Abstract
Objective:
This study aims to determine the relationship between BRAF V600E and Ki-67 expression with the recurrence of well-differentiated thyroid cancers.
Method:
The design of this study is a case-control and survival analysis. The data was taken from the thyroid cancer registry in Padang, Indonesia, where samples were taken from well-differentiated thyroid cancer patients who underwent therapy according to the protocol between 2015 and 2020. During this period, 396 well-differentiated thyroid cancer cases were obtained, of which 24 cases experienced recurrence. Of the cases that recurred, we found as many as 20 cases with complete tissue preservation documents later designated as cases. Calculating the expression of BRAF V600E and Ki-67 was performed semi-quantitatively per 100 tumor cells at random. For statistical tests, chi-square and survival analysis were performed using Kaplan-Meier and Cox regression analysis using a computer program with a determined significance level of p < 0.05.
Result:
BRAF V600E expression was found in all cases and controls in which 85% of cases had vigorous intensity and 15% had moderate intensity. Ki-67 expression was found positive in 35% of the recurrent cases, while in control, there was no expression of Ki-67. Patients with positive Ki-67 expression had shorter median survival than patients with negative Ki-67 expression of 40 months (95% CI 35-45 months) to 60 months (95% CI 53-67 months). An association was obtained between Ki-67 expression and thyroid cancer recurrence based on disease-free survival (p<0.05) with HR 1.34 (95% CI 1.13-1.92).
Conclusion:
This study confirms the association between Ki-67 expression and thyroid cancer recurrence based on disease-free survival and can be used as alternative to support the significance of Ki-67 as a predictor of thyroid cancer recurrence. In addition, Ki-67 can complement other molecular markers such as the BRAF V600E, to increase its prognostic strength.
Key Words: BRAF V600E, Ki-67, recurrence, thyroid cancer
Introduction
Thyroid cancer is the tenth most frequent cancer out of 567,000 cases of all cancers reported worldwide in 2020. Thyroid cancer most commonly occurs in women with three times higher frequency than in men (Sung et al., 2021). In Indonesia, thyroid cancer is the fifth most common cancer after breast, cervical, ovarian, and colorectal cancers out of 11,470 new cancer cases (Sung et al., 2021). Papillary and follicular thyroid cancer are well-differentiated thyroid cancers that comprise 90% of all thyroid malignancies. Thyroid cancer is a non-aggressive growth with a good prognosis and low morbidity and mortality, but more than 30% of thyroid cancer patients will experience recurrence, and approximately 5% of patients will die from this disease (Ferrari et al., 2018).
Clinicopathological data can classify patients with well-differentiated thyroid cancer into high risk and low risks in terms of recurrence. Several factors play a role in thyroid cancer recurrence: patient factors, tumor factors, and the treatment given. Patient factors also contribute to recurrences, such as age, gender, and family history, while the tumor factors that play a role are the type of histology, the size of the primary tumor, local invasion, distant metastases, and genetic changes. Treatment factors contributing to recurrence are the type of thyroidectomy performed, radioiodine ablation, and the thyroxine hormone administered (Zhao et al., 2012).
BRAF is a potent activator of the intracellular cascade RAS, RAF, MEK, ERK, and MAP plays a fundamental role in regulating cell proliferation. BRAF can be said to have an early role in developing well-differentiated thyroid cancer. In addition to the occurrence of BRAF (B-type Rapidly Accelerated Fibrosarcoma kinase) oncogene mutations, there are also reports of other oncogene mutations such as RAS (Rat Sarcoma) and RET / PTC (Rearranged during Transfection / Papillary Thyroid Carcinoma) (Fernandez et al., 2013). However, BRAF mutations are the most common genetic alteration in well-differentiated thyroid cancers. BRAF mutations are the most common activators on the MAPK signaling pathway and have significant implications for thyroid tumorigenesis. BRAF is a member of the RAF protein group that regulates signal transduction (Kim et al., 2006; Omur and Baran, 2014; Ritterhouse and Barletta, 2015). Most (about 90%) of BRAF mutations are transversions of thymine to adenine in exon 15 at nucleotide 1799 (T1799A), resulting in the replacement of valine to glutamic acid at position 600 (BRAF V600E). This BRAF V600E mutation results in the activation of BRAF kinase, subsequently leading to phosphorylation in the mitogen-activated protein kinase/ERK kinase (MEK), which will activate extracellular-signal-regulated kinase (ERK). Once ERK is activated, ERK will regulate gene transcription, which includes differentiation, proliferation, and apoptosis (Nikiforov, 2010). A recent study by Kim and colleagues reported that out of 203 individuals with papillary thyroid carcinoma, there was a positive association between BRAF mutations and tumor recurrence (Kim et al., 2006). Another study has also reported a significant correlation between BRAF mutations and recurrences of papillary thyroid cancer (Riesco-Eizaguirre et al., 2006). However, in another study, it was reported that the presence of BRAF mutation does not occur consistently with the recurrence of well-differentiated cancers (Cañadas Garre et al., 2011).
