Abstract
Importance
COVID-19 vaccination has been associated with various adverse outcomes. Although studies have reported cases of arrhythmia after COVID-19 vaccination, the precise underlying mechanism remains to be elucidated.
Objective
Here, we report the case of a patient who developed atrial fibrillation after receiving the mRNA-1273 vaccine and describe our findings in light of relevant cases in the literature.
Design, Setting, and Participants
This is a case report and a review of the relevant literature. A 55-year-old woman presented to our clinic with a history of paroxysmal atrial fibrillation, hypertension, and mild mitral valve prolapse. The patient developed atrial fibrillation 3 days after receiving a COVID-19 vaccine. She was diagnosed with moderate-to-severe tricuspid regurgitation and severe mitral regurgitation, and underwent valve repair surgery. To obtain relevant articles (December 2020 through August 2022), we searched the following key words on PubMed: atrial fibrillation and COVID-19 vaccination.
Results
A total of 5 relevant case reports were identified. COVID-19 vaccination led to arrhythmia, including atrial fibrillation, within 14 days.
Conclusions and Relevance
Cases of patients developing arrhythmia after COVID-19 vaccination have been increasingly reported. Although the underlying mechanism remains unclear, we hypothesize that mRNA vaccination may lead to arrhythmia and associated valve diseases. Thus, before administering mRNA-1273 vaccines to patients with a history of valvular heart disease or atrial fibrillation, the patients’ cardiologists must be consulted.
Keywords: atrial fibrillation, valvular heart disease, COVID-19 vaccination, case report
Plain Language Summary
Question What is the risk of atrial fibrillation (AF) after COVID-19 vaccination?
Findings Among a total of 6 cases (present case + previous cases [n = 5]) on AF related to COVID-19 vaccination, AF developed after vaccination in 5 patients, and a previous history of AF led to severe cardiovascular complications after vaccination in 1 patient.
Meaning The present case and cases in the literature reviewed herein suggest that COVID-19 vaccination may lead to arrhythmia.
Introduction
The lipid-nanoparticle-encapsulated mRNA-based COVID-19 vaccine mRNA-1273 (Moderna, Inc.) encodes the prefusion spike glycoprotein (S) of SARS-CoV-2. This vaccine remains under surveillance for potential unprecedented adverse outcomes.1 The possible side effects of this vaccine include fatigue, muscle pain, headache, chills, inflammation/edema at the injection site, joint pain, and fever.2 Here, we report the case of a patient who developed atrial fibrillation (AF) after receiving the mRNA-1273 vaccine. We further describe our findings in light of relevant literature on the development of AF after COVID-19 vaccination. The study already obtained patient’s informed consent to publish the case report and any accompanying images. It also has been reviewed and approved by the Institutional Ethics Committee Review Board.
Case Presentation
A 55-year-old Asian woman with a history of paroxysmal AF, hypertension, and mild mitral valve prolapse (2004) presented to our hospital with complaints of palpitations, acute chest tightness, and dyspnea. Three days before presentation, the patient had received her first dose of mRNA-1273. Initially, she noted palpitations, which did not resolve within 24 hours; subsequently, she started experiencing acute chest tightness and dyspnea. The patient had no known allergies, had received all standard vaccinations, and had no previous history of any adverse reactions.
