Abstract
The COVID-19 pandemic continues to present unique challenges to healthcare organizations around the world. Members of a provincial Human Factors team supported several workspace design projects prompted by the pandemic. This article highlights some of the challenges identified in a selection of these projects. It also presents the human factors methods and recommendations that were used to improve workspace designs, processes, and patient safety in healthcare environments.
Keywords: Environmental design, health systems, workspace design, system analysis, human error
In response to the COVID-19 pandemic, healthcare organizations have had to assess and modify their workspaces and processes to accommodate changing needs and requirements. Alberta Health Services (AHS), a provincial health authority in Canada, has had to update and develop new care spaces and processes across the province since the first COVID-19 cases were identified in March of 2020. The AHS Human Factors team has played a key role in addressing requests to evaluate and optimize the design of several of these work environments with the goal of improving patient and staff safety.
Our team has participated in the evaluation and optimization of the design of drive-through testing sites, assessment centers, treatment centers, new COVID-19 units, ICU expansions, pandemic response units (PRUs), and vaccination sites. We have also assisted in updating and streamlining the processes and procedures used within these new and modified spaces.
This article will highlight some of the challenges identified through our project work, and the human factors methods and recommendations applied to address them. By sharing our recommendations, we hope to help other human factors practitioners and healthcare leaders effectively modify their healthcare environments and processes in response to the continuing COVID-19 pandemic as well as future pandemics and healthcare emergencies.
HUMAN FACTORS COVID-19 WORK
This paper highlights key recommendations from seven projects that were completed in response to the COVID-19 pandemic. We received requests from frontline clinicians and operational staff to provide guidance on how to design environments for testing and vaccinations. We also consulted on surge spaces to help manage patient overflow due to an increase in hospitalizations.
To collect data and evaluate environments and processes, a number of human factors methods were applied including simulations, tabletop evaluations (end-user representatives working through a series of scenarios using a printed floor plan as a reference), task analyses, observations, interviews, and expert reviews. Our COVID-19 work frequently involved collaboration with other groups across the organization, such as Infection Prevention & Control (IPC), eSIM (simulation team), Communications, and Operations.
COMMON CHALLENGES
Within the seven projects included in this paper (described in Table 1), several common challenges emerged across the different healthcare environments, including:
• Adhering to new IPC requirements.
• Communicating risks related to COVID-19.
• Novel working conditions.
Table 1.
Description of the Methods Used to Conduct Each of the Seven Projects Discussed in This Paper and Suggestions for Post-Implementation Evaluations
| Project | Description of methods | Post-implementation evaluation* |
|---|---|---|
| Hand Sanitizer Dispenser Placement | Onsite observations to identify high traffic areas | Observations of usage rates Measure hand sanitizer usage (e.g., measure mLs used) |
| Clean and Dirty Area Delineation | Onsite walkthroughs, and consultations with subject matter experts to determine where to place clean/dirty areas | Review of adverse event reports to determine how many reports are related to clean/dirty mix ups/errors Staff interviews to collect qualitative data on how clean/dirty areas are working Observations to see if staff are adhering to clean/dirty areas |
| PPE Supply Organization and Standardization | Interviews with nursing and environmental service staff to identify equipment challenges Human factors expert review of existing organization system Tabletop evaluation to determine where equipment should be stored |
Measure task time to see if standardization of items in clean cart increases stocking speed Cart audits to determine if carts are properly stocked and organized Staff interviews to explore whether the redesign supports their task needs |
| Non-Critical Signage and Information Removal or Relocation | Onsite walkthroughs to assess current state of signage/posters Staff interviews to capture signage/poster concerns “Development of a decluttering decision support tool (Figure 3) to increase salience of essential information” |
Measure rates of signage/poster removal or consolidation following tool use Staff surveys and interviews to capture perception and understanding of signage/posters |
| COVID-19 Signage Creation and Placement | Human factors expert design review and application of design principles (Table 2) Interviews with multidisciplinary teams of clinical and non-clinical experts to determine critical sign content |
Measure frequency of inadvertent entry into isolation rooms without proper PPE Conduct surveys or staff interviews to test the comprehension of signage content |
| COVID-19 Vaccination Center Error Prevention | Review of COVID-19 vaccination patient safety reports using the Provincial Reporting and Learning System (RLS) to collect data on type and frequency of issues/errors Staff interviews and observations of vaccination registration and administration processes Task analysis of vaccination registration and administration processes |
Post-implementation review of RLS to evaluate frequency and severity of COVID-19 vaccine-related reports Conduct staff interviews to determine whether interventions helped to reduce vaccine error potential |
| Wayfinding System Development | Review of paper mock-up signage with staff and other stakeholders to identify navigation challenges | Surveys capturing end-user perceptions of the wayfinding system Simulation with patients, visitors, and staff to determine if they can successfully and efficiently navigate to their destinations using the final wayfinding system elements Live observation of patients, visitors, and staff navigating to, from, and within the PRU |
*Note that the post-implementation evaluations listed here were not performed due to time and resource constraints, but these could be employed for similar future projects.
