We read with great interest the study by Chen et al. (1). Recent developments in tissue tracking cardiac magnetic resonance (CMR) have enabled the quantitative assessment of myocardial strain based on three parameters: global radial strain (GRS), global circumferential strain (GCS), and global longitudinal strain (GLS). In addition, strain rate imaging can assess myocardial deformation during the cardiac cycle, including GRS, GCS, and GLS rates. Chen et al. demonstrated that the GCS rate was an independent predictor of the primary endpoint (1). Reportedly, CMR-derived strain parameters are associated with outcomes in hypertrophic cardiomyopathy (HCM) patients. However, different results were observed in these studies. Therefore, we performed a meta-analysis to evaluate the significant differences in CMR strain parameters between HCM patients with and without adverse events. We also investigated the hazard ratio (HR) of CMR-derived strain parameters reported in previous studies. HR is the ratio of the chance of an event occurring in patients with HCM with impaired strain and the chance of an event occurring in patients with HCM with preserved strain.
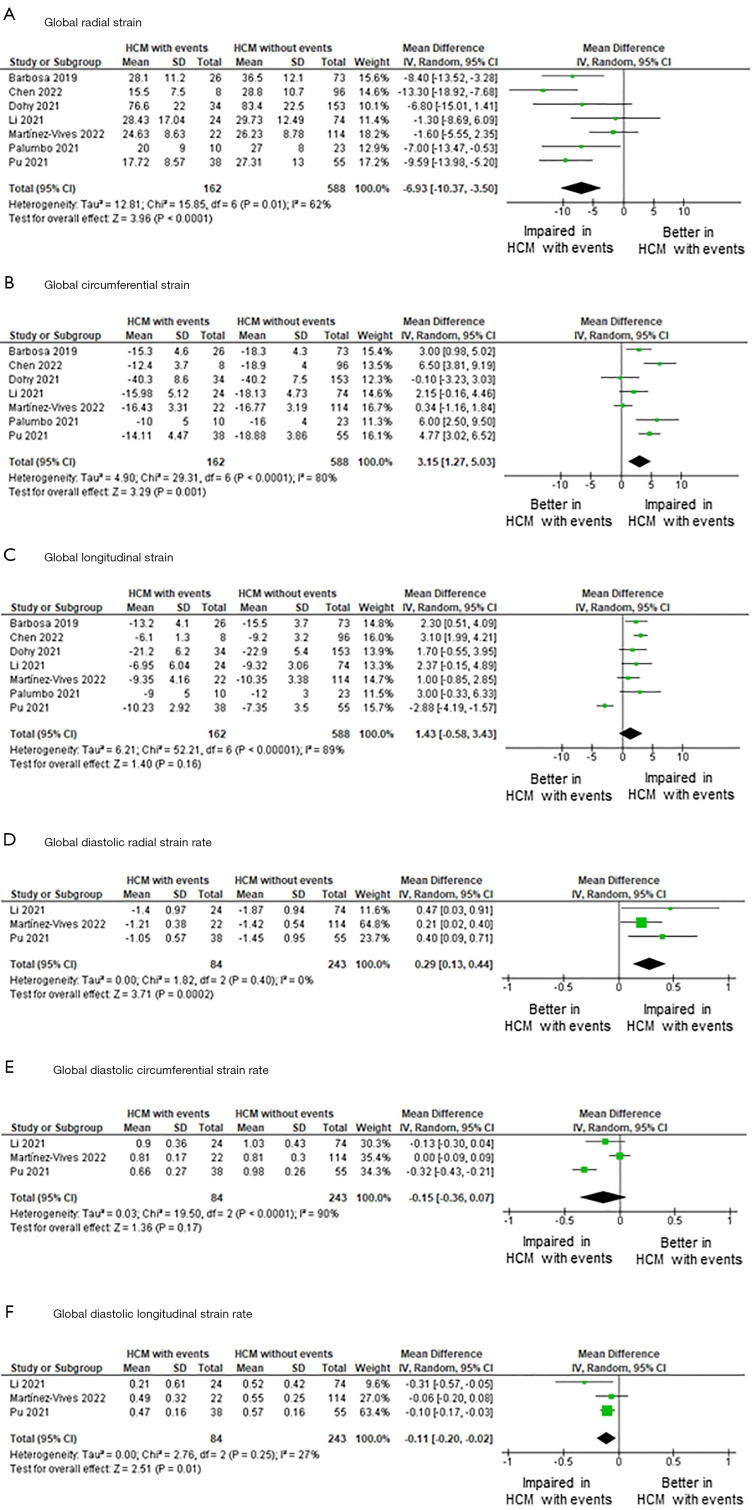
On May 5th, 2022, a literature search was performed using PubMed, Web of Science, the Cochrane library, and Embase using the search terms: (Hypertrophic cardiomyopathy OR HCM OR hypertrophic obstructive cardiomyopathy), (Feature tracking strain OR tissue tracking), (magnetic resonance imaging OR CMR OR MRI), and (Prognosis OR prognostic value OR hazard ratio). We selected eight eligible reports (1-8) based on the inclusion criteria summarized in the Table 1, including 880 patients with HCM. These reports were published between 2019 and 2022. Three reports were from China (1,4,6), two from Italy (5,8), and one each from Portugal (2), Hungary (3), and Spain (7). Seven studies compared the CMR-derived strain values between HCM patients with and without events (1-7). Five studies reported the HR of CMR-derived strains for predicting events (1,3,4,7,8). A random-model meta-analysis was performed using RevMan 5.41 (Cochrane Collaboration, London, UK). Median LVEF was 63.7%, median LV wall thickness was 19.1 mm, and median LVEDVI was 73.6 mL/m2. Figure 1 demonstrates the results of the pooled meta-analysis. Significant differences were found in GRS [mean difference (MD) =−6.93, 95% CI: −10.37 to −3.50, P<0.001, I2=62%, P for heterogeneity =0.01] and GCS (MD =3.15, 95% CI: 1.27 to 5.03, P=0.001, I2=80%, P for heterogeneity <0.001). However, the GLS was similar between the two groups (MD =1.43, 95% CI: −0.58 to 3.43, P=0.16, I2=89%, P for heterogeneity <0.001). There was a significant difference in the diastolic GRS rate (MD =0.29, 95% CI: 0.13 to 0.44, P<0.001, I2=0%, P for heterogeneity =0.40) and diastolic GLS rate (MD =−0.11, 95% CI: −0.20 to −0.02, P=0.01, I2=27%, P for heterogeneity =0.25). However, the diastolic GCS score did not significantly differ between the two groups (MD =−0.15, 95% CI: −0.36 to 0.07, P=0.17, I2=90%, P for heterogeneity <0.001). The hazard ratios of the CMR-derived strain parameters differed substantially in each study (Table 1). Four studies found a significant prognostic value of the diastolic GLS rate (4), GLS (8) and GCS rate (1), and diastolic GRS rate (7), but one study showed no association between strain parameters and adverse events (3).
