Abstract
Background:
The use of coring instrumentation for osteochondral allograft (OCA) transplantation of the femoral trochlea is challenging due to the complex topography of this anatomical area.
Purpose:
We sought to determine the effect of flat guides versus guides contoured to the surface of the trochlea on graft step-off in trochlear OCAs performed on a foam bone model. We also determined the effect of surgeon experience level and graft size on step-off.
Study Design:
Controlled laboratory study.
Methods:
Allograft harvesters were produced in 3 different sequential sizes with either a flat or a contoured undersurface. The guides matched one another in all aspects of shape and size except for the undersurface contour. The contoured undersurface generally matched the surface of the bone model trochlea but was not customized to that surface. A total of 72 foam femora were obtained. Identical trochlear stellate lesions of 3 different sizes (small, medium, and large) were created using 3-dimensional printed surface templates. A total of 6 surgeons (3 attending and 3 resident surgeons) performed OCAs of each trochlear lesion. Each surgeon performed 1 graft for each size and each guide type (n = 6 per surgeon). A specialized digital caliper was prepared that allowed the measurement of graft step-off to within 0.01 mm at a distance of 5 mm between the 2 sensors. The measurements were performed at 8 positions around the clockface of the grafts.
Results:
Grafts performed with the contoured guides had a mean step-off of 0.43 ± 0.37 mm. Grafts performed with the flat guides had a mean step-off of 0.74 ± 0.78 mm (P < .0001). Experience level did not have a significant effect on graft step-off (P = .81). There was no identifiable pattern indicating higher step-off at any one position on the clockface.
Conclusion:
In this study, contoured grafts had significantly lower step-offs compared with flat guides. Experience level, clockface position, and graft size did not affect step-off.
Keywords: patellofemoral, trochlea, cartilage, osteochondral allograft, knee
Osteochondral allografts (OCAs) play an important role in the treatment of articular cartilage lesions of the patellofemoral joint and address a spectrum of pathologies including full-thickness cartilage lesions, patellofemoral osteoarthritis, avascular necrosis, and trochlear dysplasia. A number of groups have published the results of this procedure 1,4,6,9,11,12,14 with success varying from 10-year survivorship of up to 91% 1 to as low as 37% 4 when larger shell grafts were used. Many surgical techniques for osteochondral allografting have been developed to treat trochlear lesions. These include free-hand methods and, more recently, the application of coring techniques commonly used on the femoral condyles. Despite these advances, grafting of the trochlea remains challenging due to the complex topography of this anatomic region.
An articular step-off of as small as 0.5 to 1 mm has been associated with a significant increase in contact pressures and may contribute to early failure of an OCA. 5,7,8 In addition, owing to variations in morphology, a diseased trochlea may not have the same concavity as a “normal” trochlea, making resurfacing with a coring system even more challenging. With fresh OCAs for the trochlea potentially costing more than US$11,000 based on pricing in our community, the surgeon has little room for error to prepare and implant an optimal graft for a given lesion. In order to optimize graft congruity and to limit step-off, the anteroposterior and mediolateral position of the donor and recipient must match each other precisely. Furthermore, the angle of entry for the recipient site creation and donor graft harvest for the cylindrical cores must also be identical to avoid obliquity and step-off after insertion. 7
Addressing these concerns to consistently match the position, depth, and structure of the graft donor and recipient sites has led to the development of a contoured guide system for the trochlea. These guides are designed to be positioned on the donor and recipient trochleae to obtain identical donor and recipient circumferential topography to minimize graft step-off. Other potential advantages of contoured guides include the use of larger grafts and a decrease in surgical time. This is in contrast to traditional flat guides that limit the reproducibility and accuracy of OCA harvesting and increase the likelihood of donor-recipient mismatch and incongruity.
The purpose of this study was to evaluate the reproducibility and ease of use of the new contoured coring system for OCA transplantation of the femoral trochlea. Our hypotheses were as follows: (1) contoured guides would produce smaller step-offs than flat guides; (2) attending surgeons would have smaller step-offs than resident trainees; (3) grafts with larger circumferences would have larger step-offs than smaller grafts; and (4) the proximal and distal margins of the osteochondral grafts, typically the most difficult to match on the trochlea, would benefit more from contoured guides than the medial and lateral margins of the grafts.