Adhering to New IPC Requirements
Due to the speed and intensity with which new COVID-19 safety requirements were developed for the healthcare system, managers and staff were confronted with significant implementation challenges. In addition to new personal protective equipment (PPE) requirements, we observed that there was variability in practice for the placement of hand sanitizer dispensers and other equipment. It was also necessary to find strategies to clearly delineate clean and dirty areas to prevent contamination. This was challenging in many healthcare areas that were constrained by a lack of physical space and limited guidance on the best way to visually separate clean and dirty equipment.
The broad application of the processes involved in adhering to new COVID-19 IPC requirements, the variability between these processes, and the immediacy of implementation increased the potential for errors. Through observations, expert reviews, and evidence-based guidance, the Human Factors team was able to deliver recommendations to improve PPE equipment placement and to prevent contamination errors.
Hand Sanitizer Dispenser Placement
To promote hand hygiene, alcohol-based hand rub (ABHR) dispensers were mounted outside of elevators and other high traffic areas. This placement provides a strong visual cue to remind people to sanitize their hands. Locating the dispensers in high traffic areas may also help to reduce the misuse or consumption of sanitizer, which has been recognized as an issue (Archer et al., 2007).
We collaborated with local process improvement, IPC, and facilities, maintenance, and engineering to identify optimal locations for ABHR dispensers at a hospital where it was found that access was lacking. This involved onsite observations and walk-throughs to identify consistent locations for dispensers on all hospital floors to assist users in creating a mental model of where they should expect to see a dispenser (see Figure 1). Attention was given to the movement and storage of equipment in spaces which may bump into or block ABHR dispensers, and locations were selected to avoid interactions with equipment. Finally, we recommended removing unnecessary posters on walls to reduce visual clutter and help users easily find a dispenser when needed.
Figure 1.
Pink dot shows the proposed standard location of alcohol-based hand rub dispensers outside of service elevators.
Clean and Dirty Area Delineation
The need to separate clean and dirty areas in a way that is salient and intuitive to staff was established as a priority in several projects. The use of colored tape, with green representing clean and red representing dirty, can help to visually distinguish between the areas and potentially assist in preventing contamination (see Figure 2). The colors selected, red and green, were deliberate and leveraged the automatic association with a traffic light. Red is associated with “stop,” danger, or a high level of risk. Green is commonly associated with “go,” safety, and a lower level of risk. The use of color-coded zones has been found to be helpful in reducing cross-contamination and infection (Chong, 2020).
Figure 2.
Red tape used to identify dirty areas and green to identify clean. Wall signs indicating “clean” and “dirty” were used as a secondary redundant cue to accommodate users who have color vision deficiency.
