Abstract
Background
This study aimed to develop an efficient interview sheet during pregnancy and screening tool to identify pregnant women needing social support at obstetric institutions. Moreover, we investigate the perinatal factors associated with the Edinburgh postnatal depression scale (EPDS).
Methods
This prospective cohort study was conducted at three medical institutions that commonly encounter cases with social issues. Pregnant women were assessed using an interview sheet at the first visit (n = 678), at approximately 28 weeks gestation (n = 495), 36 weeks gestation (n = 296), and the postpartum period (n = 822). We investigated the important items identified on the new screening questionnaire (NEW interview sheets) for women needing social support. The items on the interview sheet were scored by multiple linear regression analysis, and the cutoff values were calculated using the receiver operating characteristic curve. The association between perinatal factors and EPDS was assessed using multiple logistic regression analyses.
Results
The study included 166 cases for which all NEW interview sheets for all periods were available. NEW interview sheets and stepwise screening tools during the first and second trimester were developed in which 2.5% of pregnant women were identified as requiring social support, respectively. The factors associated with EPDS ≧ 9 were “Women who felt confused/troubled or did not feel anything to be pregnant” (adjusted odds ratio [aOR]: 6.51, 95% confidence interval [CI]: 1.62–26.15), “Maternal mental disorder” (aOR 4.38; CI 1.06–18.10), “Consultation request at first visit” (aOR 3.22; CI 1.09–9.45), and “Women who have difficulty or anxiety about pregnancy during the second trimester” (aOR 3.14; CI 1.29–7.67).
Conclusions
We created the NEW interview sheets and screening tools during the first and the second trimester. Future studies are needed to validate these screening tools.
Keywords: pregnant women, social support, interview sheet during pregnancy, screening tool, maternal mental health, child maltreatment
Introduction
Social problems during pregnancy and postpartum were important risk factors for child maltreatment (1, 2). Child maltreatment causes major public health problems not only in childhood but also until adulthood (3–5). Among the verified child abuse cases which resulted in death (6), children under 1 year of age accounted for about 50% of deaths due to childhood maltreatment, and half of them (25%) are within the first month of life. Previously reported background factors related to child maltreatment include unexpected/unplanned pregnancies, failure to receive pregnancy health checkups, failure to receive the Maternal and Child Health Handbook, and teenage pregnancies (6, 7). Other factors, such as unmarried mothers, maternal mental disorder, low educational achievement, a history of childhood abuse, deprivation, and low-birth-weight children have also been reported in association with child maltreatment (2, 7, 8). Therefore, early preventive efforts against child maltreatment taken during pregnancy and the postnatal period are extremely important. Identification of at-risk parents such as mother without social support, maternal mental illness, and teenager during pregnancy and early intervention resulted in a decrease in the rate of referrals to child protective centers (9). Understanding social and medical risk factors is an essential part of abuse prevention. Identifying social risk factors at the time of pregnancy and initiating support for pregnant women who need social support may help reduce child maltreatment.
Although there are many public health centers that identify pregnant women who need social support through questionnaires and interviews when issuing the Maternal and Child Health Handbook, success is limited due to few opportunities for contact with pregnant women. In Japan, pregnancy health checkups at obstetric institutions are scheduled at least 14 times, where the mother's health condition is assessed, and a medical examination and health guidance are provided. Health guidance addresses the mental health of pregnant women and relieving their anxiety about pregnancy, childbirth, and childcare. However, about half of the delivery facilities in Japan are private obstetric clinics, some of which are inadequate for resolving social and psychological problems in the affected population. This study aimed to develop a screening tool for detecting pregnant women in need of support that can be used in health guidance at all facilities, including private obstetric clinics. We investigated the items from the NEW interview sheets that were considered important by women identified to be in need of social support. The primary outcome was to develop an available interview sheet during pregnancy and the screening tool to detect pregnant women in need of support in collaboration with a public health center. A secondary outcome was to investigate the perinatal factors associated with EPDS.
Materials and methods
Study design
This was a prospective cohort study conducted at three medical institutions that were familiar with social issues such as unmarried mothers, poverty, maternal mental disorder or teenage pregnancies affecting pregnancy and childcare outcomes. Inclusion criteria in the study were pregnant women managed at the three medical institutions who consented to the study. There were no exclusion criteria.
Questionnaire and study procedures
We implemented the new screening questionnaire (NEW interview sheets) at the first visit, at approximately 28 weeks gestation, 36 weeks gestation, and the postpartum period. Table 1 provides an itemized list of question on the NEW interview sheets for each period. According to previous studies, variables to be used in the interview sheet were selected (2, 7, 10). These interviews were conducted at three medical institutions (Osaka Women's and Children's Hospital, Seibo Hospital, and Showa University Hospital) that actively identify pregnant women in need of support in collaboration with a public health center. In addition, the Edinburgh postnatal depression scale (EPDS) was administered together at one-month postpartum. We defined suspected postpartum depression as having an EPDS score of 9 or higher based on the results of a previous community study in Japan (11).
Table 1.
