PURPOSE
To estimate the prevalence of financial hardship among adult survivors of childhood cancer compared with siblings and identify sociodemographic, cancer diagnosis, and treatment correlates of hardship among survivors in the era after implementation of the Affordable Care Act.
METHODS
A total of 3,555 long-term (≥ 5 years) survivors of childhood cancer and 956 siblings who completed a survey administered in 2017-2019 were identified from the Childhood Cancer Survivor Study. Financial hardship was measured by 21 survey items derived from US national surveys that had been previously cognitively tested and fielded. Principal component analysis (PCA) identified domains of hardship. Multiple linear regression examined the association of standardized domain scores (ie, scores divided by standard deviation) with cancer and treatment history and sociodemographic characteristics among survivors.
RESULTS
Survivors were more likely than siblings to report hardship in ≥ 1 item (63.4% v 53.7%, P < .001). They were more likely to report being sent to debt collection (29.9% v 22.3%), problems paying medical bills (20.7% v 12.8%), foregoing needed medical care (14.1% v 7.8%), and worry/stress about paying their rent/mortgage (33.6% v 23.2%) or having enough money to buy nutritious meals (26.8% v 15.5%); all P < .001. Survivors reported greater hardship than siblings in all three domains identified by principal component analysis: behavioral hardship (mean standardized domain score 0.51 v 0.35), material hardship/financial sacrifices (0.64 v 0.46), and psychological hardship (0.69 v 0.44), all P < .001. Sociodemographic (eg, <college education, without private insurance) and treatment factors (eg, received ≥ 250 mg/m2 anthracycline chemotherapy, or chest radiation) were statistically significantly associated with increased hardship.
CONCLUSION
Survivors of childhood cancer were more likely to experience financial hardship than siblings. Correlates of hardship can inform survivorship care guidelines and intervention strategies.
BACKGROUND
Of the 500,000 US survivors of childhood cancer,1 most are at risk for, or have developed, physical, psychological or neurocognitive morbidities2,3 because of their cancer and its therapy. These morbidities may lead to financial hardship, which may exacerbate or cause physical and psychological harms.4
CONTEXT
Key Objective
To determine if adult survivors of childhood cancer are at elevated risk for financial hardship and to explore the domains of financial hardship experienced by survivors and their associations with survivor sociodemographic characteristics, cancer diagnosis, and treatment.
Knowledge Generated
We developed a questionnaire that assessed financial hardship in survivors and siblings and classified dimensions of hardship in three domains—behavioral hardship, material hardship/financial sacrifices, and psychological hardship. Across most of the 20 individual items assessed and all three of the domains, survivors were at elevated risk for hardship compared with their siblings. Both sociodemographic and treatment factors were associated with the risk for hardship among survivors.
Relevance (S. Bhatia)
-
Guidelines should be developed to screen for financial hardship in childhood cancer survivors. Intervention programs, such as financial navigators, should be developed and evaluated in this population.*
*Relevance section written by JCO Associate Editor Smita Bhatia, MD.
Survivors of adult cancers experience more financial hardship than adults without a cancer history,5-9 report higher out-of-pocket medical costs, and are more likely to be limited in the type or amount of work because of poor health and functional challenges.8,10,11 This may limit access to employment-based health insurance, the primary source of coverage for nonelderly adults. Work limitations and job lock can lead to lower income and asset accumulation and problems paying medical bills or purchasing necessities such as food, clothing, and housing.12-16 Financial hardship has been associated with poorer physical and mental health, reduced quality of life, and inferior survival after a cancer diagnosis.17-19
Less understood are the financial implications of surviving childhood cancer which is distinct from adult cancers because it can interrupt physical and psychological development and educational and vocational trajectories. The few studies conducted were before the implementation of the main provisions of Affordable Care Act (ACA) in 2014.20,21 In the St Jude Lifetime Cohort Study fielded between 2007 and 2015, over half of adult survivors of childhood cancer reported moderate or high levels of financial hardship which was associated with somatization, anxiety and depression, suicidal ideation, and lower quality of life.21 In a subset of the Childhood Cancer Survivor Study (CCSS) cohort surveyed in 2011-2012, about one quarter of survivors reported skipping or deferring care because of cost or difficulty paying medical bills.22 Survivors were more likely than siblings to borrow money because of medical expenses, worry about not getting needed care, and not fill prescriptions.23 Multiple provisions of the ACA, including expansion of Medicaid income eligibility to 138% of the federal poverty line in some states, establishment of marketplaces for individual purchase of insurance and income-based premium tax credits and cost-sharing subsidies, out-of-pocket caps for private coverage, and elimination of preexisting conditions exclusions, which previously allowed insurers to deny coverage to cancer survivors, may be especially beneficial for adult survivors of childhood cancer. However, the ACA became highly politicized, and numerous court cases and administrative changes created barriers to its full implementation, making comprehensive assessment of financial hardship among survivors of childhood cancer post-ACA especially critical.24 To address this research gap, the CCSS surveyed a large cohort of adult survivors of childhood cancer on a range of financial hardship measures.