PPE Supply Organization and Standardization
The COVID-19 pandemic increased the number of patient hospitalizations, and as a consequence, the volume of PPE necessary to keep staff and patients safe. The increase in PPE created a need for additional supply storage and resulted in unprecedented amounts of waste and laundry. To prevent overstocking and clutter on isolation equipment carts, which can lead to PPE equipment hanging over the sides of the cart and potentially becoming contaminated, cart organization should be standardized. Consistency and standardization, a core usability principle, helps users understand what to expect when using a system (Nielsen, 1993). We anticipated that standardization could help improve stocking speed and ease of access to the correct equipment and supplies. To further facilitate quick access and use, we recommended that items used together be stored together on the cart. We advised that high use items (e.g., hand sanitizer, masks, and gloves) be stored on the top of the cart where they can be accessed more easily.
Additionally, we recommended the use of an itemized checklist to indicate what items, and how many of each, should be stocked on the clean isolation cart. Checklists are especially helpful when tasks are carried out by busy healthcare workers in high stress environments as they can help to increase efficiency, decrease the mental burden of a task, and reduce errors of omission when stocking (Anderson et al., 2010).
We also recommended that labels be applied to the cart shelves to clarify where each item should go. A useful label should minimize the number of words used while retaining key information (Wickens et al., 2004). It was recommended that label placement be considered to ensure it is not obscured by equipment or supplies. Selecting the right font can also help to improve the overall readability of the label. Sans-serif fonts such as Tahoma or Verdana are preferred because of their consistent, easy to read strokes, and black text on a white background was suggested to maximize contrast.
Communicating Risks Related to COVID-19
A key challenge encountered by healthcare teams was how to properly communicate the risks associated with COVID-19 in specific care areas, such as isolation rooms and units on various levels of outbreak. In the early stages of the pandemic, each unit created their own signage to get COVID-19 messaging out as quickly as possible. However, many clinicians work on multiple units, so without consistency in signage appearance and messaging there is a risk of confusion. In addition, adding new signage to an already cluttered environment made it difficult for people to focus on the most important pieces of information. The Human Factors team was engaged to help optimize and standardize COVID-19 signage for use across AHS. We worked with the AHS Communications team to develop posters and signage that used human factors design principles to convey important warnings and COVID-19-related instructions with salience and clarity. Using feedback from staff interviews, we determined that one of the reasons the communication of risk was challenging was due to the sheer amount of information cluttering the physical workspaces and, in turn, healthcare workers’ minds.
If staff or patients fail to attend to important COVID-19 information, they may not adequately adhere to the required precautions. Consequently, there is a risk of self-contamination and potential spread. Although this may appear to be due to carelessness, it is more likely a case of “inattentional blindness” (Grissinger, 2012).
According to Green (2011, para. 3), inattentional blindness is the “failure to see an object located on or near the sightline because it does not engage attention.” Only the most salient information is able to capture attention. To ensure the clear communication of important COVID-19 information, human factors design principles, including the use of adequate contrast, colors, and simplified text, were used to create signage and messaging that would capture attention. Many of the previous signs containing key COVID-19 information looked similar to other signs and did not utilize strategies to ensure they stood out. The following sections describe how to improve salience of signage in detail.
Non-Critical Signage and Information Removal or Relocation
Before installing any new signs or posters, we recommended engaging in a process of decluttering. From onsite observations and staff interviews, it was noted that overwhelming amounts of visual information made it difficult to attend to the most important sign or poster. The Human Factors team created a decluttering tool (Figure 3) in response to this challenge. Applying a signal detection theory lens (see Wickens, 2001 for a detailed discussion), we anticipated that performance could be improved by reducing noise (i.e., visual clutter) using the decluttering tool, and increasing signal strength (i.e., critical COVID-19 information) using human factors design principles for signage.
Figure 3.
Decluttering decision support tool to identify what information can be removed.
COVID-19 Signage Creation and Placement
In addition to reducing the amount of competing information, it is necessary to ensure that COVID-19 information commands attention. There are a variety of strategies that can be used to increase the salience and readability of signage, as described in Table 2.
Table 2.
