Abstract
Context:
The 2014 Improving Medicare Post-Acute Care Transformation (IMPACT) Act systemized audits of long hospice stays, and the 2016 two-tier payment system decreased daily reimbursement rates after 60 days of enrollment. Both aimed to reduce long stays.
Objective:
Examine how live discharge rates and length-of-stay changed in relation to the policies.
Methods:
We computed monthly hospice-level percent live discharges and length-of-stay using 2008–2019 Medicare hospice claims. We compared pre-policies trends and post-policies trends overall, within Alzheimer’s disease and related dementias (ADRD) patients, within lung cancer patients, and stratified by hospice ownership (for-profit vs. non-profit/government-owned).
Results:
We included 10,539,912 and 10,453,025 episodes of care in the analytical samples for live discharge and length-of-stay analyses, respectively. Overall percent live discharges declined during the pre-policies period (−0.13 percentage-points per month, 95% CI: −0.14, −0.12), but exhibited no significant change during the post-policies period. Trends were driven primarily by for-profits, with similar patterns within ADRD and lung cancer patients. Overall, mean length-of-stay increased over time, with greater rate of increase during the post-policies period (0.41 days per month, 95% CI: 0.39, 0.42) compared to the pre-policies period (0.12 days per month, 95% CI: 0.10, 0.14). Length-of-stay increased faster among ADRD patients, but changed minimally for lung cancer patients.
Conclusions:
Live discharge rates declined significantly during the pre-policies period, but plateaued after implementation of the policies, driven by changes in for-profits. However, the policies did not reduce length-of-stay, which increased at faster rates, suggesting that post-policies excess live discharges were not restricted to long-stay patients.
Keywords: Medicare, hospice, end-of-life care, Alzheimer’s disease and related dementias
INTRODUCTION
Medicare is the primary insurer for decedents 65 years and older, and the primary payer for hospice in the United States. The hospice benefit is available to beneficiaries with an expected prognosis of 6 months or less.1 The incidence of long hospice stays (> 180 days) and associated costs to Medicare has increased in recent years,1 prompting concerns around potentially inappropriate and financially-motivated patient selection practices favoring patients with longer projected hospice stays, which were more profitable under the previously-used flat per-diem payment system.2–5 Two recent policy changes were enacted to discourage long stays: the 2014 Improving Medicare Post-Acute Care Transformation (IMPACT) Act that systemized audits of hospices with high proportion of long stays, and the 2016 implementation of a two-tiered payment system that reduced per-diem rates after the first 60 days of a stay.3–5 We hypothesized that providers may have responded by reducing census length-of-stay (LOS) through two strategies: (1) patient selection at admission to preferentially admit short-stay patients by delaying or denying eligibility to those with expected longer stays, and (2) live discharging long-stay patients on the basis that they are no longer terminally-ill.
Provider-initiated live discharges have been linked to financial motives. They can disrupt care continuity, increase hospitalizations and emergency room visits, and reduce quality-of-life for patients and families.6–11 Similarly, evidence suggests that timely access to hospice services and moderately long durations of hospice care are more beneficial and confer higher satisfaction than late admissions and short hospice stays.12–25 Thus, reductions in LOS achieved through delayed/missed admissions and/or increased live discharges may be detrimental to patient care.
Our goal was to describe trends in live discharges and patient LOS in relation to the 2014 IMPACT Act and the 2016 payment change using Medicare hospice claims from 2008–2019. Additionally, because we expected more pronounced policy responses (increased live discharges and reduced LOS) in for-profit hospices than in non-profit/government-owned hospices, as well as in patients with higher likelihood of long stays, we also examined these outcomes stratified by hospice ownership, as well as within two specific patient groups: (i) Alzheimer’s and related dementias (ADRD) patients, who historically have the longest LOS of all patient groups and who comprise a rapidly growing portion of the hospice and of the general aging population, and (ii) lung cancer patients, representing a sizable population in hospice with consistently short LOS.26–29
METHODS
Data sources
To assess trends in live discharges and patient LOS, we used the 100% Medicare hospice limited dataset (LDS) files spanning 2008–2019, containing ICD-9/ICD-10 diagnosis codes indicating patient primary and contributing terminal diagnoses, service dates, and discharge status (alive or deceased). We used the 100% master beneficiary summary file (MBSF) records to obtain beneficiaries’ demographic and death date information. We used publicly-accessible CMS provider-of-service (POS) files to gather information on hospice ownership status (for-profit vs. non-profit/government; freestanding vs. affiliated with another institution), and employee volume. Finally, we compiled hospice county characteristics from Census data and the Area Health Resources Files (AHRF), including total population, average household income, total number of practicing physicians, rural-urban continuum classification, and percent of county residents who were below the federal poverty level, non-Hispanic White, non-Hispanic Black, Hispanic, male, age 65+, and age 85+.
Study samples and outcomes
We identified unique, eligible hospice care episodes as in our prior work (Appendix 1).30 Patient subgroups were identified using primary or secondary ICD-9/ICD-10 codes indicating ADRD (Appendix Table 1) and lung cancer (Appendix Table 2).31 To avoid overlapping contributing diagnoses, we excluded patients with concurrent ADRD and lung cancer within the first five ICD codes in subgroup analyses.
We included episodes with non-missing discharge status that ended between July 2008 and September 2019 (N=10,539,912) for live discharge analyses, and episodes that had overlap with dates between January 2010 and December 2019 (N=10,453,025) for LOS analyses. We then computed monthly outcomes to facilitate granular examination of trend changes over time, and particularly between policies, which were enacted in close proximity. For each hospice, we computed the percent of care episodes ending each month that resulted from a live discharge. We then constructed a monthly “running LOS” metric by identifying all care episodes with at least one day of care provided in each month. For episodes ending during a given month, we computed LOS as the number of days between the episode start and end dates; for episodes that extend beyond the given month, we computed LOS as number of days between the episode start date and the last day of the month. We summarized monthly LOS at the hospice-level as: (i) mean LOS (winsorized at the 95th percentile), (ii) percent stays exceeding 60 days, and (ii) percent stays exceeding 180 days.
Statistical analyses
While we focus on the influence of two policy changes – the October 2014 IMPACT Act and the January 2016 payment change – we also acknowledge a third policy change that may have influenced our outcomes of interest: the May 2013 notice to eliminate failure-to-thrive (FTT) and debility as qualifying hospice diagnoses.29 We expected that the short time between implementation of these policies may not allow us to identify unique effects, and confirmed lack of sharp intercept changes at the time of individual policies in exploratory data analyses. Thus, we modelled trends in live discharge and LOS before (up to May 2013, the “pre-policies period”), during (June 2013 to December 2015), and after (January 2016 onward, the “post-policies period”) the set of three policy changes. Specifically, we modelled continuous trends in a pre-policies and post-policies periods using linear functions, but provide month-by-month characterization of changes to our outcomes during the June 2013-December 2015 period using monthly indicators, as follows:
where h indexes hospices, c indexes counties, and t indexes time in months. t_prePolicy and t_postPolicy are linear time splines for estimating pre- and post-policies trend slopes; i_PolicyChange represents a series of binary indicators for each calendar month during the period of policy change. Additionally, we included i_postPolicy as a binary variable to allow for intercept discontinuities at the start of the post-policies period. We adjusted for time-varying county-characteristics (C), time-varying hospice-characteristics (H), non-time-varying hospice characteristics (hospice-fixed effects (σ)), as well as seasonality (monthly indicators (γ)). We ran this model in our full sample, our ADRD and lung cancer subsamples, and after stratifying by hospice ownership.
