Abstract
Opioids like fentanyl are used both alone and in combination with other drugs to induce anesthesia and treat pain. It is also combined with heroin or cocaine when used recreationally. It starts acting quickly, and its effects usually wear off within 2 h. A typical pharmaceutical strategy for controlling the physical pain and psychological discomfort related to dental treatments, including surgery, is moderate (conscious) sedation. This study aimed to assess knowledge and awareness about dental applications of fentanyl among dental students. A 15-question survey was sent through an online platform to about 150 dental students in Tamil Nadu. Data were collected over a 6-month period and compared using SPSS software by IBM. The results were statistically analyzed and graphically interpreted. From the results obtained, we can observe that from the respondents of the current survey, 52% were undergraduates and 48% were postgraduate dental students. About 93% of them were aware of the fact that fentanyl comes under opioid analgesics, and 82% were aware that it is mostly used in case of pediatric patients. About 81% of the participants were aware that apart from benzodiazepines, fentanyl can also be used in combination with general anesthesia in dentistry. This study revealed that most of the participants are aware of the commonly used anesthesia and analgesia such as fentanyl in dental practices. However, more continuing dental education programs and seminars must be conducted to further enhance the knowledge and understanding of dental students about drugs such as fentanyl in dental practice.
Keywords: Dental applications, dosage, fentanyl, innovation, prosthodontics, sedation
INTRODUCTION
Fentanyl is one of the robust pharmacologic agents, which is actually 50–100 times more potent than its other counterparts. It has an analgesic and sedative property with a rapid onset of action. A small dose of even about 100 micrograms can produce an equivalent amount of analgesia that 10 mg of morphine can provide.[1] Clinically, it is most commonly used in intubated patients as a sedative and in severe pain in renal failure patients owing to its property of hepatic elimination. Sometimes, fentanyl is also prescribed in cases of severe pain among patients who have developed opioid tolerance.[2] As a sedative, the medication is usually administered by a drip. Finally, the application of fentanyl also includes the treatment of epilepsy. That is, as a part of therapeutic neuroleptanalgesia, in combination with specific neuroleptic medicines. This explains the indications, severe adverse effects, mechanism of action, and toxicity of fentanyl such that the providers can guide patients’ treatment toward the best possible outcomes.[3,4]
Fentanyl is similar to morphine but delivers more analgesia. The potency of this powerful agent is often 50–100 times higher.[3] Fentanyl, on the other hand, has very distinct characteristics and pharmacokinetics. Due to its largely hepatic clearance, it is most commonly used as a sedative. Due to its adaptability in titration circumstances, it is most typically delivered as a drip when used as a sedative.[5] When fentanyl is used as a sedative in patients who require artificial ventilation, it may be necessary to administer high doses. Fentanyl is often used as a perioperative premedication for procedures that are likely to induce discomfort.[6] Finally, fentanyl is sometimes used to treat epilepsy. That is, as a part of therapeutic neuroleptanalgesia, in combination with specific neuroleptic medicines.[7]
Fentanyl is also like other opioid drugs. Fentanyl molecules act by targeting a subclass of opioid receptors in the body, many of which are in the brain inside specialized structures, and are commonly involved in emotion control, sensation of pain, and, more importantly, reward.[8] It can, however, activate additional opioid receptors, including delta and commonly the kappa receptor systems. Analgesia is produced when these receptors, particularly the Mu-receptors, are activated. In addition, dopamine, which acts as a neurotransmitter, is elevated in the centers of the brain, eliciting the conventional exhilaration and relaxing effects, and is usually linked to drug addiction.
One of the most common oral surgery operations is the extraction of impacted mandibular third molars. Regardless of the procedure's difficulties, postoperative pain is so common that it is frequently used as a tool for researching the quality of analgesia of various medicines or physical techniques.[9,10]
Transdermal type of drug delivery system is a commonly known concept, but it is a concept with a wide range of possibilities in postoperative pain control.[11] The fentanyl transdermal system (FTS) is one mode of percutaneous drug delivery as a transdermal patch with an increased dosage of fentanyl, a strong, quickly effective opiate.[12] FTS contains a drug reservoir containing fentanyl in a gel-based matrix, used as a releasing membrane that permits surface-limited and time-limited drug absorption. It produces pleasure and dysphoria, and a sustained as well as a consistent analgesic action.[13] The prescribed dosage of the patch is 50 μg/h.
