Abstract
Background
Many high-income countries are heavily dependent on internationally trained doctors to staff their healthcare workforce. Over one-third of doctors practising in the UK received their primary medical qualification abroad. Simultaneously, an average of around 2.1% of doctors leave the UK medical workforce annually to go overseas. The aim of this study was to identify the drivers and barriers of international migration of doctors to and from the UK.
Methods
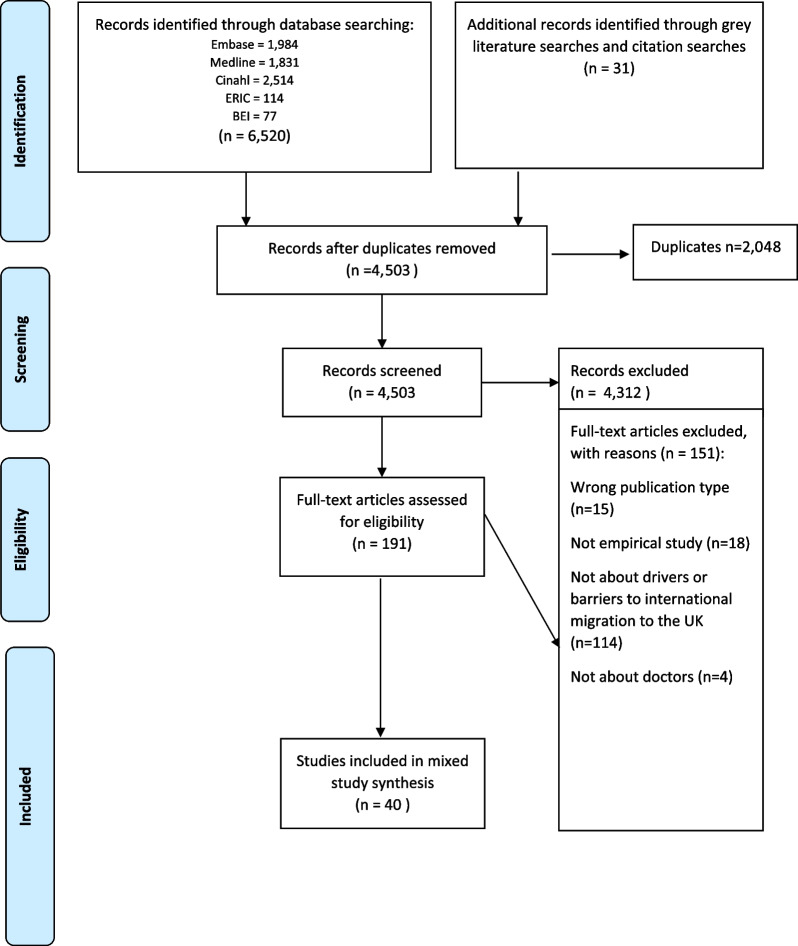
A scoping review was conducted. We searched EMBASE, MEDLINE, CINAHL, ERIC and BEI in January 2020 (updated October 2021). Grey literature and citation searching were also carried out. Empirical studies reporting on the drivers and barriers to the international migration of doctors to and from the UK published in the English language from 2009 to present were included. The drivers and barriers were coded in NVivo 12 building on an existing framework.
Results
40 studies were included. 62% were quantitative, 18% were qualitative, 15% were mixed-methods and 5% were literature reviews. Migration into and out of the UK is determined by a variety of macro- (global and national factors), meso- (profession led factors) and micro-level (personal factors). Interestingly, many of the key drivers of migration to the UK were also factors driving migration from the UK, including: poor working conditions, employment opportunities, better training and development opportunities, better quality of life, desire for a life change and financial reasons. The barriers included stricter immigration policies, the registration process and short-term job contracts.
Conclusions
Our research contributes to the literature by providing a comprehensive up-to-date review of the drivers and barriers of migration to and from the UK. The decision for a doctor to migrate is multi-layered and is a complex balance between push/pull at macro-/meso-/micro-levels. To sustain the UK’s supply of overseas doctors, it is vital that migration policies take account of the drivers of migration particularly working conditions and active recruitment while addressing any potential barriers. Immigration policies to address the impact of Brexit and the COVID-19 pandemic on the migration of doctors to and from the UK will be particularly important in the immediate future.
Trial registration PROSPERO CRD42020165748.
Keywords: Workforce planning, Workforce recruitment, Migration, Doctors
Background
The global geographic mal-distribution of doctors has been an ongoing problem for decades [1] meaning access to health services everywhere in the world is disparate [2]. This mal-distribution of doctors is a particular challenge for the UK [3, 4]. According to the World Health Organisation, the UK has 2.8 doctors per 1000 population. This figure is well below the European Union (EU) average of 3.4/1000 with only four countries, Ireland, Slovenia, Romania, and Poland, having lower numbers of doctors per capita. Workforce challenges in the NHS in England are now a greater threat to the delivery of health services than funding challenges [5]. The UK’s attempts to address this issue have been comprised of both long-term and short-term strategies. These measures have included an expansion of undergraduate medical school places by 25%, improving working conditions for junior doctors [6, 7] and even a relaxation of immigration caps in 2018 to facilitate/enable greater international recruitment from outside the EU [8]. However despite these measures the BMA reported 10,582 vacancies in secondary care medical staff positions across the UK in 2022 [9] and the Royal College of Physicians census showed that only 52% of consultant vacances were filled in 2022 [10]. These figures illustrate the dire need for qualified medical specialists in the UK medical workforce.
Similar to New Zealand, Ireland, the USA and Canada, the United Kingdom (UK) is heavily dependent on internationally trained doctors to staff its healthcare system [11, 12]. Doctors with overseas qualifications are a core part of the UK medical workforce and 34.5% of licensed doctors in the UK received their primary medical qualification (PMQ) abroad [13]. At the same time, an average of 5% of doctors left the UK medical workforce each year from 2013 to 2019; data captured on their reasons for leaving demonstrated that approximately 2.1% are going overseas [12, 14]. The most popular places UK-trained doctors migrate to are other high-income English-speaking countries especially Australia and New Zealand [12].
There have been numerous theories proposed to understand migration over the years [15]. One of the most dominant theories has been the push–pull model which we will use in this paper as a framework to understand the migration of doctors to and from the UK. Push–pull models focus on disparities in conditions to explain migration patterns. Push–pull models in some of the early literature highlighted how migrants were pushed by low incomes in their countries and pulled by better opportunities in more prosperous areas [16, 17].
Central to the push–pull model of migration is the concept of ‘drivers’. Van Hear et al. [18] outlines how structural forces lead to both the inception of migration and the perpetuation of movement and these forces can be understood as the drivers of migration [19]. Similar to Van Hear et al. [18] we use the term driver to mean the variety of factors that may make up the external structural elements shaping the decision to migrate. Thus, drivers influence the broader context within which peoples hopes and wishes to migrate are formed and in which people ultimately make their decisions to migrate. Drivers may operate at different scales, levels of social structure, in different locations, at places of origin, transit and destination and over different timeframes [18].
There has been one systematic review conducted on the migration of doctors into the UK to date. This study was conducted by Davda in 2018 [20] and examined the migration motives of international dental graduates, compared with nurses and doctors in the United Kingdom. Based on the 31 studies included in the synthesis, the review identified common drivers including active recruitment, the desire to gain postgraduate training and financial gain; however, the extent to which each of these drivers influence healthcare professionals migration is different. This review only focused on qualitative studies, did not provide a detailed description of the migration drivers for the three different healthcare professionals included and is now out of date (searches completed in January 2017). On this basis we felt that an updated scoping review of the literature incorporating a broader range of study types focusing specifically on doctors was justified. In addition, we also felt it was important to identify the barriers to the migration of doctors to the UK also, as Davda focused on factors affecting inward migration to the UK only.
Thus the aim of this study was to identify the drivers and barriers of international migration of doctors to and from the UK. By summarising the most recent knowledge on this topic, the research will seek to inform policies on international recruitment globally, retention of the workforce and identify areas, where further research is needed for future workforce planning.
Methods
Type of review
Distinguishing between a scoping review and a systematic review of the literature can be difficult, as both share many essential characteristics namely, collecting, evaluating and presenting the available research evidence [21]. Originally, we planned to conduct a systematic review and developed and registered a protocol with PROSPERO (CRD42020165748). However, Munn et al. [21] argue that if a review is more interested in the identification of certain characteristics/concepts in papers or studies and in the mapping, reporting or discussion of these characteristics/concepts then a scoping review approach is the better choice. On reflection, as the aim of our review was to identify the key characteristics of the drivers and barriers relating to the migration of doctors, we have classified this review as a scoping review rather than a systematic review in this paper. The primary consequence of this change is that in line with scoping review methods [21], we did not undertake quality assessment of the included papers. This review was informed by Arksey and O’Malley’s methodological framework for scoping reviews [22].
Review protocol
A review protocol was developed by the research team and was registered with PROPSERO (a prospective register of systematic reviews) to help avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol [23]. The PROSPERO reference number is CRD42020165748.