Strategies for Creating Salient COVID-19 Signage
| Design principle | Example application | Why it works |
|---|---|---|
| Use a high degree of contrast between foreground and background | Black text on a white background | Greater contrast results in greater contrast sensitivity and easier detection of information (Green, 2011) |
| Use bright and saturated colors to draw attention | Apply colors to sign borders or icons | Color can be used to enhance attention and perception of a visual message (Jost et al., 2005). Using color on borders can help signage stand out from white/neutral walls |
| Leverage existing color associations | The use of red, orange, and yellow are commonly associated with hazards and warnings | Red is rated as the highest in perceived hazard, followed by orange and yellow (Zielinska et al., 2017) |
| Ensure text is large enough to read | Text size should increase proportionally with expected viewing distance. For example, letter height may be 100 mm (3.9 inches) for viewing from 7 m (22.9 feet) | Using text size that allows for a visual angle of 0.003–0.007 radians is appropriate for healthcare facility signage (Johanes & Yatmo, 2018) |
| Use meaningful, simple, consistent language | When designing a wayfinding system, ensure all signs use consistent terminology | Simple and consistent wording will reduce the mental effort required to interpret a sign’s meaning and reduce the risk of confusion or misinterpretation (Nielsen, 1993) |
| Use recognizable images and icons | Use standard ISO exit icon for exit direction signs | Recognizable images and icons can help improve understanding and provide redundant cues (Wickens et al., 2004). Similarly, these can be universally understood, regardless of language spoken |
To ensure the maximum visibility of COVID-19 signage, proper sign placement is imperative. We advised that signs be posted at decision points, doorways, and as close to the associated hazard as possible. For instance, isolation precaution signage must be posted outside of the isolation room door.
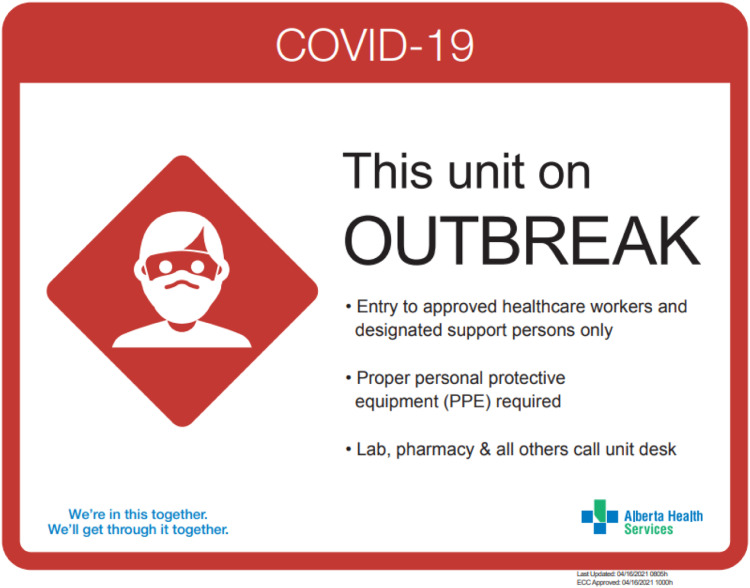
The purpose of the COVID-19 signs was to relay a warning to staff and visitors about the risk and potential consequences associated with hospital environments. Conversations with multidisciplinary teams of clinical (e.g., nursing) and non-clinical experts (e.g., AHS Communications team, IPC) were used to determine what information was critical to include on the COVID-19 posters. The information was then organized using Wickens et al. (2004) warning label design elements:
1. Trigger word to convey the hazards level of severity (e.g., “Warning”).
2. Description of the hazard (e.g., “COVID-19 Outbreak” or “Contact and droplet precautions”).
3. Consequence associated with the hazard (e.g., “Potential infection” or “Transmission”).
4. Behavior needed to avoid the hazard (e.g., “Maintain physical distance and wear a mask in all areas” or “PPE is required”).
