Abstract
Background
Delineating the compound psychological effect of the pandemic on cancer care, and the interdependency across cancer patient-caregiver dyads have yet to be explored. This study examines the levels of psychological impact of COVID-19 on patient-caregiver dyads anxiety, and the interdependent associations between their COVID-19 and cancer concerns, and risk perceptions.
Method
There were 352 patients and caregivers (patient-caregiver dyads, N = 176) included in this study (43.2% spousal dyads). Generalized Anxiety Disorder-7 and questionnaires regarding risk perception, perceived confidence in healthcare system, COVID-19, and cancer-related concerns were administered. Actor-Partner Interdependence Model (APIM) analyses were used to determine the interdependent effects. Indirect effects were tested using mediation pathway analyses.
Results
Patients reported significantly higher levels of risk perceptions and anxiety than their caregivers (p < 0.01). Anxiety rates (GAD-7 ≥ 10) were also significantly higher (26.7% vs 18.2%, p < 0.01). Dyads’ anxiety, “general COVID-19 concerns,” “cancer-related concerns,” and risk perceptions were correlated (ps < 0.01). APIM showed only actor effects of general COVID-19 concerns, cancer-related COVID-19 concerns, and risk perceptions on anxiety (βs = 0.19–0.53, ps < 0.01). No partner effects were observed. Similar results were found in the composite APIM. Indirect effects of the patient/caregiver’s variables on their partner’s anxiety were observed in the mediation analyses.
Conclusion
Concerns about COVID-19 and cancer care could be indirectly associated in patient-caregiver dyads and need to be proactively addressed. As pandemic evolves into endemicity, engagement with patients and caregivers should strive to be sensitive to their differential needs and messages should be tailored to the informational needs of each.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12529-023-10154-5.
Keywords: Coronavirus, Oncology, Dyadic, Caregiving, Psycho-oncology
Background
The COVID-19 pandemic has threatened global health with unprecedented impacts on all domains of life. The rapid proliferation of cases and ensuing public health mandates brought up changes in delivery of healthcare services [1] which is of particular concern for those populations for whom treatment cannot be deferred. Disruptions were noted for various services related to screening, chronic disease management, or elective treatments [1], even in the context of cancer in which timely treatment is imperative [2, 3]. Due to their compromised immune system, patients with cancer have significantly higher risk of infection and poor outcomes if infected with COVID-19, i.e., complications or mortality [4, 5]. Studies in cancer patients have also noted increased symptoms of anxiety and insomnia, and emotional vulnerability in the context of COVID-19 [6, 7].
Cancer patient-caregiver relationships have also been significantly impacted by COVID-19. In light of the shift in family caregiving research from looking at caregivers as individuals to conceptualizing patient-caregiver dyads as single units of analysis [8], studies of cancer patients and their caregivers have examined dyad-level concepts including communication, reciprocal influence, and caregiver-patient congruence [8, 9]. In that respect, the health and psychological outcomes of cancer patients and caregivers are highly interdependent and reciprocal, and direct and indirect influences exist within dyads [10, 11]. In the context of COVID-19, one’s concerns and fears relating to the disease and its impact on the management of cancer could directly and indirectly “spillover” to their partner’s own concerns and fears, which could then elevate their anxiety levels [12, 13]. These impacts have been documented in COVID-19 studies of dyads including pregnant women and spouses [14]; parent–child dyads [15]; romantic couples [16]; and patient-caregiver dyads with chronic illness [17]. However, studies on the direct and indirect influences within cancer patient-caregiver dyads remain limited.
In Singapore, while provision of cancer treatment continued, important changes were made in cancer care services, such as the reprioritization of elective procedures or diagnostic tests, and changes in protocol related to entry in specialized setting and visitation(s) coupled with public health measures related to social distancing. Majority of these policies remained in place since their introduction in 2020 and 2021 with the increased severity and spread of the virus in the community [18]. Multiple studies have documented the impact of the measures on cancer care, in terms of delays in cancer screenings and in patients’ own fears of being infected with COVID-19 [19–21]. However, the compound psychological effect of the pandemic on cancer care, and the interdependency across the patient-caregiver dyads have yet to be explored.
Therefore, this study set out to explore the dyadic perspectives on concerns related to COVID-19 and cancer, and to examine the degree of interdependence in cancer patient-caregiver dyads. Specifically, the objectives of this study were as follows:
-
(i)
To document the levels of anxiety, fear of COVID-19, cancer-related concerns, risk perception, and confidence in healthcare as a result of the pandemic in cancer patients and caregivers,
-
(ii)
To examine the interdependent associations between cancer patients and caregivers in their fear of COVID-19, cancer-related concerns, risk perception, and confidence in healthcare on levels of anxiety, and
-
(iii)
To explore the indirect effects and pathways between cancer patients and caregivers in their concerns of COVID-19, cancer-related concerns, risk perception, and confidence in healthcare on levels of anxiety.
It is hypothesized that there exist interdependent dyadic influences between cancer patients and their caregivers in their psychological responses towards COVID-19, and that these dyadic influences may also manifest as indirect effects of one’s own concerns and perceptions on their partner’s concerns and perceptions related to COVID-19. Given the paucity of prior evidence, we did not formulate specific directional hypotheses with regard to directionality of these dyadic direct and indirect effects.
Methods
This study was nested in a larger cross-sectional epidemiological study on the psychosocial impact of COVID-19 on cancer patients and caregivers, and healthcare workers. The main study was launched during the initial phase of the pandemic (March to June 2020) and aimed to provide rapid cross-sectional data of cancer patients and caregivers, and healthcare workers’ areas of concerns and worries regarding cancer and COVID-19, and their levels of psychological wellbeing. Main findings from the study have been previously published [22, 23]. Ethics approval was obtained from Singhealth Centralized Institutional Review Board (CIRB number: 2020/2155).
Setting and Participants
The main study where this cohort was derived from consisted of a total of N = 1453 cancer patients, caregivers, and healthcare workers. Data from patient-caregiver dyads within the study were extracted for this study. The full recruitment methodology has been described previously [22]. Participants were recruited from xxx, a tertiary specialized center providing cancer treatment for majority (60–70%) of patients with cancer in Singapore. The following inclusion criteria for patients and caregivers were applied: (a) English- or Chinese-speaking, (b) age ≥ 21 years old, and (c) current diagnosis of (any) cancer (for patients) or providing care for patient with cancer treated in xxx (for caregivers). Eligible patients were approached by research coordinators at the clinic and the caregivers were identified and recruited at the same time and completed the study questionnaires following consent. The study was conducted from 25 March to 10 June 2020.