Table 1. Hazard ratio of CMR-derived feature tracking strain parameters for predicting adverse events in patients with hypertrophic cardiomyopathy.
| Study | Number of HCM patients | Inclusion criteria | Definition of adverse events | Results |
|---|---|---|---|---|
| Dohy 2021 | 187 | Unequivocal diagnosis of HCM and lack of confounding comorbidities | All-cause mortality, heart transplantation, malignant ventricular arrhythmias, appropriate ICD therapy | Strain parameters (GRS, GCS, GLS) were not a significant predictor of adverse events in the multivariable analysis |
| Li 2021 | 98 | Diagnosis of HCM was defined as LV wall thickness ≥15 mm (or ≥13 mm with a family history of HCM) in the absence of other cardiac or systemic diseases responsible for similar myocardial hypertrophy | All-cause mortality, HF-related mortality | Longitudinal peak diastolic strain rate was the most robust predictive marker for adverse events (HR 2.65; 95% CI, 2.21–11.44; P<0.05) |
| Negri 2021 | 130 | The diagnosis of HCM was established in all patients according to the international guidelines | SCD, aborted SCD defined as resuscitated cardiac arrest due to ventricular fibrillation or hemodynamically unstable ventricular tachycardia, hospitalization due to HF | GLS was an independent predictor of outcome events in both the model including 2D strain (HR 1.12; 95% CI: 1.03–1.23, P=0.01) and the model including 3D strain (HR 1.14; 95% CI: 1.01–1.30, P=0.04) |
| Chen 2022 | 104 | The diagnostic criteria followed the 2011 American Heart Association and 2014 European Society of Cardiology guidelines | All-cause mortality, implantable cardioverter-defibrillator discharge due to ventricular fibrillation or tachycardia | GCS was an independent predictor for the primary endpoint (HR 1.58; 95% CI: 1.02–2.44, P=0.039) |
| Martínez-Vives 2022 | 136 | The diagnosis of HCM was established as an otherwise unexplained wall thickness of ≥15 mm in 1 or more left ventricle segments (or ≥13 mm in first degree relatives of patients with HCM) | All-cause death, heart failure hospital admission | GRS systolic strain rate <1.4/s and GRS diastolic strain rate value ≥1.38/s were independent predictors of clinical events (adjusted HR 6.57; 95% CI: 2.01–21.49, P=0.002; adjusted HR 5.96; 95% CI: 1.79–19.89, P=0.004, respectively) |
CMR, cardiac magnetic resonance imaging; HCM, hypertrophic cardiomyopathy; ICD, implantable cardioverter defibrillator; GRS, global radial strain; GCS, global circumferential strain; GLS, global longitudinal strain; LV, left ventricle; HF, heart failure; HR, hazard ratio; SCD, sudden cardiac death.
Figure 1.
Comparison of CMR-derived strain and strain rate parameters between HCM patients with and without events. Forest plot of CMR-derived strain (A-C) and diastolic strain rate parameters (D-F). CMR, cardiac magnetic resonance imaging; HCM, hypertrophic cardiomyopathy.