Uncontrolled cell proliferation is one of the hallmarks of cancer. Ki-67 is the marker most commonly used to measure current proliferative activity. Immunohistochemistry examination of Ki-67 expression is the most widely used, widely available, and informative technique for determining cell proliferation (Dzulkifli et al., 2019). The expression of Ki-67 is a significant marker of proliferation in various human malignancies such as prostate cancer and breast cancer, which has been published in various studies (Arshad et al., 2010; Choudhury et al., 2011). The expression of Ki-67 has long been associated with a poor prognosis, although research on thyroid disorders and cancer is still limited. There is no agreement on the value of the expression Ki-67, considered an overexpression, but some consensus determined that expressions of more than 20% are considered high or positive. High Ki-67 expression was much higher in the papillary thyroid cancer group than in the benign thyroid disease group, and Ki-67 expression was higher in the thyroid adenoma subgroup than in the nodular goiter subgroup (Mehrotra et al., 2006; Sofiadis et al., 2009).
Currently, immunohistochemistry examination is a standard procedure for determining the expression of specific proteins in a histopathological laboratory. The immunohistochemistry examination is an examination that has been proven to be sensitive and specific for detecting BRAF V600E and Ki-67 mutations in well-differentiated thyroid carcinoma (Sun et al., 2015; Urruticoechea et al., 2005). Although calculated semi-quantitatively, immunohistochemistry staining is a more accessible, cheaper, and more consistent examination to date than other markers (Urruticoechea et al., 2005). This study aimed to determine the relationship between BRAF V600E expression and Ki-67 expression as a prognosis factor for recurrence in well-differentiated thyroid cancer.
Materials and Methods
Study design and research samples
The design of this study is a case-control and survival analysis study using Kaplan-Meier and cox regression tests. The data was taken from thyroid cancer data from Padang city, Indonesia, recorded in the Cancer Registry of the Padang Branch of the Association of Oncology Surgeons from 2015-2020. The designated case group was recurrent well-differentiated thyroid cancers after complete resection, and the designated control group was non-residual well-differentiated thyroid cancers. The number of samples is determined based on the sample size formula needed was 18 cases. For this study, 20 samples were assigned for cases (patients with recurrence) and 20 for control (patients without recurrence). All cases and controls had complete clinical data and well-archived paraffin blocks that can carry out immunohistochemistry examinations of BRAF and Ki-67. The data available from the registration must be displayed in a computerized database (Excel; Microsoft Corp, Redmond, Washington). The data consists of patient features (age, gender), preoperative clinical features (sonography characteristics, fine needle aspiration biopsy results, computed tomography [CT] scan), performed surgery, postoperative radioiodine therapy, follow-up data (postoperative scintigraphy, ultrasound, or CT scan), pathological features (PTC histological variants, vascular invasion, multifocality, dimensions, node metastases), and cancer TNM (AJCC). The nodal status was assessed preoperatively through clinical examination and ultrasound of the neck for all patients.
To examine the expression of BRAF V600E and Ki-67, a 3.5-4 μm thick cutting of thyroid cancer tissue from a representative paraffin block was performed. The paraffin blocks were collected and labeled according to the corresponding PA number and medical records and were divided into recurrent and non-recurrent well-differentiated thyroid cancer cases. Deparaffinization was then carried out with xylene and stratified rehydration with ethanol 100%, 95%, 80%, and 70%, then rinsed with water. Sections were then blocked with 10% normal serum for 15 minutes at 37°C, followed by incubation with mouse anti-Ki-67 antibody at a dilution of 1:1,000 for 1 hour at room temperature. After washing three times in PBS, sections were incubated for 30 minutes at room temperature. For BRAF examination, staining with rabbit monoclonal antibody, a product of GeneTex, was performed and then rinsed and stained with secondary antibodies. For Ki-67 examination, staining with rabbit monoclonal antibody, a product of Biocare Medical, was carried out and then rinsed and stained with secondary antibodies. Counterstaining was performed to increase the contrast level if necessary and followed by drying and stabilizing the preparations and readings of the results. The Ethical Committee of Medical School of Universitas Andalas Padang, Indonesia, approved this research.
