Abstract
The Korean government initiated a plan to designate and establish Regional Trauma Centers to reduce the preventable trauma death rate to <20% so as to be on par with advanced countries by 2020. This initiative was undertaken because the reported preventable trauma death rate was close to 40% in South Korea from 1997 to 2009. This review aimed to provide an overview of these Regional Trauma Centers and discuss further development of the trauma care system to assess its performance. As of September 2021, 15 Regional Trauma Centers had been established through a metropolitan-based designation process. Each center has been equipped with Level-I facilities. These Regional Trauma Centers have had 2 positive effects; namely, an increase in the number of severely injured patients attending these centers and a decrease in the national preventable trauma death rate from 30.5% in 2015 to 19.9% in 2017. The establishment of Regional Trauma Centers can lead to improved performance, maximal efficiency, and reduction of preventable deaths in trauma patients. They can also play a key role in prehospital triage and transportation in the trauma care system.
Keywords: Delivery of health care, Injuries, Mortality, Republic of Korea, Trauma centers
INTRODUCTION
Trauma is a leading cause of morbidity and mortality in people aged <40 years in many countries [1]. According to the Korean 2018 Statistics Korea mortality report, traumatic injuries were the third highest cause of death, accounting for 9.2% of total deaths [2,3]. A higher prevalence of trauma has been reported in younger people, affecting twice as many men as women [2,3,4]. The preventable trauma death rate in South Korea is reportedly higher than that in other developed countries, despite declining from 40.5% in 1997 to 39.6% in 2003, 35.3% in 2009, and 30.5% in 2015 [5,6,7]. Trauma can be prevented through proactive interventions addressing environmental, equipment, behavioral, and individual risk factors in the public domain [8]. To intervene, the Korean government initiated a plan to design and establish Regional Trauma Centers to reduce the preventable death rate to <20% so as to be on a par with high-income countries by 2020 [9,10,11].
The Korean government introduced a health insurance system in 1963 and gradually expanded coverage, unifying multiple insurers to provide National Health Insurance (NHI) for universal population coverage in 1989 [12,13]. Simultaneously, healthcare delivery was reorganized into a 3-tier system to improve accessibility, equality, and availability of healthcare services and to meet the population’s health needs, which included a primary level involving clinics, a secondary level involving hospitals and specialist services, and a tertiary level involving university hospitals [14]. However, despite having an Emergency Medical Service (EMS) system in place [15], no optimal care model exists for patients with severe trauma.
An effective trauma care system can be expected to ensure that the right patient receives the right level of care at the right hospital at the right time [16,17]. Maintaining a trauma care system is essential from the prehospital setting through to the rehabilitation process, with a multidisciplinary team required for continuous care [18]. A trauma center forms the basis of an integrated, coordinated, and inclusive trauma system. Considering the importance of trauma care facilities, the Korean government recognized that the trauma care system required financial support and a plan was initiated to designate and establish Regional Trauma Centers in 2012, which involved equipping these Regional Trauma Centers in accordance with American-identified Level 1 requirements, as well as provide comprehensive care, education and training, innovative research, and community programs. By September 2021, 15 Level-1 Regional Trauma Centers had been established through a metropolitan-based designation process in South Korea. This study aimed to provide an overview of these Regional Trauma Centers and to discuss further development of the system to assess their performance.
INTRODUCTION AND DEVELOPMENT OF REGIONAL TRAUMA CENTERS
The Emergency Medical Service in South Korea
Despite the NHI and a tiered healthcare delivery system, EMSs remain underutilized [19]. According to the EMS Act, the EMS system was created as a special law, enforced by statute on January 1, 1995. The law guaranteed the EMS fee schedule and covered EMS management, first aid, and emergency care and transportation [15,20]. An aging population, climate change, and the risk of unexpected disasters or fatal accidents have increased the probability of injuries or emergencies [21]. Since 2000, the EMS fee schedule has been amended and developed to cover EMS costs [20] to ensure a well-functioning EMS.
