Abstract
Purpose The purpose of this study is to characterize the influence of a new night float rotation on resident wellness and performance in the Duke University Eye Center Ophthalmology Residency Program.
Methods We analyzed three classes of ophthalmology residents: one class ( n = 4) utilized the new night float rotation with no daytime clinical duties, while two senior classes ( n = 12) utilized the traditional call system wherein they had daytime and nighttime responsibilities. Residents completed a questionnaire regarding their perceptions of the night float rotation. Supervising attendings ( n = 15) were also surveyed about their perceptions of the new rotation.
Results Zero of the four residents on the night float rotation reported burnout compared with 6 of 11 residents in the traditional call system. Most residents supported the adoption of the night float rotation, but this trend was less apparent among fellows and attendings.
Most respondents believed the new night float rotation reduced burnout, fatigue, and work hours while increasing time for nonclinical activities. Perceived skills gained while on call were felt to be similar between the two call systems. Fellows and attendings believed residents in the night float system performed similarly or better than residents in the traditional system in indicators such as knowledge and enthusiasm. There was no significant difference in the average number of patient encounters (290.8 ± 30.5 vs. 310.7 ± 25.4, p = 0.163), phone encounters (430.8 ± 20.2 vs. 357.1 ± 90.0, p = 0.068), or average hours worked per week (57.3 ± 4.6 vs. 58.0 ± 5.7 p = 0.797) per resident between night float residents and traditional call residents.
Conclusions This study shows resident support for a night float rotation in ophthalmology residency at Duke, with reductions in burnout and more time for nonclinical activities without affecting perceived clinical performance. We hope this study serves as an impetus for other ophthalmology programs considering a transition to a night float system.
Keywords: ophthalmology, residency, night float, call
After completion of an integrated, joint, or nonophthalmic internship year, ophthalmology residency consists of a 3-year training program including the clinical and surgical management of eye diseases. To gain exposure of the breadth of ophthalmic pathology, residents rotate though various outpatient subspecialty clinics and evaluate ophthalmic consultations in the emergency department and inpatient units. While residency programs vary in their consultation structure, generally one resident is responsible for initially evaluating all patients and staffing each case with a supervising attending physician. This also occurs overnight, ensuring 24 hours of availability to evaluate consultation requests.
Traditionally, most ophthalmology residencies implement a similar model for overnight consultation coverage. Ophthalmology residents spend the daytime in clinics and the operating room, with one resident evaluating daytime consultations. In the Duke University Eye Center Ophthalmology Residency Program, the 6 postgraduate year 2 (PGY-2) residents equally divide nighttime and weekend coverage, with a senior resident also on call to assist with complex cases or those that require surgical intervention.
While often a source of anxiety, 1 seeing emergency and inpatient consults is certainly an important aspect of any residency program. The opportunity to explore a vast array of ophthalmologic complaints and diagnoses is crucial to the early resident's foundational knowledge. Indeed, previous studies have identified some of the most common diagnoses from consultations to be refractive error, conjunctivitis, corneal abrasion, diabetic retinopathy, and systemic conditions (such as, infections) for which a dilated exam was needed to rule out ocular involvement. 2 3 4 While evaluating consults, residents also improve their history-taking and bedside examination skills while building confidence, 1 learning to triage multiple consults, and comanaging patients with nonophthalmology providers.
Despite offering the opportunity to explore vast ophthalmologic complaints while on call, a traditional call schedule creates a situation in which residents are often working around the clock, which can lead to fatigue, burnout, or mistakes. Prior studies in other medical and surgical specialties report that work-hour reduction and regulation in residency reduce patient mortality 5 and does not affect physicians' performance as independent practitioners after graduation from residency. 6 Specific to ophthalmology residency, approximately a quarter of ophthalmology residency programs face issues involving resident depression, burnout, or suicide. 7 This is felt to be due to the complexities of ophthalmic surgery and rapid evolution of therapeutics within the field. 8
This is the first study to assess the effects of a night float system on ophthalmology residency. The purpose of this effort is to better understand how resident wellness and perceived performance have been influenced by recent changes in the call schedule within the Duke Ophthalmology Residency Program. In response to resident feedback, as of June 2020, the program transitioned to a rotational “night float” system, wherein one resident is working only the “on call” shift 5 days a week for several weeks and has no daytime responsibilities, leaving the other five residents in the program to rotate call responsibilities only for the weekends.