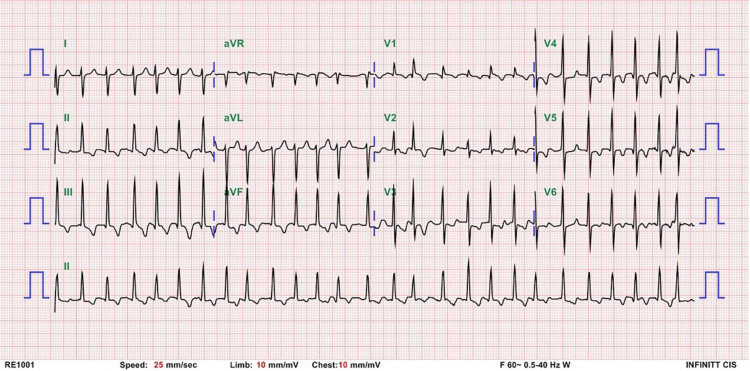
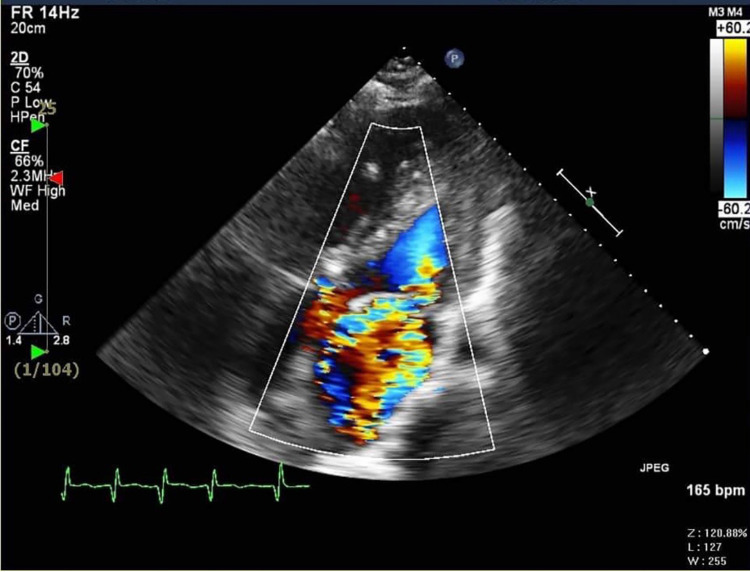
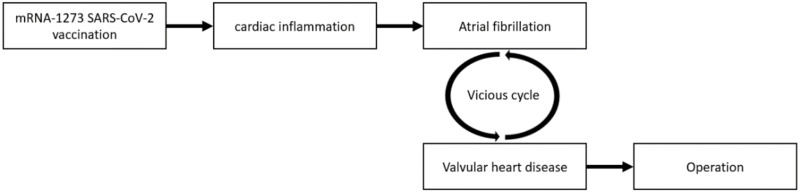
Upon admission, the patient was hemodynamically stable and afebrile. Electrocardiographic findings indicated AF (Figure 1). Laboratory examinations revealed a high-sensitivity troponin level of 0.045 (normal range < 0.026) ng/mL. Within 24 hours, the troponin level peaked to 0.086 ng/mL. The findings related to complete blood cell count with differential and C-reactive protein level were normal. Chest X-ray showed an enlarged cardiomediastinal silhouette (Figure 2). Echocardiogram indicated normal left ventricular ejection fraction (63%), moderate-to-severe tricuspid regurgitation (TR), and severe mitral regurgitation (MR) with an eccentric jet direction toward the atrial septum (Figure 3). The comparison between her present and previous (2012) echocardiograms revealed moderate eccentric MR and mild TR in 2012.
Figure 1.
Electrocardiogram Indicating Atrial Fibrillation.
Figure 2.
Chest X-Ray Showing an Enlarged Cardiomediastinal Silhouette.
Figure 3.
Echocardiogram Indicating Severe Mitral Regurgitation.
A coronary angiography was performed, which indicated severe MR, pulmonary hypertension (mean pulmonary arterial pressure, 66 mmHg), and insignificant coronary artery disease. During admission, her normal cardiac rhythm could not be restored and permanent AF was diagnosed. Because of the permanent AF with persistent palpitations, severe MR, and moderate-to-severe TR, the patient underwent mitral valve repair surgery, tricuspid valve annuloplasty, and bilateral maze ablation on day 14 of admission. She was discharged from the hospital on day 27. The patient was receiving aspirin, bisoprolol, and amiodarone and was followed up at outpatient clinic.
Discussion
The Vaccine Adverse Event Reporting System (VAERS) data in the USA was analyzed by some studies and reported more than 2000 incidences of AF post-COVID-19 vaccination.3 It is always of debate to consider such arrhythmia due to chance or vaccine induced. Since there is no way to prove a direct association between vaccines and arrhythmias currently, we have to rely on a few published case reports.
AF is a common arrhythmia and can be diagnosed by physicians through electrocardiography. Patient with AF may present with palpitations, fatigue, dizziness, and dyspnea or be asymptomatic.4 The primary risk factors for AF include diabetes, hypertension, coronary artery disease, heart valvular disease, and congestive heart failure.5 Although our patient had a history of valvular heart disease, her clinical condition was relatively stable before vaccination. Our case is rare in terms of the adverse effects of mRNA-1273. We searched PubMed for articles (December 2020 through August 2022) on AF after COVID-19 vaccination. A total of 20 articles were identified; after assessing their titles and abstracts, 5 articles were selected for further review. Data regarding the patients’ age, sex, symptoms, echocardiographic and electrocardiographic findings, vaccine type and dose, diagnosis, and treatment were collected (Table 1).