Search strategy
The search strategy was designed, piloted and carried out by an experienced information specialist (LB). The search strategy aimed for comprehensiveness through the extent and range of searching. We searched both medical and other health professions databases (EMBASE, MEDLINE, CINAHL) as well as educational databases (e.g. ERIC, BEI). The searches were carried out on the 23rd of January 2020 and were subsequently updated on the 13th of October 2021. We searched for relevant items from 2009 to 2021 in order to build a picture of the current migration drivers and barriers. The databases were searched with free text keywords and controlled vocabulary where appropriate using terms such as ‘doctors’ OR ‘physician’ AND ‘migration’ OR ‘emigration’ or ‘brain drain’ OR ‘working overseas’ OR ‘come to the UK’ OR ‘overseas trained’ OR ‘internationally trained’. See Appendix A for full search histories.
Grey literature searching was also carried out. The grey literature databases HMIC and British Library EThOS were searched on the 13th of May 2020. The websites of key organisations were searched for relevant publications on the 30th of May 2020. Key organisations that conduct research on migration were included i.e. the WHO, the ONS, Euro Stat and the OECD. We also searched the websites of the regulators of the countries UK doctors typically migrate to including the Medical Council of Ireland (MCI), GMC, Australian Medical Council, New Zealand Medical Council, Medical Council of Canada and the American Medical Association.
We searched the bibliographies of included papers. The abstracts for any relevant papers were sought and then the inclusion criteria were applied.
Study selection
In order to select studies relevant to our research questions we applied the following inclusion criteria:
Topic of interest—the international migration of doctors.
Aspect of topic—drivers and barriers of migration to and from the UK
Countries of interest—the UK. Any study that reported the drivers and barriers of migration to and from the UK
Type of participants—all studies about doctors.
Study design—all articles that reported empirical research. Literature reviews were also included if they were systematic reviews of the literature or reported systematic search methods.
Language—studies published in English language.
Date—2009 to present. This was a sufficient timeframe to access recent relevant literature.
Outcome measures—all outcome measures.
The potential relevance of all titles and abstracts was assessed using Rayyan QCRI (systematic review software) by three reviewers independently (NL, NB and LB). All articles were double screened and any discrepancies were discussed until agreement was reached.
Data extraction
The papers of all eligible studies were obtained and read in full. A standardised data extraction review form was piloted and utilised. The extraction was carried out in Microsoft Excel by two researchers (NL and NB). A random sample of 10% of all articles were data extracted independently by both researchers and then compared for consistency.
As scoping reviews do not aim to produce a critically appraised and synthesised result/answer to a particular question, and rather aim to provide an overview or map of the evidence, an assessment of methodological limitations or risk of bias of the evidence was not performed [21].
Data synthesis
Data extracted on drivers and barriers was then exported into NVivo 12 (QSR). NVivo is a computerised indexing system for coding and analysing qualitative data. In order to consistently categorise the drivers and barriers we decided to develop a coding framework. As a coding framework had already been developed by Young [24] and successfully used in the Davda [20] systematic review we decided to use the same framework as a starting point for coding our data. Young’s model categorises the factors attracting health professionals to the UK into three broad categories including macro-level (global and national factors), meso-level (profession led factors) and micro-level (personal factors) drivers of migration [24]. Additional codes identified in our data were added to Young’s framework. See Appendix B for the full coding framework. We also developed another arm to the coding framework to capture the barriers. A 10% sample of the articles was coded by two reviewers (NL and NB) to compare for consistency. One reviewer then coded the remaining papers (NL).
In the results section we present the top three macro-, meso- and micro-level drivers and barriers. A driver or barrier was identified as being in the top three based on the number of articles that had identified the driver or barrier. If a driver or barrier was identified more than once in a paper we only counted it once.
The included papers were classified according to the main country or region that the data collection related to e.g. the UK, Ireland, Africa/Asia. However, this did not mean that the paper was solely about this country/or region. For example sometimes a paper may have been classified as being about Europe but the paper may have contained a driver or barrier relating specifically to the UK.
Results
Literature identified
The search identified 4512 potentially relevant articles and, after the inclusion criteria were applied, 40 articles were included in the review (Fig. 1). The characteristics of the 40 included studies are listed in Appendix C.
Fig. 1.
PRISMA Flow Diagram
Characteristics of included studies
62% of studies were quantitative, 18% were qualitative, 15% were mixed methods and 5% were literature reviews. The main focus of 60% of the studies was migration to and from the UK, 15% were about European countries, 10% were about African or Asian countries, 10% were about Ireland and 5% were about Australia/New Zealand.
What are the drivers of the migration of doctors to and from the UK?
The drivers we identified are summarised in Table 1. We found that many of the reasons associated with attracting doctors to the UK, also constituted push factors for UK doctors to decide to leave the UK and practise abroad.
Table 1.
Drivers and barriers to the migration of doctors to and from the UK
| Macro-level drivers | |
|---|---|
| DRIVERS TO THE UK | DRIVERS FROM THE UK |
| 1.5* Employment opportunities [20, 25–30] | 1.16* Poor working conditions [31–38] |
| 1.1 Active recruitment [20, 29, 39–43] | 1.6 Attractive working conditions elsewhere [32, 34–38, 44, 46] |
| 1.16 Poor working conditions [20, 37, 39, 42, 46, 47] | 1.5 Employment opportunities [32, 34, 37, 44] |
| Meso-level drivers | |
| 2.1 Better training and development opportunities [20, 26, 27, 29, 39, 42, 46, 48–52] | 2.14 Pushed/desire to leave the NHS [31, 33, 34, 36, 38, 44] |
| 2.10 Desire to experience working in a different environment [20, 39, 42, 46, 48, 50] | 2.1 Better training and development opportunities [32, 36, 38, 53] |
| 2.19 Opportunities to gain clinical experience through short-term employment [20, 39, 42, 46, 48, 50] | 2.17 Undervalued professionally [32, 35, 54] |
| Micro-level drivers | |
| 3.17 Financial gain for self (and/or family) [20, 26, 27, 37, 39, 42, 47, 48, 51, 55–57] | 3.1 Better quality of life [32–36, 38, 44] |
| 3.2: Desire for life change [20, 37, 39, 42, 46, 50] | 3.4 Family reasons [33–35, 37, 46] |
| 3.1: Better quality of life [39, 42, 46, 48, 51] | 3.2 Desire for a life change [32–34, 36–38, 46] |
*The numbers correspond to the codes in the coding framework in Appendix C
What are the barriers to doctors coming to work in the UK and to leave the UK?
The main barriers impeding doctor migration to and from the UK are presented in Table 2.
Table 2.
Barriers to the migration of doctors to and from the UK
| Macro-level barriers | |
|---|---|
| Coding descriptor | References |
| 4.21*Stricter immigration policies | [35, 40, 42, 58, 59] |
| 4.26 Process of gaining registration | [27, 48, 60, 61] |
| 4.1 Healthcare system difficult to enter or differences in healthcare system | [27, 42, 48] |
| Meso-level Barriers | |
| 5.14 Short-term job contracts | [35, 62] |
| 5.3 Limited training opportunities | [32, 42] |
| 5.16 Negative experience of induction scheme | [27] |
| Micro-level barriers | |
| 6.8 Concerns about a new working environment | [46, 48] |
| 6.19 Lack of support | [48, 62] |
| 6.22 Language difficulties | [27, 46] |
*The numbers correspond to the codes in the coding framework in Appendix C
Discussion
Statement of principal findings and comparison with existing literature
This comprehensive review of the literature set out to identify the drivers and barriers of international migration of doctors to and from the UK. By summarising the most recent knowledge on this topic, the research will inform policies on international recruitment, retention of the workforce and identify future workforce planning research gaps. We identified a variety of push and pull factors at the macro- (global and national), meso- (professional) and micro- (personal) levels. Interestingly, many of the key drivers of migration to the UK were also factors driving migration from the UK to other countries and are thus relevant for all high-income countries. These included: poor working conditions, employment opportunities, better training and development opportunities, better quality of life, desire for a life change and personal financial gain. The barriers to the migration of doctors to and from the UK included stricter immigration policies, the process of gaining registration, short-term job contracts, limited training opportunities, concerns about a new working environment and lack of support.
The findings of the review highlight how the decision for a doctor to migrate is multi-layered and is a complex balance between push and pull factors at macro-/meso-/micro-levels. The decision to migrate is also relative to a doctors’ own values and experiences, reflecting individual priorities. Furthermore, as Franco et al. point out “not all workers will have the same mix of motives and goals, and the relative importance of particular values and work goals will change over time and situations” [63: 1258]. While the push–pull model of migration has been criticised for being simplistic [64], Van Hear highlights the strengths of the simple notion of push–pull, “with its intuitive and empirically grounded idea that structural forces shape migration processes” [18: 928]. The challenge for researchers is to establish when and why some drivers are more important than others, which combinations are more potent than others, and which are more susceptible to change through external intervention. This complexity poses a significant challenge to policy-makers in terms of planning and ensuring a supply of doctors for the medical workforce. In order to sustain the UK’s supply of overseas doctors, it is vital that UK migration policy relating to doctor migration take account of the drivers of migration while addressing any potential barriers.