Measures
Sociodemographic (age, gender, ethnicity, education, employment status, personal income) and clinical information (housing type, marital status, cancer type, stage, and details of current treatment) were collected using self-report. The respondents also indicated the number of precautionary behaviors relating to COVID-19 prevention that they have undertaken. A questionnaire battery assessing the psychological response to COVID-19 was developed guided by measures of relevant constructs in prior work (i.e., previous cross-sectional studies on SARS and avian influenza; [24–26]), experts’ input, and our formative qualitative research on psychosocial impact of COVID-19 in cancer [23] (i.e., interviews with patients and caregivers). The measures included in the questionnaire battery are listed below: (see Appendix for questionnaire set).
Anxiety
Anxiety was measured using the Generalized Anxiety Disorder-7 (GAD-7) scale [27]. The GAD-7 comprises seven items used to screen for generalized anxiety disorder and was shown to have good psychometric properties in cancer populations [28] and the local context [29]. Participants are asked to rate on a scale ranging from 0 (not at all) to 3 (nearly every day) the frequency over the past 2 weeks in which they have been bothered by each symptom (e.g., not being able to stop or control worrying). Scores were obtained by summing the items (range 0 to 21) which were classified based on the recommended cutoff for caseness of anxiety (i.e., ≥ 10) [27] (Cronbach’s alpha = 0.94 in our study).
General COVID-19 Concerns and Cancer-Related COVID-19 Concerns
Drawing on prior interviews with patients with cancer and caregivers [23], a 16-item questionnaire was developed to assess fears and concerns about COVID-19. Exploratory factor analyses on the patients’ and caregivers’ responses [22] indicated two distinct subscales: “general COVID-19 concerns” (6 items; Cronbach’s alpha = 0.92) (e.g., “I am afraid because COVID-19 may have mass community spreading”) and “cancer-related COVID-19 concerns” (9 items; Cronbach’s alpha = 0.93) (e.g., “I worry about disruptions to cancer treatment due to the COVID-19 outbreak”). Items were identical for both patients and caregivers with the exception that the wording “my cancer” was replaced with “the patient’s cancer” for the caregivers. Items were rated on a 5-point Likert scale (1—Not at all to 5—Extremely) with higher scores signifying greater concerns.
Risk Perception
A 4-item measure of perceived risk was developed based on prior work on H1N1 [24]. The items were rated on a scale from 0 to 100 and an overall risk perception score was derived by aggregating item scores, with total score indicating higher perceived risk. The items for risk perception included the “perceived risk of COVID-19 encounter(s),” “perceived risk of COVID-19 infection,” and “prognosis in terms of complications and recovery.” The Cronbach’s alpha for risk perception scale was 0.65.
Perceived Confidence in Healthcare System
A 5-item measure was developed based on prior work and our formative qualitative research [18] to measure perceived confidence in the healthcare system. Items were rated on a scale from 1 to 10 and assessed confidence in healthcare providers (e.g., “healthcare professionals’ ability to recognise symptoms of COVID-19”), healthcare system (e.g., “level of preparedness of health-care facilities in Singapore to manage the COVID-19 outbreak”), and personal abilities (e.g., “taking care of your personal hygiene to prevent contracting COVID-19”). A higher total score signifies higher confidence. Internal reliability was satisfactory (Cronbach’s alpha = 0.89).
All the newly developed scales (i.e., general COVID-19 concerns and cancer-related COVID-19 concerns, risk perception, and perceived confidence in healthcare system) in the questionnaire were reviewed first by two cancer healthcare professionals and piloted with four patients and caregivers to obtain feedback on the relevance and items comprehensibility.
Statistical Analyses
Descriptive analyses of study variables are presented in means ± standard deviations (SD) for continuous data, and frequencies and percentages for categorical data. Comparisons between patients and their caregivers were undertaken using paired t-tests. To examine the associations between the study outcome (i.e., anxiety) and sociodemographic clinical or psychological variables and to identify additional covariates for the APIM models, bivariate correlations and one-way ANOVA analyses were used. The descriptive and subsequent bivariate analyses were conducted on SPSS (version 25) [30].
To examine the degree of interdependence in the patient-caregiver dyads, the Actor-Partner Interdependence Model (APIM) analytical method was employed [31]. Anxiety was the outcome of interest in all APIM models. Actor and partner effects of the four psychological variables ((i) general COVID-19 concerns, (ii) cancer concerns, (iii) risk perception, and (iv) perceived confidence) were modelled using APIM models with anxiety as the outcome. Sociodemographic and clinical variables were added as covariates in the models if significantly associated with anxiety. A composite APIM model that combined the partner or actor effects in the individual APIM models was then modelled. The composite model will be able to tease apart the unique associations with anxiety, over and above the other factors [32]. Model fit coefficients and standardized coefficients for all models were noted. As sensitivity analyses, APIM models were rerun on the subset of cohabiting dyads, and on spousal dyads vs non-spousal dyads (i.e., child-patient, parent-patient, etc.). All the aforementioned APIM models were conducted in MPlus [33].
To explore the indirect mediating effects between patient’s and caregiver’s own psychological responses towards COVID-19 on their partner’s anxiety [34], mediation analyses were also conducted by adding the variables into individual mediation pathway models with partners’ anxiety as the outcome. The significance of the indirect effects was analyzed using bootstrapping procedures. Unstandardized indirect effects were processed for 5000 bootstrapped samples, and the 95% confidence interval was computed by determining the indirect effects at the upper and lower limits. The mediation analyses were conducted on PROCESS macro in SPSS [35].
Results
There were N = 352 participants included in this study (patient-caregiver dyads, N = 176), of which 125 (71.0%) dyads were cohabiting. The majority of respondents were female (patients: 57.8% [n = 100]; caregivers: 60.9% [n = 103]) and of Chinese ethnicity (patients: 74.7% [n = 127]; caregivers: 74.1% [n = 126]). Spouses made up 43.2% (n = 73) of the caregivers, while 36.1% (n = 61) were children and 20.7% (n = 35) were parents, siblings, or other relationships. Both groups reported high rates of precautionary behaviors to reduce risks of infection, i.e., wearing masks, hygiene, and reduced social contact (see Table 1).
Table 1.