Operational definition
The dependent variable is the recurrence of thyroid cancer in well-differentiated thyroid cancer patients who had histopathological examination results and had received treatment according to protocol. The patient also has data on physical examination/ultrasound of the neck/thyroid scan in the thyroid bed/neck lymph nodes. The independent variables of this study include a) Expression of BRAF V600E, which is an expression caused by the BRAF V600E antigen reaction present in thyroid cancer cells, as determined by immunohistochemistry examination. If the examination findings show 2 (++) and 3 (+++), the test is positive; if the test results show 0 and 1 (+), the test is negative; and b) Expression of Ki67, an image of tumor cell growth as determined by immunohistochemistry. If the test results obtained at least or equal to 15 stained tumor cells, the measurement results are considered positive, while a result of fewer than 15 cells is considered negative.
Statistical analysis
Immunohistochemistry analysis used to assess the expression of BRAF V600E and KI-67 is semiquantitative data because it combines the quality test results of the staining and the number of stained cells. In this study, we determined that only the number of stained cells by the antibody was calculated as the positive level of the test result. Statistical analysis was performed with SPSS 13.0 program for Windows (SPSS, Inc, IBM, Chicago, Illinois). The relationship between BRAF mutation and the categorical variable was tested using the x² test or fisher test. Disease-free survival curves were analyzed using the Kaplan-Meier and log-rank test to assess the statistical significance of survival differences. Statistical significance was established for P< 0.05 with a confidence interval of 95%.
Results
From the total number of patients during the observation period, 273 patients were obtained, with 24 patients experiencing recurrence. Of the recurrent cases, 20 patients were included in the research criteria, and control patients without recurrence as many as 20 patients were assigned with similar characteristics. From the characteristics of patients, the average age was 43.6 years (range 16-79 years). The histopathology results identified that most of them were papillary carcinoma in 90 % of the cases. From the characteristics shown in Table 1, there is no significant difference between the case and control groups in age, sex, tumor size, histopathological type, lymph nodes, or the type of surgery performed (p> 0.05). This finding shows that the case and control have been well matched.
Table 1.
Subject Characteristics
| Characteristics | Case | Control | p-value |
|---|---|---|---|
| (n=20) | (n=20) | ||
| Age (year), mean±SD | 42.95±14.79 | 44.30±13.44 | 0.764 |
| Sex, f (%) | 0.182b | ||
| Male | 5 (25.0) | 1 (5.0) | |
| Female | 15 (75.0) | 19 (95.0) | |
| Tumor size, f (%) | 0.514b | ||
| < 5 cm | 9 (45.0) | 6 (30.0) | |
| ≥ 5 cm | 11 (55.0) | 14 (70.0) | |
| Histopathology type | 1.000b | ||
| Papillary | 18 (90.0) | 18 (90.0) | |
| Folicular | 2 (10.0) | 2 (10.0) | |
| Lymph nodes | 0.231b | ||
| Positive | 3 (15.0) | 0 | |
| Negative | 17 (85.0) | 20 (100.0) | |
| Surgery | 0.480b | ||
| Total thyroidectomy | 16 (80.0) | 13 (65.0) | |
| Hemithyroidectomy | 4 (20.0) | 7 (35.0) |
* *p < 0.05 significant ; n/a, not available; T-test independent sample; bChi-square test
BRAF Mutation and Ki-67 expression in recurrence of thyroid cancer
This study found that the expression of BRAF V600E in the case and control groups was 100 percent, varying from moderate to high intensity, as shown in Table 2. From the analysis of cases and controls on the recurrence of well-differentiated thyroid cancer, insignificant results were obtained with OR 0.44 (CI 0.72-2.76) with p 0.661. The intensity of BRAF V600E staining found that the recurrent group averaged 80%, which was lower than the control group, which had an average intensity of 90%. However, there was no significant difference between the intensity of BRAF V600E expression and thyroid cancer recurrence (p>0.05). In the case group, positive Ki-67 expression was identified 35% of the time. It is known that there is an association between the expression of Ki-67 and the recurrence of thyroid cancer (p<0.05).
Table 2.