METHODS
The design of the CCSS has been reported in detail elsewhere.25,26 The CCSS is a retrospective cohort study with longitudinal follow-up of 5-year survivors of cancer diagnosed before 21 years between 1970 and 1999. Institutional Review Boards at each of 31 participating sites approved the study, and participants provided informed consent. Between 2017 and 2019, the CCSS surveyed 17,460 survivors and 3,648 siblings enrolled in the cohort. A randomly selected subset of 5,488 survivors and 1,592 siblings were asked to respond to items that assessed broad measures of financial hardship specific to cancer survivors. These were developed from a US National Cancer Institute27 evidence summary and systematic review of published literature.28,29 Questions were derived from items that were previously cognitively tested and fielded from the National Health Interview Survey,14 the Medical Expenditure Panel Survey Experiences with Cancer,30 and the Behavioral Risk Factor Surveillance System.31 Survey design is described in detail in the Data Supplement (online only). This analysis used 21 items about difficulties paying medical expenses, debt/bankruptcy, financial barriers to receiving medical care, the impact of financial hardship on nonmedical spending, stress/worry about finances, and delays in care because of cost (Data Supplement). Survivors answered 21 items while siblings answered 20 items because a question about cancer follow-up care was not applicable.
The analysis was restricted to individuals age 26 years or older at the time of survey, the age at which young adults are no longer eligible for coverage under their parents' private health insurance plans post-ACA. Individuals with proxy respondents and those with non-US health insurance (including Canadian participants) were excluded (Fig 1).
FIG 1.
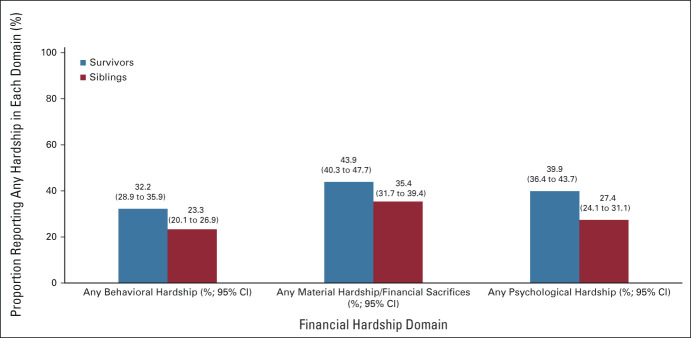
Proportion reporting any financial hardship in each domain among survivors versus siblings. P < .001 for each survivor versus sibling comparison. Comparisons adjusted for sex and age at questionnaire. GEE used to account for within-family correlation. GEE, generalized estimating equation.
We tabulated the demographic characteristics of survivors and siblings and the disease and treatment characteristics of survivors. The proportions of survivors and siblings who reported hardship for each item were compared using chi-square tests; bootstrap with resampling of families accounted for within-family correlation. An exploratory factor analysis was conducted to identify domains of financial hardship among survivors. All item responses were converted to binary outcomes as described in the Data Supplement. A polychoric correlation matrix of the items was calculated and used as the input for the factor analysis. Principal component analysis with promax rotation was used to extract factors. We retained items with factor loadings > 0.4 and assessed the reliability of each factor using the Kuder-Richardson formula 20 (KR-20), with KR-20 > 0.7 indicating acceptable reliability (Data Supplement).
Two scoring methods were used to analyze the status of each hardship domain: (1) a binary scoring for any affirmative response to the items in the domain and (2) an unweighted summated scoring method for the number of items having affirmative response in the domain. For the unweighted summated scoring method, standardized domain scores were calculated by adding the item responses and dividing by the standard deviation (SD) among survivors. Using this distribution-based approach, a difference between groups > 0.5 SD was considered moderate and a difference > 0.8 SD was considered large.32 After excluding the question regarding cancer follow-up care, standardized domain scores were compared between survivors and siblings using a generalized estimating equation with an identity link and Gaussian error to account for the potential within-family correlation, with adjustment for sex and age at survey completion. General linear models with backward variable selection were used to identify a domain-specific set of sociodemographic and cancer treatment variables that were statistically significantly associated with the binary scores for each domain among survivors. A final model for each domain was fit using the union of all domain-specific sets of selected sociodemographic and cancer treatment variables to facilitate comparing differential associations of these variables across domains of financial hardship.
All statistical analyses were conducted using SAS version 9.4; statistical tests were two-sided.
RESULTS
Of the 5,488 survivors and 1,592 siblings sent the financial hardship questions, 3,555 survivors and 956 siblings responded and were eligible for this analysis (Data Supplement). One hundred ninety-nine survivors were excluded because of proxy response, of whom 97 (48.7%) had been treated for a brain tumor. Survivors who responded were significantly more likely than nonrespondents to be female, non-Hispanic White, older at survey, ≥ college graduates, and married/living as married (P < .05). They were less likely to have received a stem-cell transplant and more likely to have received radiation (P < .05) but did not differ in terms of cancer diagnosis or receipt of alkylating or anthracycline agents (Data Supplement).