The prognostic value of CMR-derived strain/strain-rate imaging in patients with HCM continues to be debated. Our meta-analysis showed a significant difference in the GRS, GCS, diastolic GRS rate, and diastolic GLS rate between HCM patients with and without events. Consistent with the current study by Chen et al. (1), we found that GCS scores were significantly impaired in HCM patients with events. Furthermore, although the difference was not statistically significant, the GLS and diastolic GCS scores tended to be impaired in HCM patients with events. These results indicate the potential utility of CMR-derived strain/strain-rate imaging for accurate risk stratification of patients with HCM. Among the five papers evaluating predictive value using the Cox hazard model (1,3,4,7,8), four studies concluded that risk stratification using CMR-derived strain parameters is feasible (1,4,7,8). Another critical point is the cut-off value of the myocardial strain. Among the papers reviewed in this study, only three provided cut-off values. Martínez-Vives et al. (7) reported that GRS detects high-risk HCM with a sensitivity of 85.7%, specificity of 56.1%, and AUC of 0.752 with a cut-off value of 27%. Chen et al. (1) reported that GCS has a sensitivity of 75.0%, specificity of 89.6%, an AUC of 0.87 with a cut-off value of −12.90%, and the GLS with a sensitivity of 78.6%, specificity of 94.4%, and AUC 0.92 with a cut-off value of −6.4%. Pu et al. (6) presented a cut-off value of −14.3% for GCS with an AUC of 0.79. The clinical utility of the CMR-derived strain parameter for risk stratification in patients with HCM must be established in future studies. In the clinical setting, myocardial strain and deformation are mainly analyzed using echocardiography (9). CMR has advantages over echocardiography, including a more objective and reproducible assessment of cardiac function and strain. To date, evidence of CMR-derived strain is insufficient compared to echocardiographic strain. Notably, CMR strain values vary from vendor to vendor and should be considered during clinical use. The accuracy of MRI strain continues to be debated, partly because of its lower temporal resolution (20–30 frames/sec) than echocardiography (50–70 frames/sec). Therefore, accuracy of the strain might be low, especially during strain rate evaluation. However, MRI clearly delineates the endocardial and epicardial planes for strain evaluation. Therefore, more studies are necessary to validate the clinical value of CMR-derived strains in patients with HCM. Finally, the disadvantages of CMR strain should be acknowledged. The CMR strain is inadequate for routine clinical application, and there are still problems that need to be resolved. For example, CMR is a time-consuming test and not all hospitals can perform it. In addition, the time required for cine CMR is longer than that for echocardiography, and the throughput of the test is not good, so advances in high-speed imaging technology are desirable. In addition, the temporal resolution of cine MRI is low and may be inaccurate, especially with respect to diastolic strain. Due to these and many other problems, echo is still the method of choice for strain evaluation in clinical practice rather than CMR.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This work was supported by the Japan Society for the Promotion of Science: Grant-in-Aid for Early-Career Scientists (No. 19K17534 to SK).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-522/coif). The authors have no conflicts of interest to declare.