Methods
This study was given exempt designation by the Institutional Review Board at the Duke University Medical Center and utilized a combination of questionnaires administered to residents, fellows, and attendings as well as collection of objective metrics for each resident during his/her year of primary call.
Call Structure: Old versus New
The new night float and traditional call systems are described in Table 1 . In the traditional system, 2 junior residents were responsible for covering primary night call (all emergency and inpatient consultations) from Sunday night through Thursday night each week for 1-month stretches. One of the residents covered Sunday night through Tuesday night, and the other resident would cover Wednesday night and Thursday night. In addition to primary night call, each of these residents would also have at least one-half day of required daytime clinic each day. Weekday primary call responsibilities were handled by the resident on the consult rotation, and weekend coverage was provided by the remaining PGY-2 residents.
Table 1. Old versus new call structures.
| A | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Day | Day consult resident | Day consult resident | Day consult resident | Day consult resident | Day consult resident | Other resident 2 | Other resident 2 |
| Night | Night resident 1 | Night resident 1 | Night resident 2 | Night resident 2 | Other resident 1 | Other resident 1 | Night resident 1 |
| B | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Day | Day consult resident | Day consult resident | Day consult resident | Day consult resident | Day consult resident | Other resident 2 | Other resident 2 |
| Night | Night float resident | Night float resident | Night float resident | Night float resident | Other resident 1 | Other resident 1 | Night float resident |
A . Structure of the traditional call system, where two residents were responsible for night coverage while also maintaining daytime clinical responsibilities. B . Structure of the new night float system, where one resident is responsible for night coverage with no daytime clinical responsibilities.
In the new night float system, only one junior resident was responsible for covering night call from Sunday night through Thursday night each week for 1-month stretches. This resident carried virtually no daytime clinical responsibilities while on this night float rotation. Like the traditional call system, weekday primary call responsibilities were handled by the resident on the consult rotation. Weekend coverage was provided by the remaining PGY-2 residents.
In both systems, only PGY-2 took the primary call responsibilities to evaluate emergency and inpatient consultations. Senior residents (PGY-3 and PGY-4) serve as backup for surgical emergencies or high-volume situations where the junior resident requires additional assistance.
Study Design
This study analyzed three classes of ophthalmology residents in the Duke Ophthalmology Residency Program: 1 first year class (graduating 2023, n = 4, 2 residents excluded as they were study investigators), who utilized the new night float system, and 2 senior classes (graduating 2021 and 2022, respectively, total n = 12), who utilized the traditional call system in which residents who were on call at night would also have daytime clinical responsibilities.
This study was a cross-sectional analysis of perceptions of the new night float system. Each class was asked to complete a questionnaire regarding perceptions of the new night float system in comparison to the traditional system. Because the literature is lacking in studies assessing night float perceptions, this questionnaire was created by study authors. Additionally, a previously validated single-item questionnaire regarding burnout was included in this questionnaire. 9 To assess attending and fellow perspectives on the new night float system, a similar questionnaire was administered to those fellows and attendings who directly supervised first year residents ( n = 25) and who were present at Duke during both call systems. They were additionally asked about their perceptions of resident performance and fatigue during the daytime in the new night float system compared with the traditional system.
Additionally, objective metrics from each resident's primary call year were collected. These metrics included total inpatient and emergency department patient encounters, total phone consultation volume while on primary call, and self-reported average number of hours worked per week while taking primary call. These objective measures were compared between residents in the night float system and residents in the traditional call system using Student's t -tests.