Methods
Allograft Harvester Design
Donor allograft harvesters were designed and made from stainless steel in 3 different sequential sizes, with inner diameters of 37.5, 32.5, and 27.5 mm. These accommodated coring reamers with inner diameters of 32.5, 27.5, and 22.5 mm used to obtain the cylindrical grafts. Recipient harvesters were fabricated in the same way as the donor guides and sized to fit within the donor harvesters. They had an outer diameter of 37, 32, and 27 mm, respectively, and a central 2.5-mm channel for placement of a guidewire for recipient site preparation. A 2.5-mm guidewire was placed into the central channel and then the appropriately sized recipient reamer was used to create the recipient site. These reamers were produced with a radius of 32.5, 27.5, and 22.5 mm.
The harvesters were made with either a flat undersurface or a contoured undersurface closely matching the shape of the femoral trochlea (Figure 1). The flat guides were structurally similar to a number of commercially available guides on the market. We chose to fabricate the flat guides in this study rather than use commercially available flat guides in order to eliminate any differences in structure between the 2 types of guides with the exception of the undersurface contour. In order to standardize the trochlea, we used a widely used generic femoral foam bone model obtained commercially (item 1129-20; Sawbones). The contoured guide system used in this study can be fabricated with various depths of the concavity. We selected the specific contoured guide that best matched the surface topography of the foam femoral trochlea used in this study. With the exception of the undersurface, the same contoured and flat guide design was used for the entire study.
Figure 1.
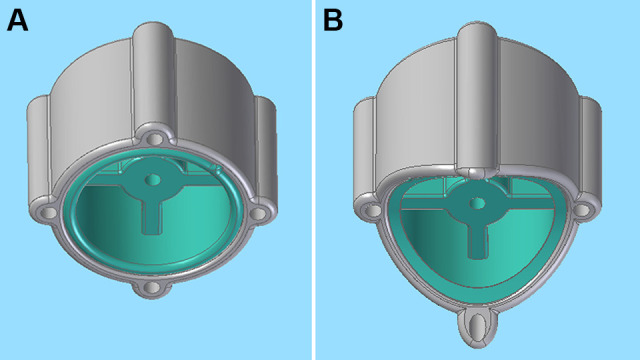
Undersurface of a matched interlocking pair of donor and recipient (A) flat guides and (B) contoured guides.
Allograft Procedure on Foam Bone Models
A total of 72 large right foam femora were obtained. Trochlear surface templates with identically shaped and localized stellate lesions of 3 different sizes (small, medium, and large) were 3-dimensionally printed. These were placed on the foam bone model trochlear surface and the lesions were outlined with a permanent marker, creating identical target lesions on the trochlea of the specific size based on the template used. A total of 6 surgeons—3 fellowship-trained attending surgeons specializing in sports medicine and cartilage repair and 3 junior residents (postgraduate year 3 or lower)—participated in the performance of the allograft procedures on the foam models. Half of the femurs were assigned as the “diseased” group and the other half were the donor femurs from which the grafts were harvested. In each case, the surgeon performed a small, medium, and large allograft harvest and transplantation with both a contoured and a flat guide (total of 6 procedures) in the order of their own preference (Figure 2).
Figure 2.
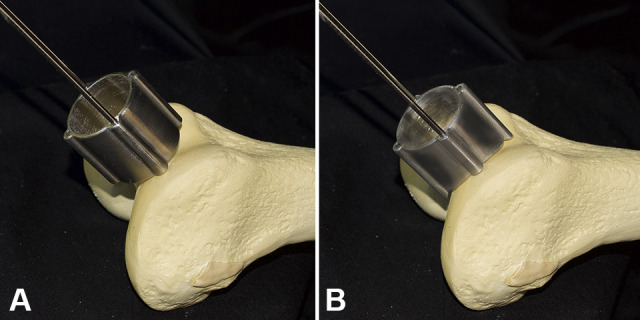
(A) A flat donor-harvesting guide and (B) a contoured donor-harvesting guide placed on the trochlea of a foam femoral model and held in place with peripheral pins.
The surgeon obtained the desired allograft cores from one of the femurs using the harvesting guide, either flat or contoured. The surgeon subsequently prepared the recipient site on another femur using a 4-blade cannulated reamer from the set to achieve a press-fit graft. The specimens were numbered, and all identifiable information including the surgeon performing the procedure and the type of guide used was deidentified.