Characteristics of participants
| Patients (N = 176) | Caregivers (N = 176) | p | ||||
|---|---|---|---|---|---|---|
| Age, M ± SD | 61.5 ± 12.8 | 48.6 ± 14.4 | < 0.01 | |||
| Gender, N (%) | ||||||
| Male | 73 (42.2) | 66 (39.1) | < 0.01 | |||
| Female | 100 (57.8) | 103 (60.9) | ||||
| Ethnicity, N (%) | ||||||
| Chinese | 127 (74.7) | 126 (74.1) | < 0.01 | |||
| Malay | 24 (14.1) | 26 (15.3) | ||||
| Indian | 19 (11.2) | 17 (10.0) | ||||
| Other | - | 1 (0.6) | ||||
| Employment, N (%) | ||||||
| Part time | 13 (7.5) | 15 (8.6) | 0.75 | |||
| Full time | 45 (25.9) | 95 (54.3) | ||||
| Not employed | 116 (66.7) | 65 (37.1) | ||||
| Personal income level, N (%) | ||||||
| < $2500 | 67 (66.3) | 55 (42.0) | 0.98 | |||
| $2500–$5000 | 17 (16.8) | 43 (32.8) | ||||
| $5000–$7500 | 9 (8.9) | 15 (11.5) | ||||
| > $7500 | 8 (7.9) | 18 (13.7) | ||||
| Education, N (%) | ||||||
| Primary | 33 (18.9) | 9 (5.1) | 0.03 | |||
| < Secondary | 80 (45.7) | 53 (30.3) | ||||
| Post-secondary | 24 (13.7) | 48 (27.4) | ||||
| Graduate/post-graduate | 32 (18.3) | 63 (36.0) | ||||
| Others | 6 (3.4) | 2 (1.1) | ||||
| Marital status, N (%) | ||||||
| Single | 17 (9.9) | 46 (26.3) | < 0.01 | |||
| Married | 127 (73.8) | 119 (68.0) | ||||
| Divorced | 10 (5.8) | 5 (2.9) | ||||
| Widowed | 18 (10.5) | 5 (2.9) | ||||
| Cancer stage, N (%) | ||||||
| 1 | 6 (5.7) | |||||
| 2 | 20 (18.9) | |||||
| 3 | 32 (30.2) | |||||
| 4 | 48 (45.3) | |||||
| On active treatment, N (%) | 122 (74.5) | |||||
| Relationship to the patient, N (%) | ||||||
| Spouse | 73 (43.2) | |||||
| Child | 61 (36.1) | |||||
| Others | 35 (20.7) | |||||
| Precautionary behaviors takena | ||||||
| Keeping away from crowded places | 163 (95.9) | 171 (98.3) | 0.21 | |||
| Minimizing social contacts and visits | 157 (92.4) | 162 (93.1) | 0.82 | |||
| Avoid non-essential contact with healthcare workers | 86 (50.9) | 91 (52.6) | 0.68 | |||
| Practice better hygiene | 154 (90.6) | 163 (93.7) | 0.25 | |||
| Stay at home | 158 (92.9) | 151 (86.8) | 0.04 | |||
| Wear masks | 152 (89.9) | 160 (92.5) | 0.40 | |||
| Daily temperature monitoring | 100 (58.8) | 98 (56.3) | 0.71 | |||
| Seek medical advice with onset of symptoms | 122 (71.8) | 116 (66.7) | 0.23 | |||
| Take vitamin and supplements to boost immunity | 74 (43.5) | 80 (46.0) | 0.53 | |||
| Measure | Range | Patients (N = 176) | Caregivers (N = 176) | p | ||
|---|---|---|---|---|---|---|
| GAD-7 score | 0–21 | 6.54 ± 6.92 | 5.02 ± 5.50 | 0.01 | ||
| GAD-7 cutoff, N (%) | ||||||
| Presence of anxiety | 47 (26.7) | 32 (18.2) | < 0.01 | |||
| No anxiety | 119 (67.6) | 141 (80.1) | ||||
| General COVID-19 concerns | 1–5 | 3.36 ± 1.11 | 3.56 ± 0.93 | 0.99 | ||
| Cancer-related COVID-19 concerns | 1–5 | 3.44 ± 1.17 | 3.62 ± 0.97 | 0.07 | ||
| Risk perception | 0–100 | 40.70 ± 17.37 | 37.11 ± 14.63 | 0.02 | ||
| Perceived confidence in healthcare system | 1–10 | 7.65 ± 1.62 | 7.60 ± 1.41 | 0.60 | ||
aPrecautionary measures taken are not mutually exclusive. Participants can report conducting more than one precautionary behavior
Pairwise comparisons indicated that patients reported significantly higher risk perceptions and anxiety symptoms than their caregivers (p = 0.02 and p = 0.01 respectively). None of the other psychological variables, i.e., “general COVID-19 concerns” and “cancer-related COVID-19 concerns,” perceived confidence in healthcare system, differed between the patients and caregivers. A greater proportion of patients met the cutoff for anxiety caseness (GAD-7 ≥ 10) (26.7%) relative to the caregivers (18.2%; p < 0.01). Significant bivariate correlations were noted for dyads’ anxiety, general COVID-19 concerns, cancer-related concerns, and risk perceptions (rs = 0.24–0.30, p < 0.01). There were also significant correlations between patients’ and caregivers’ own psychological variables with their own anxiety, i.e., patients’ own COVID-19, cancer concerns, and risk perception with patients’ own anxiety (rs = 0.23–0.55, p < 0.01), and caregivers’ own COVID-19, cancer-related COVID-19 concerns, and risk perceptions with own anxiety (rs = 0.39–0.46, p < 0.01). Perceived confidence in healthcare was not associated with own or partner’s anxiety, hence not included in the subsequent APIM models. Among the sociodemographic and clinical variables, only patient’s gender was significantly associated with own anxiety, i.e., female patients reported significantly higher anxiety relative to male patients (F(1,161) = 9.52, p < 0.01); hence, it was included as a between-dyads covariate in the subsequent APIM, and mediation analyses.