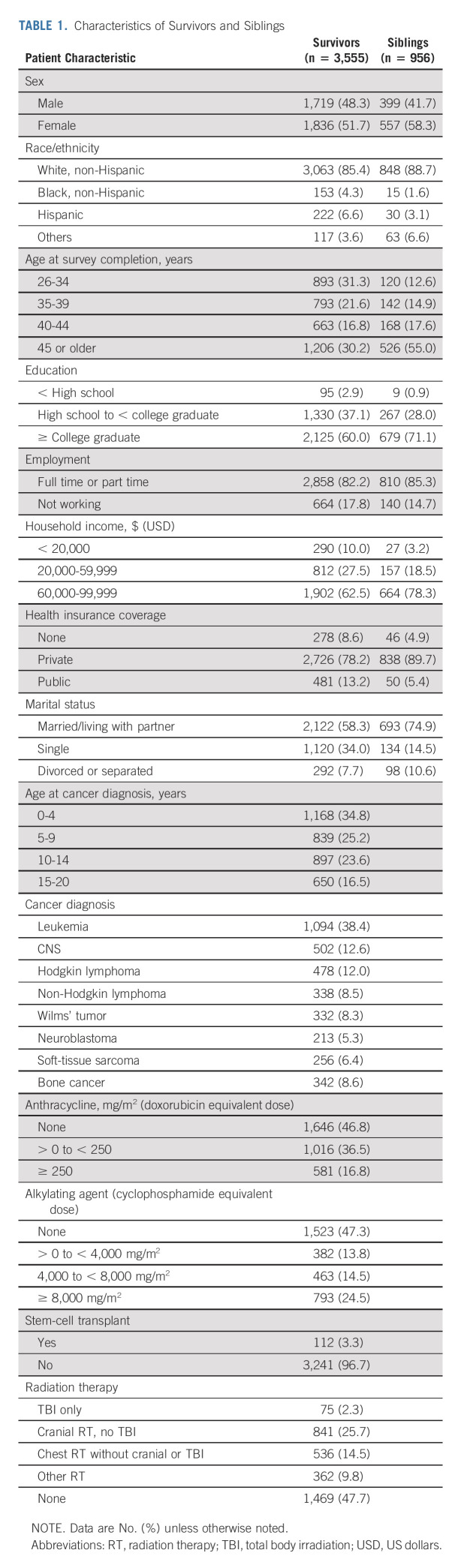
Table 1 describes the characteristics of the survivors and siblings. Survivors were at a median age of 8.5 years (interquartile range [IQR], 3.8-13.8) at diagnosis and 40.5 years (IQR 35.0-47.5) at survey. Siblings were at a median age of 46.7 years (IQR, 39.3-53.8) at survey. Female survivors were more likely than males to have higher educational attainment and be married and less likely to have received alkylating agents or radiation therapy (Data Supplement). Of the 3,555 survivors included in the study, only 213 (6%) had a sibling in the sibling respondent group.
TABLE 1.
Characteristics of Survivors and Siblings
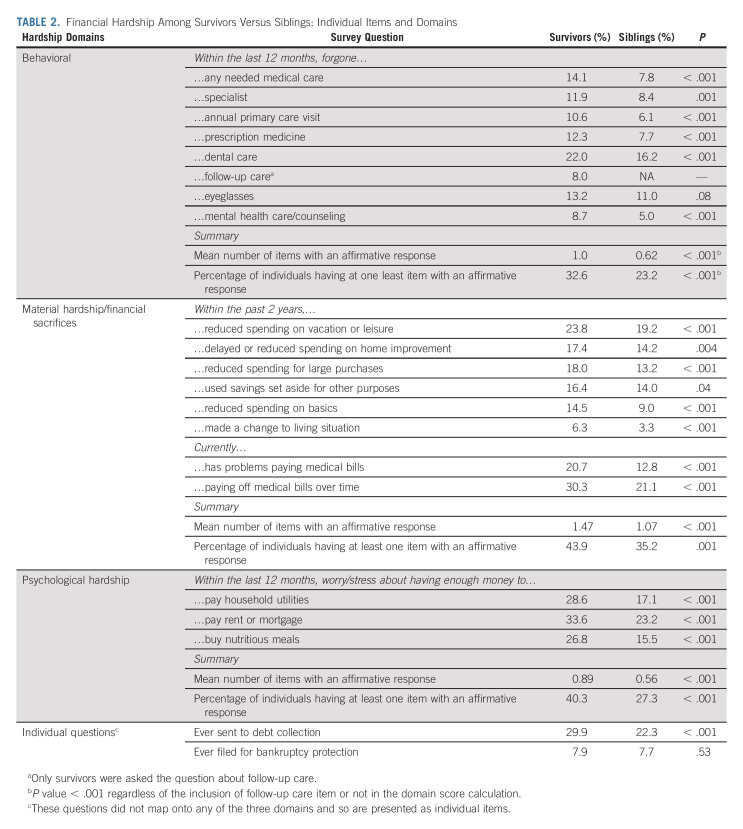
Survivors were more likely than siblings to report hardship in ≥ 1 of the 20 items (63.4% v 53.7%, P < .001). Survivors identified hardship in a median of two items (range, 0-20) while siblings reported hardship in a median of one item (range, 0-19, P = .01); (mean 3.67 v 2.55; P < .001). Survivors were statistically significantly more likely than siblings to report being sent to debt collection, problems paying medical bills, foregoing any needed medical care, worry/stress about paying rent or mortgage, or having enough money to buy nutritious meals (Table 2).
TABLE 2.