NEW interview sheets for each period.
| First visit | Positive | Negative |
|---|---|---|
| Maternal feelings toward being pregnant | Happy | Confused, Trouble, Did not feel anything to be pregnant |
| Partner's feelings toward being pregnant | Happy | Confused, Trouble, Did not feel anything to be pregnant |
| Depression symptoms | Nothing/Very few | Sometimes/Often |
| Family and social support | Yes | No |
| Economic status | No problem | Deprived/Need of public assistance |
| Partner's status | Married | Unmarried/Remarried |
| Maternal mental disorder | No | Yes |
| Illegal drug use by the mother | No | Yes |
| Illegal drug use by the partner | No | Yes |
| Worries about older child | No | Yes |
| Consultation request | No | Yes |
| Number of fetuses | Singleton pregnancies | Multiple pregnancies |
| Number of children (Exclusive of this pregnancy) | <3 | ≧3 |
| Maternal age | <25 | ≧25 |
| Second trimester | Positive | Negative |
| Maternity life | Almost happy | Difficulty/Anxiety |
| Talking with partner | Very often/Sometimes | Very few/Nothing |
| Partner violence | No | Yes |
| Worries about older child | No | Yes |
| Parent's own childhood abuse | No | Yes |
| Depression symptoms | Nothing/Very few | Sometimes/Often |
| Family and social support | Yes | No |
| Smoking | No/Discontinued after pregnant | Continued after pregnant |
| Alcohol use | No/Discontinued after pregnant | Continued after pregnant |
| Consultation request | No | Yes |
| Status of pregnancy health checkups | Usual | Less/Unscheduled |
| Third trimester | Positive | Negative |
| Depression symptoms | Nothing/Very few | Sometimes/Often |
| Worries about older child | No | Yes |
| Concerns about the course of pregnancy | No | Yes |
| Family and social support | Yes | No |
| Childbirth preparation | Almost finished | Unfinished |
| Consultation request | No | Yes |
| Pregnancy health checkups | Usual | Less/Unscheduled |
| Fetal congenital disease or fetal growth restriction | No | Yes |
| Postpartum | Positive | Negative |
| Fetal condition after childbirth | No | Yes |
| Feelings toward childcare | Happy | Neither/Unhappy |
| Partner's support | Often/Sometimes | Few |
| Family and social support | Yes | No |
| Difficulty of childcare | Nothing/Sometimes | Often |
| Consultation request | No | Yes |
| EPDS | <9 | ≧9 |
EPDS; the Edinburgh postnatal depression scale.
At the three medical institutions, information was collected from face-to-face interviews, impressions based on behavior and actions such as poor comprehension, disheveled clothing, medical information and original questionnaires including the NEW interview sheets were distributed. Medical information included maternal age, parity, medical history, maternal mental disorder, gestational age at the first visit, number of pregnancy medical examinations, multiple pregnancies, and pregnancy complications. Using information other than the NEW interview sheets, pregnant women in need of administrative cooperation were selected by conferences at Osaka Women's and Children's Hospital and Seibo Hospital and by nurses specializing in maternity nursing at Showa University. The members of the conference at Osaka Wemen's and Children's Hospitalwere nurses, midwives, public health nurses, caseworkers, and obstetricians, while the members at Seibo Hospital were nurses, midwives, caseworkers, and pediatricians.
Statistical analyses
Standardized partial regression coefficients were calculated by multiple linear regression analysis to refine and score each item on the NEW interview sheet. Scores were calculated by multiplying the standardized partial regression coefficient by 100 and rounding it off to the closest whole. The cutoff value was calculated by the receiver operating characteristic (ROC) curve. The variance inflation factor was calculated using regression analysis to confirm multi-collinearity in the multivariate analysis. The association between perinatal factors and EPDS was assessed using multiple logistic regression analysis. All statistical analyses were performed using SPSS Statistics ver. 27 software. Two-sided P-values of <0.05 were considered statistically significant.
Ethical statement
This study complied with all the relevant national regulations, institutional policies, and the tenets of the Helsinki Declaration. This research was approved by the Ethics Review Board of the University of Yamanashi (approval number 1663, approval date July 10, 2017). Written informed consent was obtained from all study subjects. At the time the NEW interview sheets from the three medical institutions were mailed to the University of Yamanashi, the data center, research IDs were assigned, and names and IDs for each hospital were deleted. The matching forms of research IDs and hospital-specific IDs were managed at each institution.
Results
Table 2 illustrates the number of responses to the interview sheet and the number of pregnant women in need of social support who were judged to need cooperation with the public health center at each of the periods. We received 678 responses at the first visit, 495 during the second trimester, 296 during the third trimester, and 822 for postpartum. Figure 1 showed that the change in support status during pregnancy and postpartum for the 166 cases for which all NEW interview sheets for all periods were available. In this study, we investigated socially high-risk pregnant women who were supported by their respective obstetric institutions as well as collaborating with a public health center. In the first trimester, 2% of pregnant women in need of support required collaboration with a public health center and 17% of the pregnant women were at high-risk of needing social support. During the second and third trimesters, 6% of pregnant women in need of support required collaboration with public health centers, higher than that in early pregnancy, and it was highest at 23% in the postpartum period. There was a change in the support status during pregnancy. In some cases, cooperation with public health centers was started but later changed to support at the respective medical institutions or some cases in which support was no longer needed. There were also 13 cases presenting without problems during pregnancy, but support was needed after delivery.
Table 2.
The number of pregnant women in need of support by the public health center.
| Osakac | Seibod | Showae | Total | |
|---|---|---|---|---|
| First visit | ||||
| Number of cases | 279 | 120 | 277 | 678 |
| Missing data | 7 | 0 | 2 | 9 |
| Social high-risk pregnant womena | 41 (15) | 5 (4) | 67 (24) | 113 (17) |
| Women in need of social supportb | 8 (3) | 0 | 6 (2) | 14 (2) |
| Second trimester | ||||
| Number of cases | 225 | 46 | 224 | 495 |
| Missing data | 10 | 1 | 0 | 11 |
| Social high-risk pregnant womena | 23 (11) | 3 (7) | 8 (4) | 34 (7) |
| Women in need of social supportb | 9 (4) | 0 | 21 (9) | 30 (6) |
| Third trimester | ||||
| Number of cases | 171 | 40 | 85 | 296 |
| Missing data | 13 | 0 | 1 | 14 |
| Social high-risk pregnant womena | 17 (11) | 2 (5) | 18 (12) | 37 (13) |
| Women in need of social supportb | 8 (5) | 0 | 10 (12) | 18 (6) |
| Postpartum | ||||
| Number of cases | 199 | 61 | 562 | 822 |
| Missing data | 8 | 1 | 294 | 303 |
| Social high-risk pregnant womena | 5 (3) | 4 (7) | 99 (38) | 108 (21) |
| Women in need of social supportb | 37 (19) | 2 (3) | 80 (30) | 119 (23) |
Data are shown as n ().