APIM Analyses
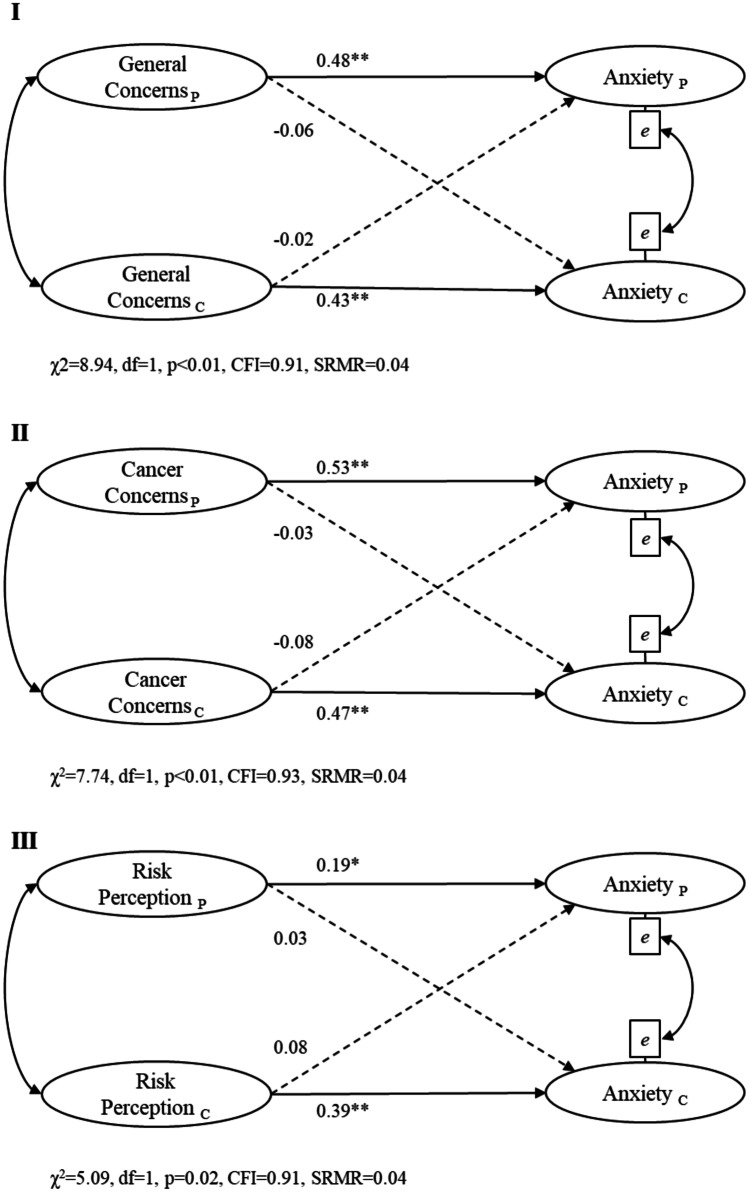
Guided by univariate analyses, three separate APIM models were tested: (a) general COVID-19 concerns on own/partner anxiety, (b) cancer-related COVID-19 concerns on anxiety, and (c) risk perception on own/partner anxiety. These indicated only significant actor effects for all three psychological parameters on own anxiety for both patient (βs = 0.19 to 0.53, ps < 0.01) and caregiver (βs = 0.39 to 0.47, ps < 0.01) (see Fig. 1). None of the partner effects was significant in the APIM models.
Fig. 1.
Actor-Partner Interdependence Model analyses. Notes: Gender of patient was added as a between-dyads covariate. Solid lines signify actor effects while dotted lines signify partner effects. Standardized path coefficients are reported. No significant partner effect observed. *p < 0.05, **p < 0.01
We then fitted a composite APIM model by including the three psychological variables (i.e., simultaneously incorporating all models in Fig. 1 in the same analysis) to explore the unique dyadic effects on own/partners’ anxiety. The composite model showed significant actor effects of cancer-related COVID-19 concerns on anxiety in both the patients (β = 0.35, p < 0.01) and caregivers (β = 0.28, p < 0.01). The actor effects for risk perception on anxiety were only significant for the caregivers (β = 0.23, p < 0.01). There were no significant partner effects. The composite APIM model exhibited adequate overall fit (CFI = 0.94, RMSEA = 0.07, SRMR = 0.03).
In sensitivity analyses, we re-estimated all APIM models (individual and composite) on the subset of cohabitating dyads (N = 125), i.e., excluding the 51 non-cohabiting dyads. Comparisons of estimates in these APIM models with those based on the full sample indicated comparable patterns of effects, i.e., only the actor effects were significant, whereas none of the partner effects was significant in the APIM for cohabiting dyads only.
The dyads were also grouped by spousal vs non-spousal dyads for comparison of effects and analyses repeated. For general COVID-19 concerns and cancer-related concerns, the resulting patterns were the same for both spousal and non-spousal dyads (i.e., significant actor effects only). For perceived confidence, a significant actor effect was observed (p = 0.03) for non-spousal caregivers’ confidence on their own anxiety rating, while no significant actor or partner effects for spousal dyads were observed. Finally, for risk perception, only the significant actor effects of caregivers’ risk perception (p < 0.05) on their own anxiety ratings were observed for both spousal and non-spousal dyads.
For the composite model, there was only a significant actor effect from patient’s cancer-related concern to their self-rating of anxiety levels in the non-spousal group, whereas there was only a significant actor effect of caregivers’ own concern to their self-rating on anxiety levels for spousal group.
Mediation Pathway Analyses
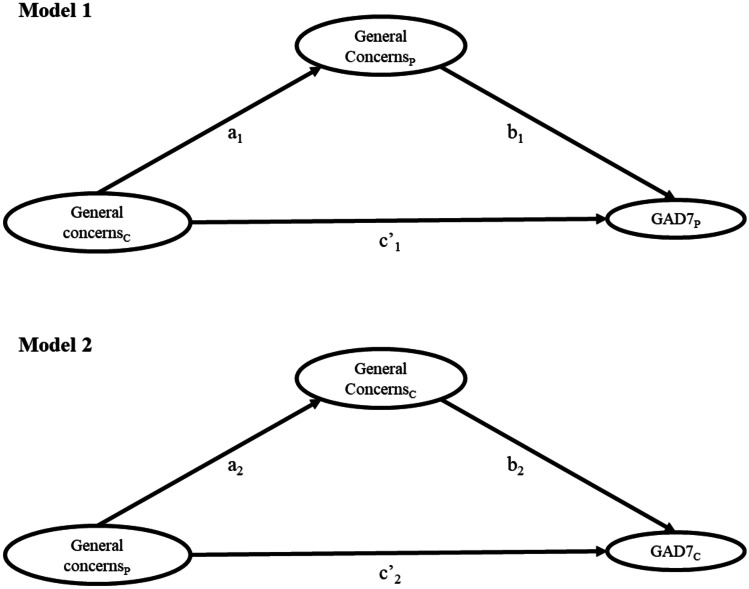
To explore indirect effects (i.e., own concerns (independent variable) influencing partner’s anxiety (dependent variable) via partners’ concerns (i.e., mediator)), mediation analyses were performed. The following variables were tested: (i) “general COVID-19 concerns,” (ii) “cancer-related COVID-19 concerns,” and (iii) “risk perception” in a total of six mediation models (see Fig. 2 for the pathways). The analyses indicated significant indirect effects in all six models. Caregiver’s psychological variables had significant indirect effects on patient’s anxiety through the following pathways: (i) caregiver’s general COVID-19 concerns had a statistically significant indirect effect on the patient’s anxiety through the patient’s general COVID-19 concerns (coefficient = 1.08, 95% CI [0.39, 1.79]); (ii) caregiver’s cancer-related COVID-19 concerns had an indirect effect on patient’s anxiety through the patient’s cancer-related COVID-19 concerns (coefficient = 1.07, 95% CI [0.44, 1.81]); (iii) the caregiver’s risk perception also had a small yet significant indirect effect on the patient’s anxiety through the patient’s own risk perception (coefficient = 0.02, 95% CI [0.002, 0.05]).