Financial Hardship Among Survivors Versus Siblings: Individual Items and Domains
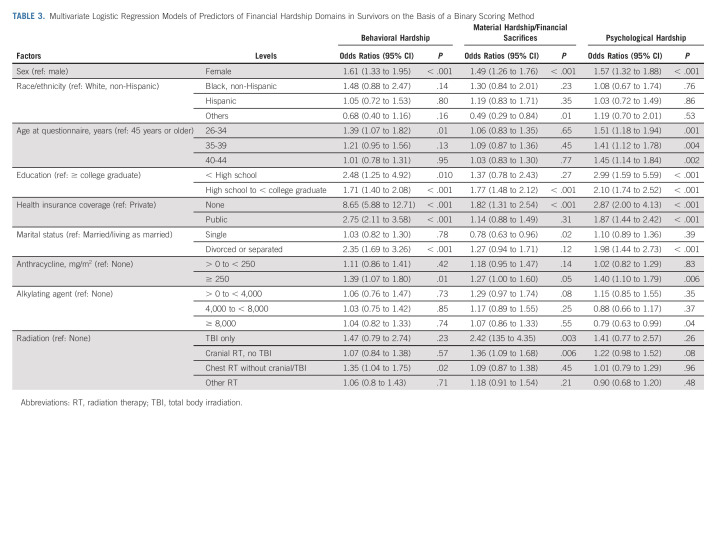
Of the 21 items, 19 mapped onto three hardship domains. These were labeled behavioral hardship (eight items), material hardship/financial sacrifices (eight items), and psychological hardship (three items). Two items (sent to debt collection and ever filed for bankruptcy) did not map onto any domain and were considered separately. When stratified by sex and age at questionnaire, the same clusters of items measuring three hardship domains were identified (data not shown). Reliability tests on the basis of the KR-20 formula were 0.85, 0.86, and 0.86 for behavioral, material hardship/financial sacrifices, and psychological domains, respectively, suggesting acceptable internal consistency within each domain. When the factor analysis was performed independently in siblings, the same clusters of items measuring three domains were identified (data not shown). A higher proportion of survivors than siblings endorsed ≥ 1 item in each of the domains (all P < .001; Fig 1). Survivors had a higher mean standardized domain score than siblings in each domain (all P < .001; Fig 2). For the binary scoring method, multivariate logistic regression models found that greater behavioral hardship was associated with being female, being younger than 35 years survey, having less than a college education, having no/public health insurance, being divorced/separated, having received ≥ 250 mg/m2 anthracycline chemotherapy, and having received chest radiation (Table 3). Greater material hardship/financial sacrifices were associated with female sex, lower educational attainment, no health insurance, being single, and having been treated with cranial or total body radiation. Psychological hardship was associated with female sex, being younger at survey, having less than a college education, no/public insurance, being divorced/separated, or having received higher doses of anthracyclines or alkylating agents. The unweighted summated scoring method yielded similar associations (Data Supplement).
FIG 2.
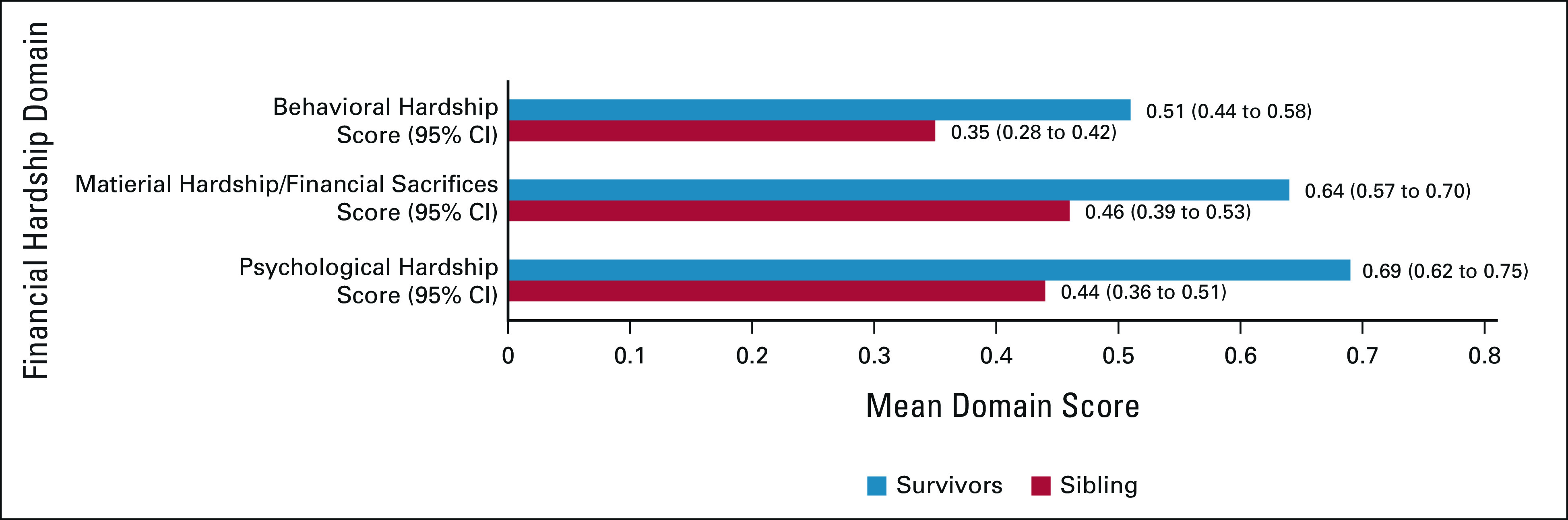
Mean standardized financial hardship domain scores in survivors versus siblings. The standardize score of each domain is shown as the departure from no financial hardship in the domain. The unit is the standard deviation of the standardized score among survivors. Calculation of the standard score in the behavioral hardship domain was adjusted to account for the fact that survivors had eight items in this domain while survivors had 7. P < .001 for each survivor versus sibling comparison. Comparisons adjusted for sex and age at questionnaire. GEE used to account for within-family correlation. GEE, generalized estimating equation.
TABLE 3.