Fentanyl is also used as a pain reliever and in combination with other anesthetics. It has a quick onset and often lasts <2 h. Moderate (conscious) sedation is a typical pharmaceutical strategy of lowering anxiety and chronic pain during oral operations, such as surgery.[14] The safety of administering moderate sedation in dentistry clinics, while developing patient response to verbal as well as tactile stimuli, is widely documented, with few problems.[15] Fentanyl with midazolam is the most commonly preferred medication alternative for providing moderate intravenous (IV) sedation.[16,17] This study aimed to assess knowledge and awareness about dental applications of fentanyl among dental students. Our research team has an extensive knowledge and research expertise that has translated as high-quality publications.[18,19,20,21,22,23,24]
MATERIALS AND METHODS
The results of this study were based on the responses of survey participants who completed an online survey. The study's advantages include the availability of data and similar ethnicity. The study's limitations include the fact that it is a single-centered study with no assessment of geographic regions or trends. The study has been approved by Saveetha University's Ethics Board. This study was approved by the University Ethical Clearance Committee (number IHEC/SDC/PROSTHO/21/089). The following data were examined for the study: a reviewing expert used images to cross-verify all applicable responses for the study and to cross-verify the required data. To reduce sample bias, measures were implemented. The study was carried out using both internal and external validation. The statistical software used for this study is the SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY:IBM Corp), and the results were systematically analyzed and graphically represented.
RESULTS
The sample size was 150 participants. From the results obtained, we can observe that from the respondents of the current survey, 52% were undergraduates and 48% were postgraduate dental students. About 93% of them were aware of the fact that fentanyl comes under opioid analgesics, and 82% were aware that it is mostly used in case of pediatric patients. About 81% of the participants were aware that apart from benzodiazepines, fentanyl can also be used in combination with general anesthesia in dentistry. Only 59% of them were aware of the adverse effects of fentanyl. From the correlation between qualification of the participants and the knowledge of adverse effects of fentanyl, only 24% of the undergraduates were aware of them, whereas 35% of the postgraduates were aware. From the results, we can know that most of them were aware about the applications of fentanyl, but the area to be emphasized is the complete knowledge among the dental students regarding the drugs commonly used for anesthesia and analgesia in dentistry such as fentanyl.
DISCUSSION
A study by Bennett in 1972 stated that remifentanil as well as fentanyl can produce less inflammatory effects of dental surgeries to the patients. The drug also revealed intraoperative hemodynamic response and postoperative analgesic effects on the patients.[25] These results also coincide with our findings, although adults were not included in the current study.
Pandey et al. concluded that when administered and monitored by a qualified anesthetist, IV sedation of cooperative healthy pediatric patients with ketamine, fentanyl, and nitrous oxide–oxygen appears to be an effective and safe sedation modality as an alternative to general anesthesia.[26] The same result is found in the present study. These results also coincide with our findings.
Similarly, Melloni revealed in his study that during unpleasant, uncomfortable, or prolonged dental operations, fentanyl reduces chronic pain, discomfort, and negative psychological sensations by providing appropriate sedation, forgetfulness, and analgesia.[27] These results coincide with the findings in our study [Graph 1-7].
Graph 1.

Bar graph representation of frequencies of males and females who took up the survey – X-axis represents gender and Y-axis represents the percentage of males and females who had participated in the survey on a scale of 1–100. About 41.61% were male and 58.39% were female
Graph 7.

Bar graph showing the response given by the participants when asked if they are aware of the fact that fentanyl and midazolam can be used in combination with sedate pediatric patients. About 58.5% of them answered yes and the remaining answered no
Graph 2.

Bar graph showing the response given by the participants when asked if they are aware of the fact that fentanyl is used in dentistry. About 84.32% of them answered yes and the remaining answered no
Graph 3.

Bar graph showing the response given by the participants when asked if they are aware of the fact that fentanyl can be administered by intravenous or as a bonus dose in pediatric patients. About 78.32% of them answered yes and the remaining answered no
Graph 4.

Bar graph showing the response given by the participants when asked which group of drugs fentanyl comes under. About 95.4% of them answered opioid analgesic and the remaining answered other groups of drugs
Graph 5.

Bar graph showing the response given by the participants when asked if they are aware of the fact that fentanyl is a potent opioid agonist and is used for rapid and strong analgesia. About 80% of them answered yes and the remaining answered no
Graph 6.