Sensitivity analyses
We conducted subset analyses using up to the first four ICD codes to identify ADRD and lung cancer patients. We then repeated our analyses excluding government-owned hospices and hospices newly entering or exiting the market during the analytical period, which may behave differently from other hospices. We repeated our live discharge analyses excluding data from 2008–2009 due to the use of quarter indicators (rather than exact dates) in the claims, and with imputation for missing live discharge status (0.95% of episodes) using claim end dates and MBSF death dates. We also repeated mean LOS analyses after winsorizing at the 99th percentile to test for potential differential effects at the highest end of the LOS distribution. Finally, because care episode day counts only reset with a re-admission that occurs at least 60 days after a prior discharge, we used an alternate episode identification strategy for LOS analyses requiring a >60 day break in claims to constitute a new unique episode for a given beneficiary-provider ID pair.
This study was approved by the George Washington University Institutional Review Board. Analyses were conducted in SAS 9.4 and Stata 15.
RESULTS
Patient and hospice characteristics of eligible episodes in live discharge analyses are summarized in Table 1. Substantially more care episodes were provided to ADRD patients (N=2,273,272) than to lung cancer patients (N=746,337) during the analytical period. Compared to lung cancer patients, ADRD patients were older, less likely male, and more likely admitted at for-profit hospices. Non-profit/government-owned and for-profit hospices provided a similar number of episodes of care. However, compared to for-profits, non-profit/government-owned hospices admitted higher proportion of non-Hispanic white patients, and provided more care in urban counties and in the Northeast and Midwest. Patient and hospice characteristics of eligible hospice episodes used in the LOS analyses were similar to those used in the live discharge analyses overall, and within groups defined by diagnostic criteria (ADRD and lung cancer) and by hospice profit status. (Appendix Table 3).
Table 1.
Summary of patient characteristics and hospice characteristics across eligible hospice episodes in live discharge analyses
| Full sample | ADRD | Lung/trachea cancer | Non-profit/government-owned | For-profit | |
|---|---|---|---|---|---|
| N | 10,539,912 | 2,185,076 | 804,194 | 5,401,820 | 5,138,092 |
| % of full sample | 20.7% | 7.6% | 51.3% | 48.8% | |
| Patient Characteristics | |||||
| Admission age, mean (SD) | 82.6 (8.5) | 85.8 (7.2) | 76.7 (7.4) | 82.5 (8.5) | 82.8 (8.5) |
| Male, % | 41.8% | 31.5% | 51.6% | 42.8% | 40.8% |
| Race/ethnicity | |||||
| Non-Hispanic white, % | 87.7% | 87.6% | 87.8% | 90.2% | 85.0% |
| Non-Hispanic Black, % | 7.9% | 8.0% | 8.3% | 6.3% | 9.6% |
| Hispanic. % | 1.7% | 2.0% | 1.0% | 1.1% | 2.4% |
| Other race, % | 2.7% | 2.5% | 2.8% | 2.5% | 2.9% |
| Had any MA coverage, % | 30.4% | 28.9% | 32.0% | 29.6% | 31.1% |
| Primary ADRD Dx, % | 20.8% | 100.0% | 0% | 18.0% | 23.7% |
| Primary lung/trachea cancer Dx, % | 7.8% | 0% | 100.00% | 9.0% | 6.6% |
| Hospice characteristics | |||||
| Ownership | |||||
| % For-profit | 48.7% | 55.6% | 40.8% | 0% | 100.0% |
| % Non-profit | 49.3% | 42.8% | 56.9% | 96.3% | 0% |
| % Government-owned | 1.9% | 1.6% | 2.2% | 3.7% | 0% |
| % Freestanding (not affiliated with another institution) | 78.8% | 82.2% | 75.3% | 67.3% | 90.9% |
| County characteristics | |||||
| Setting rurality | |||||
| % Metropolitan | 88.6% | 90.0% | 87.0% | 87.2% | 90.1% |
| % Urban | 11.0% | 9.6% | 12.6% | 12.5% | 9.4% |
| % Rural | 0.4% | 0.4% | 0.4% | 0.3% | 0.5% |
| Region | |||||
| % Northeast | 16.2% | 16.1% | 17.2% | 20.0% | 12.1% |
| % West | 20.2% | 20.9% | 17.5% | 17.6% | 22.9% |
| % South | 39.7% | 39.8% | 41.3% | 34.4% | 45.2% |
| %Midwest | 23.9% | 23.2% | 24.0% | 28.0% | 19.7% |
Abbreviations: ADRD=Alzheimer’s disease and related dementias; Dx = Diagnosis; MA=Medicare Advantage; SD=standard deviation
Overall Trends in Live Discharge Rates
During the pre-policies period, the monthly percent of live discharges declined at similar rates overall (−0.13 percentage points per month, 95% CI: −0.14, −0.12), within ADRD patients (−0.10 percentage points per month, 95% CI: −0.11, −0.09), and within lung cancer patients (−0.13 percentage points per month, 95% CI: −0.14, −0.11) (Figure 1, Table 2). These trends slowed significantly during the post-policies period, to no change over time overall, and slower rates of decline in ADRD (−0.03 percentage points per month, 95% CI: −0.04, −0.02) and in lung cancer patients (−0.04 percentage points per month, 95% CI: −0.05, −0.02) (Figure 1, Table 2). Month-to-month patterns during the period of policy changes suggest that notice to exclude FTT/debility was not associated with observable changes on the rate of decline in live discharges, which began plateauing after the IMPACT Act (Figure 1).
Figure 1.