Multivariate Logistic Regression Models of Predictors of Financial Hardship Domains in Survivors on the Basis of a Binary Scoring Method
DISCUSSION
Among a geographically diverse and contemporary cohort of over 3,500 adult survivors of childhood cancer and almost 1,000 siblings, survivors were more likely to report financial hardship in one or more of 20 items that evaluated a broad range of manifestations of financial hardship. Some studies in adults have shown that key provisions of the ACA implemented in 2014, such as Medicaid expansion and elimination of preexisting condition exclusions, were associated with insurance coverage and reductions in out-of-pocket costs, and care unaffordability among adults.33-35 However, despite implementation of these provisions, almost 30% of childhood cancer survivors reported that they were currently paying off medical bills although they were an average of 32 years from cancer diagnosis, suggesting that new and existing chronic health conditions stemming from cancer therapy led to persistent financial hardship. Concerningly, 30% of survivors reported having been sent to debt collection, a rate almost one-third higher than that observed in siblings. It is particularly concerning that between one quarter and one third of survivors were worried about their ability to pay for necessities such as shelter, nutritious food, and utilities.
This study used novel methodology to combine previously validated and fielded financial hardship questions for application to childhood cancer survivors, laying the groundwork for interventions addressing financial hardship in this population. We adopted extant items from US national surveys to build the tool, cognitive debriefing to ensure content validity, and standard measurement methods to demonstrate structural validity and internal consistency of individual domains. Factor analysis identified three conceptually distinct domains that reflect health care seeking behaviors, material hardship and financial sacrifices, and psychological stress or worry about finances. Items from each domain reliably captured specific financial hardship concepts. As with the individual items, survivors were more likely to report hardship in all three domains. Future research will be needed to explore whether and how this tool can be applied to survivors outside of the United States.
Although some prior research has investigated financial hardship in children with cancer and those who are survivors, most financial hardship research in oncology has focused on adults with cancer during active therapy or early post-treatment.7,8,10,11,16 Hospital-based programs that provide financial navigation are often available during cancer treatment. The impact of undergoing cancer therapy is substantial—families of adults with cancer report an average decrease of 20% in family income within 2 years of cancer diagnosis.36 This hardship can affect quality of life, lead to reduced treatment adherence, and an elevated risk of bankruptcy, all of which can lead to poorer outcomes, including survival.18 These challenges often persist into the survivorship phase, with 20% of survivors reporting material or psychological challenges many years after their cancer diagnosis.7 Unfortunately, most financial programs are not accessible once patients complete therapy and enter survivorship.
In children with cancer, the initial financial burden is usually borne by their parents, often driven by changes in work because of their child's treatment or by out-of-pocket medical costs.37-39 How the hardship experienced by parents affects the financial prospects of their children—both the child with cancer and their siblings—has not been established. Beyond the long-term residual impact of the financial hardship experienced by their parents, childhood cancer survivors must deal with the impact of late effects on their own finances. Survivors are at elevated risk for developing a serious or life-threatening chronic condition,2 multiple conditions,40 frailty,41 and psychological sequelae, all of which can affect education, employment, and income. Consequently, survivors are more likely to have lower educational attainment,42 not marry,43 and have difficulty obtaining adequate health insurance.44 The impact of these sociodemographic factors may be exacerbated by receipt of toxic cancer treatments. Higher doses of anthracycline and alkylating agent chemotherapy are associated with increased risk for serious late effects which may affect medical costs, leading to financial hardship. Cranial radiation often leads to neurocognitive deficits which are associated with lower educational attainment and employment prospects.45
Interestingly, many of the factors associated with a greater likelihood of hardship in survivors mirror those observed in the general population, including female sex, lower educational attainment, younger age, inadequate health insurance, and being unmarried.46 Although female survivors in this study were more likely to report hardship than males, none of the demographic or treatment characteristics associated with hardship was more common in female respondents. In fact, females had higher educational attainment and were more likely to be married while being less likely to have received alkylating agents or radiation. This suggests that the impact of sex on hardship in survivors is likely similar to its impact in the general population and is not driven by diagnosis or treatment. Other than sex and age, the remaining factors may all have been affected by prior cancer therapy. Longitudinal data will be needed to understand the pathways from sociodemographic and cancer therapy factors to financial hardship which are likely mediated by the development and evolution of chronic health conditions and factors such as changes in employment, income, and health insurance coverage.
Given the high prevalence of financial hardship observed in this study, the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancer47 is encouraged to create recommendations for surveillance for hardship. The development of cancer-specific screening tools and referral guidelines are in their infancy, focused on on-treatment patients rather than long-term survivors.48,49 Since most adult survivors of childhood cancer are no longer engaged with the cancer care system,50 it is imperative that primary care practitioners, social workers, and other providers are aware of these risks—whether through sharing of survivor care plans or other mechanisms remains to be established.