Designation and establishment of Regional Trauma Centers
In South Korea, the preventable in-hospital trauma death rate has been reported to be higher than the range of 5% to 10% in other developed countries [22]. Moreover, trauma is the leading cause of hospital utilization in all age groups [3]. In terms of medical service access, the absence of effective regional trauma settings has meant that patients who were severely injured could not access appropriate treatment [23]. Therefore, in the 2008–2009 period, the Ministry of Health and Welfare (MOHW) announced a project to build trauma-specific centers and designated 35 centers across South Korea. However, these centers could not provide definitive treatment for trauma patients owing to a lack of specialists and other shortages [4,9,24]. An analysis of 2007 Emergency Department data indicated that the national preventable trauma death rate was 2.5%, while the regions of Seoul and Jeollabuk-do had rates of 1.8% and 4.3%, respectively [22,25]. In terms of patients with severe trauma, the rate was 5.8% for Seoul and 13.0% for Jeollabuk-do. These studies found that accessibility to definitive treatment in the in-hospital phase and differences in regional resource allocation for trauma care greatly affected the preventable trauma death rate.
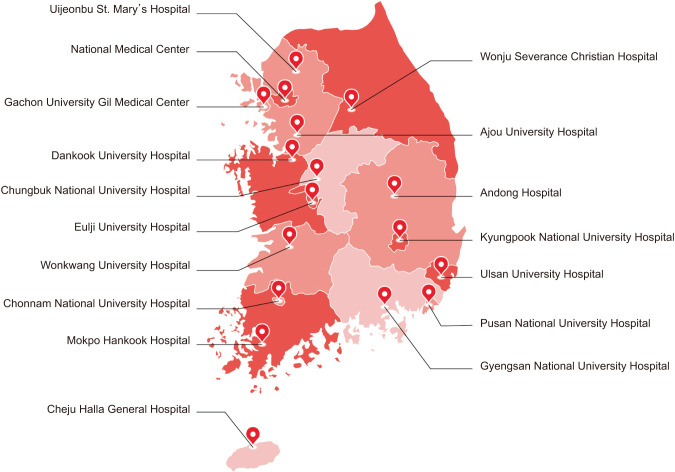
Due to the importance of an effective national trauma care system, the Korean government divided the country into 5 large regions according to whether resources met population and accessibility needs, and designated 17 Regional Trauma Centers based on national standards such as those promulgated by the MOHW by 2017 (Fig. 1) [20]. Government-supported Regional Trauma Centers, with appropriate staffing levels and adequate equipment, were opened in order of designation. Currently, 15 Regional Trauma Centers have been established and play an integral part in the healthcare delivery system in South Korea, with the capacity to treat and rapidly transport patients who are severely injured [15,26,27].
Fig. 1. Designated Regional Trauma Centers.
Financial support for the established Regional Trauma Centers
An Emergency Medical Fund (EMF) was established in 1995, based on Article 20 of the EMS Act. Initially, fund distribution was limited to eligible EMS facilities to compensate for having accepted emergency patients who did not make payments for emergency care services in hospitals. The fund collection source was then changed so that an amount equivalent to 20% of a traffic penalty was used as an EMF under the Road Traffic Act [9,28]. When the region-based trauma-specific center program was initiated in 2010, the government reviewed the use of this fund, ranging from 200 billion Korean won (KRW) to 240 billion KRW (US dollar [USD] 16.7 million–20.0 million), to create an advanced EMS system [9,28]. The government then announced a financial plan for funding assistance to establish Regional Trauma Centers by 2016, totaling 200 billion KRW (USD 16.7 million) [29]. Supporting new Regional Trauma Centers required funding of 8 billion KRW for the initial investment and 2.3 billion KRW annually for operating expenses until November 2016 [9,24]. The financial support for operating expenses has increased significantly owing to the expansion of the number of centers opening and staffing requirements [24].
REGIONAL TRAUMA CENTERS’ GENERAL FEATURES
Facilities and equipment
Most Regional Trauma Centers have been established in alliance with tertiary hospitals within the healthcare system. To ensure effective operations, all designated Regional Trauma Centers need to develop dedicated trauma facilities is equipment available 24 hours a day, including a trauma bay for initiation of assessment and resuscitation, 2 operating rooms for trauma management, trauma interventional radiology, a dedicated 20-bed trauma intensive care unit (ICU), and a dedicated 40-bed trauma ward. Since this regulation is a minimum standard, it can be operated differently for each Regional Trauma Center if necessary. All trauma centers must also have a patient monitoring system, drug infuser, defibrillator, ventilator, operating table, and body temperature controller for trauma patients. Other facilities and equipment aspects of trauma centers may allow sharing with acute care settings located in the designated trauma center. However, it is recommended that the center be used primarily for severe trauma patients [30].