Policy-makers are most likely to have an impact on the macro- and meso-level factors we have identified in the review as the micro-level factors i.e. financial gain, better quality of life and family reasons, relate to an individual’s personal values and circumstances. The most important macro-level driver of migration to the UK was employment opportunities. Due to the UKs current shortage of doctors it is likely that there will continue to be employment opportunities particularly in some specialities e.g. general practice, psychiatry and emergency medicine. Thus, policymakers should focus on ensuring the employment opportunities are advertised globally as well as focusing on ethical active recruitment for jobs (another of the macro-level drivers).
The main macro-level factor policy-makers can have a big impact on and should prioritise is working conditions in the NHS. Policy-makers are well aware of the need to improve working conditions in the NHS and this has been addressed in the 5 year plan [65, 66] and other initiatives focusing in particular on NHS staff health and well-being [67, 68]. Humphries also found in her study of the migration of doctors from Ireland to Australia that working conditions are a particularly important factor in migration decisions and whatever health system gets this aspect right will be successful in attracting and retaining doctors [49, 69]. The other macro-level factor policy-makers can target is training and development opportunities and putting policies in place to ensure the high standards of training the UK is renowned for are available for overseas trained doctors who are not yet qualified to join the specialist or GP registers.
The opposite side of the push–pull model driving migration of overseas doctors into the UK, are barriers to migration. These factors may hinder, or make difficult the ability to migrate, or they may be factors that dissuade doctors from migration, for example, positive improvements to salary or working conditions in one’s home country. The literature contained few references to the barriers to migration, prioritising instead the push/pull factors driving doctors to either immigrate into, or emigrate out of, the UK. The likely reason for this is that methodologically it is much more difficult to ascertain changed intentions to migrate, and what may have changed or obstructed a nascent decision to migrate [18, 64].
The review highlighted that stricter immigration policies and the process of registration were significant barriers. These barriers are particularly relevant for EU doctors in the BREXIT era. The fact that EU doctors qualifications are now not automatically recognised in the UK means the number of doctors migrating to the UK from the EU could decrease [70, 71]. Recent projections are that Brexit has resulted in 4,285 fewer European doctors coming to the UK [70]. Thus, policy makers will need to consider how they can make up this potential shortfall in the supply of doctors from the EU.
The findings of our review corroborate the findings of the Davda [20] review which identified active recruitment, postgraduate training and financial gain as strong common macro, meso and micro drivers that perpetuate migration into the UK. It is not surprising that the findings were similar, as the Davda review was an included paper in our review and there was also some overlap between included studies in the two reviews. Davda included 31 studies in their review, five of which were also in ours. However, despite this overlap there was still quite a number of different studies involved in our review (n = 34) with some focusing on the recent impacts of BREXIT and the COVID-19 pandemic on migration patterns. The fact that the findings were similar adds more weight to the drivers identified in both reviews. It also implies that these drivers have not changed significantly over time.
Studies on Ireland [72, 73] and other higher income countries in Europe [39] also reported poor working conditions, employment opportunities, better training and development opportunities, financial gain, better quality of life and family reasons as being important drivers of emigration. This begs the question: how can high income countries maintain a competitive advantage in this area? The COVID-19 pandemic has served as a reminder of how important the medical workforce is. Post COVID-19 health systems everywhere will be looking to strengthen their medical workforce and as this will influence expectations, future plans and migration decisions [52] it will also increase international competition.
Strengths and limitations
This is a comprehensive review of the literature. The search strategy was designed by an experienced information specialist and a variety of medical and educational databases were searched. All relevant papers identified were double-screened and data extraction consistency checks were carried out for 10% of papers. The review team were multidisciplinary including social scientists and clinicians. We included studies that were not primarily about the UK that contained drivers and barriers and we also included all study designs so a broader literature was drawn upon.
As with all research studies, there are also some limitations. A limitation of the study is that we only identified and classified the drivers and barriers from the literature and so if a driver was identified many times in a study we only reported it once. We did not carry out a quality assessment so cannot comment on the strength of the evidence underpinning each driver and barrier identified. As with all literature reviews the results are dependent on the quality of the existing literature and due to very limited literature on the barriers we were not able to address this question sufficiently. Resource constraints meant we only looked at literature since 2009 and published in the English language.
Conclusion
Our research contributes to the literature by providing an up-to-date review of the drivers and barriers of migration to and from the UK. The review found that the decision for a doctor to migrate is multi-layered and is a complex balance between push/pull at macro-/meso-/micro-levels. This complexity poses a significant challenge to policymakers in planning and ensuring a supply of doctors for high income countries. To sustain the UK’s supply of overseas doctors, it is vital that migration policy tools are developed that recognise and support the drivers of migration particularly working conditions and active recruitment while addressing any potential barriers particularly immigration policies and the process for gaining registration. Immigration policies to address the impact of Brexit and the COVID-19 pandemic on the migration of doctors to and from the UK will be particularly important in the immediate future.
Appendix A
Systematic review search histories
Search Histories 23.01.2020.
| Database | Results |
|---|---|
| Ovid Embase | 1631 |
| Ovid MEDLINE | 1533 |
| CINAHL via EBSCOhost | 2085 |
| ERIC via EBSCOhost | 109 |
| BEI via EBSCOhost | 62 |
| Total before dedup | 5423 |
| Embase < 1974 to 2020 January 23 > | ||
|---|---|---|
| Search history sorted by search number ascending | ||
| # | Searches | Results |
| 1 | exp physician/ | 720,194 |
| 2 | ("doctor*" or physician or "general practitioner*" or "GP*" or "G.P*").tw | 667,950 |
| 3 | "physician*".tw | 530,375 |
| 4 | 1 or 2 or 3 | 1,353,626 |
| 5 | foreign medical graduate/ or foreign physician/ | 277 |
| 6 | ((emigrat* or migrat* or immigrat*) adj3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")).tw | 775 |
| 7 | ((work* or practi?e) adj3 (overseas or abroad or "another country")).tw | 940 |
| 8 | "brain drain".tw | 620 |
| 9 | ((work or practise) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw | 1569 |
| 10 | ((leave or come to) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw | 359 |
| 11 | ((trained or qualified or graduated) adj3 (overseas or abroad or international* or "another country")).tw | 511 |
| 12 | international medical graduate*.tw | 943 |
| 13 | ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") adj2 (mobility or movement)).tw | 332 |
| 14 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 | 5966 |
| 15 | 4 and 14 | 2662 |
| 16 | limit 15 to year = "2009—2020" | 1705 |
| 17 | limit 16 to English language | 1631 |
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Daily and Versions(R) < 1946 to January 23, 2020 > | ||
|---|---|---|
| Search history sorted by search number ascending | ||
| # | Searches | Results |
| 1 | exp Physicians/ | 136,160 |
| 2 | ("doctor*" or "general practitioner*" or "GP*" or "G.P*").tw | 323,888 |
| 3 | "physician*".tw | 377,649 |
| 4 | 1 or 2 or 3 | 734,837 |
| 5 | foreign medical graduates/ | 3443 |
| 6 | ((emigrat* or migrat* or immigrat*) adj3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")).tw | 684 |
| 7 | ((work* or practi?e) adj3 (overseas or abroad or "another country")).tw | 826 |
| 8 | "brain drain".tw | 612 |
| 9 | ((work or practise) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw | 1094 |
| 10 | ((leave or come to) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw | 277 |
| 11 | ((trained or qualified or graduated) adj3 (overseas or abroad or international* or "another country")).tw | 391 |
| 12 | international medical graduate*.tw | 809 |
| 13 | ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") adj2 (mobility or movement)).tw | 289 |
