Abstract
Background
Developmental dysplasia of the hip (DDH) is the most common hip abnormality in children. Closed or open reduction and cast immobilization are the most commonly used treatments for patients aged 6 to 18 months with dislocation; they are also used in children younger than 6 months when brace treatment is not effective. During cast immobilization, surgeons need reliable and timely imaging methods to assess the status of hip reduction to ensure successful treatment and avoid complications. Several methods are used, but they have disadvantages. We developed and, in this study, evaluated a hip medial ultrasound method to evaluate the status of hip reduction in children treated with a spica cast.
Question/purpose
Is hip medial ultrasound more accurate than radiography for determining the status of hip reduction in children treated with a spica cast?
Methods
Between November 2017 and December 2020, we treated 136 patients with closed or open reduction and spica casting for DDH in our department. These children were 3 to 18 months old at the time of surgical reduction and had a specific medical history, physical examination findings, or AP radiographic evidence of unilateral or bilateral DDH. None had a concomitant femoral/acetabular osteotomy procedure in these hips. All patients underwent hip medial ultrasound, AP radiography, and MRI under sedation within 2 to 7 days after open or closed reduction. The examination time was from the second day after reduction to enable the patient to recover from anesthesia. MRI was performed within 7 days after reduction because of a few long appointment times, and ultrasound and AP radiography were always performed 1 or 2 days before MRI. Based on that, 65% (88 of 136 [88 hips]) of patients were excluded due to the absence of MRI, ultrasound, or AP radiography; 3% (4 of 136 [4 hips]) of patients were excluded because of concurrent congenital spina bifida, Larson syndrome, or Prader-Willi syndrome; and 1% (1 of 136 [1 hip]) of patients were excluded because the patient underwent MRI before ultrasound. A total of 32% (43 of 136 [43 hips]) of patients were eligible for analysis in this cross-sectional diagnostic study, and these 43 patients underwent AP radiography, ultrasound, and MRI. In this retrospective study, the mean age at the time of surgery was 10 ± 4 months (male:female ratio 5:38; unilateral DDH: 34; bilateral DDH: 9). To ensure the independence of the results, the study was limited to one hip per patient (in patients with bilateral DDH, the right hip was evaluated). The reduction of 43 hips (left:right ratio 26:17; closed:open reduction ratio 30:13) was evaluated by MRI, hip medial ultrasound, and radiography. Children with spica casts were placed in the supine position, which is necessary to expose the perineum for ultrasound. We used a broad-spectrum, microconvex, and intracavitary probe. The acetabular medial wall was identified by the triradiate cartilage of the ischial tuberosity and the pubis superior, and the femoral head was identified by the femoral neck. Then, the acetabulum coronal midsectional plane was used to determine the positions of the femoral head and acetabulum and to measure the triradiate cartilage–femoral distance. MRI examinations were performed using a 1.5-T MRI system with an eight-channel body coil. Each reviewer evaluated each reduction independently. Additionally, to further assess the hip medial ultrasound method’s reliability and reproducibility, we investigated the interobserver and intraobserver agreement in evaluating the reduction using hip medial ultrasound. Using ultrasound or radiography, the reviewers classified hips as reduced, uncertain status, or dislocated. MRI was considered the gold standard for assessing hip reduction, and the reviewers classified hips as reduced or dislocated by MRI. Patients with hips with an uncertain reduction status according to ultrasound or radiography were retained in the analysis. Thus, the test results of radiography and ultrasound were classified into three classifications (positive, negative, or uncertain) in the present study. The test was considered positive or negative when patients were assessed with dislocation or without dislocation, respectively. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of ultrasound and radiography were calculated and compared. We combined uncertain and positive into the positive classification to be conservative in the statistical choices. The specificity, sensitivity, PPV, and NPV were analyzed based on this premise. Furthermore, a subgroup analysis was conducted by sex. MRI evaluation revealed that 41 hips were reduced and two hips were dislocated.
Results
The sensitivity, specificity, PPV, and NPV of ultrasound were 100% (95% CI 16% to 100%), 95% (95% CI 84% to 99%), 50% (95% CI 7% to 93%), and 100% (95% CI 91% to 100%), respectively. The sensitivity, specificity, PPV, and NPV of radiography were 50% (95% CI 1% to 99%), 68% (95% CI 52% to 82%), 7% (95% CI 0% to 34%), and 97% (95% CI 82% to 100%), respectively. Ultrasound showed a higher specificity (95% versus 68%; p < 0.001) and PPV (50% versus 7%; p = 0.02) than radiography. The sensitivity, specificity, PPV, and NPV of ultrasound were 100% (95% CI 16% to 100%), 94% (95% CI 81% to 99%), 50% (95% CI 7% to 93%), and 100% (95% CI 90% to 100%), respectively, for female patients (with only five male patients, we could not perform these analyses in this group). The sensitivity, specificity, PPV, and NPV of radiography were 50% (95% CI 1% to 99%), 64% (95% CI 46% to 79%), 7% (95% CI 0% to 34%), and 96% (95% CI 79% to 100%), respectively, for female patients. The κ values for intra- and interobserver reliability both were 1.0.
Conclusion
Hip medial ultrasound can directly visualize the femoral head and acetabulum. Hip medial ultrasound is more reliable than radiography as a preliminary evaluation method and does not involve irradiation. We recommend using hip medial ultrasound during outpatient follow-up visits for patients younger than 2 years treated with hip reduction and cast immobilization.
Level of Evidence
Level III, diagnostic study.
Introduction
Developmental dysplasia of the hip (DDH) is the most common hip abnormality in children. Closed or open reduction and cast immobilization are the most commonly used treatments for patients aged 6 months to 18 months with dislocation or children younger than 6 months when brace treatment does not work [20, 21]. During cast immobilization, surgeons need to accurately assess the status of hip reduction to ensure successful treatment and avoid complications [1]. Radiography [21], CT [3, 15], and MRI [4, 8, 11, 12, 14] have been used to assess reduction status. However, radiography and CT cannot show the details of cartilage very well, and those modalities are associated with radiation; MRI also has disadvantages, such as the need for sedation, high costs, and long scanning times. More recently, ultrasound has been used to assess reduction in patients with DDH who are treated with cast immobilization after reduction [2, 5, 11, 17, 19].