social high-risk pregnant women: pregnant women with social problems supported by their respective obstetric institutions.
women in need of social support: pregnant women in need of social support who were judged to need cooperation with the public health center at each of the periods.
Osaka: Osaka Women's and Children's Hospital.
Seibo: Seibo Hospital.
Showa: Showa University Hospital.
Figure 1.
Support status change during pregnancy and the postpartum period. There were cases in which the support status changed during the gestational period. †Hospital support: socially high-risk pregnant women who were supported by their respective obstetric institutions. ‡Administrative cooperation: pregnant women in need of support to require collaboration with public health center.
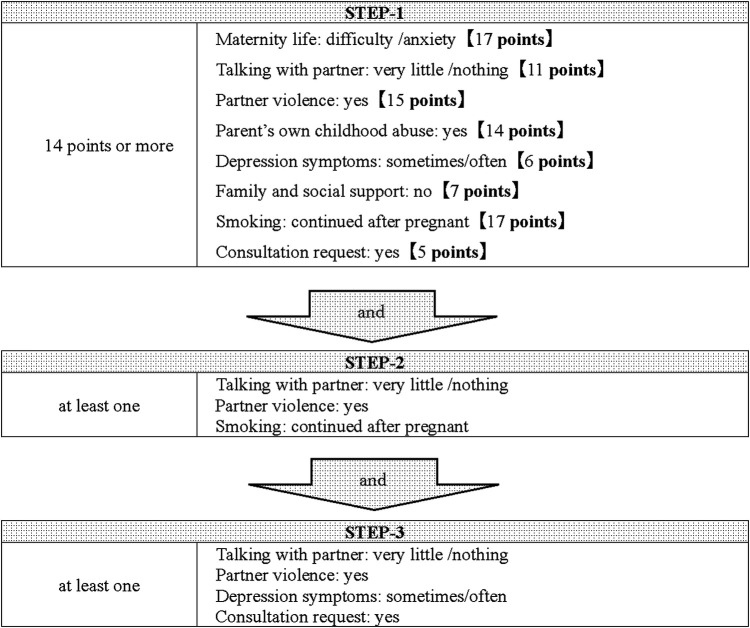
Table 3 shows the results of the multiple linear regression analysis at the first visit. Compared to the results of the single regression analysis (Model-1) for each item, in the multiple regression analysis in which all factors were input, the results of the items “partner's feelings toward being pregnant “and “consultation request “were reversed, so they were excluded from the study. Furthermore, among the items on the interview sheet, “illegal drug use by the mother and partner” were excluded from the screening tool because they clearly required cooperation with a public health center. The questionnaire after exclusion of the four items was used as Model-2, and the score of each item was calculated. The cutoff value for the detection of pregnant women in need of social support was calculated to be 22 points from the ROC curve, and scores of 22 points or more were selected as STEP-1, with an area under the curve (AUC) of 0.96, the sensitivity of 0.92, and specificity of 0.92. Of the 558 subjects analyzed at the first visit, 54 cases were detected for STEP-1. To further improve the selection rate, we checked the applicable percentage of each item including the four items excluded in STEP-1 in the group that had cooperation with a public health center in this study. The factors that accounted for more than 30% of the total were “no family and social support,” “maternal mental disorder,” “worry about the older child,” and “multiple pregnancies,” and those who had at least one of these four factors were selected as STEP-2 in addition to STEP-1. As a result, 20 cases were selected, of which six cases (30%) were involved in cooperation with a public health center. In addition, those with at least two of the following were selected as STEP-3: “depression symptoms,” “maternal mental disorder,” and “consultation request.” The number of pregnant women in need of social support based on the screening by three STEPs was 14, of which 5 (36%) required administrative cooperation. The number of positive screening results was 14 (2.5%) out of 558. The screening tool is presented in Figure 2.
Table 3.
The multiple linear regression analysis at first visit.