References
- 1.Chen X, Pan J, Shu J, Zhang X, Ye L, Chen L, Hu Y, Yu R. Prognostic value of regional strain by cardiovascular magnetic resonance feature tracking in hypertrophic cardiomyopathy. Quant Imaging Med Surg 2022;12:627-41. 10.21037/qims-21-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbosa AR, Dias Ferreira N, Martins O'Neill C, Ruivo C, Cruz I, Rocha Lopes L. Impaired myocardial deformation assessed by cardiac magnetic resonance is associated with increased arrhythmic risk in hypertrophic cardiomyopathy. Rev Esp Cardiol (Engl Ed) 2020;73:849-51. 10.1016/j.rec.2020.02.008 [DOI] [PubMed] [Google Scholar]
- 3.Dohy Z, Szabo L, Toth A, Czimbalmos C, Horvath R, Horvath V, Suhai FI, Geller L, Merkely B, Vago H. Prognostic significance of cardiac magnetic resonance-based markers in patients with hypertrophic cardiomyopathy. Int J Cardiovasc Imaging 2021;37:2027-36. 10.1007/s10554-021-02165-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li ZL, He S, Xia CC, Peng WL, Li L, Liu KL, Zhang JG, Pu J, Guo YK. Global longitudinal diastolic strain rate as a novel marker for predicting adverse outcomes in hypertrophic cardiomyopathy by cardiac magnetic resonance tissue tracking. Clin Radiol 2021;76:78.e19-25. 10.1016/j.crad.2020.08.019 [DOI] [PubMed] [Google Scholar]
- 5.Palumbo P, Masedu F, De Cataldo C, Cannizzaro E, Bruno F, Pradella S, Arrigoni F, Valenti M, Splendiani A, Barile A, Giovagnoni A, Masciocchi C, Di Cesare E. Real-world clinical validity of cardiac magnetic resonance tissue tracking in primitive hypertrophic cardiomyopathy. Radiol Med 2021;126:1532-43. 10.1007/s11547-021-01432-x [DOI] [PubMed] [Google Scholar]
- 6.Pu C, Fei J, Lv S, Wu Y, He C, Guo D, Mabombo PU, Chooah O, Hu H. Global Circumferential Strain by Cardiac Magnetic Resonance Tissue Tracking Associated With Ventricular Arrhythmias in Hypertrophic Cardiomyopathy Patients. Front Cardiovasc Med 2021;8:670361. 10.3389/fcvm.2021.670361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martínez-Vives P, Cecconi A, Vera A, Fernández C, López-Melgar B, Sanz-García A, Rojas-González A, Nogales-Romo MT, Hernandez Muñiz S, Olivera MJ, Caballero P, Jiménez-Borreguero LJ, Alfonso F. Usefulness of Tissue Tracking by Cardiac Magnetic Resonance to Predict Events in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol 2022;174:126-35. 10.1016/j.amjcard.2022.03.024 [DOI] [PubMed] [Google Scholar]
- 8.Negri F, Muser D, Driussi M, Sanna GD, Masè M, Cittar M, Poli S, De Bellis A, Fabris E, Puppato M, Grigoratos C, Todiere G, Aquaro GD, Sinagra G, Imazio M. Prognostic role of global longitudinal strain by feature tracking in patients with hypertrophic cardiomyopathy: The STRAIN-HCM study. Int J Cardiol 2021;345:61-7. 10.1016/j.ijcard.2021.10.148 [DOI] [PubMed] [Google Scholar]
- 9.Tower-Rader A, Mohananey D, To A, Lever HM, Popovic ZB, Desai MY. Prognostic Value of Global Longitudinal Strain in Hypertrophic Cardiomyopathy: A Systematic Review of Existing Literature. JACC Cardiovasc Imaging 2019;12:1930-42. 10.1016/j.jcmg.2018.07.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as