Relationship of BRAF V600E and Ki-67 Expression with Recurrence of Thyroid Cancer
| Variable | Case (f/%) (n=20) |
control (f/%) (n=20) |
Total (f/%) | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| BRAF V600E intensity | ||||||
| High | 16 (80.0) | 18 (90.0) | 34 (85.0) | 0.661 | 0.44 | 0.72-2.76 |
| Moderate | 4 (20.0) | 2 (10.0) | 6 (15.0) | |||
| Ki-67 | ||||||
| Positive | 7 (35.0) | 0 | 7 (17.5) | 0.008* | 2.54 | 1.663-3.88 |
| Negative | 13 (65.0) | 20 (100.0) | 33 (82.5) |
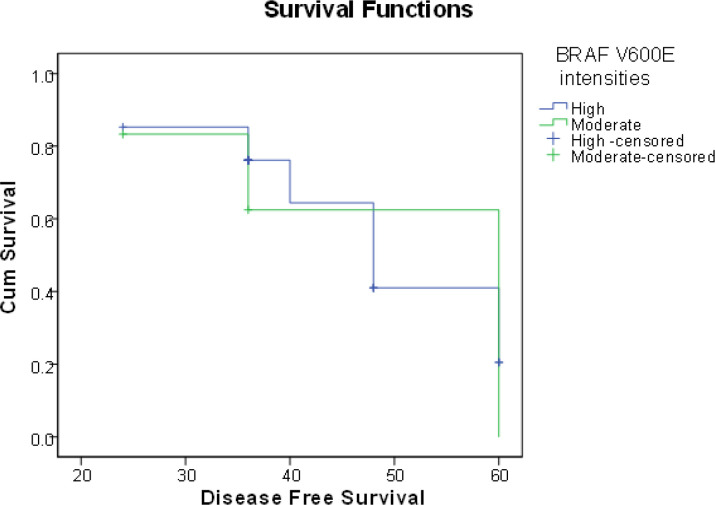
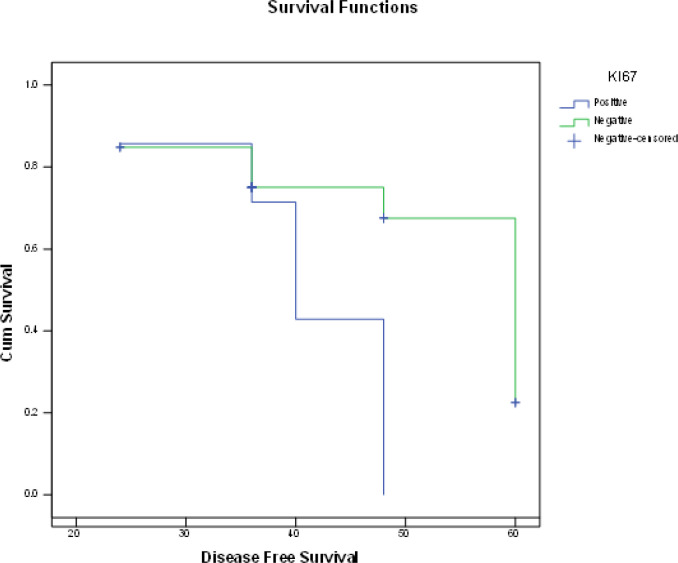
The relationship between BRAF V600E intensity and thyroid cancer recurrence based on disease-free survival (Figure 1) shows that patients with strong BRAF V600E intensity had an average survival of 48 months (95% CI 40-56 months) compared to those with moderate BRAF V600E intensity, who had an average survival of 60 months (95% CI 35-63 months). Based on statistical analysis, it is known that there is no relationship between BRAF V600E intensity and thyroid cancer recurrence based on disease-free survival (p>0.05) with a hazard ratio (HR) of 1.14. (0.37-3.49). The relationship between Ki-67 expression and recurrence of thyroid cancer based on disease-free survival (Figure 2) shows that individuals with positive Ki-67 expression had 40 months (95% CI 35-45 months) shorter average survival of thyroid cancer recurrence than those with negative Ki-67 expression, who had 60 months (95% CI 53-67 months). It is known that there is an association between Ki-67 expression and recurrence of thyroid cancer based on disease-free survival (p<0.05) with HR 1.34 (1.13-1.92).
Figure 1.
Relationship between BRAF V600E Intensity and Thyroid Cancer Recurrence based on Disease-Free Survival
Figure 2.