Fig. 2.
Mediation pathway analyses to test for indirect effects. Notes: Gender of patient was added as covariate. Models 1 and 2 are shown for illustration. Models 3 and 4 were run with cancer-related concerns as predictor and mediator, while models 5 and 6 were run with risk perception as predictor and mediator. The effect sizes are reported in Table 2
Similarly, the patient’s psychological variables had significant indirect effects on their caregiver’s anxiety through the following pathways: (i) the patient’s general COVID-19 concerns had a statistically significant indirect effect on their caregiver’s anxiety through the caregiver’s own general COVID-19 concerns (coefficient = 0.62, 95% CI [0.23, 1.08]); (ii) patient’s cancer-related COVID-19 concerns had an indirect effect on the caregiver’s anxiety through the caregiver’s own cancer-related COVID-19 concerns (coefficient = 0.58, 95% CI [0.23, 0.97]); and finally (iii) the patient’s risk perception also had an indirect but small effect on the caregiver’s anxiety through the caregiver’s own risk perception (coefficient = 0.02, 95% CI [0.006, 0.06]). Results in the mediation pathway analyses are tabulated in Table 2.
Table 2.
Mediation effect sizes for each model
| Models | Effects | ab (indirect effect) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| a − | b | c′ | coeff | 95% CI | |||||
| coeff | p | coeff | p | coeff | p | LL | UL | ||
| 1 | 0.34 | < 0.001 | 3.19 | < 0.001 | − 0.04 | 0.95 | 1.08 | 0.39 | 1.79 |
| 2 | 0.24 | < 0.001 | 2.61 | < 0.001 | − 0.35 | 0.34 | 0.62 | 0.23 | 1.08 |
| 3 | 0.32 | < 0.001 | 3.33 | < 0.001 | − 0.59 | 0.22 | 1.07 | 0.44 | 1.81 |
| 4 | 0.22 | < 0.001 | 2.62 | < 0.001 | − 0.10 | 0.76 | 0.58 | 0.24 | 0.97 |
| 5 | 0.29 | < 0.01 | 0.07 | 0.02 | 0.04 | 0.29 | 0.02 | 0.002 | 0.05 |
| 6 | 0.19 | < 0.01 | 0.15 | < 0.001 | 0.008 | 0.73 | 0.03 | 0.006 | 0.06 |
The models in this table correspond to the models in Fig. 2 (i.e., model 1 is the model with paths a1, b1, and c′1). The effects shown are unstandardized coefficients. Gender of the patient was added as covariate
Directional specificity was assessed using alternative models with reversed directions of the arrows in the APIM models (e.g., anxiety to general COVID-19 concerns) and the mediation pathways (e.g., reversing the paths a1). None of the reversed APIM models or mediation models rendered significant coefficients.
Discussion
With public health systems around the globe springing into action to reduce the impact and spread of COVID-19, the psychological impact of the pandemic on vulnerable populations was less of a priority especially in its early phases. The goals of this study were to document the magnitude and interdependence of symptoms of distress in dyads of patients with cancer and their caregivers, and their associations with cancer and COVID-19 concerns so as to guide service responsivity to their emergent needs.
Study findings indicated slightly elevated symptoms of anxiety relative to pre-pandemic levels in patients with cancer [36–38] whereas levels of anxiety in caregivers were comparable or even lower to those pre-pandemic [39, 40]. Although increased anxiety in response to threat of pandemic is common and to some degree a normative reaction to a novel threat, it may become problematic when it persists or when compounded by the stressors and mental health burden that accompany cancer diagnosis and treatment [41]. The emotional impact of COVID-19 was more pronounced in patients relative to their caregivers. Patients had higher rates of anxiety, with 26.7% meeting criteria for Generalized Anxiety Disorder compared to 18.2% of the caregivers.
This may be related to the policies and mandates introduced to reduce transmission, such as deferral of non-essential treatments (e.g., diagnostic tests, psychosocial support programs), and safe management procedures (e.g., restricted access to visitors) that brought about changes in patient journey [42]. Many settings have seen sharp declines in the number of cancer-related patient encounters as a result of the COVID-19 measures, with treatment delays increasing mortality risk [43]. While there was no delay for active cancer treatment in Singapore (and our study participants), diagnostic tests were deferred, and the new workflows implemented in clinics may have intensified the stress and anxiety related to cancer. Related to this, the temporary suspension of psycho-oncology services may have left patients grappling with the psychological challenges of cancer without the direct formal structures and support they relied on prior to the COVID-19 pandemic. Even though patients reported that they are already engaging in protective behaviors such as social distancing and wearing of masks, they still reported significantly higher risk perceptions relative to caregivers, reflecting high awareness of the implications of being immunocompromised and of older age.
The APIM analyses to identify predictors and dyadic effects indicated only actor effects for all models. The key drivers of one’s own anxiety were their own concerns about the impact of COVID-19 on cancer (“cancer-related COVID-19 concerns”) for both patients and caregivers. General concerns about COVID-19 and risk perceptions, although significant in the individual APIMs, were no longer significant in the composite APIM model. The caregivers’ own risk perceptions were significantly associated with own anxiety in the multivariable APIM, but this effect was very small, in contrast to large effects shown for own cancer-specific COVID-19 concerns. Our prior qualitative work also noted that cancer treatment amidst the pandemic was the utmost priority for both patients with cancer and caregivers [23]. The certainty of cancer diagnosis, recognition for timely treatment and/or risks related to treatment delay/undertreatment, and experience of concrete symptoms related to cancer (e.g., pain) could have overshadowed the uncertainties surrounding COVID-19 [44]. The certainty of cancer threat, as compared to the uncertainty of COVID-19, could thus compel cancer patients and their caregivers to devote their focus on the cancer rather than be concerned about the general threat of the pandemic.