Table 1.
COVID-19 Vaccine and Atrial Fibrillation
| Pat. No. | Author | Year | Age/Sex | Comorbidities | Echo | Symptoms | Vaccine | Onset | Primary Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| 114 | Li et al | 2021 | 31/M | Marfan syndrome | N/A | Palpitations and chest pain | Vero cell/first dose | Day 1 (after 8 h) | AF with a rapid ventricular rate and occasional premature ventricular beats | Medication for sinus rhythm conversion and rate control |
| 215 | Yamamoto et al | 2021 | 64/F | Colorectal cancer, diabetes mellitus, and obesity | N/A | Palpitations, respiratory distress, decreased urine output, lower limb (both) edema, and fever | BNT162b2/first dose | Day 6 | Thyrotoxic crisis complicated with AF and heart failure | Thiamazole, potassium iodine, corticosteroid, furosemide, and carvedilol |
| 316 | Scheuermeyer et al | 2022 | 49/M | N/A | Pericardial effusion | Palpitation and chest discomfort | mRNA-1273 (Moderna)/second dose | Day 8 | Pericarditis related to mRNA-1273 SARS-CoV-2 vaccination | Cardioversion (for AF), rivaroxaban, and procainamide (second AF) |
| 417 | Choi et al | 2022 | 22/F | N/A | Pericardial effusion | Fever, myalgia, sore throat, diarrhea, vomiting, and chest pain | AstraZeneca/first dose | Day 8 (symptoms; AF on day 14) | Multisystem inflammatory syndrome in adults | Cardioversion (for AF) |
| 518 | Yoshida et al | 2022 | 83/F | Persistent AF (receiving rivaroxaban) | No thrombus in the left atrial appendage | Right hemiplegia and motor aphasia | BNT162b2/first dose | Day 3 | Left middle cerebral artery infarction | Intravenous recombinant tissue-plasminogen activator, mechanical thrombectomy, and rivaroxaban |
| 6 | Our case | 2022 | 55/F | Paroxysmal AF, hypertension, and mitral valve prolapse | Severe MR and moderate-to-severe TR | Palpitations, chest tightness, and dyspnea | mRNA-1273 (Moderna)/first dose | Day 3 | Permanent AF, severe MR, moderate-to-severe TR | Mitral valve repair, tricuspid valve annuloplasty, and bilateral maze ablation |
Abbreviations: AF, atrial fibrillation; M, male; F, female; Echo, transthoracic echocardiography; MR, mitral regurgitation; N/A, not assessed; TR, tricuspid regurgitation.
Of the total 5 patients (men, 2; mean age, 49.8 years; median age, 49 years), 3 received an mRNA vaccine, whereas 1 received Vero cell vaccine and 1 received AstraZeneca vaccine. All patients developed symptoms within 2 weeks of vaccination. Of them, 4 received the first dose, and 1 received the second dose. Most patients presented with chest pain and palpitations. Among the patients, 1 (patient 1) had a history of Marfan syndrome and underwent Bentall surgery and mitral valve replacement; 1 patient (patient 2) had a history of colorectal cancer, diabetes mellitus, and obesity; and 1 patient (patient 5) had been receiving anticoagulants for persistent AF.
Patient 1 was diagnosed with AF after receiving a Vero cell vaccine. After treatment, his arrhythmia persisted with occasional premature ventricular beats. Patient 2 was diagnosed with thyrotoxic crisis complicated by AF and heart failure after mRNA vaccination. Patient 3 was diagnosed with pericarditis. He received cardioversion at the first incidence of AF and appropriate medication for recurrent AF. Patient 4 was diagnosed with multisystem inflammatory syndrome in adults in addition to AF. She received 2 sessions of cardioversion, and her cardiac rhythm was restored to a sinus rhythm. Finally, patient 5, who had a history of AF, was diagnosed as having left middle cerebral artery infarction after vaccination.
Except for patient 5 who had a history of AF, all patients developed AF after vaccination. Although their diagnoses vary, their case reports indicate the development of arrhythmia and associated symptoms after COVID-19 vaccination.