Human resource commitment
Regional Trauma Centers are staffed by various medical and ancillary professionals and each center includes a trauma resuscitation team that promptly responds to the needs of injured patients to improve the rate of preventive trauma death. In South Korea, mechanisms have been developed to manage trauma care human resources at the operational level. A full-time trauma surgeon is dedicated to a single trauma center and is available 24 hours a day, and a physician also works at the center. Although the Korean Society of Traumatology operates a training course for subspecialists in traumatology, this certificate is not a mandatory requirement for working as a trauma surgeon. Furthermore, a full-time trauma surgeon is a member of the trauma resuscitation team, which includes (1) an activation team that must be available in the trauma resuscitation area within 10 minutes and comprises at least 2 general or thoracic surgeons, and an emergency medicine physician, and (2) a back-up team that consists of the same components as an activation team but is available in the emergency room within 60 minutes [30].
Depending on the situation, more specialties could be involved in the trauma resuscitation team [30]. Specifically, all team members, including on-call specialists (anesthesiology, radiology), should coordinate their interventions as defined by the guidelines, with 24-hour continuous and timely attendance within 60 minutes, and an on-call schedule that must be maintained. The trauma coordinator plays a role in registering trauma patients and managing quality using trauma registry data. Trauma program managers are involved in trauma care and lead trauma programs.
QUALITY MANAGEMENT
Morbidity and Mortality Conferences and Quality Assessment Committees
To manage trauma care quality, Regional Trauma Centers must appoint Trauma Quality Assessment Committees (TQA Committees), and Morbidity and Mortality Conferences (M&M Conferences) should be held regularly. The trauma center director, clinical department head, nursing department head, and medical staff participate in the TQA Committee. Typically, TQA Committees should evaluate all types of quality indicators, including the process and time of care, prevention of medical errors, improvement in adherence to medical guidelines, and verification of trauma registry, and move forward with quality improvement projects [30]. Conversely, M&M Conferences involve a discussion of all deaths, complications, adverse events, and errors, and provide opportunities to identify problems, discuss solutions, and act accordingly. Through this process, M&M Conferences can optimize effectiveness and improve the quality of care [1,30].
Assessing Regional Trauma Centers
An assessment program for Regional Trauma Centers was introduced in 2016 not only to establish sustainable quality management systems to reduce mortality and disability among trauma patients but also to maintain well-functioning trauma centers. Regional Trauma Center assessment is conducted every year, and the results are applied in relation to the Trauma Fee, graded A, B, and C, according to quality conditions [31]. The assessment includes a comprehensive evaluation of 8 domains; namely, requirements, quality of care, quality management, function, regional trauma system operating leadership, monitoring, benefits or incentives, utilization, and 63 subindicators [31].
Korean Trauma Data Bank
A Korean Trauma Data Bank (KTDB) was established to enhance the trauma care system by aggregating the national trauma registry in 2013 [32]. A trauma registry is a disease-specific data collection composed of a file of uniform data elements that describe the injury event, prehospital information, demographics (including sex, age, and residence), diagnosis, and outcomes of treatment for injured patients who correspond to S and T codes of Korean Standard Classification of Diseases ver. 7 [32]. The goal of the KTDB is to apply nationally defined standards for data collection and inform decision-makers about a wide variety of issues that characterize the current state of trauma care, including analysis, research, and monitoring.
Trauma fee schedule
The Korean healthcare system has used a fee-for-service payment scheme for both inpatient and outpatient services since the introduction of the health insurance program in 1977 [33]. In this context, Regional Trauma Centers have insisted that the correct fee is subject to meeting the specific features and clinical feasibility of the trauma service [34]. Thus, a fee for trauma management has been set in accordance with the process of trauma care, along with transportation, patient assessment, and emergency operation hospital care since 2018 [34]. Moreover, all trauma fees have been graded according to the result of quality assessment and are paid incentives that are linked to the following levels: (1) level A is subject to an increase of 10% from baseline; (2) level B is a baseline fee; and (3) level C is subject to a 10% reduction from baseline [35]. Additionally, there is another incentive for a trauma service provided by a dedicated surgeon or physician [36].