| 14 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 | 7462 |
| 15 | 4 and 14 | 4973 |
| 16 | limit 15 to yr = "2009—2020" | 1662 |
| 17 | limit 16 to english language | 1533 |
| # | Query—Database—CINAHL Plus with Full Text | Results |
|---|---|---|
| 1 | (MH "Physicians + ") | 103,131 |
| 2 | TI ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") OR AB ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") | 85,840 |
| 3 | TI physician* OR AB physician* | 128,694 |
| 4 | S1 OR S2 OR S3 | 269,064 |
| 5 | (MH "Foreign Medical Graduates") | 795 |
| 6 | TI ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")) OR AB ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") | 204 |
| 7 | TI ( (work* or practi?e) N3 (overseas or abroad or "another country")) OR AB ( (work* or practi?e) N3 (overseas or abroad or "another country")) | 564 |
| 8 | TI ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) OR AB ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) | 10,406 |
| 9 | TI ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) OR AB ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) | 469 |
| 10 | TI ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) OR AB ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) | 296 |
| 11 | TI ("international medical graduate*" or "brain drain") OR AB ("international medical graduate*" or "brain drain") | 598 |
| 12 | TI ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) OR AB ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) | 118 |
| 13 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 | 12,831 |
| 14 | S4 AND S13 | 3119 |
| 15 | S4 AND S13 | 3119 |
| 16 | S4 AND S13 | 2085 |
| # | Query—Database—British Education Index; ERIC | Results |
|---|---|---|
| 1 | (MH "Physicians + ") | 15 |
| 2 | TI ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") OR AB ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") | 22,431 |
| 3 | TI physician* OR AB physician* | 6,182 |
| 4 | S1 OR S2 OR S3 | 28,133 |
| 5 | (MH "Foreign Medical Graduates") | 1218 |
| 6 | TI ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")) OR AB ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") | 35 |
| 7 | TI ( (work* or practi?e) N3 (overseas or abroad or "another country")) OR AB ( (work* or practi?e) N3 (overseas or abroad or "another country")) | 449 |
| 8 | TI ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) OR AB ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) | 6114 |
| 9 | TI ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) OR AB ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) | 507 |
| 10 | TI ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) OR AB ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) | 131 |
| 11 | TI ("international medical graduate*" or "brain drain") OR AB ("international medical graduate*" or "brain drain") | 407 |
| 12 | TI ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) OR AB ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) | 37 |
| 13 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 | 7548 |
| 14 | S4 AND S13 | 310 |
| 15 | S4 AND S13 | 310 |
| 16 | S4 AND S13 174 = 109 in ERIC and 65 in BEI | 174 |
| # | Database | Search term | Results |
|---|---|---|---|
| 1 | HMIC | exp "MEDICAL STAFF"/ | 22,072 |
| 2 | HMIC | "doctor*" OR physician OR "general practitioner*" OR "GP*" OR "G.P*" | 35,935 |
| 3 | HMIC | (1 OR 2) | 42,114 |
| 4 | HMIC | exp "LABOUR MOBILITY"/ | 61 |
| 5 | HMIC | "LABOUR MIGRATION"/ | 87 |
| 6 | HMIC | (emigrat* OR migrat* OR immigrat*) ADJ3 (doctor* OR physician* OR "general practitioner*" OR "GP*" OR "G.P*") | 50 |
| 7 | HMIC | ((work* OR practi?e) ADJ3 (overseas OR abroad OR "another country")).ti,ab | 166 |
| 8 | HMIC | ("brain drain").ti,ab | 34 |
| 9 | HMIC | (work OR practise) ADJ3 (UK OR Britain OR "U.K." OR EU OR "European Union" OR "E.U." OR Ireland OR Canada OR Australia OR Zealand OR USA OR "U.S.A" OR America) | 271 |
| 10 | HMIC | (leave OR come to) ADJ3 (UK OR Britain OR "U.K." OR EU OR "European Union" OR "E.U." OR Ireland OR Canada OR Australia OR Zealand OR USA OR "U.S.A" OR America) | 80 |
| 11 | HMIC | ((trained OR qualified OR graduated) ADJ3 (overseas OR abroad OR international* OR "another country")).ti,ab | 80 |
| 12 | HMIC | (doctor* OR physician* OR "general practitioner*" OR "GP*" OR "G.P*") ADJ2 (mobility OR movement) | 28 |
| 13 | HMIC | (4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12) | 766 |
| 14 | HMIC | (3 AND 13) | 247 |
| 15 | HMIC | 14 [DT 2009–2020] | 82 (27 after de-dup) |
|
BL EThOS: Doctor (title) AND migration (title) AND UK (abstract) = 1 result |
| The migration of medical doctors from Poland to the United Kingdom following the expansion of the European Union in May 2004 https://discovery.ucl.ac.uk/id/eprint/1302279/ (not available) |
|
Doctors (title) AND migration (title) Doctors (title) AND “brain drain” (abstract) Doctors (title) AND immigration (title) Doctors (title) AND emmigration (title) Doctors (title) AND migrate (title) Doctors (title) AND abroad (title) Doctors (title) AND Britain (title) Doctors (title) AND United Kingdom (title) General Practitioners (title) AND United Kingdom (title) General Practitioners (title) AND Britain (title) Doctors (title) AND abroad (title) General Practitioners (title) AND migration (title) General Practitioners (title) AND migrate (title) General Practitioners (title) AND immigration (title) General Practitioners (title) AND emmigration (title) General Practitioners (title) AND mobility (title) = 0 results |
Search Histories 13.10.21.
| Database | Results |
|---|---|
| Ovid Embase | 353 |
| Ovid MEDLINE | 298 |
| CINAHL via EBSCOhost | 429 |
| ERIC via EBSCOhost | 5 |
| BEI via EBSCOhost | 15 |
| Total before dedup | 1088 |
| After dedup | 782 |
Embase < 1974 to 2021 October 12 >
1exp physician/830272.
2("doctor*" or physician or "general practitioner*" or "GP*" or "G.P*").tw.743173.
3"physician*".tw.589350.
41 or 2 or 31,530,923.
5foreign medical graduate/ or foreign physician/390.
6((emigrat* or migrat* or immigrat*) adj3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")).tw.846.
7((work* or practi?e) adj3 (overseas or abroad or "another country")).tw.1034.
8"brain drain".tw.674.
9((work or practise) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw.1763.
10((leave or come to) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw.409.
11((trained or qualified or graduated) adj3 (overseas or abroad or international* or "another country")).tw.593.
12international medical graduate*.tw.1097.
13((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") adj2 (mobility or movement)).tw.396.
145 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 136,767.
154 and 143,045.
16limit 15 to yr = "2020—2021"363.
17limit 16 to english language353.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) < 1946 to October 12, 2021 >
1exp Physicians/156743.
2("doctor*" or "general practitioner*" or "GP*" or "G.P*").tw.360787.
3"physician*".tw.415660.
41 or 2 or 3,817,995.
5foreign medical graduates/3553.
6((emigrat* or migrat* or immigrat*) adj3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")).tw.752.
7((work* or practi?e) adj3 (overseas or abroad or "another country")).tw.893.
8"brain drain".tw.660.
9((work or practise) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw.1243.
10((leave or come to) adj3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)).tw.320.
11((trained or qualified or graduated) adj3 (overseas or abroad or international* or "another country")).tw.454.
12international medical graduate*.tw.942.
13((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") adj2 (mobility or movement)).tw.338.
145 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 138,106.
154 and 145,279.
16limit 15 to yr = "2020—current"303.
17limit 16 to english language298.
CINAHL; ERIC; BEI.
| # | Query | Results |
|---|---|---|
| S1 | (MH "Physicians + ") | 123,630 |
| S2 | TI ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") OR AB ( "doctor*" or "general practitioner*" or "GP*" or "G.P*" or "medical personnel") | 131,231 |
| S3 | TI physician* OR AB physician* | 163,335 |
| S4 | S1 OR S2 OR S3 | 357,698 |
| S5 | (MH "Foreign Medical Graduates") | 905 |
| S6 | TI ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*")) OR AB ( (emigrat* or migrat* or immigrat*) N3 (doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") | 295 |
| S7 | TI ( (work* or practi?e) N3 (overseas or abroad or "another country")) OR AB ( (work* or practi?e) N3 (overseas or abroad or "another country")) | 1,163 |
| S8 | TI ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) OR AB ( (work* or practise) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U." or Ireland or Canada or Australia or Zealand or USA or "U.S.A" or America)) | 22,672 |
| S9 | TI ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U.")) OR AB ( (leave or come) N3 (UK or Britain or "U.K." or EU or "European Union" or "E.U.")) | 313 |
| S10 | TI ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) OR AB ( (trained or qualified or graduated) N3 (overseas or abroad or international* or "another country")) | 496 |
| S11 | TI ("international medical graduate*" or "brain drain") OR AB ("international medical graduate*" or "brain drain") | 1,143 |
| S12 | TI ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) OR AB ((doctor* or physician* or "general practitioner*" or "GP*" or "G.P*") N2 (mobility or movement)) | 201 |