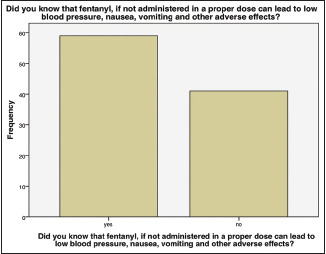
Bar graph showing the response given by the participants when asked if they are aware of the fact that fentanyl, if not administered in proper dose, can lead to low blood pressure and other adverse effects. About 59.7% of them answered yes and the remaining answered no
Limitations of the study are as follows: there was noninclusion of some data in the study that were not clear of certain reporting parameters. There was no limitation for external validity. The generalizability of this study results is possible. However, the drawback of the current study is the small sample size. A larger study with more subjects in different ethnic backgrounds can be assessed.
Future prospects of this study include overcoming the limitations and throwing the limelight on knowledge of fentanyl among dentists, as it is important for a dental practitioner. In the hospital setting, fentanyl is a commonly utilized narcotic. Health-care workers should have a complete knowledge of new opioid prescribing laws, which can lead to medicolegal issues including the loss of prescription privilege. Fentanyl medication can be beneficial and adverse outcomes avoided or treated if they occur with interprofessional coordination of actions and open communication.
CONCLUSION
This study revealed that most of the participants are aware of the commonly used anesthesia and analgesia such as fentanyl in dental practices. However, more continuing dental education programs and seminars must be conducted to further enhance the knowledge and understanding of dental students about drugs such as fentanyl in dental practice.
Financial support and sponsorship
The present study is funded by the:
Saveetha Institute of Medical and Technical Sciences
Saveetha Dental College and Hospitals
Saveetha University
Satyam Enterprises, Chennai.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors acknowledge Saveetha University for all the help and support.
REFERENCES
- 1.Lobb D, Ameli N, Ortiz S, Lai H. Comparison of the effects of target-controlled infusion-remifentanil/midazolam and manual fentanyl/midazolam administration on patient parameters in dental procedures. J Dent Anesth Pain Med. 2022;22:117–28. doi: 10.17245/jdapm.2022.22.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deshmukh M, Rajaraman V, Duraisamy R, Maiti S. Knowledge, awareness, and attitude of dentists toward use of denture adhesives in Tamil Nadu: A questionnaire survey. J Adv Pharm Technol Res. 2022;13(Suppl S1):243–8. doi: 10.4103/japtr.japtr_148_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moran JH, Marshall BM. A report on clinical uses of droperidol and fentanyl. Can Anaesth Soc J. 1966;13:272–81. doi: 10.1007/BF03003550. [DOI] [PubMed] [Google Scholar]
- 4.Clotz MA, Nahata MC. Clinical uses of fentanyl, sufentanil, and alfentanil. Am J Health Syst Pharm. 1991;48:2021–4. [PubMed] [Google Scholar]
- 5.Barnes NM, Bunce KT, Naylor RJ, Rudd JA. The actions of fentanyl to inhibit drug-induced emesis. Neuropharmacology. 1991;30:1073–83. doi: 10.1016/0028-3908(91)90136-y. [DOI] [PubMed] [Google Scholar]
- 6.Boas RA, Villiger JW. Clinical actions of fentanyl and buprenorphine. The significance of receptor binding. Br J Anaesth. 1985;57:192–6. doi: 10.1093/bja/57.2.192. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal S, Ashok V, Maiti S, Agarwal V. Dentists’ Preference toward Fixed Versus Removable Implant Prosthesis on Edentulous Jaws to Improve Quality of Life? J Long Term Eff Med Implants. 2022;33:83–9. doi: 10.1615/JLongTermEffMedImplants.2022038746. doi: 10.1615/JLongTermEffMedImplants. [DOI] [PubMed] [Google Scholar]
- 8.Bilfinger TV, Fimiani C, Stefano GB. Morphine's immunoregulatory actions are not shared by fentanyl. Int J Cardiol. 1998;64:S61–6. doi: 10.1016/s0167-5273(98)00037-0. [DOI] [PubMed] [Google Scholar]
- 9.Canning HB, Frost DE, McDonald DK, Joyner RW. Comparison of the use of nalbuphine and fentanyl during third molar surgery. J Oral Maxillofac Surg. 1988;46:1048–50. doi: 10.1016/0278-2391(88)90449-1. [DOI] [PubMed] [Google Scholar]