Results
A total of 4 first year residents participating in the new night float system from 2020 to 2021 (100% response rate) and 11 senior residents who participated in the traditional call system from 2018 to 2020 (91.7% response rate) participated in the questionnaires. A total of 15 fellows and attendings completed the questionnaire (60% response rate).
Table 2 describes the responses to the single-item burnout questionnaire question, “Overall, based on your definition of burnout, how would you rate your level of burnout?” While a total of 4 of 9 residents in the traditional call system (44%) reported burnout while on call, 0 of the 4 residents in the new night float system reported burnout.
Table 2. Burnout inventory scores.
|
Question:
Overall, based on your definition of burnout, how would you rate your level of burnout?
Response options: 1. I enjoy my work. I have no symptoms of burnout. 2. Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out. 3. I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion. 4. The symptoms of burnout that I'm experiencing won't go away. I think about frustration at work a lot. 5. I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help | |
| Resident type | Residents burned out, number (%) |
| New night float resident, n = 4 | 0 (0%) |
| Traditional call system resident, n = 11 | 6 (54.5%) |
Comparing resident perceptions of burnout between the new night float system to the traditional call system. Presence of burnout was defined as choosing a level of 3–5 on the single-item questionnaire. NOTE: Two residents in the new night float system were excluded from the questionnaire because they are investigators of this study (SA and AG).
Residents who were part of the new night float system unanimously supported this new call system. Most residents (77%, n = 7) who completed the traditional call rotation were also very likely to support the adoption of this new call schedule; only one resident was unlikely to support it. Finally, responses by attendings and fellows were more variable. While 4/9 respondents were very likely to support the new rotation, 3 were neutral regarding their support, and 1 was very unlikely to support it ( Fig. 1A ).
Fig. 1.
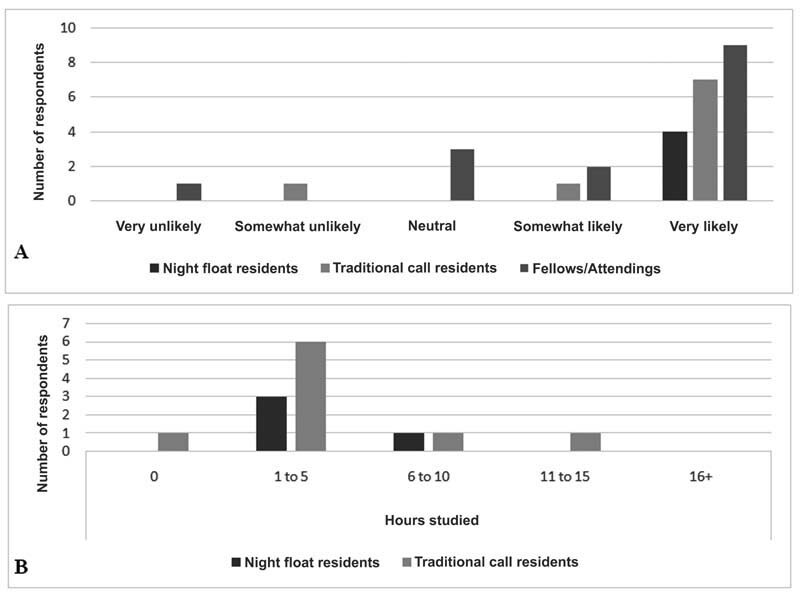
( A ) Likelihood of residents, fellows, and attendings to support the new night float rotation. Residents who were in the new night float rotation and residents in the traditional call rotation were asked how likely they would be to support the new night float system ( n = 9). Fellows and attendings were asked the same question ( n = 15) ( B ) Study time during call. Residents were asked approximately how many hours per week they studied for the Ophthalmic Knowledge Assessment Program while on the night float rotation or the traditional call system.
With regard to time to study per week, most residents studied 1 to 5 hours per week while on the new night float rotation and traditional call rotation, without clear differences in study time between the two systems ( Fig. 1B ).