| Model-1 (clude) | Model-2 (adjusted; n = 554) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | OR | 95% CI | P | SPRC | Score | OR | 95% CI | P | VIF |
| Maternal feelings toward being pregnant | |||||||||
| Happy | 1 | Reference | 1 | Reference | |||||
| Unhappya | 10.985 | 3.966–30.422 | 0 | 0.069 | 6.9 | 2.72 | 0.509–14.527 | 0.242 | 1.095 |
| Partner's feelings toward being pregnant | – | ||||||||
| Happy | 1 | Reference | |||||||
| Unhappya | 5.566 | 1.723–17.98 | 0.004 | ||||||
| Depression symptoms | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 3.987 | 1.135–14.005 | 0.031 | 0.019 | 1.9 | 1.794 | 0.312–10.298 | 0.512 | 1.058 |
| Family and social support | |||||||||
| Yes | 1 | Reference | 1 | Reference | |||||
| No | 13.489 | 1.325–137.317 | 0.028 | 0.117 | 11.7 | 32.455 | 1.386–759.856 | 0.031 | 1.059 |
| Economic status | |||||||||
| No problem | 1 | Reference | 1 | Reference | |||||
| Poverty | 10.235 | 3.787–27.66 | 0 | 0.076 | 7.6 | 2.24 | 0.473–10.613 | 0.31 | 1.167 |
| Partner's status | |||||||||
| Married | 1 | Reference | 1 | Reference | |||||
| Unmarried/remarried | 6.433 | 2.324–17.812 | 0 | 0.129 | 12.9 | 6.068 | 1.33–27.686 | 0.02 | 1.086 |
| Maternal mental disorder | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 13.593 | 4.653–39.709 | 0 | 0.16 | 16 | 11.131 | 1.662–74.542 | 0.013 | 1.034 |
| Illegal drug use by mother | – | ||||||||
| No | 1 | Reference | |||||||
| Yes | 0 | 0 | 0.999 | ||||||
| Illegal drug use by partner | – | ||||||||
| No | 1 | Reference | |||||||
| Yes | 0 | 0 | 0.999 | ||||||
| Worries about older child | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 2.154 | 0.685–6.767 | 0.189 | 0.028 | 2.8 | 2.917 | 0.367 | 0.312 | 1.02 |
| Consultation request | – | ||||||||
| No | 1 | Reference | |||||||
| Yes | 3.689 | 1.322–10.296 | 0.013 | ||||||
| Number of fetuses | |||||||||
| Singleton | 1 | Reference | 1 | Reference | |||||
| Multiple | 4.96 | 1.049 | 0.043 | 0.105 | 10.5 | 14.601 | 1.557 | 0.019 | 1.01 |
| Number of children | |||||||||
| <3 | 1 | Reference | 1 | Reference | |||||
| ≧3 | 7.239 | 1.903 | 0.004 | 0.141 | 14.1 | 19.624 | 2.45 | 0.005 | 1.103 |
| Maternal age | |||||||||
| ≧25 | 1 | Reference | 1 | Reference | |||||
| <25 | 15.49 | 4.909 | 0 | 0.212 | 21.2 | 37.134 | 5.458 | 0 | 1.039 |
OR: odds ratio.
95% CI: 95% confidential interval.
VIF: variance inflation factor.
SPRC: standardized partial regression coefficient.
Unhappy: confused, trouble, did not feel anything to be pregnant.
Figure 2.
The screening tool used at the first visit. Pregnant women with score of 22 points or more were selected as STEP-1. Then, pregnant women are narrowed down as STEP 2 and 3 according to the items on the interview sheet at first visit.
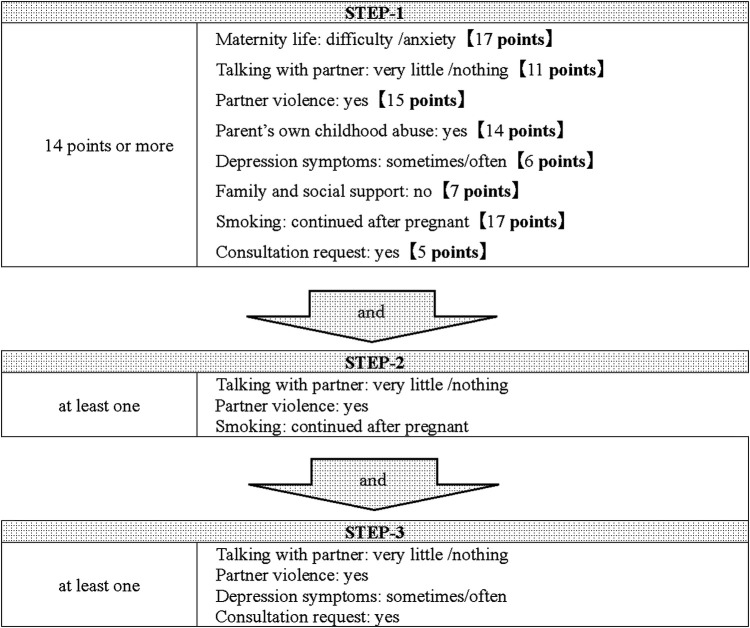
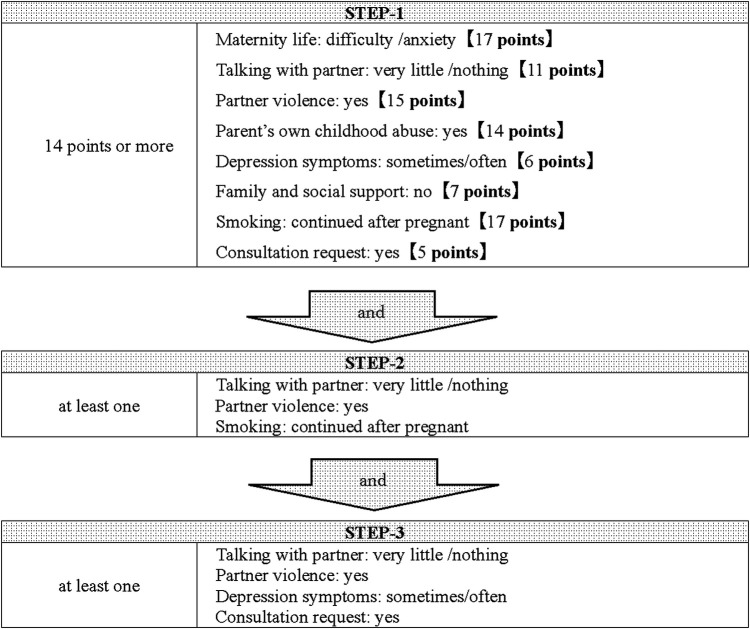
Table 4 shows the results of the multiple linear regression analysis during the second trimester. Compared to the results of the single regression analysis (Model-1) for each item, in the multiple regression analysis in which all factors were entered, the item “worries about the older child “was reversed, so it was excluded from the study. In addition, “alcohol use” and “status of pregnancy health checkups “were excluded because they could not be analyzed due to missing data. The NEW interview sheets after the exclusion of the three items were used as Model-2, and the scores for each item were calculated. The cutoff value for pregnant women in need of social support was determined to be 14 points from the ROC curve, and scores of 14 points or more were extracted as STEP-1, with an AUC of 0.77, sensitivity of 0.82, and specificity of 0.62. Of the 483 cases analyzed during the second trimester, 110 cases were extracted by STEP-1, of which 34 cases (31%) were had cooperation