In the APIM analyses, we found no evidence of direct interdependence in the dyads. None of the APIM models showed significant partner effects, contrary to previous studies of patient-caregivers dyads such as in breast and head and neck cancers [45, 46]. Substantial uncertainty surrounding the nature, prognosis, and management inevitably exists with new health crises such as COVID-19. Given the stressful experience of cancer, it is plausible that open and explicit communication is discouraged among caregiver-patient dyads in this study so as not to cause additional burden on top of the existing stress of cancer. In addition, there may be a generally higher level of trust placed on government communication channels as the primary source of information on pandemic [47], which could lead to limited discussions between patient and caregivers.
Despite no evidence of direct interdependence in APIM, mediation analyses revealed significant indirect effects between patient-caregiver dyads, with ones’ perceptions about risk, COVID-19 concerns, or impact of COVID-19 on cancer influencing the partners’ anxiety by affecting partners’ own perceptions of risk, COVID-19, or impact of COVID-19 on cancer. The vast majority of dyadic studies thus far have focused mostly on spousal dyads [46, 48], and were conducted in non-Asian settings. In our study, we have recruited a large and fairly equal proportion of spouse and children caregivers (mostly Chinese) to better represent the caregivers’ landscape in the local context. In Singapore, it is common for parents in ill-health to reside with their adult children [49]. Caregiving responsibilities are often shared across family members (spouse and children) in the Asian context. As such, communication patterns and influences among patients and their caregiver(s) may be more complex and nuanced compared to other settings where caregiving may be only between spouses or one child. The norms and dynamics in child-patient dyads may also be different to those of spousal dyads in Asian cultures [50]. Offspring (adult) caregivers may be more filtered in sharing their perspectives and defer to parents out of respect. They may also purposefully put a brave front to emotionally shield the care recipients.
Sensitivity analyses comparing spousal and non-spousal dyads and cohabiting vs non-cohabiting dyads showed no significant partner effects while most of the actor effects persisted. This suggests inherent differences between the population in this study with studies conducted elsewhere. Asian patients in general have been shown to be more reluctant about emotional disclosure and less likely to seek social support from their friends and family [51]. Hence, contagion may be less likely. More in-depth studies on the indirect influences through understanding of family dynamics and social support are required.
Study Limitations
Our study should be interpreted in light of its limitations. Data is cross-sectional; hence, no causal inferences can be established. Caution is needed to interpret any mediation effects and their corresponding directions. Although reverse relationships were explored and not supported in the models, longitudinal designs are needed to map course and directionality of the effects. Furthermore, dyadic communication and relationship quality were not measured, but can be important moderators of the relationships [9]. Future studies of patient-caregiver dyads could consider assessing the relationship and communication perceptions.
Data were collected in spring 2020 (March to June) and study findings may not be generalizable to other countries or in later course of pandemic (e.g., resurge or spike in infections in second or third waves). The modest study sample (N = 176 dyads) also limits conclusion(s) to be drawn and highlights need for replication. More longitudinal work is needed to elucidate the long-term impact of the pandemic on patient-caregiver dyads in the context of cancer. More information about the time since the cancer diagnosis would help provide more context into the analyses. It is thus crucial that we systematically collect and analyze, on a larger scale, the data of patients and caregivers’ first-hand experiences of COVID-19 (and future infectious outbreaks or crises), and the associated measures, as well as service utilization, to inform longer-term decisions and optimization/refinement of services during infectious outbreaks.
Clinical Implications
The ongoing threat of contracting COVID-19 represents a considerable mental burden in cancer patients. Cancer patients with elevated anxiety and depression symptoms are at significantly greater risks of suicide and poor self-care and medication adherence [52, 53]. To reduce their vulnerability to the negative impacts of the pandemic, we need to proactively monitor symptoms as the pandemic prolong. As one’s concerns about pandemic may affect partner’s concerns and in turn partner’s anxiety, cancer care consultations should focus on dyads of patients and caregivers despite the challenges of pandemic-related containment and safe management measures. It is important to recognize that there are specific concerns related to cancer in the pandemic that can fuel anxiety, and hence, targeted efforts to actively elicit these concerns are necessary. Healthcare messages and communication tailored to the needs of patients and caregivers especially in face of pandemic uncertainty can boost confidence and trust and support emotional resilience.
Preventive measures such as the restrictions of house visits and the one-visitor policy in healthcare settings present a significant barrier to engagement in this regard. These policies may disempower family members from being collectively involved in the decision-making process for the patient. With Singapore and other countries moving towards endemicity of the disease, resources should be put in for innovations in alternative models of healthcare communication, such as in telehealth/e-health, which can better increase accessibility of holistic psycho-oncology care. Telecommunication technologies (e.g., video conferencing) have been widely adopted in multiple sectors including healthcare. Video conferencing has enabled healthcare providers to involve the patient and all other caregivers during the consultation. Shared decision-making with the patient and all caregivers, and the multidisciplinary care team can be achieved without all being in the same location, thus reducing infection risks. Through technology, education about cancer care and COVID-19 precautionary measures can be better delivered. Ongoing trials for telehealth oncology care have shown some preliminary success, but further research is needed [54]. The adoption rate is dependent on easy and equitable access to technology as well as digital health literacy skills support for both healthcare providers and users.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This study is supported by the National Research Foundation Singapore’s National Medical Research Council Clinician Scientist Award (NMRC/CSA-INV/0017/2017) and administered by the Singapore Ministry of Health’s National Medical Research Council. In addition, this research is supported by the National Cancer Centre Cancer Fund.
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Joanne Ngeow is in an honorarium consulting or advisory role and has research fundings with AstraZeneca.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zack Zhong Sheng Goh, Email: zack_zs_goh@whc.sg.
Moon-ho R. Ho, Email: ringo_ho@ntu.edu.sg
Kennedy Yao Yi Ng, Email: kennedy.ng.y.y@nccs.com.sg.
Jace Ming Xuan Chia, Email: jace.chiamx@ntu.edu.sg.
Nur Diana Binte Ishak, Email: nur.diana.ishak@nccs.com.sg.
Than Than Shwe, Email: ma.than.t.s@nccs.com.sg.
Zi Yang Chua, Email: chua.zi.yang@nccs.com.sg.
Joanne Yuen Yie Ngeow, Email: joanne.ngeow.y.y@singhealth.com.sg.
Konstadina Griva, Email: konstadina.griva@ntu.edu.sg.
References
- 1.World Health Organisation. COVID-19 significantly impacts health services for noncommunicable diseases [Internet]. 2020. [cited 21 Nov 2021]. Available from: https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases.