Fig. 2 outlines the resident and fellow/attending perceptions of the effects of the new night float system. The overwhelming majority of resident, fellow, and attending respondents believed that the new night float rotation reduces burnout, fatigue, and work hours. Conversely, the time to study, pursue scholarly activity, and spend time with family and friends was felt to increase with the initiation of the night float rotation. The degree of clinical independence and ability to handle ophthalmologic emergencies by the end of the first year of training was generally felt to be similar between the new night float rotation and traditional call rotation.
Fig. 2.
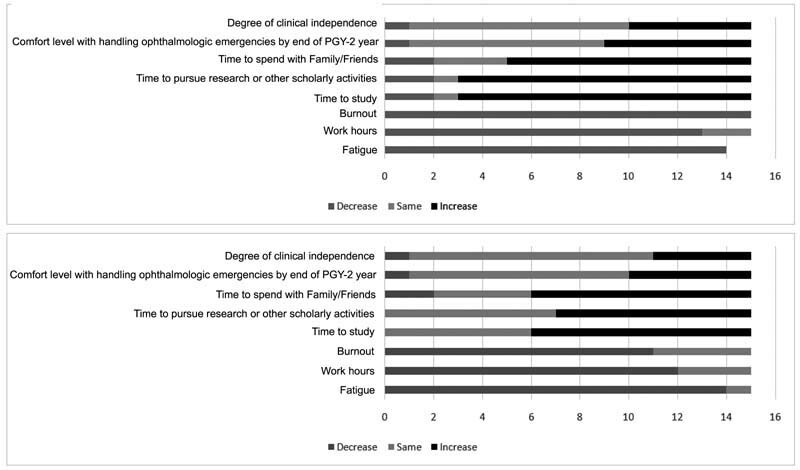
( A ) Residents were asked if they believe the night float system increases or decreases several different parameters, listed on left. n = 15, except for the parameter “fatigue,” which only had 14 respondents. ( B ) Fellows and attending were asked if they believe the night float system increases or decreases several different parameters, listed on left. n = 15. PGY-2, postgraduate year 2.
In terms of objective measures, there was no statistically significant difference in the number of inpatient or emergency department examinations completed per resident between those residents in the night float system and those in the traditional call system (290.8 ± 30.5 vs. 310.7 ± 25.4, respectively, p = 0.163; Fig. 3 ). The same was true of the after-hours phone consultation volume (430.8 ± 20.2 vs. 357.1 ± 90.0, respectively, p = 0.068, Fig. 3 ). Finally, there was no significant difference in the number of hours worked per week on average for the academic year between the 2 groups (57.3 ± 4.6 for night float residents versus 58.0 ± 5.7 for traditional call residents, p = 0.797; Fig. 4 ).
Fig. 3.
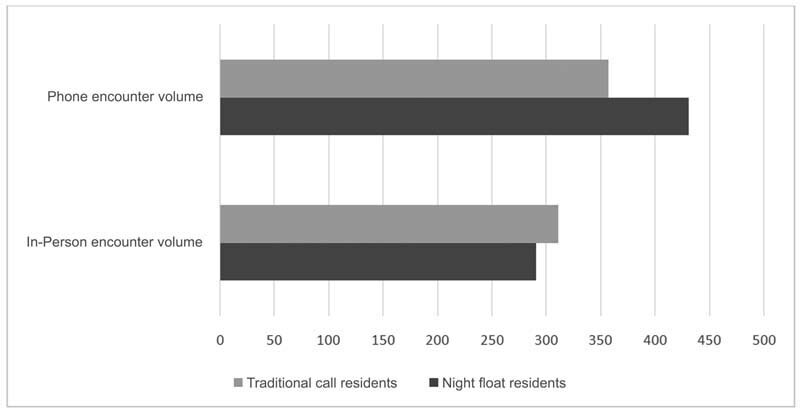
Encounter volume, in-person and phone, between residents in the night float system and residents in the traditional call system. There was no significant difference in phone and in-person encounter volumes between the two groups (290.8 ± 30.5 vs. 310.7 ± 25.4, respectively, p = 0.163). The same was true of the after-hours phone consultation volume (430.8 ± 20.2 vs. 357.1 ± 90.0, respectively, p = 0.068).