In their study, van Douveren et al. [19] applied a transinguinal probe to scan via the cross-section of the inguinal region from the anterior side of the hip and to assess reduction since the pubis superior ramus, acetabulum, femoral head, and femoral neck were on the same plane. This method requires the cast opening to be sufficiently large to completely display the inguinal region and the above anatomical structures on the same image. Mehdizadeh et al. [11] used a transgluteal ultrasonography approach to examine the position of the femoral head in relation to the posterior rim of the acetabulum in spica casts. In the transgluteal approach, the medial ultrasonography probe was placed on the gluteus maximus muscle. However, it can be difficult to determine where the femoral head is dislocated using the transgluteal approach because sometimes the posterior opening area of the spica cast is not large. Also, in older patients or when the gluteus maximus muscle is thick, it may be difficult to view the hip clearly. In addition, none of the above studies directly showed the triradiate cartilage and the acetabulum coronal mid sectional plane. Furthermore, the distance between the femoral head and acetabulum could not be measured on the acetabulum coronal midsectional plane. Thus, it is difficult to conduct a quantitative assessment in these studies. Because of these limitations, to this point, ultrasound has not been widely used for the postoperative assessment of hip reduction.
We therefore developed a hip medial ultrasound method to evaluate the status of hip reduction in children treated with a spica cast. This method does not require a large opening window on casting. An important ultrasound section—the acetabulum coronal mid sectional plane—is applied in this method, which allows for not only the visualization of the positional relationship between the femoral head and acetabulum, but also the measurement of the above distance as a quantitative indicator, which provides additional clinical information.
In this study, we asked: Is hip medial ultrasound more accurate than radiography for determining the status of hip reduction in children treated with a spica cast?
Patients and Methods
Study Design and Setting
This cross-sectional study was performed at our institution, which is a large referral center in an urban area. In the past 10 years, approximately 5000 ultrasound examinations for DDH screening have been performed at our outpatient clinic annually, and approximately 440 DDH patients have been treated surgically each year.
Research Participants
Between November 2017 and December 2020, we treated 136 patients with closed or open reduction and spica casting for DDH in our department. These children were 3 to 18 months old at the time of surgical reduction and had a specific medical history, physical examination findings, or AP radiographic evidence of unilateral or bilateral DDH. None had a concomitant femoral/acetabular osteotomy procedure. Radiography was needed to determine that the femoral head was not in contact or was only partially in contact with the acetabulum, that there was a discontinuous Shenton line, and that the midpoint of the superior margin of the ossified proximal femoral metaphysis was lateral to the Perkin line. There are eight treatment groups in our department. Radiography is generally used in all of them for verifying the position of the femoral head after reduction and spica casting; when the position was considered uncertain on radiography, MRI was also performed. To introduce and verify the applicability and reliability of hip medial ultrasound, we applied hip medial ultrasound in three treatment groups (the groups of the study authors XML,YKW, GF) in addition to the above examinations. We considered those who underwent hip medial ultrasound, radiography, and MRI as potentially eligible.
Based on that, 65% (88 of 136 [88 hips]) of patients were excluded due to the absence of MRI, ultrasound, or AP radiography; 3% (4 of 136 [4 hips]) of patients were excluded because of concurrent congenital spina bifida, Larson syndrome, or Prader-Willi syndrome; and 1% (1 of 136 [1 hip]) of patients were excluded because the patient underwent MRI before ultrasound. A total of 32% (43 of 136 [43 hips]) of patients were eligible for analysis in this cross-sectional diagnostic study, and all 43 patients underwent AP radiography, ultrasound, and MRI.
All patients underwent hip medial ultrasound, AP radiography, and MRI within 2 to 7 days after open or closed reduction. The examination time was from the second day after reduction to enable the patient to recover from the anesthesia and return to daily activities. MRI was performed within 7 days after reduction because of a few long appointment times, and ultrasound and AP radiography were always performed 1 or 2 days before MRI.
Demographic and Clinical Characteristics of the Enrolled Patients
Forty-three patients were enrolled in this retrospective study (male:female ratio 5:38; unilateral DDH: 34; bilateral DDH: 9). The mean age at the time of surgery was 10 ± 4 months. To ensure the independence of the results, the study was limited to one hip per patient. In patients with unilateral DDH, only the affected hip was evaluated. In patients with bilateral DDH, the right hip was evaluated. The reduction of 43 hips (left:right ratio 26:17; closed:open reduction ratio 30:13) was evaluated by MRI, hip medial ultrasound, and radiography (Table 1).
Table 1.
Demographic and clinical characteristics of the enrolled patientsa
| Patient number | Sex | Age in months | Unilateral or bilateral | Hip number | Left or right | Closed or open reduction |
| 1 | Male | 6 | Bilateral | 1 | R | Open |
| 2 | Male | 11 | Unilateral | 2 | R | Closed |
| 3 | Female | 7 | Unilateral | 3 | L | Closed |
| 4 | Female | 6 | Unilateral | 4 | L | Closed |
| 5 | Female | 10 | Unilateral | 5 | L | Closed |
| 6 | Female | 15 | Unilateral | 6 | L | Closed |
| 7 | Female | 14 | Unilateral | 7 | L | Open |
| 8 | Female | 8 | Unilateral | 8 | L | Closed |
| 9 | Female | 5 | Unilateral | 9 | L | Closed |
| 10 | Female | 13 | Unilateral | 10 | R | Closed |
| 11 | Female | 8 | Unilateral | 11 | L | Closed |
| 12 | Female | 11 | Bilateral | 12 | R | Closed |
| 13 | Female | 6 | Unilateral | 13 | R | Closed |
| 14 | Female | 7 | Bilateral | 14 | R | Closed |
| 15 | Female | 8 | Unilateral | 15 | L | Closed |
| 16 | Female | 18 | Unilateral | 16 | L | Open |
| 17 | Female | 15 | Unilateral | 17 | L | Closed |
| 18 | Female | 9 | Unilateral | 18 | L | Open |
| 19 | Female | 12 | Unilateral | 19 | L | Closed |
| 20 | Female | 4 | Unilateral | 20 | L | Closed |
| 21 | Female | 7 | Unilateral | 21 | L | Closed |
| 22 | Female | 15 | Unilateral | 22 | L | Open |
| 23 | Female | 9 | Unilateral | 23 | L | Open |
| 24 | Female | 14 | Unilateral | 24 | L | Closed |
| 25 | Female | 7 | Unilateral | 25 | L | Closed |
| 26 | Female | 3 | Bilateral | 26 | R | Closed |
| 27 | Female | 14 | Bilateral | 27 | R | Open |
| 28 | Female | 7 | Unilateral | 28 | R | Closed |
| 29 | Female | 5 | Unilateral | 29 | L | Closed |
| 30 | Female | 10 | Unilateral | 30 | R | Closed |
| 31 | Female | 17 | Unilateral | 31 | L | Closed |
| 32 | Female | 12 | Bilateral | 32 | R | Closed |
| 33 | Female | 8 | Unilateral | 33 | L | Closed |
| 34 | Female | 7 | Unilateral | 34 | R | Closed |
| 35 | Female | 15 | Unilateral | 35 | L | Closed |
| 36 | Female | 10 | Unilateral | 36 | R | Open |
| 37 | Male | 10 | Bilateral | 37 | R | Closed |
| 38 | Female | 19 | Bilateral | 38 | R | Open |
| 39 | Female | 11 | Unilateral | 39 | L | Open |
| 40 | Male | 8 | Unilateral | 40 | R | Closed |
| 41 | Female | 5 | Unilateral | 41 | L | Open |
| 42 | Female | 8 | Bilateral | 42 | R | Open |
| 43 | Male | 8 | Unilateral | 43 | L | Open |
The study was limited to one hip per patient. Unilateral DDH was evaluated only for the affected hip. In patients with bilateral DDH, the right hip was evaluated.