Graft Step-Off Measurements
A specialized digital caliper was prepared that allowed the measurement of graft step-off to within 0.01 mm at a distance of 3 mm between the 2 sensors (Figure 3A). A commercially available digital caliper was used (Neiko; Amazon). A caliper attachment accessory set (Colibrox; Amazon) was used with each of the 2 attachment accessories being glued in a parallel configuration to a separate limb of the digital caliper. To find a suitable tip, the tips from a retaining ring plier set (Chanellock) were used with each tip being screwed into the end of the caliper accessory holder. This led to robust fixation of the tips coming off the end of the caliper in such an orientation to allow measurement of the displacement in the same axis as the caliper. Next, the caliper was held vertically with the 2 tips placed on a flat metal surface. The caliper was zeroed. The zeroed caliper was placed by hand perpendicular to the area of the trochlear grafts to be sampled with one tip contacting the graft and the second tip contacting the surrounding native foam bone. The measured absolute value of the step-off was measured as the displacement between the 2 tips upon being pressed on the interface between the graft and surrounding foam bone. This was taken directly from the digital caliper reading (Figure 3B). The measurements were performed at 8 positions around the clockface of the grafts.
Figure 3.
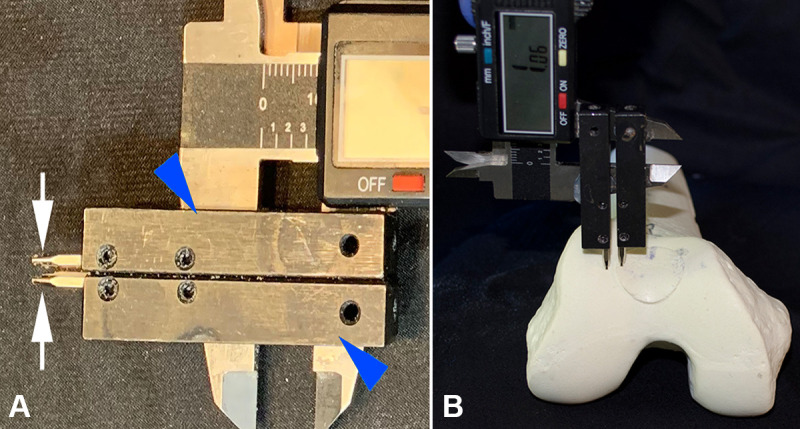
(A) A modified digital caliper used for measuring graft step-off. The rectangular caliper accessories were glued sequentially to each leg of the caliper (blue arrowheads). A 1.2-mm metal tip (white arrows) had been attached to each caliper accessory and screwed in place with an Allen wrench. The 2 metal tips were approximately 3 mm apart. (B) After zeroing the caliper on a flat metal surface, the caliper was applied manually to each zone for step-off testing by placing it perpendicular to the surface to be tested and measuring the absolute step-off directly from the caliper screen.
Two of the authors (Z.C.L. and M.H.) measured the step-off between the graft and the surrounding foam joint surface on 2 different occasions, for a total of 4 measurements per position for a total of 32 measurements per graft. Reliability of step-off measurements was analyzed using the intraclass correlation coefficient, with a random-effects model to control for clustering.
Statistical Analysis
Results were reported as median and interquartile range of step-off values using box-and-whisker plots. A mixed-effects analysis of variance (ANOVA) was used to test for the effects of experience (attending versus resident), clockface position, graft size (small, medium, and large), and guide type (flat versus contoured) on the absolute value of the height of the step-off. The step-off value was log-transformed to achieve normality for the ANOVA. All analyses were performed using SAS software for Windows (Version 9.4; SAS Institute Inc).
Results
The intraclass correlation coefficient for intraobserver reliability was 0.96 for both observers and for interobserver reliability was 0.97, indicating excellent reliability. Grafts performed with contoured guides had a significantly smaller step-off compared with those performed with flat guides (0.43 ± 0.37 versus 0.74 ± 0.78 mm; P < .0001). After data were normalized by logarithmic conversion, graft size was noted to have a statistically significant effect on step-off (P = .014). Graft position along the clockface and graft size also had a significant effect on graft step-off (P < .0001). However, after performing a Tukey test for multiple comparisons, step-off for medium grafts was significantly different from small and large grafts, but step-off was not significantly different between small and large grafts. When looking at various graft positions for both the flat and the contoured guides, there was no pattern to indicate higher step-off in any one position on the clockface (Figure 4).
Figure 4.