| S13 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 | 26,328 |
| S14 | S4 AND S13 | 4,549 |
| S16 | S4 AND S13 Limiters—Publication Date: 20,200,101–20,211,231 | 449 |
CINAHL: 429; BEI: 15 ERIC: 5
Appendix B
Coding framework for systematic review
| Level of analysis | Themes and descriptions | Codes | Label |
|---|---|---|---|
| 1. Macro-level drivers | Health system factors | 1.1 | Active recruitment |
| 1.2 | Passive recruitment | ||
| 1.3 | Good healthcare infrastructure | ||
| 1.4 | Workforce demand | ||
| 1.5 | Employment opportunities | ||
| 1.6 | Attractive working conditions | ||
| 1.7 | Safety and security of NHS | ||
| 1.8 | Support offered for relocation induction | ||
| 1.9 | Overproduction of nurses and doctors | ||
| 1.10 | Low unemployment | ||
| 1.11 | Unemployment | ||
| 1.12 | Underemployment | ||
| 1.13 | Poor healthcare infrastructure | ||
| 1.14 | Poor job opportunities | ||
| 1.15 | Poor salaries | ||
| 1.16 | Poor working conditions | ||
| 1.17 | Lack of support | ||
| 1.18 | Ease of assessment registration revalidation process | ||
| Economic factors | 1.19 | Macroeconomic factors | |
| 1.20 | Economic and political stability | ||
| 1.21 | Recession/economic instability | ||
| 1.22 | Devaluation of money | ||
| 1.23 | Remittance to home coutnry | ||
| 1.24 | Changes to renumeration | ||
| 1.25 | Corruption in everyday life | ||
| Political factors | 1.26 | Political situation | |
| 1.27 | Policy issues | ||
| 1.28 | Safety for family, self, fleeing violence | ||
| 1.29 | Bilateral agreements | ||
| 1.30 | Immigration policies | ||
| 1.31 | Ease of obtaining right to remain | ||
| 1.32 | Ease of movement to the UK from EU | ||
| 1.33 | Ease of movement within the EU | ||
| 1.34 | Citizenship status | ||
| 1.35 | UK referendum vote to leave EU | ||
| 1.36 | Colonial connections | ||
| 1.37 | Compulsory service in the public sector | ||
| Social factors | 1.38 | Social conditions | |
| 1.39 | Promotes multiculturalism | ||
| 1.40 | History culture of medical migration | ||
| 1.41 | Historical ties | ||
| 1.42 | Xenophobia discrimination | ||
| 1.43 | Gender equity | ||
| 1.44 | Unequal opportunities | ||
| 1.45 | Established networks | ||
| 2. Meso-level drivers | Training opportunities | 2.1 | Better training and development opportunities |
| 2.2 | Desire to learn the state of the art in the profession | ||
| 2.3 | Status of gaining qualifications and training from specific country | ||
| 2.4 | Opportunity to advance knowledge and education of self | ||
| 2.5 | Opportunity to advance knowledge, skills of sector country | ||
| 2.6 | Lack of professional development opportunities | ||
| 2.7 | Shortage of postgraduate training opportunities | ||
| 2.8 | Shortage of posts in a particular specialty profession | ||
| 2.9 | Poor standard of training | ||
| Employment opportunities | 2.10 | Desire to experience working in a different environment | |
| 2.11 | Better working relationships | ||
| 2.12 | Job satisfaction experience | ||
| 2.13 | Poor working relationships | ||
| 2.14 | Pushed desire to leave the NHS | ||
| 2.15 | Poor intellectual stimulation | ||
| 2.16 | Healthcare professionals are valued | ||
| 2.17 | Undervalued professionally | ||
| Career progression opportunities | 2.18 | Career progression | |
| 2.19 | Opportunities to gain clinical experience through short-term employment | ||
| 2.20 | Opportunity for research | ||
| 2.21 | Opportunity for networking | ||
| 2.22 | Lack of promotion | ||
| 2.23 | Limited career opportunities | ||
| 2.24 | Negative research environment | ||
| 2.25 | Healthcare structure, management issues | ||
| 3. Micro-level drivers | Personal fulfilment | 3.1 | Better quality of life |
| 3.2 | Desire for life change | ||
| 3.3 | Adventure | ||
| 3.4 | Family reasons | ||
| 3.5 | Better education for children | ||
| 3.6 | Better climate environment | ||
| 3.7 | Future hopes and goals | ||
| 3.8 | Better morale and well-being | ||
| 3.9 | Personal growth | ||
| 3.10 | To be competitive enhance CV | ||
| 3.11 | To provide better patient care | ||
| 3.12 | Improve languages | ||
| 3.13 | Humanitarian work | ||
| 3.14 | Poor work–life balance quality of life | ||
| 3.15 | Lack of morale | ||
| 3.16 | Burnout stress | ||
| Financial factors | 3.17 | Financial gain for self | |
| 3.18 | Financial gain for family | ||
| 3.19 | Scholarship | ||
| 3.20 | Financial hardship | ||
| Location factors | 3.21 | Proximity Location of destination country | |
| 3.22 | Stepping stone to another destination | ||
| 3.23 | Prior experience in destination country | ||
| 3.24 | Common Language | ||
| 3.25 | Language problems | ||
| Themes and descriptions | Codes | Label | |
| 4. Macro-level barriers | Health system factors | 4.1 | Healthcare system difficult to enter |
| 4.2 | Institutional change | ||
| 4.3 | Improvements to healthcare system in home country | ||
| 4.4 | Increased salary | ||
| 4.5 | Investment in working and living conditions | ||
| 4.6 | Creating job opportunities | ||
| 4.7 | Workforce demand | ||
| 4.8 | Healthcare workers are valued in home country | ||
| 4.9 | Poor salaries | ||
| 4.10 | Poor working conditions | ||
| 4.11 | Limited employment opportunities | ||
| 4.12 | Decrease in workforce demand | ||
| 4.13 | Underemployment skills loss | ||
| 4.14 | Limitations on recruitment | ||
| 4.15 | Limiting the number of students seeking medical education training | ||
| 4.16 | Bureaucratic process | ||
| Economic factors | 4.17 | Economic crisis | |
| 4.18 | Financial loss for country | ||
| 4.19 | Financial support | ||
| Political factors | 4.20 | Political situation | |
| 4.21 | Stricter immigration policies | ||
| 4.22 | Policy changes | ||
| 4.23 | Bilateral agreement | ||
| 4.24 | Lack of citizenship | ||
| 4.25 | Obtaining residence permit | ||
| 4.26 | Process of gaining registration | ||
| 4.27 | Bonded to work in home country | ||
| 4.28 | Long emigration process | ||
| 4.29 | UK decision to leave the EU | ||
| Social factors | 4.30 | Xenophobia discrimination | |
| 4.31 | Cultural factors | ||
| 4.32 | Gender | ||
| 4.33 | Religious factors | ||
| 5. Meso-level barriers | Training factors | 5.1 | More domestic training opportunities |
| 5.2 | Investment in language training | ||
| 5.3 | Limited training opportunities | ||
| 5.4 | Restructure of training process | ||
| 5.5 | Difficult to get a specialist training post | ||
| 5.6 | Expensive examinations | ||
| 5.7 | Qualifications undervalued | ||
| 5.8 | Training deanery | ||
| 5.9 | Cost of training relocation | ||
| Employment factors | 5.10 | Improving career opportunities | |
| 5.11 | Provision of professional development opportunities | ||
| 5.12 | Positive working relationships | ||
| 5.13 | Measures to prevent burnout | ||
| 5.14 | Negative job security/short-term job contract | ||
| 5.15 | Lack of recognition of qualifications or experience | ||
| 5.16 | Negative induction scheme | ||
| 6. Micro-level barriers | Personal factors | 6.1 | Family ties |
| 6.2 | Better quality of life in home country | ||
| 6.3 | Concerns about starting a new life experience | ||
| 6.4 | Loyalty to profession in home country | ||
| 6.5 | Homesickness | ||
| 6.6 | Stress and or isolation | ||
| 6.7 | Long-term settlement plan | ||
| Employment factors | 6.8 | Concerns about a new working environment | |
| 6.9 | Concerns regarding Appraisal revalidation certification | ||
| 6.10 | Good job in home country | ||
| 6.11 | Higher workplace satisfaction | ||
| 6.12 | Lack of work experience | ||
| 6.13 | Negative experiences | ||
| 6.14 | Lack of references from destination country | ||
| Financial factors | 6.15 | Financial loss for self family | |
| 6.16 | Government scholarship | ||
| 6.17 | Potential loss of employment benefits | ||
| Social factors | 6.18 | Social status | |
| 6.19 | Lack of support | ||
| 6.20 | Lack of overseas network | ||
| Location factors | 6.21 | Limited knowledge of destination country | |
| 6.22 | Language difficulties |
Appendix C
Characteristics of included studies
| Author | Year | Aim of study | Methods | Country | DRIVER CODES | BARRIER CODES | |
|---|---|---|---|---|---|---|---|
| 1 | Adebayo [51] | 2021 | To assess the emigration intentions of doctors undergoing residency training in a tertiary healthcare centre in Nigeria and the factors that influence these intentions | Mixed Methods | Africa/Asia | 3.1, 1.6, 3.17, 3.4, 1.13, 2.4, 2.1 | |
| 2 | Bailey [59] | 2012 | To explore the factors influencing the career plans of medical students and recent graduates with regard to four policy-relevant aspects | Qualitative | Africa/Asia | 1.12, 1.16, 1.3, 2.10, 2.12, 2.17, 2.5, 2.7, 3.17, 3.18 | 4.21, 4.22, 6.4, 6.20 |
| 3 | Bezuidenhout [30] | 2009 | To investigate the profile of South African qualified physicians who emigrated from South Africa | Quantitative | Africa/Asia | 1.5, 3.17 | 4.10, 4.13, |
| 4 | Labonté [61] | 2015 | To better understand the drivers of skilled health worker migration, its consequences, and the strategies countries have employed to mitigate negative impacts | Mixed Methods | Africa/Asia | 1.19, 1.21, 1.25, 1.1, 1.13, 1.14, 1.15, 1.16, 1.5, 1.6, 1.28, 2.18, 2.17, 2.6, 3.17, 3.20, 3.1, 3.16, 3.4 | 4.17, 4.12, 4.14, 4.3, 4.5, 4.23, 4.26, 4.31, 6.1, 6.2 |
| 5 | Gureje [29] | 2009 | To understand the brain drain of health professionals | Mixed methods | Australia | 1.1, 1.14, 1.15, 1.5, 1.6, 1.28, 2.24, 2.25, 2.12, 2.13, 2.1, 2.4, 2.9, 3.17, 3.1, 3.5 | |