Imaging Test Methods
Hip medial ultrasound, radiography, and MRI were performed within 2 to 7 days after open or closed reduction to evaluate the status of hip reduction. After the patient emerges from anesthesia, there inevitably will be positional changes, and during this time, dislocation may occur again if the reduction is unstable. We chose 2 to 7 days after surgery to conduct ultrasound, radiography, and MRI to evaluate the dynamic hip position more appropriately.
Reviewers (JMY, XML, YKW, WG, GF) evaluated hip reduction independently on ultrasound, radiographs, and MR images, and they were blinded to the other imaging results. When the reviewers read an ultrasound, they did not know the results of the plain radiograph or MRI examination, and vice versa. Two reviewers (JMY, WG), each with more than 8 years of experience in DDH imaging, independently evaluated the ultrasound results regarding the status of reduction.
To further assess hip medial ultrasound method reliability and reproducibility, we investigated the interobserver and intraobserver agreement in evaluating the reduction using hip medial ultrasound. The interobserver agreement was estimated by calculating the kappa value and 95% confidence interval (CI) between the two observers (JMY, WG). For intraobserver agreement, one observer (JMY) performed a blinded second reading of all ultrasound images with a 6-month interval between readings. Anonymized AP radiograph and MRI data were assigned in a random order to the reviewers to evaluate the status of reduction. The radiograph and MRI reviewers were two pediatric orthopaedic surgeons (YKW, GF), each of whom had 10 years of clinical experience in treating pediatric hip disease.
Radiography Evaluation Criteria
Reduction was assessed using radiography because all hips were in a cast. Hips were determined to be reduced, have an uncertain status, or be dislocated based on the height of the superior margin of the ossified metaphysis with respect to the superolateral margin of the triradiate cartilage, the distance between the superior margin of the ossified metaphysis and the acetabulum, the direction of the long axis of the metaphysis of the proximal femur, and the continuity of the Shenton line (Fig. 1).
Fig. 1.
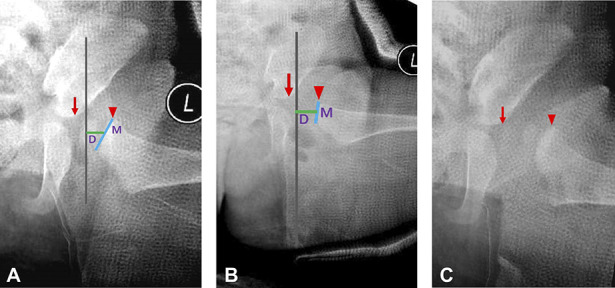
A-C (A) Radiography evaluation criteria for the reduced hip: The highest point of the superior margin of the ossified metaphysis (arrowhead) was not higher than the superolateral margin of the triradiate cartilage (small arrow), the direction of the long axis of the metaphysis of the proximal femur was toward the triradiate cartilage, and the distance (D) from the midpoint of the superior margin of the ossified metaphysis to the perpendicular line from the superolateral margin of the acetabulum was smaller than the length of the superior margin of the ossified metaphysis (M). (B) Radiography evaluation criteria for the uncertain hip: The highest point of the superior margin of the ossified metaphysis (arrowhead) was not higher than the superolateral margin of the triradiate cartilage (small arrow), the direction of the long axis of the metaphysis of the proximal femur was toward the triradiate cartilage, and the distance (D) from the midpoint of the superior margin of the ossified metaphysis to the perpendicular line from the superolateral margin of the acetabulum was larger than the length of the superior margin of the ossified metaphysis (M). (C) Radiography evaluation criteria for the dislocated hip: The Shenton line was broken, the highest point of the superior margin of the ossified metaphysis (arrowhead) was higher than the superolateral margin of the triradiate cartilage (small arrow), and the direction of the long axis of the metaphysis of the proximal femur was not toward the triradiate cartilage. A color image accompanies the online version of this article.
MRI Evaluation Criteria
Reduction was assessed using MRI because all hips were in a cast. In hips that were reduced, the femoral head pointed toward the triradiate cartilage, and all or part of the femoral head was inside the acetabulum in both coronal and axial images. In hips with dislocation, the femoral head was outside the outer edge of the acetabulum and was separated from the acetabulum by the inverted labrum in both coronal and axial images (Fig. 2).
Fig. 2.
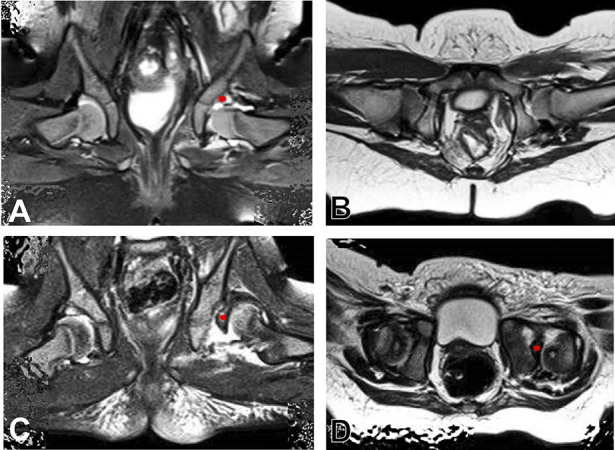
MRI evaluation criteria for (A-B) the reduced hip: Coronal imaging demonstrated that the femoral head was below the labrum (*). Coronal and axial imaging demonstrated that the femoral head was in the acetabulum and that the direction of the femoral head was toward the triradiate cartilage. (C-D) For the dislocated hip: Coronal and axial imaging demonstrated that the femoral head was completely dislocated and was separated from the acetabulum by the inverted labrum (*). A color image accompanies the online version of this article.