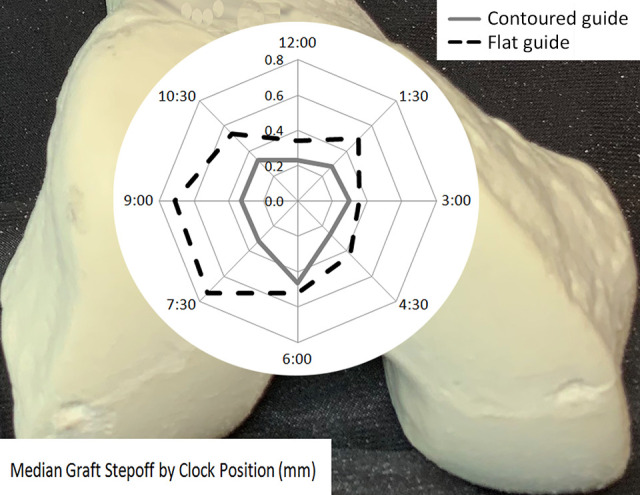
Graphical representation of median graft step-off on polar coordinates demonstrating improved graft step-off with the contoured guides. A photograph of a sample trochlea is shown in the background to clarify the positions described.
Median step-off was 0.31mm for contoured guides and 0.50 mm for flat guides. Median step-off was 0.39mm for residents and 0.38mm for attendings. Median step-off was 0.42mm for small grafts, 0.30mm for medium grafts, and 0.48mm for large grafts. The differences between residents and staff were quite small and did not reach statistical significance for this small cohort (P = .81). Figure 5 shows box-and-whisker plots depicting the differences between various parameters, including guide type, experience level, and graft size.
Figure 5.
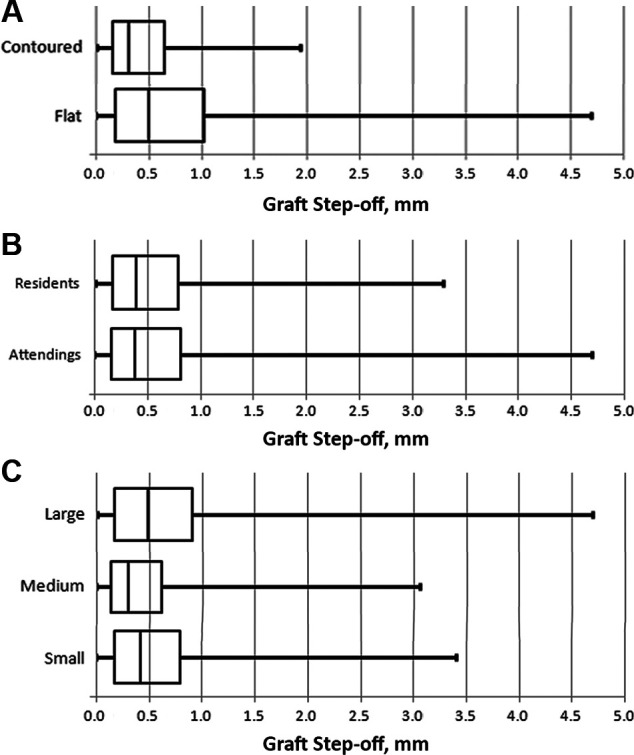
Box-and-whisker plots comparing graft step-off between (A) contoured and flat guides, (B) attending surgeons and resident surgeons, and (C) large, medium, and small grafts. The middle line represents the median, the sides of the box represent the interquartile range, and the error bars represent the minimum and maximum values.
Discussion
In this study, we sought to determine the factors that would optimize the performance of trochlear OCAs in a foam bone model—surgeon experience, graft size, harvester type, and location along the margin of the graft—with the primary study endpoint being graft step-off.
The first hypothesis, that contoured guides would result in smaller step-offs than flat guides, was supported. Furthermore, the 42% decreased step-off for the contoured guides relative to the flat guides could positively affect graft survival and knee function. A clear representation of this difference is seen when median graft step-off is plotted on polar coordinates in terms of graft position. Our second hypothesis, that attending surgeons would perform better than residents, was not supported, as the residents performed at a high level, with no difference relative to attending surgeons. Our third hypothesis was that large grafts would have larger step-offs than small grafts, and although graft size was a statistically significant factor in the ANOVA, it did not follow a logical progression. In other words, the medium grafts had a smaller median step-off (0.30 mm) relative to small and large grafts (0.42 and 0.48 mm). As a result, this hypothesis was not supported. Finally, we hypothesized that the step-offs would be larger at the proximal and distal margins of the osteochondral grafts relative to the medial and lateral margins. Although position was a significant factor as a whole, there was no pattern to indicate that any specific position or region had a larger graft step-off.