ADVANTAGES OF THE PROJECT
The current status of establishing Regional Trauma Centers
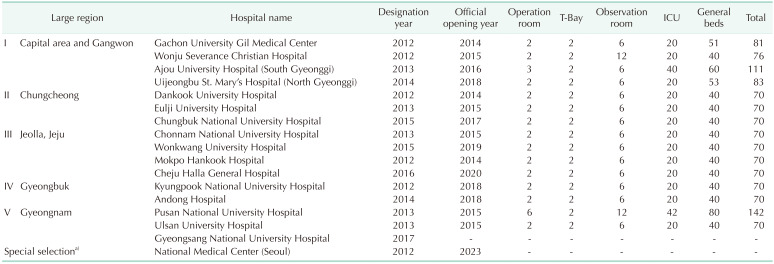
Of 17 Regional Trauma Centers that had been designated for establishment in 5 large regions across South Korea from 2012 through 2017, 5 centers were established in the capital area and Gangwon region, 5 centers in the Jeolla and Jeju region, 3 centers in the Chungcheong and Gyeongnam regions, and 2 centers in the Gyeongbuk region (Table 1) [24,34]. As of 2021, initial trauma center planning has been completed in 15 of 17 designated Regional Trauma Centers. The National Medical Center in the capital area and Gangwon region, designated in 2012, are scheduled to open in 2023 and the Gyeongsang National University Hospital in the Gyeongnam region, designated in 2017, is being prepared for establishment. All 15 Regional Trauma Centers currently operating have dedicated facilities, including resources such as an operating room, 2 resuscitation rooms, 6 observation rooms, an ICU, and general beds for trauma care, according to administrative guidelines. Several centers with a large number of patients are operating by expanding the number of operating rooms, observation rooms, ICUs, and general beds.
Table 1. Current status of the Regional Trauma Centers.
Operational status of the Regional Trauma Centers
Increasing the number of severe trauma patients accessing the Regional Trauma Centers
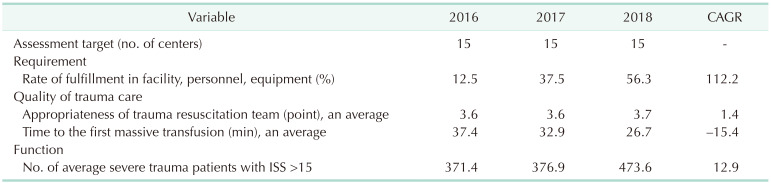
Following the establishment of the Regional Trauma Centers, the number of patients visiting these 15 centers increased by 30.8%, from 24,445 to 31,968 during the 2016–2017 period. In terms of trauma severity, the number of more severely injured patients visiting trauma centers gradually increased. The number of inpatients with an injury severity score >15 increased by 12.9% on average over 3 years (2016–2018) (Table 2) [34]. This increase showed that Regional Trauma Centers can provide adequate and effective care for the number of trauma patients in a given region through the application of strict criteria [7]. Moreover, the formation of a trauma resuscitation team that responds promptly to severely injured patients promotes a well-coordinated multidisciplinary approach.
Table 2. Results of Regional Trauma Center evaluations.
CAGR, compound annual growth rate; ISS, injury severity score.
Data from Heo et al. [34].
Improving performance in the treatment of severe trauma patients
Given the benefits of trauma care and the proven efficacy of a timely approach, it is useful to measure the time to first transfusion as a quality indicator to help reduce the time required for trauma care. The average time to the first transfusion steadily decreased from 37.4 minutes in 2016 to 32.9 minutes in 2017 and to 26.7 minutes in 2018 in these centers [34]. Additionally, a retrospective study compared the 90-day survival rate between patients at a post-trauma center in terms of a massive transfusion protocol (post-TCMTP) group and an interim-TCMTP group during the 2010–2016 period at a single Regional Trauma Center in South Korea and showed that the post-TCMTP group had a 1.3-fold higher survival rate than the interim-TCMTP group (75.8% vs. 56.3%, log-rank P = 0.027) [37]. Consequently, shortening the time to the first transfusion is likely to enhance the likelihood of more effective outcomes in well-functioning appropriate facilities, with well-trained trauma resuscitation teams, and well-allocated resources [7].
Reduction in the preventable trauma death rate
According to a study investigating preventable trauma deaths in South Korea, the national preventable trauma death rate has substantially improved (40.5% in 1997, 30.5% in 2015, and 19.9% in 2017) [6,11,38,39]. In 2015 and 2017, Gwangju, Jeolla, and Jeju regions showed the greatest level of improvement among the 5 divided regions, with a 14.8% reduction from 40.7% in 2015 to 25.9% in 2017 [38,39]. However, in the Seoul, which had yet to establish Regional Trauma Centers, the preventable trauma death rate had reduced only slightly by 0.6%, from 30.8% in 2015 to 30.2% in 2017.
