Abstract
A 32-year-old woman presented to the outpatient clinic with persistent fever, anterior neck pain, and palpitations over the past week which developed 2 days after she had received the first dose of the Pfizer/BioNTech SARS-CoV-2 mRNA vaccine. On examination, the patient’s heart rate was 140 beats per minute and the thyroid gland was tender on palpation. Laboratory studies showed a low serum TSH level with elevated free thyroxine. Thyroid ultrasound revealed low-echoic lesions compatible with the site of tenderness. The patient was diagnosed with subacute thyroiditis and treatment was initiated with acetaminophen and propranolol, which resulted in symptom resolution within 2 weeks. Clinicians should be aware that subacute thyroiditis may occur within a few days following COVID-19 vaccination, especially in patients with anterior cervical pain with no significant abnormal pharyngeal findings and/or severe palpitations, because differentiating them from early non-specific adverse reactions can be challenging.
LEARNING POINTS
Cases of subacute thyroiditis after vaccination, including against COVID-19, have been increasingly reported.
Subacute thyroiditis should be considered in patients with anterior cervical pain with no significant abnormal pharyngeal findings and/or severe palpitations after COVID-19 vaccination because these can be diagnostic clues.
It is important to note that this condition can occur as early as a few days after vaccination, in order to avoid diagnostic pitfalls.
Keywords: Subacute thyroiditis, COVID-19 vaccination, COVID-19, vaccination
INTRODUCTION
Subacute thyroiditis (SAT) is an inflammatory thyroid disease which is presumed to be an immune response of the thyroid gland, most commonly characterized by anterior neck pain, a tender diffuse goitre, and hyperthyroidism in the early phase [1, 2]. SAT most commonly occurs following viral infections. However, cases of SAT after vaccination, including against COVID-19, have been increasingly reported [1–4]. Early recognition of post-vaccination SAT is crucial but can be a diagnostic challenge due to its similarity with the systemic adverse events of vaccines. We report an instructive case that illustrates the importance of vital signs and physical examination in the early diagnosis of SAT.
CASE DESCRIPTION
A 32-year-old woman with a history of Hashimoto’s disease presented with a persistent fever, anterior neck pain, and palpitations. Ten days earlier, she had developed mild fever the day after her first dose of the Pfizer/BioNTech SARS-CoV-2 mRNA vaccine. Two days after vaccination, she developed a high fever accompanied by anterior neck pain and palpitations. The patient did not report any contact with sick individuals, including COVID-19 cases, or preceding symptoms suggestive of recent viral infection. On physical examination, the patient’s heart rate was 140 beats per minute and the thyroid gland was tender on palpation and slightly enlarged. No significant abnormal pharyngeal findings were noted.
Laboratory investigations revealed a low serum TSH level of <0.020 μIU/ml (reference range 0.541–4.261 μIU/ml), with elevated free thyroxine (FT4) of 3.63 ng/dl (reference range 0.76–1.65 ng/dl). The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were high. Antibodies to thyroglobulin (TgAb) were positive, and negative for thyroid peroxidase (TPOAb) and thyrotrophin receptor (TRAb). Thyroid ultrasound revealed a slightly enlarged thyroid gland with heterogeneous echogenicity and low-echoic lesions compatible with the site of tenderness (Fig. 1). The patient was diagnosed with SAT possibly related to COVID-19 vaccination. Treatment was initiated with acetaminophen and propranolol, which resulted in symptom resolution within 2 weeks. After 12 weeks, TSH and FT4 had declined to the normal range.
Figure 1.
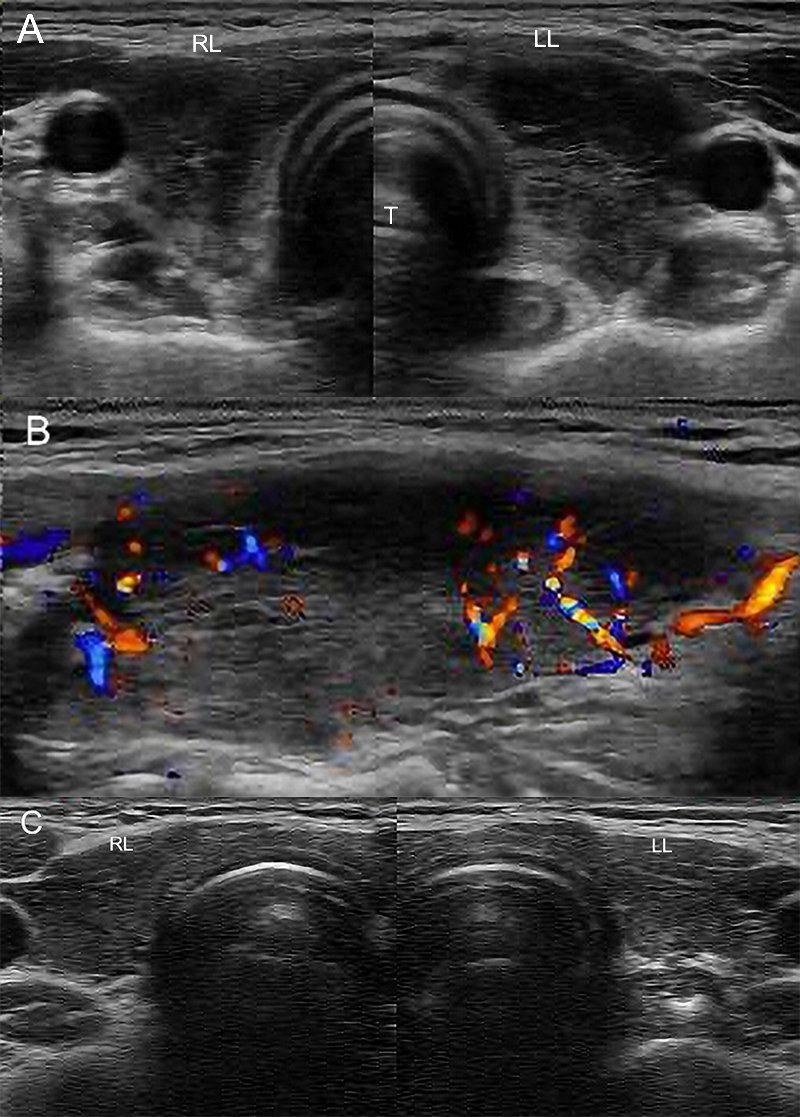