| 6 | McDermott [44] | 2015 | To explore the increasing numbers of emergency medicine (EM) registrars that obtained their primary medical degree from UK or Irish universities, who work in emergency departments (ED) throughout Australia and New Zealand | Quantitative | Australia | 1.21, 1.16, 1.6, 2.25, 2.14, 3.1 | 4.21 |
| 7 | Mara [57] | 2020 | To analyse the recent trends in the mobility of health professionals in Europe | Mixed Method | Europe | 3.17 | |
| 8 | Ramos [47] | 2017 | To determine the prevalence of migration intentions among Portuguese junior doctors and to identify the most important drivers of career choice for those who are considering migrating in the near future | Quantitative | Europe | 1.16, 1.5, 2.20, 3.17 | |
| 9 | Schumann [60] | 2019 | To explore the driving forces in a group of Egyptian physicians and final-years medical students preparing to migrate to Germany | Qualitative | Europe | 1.13, 1.18, 1.3, 1.5, 1.40, 1.45, 2.25, 2.1, 2.7, | |
| 10 | Ognyanovaa [40] | 2012 | To shed light on the changes in the scale of movement, trends and directions of flows of health professionals pre and post 2004 and 2007 EU enlargements | Quantitative | Europe | 1.1, 1.6, 1.33, 2.1, 3.17, 3.21 | 4.4, 4.5, 4.21, |
| 11 | Wismar [39] | 2011 | To enhance knowledge on the nature and extent of health professional mobility in the EU, assess its impact on country health systems and outline some major policy strategies to address mobility | Quantitative | Europe | 1.20, 1.21, 1.23, 1.25, 1.1, 1.11, 1.12, 1.14, 1.15, 1.16, 1.2, 1.3, 1.4, 1.6, 1.8, 1.9, 1.26, 1.27, 1.31, 1.32, 1.33, 1.38, 1.44, 2.18, 2.19, 2.20, 2.21, 2.24, 2.25, 2.10, 2.12, 2.16, 2.17, 2.1, 2.2, 2.3, 2.4, 2.6, 2.7, 2.8, 2.9, 3.17, 3.21, 3.22, 3.23, 3.24, 3.25, 3.1, 3.11, 3.12, 3.15, 3.2, 3.3, 3.4, 3.5 | 4.11, 4.21, 4.26, 6.21, 6.22, 6.1, 5.14, 5.15, 5.3 |
| 12 | Buchan [42] | 2014 | To assess the scale of mobility of health professionals from the new to the old EU Member States before and after the 2004 and 2007 EU enlargements | Quantitative | Europe | 1.20, 1.21, 1.23, 1.25, 1.1, 1.11, 1.12, 1.13, 1.15, 1.16, 1.3, 1.6, 1.8, 1.26, 1.32, 1.38, 1.45, 2.18, 2.19, 2.20, 2.21, 2.25, 2.10, 2.13, 2.17, 2.1, 2.2, 2.3, 2.6, 2.7, 2.8, 3.17, 3.22, 3.24, 3.1, 3.11, 3.12, 3.14, 3.2, 3.3, 3.4, 3.5 | 4.1, 4.11, 4.21, 4.31, 6.22, 6.1, 6.3, 6.4, 6.18, 5.15, 5.3 |
| 13 | Bidwell [49] | 2012 | To explore the extent of increased dependence on international medical migration which has both national and international policy implications (2000–2010) | Quantitative | Ireland | 1.2, 2.18 | 4.9, 4.26, 5.14 |
| 14 | Humphries [74] | 2013 | To provide insight into the experiences of non-EU migrant doctors in the Irish health workforce | Qualitative | Ireland | 1.12, 1.16, 2.1, 2.6 | |
| 15 | Humphries [52] | 2021 | To ascertain whether (and how) the COVID‑19 pandemic might disrupt or reinforce existing patterns of doctor emigration | Qualitative | Ireland | 2.1, 1.46 | |
| 16 | Wójcicka [28] | 2009 | To provide a national profile of migration of health professionals in Ireland | Qualitative | Ireland | 1.20, 1.21, 1.10, 1.11, 1.14, 1.16, 1.18, 1.3, 1.4, 1.5, 1.32, 1.40, 1.45, 2.1, 2.3, 2.7, 3.17, 3.21, 3.1 | 4.11, 4.9 |
| 17 | Begum [58] | 2019 | To examine how many senior scientists and clinicians were from other countries, particularly from Europe, in two time periods | Quantitative | UK | 1.8, 1.30 | 4.20, 4.21, |
| 18 | Blacklock [43] | 2012 | To investigate the effect of UK policy on medical migration | Quantitative | UK | 1.1, 1.30, | 4.23 |
| 19 | Bornat [25] | 2011 | To examine the push/pull factors and oral histories of overseas trained doctors from South Asia who have entered the UK workforce in geriatric medicine | Qualitative | UK | 1.5, 2.3 | |
| 20 | Crossland [56] | 2021 | To report the numbers of consultant congenital cardiac surgeons and cardiologists who have joined and left UK practice over the last 10 years and explore the reasons for leaving | Quantitative | UK | 3.9, 3.17, 2.14, 3.14, 2.1, 2.20, 2.8 | |
| 21 | Davda [20] | 2018 | To examine the migration motives, the barriers to and facilitators of integration of international dental graduates, compared with nurses and doctors in the United Kingdom | Literature review | UK | 1.21, 1.22, 1.24, 1.25, 1.1, 1.11, 1.12, 1.13, 1.15, 1.16, 1.5, 1.7, 1.29, 1.30, 1.45, 2.19, 2.22, 2.10, 2.1, 2.7, 3.1, 3.18, 3.1, 3.2, 3.3, 3.5 | |
| 22 | Gauld [36] | 2015 | To examine why these doctors go to New Zealand and do not stay for long | Quantitative | UK | 1.5, 1.6, 2.14, 2.1, 3.17, 3.1 | 6.1 |
| 23 | George [55] | 2017 | To examine the salaries of selected HRH in India and four popular destination countries (United States of America, United Kingdom, Canada and the United Arab Emirates) while accounting for the in-country cost of living | Quantitative | UK | 3.17 | |
| 24 | Herfs [26] | 2014 | To present data relating to the changes in IMG migration in the UK since the extension of the European Union in May 2004. In addition, data are presented on IMG migration in the Netherlands. These migration flows show that migration patterns differ strongly within these two EU-countries | Quantitative | UK | 1.18, 1.5, 1.40, 2.1, 2.4, 3.17, 3.24 | |
| 25 | Hosni [50] | 2017 | To find out if doctors leaving the UK at the end of the 2 year "International Doctors Training Programme of Obstetrics and Gynaecology" feel that they achieved what they expected to achieve, what went well and what did not go well | Quantitative | UK | 2.19, 2.10, 2.1, 3.2 | |
| 26 | Iacobucci [14] | 2017 | To explore if EU doctors are considering leaving UK | Quantitative | UK | 1.30, 1.35, 1.42, | |
| 27 | Lambert [34] | 2017 | To report the changes to UK medicine which doctors who have emigrated tell us would increase their likelihood of returning to a career in UK medicine | Quantitative | UK | 1.14, 1.15, 1.16, 1.18, 2.20, 2.25, 2.17, 3.17, 3.1, 3.15, 3.4, 3.6 | 4.21, 5.14 |
| 28 | Legido-Quigley [27] | 2015 | To describe the experiences of doctors who decide to move to the UK from other EU member states, exploring their motivations for moving and their experiences of registering and working in the UK | Qualitative | UK | 1.13, 1.5, 2.1, 2.4, 3.17, 3.24, 3.12, 3.9 | 4.1, 4.12, 4.26, 6.22, 5.16 |
| 29 | Milner [71] | 2021 | To assess how Brexit relates to doctors’ migration intentions in relation to their feelings that Brexit has impacted their professional life, national identity, and demographic factors | Quantitative | UK | 1.35 | |
| 30 | Milner [75] | 2021 | To provide a detailed examination of European doctors’ feelings towards Brexit, their intentions to leave the UK, and factors that may contribute to their potential decisions to migrate | Quantitative | UK | 1.35 | |
| 31 | Quantin [37] | 2012 | To analyse the migration of doctors between the UK and France, in an attempt to identify the reasons for these migrations | Quantitative | UK | 1.16, 1.6, 1.7, 2.18, 2.1, 3.17, 3.2, 3.4, 3.6 | |
| 32 | Sharma [33] | 2012 | To investigate factors which influenced UK-trained doctors to emigrate to New Zealand and factors which might encourage them to return | Quantitative | UK | 1.14, 1.5, 2.12, 2.14, 3.23, 3.1, 3.2, 3.4 | 4.3, |
| 33 | Smith [62] | 2012 | To conduct an exploratory study to learn about the experiences of GPs who have undertaken international work | Quantitative | UK | 6.9, 6.15, 6.17, 6.1, 6.19, 5.14, 5.8 | |
| 34 | Smith [32] | 2018 | To explore the reasons that doctors choose to leave UK medicine after their foundation year 2 posts | Quantitative | UK | 1.19, 1.13, 1.16, 1.6, 1.26, 1.30, 1.32, 2.19, 2.11, 2.13, 2.16, 2.17, 2.1, 2.6, 2.9, 3.1, 3.14, | 4.29, |
| 35 | Torjesen [54] | 2017 | To examine the affect of Brexit on EEA doctors intent to continue working in the UK | Quantitative | UK | 1.35, 2.17, 3.15 | |
| 36 | Van der Pol [31] | 2019 | To examine the association between risk attitudes and the migration of UK GPs to Australia | Quantitative | UK | 1.5, 2.14 | |
| 37 | Khan [48] | 2015 | To review and inform the relevant authorities about the barriers faced by IMGs in training and career progression in the UK health service | Literature Review | UK | 1.28, 2.19, 2.20, 2.10, 2.1, 2.4, 3.17, 3.1 | 4.1, 4.26, 6.8, 6.6, 6.19 |
| 38 | Lambert [34] | 2017 | To report the reasons why doctors are considering leaving medicine or the UK | Quantitative | UK | 1.16, 1.5, 1.6, 2.10, 2.14, 2.1, 3.17, 3.1, 3.11, 3.14, 3.4 | |
| 39 | BMA [38] | 2010 | To provide information on the careers of doctors, and particularly to: –– identify doctors who leave medicine as a career, or who choose to work in another country and to assess the factors which influence it | Mixed Methods | UK | 1.6, 2.19, 2.10, 2.14, 3.1, 3.13, 3.2 | |
| 40 | Young [45] | 2010 | To scope the main issues and identify gaps in knowledge around two key aspects of health professional mobility/migration – within- UK mobility (i.e. movement between England, Scotland, Wales and Northern Ireland) and mobility to and from the different UK countries and Europe | Mixed Methods | UK | 1.23, 1.11, 1.12, 1.15, 1.16, 1.26, 1.32, 1.40, 1.45, 2.18, 2.19, 2.20, 2.21, 2.10, 2.1, 2.2, 2.3, 2.7, 2.8, 3.18, 3.24, 3.1, 3.12, 3.2, 3.3, 3.4, 3.7 | 6.8, 6.22 |
Acknowledgements
We would like to acknowledge Francis Leng at the General Medical Council for providing feedback throughout the study.