Association between Ki-67 Expression and Recurrence of Thyroid Cancer based on Disease-Free Survival
Discussion
According to this study, there was no relationship between BRAF V600E expression and recurrence of thyroid cancer. The findings of this study contrast with previous studies that have found a link between BRAF mutations and recurrences in papillary thyroid carcinoma, a relationship that has been investigated in several studies (Kim et al., 2006; Riesco-Eizaguirre et al., 2006). Other studies, on the other hand, support the findings of this research which claim that BRAF mutations in papillary thyroid carcinomas are not associated with recurrence (Garre et al., 2011; Yan et al., 2019).
The effects of geographical area and ethnicity should be considered when assessing the relationship between the BRAF V600E mutation and the recurrence of well-differentiated thyroid cancer, which is one of the reasons for the difference in the results of this study with studies that found the role of BRAF on the recurrence of papillary thyroid cancer. Thyroid cancer patients with BRAF mutations in America have a higher risk of recurrence, while thyroid cancer patients with BRAF mutations in Europe have a lower risk of recurrence, according to a meta-analysis (Li and Kwon, 2020).
Secondly, some studies found the mutation rate of BRAF V600E to be very low in papillary thyroid carcinoma with lymphocytic infiltrates. These findings suggest that papillary thyroid cancer in the absence of lymphocytic infiltration has a different developmental mechanism than papillary thyroid cancer without lymphocytic infiltration in the absence of a BRAF V600E mutation. However, some studies have found that the BRAF V600E mutation is more common in papillary thyroid carcinoma with lymphocytic infiltrates (Tufano et al., 2012). The increased inflammatory response in papillary thyroid cancer can cause DNA damage by producing reactive oxygen species, which promotes the development of papillary thyroid cancer (Chen et al., 2016).
This study found that patients with strong BRAF V600E intensity had an average survival of 48 months (95% CI 40-56 months) compared to those with moderate BRAF V600E intensity, with an average survival of 60 months (95% CI 35-63 months). Based on statistical testing, it is known that there is no relationship between BRAF V600E intensity and thyroid cancer recurrence based on disease-free survival (p>0.05) with a hazard ratio (HR) of 1.14. (0.37-3.49). Although this study found no association between BRAF V600E intensity and thyroid cancer recurrence based on disease-free survival, however, the findings of this study were consistent with previous studies that found that patients with a positive BRAF V600E test had lower average survival than those who had a negative BRAF V600E test (Tufano et al., 2012). Patients with papillary thyroid cancer with BRAF V600E mutation had a 3.34-fold greater risk of recurrence, according to a review study (95% CI 2.36-4.73) (Chen et al., 2016).
Positive Ki-67 expression was found in 35% of the case group, and there was a relationship between Ki-67 expression and recurrence of thyroid cancer. Patients with ki-67 positive expression had 40 months (95% CI 35-45 months) shorter average survival of thyroid cancer recurrence than those with negative Ki-67 expression, who had 60 months (95% CI 53-67 months). It is known that there is an association between Ki-67 expression and recurrence of thyroid cancer based on disease-free survival (p<0.05) with HR 1.34 (1.13-1.92).
The expression of Ki-67 is associated with the proliferation and growth of tumor cells. It was commonly used as a marker of proliferation in pathological research. Previous studies have revealed that increased expression of Ki-67 is associated with a poor prognosis in breast and prostate cancer. Previous studies looked into the predictive importance of Ki-67 expression in papillary thyroid cancer and found that it is an independent prognostic factor for disease-free survival in individuals with papillary thyroid cancer. In the current study, there is a significant relationship between the presence of Ki-67 expressions in the recurrent and the control group, in which the majority of people do not have this marker expressed or have a weak immunoexpression if they do so (Berney et al., 2009; Luporsi et al., 2012).
Several previous studies have shown a substantial association between Ki-67 expression and recurrence. Ki-67 immunoexpression is higher in papillary thyroid carcinomas greater than 1.0 cm in size and those suffering from thyroiditis, but not in those with multifocal, extra thyroid extension, or lymph node metastases (Tang et al., 2018). Another study found an association between high Ki-67 expression and extra thyroid extension and lymph node metastases (Zhao et al., 2012). Patients with increased Ki-67 immunoexpression had lower survival in terms of tumor size, lymph node metastases, and extra thyroid extension, according to a meta-analysis of 51 studies on thyroid cancer (Pan et al., 2017).