One aspect affecting the preventable trauma death rate involves rapid transport to the trauma center [39]. The preventable trauma death rate was 15.5% when patients had been promptly transported from a disaster site directly to a trauma center without going through another hospital, which was significantly lower than the 31.1% rate when arriving at another hospital, or the 40.0% rate when being transferred from more than one other hospital. Furthermore, when transported to a trauma center by one of the 119 ambulances available, the preventable trauma death rate was 15.6%, which was lower than that using other modes of transport. Efforts are being made to operate the Regional Trauma Centers more efficiently by improving transportation systems and utilizing trauma resources more effectively.
Expanding the use of the trauma registry
The KTDB is a disease-specific data collection composed of a file of uniform data elements that describe the injury event, demographics, prehospital information, diagnosis and care information, and treatment outcomes of injured patients, making it possible to examine the composition of patients and injuries, the epidemiology of injury, and patient outcomes in each center. This information can be used for specific purposes: preparation of annual emergency medical reports, sample data for evaluating mortality, preparation of policy documents, and evaluation of Regional Trauma Centers.
DISCUSSION
By September 2021, 15 Regional Trauma Centers had been designated in South Korea. Several target performance measures had been met, including increasing the volume of severe trauma patients to the centers, reducing the preventable trauma death rate, and expanding the use of the Trauma Registry. Despite substantial support from the government for the establishment and operation of these 15 Regional Trauma Centers, they face operational limitations as discussed below.
Lack of trauma surgeons
The lack of trauma surgeons in the Regional Trauma Centers can be attributed to the dedicated surgeon system and the medical education program. Initially, the dedicated surgeon system was introduced solely to develop the Regional Trauma Centers, and the trauma surgeon working in a center was dedicated solely to trauma surgery. This system has led to surgeons avoiding working at Regional Trauma Centers [40]. Furthermore, it leads to a reluctance to increase the number of trauma surgeons to meet the functional needs of the team, regardless of the volume of trauma surgery, due to the burden of their maintenance. Therefore, “personnel requirements” and “trauma resuscitation team composition” indicators did not achieve 100% from 2016 through 2018 [34]. These results indicated that the shortage of trauma specialists due to the dedicated surgeon system has remained an unresolved issue.
Another reason for the lack of trauma surgeons relates to deficiencies in trauma medicine in terms of medical education and training programs, which has resulted in low numbers of applicants for trauma surgery fellowships and difficulties maintaining high-quality personnel, because of a poor understanding of trauma care. Currently, working trauma surgeons have been negatively affected due to increased workloads, inadequate compensation and quality of life, and restrictions on promotion and career, which further depletes the number of trauma surgeons.
Delivering high-quality trauma care depends on the availability of skilled human resources. Therefore, efforts to provide opportunities for trauma surgeons should involve the development of training programs [41,42] and the addition of non-trauma emergency surgery to trauma surgery responsibilities [42]. Additionally, to promote the management and sustainability of the Regional Trauma Centers, trauma resuscitation teams should be rewarded with additional monetary compensation.
Inadequate trauma quality management systems
Regional Trauma Centers have engaged in regular evaluations to improve trauma care as one quality indicator measure. These evaluations cannot be completed using comprehensive quality management because the relevant indicators do not focus on a sufficiently wide variety of clinical results nor identify the optimal care of trauma patients, including risk-adjusted outcome measures. Moreover, quality evaluation must consider the trauma care undertaken to achieve the desired goal and objectives; however, the trauma registry is not appropriate for use in evaluating quality adequacy because all of the required data are not contained in the trauma registry.
In the United States, trauma centers are by volunteers and are selected to participate in a Trauma Quality Improvement Program (TQIP) for quality improvement. The TQIP aims to provide risk-adjusted data to reduce variability in adult trauma outcomes, offer best practice guidelines to improve trauma care, and allow trauma centers to evaluate their performance relative to other centers objectively. In this way, the TQIP provides an opportunity for comprehensive quality management by enhancing data validity in the trauma registry and by using a risk-adjusted benchmarking system to measure performance and outcomes. Therefore, it is essential to apply a comprehensive quality management system for the Regional Trauma Centers, including providing a reevaluation mechanism in the designation phase, facilitating personnel support for accurate data collection, developing a rigorous process to standardize data and risk adjustment, and designing a quality improvement program with a self-reflective tool.