Instruments
We used the GE LOGIQ E9 color Doppler ultrasound system (GE Medical Systems Ultrasound and Primary Care Diagnostics LLC). We used a broad-spectrum, microconvex, and intracavitary probe in the hip medial ultrasound method to evaluate the status of hip reduction in children treated with a spica cast. We selected this probe for several reasons. First, the contact area between the probe and the skin is small. The probe, with a length of 2 mm, can be properly placed in the opening of the medial hip without being shielded by the spica cast and also avoids contact with the labia and scrotum in females and males, respectively. Second, the probe has a wide frequency of 3 to 10 MHz; therefore, it can be used in both small infants with thin, soft tissue and older infants with thick, soft tissue. Third, the probe has an extensive bandwidth with a 145° field of view, which enables the femoral neck, femoral head, and acetabulum to be fully visualized in the ultrasound image.
MRI examinations were performed using a 1.5-T MRI system (MagnetomEspree, Siemens AG) with an eight-channel body coil. The imaging sequences included axial spin-echo T1-weighted images (repetition time and echo time of 400 ms and 17 ms, respectively; slice thickness and slice gap of 3 mm and 0.3 mm, respectively), coronal short tau inversion recovery (repetition time, inversion time, and echo time of 3860 ms, 160 ms, and 60 ms, respectively; slice thickness and slice gap of 4 mm and 0.4 mm, respectively), and coronal 3D T1-weighted image volume interpolated body examination (repetition time and echo time of 15.4 ms and 6 ms, respectively; flip angle = 15°; field of view = 20 cm × 20 cm; voxel size = 0.6 mm × 0.6 mm).
Hip Medial Ultrasound Examination
Scanning Procedure
The probe was covered by a disposable polyethylene glove to keep the child’s perineal area clean. Children with spica casts were placed in the supine position, and the perineum was exposed. The parents remained nearby to comfort the children (Fig. 3). The probe was placed laterally on the skin of the medial hip side of the cast, and the sound beam was oriented toward the child’s head and parallel to the body’s coronal plane. The ischial tuberosity was observed as a thick, bright echo with an acoustic shadow (Fig. 4A).
Fig. 3.

This photograph shows positioning of the probe on a child in a spica cast. The probe was placed at the medial side of the hip, and the sound beam was parallel to the coronal plane of the body.
The probe was moved toward the ventral side of the child until the pubic superior ramus and body were visualized as a thick, broken line–shaped, strong echo (Fig. 4B). Subsequently, the probe was moved slightly toward the dorsal side. When the echo disappeared and the hyperechoic ischium was not visible, triradiate cartilage between the pubis and ischium appeared (Fig. 4C), which showed a wide, strip-shaped, low echo (area “A” in Fig. 5). The acetabular bony roof was in the deep portion of the outer side on the sonogram, which showed a strong, thick, line-shaped echo (area “B” in Fig. 5). When the triradiate cartilage and acetabular bony roof were displayed, the acetabulum coronal mid sectional plane was identified.
Fig. 4.
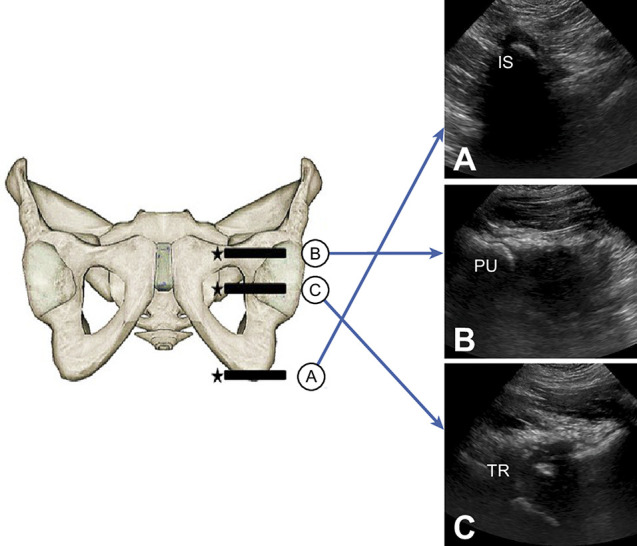
A-C This figure shows the scanning procedure for hip medial ultrasound. According to the bony markers of the (A) ischial tuberosity and (B) pubis superior ramus, the probe was moved up and down to identify (C) the triradiate cartilage between the pubis and ischium; PU = pubis; TR = triradiate cartilage; IS = ischium.
Fig. 5.
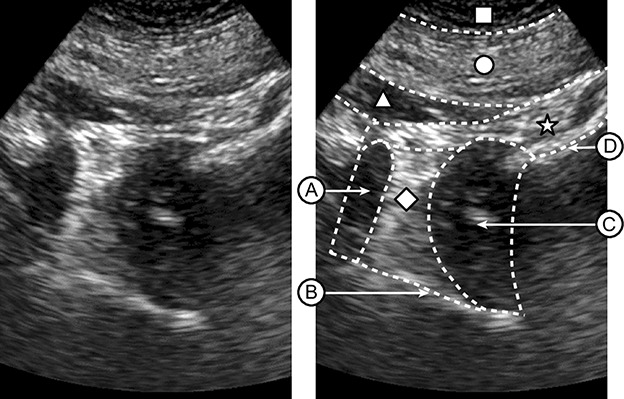
These images are of the hip’s anatomic structures in the acetabulum coronal midsectional plane: (A) triradiate cartilage, (B) bony acetabular roof (ilium), (C) femoral head, and (D) femoral neck; □ = skin layer and subcutaneous tissue; ○ = hip adductor; △ = obturator externus; ☆= joint capsule; ◇ = acetabular component, such as the pulvinar fat pad and ligament teres.
The femoral head showed a nut-shaped, low echo (area “C” in Fig. 5). Before femoral ossification signals appeared, the femoral head was not easily visible ultrasonically. We identified the femoral head by the femoral neck, which appeared as a slightly curved, thick, linear echo (area “D” in Fig. 5). Furthermore, the AP position of the femoral head and acetabulum was determined by moving the probe up and down the coronal sections of the pubis, cartilage, and ischium. During the examination, the sonographer continually adjusted the ultrasound parameters, such as depth, focus, and frequency, according to the patient’s age and body size.
Reduction Evaluation
The triradiate cartilage–femoral distance (TFD) is the distance between the femoral head and the medial wall of the acetabulum, and it was measured as the distance between the internal edge of the femoral head and the lateral edge of the triradiate cartilage between the pubis and ischium on the acetabulum coronal midsectional plane.
Reduction status was classified by hip medial ultrasound findings as follows: reduced, the femoral head could be seen on the acetabulum coronal mid sectional plane and the TFD was no more than 10 mm; uncertain, the femoral head could be seen on the acetabulum coronal mid sectional plane and the TFD was more than 10 mm; and dislocated, the femoral head could not be seen on the acetabulum coronal mid sectional plane.
Ethical Approval
This retrospective study was approved by our institutional review board, and the requirement to obtain informed consent was waived.