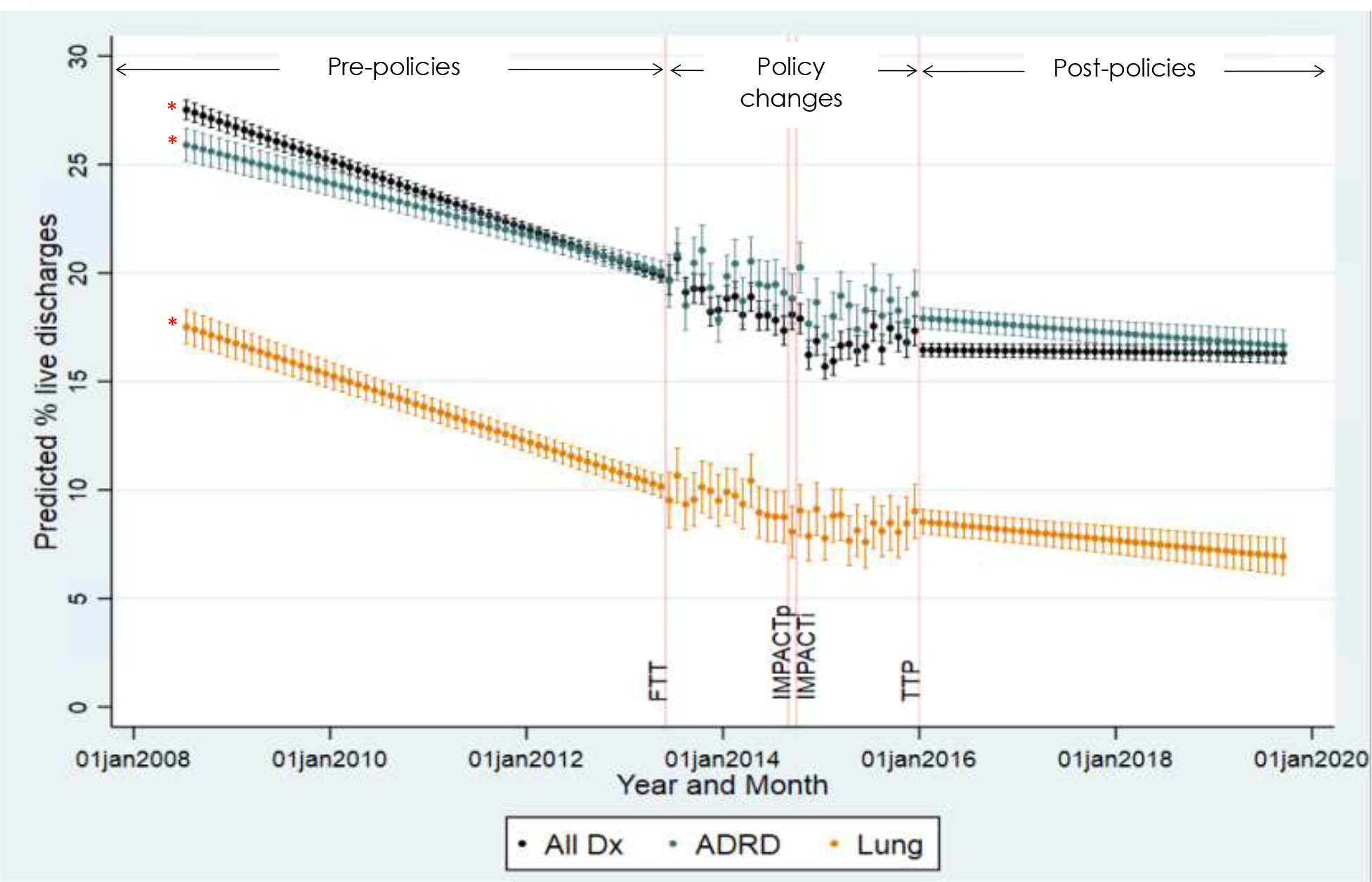
Predicted monthly percent of live discharges in all patients, patients with ADRD, and patients with lung/trachea cancer,a July 2008 – Sept 2019
Abbreviations: Dx=Diagnoses; FTT=Failure-to-thrive/debility exclusion notice; IMPACTp = IMPACT Act passage; IMPACTi = IMPACT Act implementation; TTP=two-tier pay implementation
a Predicted trends in this figure were estimated for the “average” hospice, by fitting fully adjusted models to each hospice-month observation, with time-varying hospice- (H) and county- (C) covariates set to the average sample values; additionally, month fixed effects coefficients were set to 0 in these computations in order to exclude seasonality effects and more clearly show trends over time. Red asterisks indicate statistically significant (p<0.05) differences between pre-policies and post-policies slopes.
Table 2.
Estimates of pre-policies (before May 2013) and post-policies (after January 2016) trends in live discharge and length-of-stay, overall, and within ADRD and lung cancer subsamplesa
| All patient diagnoses | ADRD | Lung cancer | ||||
|---|---|---|---|---|---|---|
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Percent live discharges | ||||||
| pre-policies slope | −0.13 (−0.14, −0.12) | <.001 | −0.10 (−0.11, −0.09) | <.001 | −0.13 (−0.14, −0.11) | <.001 |
| post-policies slope | 0 (−0.01, 0) | 0.409 | −0.03 (−0.04, −0.02) | <.001 | −0.04 (−0.05, −0.02) | <.001 |
| pre-policies vs. post-policies p-value b | <.001 | <.001 | <.001 | |||
| Mean length-of-stay | ||||||
| pre-policies slope | 0.12 (0.1, 0.14) | <.001 | 0.27 (0.23, 0.3) | <.001 | 0 (−0.02, 0.03) | 0.867 |
| post-policies slope | 0.41 (0.39, 0.42) | <.001 | 0.57 (0.54, 0.6) | <.001 | 0.02 (0, 0.04) | 0.077 |
| pre-policies vs. post-policies p-value b | <.001 | <.001 | 0.228 | |||
| Percent stays exceeding 60 days | ||||||
| pre-policies slope | 0.04 (0.03, 0.04) | <.001 | 0.04 (0.03, 0.05) | <.001 | 0.01 (−0.01, 0.03) | 0.571 |
| post-policies slope | 0.14 (0.14, 0.15) | <.001 | 0.13 (0.12, 0.14) | <.001 | 0.02 (0, 0.03) | 0.065 |
| pre-policies vs. post-policies p-value b | <.001 | <.001 | 0.37 | |||
| Percent stays exceeding 180 days | ||||||
| pre-policies slope | 0.04 (0.03, 0.04) | <.001 | 0.05 (0.04, 0.06) | <.001 | 0 (−0.01, 0.02) | 0.61 |
| post-policies slope | 0.14 (0.14, 0.15) | <.001 | 0.15 (0.14, 0.16) | <.001 | 0.02 (0, 0.03) | 0.013 |
| pre-policies vs. post-policies p-value b | <.001 | <.001 | 0.15 | |||
Abbreviations: ADRD=Alzheimer’s disease and related dementias; CI=confidence interval.
Estimated from models adjusted for month indicators + hospice fixed effects + hospice time-varying covariates (ownership (for-profit vs. non-profit, free-standing vs. affiliated), total registered nurses, total employees, monthly demographic distributions (age, gender, race/ethnicity) of new enrollees, monthly percent of total care days provided at the routine home care level and continuous home care level, and monthly percent of care days provided in the community/home setting, nonskilled long-term care setting, and skilled nursing home/inpatient setting) + county time-varying covariates (total population, percent population aged 65+ and 85+, gender and race/ethnicity distributions, number of active physicians, rural-urban setting, percent below poverty level, median household income)
p-values indicates whether the pre-policies slope and post-policies slope presented in the two preceding rows are significantly different, i.e. whether we can statistically reject H0: pre-policy slope − post-policy slope = 0.
Trends in Live Discharge Rates by Hospice Ownership
Trends in live discharge rates by hospice ownership generally mirrored overall trends, with some variation. Live discharge rates were consistently higher in for-profit hospices than in non-profit/government-owned hospices (Figure 2). Pre-policies vs. post-policies differences in monthly discharge trends were also more pronounced in for-profit hospices. For example, in for-profit hospices, overall rates of decline slowed from −0.16 percentage points per month (95% CI: −0.17, −0.15) during the pre-policies period to no significant change (0.01 percentage points per month, 95% CI: 0, 0.02) during the post-policies period (Figure 2, Appendix Table 4). Conversely, in non-profit/government-owned hospices, overall rates slowed from −0.10 (95% CI: −0.11, −0.08) to −0.04 (95% CI: −0.05, −0.02) percentage points per month (Figure 2, Appendix Table 4). Notably, within ADRD patients, rates of decline in live discharges were not significantly different between the pre- vs. post-policies periods in non-profit/government-owned hospices (Figure 2, Appendix Table 4).
Figure 2.