Fig. 4.
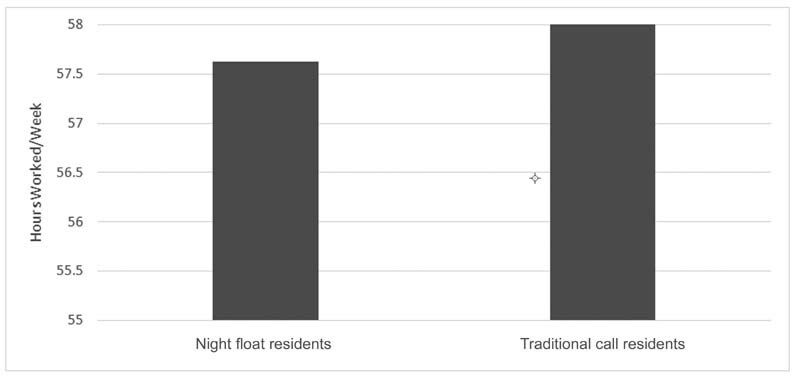
Mean hours worked per week between residents in the night float system and residents in the traditional call system. There was no statistically significant difference in hours worked per week between the two groups (57.3 ± 4.6 for night float residents vs. 58.0 ± 5.7 for traditional call residents, p = 0.797).
Finally, fellows and attendings were asked if they believed that there was a difference in performance between residents who participated in the new night float rotation versus those in the traditional call rotation. Across all the key parameters of on-time arrival to clinic, knowledge, volume of clinic patients seen by the residents, appearance of fatigue, surgical performance, and enthusiasm, fellows and attendings felt that residents in the new night float system performed similarly if not better than residents in the traditional system ( Table 3 ).
Table 3. Perceptions of resident performance.
| In comparison to the residents who were part of the old call system, how do you think the residents participating in the night float system are performing in the following parameters? | |||
|---|---|---|---|
| Parameter | Worse | Same | Better |
| On-time arrival to daytime clinic | 0 (0%) | 12 (92.3%) | 1 (7.7%) |
| Knowledge | 0 (0%) | 11 (78.6%) | 3 (21.4%) |
| Volume of clinic patients seen | 1 (11.1%) | 10 (76.9%) | 2 (15.4%) |
| Appearance of fatigue | 0 (0%) | 6 (46.2%) | 7 (53.9%) |
| Surgical performance | 0 (0%) | 8 (66.7%) | 4 (33.3%) |
| Enthusiasm | 0 (0%) | 7 (53.9%) | 6 (46.2%) |
Fellows and attendings were asked if they believe that residents in the night float system performed better, worse, or about the same compared with residents in the traditional call system, for their daytime clinical duties. a
n = 12–14 (not all participants answered every question).
Discussion
Resident duty hour limits—80 hours per week—were initially established by the Accreditation Council for Graduate Medical Education in 2003, leading residency programs to replace 24-hour (or more) call systems with night float rotations to meet the new restrictions. Since then, several studies have been published to assess the advantages and disadvantages of night float rotations. 10
Programs that transitioned to a night float system found better success in reducing resident work hours, as well resident fatigue, while increasing time for sleep. 11 12 13 Patients also seem to benefit from a night float system. Previous studies describe improved quality of care as perceived by ancillary staff and better adherence to evidence-based guidelines, improving perceived patient care as determined by patients themselves and ancillary staff. 11 14
Other studies have found drawbacks to night float systems. One major disadvantage of a night float system is an increased frequency of handoffs, leading to decreased continuity of care. 11 15 Certainly, ophthalmology residents in a night float system often do not have the opportunity to see emergency department patients again on follow-up, limiting the opportunity for feedback and learning from each case. Further, one study found that while on night float, residents may have decreased sleep quantity and quality. 16 Finally, some have argued that residents have fewer educational opportunities, reduced lecture attendance, and limited supervision while on night float rotations. 17 18 However, Welling et al found no such difference in conference attendance between surgical residents in a traditional call system compared with night float system. 19
This is the first study to directly assess the effects of a night float system on an ophthalmology residency program. While the sample size is small, and the study is limited to a single residency program, there is strong support for this transition among the residents evaluated. Most fellows and attendings support this system, with a minority remaining neutral in their support between the new night float system and traditional system.