Underutilization of the Korean Trauma Data Bank
The trauma registry is a rich source of quality management information for trauma care [1]. To improve patient outcomes, trauma centers must also use data to evaluate how to improve quality, safety, and medical interventions at the organizational level [43]. The American College of Surgeons Committee on Trauma strives to ensure high-quality data for the National Trauma Data Bank dataset, which is the largest aggregation of trauma registry data [17,44]. In South Korea, following planning of the Regional Trauma Centers, mechanisms for data collection in relation to trauma care and a data entry form were created. The data populating the trauma registries (the National Emergency Department Information System or the KTDB) need to be as reliable as possible. However, the data in these trauma registries cannot be readily used. The number of studies using trauma data is increasing, but efforts to link research findings to policy improvement or trauma education are insufficient. Therefore, at the academic or professional level, it is necessary to continue to develop ways to use the KTDB more effectively; for example, through providing funds to support research activities when answering essential questions across the continuum of injury care or encouraging the use of trauma registry data for research. There is also a need to develop an ongoing monitoring system based on standardized data to assess not only the available performance indicators of trauma centers but also the injury events and the treatment of injured patients. Analyses can be expanded using such trauma data.
The need for a comprehensive trauma system
Since the establishment of Regional Trauma Centers, trauma resuscitation team performance has improved, with an increase in the number of severe trauma patients attending the centers, a reduction in the time to the first transfusion, and a decrease in preventable trauma death rates. As inappropriate prehospital triage and transportation might increase the risk of preventable trauma death rates [6,39,45], trauma care must be initiated in the field to ensure a continuum in trauma care. Additionally, the strong role of trauma system organization in Regional Trauma Centers demonstrates effective trauma care system leadership; however, this involves the provision of leadership to individual hospitals. Given that the pilot project is underway in Gangwon, Incheon, Jeju, and Gyeonggi, it can lead to the role of developing a regional trauma system. Therefore, it is essential to establish a comprehensive trauma system for injured patients encompassing all phases of care [46,47].
CONCLUSIONS
This review examined the designation and establishment of Regional Trauma Centers in South Korea. These centers were designated to provide rapid response emergency care 24 hours, 7 days/week for multiorgan failure and patients with massive blood loss, and optimal treatment with high-quality facilities, equipment, and personnel at specialized facilities. Regional Trauma Centers are critical in the first phase of developing a trauma system and in addressing challenges to providing optimal care to trauma patients. Additionally, the establishment of Regional Trauma Centers has led to improved performance and reduced preventable death rates for trauma patients, played a key role in prehospital triage, transportation coordination during all aspects of treatment, and allowed leadership to be demonstrated in developing a comprehensive trauma system in 5 regions of South Korea.
A trauma care system is initiated to reduce preventable trauma death rates and enhance patient recovery [47]. Over the past 10 years, Regional Trauma Centers have improved the treatment of severe trauma patients in South Korea. Establishing an inclusive regional trauma system is necessary to maximize treatment efficiency for severely injured patients. Most trauma patients can now receive appropriate care within their region because the benefits of creating these centers include the efficient use of all available resources, reduction in the potential occurrence of the injury events, and improvement in trauma quality through regional committees.
Footnotes
Fund/Grant Support: None.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization, Project Administration: JK.
- Formal Analysis, Visualization: EWS.
- Investigation: EWS.
- Data Curation, Methodology: JI.
- Supervision, Validation: KJ.
- Writing – Original Draft: JI, EWS.
- Writing – Review & Editing: JK, KJ.
Availability of Data and Materials
All data generated or analyzed during this study are available in the “Statistics Annual Report” section of the homepage of the Korean National Emergency Medical Center. However, the original text is not provided in English. (https://www.e-gen.or.kr/nemc/statistics_annual_report.do?brdclscd=04).