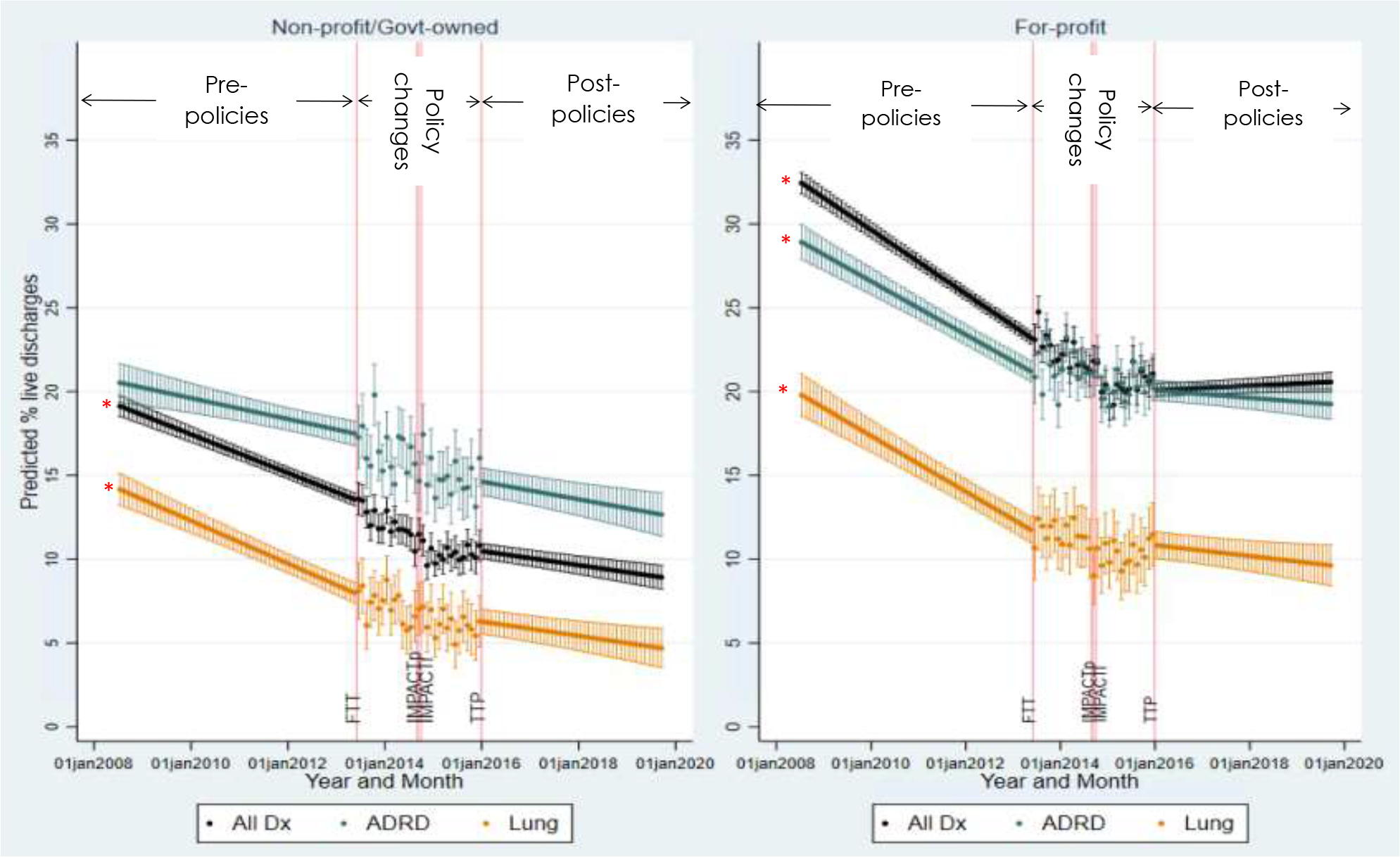
Predicted monthly percent of live discharges in all patients, patients with ADRD, and patients with lung/trachea cancer,a stratified by hospice ownership, July 2008 – September 2019
Abbreviations: Dx=Diagnoses; FTT=Failure-to-thrive/debility exclusion notice; IMPACTp = IMPACT Act passage; IMPACTi = IMPACT Act implementation; TTP=two-tier pay implementation
a Predicted trends in this figure were estimated for the “average” non-profit/govt-owned hospice and “average” for-profit hospice by fitting fully adjusted models to each hospice-month observation, with time-varying hospice- (H) and county- (C) covariates set to the average sample-specific values; additionally, month fixed effects coefficients were set to 0 in these computations in order to exclude seasonality effects and more clearly show trends over time. Red asterisks indicate statistically significant (p<0.05) differences between pre-policies and post-policies slopes.
Overall Trends in Patient LOS
Unlike live discharge rates, overall mean LOS increased in both the pre-policies and post-policies periods; however, rates of increase were significantly faster during the post-policies period (0.41 days per month, 95% CI: 0.39, 0.42) compared to the pre-policies period (0.12 days per month, 95% CI: 0.10, 0.14) (Figure 3, Table 2). Trends differed across our subgroups, with increases in LOS in both the pre-policies and post-policies periods among ADRD patients (pre-policies: 0.27 days per month, 95% CI: 0.23, 0.30; post-policies: 0.57 days per month, 95% CI: 0.54, 0.60), but no significant trend in either period among lung cancer patients (Figure 3, Table 2). ADRD LOS exhibited an immediate decline coinciding with notice to exclude FTT/debility, and stabilized after implementation of the IMPACT Act, before resuming an increasing trend following implementation of the two-tier payment (Figure 3).
Figure 3.
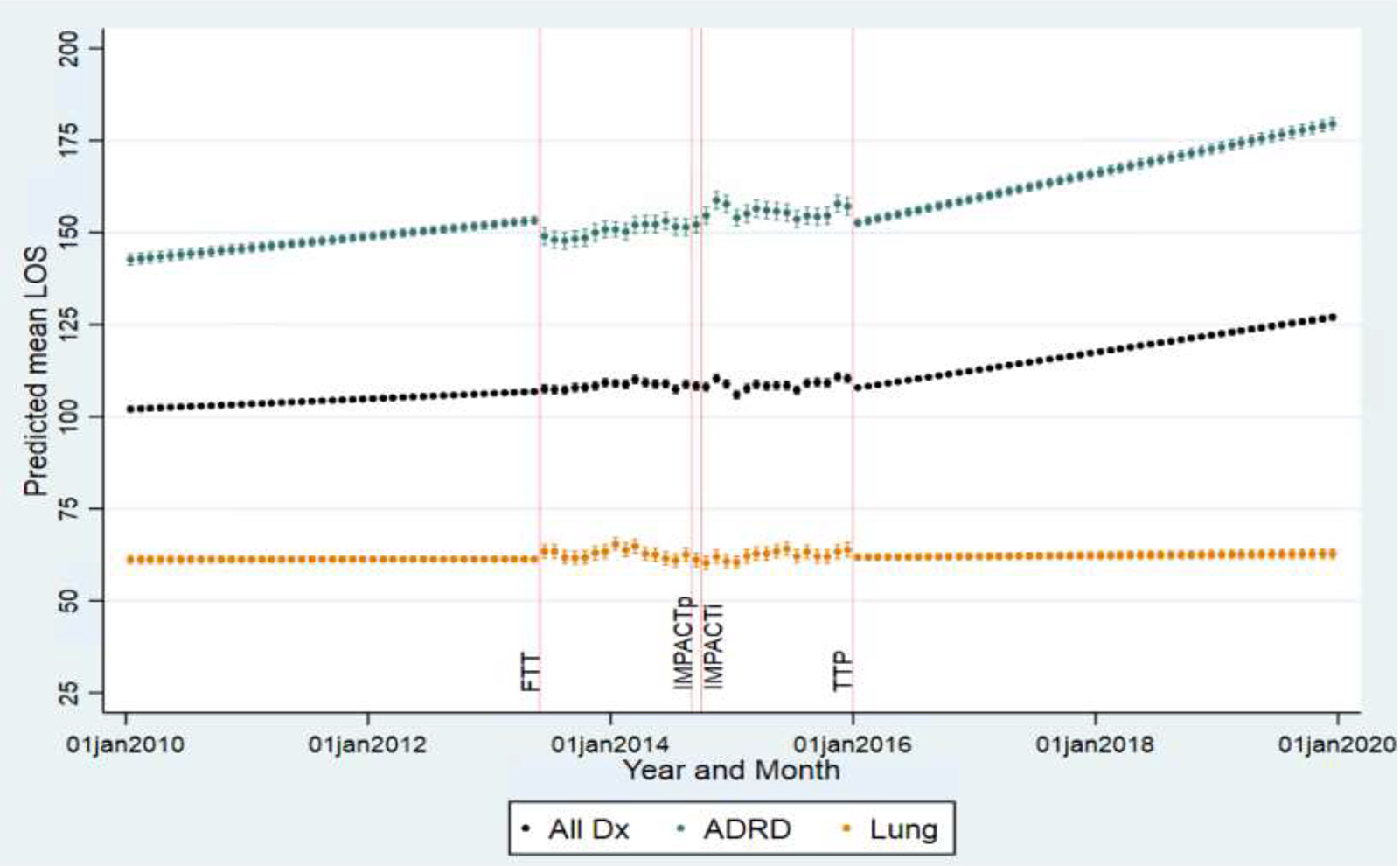
Predicted monthly mean length-of-stay in all patients, patients with ADRD, and patients with lung/trachea cancer,a January 2010 – December 2019
Abbreviations: Dx=Diagnoses; FTT=Failure-to-thrive/debility exclusion notice; IMPACTp = IMPACT Act passage; IMPACTi = IMPACT Act implementation; LOS=length-of-stay; TTP=two-tier pay implementation
a Predicted trends in this figure were estimated for the “average” hospice by fitting fully adjusted models to each hospice-month observation, with time-varying hospice- (H) and county- (C) covariates set to the average sample values; additionally, month fixed effects coefficients were set to 0 in these computations in order to exclude seasonality effects and more clearly show trends over time. Red asterisks indicate statistically significant (p<0.05) differences between pre-policies and post-policies slopes.