with public health centers in this study. To increase the selection rate, we examined the factors on the NEW interview sheets of the women who scored more than 14 points. Since the percentage of the risk group was more than 30% for all items, we calculated the Spearman correlation coefficient for the subjects with 14 points or more, weighted the correlation coefficient by a factor of 10, and considered variables with 2 points or more to be factors with higher risk. These items were “no talking with partner,” “partner violence,” and “smoking,” and if any of these items were applicable, they were narrowed down as STEP-2 in addition to STEP-1. Twenty-one people were selected for STEP-1 and STEP-2, of whom 12 (57%) required administrative cooperation in this study. In addition, STEP-3 was selected for those who had at least one of the following: “no talking with partner,” “partner violence,” “depression symptoms,” and “consultation request.” As a result, 12 cases were selected, and all of them were the subjects of the actual administrative collaboration in this study. The number of positive cases by the screening by three STEPs was 12 out of 483 (2.5%). The screening tool is shown in Figure 3.
Table 4.
The multiple linear regression analysis during the second trimester.
| Model-1 (clude) | Model-2 (adjusted) (n = 472) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | OR | 95% CI | P | SPRC | score | OR | 95% CI | P | VIF |
| Maternity life | |||||||||
| Happy | 1 | reference | 1 | Reference | |||||
| Difficulty/Anxiety | 4.165 | 2.306–7.525 | 0 | 0.167 | 17 | 3.19 | 1.603–6.35 | 0.001 | 1.119 |
| Talking with partner | |||||||||
| Yes | 1 | Reference | 1 | Reference | |||||
| No | 6.773 | 2.413–19.008 | 0 | 0.108 | 11 | 3.102 | 0.819–11.752 | 0.096 | 1.233 |
| Partner violence | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 12.918 | 3.523–47.367 | 0 | 0.15 | 15 | 7.081 | 1.502–33.388 | 0.013 | 1.236 |
| Worries about older child | |||||||||
| No | 1 | Reference | |||||||
| Yes | 1.342 | 0.598–3.009 | 0.476 | ||||||
| Parent's own childhood abuse | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 6.413 | 2.695–15.259 | 0 | 0.135 | 14 | 3.566 | 1.281–9.929 | 0.015 | 1.083 |
| Depression symptoms | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 2.74 | 1.547–4.852 | 0.001 | 0.058 | 6 | 1.531 | 0.785–2.984 | 0.211 | 1.114 |
| Family and social support | |||||||||
| Yes | 1 | Reference | 1 | Reference | |||||
| No | 7.691 | 0.474–124.717 | 0.151 | 0.072 | 7 | 7.517 | 0.407–138.934 | 0.175 | 1.004 |
| Smoking | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 24.113 | 2.464–236.008 | 0.006 | 0.165 | 17 | 26.667 | 2.316–306.98 | 0.008 | 1.019 |
| Alcohol use | |||||||||
| No | 1 | Reference | |||||||
| Yes | 0 | 0 | 0.999 | ||||||
| Consultation request | |||||||||
| No | 1 | Reference | 1 | Reference | |||||
| Yes | 2.051 | 1.158–3.632 | 0.014 | 0.053 | 5 | 1.499 | 0.78–2.881 | 0.225 | 1.064 |
| Pregnancy health checkups | |||||||||
| Usual | 1 | reference | |||||||
| Less/unscheduled | 125,419,59234 | 0 | 1 | ||||||
OR: odds ratio.
95% CI: 95% Confidential Interval.
VIF: Variance Inflation Factor.
SPRC: standardized partial regression coefficient.
Figure 3.
The screening tool used during the second trimester. Pregnant women with score of 14 points or more were selected as STEP-1. Then, pregnant women are narrowed down as STEP 2 and 3 according to the items on the interview sheet during the second trimester.
Table 5 shows the results of the multiple linear regression analysis during the third trimester. Each item on the NEW interview sheets was scored, and a cutoff value of 7 points was calculated using the ROC curve. The AUC, sensitivity, and specificity were 0.46, 0.43, and 0.57, respectively, which were inappropriate for screening.
Table 5.