References
- 1.World Health Organization (WHO) Guidelines for trauma quality improvement programme [Internet] WHO Press; 2009. [cited 2022 Jul 12]. Available from: https://apps.who.int/iris/handle/10665/4406 . [Google Scholar]
- 2.Statistics Korea. Annual report on cause of death statistics [Internet] Statistics Korea; 2019. [updated 2020 Sep 20]. [cited 2022 Jul 12]. Available from: https://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&bSeq=&aSeq=385219&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= [Google Scholar]
- 3.Statistics Research Institute. Korean social trends 2018 [Internet] Statistics Korea: 2018; [updated 2018 Dec 14]. [cited 2022 Jul 12]. Available from: http://kostat.go.kr/sri/srikor/srikor_pbl/7/2/index.board?bmode=read&bSeq=&aSeq=372068&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= [Google Scholar]
- 4.Park DJ, Park CY, Cho HM, Lee KH, Han HS. Current status and future prospects of trauma centers in Korea. J Korean Med Assoc. 2017;60:530–532. [Google Scholar]
- 5.Ministry of Health and Welfare (MOHW) Press release: The nationwide ‘preventable trauma mortality rate’ significantly improved from 30.5% to 19.9% [Internet] MOHW; 2019. Dec 11, [cited 2022 Jul 12]. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=351836 . [Google Scholar]
- 6.Kwon J, Lee JH, Hwang K, Heo Y, Cho HJ, Lee JC, et al. Systematic preventable trauma death rate survey to establish the region-based inclusive trauma system in a representative province of Korea. J Korean Med Sci. 2020;35:e417. doi: 10.3346/jkms.2020.35.e417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu B, Lee G, Lee MA, Choi K, Hyun S, Jeon Y, et al. Trauma volume and performance of a regional trauma center in Korea: initial 5-year analysis. J Trauma Inj. 2020;33:31–37. [Google Scholar]
- 8.Christoffel T, Callagher SS. Injury prevention and public health: practical knowledge, skills, and strategies. 2nd ed. Johns and Bartlett Publisher; 2006. [Google Scholar]
- 9.Yoon HD. Background and progress of regional trauma center development. J Korean Med Assoc. 2016;59:919–922. [Google Scholar]
- 10.Jung K, Lee JC, Kim J. Injury severity scoring system for trauma patients and trauma outcomes research in Korea. J Acute Care Surg. 2016;6:11–17. [Google Scholar]
- 11.Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci. 2019;34:e65. doi: 10.3346/jkms.2019.34.e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin YS. 30 years of Korean Health Insurance: its success, failure, and future directions. J Korean Med Assoc. 2007;50:568–571. [Google Scholar]
- 13.Choi E, Kim J, Lee W. Health care system in Korea. Korea Institute for Health and Social Affairs; 1998. [Google Scholar]
- 14.Cho JK. An improvement plan for health care delivery system. Health Welf Policy Forum. 2010;11:6–15. [Google Scholar]
- 15.Im J. Improved status of EMS schedule and its issues. HIRA Policy Brief. 2020;14:26–36. [Google Scholar]
- 16.Martin RS, Meredith JW. In: Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th ed. Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Elsevier, Inc.; 2017. Management of acute trauma; pp. 409–448. [Google Scholar]
- 17.Committee on Trauma, American College of Surgeons. Resources for optimal care of injured patients. American College of Surgeons; 2014. [Google Scholar]
- 18.David BH, Coimbra R, Winchell RJ. In: Sabiston textbook of surgery: the biological basis of modern surgical practice. 16th ed. Townsend CM, Sabiston DC, editors. W.B. Saunders; 2001. Management of acute trauma; pp. 311–344. [Google Scholar]
- 19.Oh YH. Current problems of EMS and a plan for its improvement in Korea. KIHASA Issue Focus. 2011;(105):1–8. [Google Scholar]
- 20.Seo EW, Im J. A review of quality management and improvement of trauma fee schedule in regional trauma center. Health Policy Manag. 2021;31:399–408. [Google Scholar]
- 21.Yoo IS. The current status of affairs in emergency care system. HIRA Policy Brief. 2015;9:17–30. [Google Scholar]
- 22.Kim Y, Shin SD, Park JH, Lee TJ, Park CB, Lee YT, et al. A study on building and operational modeling of Korean regional trauma center. Ministry of Health and Welfare; 2010. [Google Scholar]
- 23.Ministry of Health and Welfare (MOHW) A handbook of a regional trauma center project. MOHW; 2013. [Google Scholar]
- 24.Park JM. Outcomes of the support services for the establishment of regional level 1 trauma centers. J Korean Med Assoc. 2016;59:923–930. [Google Scholar]
- 25.Kim Y, Kang DW, Ro YS, Park SB, Park JH, Park CB, et al. A study on the construction of trauma medical service system. Ministry of Health and Welfare; 2011. [Google Scholar]