These design elements were used in the creation of many COVID-19 signs at AHS (see Figure 4). However, AHS branding requirements posed some constraints which did not allow for perfect alignment with warning label design principles.
Figure 4.
Example of COVID-19 warning sign. Trigger word: COVID-19. Hazard: “This unit is on OUTBREAK.” Consequence: not explicitly described, but it was anticipated that the consequence (i.e., COVID-19 exposure and infection) would be widely understood. Required behavior: “Proper personal protective equipment (PPE) required.”
Novel Working Conditions
The COVID-19 pandemic required staff to work in novel and modified work environments including drive-through testing sites, mass vaccination sites, and PRUs. From a patient safety perspective, this can be challenging because novel situations are often the breeding ground for knowledge-based mistakes (Reason, 1995). When a solution has to be developed in a new environment while performing a new task, healthcare workers cannot necessarily rely on the preprogrammed solutions that they would normally use in a more familiar circumstance or environment (reason). This combination of factors can lead to an increased likelihood for errors.
COVID-19 Vaccination Center Error Prevention
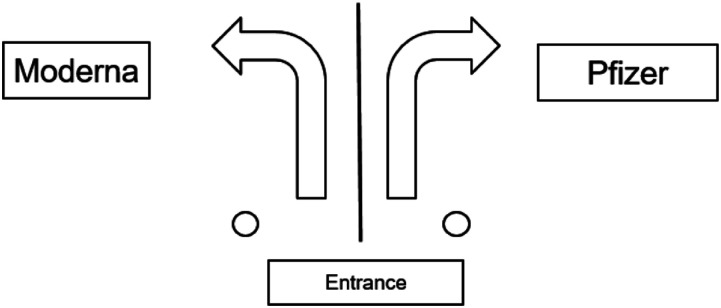
Early on in the COVID-19 vaccine roll out, youth clients were only eligible to receive the Pfizer vaccine. However, vaccination centers often had two or three different vaccines (Pfizer, Moderna, and AstraZeneca) on site at any given time. Having multiple vaccines available at one site can create an opportunity for selection errors to occur (i.e., accidently selecting the wrong vaccine). To prevent youth vaccine selection and administration errors, the Human Factors team recommended updates to the vaccination site layout. It was suggested that vaccination sites physically divide and constrain the workspace based on the type of vaccine being administered. For example, Moderna would only be stored and administered on the left side of the room and Pfizer on the right (see Figure 5).
Figure 5.
Visually divide the physical space to prevent vaccine selection errors.
Ensuring that only one vaccine option is physically present can reduce the potential for selection errors during the administration of vaccinations. According to the Institute for Safety Medication Practices (ISMP) hierarchy of effectiveness, physical separation is a strong system-focused error prevention strategy (ISMP, 1999). Alberta Health Services uses a modified version of the hierarchy of effectiveness as shown in Figure 6.
Figure 6.
Alberta Health Services-modified hierarchy of effectiveness.
Wayfinding System Development
Patients, clients, and their designated support people must be able to navigate unfamiliar healthcare environments. An effective wayfinding system is required to support them in this goal. Ensuring that users can efficiently navigate to their destination can help minimize delays and congestion, promote physical safety, and reduce stress and confusion (Devlin, 2014; Huelat, 2007). Similarly, effective wayfinding is essential for healthcare staff working in new or modified environments.
The Human Factors team was asked to help create a signage and wayfinding system for COVID-19 assessment centers and PRUs. While the assessment centers were temporary, the PRUs were set up for longer term usage in shell spaces within existing hospitals to provide additional capacity for lower acuity patients. The signage design principles described in Table 2 similarly apply to assessment center and PRU signage. Examples of assessment center signs are shown in Figure 7. A “soft launch” at an assessment center provided an opportunity to review the effectiveness of the wayfinding system with staff and make tweaks prior to operating at full testing capacity.
Figure 7.
Examples of assessment center signs. These designs featured concise descriptions written in large, high contrast text. Blue boarders were used to help make the signs stand out from various backgrounds, while the icons and images provided redundant visual information.