Trends in Patient LOS by Hospice Ownership
There were also pronounced differences in LOS trends by hospice ownership. Mean LOS was consistently higher in for-profit hospices compared to non-profit/government-owned for all diagnostic subgroups (Figure 4). Overall mean LOS also increased in for-profit hospices during the pre-policies period (0.23 days per month, 95% CI: 0.21, 0.26), while it declined in non-profit hospices (−0.07 days per month, 95% CI: −0.09, −0.04) (Figure 4, Appendix Table 5). However, both for-profit and non-profit/government-owned hospices exhibited significantly faster rates of increase for overall mean LOS in the post-policies period than in the pre-policies period (Figure 4, Appendix Table 5). These overall trends mask differences by qualifying diagnosis: for ADRD patients, mean LOS increased in both periods in both for-profit and hospice/government-owned hospices, although increases were more substantial in for-profit hospices (Figure 4, Appendix Table 5). Conversely, mean LOS declined for lung cancer patients at non-profit hospices but increased at for-profit hospices in the pre-policies period, with no evidence of significant changes in either hospice type in the post-policies period (Figure 4, Appendix Table 5). An immediate decline in ADRD LOS following notice to exclude FTT/debility was observed in both for-profit and non-profit/government-owned hospices (Figure 4), but only for-profits exhibited a temporary stabilization in ADRD LOS between IMPACT Act and two-tier pay implementation.
Figure 4.
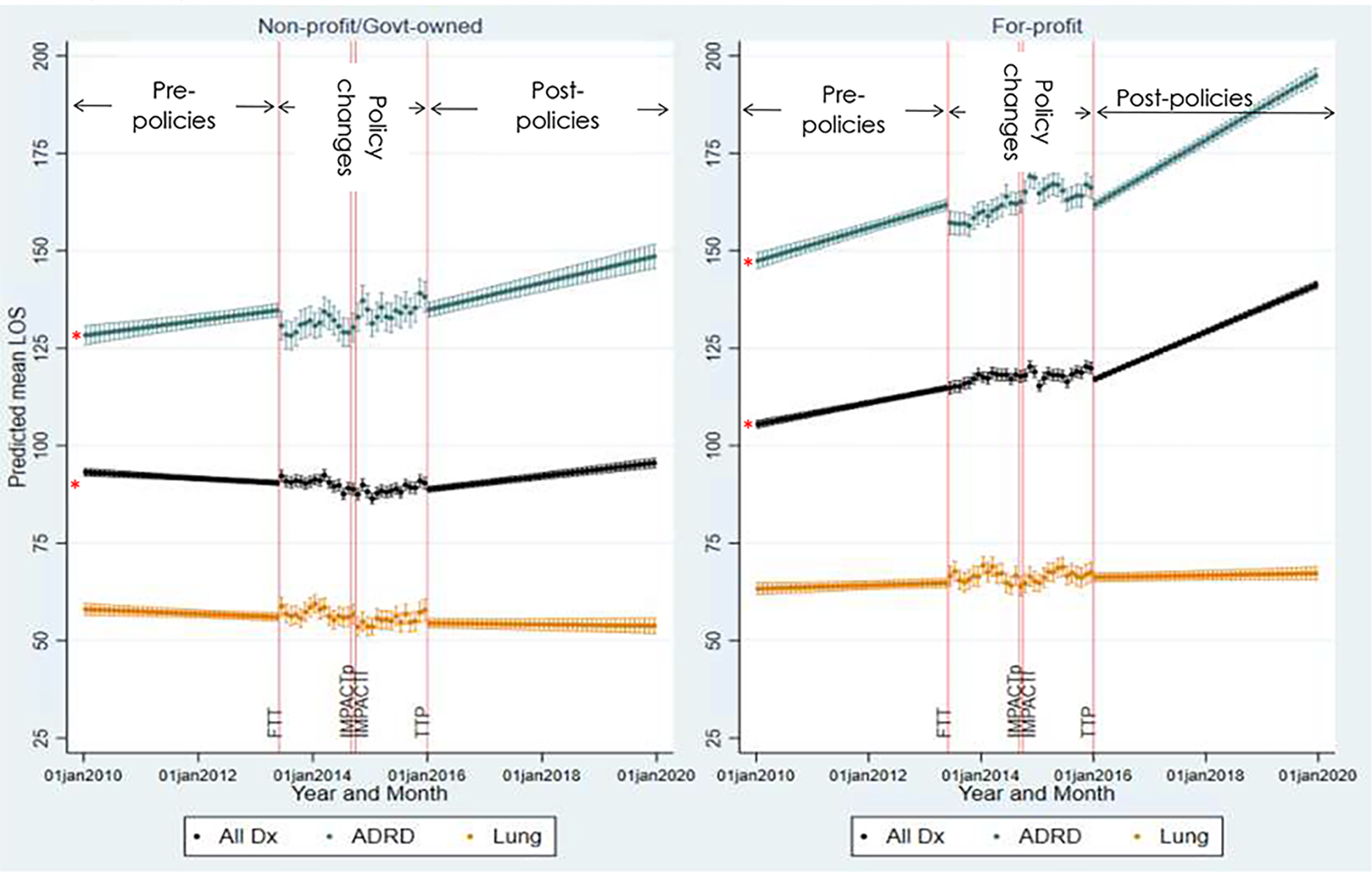
Predicted monthly mean length-of-stay in all patients, patients with ADRD, and patients with lung/trachea cancer,a stratified by hospice ownership, January 2010 – December 2019
Abbreviations: Dx=Diagnoses; FTT=Failure-to-thrive/debility exclusion notice; IMPACTp = IMPACT Act passage; IMPACTi = IMPACT Act implementation; LOS=length-of-stay; TTP=two-tier pay implementation
a Predicted trends in this figure were estimated for the “average” non-profit/govt-owned hospice and “average” for-profit hospice, by fitting fully adjusted models to each hospice-month observation, with time-varying hospice- (H) and county- (C) covariates set to the average sample-specific values; additionally, month fixed effects coefficients were set to 0 in these computations in order to exclude seasonality effects and more clearly show trends over time. Red asterisks indicate statistically significant (p<0.05) differences between pre-policies and post-policies slopes.