This is among the largest studies of financial hardship conducted in cancer survivors, particularly survivors of cancer during childhood. Other strengths include its geographic diversity, use of previously cognitively tested and fielded measures and its focus on hardship in the post-ACA implementation era. However, there are limitations. First, as with other CCSS studies, siblings are the comparison cohort, rather than unaffected individuals in the general population. Although the sibling cohort more commonly reports being married/living as married and higher educational attainment and private health insurance coverage than the general population in published studies,13 siblings could have increased risk for financial hardship compared with children of families without a child who experienced a life-threatening illness because of the impact of cancer on their parents' finances and the increased risk for mental health challenges51,52 among some siblings of cancer survivors. Thus, understanding the effects of a sibling cancer diagnosis and risk of financial hardship relative to the general population will be important for future research. Second, we relied on self-report to assess financial hardship—discussion about finances is a sensitive topic and may render our observations susceptible to social desirability bias, which may understate the prevalence of hardship. Nonrespondents were more likely to have sociodemographic features that have been associated with greater financial hardship, such as being male, non-White, unmarried, and having lower educational achievement. Furthermore, almost half of the 199 survivors excluded from the analysis because their survey was completed by a proxy had a history of a brain tumor, a diagnosis associated with an elevated risk for poor psychosocial outcomes and potentially greater financial hardship. Third, although the CCSS has undertaken several initiatives to maximize the inclusion of racial/ethnic minorities in the cohort,53 this is a largely White population, which might lead to underestimation of financial hardship in the broader survivor population. Fourth, since we did not have comparable data from before ACA implementation, we were unable to show whether financial hardship diminished in this population after ACA. Future CCSS surveys will capture the same items to generate longitudinal data on changes in financial hardship as survivors age and the impact of financial hardship on health outcomes. Finally, the methods used to combine individual items into domains and to report the scores on a linear scale are novel in the financial hardship literature—future work will be needed to demonstrate that this approach and the domains identified by our study are generalizable to other populations.
The findings of this study reveal that adults who had cancer during childhood are more likely to experience a range of financial challenges despite safeguards introduced by the ACA. Sociodemographic and treatment characteristics associated with greater prevalence of financial hardship can be used to inform the creation of screening tools and the development of targeted intervention strategies to reduce the risk of poor financial outcomes in this vulnerable population.
ACKNOWLEDGMENT
The patient survey fielded in this effort was based in part on surveys developed for use in the conduct of Alliance/NCI A231602CD “Assessing Financial Difficulty In Patients.”
Tara O. Henderson
Other Relationship: Seattle Genetics
Uncompensated Relationships: National Academies of Medicine, Engineering and Sciences Committee on Disability and Childhood Cancer
Open Payments Link: https://openpaymentsdata.cms.gov/physician/402343
Elyse R. Park
Honoraria: UpToDate
Anne C. Kirchhoff
Stock and Other Ownership Interests: Medtronic (I)
Kevin Krull
Patents, Royalties, Other Intellectual Property: Royalties from Wolters Kluwer
Wendy Leisenring
This author is a member of the Journal of Clinical Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Gregory T. Armstrong
Honoraria: Grail
K. Robin Yabroff
Consulting or Advisory Role: Flatiron Health (Inst)
No potential conflicts of interest were reported.
SUPPORT
CCSS is supported by the National Cancer Institute (CA55727, G.T.A., principal investigator) and the American Lebanese-Syrian Associated Charities (ALSAC). R.M.C. received support from the Leukemia and Lymphoma Society, the National Cancer Institute, and the American Cancer Society for her work on this study.
PRIOR PRESENTATION
Presented in part at the ASCO Annual Meeting, Chicago, IL, June 4-8, 2021.
AUTHOR CONTRIBUTIONS
Conception and design: Paul C. Nathan, I-Chan Huang, Tara O. Henderson, Elyse R. Park, Anne C. Kirchhoff, Leslie L. Robison, Wendy Leisenring, Gregory T. Armstrong, Rena M. Conti, K. Robin Yabroff
Financial support: Leslie L. Robison, Gregory T. Armstrong
Administrative support: Leslie L. Robison, Gregory T. Armstrong
Provision of study materials or patients: Leslie L. Robison, Gregory T. Armstrong, Rena M. Conti
Collection and assembly of data: Leslie L. Robison, Wendy Leisenring, Gregory T. Armstrong
Data analysis and interpretation: Paul C. Nathan, I-Chan Huang, Yan Chen, Tara O. Henderson, Kevin Krull, Rena M. Conti, Yutaka Yasui, K. Robin Yabroff
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Financial Hardship in Adult Survivors of Childhood Cancer in the Era After Implementation of the Affordable Care Act: A Report From the Childhood Cancer Survivor Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Tara O. Henderson
Other Relationship: Seattle Genetics
Uncompensated Relationships: National Academies of Medicine, Engineering and Sciences Committee on Disability and Childhood Cancer
Open Payments Link: https://openpaymentsdata.cms.gov/physician/402343
Elyse R. Park
Honoraria: UpToDate
Anne C. Kirchhoff
Stock and Other Ownership Interests: Medtronic (I)
Kevin Krull
Patents, Royalties, Other Intellectual Property: Royalties from Wolters Kluwer
Wendy Leisenring
This author is a member of the Journal of Clinical Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Gregory T. Armstrong
Honoraria: Grail
K. Robin Yabroff
Consulting or Advisory Role: Flatiron Health (Inst)
No potential conflicts of interest were reported.