- 2.Yadav UN, Rayamajhee B, Mistry SK, Parsekar SS, Mishra SK. A syndemic perspective on the management of non-communicable diseases amid the COVID-19 pandemic in low- and middle-income countries. Front Public Heal. 2020;8. [DOI] [PMC free article] [PubMed]
- 3.Edge R, Meyers J, Tiernan G, Li Z, Schiavuzzi A, Chan P, et al. Cancer care disruption and reorganisation during the COVID-19 pandemic in Australia: A patient, carer and healthcare worker perspective. PLoS One [Internet]. [cited 2021 Nov 21] 2021;16(9):e0257420. 10.1371/journal.pone.0257420. [DOI] [PMC free article] [PubMed]
- 4.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 Transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6:1108–10. [DOI] [PMC free article] [PubMed]
- 5.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020. [DOI] [PMC free article] [PubMed]
- 6.Massicotte V, Ivers H, Savard J. Covid-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr Oncol. 2021;28(1):294–300. doi: 10.3390/curroncol28010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leader A, Selvan P, Capparella L, Cammy R, Palidora J, Shimada A, et al. Abstract S11–01: Assessing the impact of the COVID-19 pandemic on cancer patients, survivors, and caregivers. Clin Cancer Res [Internet]. 2020;26(18 Supplement):S11–01-S11–01. Available from: http://clincancerres.aacrjournals.org/content/26/18_Supplement/S11-01.abstract.
- 8.Fletcher BS, Miaskowski C, Given B, Schumacher K. The cancer family caregiving experience: An updated and expanded conceptual model. Eur J Oncol Nurs. 2012;16:387–98. [DOI] [PMC free article] [PubMed]
- 9.Li Q, Loke AY. A literature review on the mutual impact of the spousal caregiver–cancer patients dyads: ‘Communication’, ‘reciprocal influence’, and ‘caregiver–patient congruence’. Eur J Oncol Nurs. 2014;18(1):58–65. doi: 10.1016/j.ejon.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Streck BP, Wardell DW, LoBiondo-Wood G, Beauchamp JES. Interdependence of physical and psychological morbidity among patients with cancer and family caregivers: Review of the literature. Psycho Oncol. 2020;29:974–89. [DOI] [PubMed]
- 11.You J, Lu Q. Sources of social support and adjustment among Chinese cancer survivors: gender and age differences. Support Care Cancer [Internet]. [cited 2021 Nov 5] 2013;22(3):697–704. Available from: 10.1007/s00520-013-2024-z. [DOI] [PubMed]
- 12.Wittenberg E, James LP, Prosser LA. Spillover effects on caregivers’ and family members’ utility: a systematic review of the literature. PharmacoEconomics [Internet]. [cited 2022 Jun 21] 2019;37(4):475–99. Available from: 10.1007/s40273-019-00768-7. [DOI] [PubMed]
- 13.Nelson JA, O’Brien M, Blankson AN, Calkins SD, Keane SP. Family stress and parental responses to children’s negative emotions: tests of the spillover, crossover, and compensatory hypotheses. J Fam Psychol [Internet]. 2009 Oct [cited 2022 Jun 21];23(5):671. Available from: 10.1037/a0015977 [DOI] [PMC free article] [PubMed]
- 14.Ahorsu DK, Imani V, Lin CY, Timpka T, Broström A, Updegraff JA, et al. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int J Ment Health Addict. 2020. [DOI] [PMC free article] [PubMed]
- 15.Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum Dev [Internet]. [cited 2022 Jun 21] 2020;51(5):671–82. Available from: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed]
- 16.Pietromonaco PR, Overall NC. Applying relationship science to evaluate how the COVID-19 pandemic may impact couples’ relationships. Am Psychol. 2020. [DOI] [PubMed]
- 17.Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed S, Tan WLG, Chong YL. Surgical Response to COVID-19 Pandemic: A Singapore Perspective. J Am Coll Surg. 2020;230(6):1074–1077. doi: 10.1016/j.jamcollsurg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan WL, Ho P-YP, Yuen K-K. Social distancing and cancer care during the COVID-19 pandemic. BMJ Support Palliat Care [Internet]. [cited 2022 Jun 22] 2021. Available from: https://spcare.bmj.com/content/early/2021/08/24/bmjspcare-2020-002489. [DOI] [PubMed]
- 20.Sha Z, Chang K, Mi J, Liang Z, Hu L, Long F, et al. The impact of the COVID-19 pandemic on lung cancer patients. Ann Palliat Med [Internet]. cited 2022 Jun 22] 2020;9(5):3373378–3373378. Available from: https://apm.amegroups.com/article/view/52221/html. [DOI] [PubMed]
- 21.de Joode K, Dumoulin DW, Engelen V, Bloemendal HJ, Verheij M, van Laarhoven HWM, et al. Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients’ perspective. Eur J Cancer. 2020;1(136):132–139. doi: 10.1016/j.ejca.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng KYY, Zhou S, Tan SH, Ishak NDB, Goh ZZS, Chua ZY, et al. Understanding the Psychological Impact of COVID-19 Pandemic on Patients With Cancer, Their Caregivers, and Health Care Workers in Singapore. JCO Glob Oncol. 2020;6:1494–1509. doi: 10.1200/GO.20.00374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chia JMX, Goh ZZS, Chua ZY, Ng KYY, Ishak D, Fung SM, et al. Managing cancer in context of pandemic: A qualitative study to explore the emotional and behavioural responses of patients with cancer and their caregivers to COVID-19. BMJ Open. 2021;11(1). [DOI] [PMC free article] [PubMed]
- 24.Liao Q, Cowling BJ, Lam WWT, Ng DMW, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infect Dis. 2014;14(1). [DOI] [PMC free article] [PubMed]
- 25.Tiwari A, Chan S, Wong A, Tai J, Cheng K, Chan J, et al. Severe acute respiratory syndrome (SARS) in Hong Kong: Patients’ experiences. Nurs Outlook. 2003;51(5):212–219. doi: 10.1016/j.outlook.2003.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leung GM, Quah S, Ho L-M, Ho S-Y, Hedley AJ, Lee H-P, et al. A Tale of Two Cities: Community Psychobehavioral Surveillance and Related Impact on Outbreak Control in Hong Kong and Singapore During the Severe Acute Respiratory Syndrome Epidemic. Infect Control Hosp Epidemiol. 2004;25(12):1033–1041. doi: 10.1086/502340. [DOI] [PubMed] [Google Scholar]
- 27.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 28.Esser P, Hartung TJ, Friedrich M, Johansen C, Wittchen HU, Faller H, et al. The Generalized Anxiety Disorder Screener (GAD-7) and the anxiety module of the Hospital and Depression Scale (HADS-A) as screening tools for generalized anxiety disorder among cancer patients. Psychooncology. 2018. [DOI] [PubMed]
- 29.Yap CK, Wong MY, Lim KK. Illness Perception of Anxiety Patients in Primary Care in Singapore. Indian J Psychol Med. 2019;41(1):75–80. doi: 10.4103/IJPSYM.IJPSYM_101_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.IBM Corp. IBM SPSS Statistics for Windows. Version 25.0. Armonk, NY: IBM Corp. 2017.