Before opening the PRU, it became apparent that the large, shelled space with several intersecting corridors and few landmarks would pose a wayfinding challenge. Following a discussion of user needs, a mock-up wayfinding system, using paper-printed wayfinding elements and tape, was created to review the designs with stakeholders and prospective users.
Colors are noted to be useful for visual search tasks (Sanders & McCormick, 1993), so the proposed wayfinding system featured color-coded units to differentiate between sections of beds and help users find their desired destination. These colors were utilized on signs, wall markings, and bed number markers to help users build a mental model of the space. In the mock-up review, the color codes were viewed favorably. Some improvement opportunities were also identified at this stage by the users. In particular, protruding blade signs featuring the color codes were proposed to help see the unit boundaries from further down the corridor, and some signage terminology changes were suggested.
In the final wayfinding system design, unit-specific icons were also created to provide a redundant visual cue (Figure 8). Additionally, maps—which similarly leveraged these color codes and icons—were placed at entrances and other key areas in a PRU to further aid navigation.
Figure 8.
Examples of wayfinding elements in a pandemic response unit. The entrances to each corridor listed the unit’s name (e.g., Blue Unit), bed numbers within the row, the unit icon, and associated color markings (A and B). Signs showing the directions to each unit, along with other key destinations, were similarly designed to ensure readability and leverage color codes (C). For all designs, black text was used on white backgrounds to maximize readability, and the text was sized according to expected viewing distance.
Following a period of patient occupation, feedback from operations indicated that the wayfinding system was seen as integral to the success of this PRU. No major navigation challenges for staff, patients, or visitors were identified. The color codes were reported to make navigation easy for all users, and these colors were further utilized on patient wristbands. Likewise, color-coded stickers were used to mark which mobile equipment belonged on each unit.
DISCUSSION AND CONCLUSION
The availability of stakeholders from other teams meant that work could be completed quickly, as some of the usual scheduling and process barriers were substantially reduced to accommodate the shifting priorities. However, the fast-paced nature of the work, and demands on frontline staff, also meant that there was little opportunity to formally evaluate the success of the recommended interventions. In some situations, we were able to be present for on-the-fly adjustments to designs and workflows, but more often we were pulled into other urgent projects.
The COVID-19 pandemic has created unique challenges in healthcare. As we all look for ways to manage these challenges and improve patient safety, it is important that we share our experiences and solutions.
Human factors offers a unique and systematic approach to patient safety. Multi-layered strategies are needed to help find solutions and risk mitigation strategies for the challenges created by the pandemic. The use and implementation of human factors design principles and methods can assist in creating safer and more usable workspaces and processes for patients and healthcare workers alike.
Biography
 Jessica Martel is a Human Factors Specialist at Alberta Health Services. She works to improve patient safety by applying human factors principles to the design and evaluation of medical devices, workspaces, and information. Jessica received her MSc in Cognitive Experimental Psychology from the University of Calgary in 2014. She also holds BAs in Psychology and Communications and Culture. Email: jessica.martel@albertahealthservices.ca.
Jessica Martel is a Human Factors Specialist at Alberta Health Services. She works to improve patient safety by applying human factors principles to the design and evaluation of medical devices, workspaces, and information. Jessica received her MSc in Cognitive Experimental Psychology from the University of Calgary in 2014. She also holds BAs in Psychology and Communications and Culture. Email: jessica.martel@albertahealthservices.ca.
 Jared Dembicki is a Human Factors Specialist with Alberta Health Services. In this role, Jared works to evaluate the designs of tools, equipment, workspaces, and information, ultimately with the goal of generating solutions to improve patient safety. Jared holds an MSc in Human Factors from Loughborough University and a BA in Psychology from the University of Calgary.