OCAs have a longstanding history in the treatment of cartilage injury and defects within the knee. 3,10,13 Studies evaluating outcomes in the patellofemoral joint have generally included other types of grafts, thus limiting the utility of these initial studies. The treatment of the patellofemoral joint presents a unique challenge due to its anatomy and inherent instability along with the high compressive and shear forces across the joint. Resurfacing of the trochlea has been very challenging due to its variable morphology and because only 1 graft can typically be harvested from a given cadaveric trochlea.
The results of OCAs isolated to the patellofemoral joint were reported by 2 groups in the early 2000s. 6,14 More recently, additional series of patients treated with OCAs of the patellofemoral joint have been reported. In a series of 28 patients with isolated trochlear lesions treated at one of the busiest centers in the United States, survivorship was 91.7% at 10 years with 89% of patients being satisfied. 1 In another series, Cotter et al 4 reported on 50 patients treated with patellofemoral OCAs, comparing a cylindrical plug graft to a shell graft. The patients in each group also underwent additional procedures including femoral condyle grafts. Within the plug group, only 3 underwent isolated trochlear grafting and 1 underwent isolated bipolar patellofemoral grafting. In the shell group, which consisted of 34 knees, 16 patients had isolated patellar grafts, 2 had isolated trochlear grafts, and 12 had bipolar grafting of both the patella and the trochlea. These authors reported survivorship of 66% at 9.8 years for the plug allografts and 37% at 10.6 years for the shell grafts. The inclusion of concomitant grafts and lack of detail regarding the graft sizes makes drawing conclusions from this series challenging. However, it is clear that shell grafts did not perform as well as plug grafts, presumably due to the larger surface area involved or possibly due to reduced stability of these grafts, requiring fixation rather than a press-fit technique utilized with the plugs.
The challenges in certain anatomical locations such as the trochlea led to the development of a contoured grafting system to allow for a best match fit between a given variable surface topography of the donor and recipient trochleae. These guides were developed to give surgeons more confidence in performing larger single trochlear graft plugs rather than multiple smaller grafts as some surgeons have preferred in the past. This study supports the use of contoured grafts for the performance of OCAs in the trochlea. In general, most surgeons agree that reducing and limiting step-off while optimizing surface matching to the surrounding cartilage is one of the most important predictors of success for an OCA procedure. 2,5,7,8 We used this as our technical objective and endpoint in a foam bone study. The strengths of this study include the use of identical guides with the exception of the undersurface contour, an identical surgical procedure on identical foam femora, and a robust and reliable measurement method using a digital caliper.
Limitations
There are a number of key limitations of the study. These include the use of sawbones foam models. Performing a procedure using a sawbones model is inherently different than doing so on a cadaveric specimen or on a patient. The feel of the instruments, the material properties of the foam, the lack of time constraints, and complete exposure in the lab setting differ from procedural factors typically encountered during surgery. Furthermore, the shape of the femora of the donor and the recipient are different in the clinical setting, a significant contrast from the technique in this study where all femora, both donor and recipient, were geometrically identical. Another limitation of the study is the emphasis on the graft step-off as the measured endpoint. Despite its importance, graft step-off is only 1 of several factors predicting the clinical success of a fresh OCA procedure in the trochlea. Other factors include the general health of the joint and absence of global arthritis, the mechanical environment of the patellofemoral joint and the absence of trochlear dysplasia, immunological factors that may affect graft survival, the force of impaction of the grafts, the chondrocyte viability of the grafts, and other factors such as patient age and absence of systemic disease. Some of these factors can be addressed by the combination of the trochlear graft procedure with additional procedures such as patellar osteochondral grafting, trochleoplasty, lateral retinacular release, or lateral retinacular lengthening. Nevertheless, addressing step-off and incongruity at the allograft donor-recipient surface is a necessary component to a successful outcome.