- 31.Fitzpatrick J, Gareau A, Lafontaine M-F, Gaudreau P. How to Use the Actor-Partner Interdependence Model (APIM) To Estimate Different Dyadic Patterns in MPLUS: A Step-by-Step Tutorial. Quant Methods Psychol. 2016;12(1):74–86. doi: 10.20982/tqmp.12.1.p074. [DOI] [Google Scholar]
- 32.Humbad MN, Donnellan MB, Iacono WG, Burt SA. Externalizing Psychopathology and Marital Adjustment in Long-Term Marriages: Results from a Large Combined Sample of Married Couples. J Abnorm Psychol [Internet]. [cited 2022 Aug 2] 2010;119(1):151. Available from: 10.1037/a0017981 [DOI] [PMC free article] [PubMed]
- 33.Muthén LK, Muthén BO. Mplus user’s guide. [cited 2021 Oct 25] 2010. Available from: https://www.statmodel.com/html_ug.shtml.
- 34.Coutts JJ, Hayes AF, Jiang T. Easy statistical mediation analysis with distinguishable dyadic data. J Commun [Internet]. [cited 2022 Jun 22] 2019;69(6):612–49. Available from: https://academic-oup-com.libproxy1.nus.edu.sg/joc/article/69/6/612/5658499.
- 35.Hayes AF. The process macro for SPSS, SAS, and R [Internet]. 2019. Available from: https://processmacro.org/index.html.
- 36.Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: A systematic review and meta-analysis. Lancet Oncol. 2013;14(8):721–732. doi: 10.1016/S1470-2045(13)70244-4. [DOI] [PubMed] [Google Scholar]
- 37.Naser AY, Hameed AN, Mustafa N, Alwafi H, Dahmash EZ, Alyami HS, et al. Depression and Anxiety in Patients With Cancer: A Cross-Sectional Study. Front Psychol. 2021;15(12):1067. doi: 10.3389/fpsyg.2021.585534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Endo M, Matsui K, Akaho R, Mitsui K, Yan Y, Imai Y, et al. Depressive and anxiety symptoms among Japanese cancer survivors: Japan cancer survivorship research project. BMC Cancer [Internet]. [cited 2022 Jun 22] 2022;22(1). Available from: 10.1186/s12885-022-09215-x [DOI] [PMC free article] [PubMed]
- 39.Geng H mei, Chuang D mei, Yang F, Yang Y, Liu W min, Liu L hui, et al. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine (Baltimore) [Internet]. 2018 Sep 1 [cited 2022 Jun 22];97(39). Available from: 10.1097/MD.0000000000011863 [DOI] [PMC free article] [PubMed]
- 40.Li Q, Lin Y, Xu Y, Zhou H. The impact of depression and anxiety on quality of life in Chinese cancer patient-family caregiver dyads, a cross-sectional study. Heal Qual Life Outcomes [Internet]. [cited 2022 Jun 22] 2018;16(1):1–15. Available from: 10.1186/s12955-018-1051-3. [DOI] [PMC free article] [PubMed]
- 41.Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25(7):1487–1499. doi: 10.1038/s41380-019-0595-x. [DOI] [PubMed] [Google Scholar]
- 42.Chen-See S. Disruption of cancer care in Canada during COVID-19. Lancet Oncol [Internet]. 2020;21(8):e374. Available from: 10.1016/S1470-2045(20)30397-1. [DOI] [PMC free article] [PubMed]
- 43.Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi: 10.1136/bmj.m4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim TK. The facts, fallacies and uncertainties about Coronavirus Disease 2019 (COVID-19). Ann Acad Med. 2020. Singapore. [PubMed]
- 45.Segrin C, Badger TA, Sikorskii A, Crane TE, Pace TWW. A dyadic analysis of stress processes in Latinas with breast cancer and their family caregivers. Psychooncology. 2018;27(3):838–846. doi: 10.1002/pon.4580. [DOI] [PubMed] [Google Scholar]
- 46.Badr H, Herbert K, Bonnen MD, Asper JA, Wagner T. Dyadic coping in patients undergoing radiotherapy for head and neck cancer and their spouses. Front Psychol. 2018;9(OCT). [DOI] [PMC free article] [PubMed]
- 47.Lim VW, Lim RL, Tan YR, Soh ASE, Tan MX, Othman NB, et al. Government trust, perceptions of covid-19 and behaviour change: Cohort surveys, singapore. Bull World Health Organ. 2021;99(2):92–101. doi: 10.2471/BLT.20.269142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee MS, Kim K, Lim C, Kim JS. Posttraumatic growth in breast cancer survivors and their husbands based on the actor-partner interdependence model. Psychooncology. 2017;26(10):1586–1592. doi: 10.1002/pon.4343. [DOI] [PubMed] [Google Scholar]
- 49.Chu CYC, Xie Y, Yu RR. Coresidence with elderly parents: A comparative study of Southeast China and Taiwan. J Marriage Fam. 2011;73(1):120–135. doi: 10.1111/j.1741-3737.2010.00793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chong JA, Quah YL, Yang GM, Menon S, Krishna LKR. Patient and family involvement in decision making for management of cancer patients at a centre in Singapore. BMJ Support Palliat Care. 2015;5(4):420–426. doi: 10.1136/bmjspcare-2012-000323. [DOI] [PubMed] [Google Scholar]
- 51.Kim HS, Sherman DK, Taylor SE. Culture and Social Support. Am Psychol. 2008;63(6):518–526. doi: 10.1037/0003-066X. [DOI] [PubMed] [Google Scholar]
- 52.Vartolomei L, Ferro M, Mirone V, Shariat SF, Vartolomei MD. Systematic Review: Depression and Anxiety Prevalence in Bladder Cancer Patients. Bl Cancer. 2018;4(3):319–326. doi: 10.3233/BLC-180181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Klaassen Z, Jen RP, Dibianco JM, Reinstatler L, Li Q, Madi R, et al. Factors associated with suicide in patients with genitourinary malignancies. Cancer. 2015;121(11):1864–1872. doi: 10.1002/cncr.29274. [DOI] [PubMed] [Google Scholar]
- 54.Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID-19 pandemic: Scoping review. J Med Internet Res. 2020;22(12). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.