Patterns in the percent of stays exceeding 60 days and exceeding 180 days were similar to those for mean LOS (Appendix Figure 1, Appendix Figure 2, Table 2, Appendix Table 6).
Sensitivity analyses
All sensitivity analyses for live discharge were consistent with primary analyses (Appendix Table 7; Appendix Table 8). Sensitivity analyses in mean LOS and percent stays exceeding 60 and 180 days using alternate ADRD and lung cancer identification strategies (Appendix Table 7), excluding government-owned hospices, and using alternate episode identification (Appendix Table 9, Appendix Table 10) were also consistent with primary analyses. However, findings across all three measures of LOS differed when excluding hospices newly entering or exiting the market during the observation period: the rates of change in LOS during the post-policies period were similar to the those in the pre-policies period overall, and slower than those in the pre-policies period within ADRD patients (Appendix Table 9; Appendix Table 10). Finally, rates of change in mean LOS winsorized at the 99th percentile were faster than those in mean LOS primary analyses (winsorized at the 95th percentile), including a significant rate of increase within lung/trachea cancer patients during the post-policies period (Appendix Table 9).
DISCUSSION
This work found evidence of stabilization of hospice live discharges after implementation of regulatory and payment policy changes aimed to reduce long-stay patients in hospice. This change appeared to begin with implementation of the IMPACT Act and was driven by the behavior of for-profit hospices. Contrary to expectations, LOS rose at faster rates following policy changes compared to prior trends, regardless of hospice ownership. Given the rapid growth in hospice use that occurred during this time period (from 40% (over 1 million) of Medicare decedents in 2008 to 51.6% (close to 1.6 million) of Medicare decedents in 2019)1,32, the increased LOS indicates an outsized growth in the number of patients with long stays. Driven by these trends, Medicare hospice expenditures nearly doubled during this period, from $11 billion in 2008 to $20.9 billion in costs in 2019.1,32
The overall monthly percent of live discharges declined during the pre-policies period. The factors driving this decline have not been studied, but may include both financial and quality concerns: longer stays are financially beneficial, while live discharge is understood widely to reflect poor hospice quality. Overall live discharge rates subsequently plateaued after implementation of the IMPACT Act, and exhibited no further change over time in the post-policies period. This may reflect a relatively greater willingness by providers to discharge patients and mitigate risk of long stays, potentially involving organizational changes implemented in anticipation to or in response to the policy changes. Interestingly, though ADRD patients have substantially longer hospice stays than lung cancer patients, rates of change in live discharges were similar between the two groups in the pre- and post-policies periods, suggesting that drivers of change in live discharges affected patients across the distribution of LOS similarly. Consistent with existing evidence, rates of live discharge were higher in for-profit than in non-profit/government-owned hospices.33–35 However, the post-policies stabilization in live discharge rates appeared to be driven primarily by for-profit hospices, potentially due to a combination of greater risk-mitigation behavior and higher proportion of longer-stay patients.36–40
Monthly LOS increased over the analytical period overall and within ADRD patients. Contrary to expectations, LOS increased at significantly faster rates during the post-policies period than during the pre-policies period. Notably, there was an immediate decline in mean LOS among ADRD patients following notice to exclude FTT/debility. Because FTT/debility patients had historically lower LOS than ADRD patients,41,42 this is consistent with code-shifting from FTT/debility to ADRD.30 Additionally, the relatively stable lung cancer LOS over this time period indicates that the overall rising LOS was at least partially driven by changing patient mix toward greater proportion of longer-stay patients, such as those with ADRD, as shown in our prior work.30
Notably, when limited to hospices in operation throughout the observation period, there were no significant differences in overall LOS rate of change between the pre- and post-policies periods, and slower rate of increase in ADRD LOS during the post-policies than the pre-policies period. This suggests that the faster post-policies rate of increase observed in primary analyses was driven by new hospices entering after 2010. These were primarily for-profit agencies, which have longer average LOS.27 In contrast, the policies appeared to have slowed the rate of LOS growth in ADRD patients, and potentially other patient groups, within hospices that were in operation since 2010 or earlier. Finally, faster rates of increase in mean LOS winsorized at the 99th percentile relative to rates of increase in mean LOS winsorized at the 95th percentile suggest that LOS grew fastest at the highest end of the LOS distribution. Consistent with existing evidence, LOS was higher in for-profit hospices.34,35,40 However, despite some evidence to suggest that ADRD LOS temporarily stabilized at for-profit hospices in the months following the IMPACT Act, there was no evidence that the IMPACT Act or two-tier payment had any long-term effects on ADRD LOS. Notably, our findings on LOS trends are contrary to evaluation of the two-year period of heighted hospice audits under Clinton’s 1995 Operation Restore Trust (ORT), which found an associated 20% decrease in average hospice LOS.43,44 This divergence may be driven by differences in the hospice patient population, with primarily cancer patients in the 1990s vs. primarily non-cancer patients with longer end-of life trajectories in the 2010s,27,42,45 and/or differences in the hospice industry, comprising 5% for-profit agencies in 1990 vs. 56% and 71% for-profit agencies by 2010 and 2019;27,35 as evidenced in this analysis, long LOS at for-profit hospices appear to be more resistant to audits. Our findings also suggest that the two-tier payment structure does not sufficiently disincentivize long-stays financially. This is consistent with recent MedPAC reports, which noted that the new payment system has only “modestly” reduced profitability of long stays, citing ongoing concerns of associated “revenue-generating strategies” driving continued growth in profit margins and entries of for-profit agencies.1,46–49
Overall, this work suggests that the IMPACT Act and two-tier payment were associated with a plateauing in live discharge rates in for-profit hospices, which were on a declining trend during the pre-policies period. Because live discharges disrupt care continuity, reduce patient quality-of-life, and are burdensome to patient families,6–11,50,51 these findings may be associated with negative implications for end-of-life quality-of-care. Furthermore, there was no corresponding decline in LOS, which instead increased at faster rates in the post-policies period. This strongly suggests that the excess live discharges were occurring in patients across the spectrum of potential LOS, possibly due to the demonstrated low correlation between Medicare hospice patient eligibility guidelines and 6-month mortality.52 Importantly, further research is critical for better understanding the clinical implications of these findings, and how clinicians may better improve appropriate use of hospice care.