As mentioned, our patient experienced palpitations, chest tightness, and dyspnea within 3 days of vaccination. She was eventually diagnosed with AF. Her echocardiogram revealed severe MR. Thus, we performed mitral valve replacement.
With the increasing number of mRNA vaccines administered worldwide, an increasing number of studies have reported the development of acute cardiac outcomes, such as myocarditis or arrhythmia, after vaccination.6 Furthermore, on the basis of endomyocardial biopsy findings, a case of intramyocardial inflammation after COVID-19 vaccination has been reported.7 Another study indicated that mRNA vaccines increase the levels of the biomarkers of cardiac inflammation in the endothelium.8
The mechanisms underlying AF remain poorly understood. Some studies have suggested alterations in ion channel function, calcium homeostasis, and atrial structure as well as atrial remodeling as the possible mechanisms underlying AF.9,10 Furthermore, local and systemic inflammation and various inflammatory biomarkers have been associated with AF.11 Patients with degenerative MR may present with AF (linearized annual incidence rate, 5%). Moreover, valvular lesions may lead to AF.12 Notably, AF leads to atrial remodeling with fibrosis, stretch, and electrical changes. Therefore, AF may cause left atrial and mitral annular dilatation, resulting in inadequate leaflet adaptation and impaired mitral annulus dynamics, which leads to severe MR.13
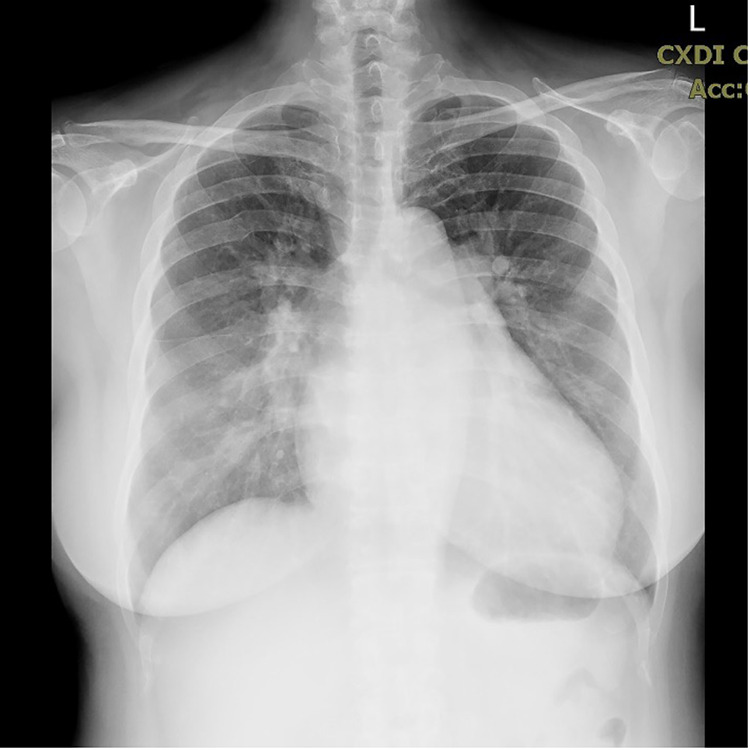
We propose the following hypothetical mechanism on the basis of a strong chronological association among the events that led to AF in our patient: the patient received the mRNA-1273 vaccine, which might have induced local or systemic inflammation, such as cardiac inflammation of the endothelium. This inflammation led to AF, which persisted despite treatment. A vicious cycle might have been triggered between the permanent AF and her history of mitral valve prolapse. This worsened the MR, which necessitated valve replacement (Figure 4).
Figure 4.
Hypothetical Mechanism in the case.
Limitations
The generalizability of these findings is limited by the small number of cases reported. The lack of standardization of reported variables among published cases makes it challenging to draw conclusions about the hypothetical mechanism of this condition.
Conclusions
The findings of the present and previous case reports may be useful for clinicians, the general public, and policymakers. The mRNA vaccines are relatively new to us, and we are still learning the adverse event profile. More research is needed to confirm such adverse events. We propose that mRNA vaccination is associated with cardiac endothelial inflammation, which may lead to arrhythmia, including AF. If patients have any valvular heart disease, a vicious cycle may develop between AF and the disease. The vital role of vaccination for COVID-19 prevention is undeniable. Thus, the mRNA-1273 vaccine should be administered to patients with a history of valvular heart disease or AF under consulting their cardiologists for potential side effects.