Author contributions
NB, MB, TG and LB conceptualised the study. LB scoped and designed the search strategy. NL, NB and LB conducted the article selection. NL and NB conducted the data extraction. NL and NB conducted the coding of data and analysis. NB wrote the first draft of the paper. NB, NL, MB, TG, NH and AK critically reviewed it and provided comments to improve the manuscript. All authors read and approved the final manuscript.
Funding
This study was commissioned and funded by the General Medical Council. The GMC gave feedback on the search strategy and data analysis, and approved the manuscript for publication.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable as ethics approval is not required for a literature review.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ono T, Schoenstein M, Buchan J. Geographic imbalances in doctor supply and policy responses. OECD health working papers. 2014.
- 2.MacKay DI. Geographical mobility and the brain drain: a case of Aberdeen University graduates, 1860–1960. Allen and Unwin; 1969. [Google Scholar]
- 3.World Health Organization. Global strategy on human resources for health: workforce 2030. 2016.
- 4.Taylor M. Why is there a shortage of doctors in the UK? Bull R Coll Surg Engl. 2020;102:78–81. doi: 10.1308/rcsbull.2020.78. [DOI] [Google Scholar]
- 5.The Kings Fund. The healthcare workforce in England: make or break. 2018.
- 6.NHS England. Strengthening our workforce. vol. 2021; 2021.
- 7.Health Education England . Facing the facts, shaping the future: A draft health and care workforce strategy for England to 2027. London: Health Education England; 2017. [Google Scholar]
- 8.BBC News. NHS groups welcome immigration change for doctors and nurses—BBC news. 2018.
- 9.NHS medical staffing data analysis. https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/workforce/nhs-medical-staffing-data-analysis#:~:text=High%20vacancies&text=As%20of%20June%202022%2C%20over,are%20having%20on%20staff%20retention. Accessed 26 Jan 2023.
- 10.RCP census finds record number of physician jobs unfilled. https://www.rcplondon.ac.uk/news/rcp-census-finds-record-number-physician-jobs-unfilled#:~:text=More%20than%20half%20(52%25),Physicians%20and%20Surgeons%20of%20Glasgow. Accessed 26 Jan 2023.
- 11.Recent Trends in International Migration of Doctors, Nurses and Medical Students. https://www.oecd.org/health/recent-trends-in-international-migration-of-doctors-nurses-and-medical-students-5571ef48-en.htm.
- 12.Brennan N, Langdon N, Bryce M, Gale T, Knapton A, Burns L, Humphries N. Drivers of international migration of doctors to and from the United Kingdom. General Medical Council; 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.State of medical education in practice: the workforce report 2019 and data tables. https://www.gmc-uk.org/-/media/about/what-we-do-and-why/data-and-research/somep-2018/version-one---0412pm/somep-book-20187.pdf?la=en&hash=4368CA4DBF85A811AF171B70C4CD45843C0D5E7A. Accessed 10 Jan 2023.
- 14.Iacobucci G. Half of doctors from other EEA countries working in UK may leave, poll shows. BMJ (Clinical research ed) 2017;359:j5273. doi: 10.1136/bmj.j5273. [DOI] [PubMed] [Google Scholar]
- 15.De Haas H. A theory of migration: the aspirations-capabilities framework. Comp Migr Stud. 2021;9:1–35. doi: 10.1186/s40878-020-00210-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris JR, Todaro MP. Migration, unemployment and development: a two-sector analysis. Am Econ Rev. 1970;60:126–142. [Google Scholar]
- 17.Lee ES. A theory of migration. Demography. 1966;3:47–57. doi: 10.2307/2060063. [DOI] [Google Scholar]
- 18.Van Hear N, Bakewell O, Long K. Push-pull plus: reconsidering the drivers of migration. J Ethn Migr Stud. 2018;44:927–944. doi: 10.1080/1369183X.2017.1384135. [DOI] [Google Scholar]
- 19.Massey DS, Arango J, Hugo G, Kouaouci A, Pellegrino A. Worlds in motion: understanding international migration at the end of the millennium: understanding international migration at the end of the millennium. Clarendon Press; 1999. [Google Scholar]
- 20.Davda LS, Gallagher JE, Radford DR. Migration motives and integration of international human resources of health in the United Kingdom: Systematic review and meta-synthesis of qualitative studies using framework analysis. Hum Resour Health. 2018;16. [DOI] [PMC free article] [PubMed]
- 21.Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 23.Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, Stewart L. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. doi: 10.1186/2046-4053-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Young R, Humphrey C, Rafferty A. Motivation and experience of health professionals who migrate to the United Kingdom from other EU member countries. In: Buchan J, Wismar M, Glinos IA, Bremner J, editors. Health professional mobility in a changing Europe: new dynamics, mobile individuals and diverse responses. Geneva: World Health Organization; 2014. [Google Scholar]
- 25.Bornat J, Henry L, Raghuram P. The making of careers, the making of a discipline: luck and chance in migrant careers in geriatric medicine. J Vocat Behav. 2011;78:342–350. doi: 10.1016/j.jvb.2011.03.015. [DOI] [Google Scholar]
- 26.Herfs PG. Aspects of medical migration with particular reference to the United Kingdom and the Netherlands. Hum Resour Health. 2014;12:59. doi: 10.1186/1478-4491-12-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Legido-Quigley H, Saliba V, McKee M. Exploring the experiences of EU qualified doctors working in the United Kingdom: a qualitative study. Health Policy. 2015;119:494–502. doi: 10.1016/j.healthpol.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Wójcicka ABA, Salamonska J. National profile of migration of health professionals—Ireland. 2011.
- 29.Gureje O, Hollins S, Botbol M, Javed A, Jorge M, Okech V, Riba M, Trivedi JK, Sartorius N, Jenkins R. Report of the WPA task force on brain drain. World Psychiatry. 2009;8:115–118. doi: 10.1002/j.2051-5545.2009.tb00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bezuidenhout MM, Joubert G, Hiemstra LA, Struwig MC. Reasons for doctor migration from South Africa. S Afr Fam Pract. 2009;51:211–215. doi: 10.1080/20786204.2009.10873850. [DOI] [Google Scholar]
- 31.van der Pol M, Scott A, Irvine A. The migration of UK trained GPs to Australia: does risk attitude matter? Health Policy. 2019;123:1093–1099. doi: 10.1016/j.healthpol.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Smith SE, Tallentire VR, Pope LM, Laidlaw AH, Morrison J. Foundation year 2 doctors' reasons for leaving UK medicine: an in-depth analysis of decision-making using semistructured interviews. BMJ Open. 2018;8:e019456. doi: 10.1136/bmjopen-2017-019456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma A, Lambert TW, Goldacre MJ. Why UK-trained doctors leave the UK: cross-sectional survey of doctors in New Zealand. J R Soc Med. 2012;105:25–34. doi: 10.1258/jrsm.2011.110146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lambert T, Smith F, Goldacre MJ. Why doctors consider leaving UK medicine: qualitative analysis of comments from questionnaire surveys three years after graduation. J R Soc Med. 2017;1–13. [DOI] [PMC free article] [PubMed]
- 35.Lambert TW, Smith F, Goldacre MJ. Changes needed to medicine in the UK before senior UK-trained doctors, working outside the UK, will return: questionnaire surveys undertaken between 2004 and 2015. JRSM Open. 2017;8. [DOI] [PMC free article] [PubMed]
- 36.Gauld R, Horsburgh S. What motivates doctors to leave the UK NHS for a “life in the sun” in New Zealand; and once there, why don’t they stay? Hum Resour Health. 2015;13:75. doi: 10.1186/s12960-015-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quantin C, Abbas R, Hagi M, Le Breton G, Romestaing M, Carnet D: Comparison of British and French expatriate doctors' characteristics and motivations. BMJ Open 2012;2. [DOI] [PMC free article] [PubMed]
- 38.BMA. Cohort study of 2006 medical graduate’s Ninth report. 2010.