This timely analysis leveraged the 100% Medicare claims data, and findings are applicable to the whole Medicare population. However, our work has limitations. First, this is a descriptive analysis, and though we used similar techniques to an interrupted time-series analysis, we cannot strictly attribute causality due to the close proximity during which the three policies were introduced. We are also unable to attribute causality due to lack of a control group: observed post-policies changes in trends may have been confounded by other proximate or concurrent policy changes (including: implementation of the physician face-to-face recertification requirement (2011)53 and hospice quality reporting system (2012)54; elimination of non-specific dementia codes as primary diagnoses (2014);55 and the IMPACT Act’s increased frequency of routine hospice surveys (2015)4), or other concurrent drivers of utilization trends (e.g. changes in family/patient-initiated live discharges, changes in organizational structures, and changes in provider profit-seeking strategies resulting from entry of private equity and acquisitions of non-profits in the hospice industry56). Second, though LOS is a function of both admission timing and live discharge, we were unable to directly assess whether and how admissions timing and initial access barriers have changed in relation to the policies.
In summary, we found a declining trend in hospice live discharge rates between 2008 and 2013, which plateaued after implementation of the IMPACT Act and two-tier payment, driven primarily by changes in for-profit hospices. Importantly, however, neither policy had the intended effect of reducing long stays, as LOS increased at faster rates during the post-policies period. This suggests that the post-policies excess in live discharges were not restricted to patients who would have had longer LOS, and may potentially have important implications for clinical practice and patient outcomes. Additional research is necessary to better understand these considerations in the context of the large and growing ADRD decedent population,57 as well as the mechanisms through which hospices have responded to the IMPACT Act audits and two-tier payment in order to inform future Medicare hospice policy changes, particularly as they pertain to goals of reducing the proportion of long-stay patients.
Supplementary Material
Acknowledgements:
This work was funded by NIA grant 5R03AG061499-02, awarded to MCP.
Footnotes
Conflicts of Interest:
KZG reports current funding support from grants and contracts from NIH and CMS.
MCP has received research funding from NIH, DOD, and DC Health. She serves as a member of the Biogen Healthy Climate, Healthy Lives Scientific Advisory Council.
DL has received research funding from PCORI, the Gordon and Betty Moore Foundation, and the Fan Fox and Leslie R. Samuels Foundation, NIH, DOD, and DC Health. She serves on the executive committee of the Coalition for Supportive Care of Kidney Patients and on the advisory group of Monogram.
CPP has received research funding from NIH, AHRQ, and DC Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Medicare Payment Advisory Commission. Hospice services. In: Report to Congress: Medicare Payment Policy. Washington D.C.; 2021:307–350. [Google Scholar]
- 2.Medicare Payment Advisory Commission. Section 11: Other Services. In: July 2016: A Data Book - Healthcare Spending and the Medicare Program. Washington, D.C.; 2016:178–197. [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Implementation of the Hospice Payment Reforms. Medicare Learn Netw. 2015;MM9201:1–6. [Google Scholar]
- 4.113th Congress. Improving Medicare Post-Acute Care Transformation (IMPACT) Act. Public Law 113–185-Oct 6, 2014.:1–20. [Google Scholar]
- 5.Advisory Board. How hospices can prepare for increased federal audits under the IMPACT Act. https://www.advisory.com/daily-briefing/2014/11/07/how-hospices-can-prepare-for-increased-federal-audits-under-the-mpact-act. Published 2014.
- 6.Dolin R, Silberman P, Kirk DA, et al. Do live discharge rates increase as hospices approach their Medicare aggregate payment caps? J Pain Symptom Manage. 2017;In press; [DOI] [PubMed] [Google Scholar]
- 7.Wu S, Volker DL. Live Discharge From Hospice. J Hosp Palliat Nurs. 2019:1. doi: 10.1097/njh.0000000000000547 [DOI] [PubMed] [Google Scholar]
- 8.Dolin R, Hanson LC, Rosenblum SF, Stearns SC, Holmes GM, Silberman P. Factors Driving Live Discharge From Hospice: Provider Perspectives. J Pain Symptom Manage. 2017;53(6):1050–1056. doi: 10.1016/j.jpainsymman.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 9.Dolin R, Holmes GM, Stearns SC, et al. A positive association between hospice profit margin and the rate at which patients are discharged before death. Health Aff. 2017;36(7):1291–1298. [DOI] [PubMed] [Google Scholar]
- 10.Wladkowski SP. Live Discharge from Hospice and the Grief Experience of Dementia Caregivers. J Soc Work End-of-Life Palliat Care. 2016;12(1–2):47–62. [DOI] [PubMed] [Google Scholar]
- 11.Watson Campbell R Being Discharged from Hospice Alive: The Lived Experience of Patients and Families. J Palliat Med. 2015;18(6):495–499. doi: 10.1089/jpm.2014.0228 [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. Washington, D.C.: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 13.Schockett ER, Teno JM, Miller SC, Stuart B. Late referral to hospice and bereaved family member perception of quality of end-of-life care. J Pain Symptom Manage. 2005;30(5). doi: 10.1016/j.jpainsymman.2005.04.013 [DOI] [PubMed] [Google Scholar]
- 14.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families’ perceptions of services: are earlier hospice referrals better? J Am Geriatr Soc. 2005;53(5):819–823. doi: 10.1111/j.1532-5415.2005.53259.x [DOI] [PubMed] [Google Scholar]
- 15.MacKenzie MA, Buck HG, Meghani SH, Riegel B. Unique correlates of heart failure and cancer caregiver satisfaction with hospice care. J Pain Symptom Manage. 2016;51(1):71–78. doi: 10.1016/j.jpainsymman.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 16.Diamond EL, Russell D, Kryza-Lacombe M, et al. Rates and risks for late referral to hospice in patients with primary malignant brain tumors. Neuro Oncol. 2016;18(1):78–86. doi: 10.1093/neuonc/nov156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller SC, Kinzbrunner B, Pettit P, Williams JR. How does the timing of hospice referral influence hospice care in the last days of life? J Am Geriatr Soc. 2003;51(6):798–806. doi: 10.1046/j.1365-2389.2003.51253.x [DOI] [PubMed] [Google Scholar]
- 18.Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Sean Morrison R. Hospice enrollment saves money for medicare and improves care quality across a number of different lengths-of-stay. Health Aff. 2013;32(3). doi: 10.1377/hlthaff.2012.0851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar P, Wright AA, Hatfield LA, Temel JS, Keating NL. Family Perspectives on Hospice Care Experiences of Patients with Cancer. J Clin Oncol. 2017;35(4):432–439. doi: 10.1200/JCO.2016.68.9257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shega JW, Hougham GW, Stocking CB, Cox-Hayley D, Sachs GA. Patients Dying with Dementia: Experience at the End of Life and Impact of Hospice Care. J Pain Symptom Manage. 2008;35(5):499–507. [DOI] [PubMed] [Google Scholar]
- 21.Volicer L, Hurley A. Hospice Care for Patients with Advanced Progressive Dementia. New York, NY: Springer Publishing Company, Inc.; 1998. [Google Scholar]