Statistical Analysis
Normally distributed measurement data are described as the means and SDs. Skewed measurement data are presented as medians and interquartile ranges. We used a chi-square test to compare count data among groups. Intraobserver and interobserver agreement between the observers were assessed by estimating κ values along with 95% CIs. Herein, κ values between 0 and 0.20 represented poor reliability, values between 0.21 and 0.40 represented fair reliability, values between 0.41 and 0.60 represented moderate reliability, values between 0.61 and 0.80 represented substantial reliability, and values between 0.81 and 1.00 represented excellent reliability [7]. To ensure the independence of the results, one hip of each patient was evaluated. Unilateral DDH was evaluated only for the affected hip. Bilateral DDH was assessed using the right hip. MRI was considered the gold standard for assessing hip reduction. Patients with hips with an uncertain reduction status by ultrasound or radiography were retained in the analysis. Thus, the test results of radiography and ultrasound were classified into three classifications (positive, negative, or uncertain) in the present study. The test was considered positive or negative when patients were assessed with dislocation or without dislocation, respectively. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of ultrasound and radiography were calculated and compared statistically. Notably, specificity is the percentage of true negatives of all subjects who do not have a disease or condition. A highly specific screening test is unlikely to report false-positive results; the diagnostic test of participants is very unlikely to indicate a disease or condition if they indeed do not have it. That is, high specificity permits participants to be confidently regarded as having a disease or condition if they are categorized as positive [18]. We combined uncertain and positive into the positive classification to be conservative in the statistical choices. We analyzed the specificity, sensitivity, PPV, and NPV based on this premise. For comparisons of sensitivity, specificity, PPV, and NPV between radiography and ultrasound, we used the “DTComPair” package [9, 16]. Furthermore, we conducted a subgroup analysis. Data analyses were performed using SPSS (version 22, 2013, IBM Corp) and R Statistical Software (version 4.1.3; R Foundation for Statistical Computing). All tests were two-sided, and p values less than 0.05 were considered significant.
A power analysis indicated that to detect a κ value of at least 0.95 when the null value is 0.4, we would require a minimum of 37 patients across observers based on a significance level of 0.05, assuming there were three categories with frequencies equal to 0.9, 0.04, and 0.06 in the sample [6, 10].
MRI Findings (Gold Standard for Hip Reduction)
The MRI evaluation revealed that 41 hips were reduced and two were dislocated.
Results
Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value
The sensitivity, specificity, PPV, and NPV of ultrasound were 100% (95% CI 16% to 100%), 95% (95% CI 84% to 99%), 50% (95% CI 7% to 93%), and 100% (95% CI 91% to 100%), respectively. The sensitivity, specificity, PPV, and NPV of radiography were 50% (95% CI 1% to 99%), 68% (95% CI 52% to 82%), 7% (95% CI 0% to 34%), and 97% (95% CI 82% to 100%), respectively (Table 2).
Table 2.
Measures of the diagnostic accuracy of ultrasound and radiography for diagnosing the status of hip reduction in patients treated with a spica cast
| Method | Sensitivity (95% CI), % | Specificity (95% CI), % | PPV (95% CI), % | NPV (95% CI), % |
| Ultrasound | 100 (16-100) | 95 (84-99) | 50 (7-93) | 100 (91-100) |
| Radiography | 50 (1-99) | 68 (52-82) | 7 (0-34) | 97 (82-100) |
Ultrasound showed a higher specificity (95% versus 68%; p < 0.001) and PPV (50% versus 7%; p = 0.02) than radiography. With the numbers available, there was no difference in sensitivity (100% versus 50%; p = 0.32) or NPV (100% versus 97%; p = 0.32) between ultrasound and radiography (Table 3).
Table 3.
Comparison of diagnostic performance between radiography and ultrasound in terms of sensitivity, specificity, PPV, and NPV in patients treated with a spica cast
| Methods compared | Parameter | |||
| Sensitivity | Specificity | PPV | NPV | |
| Radiography vs ultrasound | 50% vs 100% | 68% vs 95% | 7% vs 50% | 97% vs 100% |
| p value | 0.32 | < 0.001 | 0.02 | 0.32 |
Subgroup Analysis by Sex
Additionally, we also conducted a subgroup analysis by sex. Five male patients were included in the study. Notably, the results of the diagnostic test among ultrasound, radiography, and MRI methods were consistent (all of them were diagnosed without dislocation). We then explored the diagnostic accuracy of ultrasound and radiography in 38 female patients. The sensitivity, specificity, PPV, and NPV of ultrasound were 100% (95% CI 16% to 100%), 94% (95% CI 81% to 99%), 50% (95% CI 7% to 93%), and 100% (95% CI 90% to 100%), respectively, for the female patients. The sensitivity, specificity, PPV, and NPV of radiography were 50% (95% CI 1% to 99%), 64% (95% CI 46% to 79%), 7% (95% CI 0% to 34%), and 96% (95% CI 79% to 100%), respectively, for the female patients (Table 4).
Table 4.
Measures of the diagnostic accuracy of ultrasound and radiography for diagnosing the status of hip reduction in female patients treated with a spica cast
| Method | Sensitivity (95% CI), % | Specificity (95% CI), % | PPV (95% CI), % | NPV (95% CI), % |
| Ultrasound | 100 (16-100) | 94 (81-99) | 50 (7-93) | 100 (90-100) |
| Radiography | 50 (1-99) | 64 (46-79) | 7 (0-34) | 96 (79-100) |
In female patients, ultrasound showed a higher specificity (94% versus 64%; p < 0.001) and PPV (50% versus 7%; p = 0.02) than radiography. With the numbers available, there was no difference in sensitivity (100% versus 50%; p = 0.32) or NPV (100% versus 96%; p = 0.32) between ultrasound and radiography (Table 5).
Table 5.
Comparison of diagnostic performance between radiography and ultrasound in terms of sensitivity, specificity, PPV, and NPV in female patients treated with a spica cast
| Methods compared | Parameter | |||
| Sensitivity | Specificity | PPV | NPV | |
| Radiography vs ultrasound | 50% vs 100% | 64% vs 94% | 7% vs 50% | 96% vs 100% |
| p value | 0.32 | < 0.001 | 0.02 | 0.32 |
Interobserver and Intraobserver Agreement in Evaluating the Reduction Using Hip Medial Ultrasound
To further assess hip medial ultrasound method reliability and reproducibility, we investigated the interobserver and intraobserver agreement in evaluating the reduction using hip medial ultrasound. The interobserver agreement was estimated by calculating the κ value and 95% CI between the two observers (JMY, WG). Interobserver agreement was excellent between the observers (κ =1.000; p < 0.001). The intraobserver agreement (JMY, rereading the same images in a blinded fashion at a 6-month interval) was likewise almost perfect, with a κ of 1 (Table 6).