We speculate that the widespread support for a night float rotation is multifactorial. First, residents in this study were less likely to experience burnout with night float rotations. The single-item burnout inventory showed that none of the residents in the new night float rotation reported burnout, compared with nearly half of the residents in the old call system reporting at least some degree of burnout. Second, we believe that residents in the traditional call system, by virtue of carrying both night and daytime clinical duties, have more fragmented sleep schedules. Not only does this negatively impact their overall health and well-being, but fragmented sleep itself is associated with burnout. 20 Finally, residents perceive more time to engage in other scholarly activity, study, and spend time with friends and family with the new night float system.
Interestingly, fellows and attendings generally believed that resident performance was the same or better when comparing residents in the new night float system to residents in the traditional system. Again, we hypothesize that more time for continuous sleep, more perceived time to study, and more time to decompress outside of work contribute to high performance while at work. All of this occurred without changes in the number of patient encounters, phone encounters, or overall clinical hours worked per week throughout the year between residents in the night float system and residents in the traditional call system. Further, the transition to the night float system did not lead to sacrificing other daytime activities; in fact, residents in both systems had the same core rotations. The key difference was that instead of splitting weeknight call and daytime clinical responsibilities between two residents who were on two separate rotations, this call was consolidated for one resident to handle only weeknight call and one resident to handle only weekday clinical duties. Thus, a transition to a night float system does not affect the clinical volume residents are exposed to.
Despite this promising data about night float rotations for ophthalmology residency, there are only a handful of ophthalmology programs in the United States with a true night float rotation, where a single resident sees nighttime consultations and has no daytime clinical responsibilities. In many cases, this may simply be due to the small number of residents in each class. This necessitates residents help in busy clinics during the daytime while also providing call coverage at night. An additional barrier is a lack of guidance or templates for creating a schedule that allows residency programs to implement night float rotations. Finally, it is difficult to adopt the new system without clear data on the impact of night float rotations on ophthalmology resident performance and wellness. We hope this study initiates a trend toward more ophthalmology residency programs adopting and analyzing the impact night float rotations.
This study was limited by the small sample size and only reflects the experience of one program, which may not be generalizable across all residency programs in ophthalmology. Further, objective metrics of hours worked per week were self-reported. Ophthalmic Knowledge Assessment Program scores were also not collected due to small sample sizes and inability to draw conclusive comparisons of scores during the coronavirus disease 2019 (COVID-19) pandemic. Additionally, the response rate among fellow and attendings was 60%, which may introduce non-response bias. Moreover, the questionnaire responses of the senior residents in the old night float system are highly dependent on memories of the rotation completed during their first year of training any may be affected by current or cumulative levels of burnout. Finally, the night float sample residents took call during the COVID-19 pandemic, which likely caused fluctuations in emergency, inpatient, and phone consultation volumes when compared with pre-pandemic volumes.
Further studies must be done to better understand the objective aspects of night float rotations in ophthalmology residency. Important hypotheses to be tested include whether night float rotations during ophthalmology residency reduce clinical duty hours, how night float systems impact resident clinical and surgical volume, and if night float rotations improve clinical knowledge and board exam performance.
Conflict of Interest No conflicting relationship exists for any author.
Financial Support
None.
