yedidia MJ, Todd M, Ohri-Vachaspati P. Impact of the 2010 US Healthy, Hunger-Free Kids Act on school breakfast and lunch participation rates between 2008 and 2015. Am J Public Health. 2018;108(1):84-86. doi: 10.2105/AJPH.2017.304102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson AS, Weden MM, Cabreros I, Datar A. Association of the Healthy, Hunger-Free Kids Act of 2010 with body mass trajectories of children in low-income families. JAMA Netw Open. 2022;5(5):e2210480. doi: 10.1001/jamanetworkopen.2022.10480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanchez-Vaznaugh EV, Matsuzaki M, Braveman P, et al. School nutrition laws in the US: do they influence obesity among youth in a racially/ethnically diverse state? Int J Obes (Lond). 2021;45(11):2358-2368. doi: 10.1038/s41366-021-00900-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Department of Agriculture; Food and Nutrition Service . Meal requirements under the NSLP & SBP: Q&A for program operators updated to support the transitional standards effective July 1, 2022. Accessed August 10, 2022. https://www.fns.usda.gov/cn/sp052022-questions-answers-program-operators
- 19.Gillman MW, Blaisdell CJ. Environmental influences on child health outcomes, a research program of the National Institutes of Health. Curr Opin Pediatr. 2018;30(2):260-262. doi: 10.1097/MOP.0000000000000600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 21.US Census Bureau . 2010 Census regions and divisions of the United States. October 8, 2021. Accessed June 15, 2022. https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html
- 22.Causality PJ. Models, Reasoning, and Inference. 2nd ed. Cambridge University Press; 2009. [Google Scholar]
- 23.Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: a new growth chart. Pediatrics. 2012;130(6):1136-1140. doi: 10.1542/peds.2012-0596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2- to 4-year-old children. J Pediatr. 2017;188:50-56.e1. doi: 10.1016/j.jpeds.2017.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention . Growth chart training: SAS program for the 2000 CDC growth charts that includes the extended BMI calculations. Accessed June 1, 2022. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
- 26.Kubik MY, Lytle LA, Hannan PJ, Perry CL, Story M. The association of the school food environment with dietary behaviors of young adolescents. Am J Public Health. 2003;93(7):1168-1173. doi: 10.2105/AJPH.93.7.1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wechsler H, Devereaux RS, Davis M, Collins JL. Using the school environment to promote physical activity and healthy eating. Prev Med. 2000;31(2):S121-S137. doi: 10.1006/pmed.2000.0649 [DOI] [Google Scholar]
- 28.US Department of Agriculture . Food and Nutrition Service. Child nutrition programs income eligibility guidelines (2016-2017). Accessed June 15, 2022. https://www.fns.usda.gov/cn/fr-032316
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Change in Body Mass Index as a Percentage of the 95th Percentile Following Implementation of the Healthy, Hunger-Free Kids Act of 2010
Data Sharing Statement