Table 6.
Kappa coefficients of interobserver and intraobserver agreement for ultrasound
| Agreement | Number | κ (95% CI) | p value |
| Interobserver agreement | 43 | 1.00 (1.00-1.00) | < 0.001 |
| Intraobserver agreementa | 43 | 1.00 (1.00-1.00) | < 0.001 |
One experienced ultrasound radiologist performed a second reading for all patients, with a 6-month interval between readings.
Discussion
Verifying the femoral head position in a spica cast after closed or open reduction is important to ensure that reduction has been performed properly [20, 21]. Postoperative radiography alone appears to be inadequate for assessing whether the hip is reduced or dislocated, and surgeon experience and subspecialty training cannot prevent errors [22]. Although there has been some research on the use of ultrasound in this field [2, 5, 11, 17, 19], the spica cast and commonly used probes limit the applicability of ultrasound. We therefore developed hip medial ultrasound, using a microconvex probe, and set the acetabulum coronal mid sectional plane as the fixed section for the index measurement. This method did not require a large window in the spica cast. A comparison of diagnostic parameters between ultrasound and radiography method revealed higher specificity and PPV in the hip medial ultrasound. However, with the numbers available, the sensitivity and NPV of ultrasound did not differ from that of radiography. Intraobserver and interobserver reliability were nearly perfect, suggesting that the hip medial ultrasound method is a reliable way to determine the status of hip reduction in children treated with a spica cast.
Limitations
This study has some limitations. First, we wished to evaluate the diagnostic value of ultrasound and radiography in a subgroup analysis by sex, but with only five male patients, it was not possible to do this statistically. However, in that small group, the results of the diagnosis made by ultrasound, radiography, and MRI were consistent. We performed the subgroup analysis separately in females and given the larger number of females (female sex is a risk factor for DDH [19]), we found medial ultrasound to be very reliable in female patients.
Second, although linear probes are preferred for musculoskeletal ultrasonographic examination of hips in infants (such as screenings), linear probes are approximately 5 cm long and 1 cm wide and require a body surface contact area of approximately 5 cm2. Moreover, there was only a small opening on each side of the medial hip in children treated with a spica cast after closed or open reduction. The front of the rod-shaped intracavity probe is circular with a diameter of approximately 2 cm, which requires a much smaller surface contact area than the linear probe and a lower requirement on the shape of the spica cast opening. If a linear probe is used to obtain a view of the acetabulum coronal mid sectional plane to observe the relationship between the femoral head and the acetabulum and to measure the distance, the probe must be placed horizontally with a large cast opening. Intracavity probes can overcome this shortcoming. In addition, based on the characteristics including broad-spectrum and extensive bandwidth, the intracavitary probe is the most suitable probe to observe the relationship between the femoral head and the acetabulum in the scanning of the medial hip with spica cast (see the Methods section).
Third, a TFD greater than 10 mm was set as the uncertain group. When the TFD was more than 10 mm, although the femoral head could be seen in the acetabulum coronal mid sectional plane, the distance between the femoral head and the acetabulum was large. It is also necessary to evaluate dislocation or reduction based on the diagonal relationship between the femoral head and the center of the acetabulum, as well as the AP position of the femoral head and the acetabulum (the maximum diameter of the femoral head is located in the middle coronal section of the acetabulum, the ischial ramus section, or the ischial tuberosity section). Therefore, an MRI was needed to determine the reduction of the femoral head when the TFD was greater than 10 mm. In this situation, it is difficult to judge whether the femoral head is dislocated laterally, and it is better to perform an MRI to ensure the related position of the femoral head and acetabulum.
Discussion of Key Findings
We found ultrasound to be considerably more reliable than plain radiography in terms of ascertaining whether a hip has remained reduced in a spica cast after open or closed reduction in patients with DDH. First, AP radiography provides only frontal plane images. When the femoral head is dislocated behind the acetabulum in a spica cast, the overlapping effect of radiography may lead to misjudgment of the alignment of the femoral head and acetabulum on AP radiography (Fig. 6). However, when the femoral head is too close to the acetabulum, the surgeon might not be sure whether the reduction is successful or whether the femoral head is dislocated and posteriorly displaced (Fig. 7). In addition, when the femoral head is far from the acetabulum, it might be considered to have an uncertain or dislocated status (Fig. 8). Radiography involves planar images, whereas an ultrasound probe can be moved up and down the coronal sections of the pubis, cartilage, and ischium to obtain information on the coronal and cross-sectional planes. This method achieved the same effect as cross-sectional MRI to avoid missed diagnoses because of the examination of a single two-dimensional image. Furthermore, obtaining a standard AP radiograph demands that the hip be perpendicular to the source of radiation, but sometimes it is difficult to obtain a suitable position because the patient is in a spica cast. A nonstandard AP radiograph will provide false information and increase the difficulty of verifying the related position of the femoral head and acetabulum. Second, the femoral head is not visible on radiography until ossification occurs. Therefore, radiography cannot be used to determine the position of the femoral head in young children and may sometimes lead to false-positive and false-negative diagnoses [1, 22]. When the cast image interferes with the hip image, it can be more difficult to locate the femoral head on radiography. Ultrasound has a strong advantage in revealing cartilage in this age group. Third, ultrasound is repeatable.
Fig. 6.
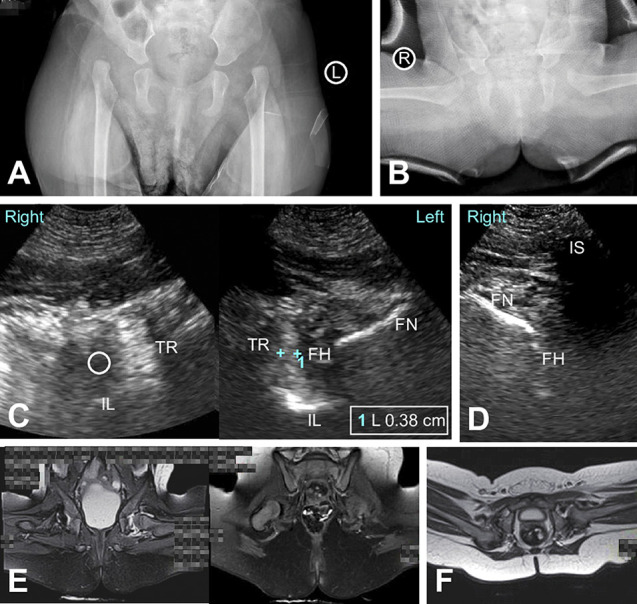
A-F An 11-month-old female with a bilaterally dislocated hip underwent closed reduction and spica cast immobilization. (A) A preoperative AP radiograph of the pelvis shows bilateral hip dislocation. (B) A postoperative AP radiograph shows bilateral hip reduction. (C) Hip medial ultrasound after reduction shows that the left hip was reduced (TFD = 3.8 mm), the right hip was dislocated, and the femoral head could not be seen in the acetabulum coronal midsectional plane (“○” indicates that the femoral head was not in the acetabulum). (D) Hip medial ultrasound after reduction shows that the right femoral head is in the ischial tuberosity coronal plane and was dislocated behind the acetabulum. (E) A postoperative MR image of the coronal midsectional plane shows that the left hip was reduced and the right hip was dislocated, and ischial tuberosity in the coronal plane shows that the right femoral head was dislocated toward the back of the acetabulum. (F) A postoperative MR image in the axial plane shows dislocation of the right femoral head toward the posterior acetabulum; IL = ilium (bony acetabular roof); TR = triradiate cartilage; FH = femoral head; FN = femoral neck; IS = ischium.