Conclusion
Contoured guides performed better than flat guides in this sawbones surgical model for OCA transfer of the trochlea regardless of surgeon experience. Future work in this area will focus on the optimization of the surgical technique using these contoured guides with the ultimate goal of correlating clinical outcomes to graft survivorship utilizing contoured guides. For example, shape templates may be helpful in the clinical setting to allow surgeons to pick the best fit guides that match both the donor and the recipient and address the specific area of damage. Clinical outcomes looking at survivorship, ability to perform larger grafts, numbers of wasted grafts, and surgical time will undoubtedly be needed to fully determine the advantages of contoured guides.
Footnotes
Final revision submitted July 31, 2022; accepted September 13, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH; grant UL1 TR001860). C.M.D. and M.H. have received education payments from Sequoia Surgical. Z.C.L. has received education payments from Sequoia Surgical and hospitality payments from Stryker. A.A.J. is the principal shareholder of Joint Preservation Solutions, which holds intellectual property rights related to the contoured guides used in this study; is a scientific advisor and has stock options in Roam Robotics; has received education payments from Evolution Surgical; and has received hospitality payments from Encore Medical, Linvatec, Stryker, and Zimmer Biomet. C.A.L. has received education payments from Sequoia Surgical; consulting fees from Hyalex, KCI, Ossur, Smith & Nephew, and Vericel; speaking fees from Smith & Nephew; honoraria from Fidia Pharma; and hospitality payments from Aesculap Biologics and RTI Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Cameron JI, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation of the femoral trochlea. Am J Sports Med. 2016;44(3):633–638. [DOI] [PubMed] [Google Scholar]
- 2. Chahla J, Hinckel BB, Yanke AB, et al. An expert consensus statement on the management of large chondral and osteochondral defects in the patellofemoral joint. Orthop J Sports Med. 2020;8(3):2325967120907343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chu CR, Convery FR, Akeson WH, Meyers M, Amiel D. Articular cartilage transplantation. Clinical results in the knee. Clin Orthop Relat Res. 1999;360:159–168. [PubMed] [Google Scholar]
- 4. Cotter EJ, Christian DR, Frank RM, et al. Survivorship of patellofemoral osteochondral allograft transplantation. Arthrosc Sports Med Rehabil. 2019;1(1):e25–e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Du PZ, Markolf KL, Boguszewski DV, et al. Effects of proud large osteochondral plugs on contact forces and knee kinematics: a robotic study. Am J Sports Med. 2018;46(9):2122–2127. [DOI] [PubMed] [Google Scholar]
- 6. Jamali AA, Emmerson BC, Chung C, Convery FR, Bugbee WD. Fresh osteochondral allografts: results in the patellofemoral joint. Clin Orthop Relat Res. 2005;437:176–185. [PubMed] [Google Scholar]
- 7. Koh JL, Kowalski A, Lautenschlager E. The effect of angled osteochondral grafting on contact pressure: a biomechanical study. Am J Sports Med. 2006;34(1):116–119. [DOI] [PubMed] [Google Scholar]
- 8. Koh JL, Wirsing K, Lautenschlager E, Zhang LO. The effect of graft height mismatch on contact pressure following osteochondral grafting: a biomechanical study. Am J Sports Med. 2004;32(2):317–320. [DOI] [PubMed] [Google Scholar]
- 9. Lattermann C, Kremser V, Altintas B. Use of fresh osteochondral allografts in the patellofemoral joint. J Knee Surg. 2018;31(3):227–230. [DOI] [PubMed] [Google Scholar]
- 10. McDermott AG, Langer F, Pritzker KP, Gross AE. Fresh small-fragment osteochondral allografts. Long-term follow-up study on first 100 cases. Clin Orthop Relat Res. 1985;197:96–102. [PubMed] [Google Scholar]
- 11. Meric G, Gracitelli GC, Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allograft transplantation for bipolar reciprocal osteochondral lesions of the knee. Am J Sports Med. 2015;43(3):709–714. [DOI] [PubMed] [Google Scholar]
- 12. Mestriner AB, Ackermann J, Gomoll AH. Patellofemoral cartilage repair. Curr Rev Musculoskelet Med. 2018;11(2):188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oakeshott RD, Farine I, Pritzker KP, Langer F, Gross AE. A clinical and histologic analysis of failed fresh osteochondral allografts. Clin Orthop Relat Res. 1988;233:283–294. [PubMed] [Google Scholar]
- 14. Torga Spak R, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: long-term followup. Clin Orthop Relat Res. 2006;444:193–200. [DOI] [PubMed] [Google Scholar]