Axial view of the thyroid (A) and longitudinal view of the left thyroid lobe (B) taken at the initial visit (8 days after symptom onset) revealed low-echoic lesions compatible with the site of pain on palpation. (C) Image after 12 weeks of treatment showing normal gland size and internal texture. LL, left lobe of the thyroid; RL, right lobe of the thyroid; T, trachea
DISCUSSION
In previous reports, the time between vaccination against SARS-CoV-2 and SAT symptom onset varied depending on the type of vaccine. SAT usually occurs between 1 and 8 weeks after the initial dose of mRNA COVID-19 vaccine [1–3], while cases triggered by adjuvants have been reported to develop relatively earlier, within a few days after exposure [4]. To the best of our knowledge, however, there have been no cases of SAT developing as early as 2 days after the initial dose of mRNA vaccine, as in the present case. Although mRNA vaccines do not contain adjuvants, it has been suggested that the mRNA itself may act as an adjuvant [5]. Furthermore, SARS-CoV-2 spike protein production peaks 24–48 h after mRNA administration, which may trigger humoral T-cell-mediated cross-reactivity with thyroid cells owing to molecular mimicry [6].
Genetically predisposed patients may be at higher risk of developing SAT after immunization. Chatzi et al. reported the cases of two sisters who presented with SAT a few days after being administered a COVID-19 mRNA vaccine; their mother had a family history of Hashimoto’s thyroiditis, as in our case [7]. The roll of genetic predisposition for SAT development after the administration of mRNA vaccines needs to be clarified further.
SAT following COVID-19 vaccination is rare but probably under-reported due to difficulties in differentiating it from non-specific adverse effects such as fever, malaise and headache after vaccination. Given the widespread use of COVID-19 vaccination, physicians should be aware that immune responses, including SAT, may occur within a few days after immunization to avoid delays in diagnosis.
Footnotes
Conflicts of Interests: The authors declare there are no competing interests.
Patient Consent: Informed consent has been obtained from the patient.
REFERENCES
- 1.Siolos A, Gartzonika K, Tigas S. Thyroiditis following vaccination against COVID-19: report of two cases and review of the literature. Metabol Open. 2021;12:100136. doi: 10.1016/j.metop.2021.100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sözen M, Topaloğlu Ö, Çetinarslan B, Selek A, Cantürk Z, Gezer E, et al. COVID-19 mRNA vaccine may trigger subacute thyroiditis. Hum Vaccin Immunother. 2021;17(12):5120–5125. doi: 10.1080/21645515.2021.2013083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pla Peris B, Merchante Alfaro AÁ, Maravall Royo FJ, Abellán Galiana P, Pérez Naranjo S, González Boillos M. Thyrotoxicosis following SARS-COV-2 vaccination: a case series and discussion. J Endocrinol Invest. 2022;45(5):1071–1077. doi: 10.1007/s40618-022-01739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.İremli BG, Şendur SN, Ünlütürk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: postvaccination ASIA syndrome. J Clin Endocrinol Metab. 2021;106:2600–2605. doi: 10.1210/clinem/dgab373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung YH, Beiss V, Fiering SN, Steinmetz NF. COVID-19 vaccine frontrunners and their nanotechnology design. ACS Nano. 2020;14:12522–12537. doi: 10.1021/acsnano.0c07197. [DOI] [PubMed] [Google Scholar]
- 6.Verbeke R, Lentacker I, De Smedt SC, Dewitte H. Three decades of messenger RNA vaccine development. Nano Today. 2019;28:100766. [Google Scholar]
- 7.Chatzi S, Karampela A, Spiliopoulou C, Boutzios G. Subacute thyroiditis after SARS-CoV-2 vaccination: a report of two sisters and summary of the literature. Hormones (Athens) 2022;21:177–179. doi: 10.1007/s42000-021-00332-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