Fig. 7.
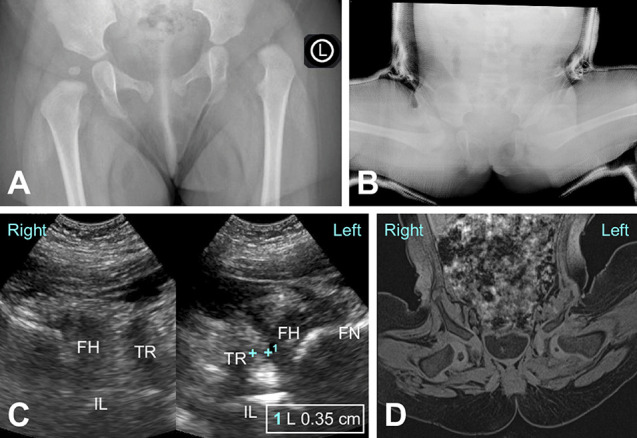
A-D A 9-month-old female had a dislocated left hip after open reduction and spica cast immobilization. (A) An intraoperative AP radiograph of the pelvis before reduction shows left hip dislocation. (B) A postoperative AP radiograph shows an uncertain left hip reduction status because the femoral head was too close to the acetabulum. (C) Hip medial ultrasound after reduction shows that the left hip was reduced (left hip TFD = 3.5 mm). (D) A postoperative MR image in the coronal midsectional plane shows that the hip was reduced; IL = ilium (bony acetabular roof); TR = triradiate cartilage; FH = femoral head; FN = femoral neck.
Fig. 8.
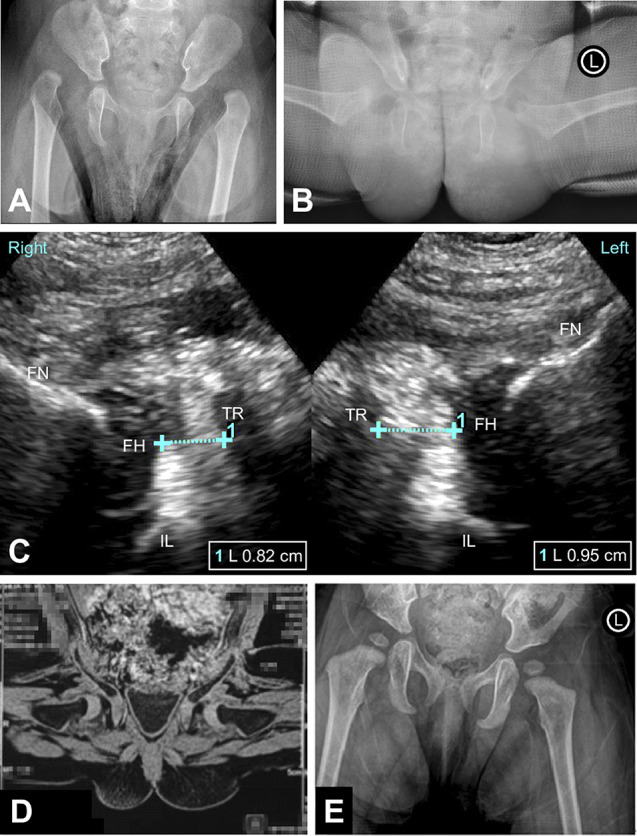
A-E A 7-month-old female had bilaterally dislocated hips after open reduction and spica cast immobilization. (A) An intraoperative AP radiograph of the pelvis before reduction shows bilateral hip dislocation. (B) A postoperative AP radiograph shows that both hips have an uncertain status because the femoral head was far from the medial wall of the acetabulum. (C) Hip medial ultrasound after reduction shows that both hips were reduced (left hip TFD = 9.5 mm; right hip TFD = 8.2 mm). (D) A postoperative MR image in the coronal midsectional plane shows bilateral hip reduction. (E) At 9 months postoperatively, an AP radiograph at the clinical follow-up visit shows bilateral hip reduction; IL = ilium (bony acetabular roof); TR = triradiate cartilage; FH = femoral head; FN = femoral neck.
In this study, we used hip medial ultrasound to identify the acetabulum coronal mid sectional plane, measure the TFD, and quantify the relative positions of the femoral head and acetabulum to determine the reduction status more accurately. As an index, in a previous study [23], the TFD was confirmed to have good consistency on the acetabulum coronal mid sectional plane by ultrasound and on the median coronal plane by MRI. We set the TFD threshold for reduced and uncertain-status hips as 10 mm to quantify hip reduction. The 10-mm threshold was derived from a classic article which reported that the width of the medial dye pool for good or adequate reduction was less than 7 mm [13]. The TFD and medial dye pool represent the distance between the femoral head and acetabulum, whereas the medial dye pool is the region where contrast passes between the femoral head and acetabulum, not including the interposed soft tissue fat or other components. However, the TFD includes acetabular components, such as the pulvinar fat pad; thus, the threshold was increased from 7 mm to 10 mm. Our results showed that for patients with TFDs less than 10 mm according to ultrasound, the classifications were consistent with those judged by MRI, indicating that the threshold of 10 mm with hip medial ultrasound prevents missed diagnoses and excludes false negatives. Therefore, hip medial ultrasound can be used as an imaging method for the preliminary assessment of hip reduction instead of radiography. Hip medial ultrasound can accurately evaluate reduction when the TFD is less than 10 mm, and no other imaging methods such as MRI are required. MRI is recommended only when the TFD is more than 10 mm.