References
- 1.McCoskey M, Shafer B, Nti A. First-year ophthalmology residency call structure and its association with resident anxiety and confidence. J Acad Ophthalmol. 2019;11(01) doi: 10.1055/s-0039-1677845. [DOI] [Google Scholar]
- 2.Carter K, Miller K M. Ophthalmology inpatient consultation. Ophthalmology. 2001;108(08):1505–1511. doi: 10.1016/s0161-6420(01)00630-3. [DOI] [PubMed] [Google Scholar]
- 3.Mayer J, Landis Z, Wang M. Scott IU. Characteristics of inpatient ophthalmology consults associated with ocular pathology and need for ophthalmologic intervention. Invest Ophthalmol Vis Sci. 2014;55(13):5554. [Google Scholar]
- 4.Rizzuti A E, Vastardi M, Hajee M, Lazzaro D R. Scope of resident ophthalmology consultation service and patient follow-up rates at a level 1 trauma center in Brooklyn, New York. Clin Ophthalmol. 2013;7:643–647. doi: 10.2147/OPTH.S43345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shetty K D, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147(02):73–80. doi: 10.7326/0003-4819-147-2-200707170-00161. [DOI] [PubMed] [Google Scholar]
- 6.Jena A B, Farid M, Blumenthal D, Bhattacharya J. Association of residency work hour reform with long term quality and costs of care of US physicians: observational study. BMJ. 2019;366:l4134. doi: 10.1136/bmj.l4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tran E M, Scott I U, Clark M A, Greenberg P B. Assessing and promoting the wellness of united states ophthalmology residents: a survey of program directors. J Surg Educ. 2018;75(01):95–103. doi: 10.1016/j.jsurg.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Sadun A A. The challenge of teaching ophthalmology: a Residency Review Committee perspective. Ophthalmology. 2000;107(11):1971–1972. doi: 10.1016/s0161-6420(00)00088-9. [DOI] [PubMed] [Google Scholar]
- 9.Dolan E D, Mohr D, Lempa M. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(05):582–587. doi: 10.1007/s11606-014-3112-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine A C, Adusumilli J, Landrigan C P. Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010;33(08):1043–1053. doi: 10.1093/sleep/33.8.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldstein M J, Kim E, Widmann W D, Hardy M A. A 360 degrees evaluation of a night-float system for general surgery: a response to mandated work-hours reduction. Curr Surg. 2004;61(05):445–451. doi: 10.1016/j.cursur.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Harvard Work Hours, Health and Safety Group . Lockley S W, Cronin J W, Evans E E. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 13.Carey J C, Fishburne J I. A method to limit working hours and reduce sleep deprivation in an obstetrics and gynecology residency program. Obstet Gynecol. 1989;74(04):668–672. [PubMed] [Google Scholar]
- 14.Bhavsar J, Montgomery D, Li J. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120(11):968–974. doi: 10.1016/j.amjmed.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 15.Vaughn D M, Stout C L, McCampbell B L.Three-year results of mandated work hour restrictions: attending and resident perspectives and effects in a community hospital Am Surg 20087406542–546., discussion 546–547 [PubMed] [Google Scholar]
- 16.Dunn L K, Kleiman A M, Forkin K T. Anesthesiology resident night float duty alters sleep patterns: an observational study. Anesthesiology. 2019;131(02):401–409. doi: 10.1097/ALN.0000000000002806. [DOI] [PubMed] [Google Scholar]
- 17.Bricker D A, Markert R J. Night float teaching and learning: perceptions of residents and faculty. J Grad Med Educ. 2010;2(02):236–241. doi: 10.4300/JGME-D-10-00005.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lefrak S, Miller S, Schirmer B, Sanfey H. The night float system: ensuring educational benefit. Am J Surg. 2005;189(06):639–642. doi: 10.1016/j.amjsurg.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 19.Welling R E, Boberg J T, Weinberg E, Gulley J. Work hours compliance in a community hospital. Curr Surg. 2004;61(02):241–243. doi: 10.1016/j.cursur.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Söderström M, Jeding K, Ekstedt M, Perski A, Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. 2012;17(02):175–183. doi: 10.1037/a0027518. [DOI] [PubMed] [Google Scholar]