The multiple linear regression analysis during the third trimester.
| Model-1 (clude) | Model-2 (adjusted) (n = 296) | |||||||
|---|---|---|---|---|---|---|---|---|
| Items | OR | 95% CI | P | SPRC | score | OR | 95% CI | P |
| Depression symptoms | ||||||||
| No | 1 | Reference | 1 | Reference | ||||
| Yes | 2.329 | 0.617–8.793 | 0.2123 | 0.288 | 29 | 2.865 | 0.54–15.204 | 0.2165 |
| Worries about older child | ||||||||
| No | 1 | Reference | 1 | Reference | ||||
| Yes | 3.039 | 0.872–10.591 | 0.0809 | 0.1226 | 12 | 1.88 | 0.344–10.28 | 0.4664 |
| Concerns about the course of pregnancy | ||||||||
| No | 1 | Reference | ||||||
| Yes | 2.483 | 0.73–8.446 | 0.1453 | |||||
| Family and social support | ||||||||
| Yes | 1 | Reference | 28 | 1 | Reference | |||
| No | 53.397 | 4.462–638.95 | 0.0017 | 0.276 | 124.973 | 3.724–>999.9 | 0.0071 | |
| Childbirth preparation | ||||||||
| Finished | 1 | Reference | 1 | Reference | ||||
| Unfinished | 3.416 | 0.386–30.227 | 0.2695 | 0.0653 | 7 | 2.027 | 0.144–28.527 | 0.6006 |
| Consultation request | ||||||||
| No | 1 | Reference | 1 | Reference | ||||
| Yes | 4.458 | 1.306–15.218 | 0.017 | 0.5232 | 52 | 7.603 | 1.54–37.545 | 0.0128 |
| Pregnancy health checkups | ||||||||
| Usual | 1 | Reference | 1 | Reference | ||||
| Less/unscheduled | 12.182 | 1.025–144.745 | 0.0477 | 0.2416 | 24 | 68.484 | 3.034–>999.9 | 0.0079 |
| Fetal congenital disease or fetal growth restriction | ||||||||
| No | 1 | Reference | 1 | Reference | ||||
| Yes | 7 | 1.923–25.48 | 0.0032 | 0.4354 | 44 | 18.455 | 3.628–93.887 | 0.0004 |
OR: odds ratio.
95% CI: 95% Confidential Interval.
VIF: Variance Inflation Factor.
SPRC: standardized partial regression coefficient.
In addition, we examined the relationship between the EPDS at the one-month postpartum and each item on the NEW interview sheets. Of those who completed the NEW interview sheets at the first visit, during second trimester, and during third trimester, and third trimester, 415 (66.7%), 384 (77.6%), and 232 (78.4%), respectively, underwent postpartum EPDS. Of these, 28 (6.7%) at the first visit, 24 (6.3%) during second trimester, and 17 (7.3%) during third trimester had an EPDS score of 9 or higher. Table 6 showed the relationship between EPDS ≧ 9 and each item on the NEW interview sheets. The factor “no family and social support” (n = 1) and “ illegal drug use by the mother(n = 4) and partner” (n = 3) at the first visit, and “no family and social support,”(n = 2) “alcohol use,” (n = 2) and “less or unscheduled pregnancy health checkups”(n = 1) during the second trimester were excluded due to their small number. The factors associated with EPDS ≧ 9 were “Women who felt confused/troubled or did not feel anything to be pregnant” (adjusted odds ratio [aOR]: 6.51, 95% confidence interval [CI]: 1.62–26.15), “Maternal mental disorder”(aOR 4.38, CI 106–18.10), “Consultation request at first visit” (aOR 3.22, CI 1.09–9.45), and “Women who have difficulty or anxiety about pregnancy during the second trimester” (aOR 3.14, CI 1.29–7.67). The factor “less or unscheduled pregnancy health checkups” (n = 3) during the third trimester was excluded due to the small number of cases, and no factor associated with EPDS was found.
Table 6.
Relationship between EPDS ≧ 9 and each item on the NEW interview sheets.
| cOR | 95% CI | P | aOR | 95% CI | P | |
|---|---|---|---|---|---|---|
| At first visit | ||||||
| Maternal feelings (confused/troubled or did not feel anything) | 4.62 | 1.80–11.86 | 0.002 | 6.51 | 1.62–26.14 | 0.008 |
| Partner's feelings (confused/troubled or did not feel anything) | 1.46 | 0.32–6.6 | 0.62 | 0.35 | 0.03–3.51 | 0.37 |
| Depression symptoms | 2.75 | 1.19–7.11 | 0.02 | 2.86 | 0.75–10.92 | 0.13 |
| Poverty | 1.9 | 0.74–4.93 | 0.19 | 1.46 | 0.37–5.72 | 0.58 |
| Unmarried/remarried | 1.25 | 0.42–3.77 | 0.69 | 2.44 | 0.61–9.69 | 0.21 |
| Maternal mental disorder | 5.92 | 1.95–18.00 | 0.002 | 4.38 | 1.06–18.10 | 0.04 |
| Worries about older child | 1.43 | 0.52–3.92 | 0.49 | 1.41 | 0.33–6.14 | 0.64 |
| Consultation request | 3.31 | 1.47–7.43 | 0.004 | 3.22 | 1.09–9.45 | 0.03 |
| Multiple pregnancy | 3.18 | 0.65–15.48 | 0.15 | 1.97 | 0.19–20.43 | 0.57 |
| Number of children ≧3 | 1 | 0.13–7.91 | 1 | 0.85 | 0.05–13.43 | 0.91 |
| Maternal age <25 | 1.06 | 0.06–5.62 | 0.96 | 0.8 | 0.06–10.22 | 0.86 |
| During the second trimester | ||||||
| Matanity life (Difficulty/Anxiety) | 4.18 | 1.81–10.02 | 0.0009 | 3.15 | 1.29–7.67 | 0.01 |
| Talking with partner | 2.63 | 0.55–12.48 | 0.22 | 1.76 | 0.27–11.41 | 0.56 |
| Partner violence | 1.91 | 0.23–15.91 | 0.55 | 1.12 | 0.09–13.48 | 0.93 |
| Worries about older child | 1.78 | 0.64–5.01 | 0.27 | 1.14 | 0.37–3.52 | 0.82 |
| Parent's own childhood abuse | 1.95 | 0.42–9.04 | 0.39 | 0.77 | 0.13–4.42 | 0.77 |
| Depression symptoms | 3.11 | 1.3–7.45 | 0.01 | 2.42 | 0.96–6.10 | 0.06 |
| Smoking | 5.17 | 0.52–51.71 | 0.16 | 5.85 | 0.50–68.9 | 0.16 |
| Consultation request | 2.5 | 1.08–5.76 | 0.03 | 1.96 | 0.80–4.80 | 0.14 |
| During the third trimester | ||||||
| Depression symptoms | 3.36 | 0.94–12.04 | 0.06 | 4.65 | 0.94–22.94 | 0.06 |
| Worries about older child | 1.68 | 0.45–5.08 | 0.41 | 1.7 | 0.41–7.10 | 0.46 |
| Concerns about the course of pregnancy | 2.36 | 0.83–6.73 | 0.11 | 2.01 | 0.54–7.54 | 0.3 |
| Family and social support | 13.25 | 0.79–221.8 | 0.07 | 24.14 | 0.56–1035.66 | 0.1 |
| Childbirth preparation | 0.96 | 0.26–2.86 | 0.95 | 0.33 | 0.066–1.69 | 0.18 |
| Consultation request | 2.49 | 0.89–6.94 | 0.08 | 1.71 | 0.48–6.09 | 0.41 |
| Fetal congenital disease or fetal growth restriction | 1.66 | 0.25–6.61 | 0.55 | 0.56 | 0.06–5.24 | 0.62 |
OR: odds ratio.