Jared Dembicki is a Human Factors Specialist with Alberta Health Services. In this role, Jared works to evaluate the designs of tools, equipment, workspaces, and information, ultimately with the goal of generating solutions to improve patient safety. Jared holds an MSc in Human Factors from Loughborough University and a BA in Psychology from the University of Calgary.
 Katherine Bubric is a User Experience Researcher with WestJet Airlines, where it is her role to optimize the guest journey across digital and physical touchpoints. Previously, Katherine worked as a Human Factors Specialist for Alberta Health Services, where her goal was to improve patient safety and prevent human error in the healthcare system. Katherine holds an MSc in Human Factors and Ergonomics from Cornell University and a BSc in Psychology from the University of Calgary.
Katherine Bubric is a User Experience Researcher with WestJet Airlines, where it is her role to optimize the guest journey across digital and physical touchpoints. Previously, Katherine worked as a Human Factors Specialist for Alberta Health Services, where her goal was to improve patient safety and prevent human error in the healthcare system. Katherine holds an MSc in Human Factors and Ergonomics from Cornell University and a BSc in Psychology from the University of Calgary.
References
- Anderson J., Gosbee L. L., Bessesen M., Williams L. (2010). Using human factors engineering to improve the effectiveness of infection prevention and control. Critical Care Medicine, 38(8 Suppl), S269–S281. [DOI] [PubMed] [Google Scholar]
- Archer J. R., Wood D. M., Tizzard Z., Jones A. L., Dargan P. I. (2007). Alcohol hand rubs: Hygiene and hazard. British Medical Journal, 335(7630), 1154–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong C. F. (2020). Dividing the emergency department into red, yellow, and green zones to control COVID-19 infection; a letter to editor. Archives of Academic Emergency Medicine, 8(1), e60. [PMC free article] [PubMed] [Google Scholar]
- Devlin A. S. (2014). Wayfinding in healthcare facilities: Contributions from environmental psychology. Behavioral Sciences, 4(4), 423–436. 10.3390/bs4040423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M. (2011). “Inattentional blindness & conspicuity”. Visual Expert. https://www.visualexpert.com/Resources/inattentionalblindness.html [Google Scholar]
- Grissinger M. (2012). ‘Inattentional blindness’: What captures your attention? Pharmacy and Therapeutics, 37(10), 542–555. [PMC free article] [PubMed] [Google Scholar]
- Huelat B. J. (2007). Wayfinding: Design for understanding. The Center for Health Design. [Google Scholar]
- Institute for Safe Medication Practices (ISMP) . (1999). Medication error prevention "Toolbox". https://www.ismp.org/resources/medication-error-prevention-toolbox
- Johanes M., Yatmo Y. (2018). Application of visibility analysis and visualization in hospital wayfinding design. Journal of Architecture and Built Environment, 45(1), 1–8. [Google Scholar]
- Jost T., Ouerhani N., Wartburg R. v., Muri R., Hugli H. (2005). Assessing the contribution of color in visual attention. Computer Vision and Image Understanding, 100(1-2), 107–123. 10.1016/j.cviu.2004.10.009 [DOI] [Google Scholar]
- Nielsen J. (1993). Usability engineering. Morgan Kaufmann. [Google Scholar]
- Reason J. (1995). Understanding adverse events: Human factors. Quality in Health Care: QHC, 4(2), 80–89. 10.1136/qshc.4.2.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders M. S., McCormick E. J. (1993). Human factors in engineering and design (7th ed.). McGraw Hill. [Google Scholar]
- Wickens C. D., Gordon S. E., Liu Y., Lee J. (2004). An introduction to human factors engineering (2nd ed.). Pearson Prentice Hall. [Google Scholar]
- Wickens T. D. (2001). Elementary signal detection theory. Oxford university press. [Google Scholar]
- Zielinska O. A., Mayhorn C. B., Wogalter M. S. (2017). Connoted hazard and perceived importance of fluorescent, neon, and standard safety colors. Applied Ergonomics, 65, 326–334. 10.1016/j.apergo.2017.07.011 [DOI] [PubMed] [Google Scholar]