Ethics and Consent Statements
The study already obtained patient’s informed consent to publish the case report and any accompanying images. It also has been reviewed and approved by the Institutional Ethics Committee Review Board.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Baden LR, El Sahly HM, Essink B., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2020;384(5):403–416. doi: 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beatty AL, Peyser ND, Butcher XE, et al. Analysis of COVID-19 Vaccine Type and Adverse Effects Following Vaccination. JAMA Network Open. 2021;4(12):e2140364–e64. doi: 10.1001/jamanetworkopen.2021.40364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajmera KM. Association between COVID-19 Vaccine and New-Onset Atrial Fibrillation. Cardiol Cardiovasc Med. 2022;6:1–6. [Google Scholar]
- 4.Baman JR, Passman RS. Atrial Fibrillation. JAMA. 2021;325(21):2218. doi: 10.1001/jama.2020.23700 [DOI] [PubMed] [Google Scholar]
- 5.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent Risk Factors for Atrial Fibrillation in a Population-Based Cohort: the Framingham Heart Study. JAMA. 1994;271(11):840–844. doi: 10.1001/jama.1994.03510350050036 [DOI] [PubMed] [Google Scholar]
- 6.Patone M, Mei XW, Handunnetthi L, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baumeier C, Aleshcheva G, Harms D, et al. Intramyocardial Inflammation after COVID-19 Vaccination: an Endomyocardial Biopsy-Proven Case Series. Int J Mol Sci. 2022;23(13):6940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gundry SR. Observational Findings of PULS Cardiac Test Findings for Inflammatory Markers in Patients Receiving mRNA Vaccines. Circulation. 2021;144(Suppl_1):A10712–A12. [Google Scholar]
- 9.Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124(20):2264–2274. doi: 10.1161/circulationaha.111.019893 [DOI] [PubMed] [Google Scholar]
- 10.Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev. 2011;91(1):265–325. doi: 10.1152/physrev.00031.2009 [DOI] [PubMed] [Google Scholar]
- 11.Zhou X, Dudley SC. Evidence for Inflammation as a Driver of Atrial Fibrillation. Front Cardiovasc Med. 2020;7. doi: 10.3389/fcvm.2020.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grigioni F, Avierinos J-F, Ling LH, et al. Atrial fibrillation complicating the course of degenerative mitral regurgitation: determinants and long-term outcome. J Am Coll Cardiol. 2002;40(1):84–92. [DOI] [PubMed] [Google Scholar]
- 13.Deferm S, Bertrand PB, Verbrugge FH, et al. Atrial Functional Mitral Regurgitation: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(19):2465–2476. doi: 10.1016/j.jacc.2019.02.061 [DOI] [PubMed] [Google Scholar]
- 14.Li K, Huang B, Ji T, Xu SG, Jiang W. A Postoperative Man with Marfan Syndrome with Palpitations and Chest Pain After Receiving the SARS-CoV-2 Vaccine. Infect Drug Resist. 2021;14:2953–2956. In eng. doi: 10.2147/idr.S323280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamamoto K, Mashiba T, Takano K, et al. A Case of Exacerbation of Subclinical Hyperthyroidism after First Administration of BNT162b2 mRNA COVID-19 Vaccine. Vaccines. 2021;9(10). In eng. doi: 10.3390/vaccines9101108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scheuermeyer FX, Yoo J, Greene M, O’Donnell S. Atrial fibrillation as a precursor of mRNA-1273 SARS-CoV-2 vaccine-induced pericarditis. CJEM. 2022;24(2):230–232. In eng. doi: 10.1007/s43678-021-00250-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi YK, Moon JY, Kim J, et al. Postvaccination Multisystem Inflammatory Syndrome in Adult with No Evidence of Prior SARS-CoV-2 Infection. Emerg Infect Dis. 2022;28(2):411–414. In eng. doi: 10.3201/eid2802.211938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshida K, Tanaka K, Suto Y, Fukuda H. Repeated Cardioembolic Stroke after COVID-19 mRNA Vaccination: a Case Report. J Stroke Cerebrovasc Dis. 2022;31(2):106233. In eng. doi: 10.1016/j.jstrokecerebrovasdis.2021.106233 [DOI] [PMC free article] [PubMed] [Google Scholar]