95% CI: 95% Confidential Interval.
Discussion
The NEW interview sheets and the stepwise screening tool by three STEPs tools during the first and second trimester were developed in which 2.5% of pregnant women were identified as requiring social support, respectively. The screening tool was created with the intention of narrowing down the number of targets because if there are too many targets, the health center may not be able to handle them. According to a survey in Osaka Prefecture, cases of deliveries of little or no receiving for pregnancy health checkups accounted for about 0.3%. (Unpublished data) In addition, the frequency of specified expectant mothers was reported to be 2%–5% (12, 13). Specified expectant mothers are defined in the Child Welfare Act as “pregnant women who are recognized as being in particular need of support during pregnancy with regard to postpartum care.” A specified expectant mother is determined by the health center. This study aims to detect pregnant women in need of support in collaboration with health centers, that is, cases corresponding to specified pregnant women. Therefore, we believe that the detection rate of pregnant women in need of social support using this screening tool is reasonable. The screening tool was created with the goal of being able to detect women, even in obstetric clinics that were not familiar with social issues, automatically. In the future, it will be necessary to verify whether these NEW interview sheets and screening tools can appropriately identify pregnant women in need of social support, and we are planning to create a system that can automatically identify pregnant women in need of social support by inputting the results of the NEW interview sheets.
The frequency of postpartum depression is reported to be 5%–10% in a prospective study in Japan (14) and 9% in the final report of the “Healthy Parents and Children 21” (15). Furthermore, postpartum depression may lead to maternal suicide as well as child maltreatment (16–18). In Japan, a suicide prevention program (Nagano model) (19) has been developed to improve postpartum mental health and reduce maternal suicide, and its effectiveness has been reported. In the present study, the factors associated with EPDS ≧ 9 at one-month postpartum were “Women who felt confused/troubled or did not feel anything to be pregnant,” “Maternal mental disorder,” “Consultation request at first visit,” and “Women who have difficulty or anxiety about pregnancy during the second trimester.” Although postpartum depression may develop unexpectedly, our findings have been suggested that conditions that could cause postpartum depression existed during pregnancy. In addition, it suggested that identifying mothers who have mental disorder, unwanted pregnancy, and anxiety during pregnancy may be useful in early detecting women who have postpartum depression. According to the reports of the Japan Environment and Children's Study, compared with women who felt very happy to be pregnant, those whose pregnancy was unintended but happy, unintended, and confused, those who felt troubled, and those who felt no emotion toward being pregnant had increased risks of postpartum depression (20).
The strength of this study is a prospective survey conducted in several obstetric institutions that are specialized in addressing social issues, and various criteria were used to determine the detection of pregnant women in need of social support. In addition, considering the possibility of changes in the mother's and family's condition during pregnancy and background factors that may become apparent through the establishment of a relationship between the mother and the obstetric institution, NEW interview sheets and screening tools were developed that included items tailored to each period and items common to all periods.
Several limitations should be addressed. First, less than half of the cases had a complete NEW interview sheets for all time periods. This was because two of the three facilities in this study handle many medically high-risk pregnancies, which may result in first visits at various times. In those facilities, the number of patients who were referred in the second trimester and later due to medical risks such as fetal growth retardation or threatened premature birth means that a larger percentage of patients do not receive the NEW interview sheets, especially in the early and middle trimester of pregnancy. Second, although it had been reported that a late first visit is associated with pregnant women in need of social support, it was not included in this study. This was because the study includes many cases in which the first visit was made after the second trimester due to medical risks. Finally, this study was conducted up to one month after childbirth, and the relationship with the need for support at a public health center after that was unknown. Although it would be desirable to collate the data with information from the public health center if there was an actual fear of child maltreatment several months after the birth, it was difficult to obtain the data from the public health center from the viewpoint of personal information protection. In a survey such as this one, it is considered necessary to create an environment where medical institutions and government agencies can collaborate to collect information in Japan.
In conclusion, we developed the NEW interview sheets and the stepwise screening tools during the first and the second trimester to detect pregnant women in need of support to require collaboration with a public health center. We plan to further validate these NEW interview sheets and screening tools by increasing the number of participating obstetrics clinics.
Acknowledgments
We would like to express our gratitude to the outpatient staff of the Osaka Women's and Children's Hospital, Seibo Hospital, and Showa University Hospital for their cooperation in this study.