- 26.Hendrikson H. The right patient, the right place, the right time: a look at trauma and emergency medical services policy in the States. National Conference of State Legislatures; 2012. [Google Scholar]
- 27.Institute of Medicine. Emergency medical services at the crossroads. The National Academies Press; 2007. [Google Scholar]
- 28.Ministry of Health and Welfare (MOHW) Press release: The National Assembly passes the revised Emergency Medical Service Act [Internet] MOHW; 2008. Aug 10, [revised 2012 Aug 16]. [cited 2022 Jul 12]. Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=817&CONT_SEQ=202891 . [Google Scholar]
- 29.Baek HS, Lee JH, Kim LS, Park HS, Park SS. EMS fund, it is functioning or fumbling? J Korean Clin Health Sci. 2013;1:35–45. [Google Scholar]
- 30.Ministry of Health and Welfare. Administrative guidelines for regional trauma center. National Emergency Medical Center; 2020. [Google Scholar]
- 31.Ministry of Health and Welfare. 2021 Guidelines for quality assessment of regional trauma center. National Emergency Medical Center; 2020. [Google Scholar]
- 32.Ministry of Health and Welfare. 2019 Annual report on Korea trauma data bank. National Emergency Medical Center; 2020. [Google Scholar]
- 33.Shon C, You M. Evaluation of health policy governance in the introduction of the new DRG-based hospital payment system from interviews with policy elites in South Korea. Int J Environ Res Public Health. 2020;17:3757. doi: 10.3390/ijerph17113757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heo YJ, Im J, Lee TH, Seo EW, Yoon SY, Kim SW, et al. A study on building operation standardization for regional trauma centers. Ministry of Health and Welfare; 2019. [Google Scholar]
- 35.Health Insurance Review and Assessment Service (HIRA) A handbook of medical benefit cost in National Health Insurance. HIRA; 2018. [Google Scholar]
- 36.Health Insurance Review and Assessment Service (HIRA) A handbook of medical care benefit cost in National Health Insurance. HIRA; 2021. [Google Scholar]
- 37.Hwang K, Kwon J, Cho J, Heo Y, Lee JC, Jung K. Implementation of trauma center and massive transfusion protocol improves outcomes for major trauma patients: a study at a single institution in Korea. World J Surg. 2018;42:2067–2075. doi: 10.1007/s00268-017-4441-5. [DOI] [PubMed] [Google Scholar]
- 38.Kim Y, Park SK, Jung K, Cho HM, Park CY, Yoon JH, et al. Evaluation of preventable trauma death rate and development of operational management plan for regional trauma center. Ministry of Health and Welfare; 2017. [Google Scholar]
- 39.Kim Y, Jung K, Kwon J, Heo Y, Moon JH, Hwang K, et al. A study on evaluation of preventable trauma death rate. Ministry of Health and Welfare; 2019. [Google Scholar]
- 40.Lee M, Lee G, Lee J, Yu B. Surgical volumes in a regional trauma center: is it enough? J Acute Care Surg. 2020;10:10–12. [Google Scholar]
- 41.Richardson JD, Miller FB. Will future surgeons be interested in trauma care? Results of a resident survey. J Trauma. 1992;32:229–235. doi: 10.1097/00005373-199202000-00020. [DOI] [PubMed] [Google Scholar]
- 42.Moore HB, Moore PK, Grant AR, Tello TL, Knudson MM, Kornblith LZ, et al. Future of acute care surgery: a perspective from the next generation. J Trauma Acute Care Surg. 2012;72:94–99. doi: 10.1097/TA.0b013e31823b990a. [DOI] [PubMed] [Google Scholar]
- 43.Drake SA, Wolf DA, Meininger JC, Cron SG, Reynold T, Wade CE, et al. Methodology to reliably measure preventable trauma death rate. Trauma Surg Acute Care Open. 2017;2:e000106. doi: 10.1136/tsaco-2017-000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Committee on Trauma Leadership, American College of Surgeons. National Trauma Data Bank 2016 Annual Report. American College of Surgeons; 2016. [Google Scholar]
- 45.Seo GJ, Yoo IS, Lee KH, Heo T, Lee JE, Hong ES, et al. Improvement of prehospital emergency care. Ministry of Health and Welfare; 2011. [Google Scholar]
- 46.National Health Service (NHS) Regional networks for major trauma: NHS Clinical Advisory Groups report, September 2010. NHS; 2010. [Google Scholar]
- 47.Committee on Trauma, American College of Surgeons. Regional trauma systems: optimal elements, integration, and assessment systems consultation guide. American College of Surgeons; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are available in the “Statistics Annual Report” section of the homepage of the Korean National Emergency Medical Center. However, the original text is not provided in English. (https://www.e-gen.or.kr/nemc/statistics_annual_report.do?brdclscd=04).