REFERENCES
- 1. Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: Life-long risks and responsibilities. Nat Rev Cancer. 2014;14:61–70. doi: 10.1038/nrc3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309:2371–2381. doi: 10.1001/jama.2013.6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nathan PC, Nachman A, Sutradhar R, et al. Adverse mental health outcomes in a population-based cohort of survivors of childhood cancer. Cancer. 2018;124:2045–2057. doi: 10.1002/cncr.31279. [DOI] [PubMed] [Google Scholar]
- 4. Lathan CS, Cronin A, Tucker-Seeley R, et al. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;34:1732–1740. doi: 10.1200/JCO.2015.63.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soni A. Trends in the Five Most Costly Conditions Among the U.S. Civilian Institutionalized Population, 2002 and 2012. Statistical Brief 470. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [PubMed] [Google Scholar]
- 6. Bradley CJ, Yabroff KR, Warren JL, et al. Trends in the treatment of metastatic colon and rectal cancer in elderly patients. Med Care. 2016;54:490–497. doi: 10.1097/MLR.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 7. Yabroff KR, Dowling EC, Guy GP, Jr, et al. Financial hardship associated with cancer in the United States: Findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34:259–267. doi: 10.1200/JCO.2015.62.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ekwueme DU, Yabroff KR, Guy GP, Jr., et al. Medical costs and productivity losses of cancer survivors--United States, 2008-2011. MMWR Morb Mortal Wkly Rep. 2014;63:505–510. [PMC free article] [PubMed] [Google Scholar]
- 9. Nipp RD, Shui AM, Perez GK, et al. Patterns in health care access and affordability among cancer survivors during implementation of the Affordable Care Act. JAMA Oncol. 2018;4:791–797. doi: 10.1001/jamaoncol.2018.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guy GP, Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31:3749–3757. doi: 10.1200/JCO.2013.49.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guy GP, Jr, Yabroff KR, Ekwueme DU, et al. Healthcare expenditure burden among non-elderly cancer survivors, 2008-2012. Am J Prev Med. 2015;49:S489–S497. doi: 10.1016/j.amepre.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Doroudi M, Coughlan D, Banegas MP, et al. Is cancer history associated with assets, debt, and net worth in the United States? JNCI Cancer Spectr. 2018;2:pky004. doi: 10.1093/jncics/pky004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lu AD, Zheng Z, Han X, et al. Medical financial hardship in survivors of adolescent and young adult cancer in the United States. J Natl Cancer Inst. 2021;113:997–1004. doi: 10.1093/jnci/djab013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zheng Z, Han X, Zhao J, et al. Financial hardship, healthcare utilization, and health among U.S. cancer survivors. Am J Prev Med. 2020;59:68–78. doi: 10.1016/j.amepre.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 15. Banegas MP, Schneider JL, Firemark AJ, et al. The social and economic toll of cancer survivorship: A complex web of financial sacrifice. J Cancer Surviv. 2019;13:406–417. doi: 10.1007/s11764-019-00761-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Han X, Zhao J, Zheng Z, et al. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29:308–317. doi: 10.1158/1055-9965.EPI-19-0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors' quality of life. JCO Oncol Pract. 2014;10:332–338. doi: 10.1200/JOP.2013.001322. [DOI] [PubMed] [Google Scholar]
- 18. Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34:980–986. doi: 10.1200/JCO.2015.64.6620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yabroff KR, Han X, Song W, et al. Association of cancer history and medical financial hardship with mortality in the United States. J Clin Oncol. 2022;38 doi: 10.1093/jnci/djac044. suppl 29; abstr 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fair D, Park ER, Nipp RD, et al. Material, behavioral, and psychological financial hardship among survivors of childhood cancer in the Childhood Cancer Survivor Study. Cancer. 2021;127:3214–3222. doi: 10.1002/cncr.33613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huang IC, Bhakta N, Brinkman TM, et al. Determinants and consequences of financial hardship among adult survivors of childhood cancer: A report from the St. Jude Lifetime Cohort Study. J Natl Cancer Inst. 2019;111:189–200. doi: 10.1093/jnci/djy120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nipp RD, Kirchhoff AC, Fair D, et al. Financial burden in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2017;35:3474–3481. doi: 10.1200/JCO.2016.71.7066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park ER, Kirchhoff AC, Nipp RD, et al. Assessing health insurance coverage characteristics and impact on health care cost, worry, and access: A report from the Childhood Cancer Survivor Study. JAMA Intern Med. 2017;177:1855–1858. doi: 10.1001/jamainternmed.2017.5047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jost TS, Keith K. The ACA and the courts: Litigation's effects on the law's implementation and beyond. Health Aff (Millwood) 2020;39:479–486. doi: 10.1377/hlthaff.2019.01324. [DOI] [PubMed] [Google Scholar]
- 25. Robison LL, Mertens AC, Boice JD, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: A multi-institutional collaborative project. Med Pediatr Oncol. 2002;38:229–239. doi: 10.1002/mpo.1316. [DOI] [PubMed] [Google Scholar]
- 26. Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: A national cancer institute-supported resource for outcome and intervention research. J Clin Oncol. 2009;27:2308–2318. doi: 10.1200/JCO.2009.22.3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Board PATE . PDQ Financial Toxicity and Cancer Treatment. Bethesda, MD: National Cancer Institute; 2021. [Google Scholar]
- 28. Altice CK, Banegas MP, Tucker-Seeley RD, et al. Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst. 2017;109:djw205. doi: 10.1093/jnci/djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Azzani M, Roslani AC, Su TT. The perceived cancer-related financial hardship among patients and their families: A systematic review. Support Care Cancer. 2015;23:889–898. doi: 10.1007/s00520-014-2474-y. [DOI] [PubMed] [Google Scholar]