- 39.Wismar M, Maier C, Glinos I, Dussault G, Figueras J. Health Professional Mobility and Health Systems: Evidence from 17 European countries. 2011.
- 40.Ognyanova D, Maier CB, Wismar M, Girasek E, Busse R. Mobility of health professionals pre and post 2004 and 2007 EU enlargements: evidence from the EU project PROMeTHEUS. Health Policy. 2012;108:122–132. doi: 10.1016/j.healthpol.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 41.Bidwell P, Laxmikanth P, Blacklock C, Hayward G, Willcox M, Peersman W, Moosa S, Mant D. Security and skills: the two key issues in health worker migration. Glob Health Action. 2014;7:24194. doi: 10.3402/gha.v7.24194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buchan J, Wismar M, Glinos I, Bremner J. Health Professional Mobility in a Changing Europe: New dynamics, mobile individuals and diverse responses. 2014.
- 43.Blacklock C, Heneghan C, Mant D, Ward AM. Effect of UK policy on medical migration: a time series analysis of physician registration data. Hum Resour Health. 2012;10:35. doi: 10.1186/1478-4491-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McDermott C, Sheridan M, Moore K, Gosbell A. The medical boomerang: will it come back? Emerg Med J. 2015;32:330–332. doi: 10.1136/emermed-2014-204129. [DOI] [PubMed] [Google Scholar]
- 45.Young R. Motivations and experience of health professionals who migrate to the United Kingdom. Evaluation of international recruitment of health professionals in England. J Health Serv Res Policy. 2010;15:195–203. doi: 10.1258/jhsrp.2010.009068. [DOI] [PubMed] [Google Scholar]
- 46.Young R, Weir H, Buchan J. Health Professional Mobility in Europe and the UK: a scoping study of issues and evidence. In: Produced for the National Institute for health research service delivery and organisation programme. 2010.
- 47.Ramos P, Alves H. Migration intentions among Portuguese junior doctors: results from a survey. Health Policy. 2017;121:1208–1214. doi: 10.1016/j.healthpol.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 48.Khan F, Chikkatagaiah S, Shafiullah M, Nasiri M, Saraf A, Sehgal T, Rana A, Tadros G, Kingston K. International medical graduates (IMGs) in the UK—a systematic review of their acculturation and adaptation. Int Migr Integr. 2015;16:743–759. doi: 10.1007/s12134-014-0368-y. [DOI] [Google Scholar]
- 49.Bidwell P, Humphries N, Dicker P, Thomas S, Normand C, Brugha R. The national and international implications of a decade of doctor migration in the Irish context. Health Policy. 2013;110:29–38. doi: 10.1016/j.healthpol.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 50.Hosni MM, Rishard M. Take-home experience of overseas doctors at the end of their two years training placements in the International Doctors Training Programme in Obstetrics and Gynaecology in the United Kingdom: a questionnaire-based study. J Obstetrics Gynaecol. 2017;37:64–68. doi: 10.1080/01443615.2016.1209173. [DOI] [PubMed] [Google Scholar]
- 51.Adebayo A, Akinyemi OO. “What are you really doing in this Country?”: Emigration intentions of Nigerian doctors and their policy implications for human resource for health management. J Int Migr Integr. 2021:1–20. [DOI] [PMC free article] [PubMed]
- 52.Humphries N, Creese J, Byrne J-P, Connell J. COVID-19 and doctor emigration: the case of Ireland. Hum Resour Health. 2021;19:29. doi: 10.1186/s12960-021-00573-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Surman G, Goldacre MJ, Lambert TW. UK-trained junior doctors’ intentions to work in UK medicine: questionnaire surveys, three years after graduation. J R Soc Med. 2017;110:493–500. doi: 10.1177/0141076817738500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Torjesen I. Four in 10 European doctors may leave UK after Brexit vote, BMA survey finds. BMJ. 2017;356:j988. doi: 10.1136/bmj.j988. [DOI] [PubMed] [Google Scholar]
- 55.George G, Rhodes B. Is there a financial incentive to immigrate? Examining of the health worker salary gap between India and popular destination countries. Hum Resour Health. 2017;15:74. doi: 10.1186/s12960-017-0249-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Crossland DS, Ferguson R, Magee A, Jenkins P, Bulock FA, Parry A, Babu-Narayan SV, Carroll A, Daubeney PE, Simpson J. Consultant staffing in UK congenital cardiac services: A 10-year survey of leavers and joiners. Open Heart. 2021;8:e001723. doi: 10.1136/openhrt-2021-001723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mara I. Health professionals wanted: chain mobility across European countries. WIIW Research Report;2020.
- 58.Begum M, Lewison G, Lawler M, Sullivan R. The value of European immigration for high-level UK research and clinical care: cross-sectional study. J R Soc Med. 2019;112:29–35. doi: 10.1177/0141076818803427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bailey N, Mandeville KL, Rhodes T, Mipando M, Muula AS. Postgraduate career intentions of medical students and recent graduates in Malawi: a qualitative interview study. BMC Med Educ. 2012;12. [DOI] [PMC free article] [PubMed]
- 60.Schumann M, Maaz A, Peters H. Doctors on the move: a qualitative study on the driving factors in a group of Egyptian physicians migrating to Germany. Glob Health. 2019;15:2. doi: 10.1186/s12992-018-0434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Labonte R, Sanders D, Mathole T, Crush J, Chikanda A, Dambisya Y, Runnels V, Packer C, MacKenzie A, Tomblin Murphy G, Bourgeault I. Health worker migration from South Africa: causes, consequences and policy responses. Human Resour Health. 2015;13. [DOI] [PMC free article] [PubMed]
- 62.Smith C, Pettigrew LM, Seo H-N, Dorward J. Combining general practice with international work: online survey of experiences of UK GPs. JRSM Short Rep. 2012;3:46. doi: 10.1258/shorts.2012.012054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Soc Sci Med. 2002;54:1255–1266. doi: 10.1016/S0277-9536(01)00094-6. [DOI] [PubMed] [Google Scholar]
- 64.Skeldon R. Population mobility in developing countries. Belhaven Press; 1990. [Google Scholar]
- 65.NHS England. Five year forward review. 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf. Accessed 10 Jan 2023.
- 66.NHS England. Next steps on the NHS five year forward view. 2017. https://www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf. Accessed 10 Jan 2023.
- 67.Sanders JGG. NHS staff health and wellbeing: CQUIN supplementary guidance. 2016.
- 68.West M, Coia D. Caring for doctors, caring for patients. General Medical Council. 2019.
- 69.Humphries N, McAleese S, Matthews A, Brugha R. Emigration is a matter of self-preservation. The working conditions... are killing us slowly' qualitative insights into health professional emigration from Ireland. Human Resour Health. 2015;13:35. doi: 10.1186/s12960-015-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Campbell D. Brexit has worsened shortage of NHS doctors, analysis shows. In: The Guardian; 2022.
- 71.Milner A, Nielsen R, Norris E. Brexit and European doctors’ decisions to leave the United Kingdom: a qualitative analysis of free-text questionnaire comments. BMC Health Serv Res. 2021;21:1–8. doi: 10.1186/s12913-021-06201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Humphries N, Crowe S, McDermott C, McAleese S, Brugha R. The consequences of Ireland's culture of medical migration. Hum Resour Health. 2017;15:87. doi: 10.1186/s12960-017-0263-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Clarke N, Crowe S, Humphries N, Conroy R, O'Hare S, Kavanagh P, Brugha R. Factors influencing trainee doctor emigration in a high income country: a mixed methods study. Hum Resour Health. 2017;15:66. doi: 10.1186/s12960-017-0239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Humphries N, Tyrrell E, McAleese S, Bidwell P, Thomas S, Normand C, Brugha R. A cycle of brain gain, waste and drain—a qualitative study of non-EU migrant doctors in Ireland. Hum Resour Health. 2013;11:63. doi: 10.1186/1478-4491-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Milner A, Nielsen R, Verdery AM. Brexit and the European national health service England workforce: a quantitative analysis of doctors’ perceived professional impact and intentions to leave the United Kingdom. Ann Glob Health. 2021;87. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.