Funding Statement
This study was supported by Health and Labour Sciences Research Grants (19DA1003). The funder of this research did not interfere with the design, data collection, analysis, or writing for this project.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by he Ethics Review Board of the University of Yamanashi (approval number 1663, approval date July 10, 2017). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
HK planned the research, collected patient data, and was a major contributor in writing the manuscript. RS, YA, and MK analyzed and interpreted the patient data. YM aided in planning the research and writing the paper. MY and TY collected patient data. ZY aided in planning the research and interpreted the patient data. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Sidebotham P, Heron J. Child maltreatment in the “children of the nineties": a cohort study of risk factors. Child Abuse Negl. (2006) 30(5):497–522. 10.1016/j.chiabu.2005.11.005 [DOI] [PubMed] [Google Scholar]
- 2.Kawaguchi H, Fujiwara T, Okamoto Y, Isumi A, Doi S, Kanagawa T, et al. Perinatal determinants of child maltreatment in Japan. Front Pediatr. (2020) 8:143. 10.3389/fped.2020.00143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. (2012) 9(11):e1001349. 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mills R, Scott J, Alati R, O'Callaghan M, Najman JM, Strathearn L. Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse Negl. (2013) 37(5):292–302. 10.1016/j.chiabu.2012.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strathearn L, Giannotti M, Mills R, Kisely S, Najman J, Abajobir A. Long-term cognitive, psychological, and health outcomes associated with child abuse and neglect. Pediatrics. (2020) 146(4). 10.1542/peds.2020-0438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health Law. Results of Investigation on Child Abuse Deaths and Number of Child Abuse Consultation. (2020).
- 7.Sakai S, Nagamitsu S, Koga H, Kanda H, Okamatsu Y, Yamagata Z, et al. Characteristics of socially high-risk pregnant women and children's outcomes. Pediatr Int. (2020) 62(2):140–5. 10.1111/ped.14058 [DOI] [PubMed] [Google Scholar]
- 8.Sidebotham P, Heron J. Child maltreatment in the “children of the nineties": a cohort study of risk Factors. Child Abuse Negl. (2006) 30(5):497–522. 10.1016/j.chiabu.2005.11.005 [DOI] [PubMed] [Google Scholar]
- 9.Ninomiya T, Hashimoto H, Tani H, Mori K. Effects of primary prevention of child abuse that begins during pregnancy and immediately after childbirth. J Med Investig. (2017) 64(1.2):153–9. 10.2152/jmi.64.153 [DOI] [PubMed] [Google Scholar]
- 10.Isumi A, Fujiwara T. Synergistic effects of unintended pregnancy and young motherhood on shaking and smothering of infants among caregivers in Nagoya city, Japan. Front Public Health. (2017) 5:245. 10.3389/fpubh.2017.00245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshida K, Marks MN, Kibe N, Kumar R, Nakano H, Tashiro N. Postnatal depression in Japanese women who have given birth in England. J Affect Disord. (1997) 43(1):69–77. 10.1016/s0165-0327(96)01419-x [DOI] [PubMed] [Google Scholar]
- 12.Runa Ito YY, Haruna Y, Tamaki E, Yajima M, Ando M, Iwashita M. Selection criteria and progress of mothers require cares in our hospital. J Jp Soc Psychosom Obstet Gynecol. (2020) 24(3):237–41. [Google Scholar]
- 13.Yoshifumi K, Masumi T, Takeshi S, Seon-Hye KIM, Takayuki H, Kazunori U. The background of specified expectant mothers in our institution. JJapan Soc Perinat Neonatal Med. (2018) 54:965–8. [Google Scholar]
- 14.Kitamura T, Yoshida K, Okano T, Kinoshita K, Hayashi M, Toyoda N, et al. Multicentre prospective study of perinatal depression in Japan: incidence and correlates of antenatal and postnatal depression. Arch Women's Ment Health. (2006) 9(3):121–30. 10.1007/s00737-006-0122-3 [DOI] [PubMed] [Google Scholar]
- 15.Ministry of Health LaW. Healthy Parents and Children 21. (2013).
- 16.Poyatos-León R, García-Hermoso A, Sanabria-Martínez G, Álvarez-Bueno C, Cavero-Redondo I, Martínez-Vizcaíno V. Effects of exercise-based interventions on postpartum depression: a meta-analysis of randomized controlled trials. Birth (Berkeley, Calif). (2017) 44(3):200–8. 10.1111/birt.12294 [DOI] [PubMed] [Google Scholar]
- 17.Sockol LE, Epperson CN, Barber JP. Preventing postpartum depression: a meta-analytic review. Clin Psychol Rev. (2013) 33(8):1205–17. 10.1016/j.cpr.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Missler M, Donker T, Beijers R, Ciharova M, Moyse C, de Vries R, et al. Universal prevention of distress aimed at pregnant women: a systematic review and meta-analysis of psychological interventions. BMC Pregnancy Childbirth. (2021) 21(1):276. 10.1186/s12884-021-03752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tachibana Y, Koizumi N, Mikami M, Shikada K, Yamashita S, Shimizu M, et al. An integrated community mental healthcare program to reduce suicidal ideation and improve maternal mental health during the postnatal period: the findings from the Nagano trial. BMC Psychiatry. (2020) 20(1):389. 10.1186/s12888-020-02765-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baba S, Kimura T, Ikehara S, Honjo K, Eshak ES, Sato T, et al. Impact of intention and feeling toward being pregnant on postpartum depression: the Japan environment and Children's Study (jecs). Arch Women's Ment Health. (2020) 23(1):131–7. 10.1007/s00737-018-0938-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.