- 30. Yabroff KR, Dowling E, Rodriguez J, et al. The Medical Expenditure Panel Survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv. 2012;6:407–419. doi: 10.1007/s11764-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coughlin SS, Datta B, Berman A, et al. A cross-sectional study of financial distress in persons with multimorbidity. Prev Med Rep. 2021;23:101464. doi: 10.1016/j.pmedr.2021.101464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen J, Hillsdale NJ. Statistical Power Analysis for the Behavioral Sciences. ed 2. New York, NY, L. Erlbaum Associates; 1988. [Google Scholar]
- 33. Zhao J, Zheng Z, Nogueira L, et al. Preexisting condition protections under the Affordable Care Act: Changes in insurance coverage, premium contributions, and out-of-pocket spending. Value Health. 2022;25:1360–1370. doi: 10.1016/j.jval.2022.01.016. [DOI] [PubMed] [Google Scholar]
- 34. Han X, Jemal A, Zheng Z, et al. Changes in noninsurance and care unaffordability among cancer survivors following the Affordable Care Act. J Natl Cancer Inst. 2020;112:688–697. doi: 10.1093/jnci/djz218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhao J, Mao Z, Fedewa SA, et al. The Affordable Care Act and access to care across the cancer control continuum: A review at 10 years. CA Cancer J Clin. 2020;70:165–181. doi: 10.3322/caac.21604. [DOI] [PubMed] [Google Scholar]
- 36. Zajacova A, Dowd JB, Schoeni RF, et al. Employment and income losses among cancer survivors: Estimates from a national longitudinal survey of American families. Cancer. 2015;121:4425–4432. doi: 10.1002/cncr.29510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Warner EL, Kirchhoff AC, Nam GE, et al. Financial burden of pediatric cancer for patients and their families. JCO Oncol Pract. 2015;11:12–18. doi: 10.1200/JOP.2014.001495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lindahl Norberg A, Montgomery SM, Bottai M, et al. Short-term and long-term effects of childhood cancer on income from employment and employment status: A national cohort study in Sweden. Cancer. 2017;123:1238–1248. doi: 10.1002/cncr.30436. [DOI] [PubMed] [Google Scholar]
- 39. Bona K, London WB, Guo D, et al. Trajectory of material hardship and income poverty in families of children undergoing chemotherapy: A prospective cohort study. Pediatr Blood Cancer. 2016;63:105–111. doi: 10.1002/pbc.25762. [DOI] [PubMed] [Google Scholar]
- 40. Bhakta N, Liu Q, Ness KK, et al. The cumulative burden of surviving childhood cancer: An initial report from the St Jude Lifetime Cohort Study (SJLIFE) Lancet. 2017;390:2569–2582. doi: 10.1016/S0140-6736(17)31610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hayek S, Gibson TM, Leisenring WM, et al. Prevalence and predictors of frailty in childhood cancer survivors and siblings: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2020;38:232–247. doi: 10.1200/JCO.19.01226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mitby PA, Robison LL, Whitton JA, et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer. 2003;97:1115–1126. doi: 10.1002/cncr.11117. [DOI] [PubMed] [Google Scholar]
- 43. Janson C, Leisenring W, Cox C, et al. Predictors of marriage and divorce in adult survivors of childhood cancers: A report from the Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev. 2009;18:2626–2635. doi: 10.1158/1055-9965.EPI-08-0959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Park ER, Li FP, Liu Y, et al. Health insurance coverage in survivors of childhood cancer: The Childhood Cancer Survivor Study. J Clin Oncol. 2005;23:9187–9197. doi: 10.1200/JCO.2005.01.7418. [DOI] [PubMed] [Google Scholar]
- 45. Scholtes C, Baust K, Weinhold L, et al. Health status, health-related quality of life, and socioeconomic outcome in childhood brain tumor survivors: A German cohort study. Neuro Oncol. 2019;21:1069–1081. doi: 10.1093/neuonc/noz044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yabroff KR, Zhao J, Han X, et al. Prevalence and correlates of medical financial hardship in the USA. J Gen Intern Med. 2019;34:1494–1502. doi: 10.1007/s11606-019-05002-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Children’s Oncology Group: Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancers 2018www.survivorshipguidelines.org.
- 48. Bradley CJ, Yabroff KR, Zafar SY, et al. Time to add screening for financial hardship as a quality measure? CA Cancer J Clin. 2021;71:100–106. doi: 10.3322/caac.21653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yabroff KR, Bradley CJ, Shih YT. Improving the process of screening for medical financial hardship in oncology practice. Cancer Epidemiol Biomarkers Prev. 2021;30:593–596. doi: 10.1158/1055-9965.EPI-21-0111. [DOI] [PubMed] [Google Scholar]
- 50. Nathan PC, Greenberg ML, Ness KK, et al. Medical care in long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2008;26:4401–4409. doi: 10.1200/JCO.2008.16.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. van Warmerdam J, Sutradhar R, Kurdyak P, et al. Long-term mental health outcomes in mothers and siblings of children with cancer: A population-based, matched cohort study. J Clin Oncol. 2020;38:51–62. doi: 10.1200/JCO.19.01382. [DOI] [PubMed] [Google Scholar]
- 52. Lund LW, Winther JF, Dalton SO, et al. Hospital contact for mental disorders in survivors of childhood cancer and their siblings in Denmark: A population-based cohort study. Lancet Oncol. 2013;14:971–980. doi: 10.1016/S1470-2045(13)70351-6. [DOI] [PubMed] [Google Scholar]
- 53. Bhatia S, Gibson TM, Ness KK, et al. Childhood cancer survivorship research in minority populations: A position paper from the Childhood Cancer Survivor Study. Cancer. 2016;122:2426–2439. doi: 10.1002/cncr.30072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity (COST) Cancer. 2017;123:476–484. doi: 10.1002/cncr.30369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. DiStefano C, Zhu M, Mindrila D. Understanding and using factor scores: Considerations for the applied researcher. Pract Assess Res Eval. 2009;14:1–10. [Google Scholar]