- 10.Sivakumar N, Ganapathy D, Pandurangan KK, Velayudhan A. Awareness on commonly used sedatives hypnotic in dental practices among dental students. J Pharm Res Int. 2020;32:188–96. [Google Scholar]
- 11.Todorovic VS, Vasovic M, Andric M, Todorovic L, Kokovic V. Efficacy of fentanyl transdermal patch in pain control after lower third molar surgery: A preliminary study. Med Oral Patol Oral Cir Bucal. 2016;21:e621–5. doi: 10.4317/medoral.21161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agarwal S, Ashok V, Maiti S, Agarwal V. Dentists’ Preference toward Fixed Versus Removable Implant Prosthesis on Edentulous Jaws to Improve Quality of Life? J Long Term Eff Med Implants. 2022;33:83–9. doi: 10.1615/JLongTermEffMedImplants.2022038746. doi: 10.1615/JLongTermEffMedImplants. [DOI] [PubMed] [Google Scholar]
- 13.Romualdi P, Santi P, Candeletti S. Alghedon fentanyl transdermal system. Minerva Med. 2017;108:169–75. doi: 10.23736/S0026-4806.16.04930-2. [DOI] [PubMed] [Google Scholar]
- 14.Frederickson GC. Diazepam in Combination with Meperidine or Fentanyl: A Double Blind Clinical Evaluation of Administration and Recovery: A Thesis Submitted in Partial Fulfillment. In Oral Surgery. 1974 [Google Scholar]
- 15.Göktay O, Satilmiş T, Garip H, Gönül O, Göker K. A comparison of the effects of midazolam/fentanyl and midazolam/tramadol for conscious intravenous sedation during third molar extraction. J Oral Maxillofac Surg. 2011;69:1594–9. doi: 10.1016/j.joms.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Hargreaves KM, Dionne RA, Mueller GP, Goldstein DS, Dubner R. Naloxone, fentanyl, and diazepam modify plasma beta-endorphin levels during surgery. Clin Pharmacol Ther. 1986;40:165–71. doi: 10.1038/clpt.1986.159. [DOI] [PubMed] [Google Scholar]
- 17.George A, Kumar N, Ganapathy D. Analgesic effect of dermatological patch in orthodontic Patients. Eur J Mol Clin Med. 2021;8:441–8. [Google Scholar]
- 18.Ponnanna AA, Maiti S, Rai N, Jessy P. Three-dimensional-printed malo bridge: Digital fixed prosthesis for the partially edentulous maxilla. Contemp Clin Dent. 2021;12:451–3. doi: 10.4103/ccd.ccd_456_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aparna J, Maiti S, Jessy P. Polyether ether ketone – As an alternative biomaterial for Metal Richmond crown-3-dimensional finite element analysis. J Conserv Dent. 2021;24:553–7. doi: 10.4103/jcd.jcd_638_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merchant A, Ganapathy DM, Maiti S. Effectiveness of local and topical anesthesia during gingival retraction. Braz Dent Sci. 2022;25:e2591. [Google Scholar]
- 21.Kasabwala H, Maiti S, Ashok V, Sashank K. Data on dental bite materials with stability and displacement under load. Bioinformation. 2020;16:1145–51. doi: 10.6026/973206300161145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwal S, Maiti S, Ashok V. Correlation of soft tissue biotype with pink aesthetic score in single full veneer crown. Bioinformation. 2020;16:1139–44. doi: 10.6026/973206300161139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal S, Ashok V, Maiti S. Open- or closed-tray impression technique in implant prosthesis: A dentist's perspective. J Long Term Eff Med Implants. 2020;30:193–8. doi: 10.1615/JLongTermEffMedImplants.2020035933. [DOI] [PubMed] [Google Scholar]
- 24.Rupawat D, Maiti S, Nallaswamy D, Sivaswamy V. Aesthetic outcome of implants in the anterior zone after socket preservation and conventional implant placement: A retrospective study. J Long Term Eff Med Implants. 2020;30:233–9. doi: 10.1615/JLongTermEffMedImplants.2020035942. [DOI] [PubMed] [Google Scholar]
- 25.Bennett CR. A clinical evaluation of fentanyl for outpatient sedation in dentistry. Oral Surg Oral Med Oral Pathol. 1972;34:880–5. doi: 10.1016/0030-4220(72)90226-5. [DOI] [PubMed] [Google Scholar]
- 26.Pandey RK, Padmanabhan MY, Saksena AK, Chandra G. Midazolam-fentanyl analgo-sedation in pediatric dental patients – A pilot study. J Clin Pediatr Dent. 2010;35:105–10. doi: 10.17796/jcpd.35.1.t275680587226k66. [DOI] [PubMed] [Google Scholar]
- 27.Maiti S, Rai N, Appanna P, Jessy P. Digital Telescopic Denture- A Viable Treatment Modality of Preventive Prosthodontics: Clinical Report. Ann Dent Spec. 2022;10:1–4. [Google Scholar]