We believe there are several reasons why ultrasound outperformed plain radiography in assessing the status of dysplastic hips after reduction and casting. First, ultrasound has no radiation risk. Second, parents can accompany and comfort their children during an ultrasound examination. Third, ultrasound is more reliable than plain radiography in ascertaining whether a hip has remained reduced in a spica cast, as mentioned previously. Hip medial ultrasound has several unique characteristics compared with other ultrasound methods in this field. First, there is no need for a large open window in casting. Second, the acetabulum coronal mid sectional plane could be identified and the TFD could be measured, allowing a quantitative evaluation to be conducted with this method. Moving the probe up and down allows the surgeon to observe the femoral head on different planes, to determine whether the TFD is the closest distance between the femoral head and the medial wall of the acetabulum that can be judged, and to assess whether the diameter of the femoral head is the largest on the acetabulum coronal mid sectional plane, which would indicate good reduction of the femoral head. We suggest that this hip medial ultrasound method be initiated with outpatient patients who have undergone harness treatment because the position of patients in a harness is similar to the position of patients in a spica cast. In addition, we recommend using hip medial ultrasound during outpatient follow-up visits for patients treated with hip reduction and cast immobilization.
Conclusion
After hip reduction and cast immobilization, hip medial ultrasound can directly show the femoral head and acetabulum. Hip medial ultrasound is more reliable than radiography as a preliminary evaluation method, and there is no irradiation. Based on our findings, we recommend using hip medial ultrasound during outpatient follow-up visits for patients treated with hip reduction and cast immobilization.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Ethical approval for this study was obtained from Beijing Jishuitan Hospital, Beijing, China (number 202105-05).
The first two authors contributed equally to this manuscript.
References
- 1.Barrera CA, Cohen SA, Sankar WN, Ho-Fung VM, Sze RW, Nguyen JC. Imaging of developmental dysplasia of the hip: ultrasound, radiography and magnetic resonance imaging. Pediatr Radiol. 2019;49:1652-1668. [DOI] [PubMed] [Google Scholar]
- 2.Beek FJA, Nievelstein RJ, Pruijs HE, de Jong PA, Sakkers RJB. Transinguinal sonographic determination of the position of the femoral head after reposition and follow-up in a spica cast. Pediatr Radiol. 2010;40:1794-1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper A, Evans O, Ali F, Flowers M. A novel method for assessing postoperative femoral head reduction in developmental dysplasia of the hip. J Child Orthop. 2014;8:319-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dibello D, Odoni L, Pederiva F, Di Carlo V. MRI in post reduction evaluation of developmental dysplasia of the hip. J Pediatr Orthop. 2019;39:449-452. [DOI] [PubMed] [Google Scholar]
- 5.Eberhardt O, Zieger M, Langendoerfer M, Wirth T, Fernandez FF. Determination of hip reduction in spica cast treatment for DDH: a comparison of radiography and ultrasound. J Child Orthop. 2009;3:313-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flack VF, Afifi AA, Lachenbruch PA, Schouten HJA. Sample size determinations for the two rater kappa statistic. Psychometrika. 1988;53:321-325. [Google Scholar]
- 7.Fleiss JL. Measuring nominal scale agreement among many raters. Psychological Bulletin. 1971;76:378. [Google Scholar]
- 8.Jadhav SP, More SR, Shenava V, Zhang W, Kan JH. Utility of immediate postoperative hip MRI in developmental hip dysplasia: closed versus open reduction. Pediatr Radiol. 2018;48:1096-1100. [DOI] [PubMed] [Google Scholar]
- 9.Litvin TV, Bresnick GH, Cuadros JA, Selvin S, Kanai K, Ozawa GY. A revised approach for the detection of sight-threatening diabetic macular edema. JAMA Ophthalmol. 2017;135:62-68. [DOI] [PubMed] [Google Scholar]
- 10.Maranho DA, Bixby SD, Miller PE, et al. What is the accuracy and reliability of the peritubercle lucency sign on radiographs for early diagnosis of slipped capital femoral epiphysis compared with MRI as the gold standard? Clin Orthop Relat Res. 2020;478:1049-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mehdizadeh M, Dehnavi M, Tahmasebi A, et al. Transgluteal ultrasonography in spica cast in postreduction assessment of developmental dysplasia of the hip. J Ultrasound. 2020;23:509-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ömeroğlu H. MRI after operative reduction for developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:556. [PubMed] [Google Scholar]
- 13.Race C, Herring JA. Congenital dislocation of the hip: an evaluation of closed reduction. J Pediatr Orthop. 1983;3:166-172. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum DG, Servaes S, Bogner EA, Jaramillo D, Mintz DN. MR imaging in postreduction assessment of developmental dysplasia of the hip: goals and obstacles. Radiographics. 2016;36:840-854. [DOI] [PubMed] [Google Scholar]
- 15.Smith BG, Kasser JR, Hey LA, Jaramillo D, Millis MB. Postreduction computed tomography in developmental dislocation of the hip: part I: analysis of measurement reliability. J Pediatr Orthop. 1997;17:626-630. [DOI] [PubMed] [Google Scholar]
- 16.Stock C, Hielscher T. DTComPair: comparison of binary diagnostic tests in a paired study design. R package version 1.0.3. Available at: https://mran.microsoft.com/snapshot/2017-04-22/web/packages/DTComPair/index.html. Accessed September 28, 2016. [Google Scholar]
- 17.Teng JB, Yu CW, Wang YZ, Mu KX. Sonographic detection of unilateral hip dislocation in a spica cast after closed reduction for developmental dysplasia of the hip. J Ultrasound Med. 2012;31:827-831. [DOI] [PubMed] [Google Scholar]
- 18.Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health. 2017;5:307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Douveren FQMP, Pruijs HEH, Sakkers RJB, Nievelstein RAJ, Beek FJA. Ultrasound in the management of the position of the femoral head during treatment in a spica cast after reduction of hip dislocation in developmental dysplasia of the hip. J Bone Joint Surg Br. 2003;85:117-120. [DOI] [PubMed] [Google Scholar]
- 20.Vaquero-Picado A, González-Morán G, Garay EG, Moraleda L. Developmental dysplasia of the hip: update of management. EFORT Open Rev. 2019;4:548-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang S, Zusman N, Lieberman E, Goldstein RY. Developmental dysplasia of the hip. Pediatrics. 2018;143:e20181147. [DOI] [PubMed] [Google Scholar]
- 22.Yong B, Li Y, Li J, et al. Post-operative radiograph assessment of children undergoing closed reduction and spica cast immobilization for developmental dysplasia of the hip: does experience matter? Int Orthop. 2018;42:2725-2731. [DOI] [PubMed] [Google Scholar]
- 23.Yu J, Duan F, Guo W, et al. Consistency of indices obtained via hip medial ultrasound and magnetic resonance imaging in reduction and spica cast treatment for developmental dysplasia of the hip. Ultrasound Med Biol. 2021;47:58-67. [DOI] [PubMed] [Google Scholar]