- 22.Hendriks SA, Smalbrugge M, Hertogh CMPM, Van Der Steen JT. Dying with dementia: Symptoms, treatment, and quality of life in the last week of life. J Pain Symptom Manage. 2014;47(4):710–720. [DOI] [PubMed] [Google Scholar]
- 23.Broady TR, Saich F, Hinton T. Caring for a family member or friend with dementia at the end of life: A scoping review and implications for palliative care practice. Palliat Med. 2018:1–14. [DOI] [PubMed] [Google Scholar]
- 24.Solomon MZ, Jennings B. Palliative Care for Alzheimer Patientsl Implications for Institutions, Caregivers, and Families. In: Volicer L, Hurley A, eds. Hospice Care for Patients with Advanced Progressive Dementia1. New York, NY: Springer Publishing Company, Inc.; 1998:132–154. [Google Scholar]
- 25.Van Der Steen JT, Radbruch L, Hertogh CM, et al. White paper defining optimal palliative care in older people with dementia: A Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. 2014;28(3):197–209. [DOI] [PubMed] [Google Scholar]
- 26.Medicare Payment Advisory Commission. Section 11: Other Services. In: June 2012: A Data Book - Healthcare Spending and the Medicare Program. Washington D.C.; 2012:183–202. [Google Scholar]
- 27.Medicare Payment Advisory Commission. Section 11: Other Services. In: July 2021 Data Book. Washington, D.C.; 2021:183–204. [Google Scholar]
- 28.Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–1783. doi: 10.1212/WNL.0b013e31828726f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Department of Health and Human Services. Medicare Program; FY 2014 Hospice Wage Index and Payment Rate Update; Hospice Quality Reporting Requirements; and Updates on Payment Reform. Fed Regist. 2013;78(91):27923–27852. [PubMed] [Google Scholar]
- 30.Gianattasio KZ, Moghtaderi A, Lupu D, Prather C, Power MC. Evaluation of Federal Policy Changes to the Hospice Benefit and Use of Hospice for Persons With ADRD. JAMA Heal Forum. 2022;3(5):e220900. doi: 10.1001/jamahealthforum.2022.0900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas SK, Brooks SE, Mullins CD, Baquet CR, Merchant S. Use of ICD-9 coding as a proxy for stage of disease in lung cancer. Pharmacoepidemiol Drug Saf. 2002;11(8):709–713. doi: 10.1002/pds.759 [DOI] [PubMed] [Google Scholar]
- 32.Medicare Payment Advisory Commission. Hospice Services. In: Report to Congress: Medicare Payment Policy.; 2010:141–161. [Google Scholar]
- 33.Teno JM, Plotzke M, Gozalo P, Mor V. A National Study of Live Discharges from Hospice. J Palliat Med. 2014;17(10):1121–1127. doi: 10.1089/jpm.2013.0595 [DOI] [PubMed] [Google Scholar]
- 34.Stevenson DG, Grabowski DC, Keating NL, Huskamp HA. Effect of Ownership on Hospice Service Use: 2005–2011. J Am Geriatr Soc. 2016;64(5):1024–1031. doi: 10.1111/jgs.14093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aldridge MD, Schlesinger M, Barry CL, et al. National hospice survey results for-profit status, community engagement, and service. JAMA Intern Med. 2014;174(4):500–506. doi: 10.1001/jamainternmed.2014.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hunt M, Rezaee ME, Luallen J, et al. Medicare Hospice Payment Reform: A Review of the Literature (2013 Update). Report prepared for Medicare and Medicaid Services. [Google Scholar]
- 37.Gandhi SO. Differences between non-profit and for-profit hospices: Patient selection and quality. Int J Health Care Finance Econ. 2012;12(2):107–127. [DOI] [PubMed] [Google Scholar]
- 38.Huskamp HA, Buntin MB, Wang V, Newhouse JP. Providing care at the end of life: Do Medicare rules impede good care? Health Aff. 2001;20(3):204–211. [DOI] [PubMed] [Google Scholar]
- 39.Thompson JW, Carlson MDA, Bradley EH. US Hospice Industry Experienced Considerable Turbulence From Changes In Ownership, Growth, And Shift To For-Profit Status. Health Aff. 2012;31(6):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wachterman MW, Marcantonio ER, Davis RB, McCarthy EP. Association of Hospice Agency Profit Status With Patient Diagnosis, Location of Care, and Length of Stay. Jama. 2011;305(5):472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Medicare Payment Advisory Commission. Section 11: Other Services. In: June 2013: A Data Book - Healthcare Spending and the Medicare Program. Washington D.C.; 2013:185–205. [Google Scholar]
- 42.Medicare Payment Advisory Commission. Section 11: Other Services. In: June 2014: A Data Book - Healthcare Spending and the Medicare Program. Washington D.C.; 2014:177–197. [Google Scholar]
- 43.Morris GM. Hospice fraud and abuse: Operation Restore Trust and beyond. Am J Hosp Palliat Med. 2003;20(1):1–8. [Google Scholar]
- 44.Scanlon WJ. Testimony Before the Special Committee on Aging, U.S. Senate. MEDICARE: More Beneficiaries Use Hospice, Many Factors Contribute to Shorter Periods of. GAO. 2000. [Google Scholar]
- 45.Han B, Remsburg RE, McAuley WJ, Keay TJ, Travis SS. National trends in adult hospice use: 1991–1992 to 1999–2000. Health Aff. 2006;25(3):792–799. doi: 10.1377/hlthaff.25.3.792 [DOI] [PubMed] [Google Scholar]
- 46.Medicare Payment Advisory Commission. Hospice Services. In: Report to Congress: Medicare Payment Policy. Washington D.C.; 2017:315–342. [Google Scholar]
- 47.Medicare Payment Advisory Commission. Hospice services. In: Report to Congress: Medicare Payment Policy. Washington, D.C.; 2018:321–350. [Google Scholar]
- 48.Medicare Payment Advisory Commission. Hospice Services. In: Report to Congress: Medicare Payment Policy. Washington D.C.; 2019:309–340. http://www.medpac.gov/docs/default-source/reports/mar19_medpac_ch12_sec.pdf.
- 49.Medicare Payment Advisory Commission. Hospice services. In: Report to Congress: Medicare Payment Policy. Vol March.; 2020:1014. doi: 10.1111/j.1532-5415.1996.tb01887.x [DOI] [Google Scholar]
- 50.Clayton MF, Utz R, Iacob E, et al. Live hospice discharge: Experiences of families, and hospice staff. Patient Educ Couns. 2021;104(8):2054–2059. doi: 10.1016/j.pec.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hunt LJ, Harrison KL. Live discharge from hospice for people living with dementia isn’t “graduating”—It’s getting expelled. J Am Geriatr Soc. 2021;69(6):1457–1460. doi: 10.1111/jgs.17107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fine PG. Hospice Underutilization in the U.S.: The Misalignment of Regulatory Policy and Clinical Reality. J Pain Symptom Manage. 2018;56(5):808–815. doi: 10.1016/j.jpainsymman.2018.08.005 [DOI] [PubMed] [Google Scholar]
- 53.Public Law 111–148 - Mar. 23, 2010: An Act, Entitled The Patient Protection and Affordable Care Act. 111th Congr.:1–906. https://www.govinfo.gov/content/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf.
- 54.Centers of Medicare & Medicaid Services. Medicare program; hospice wage index for fiscal year 2012. Final rule. Fed Regist. 2011;76(150):47302–47352. [PubMed] [Google Scholar]
- 55.Centers of Medicare & Medicaid Services. CMS Manual System: Pub100–04 Medicare Claims Processing: Transmittal 3032. Dep Heal Hum Serv. 2014. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R3032CP.pdf.
- 56.Teno JM. Hospice Acquisitions by Profit-Driven Private Equity Firms. JAMA Heal Forum. 2021;2(9):e213745. doi: 10.1001/jamahealthforum.2021.3745 [DOI] [PubMed] [Google Scholar]
- 57.Weuve J, Hebert LE, Scherr PA, Evans DA. Deaths in the United States among persons with Alzheimer’s disease. Alzheimers Dement. 2014;10(2):e40–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