The limitation of this study is that it did not stratify the expression of BRAF V600E based on patient characteristics, such as the effects of age, sex, tumor size, histopathological type, lymph nodes, and surgery on recurrence of well-differentiated thyroid cancer since all the results of BRAF V600E expression were well distinguished. Researchers have concluded that this is a good thing. Since there is not enough heterogeneity in the BRAF V600E fraction, additional analysis based on stratification is not possible.
The findings of this study can be used as alternative to support the significance of Ki-67 as a predictor of thyroid cancer recurrence. In addition, Ki-67 must be paired with other molecular markers, such as the BRAF V600E, to increase its prognostic strength. Researchers, on the other hand, acknowledge the limitations of this research. This study is retrospective research and takes a short follow-up time. Long-term follow-up studies using a prospective method are required in the future to confirm these conclusions.
Author Contribution Statement
All authors contributed equally in this study.
Acknowledgements
Conflict of interest
The authors declare no conflict of interest.
References
- Arshad H, Ahmad Z, Hasan SH. Gliomas: correlation of histologic grade, Ki67 and p53 expression with patient survival. Asian Pac J Cancer Prev. 2010;11:1637–40. [PubMed] [Google Scholar]
- Berney DM, Gopalan A, Kudahetti S, et al. Ki-67 and outcome in clinically localised prostate cancer: Analysis of conservatively treated prostate cancer patients from the trans-atlantic prostate group study. Br J Cancer. 2009;100:888–93. doi: 10.1038/sj.bjc.6604951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- Cañadas Garre M, López de la Torre Casares M, Becerra Massare P, et al. BRAF(T1799A) mutation in the primary tumor as a marker of risk, recurrence, or persistence of papillary thyroid carcinoma. Endocrinol Nutr. 2011;58:175–84. doi: 10.1016/j.endonu.2011.02.006. [DOI] [PubMed] [Google Scholar]
- Choudhury M, Singh S, Agarwal S. Diagnostic utility of Ki67 and p53 immunostaining on solitary thyroid nodule--a cytohistological and radionuclide scintigraphic study. Indian J Pathol Microbiol. 2011;54:472–5. doi: 10.4103/0377-4929.85077. [DOI] [PubMed] [Google Scholar]
- Dzulkifli FA, Mashor MY, Jaafar H. An overview of recent counting methods for Ki67 IHC staining. J Biomed Clin Sci. 2019;3:10–7. [Google Scholar]
- Fernandez IJ, Piccin O, Sciascia S. Clinical significance of BRAF mutation in thyroid papillary cancer. Otolaryngol Head Neck Surg. 2013;148:919–25. doi: 10.1177/0194599813481942. [DOI] [PubMed] [Google Scholar]
- Ferrari SM, Fallahi P, Ruffilli I. Molecular testing in the diagnosis of differentiated thyroid carcinomas. Gland Surg. 2018;7:19–29. doi: 10.21037/gs.2017.11.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TY, Kim WB, Rhee YS. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol. 2006;65:364–8. doi: 10.1111/j.1365-2265.2006.02605.x. [DOI] [PubMed] [Google Scholar]
- Li X, Kwon H. The impact of BRAF mutation on the recurrence of papillary thyroid carcinoma: A Meta-Analysis. Cancers. 2020;12:2056. doi: 10.3390/cancers12082056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luporsi E, André F, Spyratos F. Ki-67: level of evidence and methodological considerations for its role in the clinical management of breast cancer: analytical and critical review. Breast Cancer Res Tr. 2012;132:895–915. doi: 10.1007/s10549-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra P, Gonzalez MA, Johnson SJ. Mcm-2 and Ki-67 have limited potential in preoperative diagnosis of thyroid malignancy. Laryngoscope. 2006;116:1434–8. doi: 10.1097/01.mlg.0000225931.59644.93. [DOI] [PubMed] [Google Scholar]
- Nikiforov YE. Endocrine Pathology: Differential Diagnosis and Molecular Advances. New York, NY: Springer; 2010. Recent Developments in the Molecular Biology of the Thyroid ; pp. 237–60. [Google Scholar]
- Omur O, Baran Y. An update on molecular biology of thyroid cancers. Crit Rev Oncol Hematol. 2014;90:233–52. doi: 10.1016/j.critrevonc.2013.12.007. [DOI] [PubMed] [Google Scholar]
- Pan D, Wen D, Luo Y. The diagnostic and prognostic values of Ki-67/MIB-1 expression in thyroid cancer: a meta-analysis with 6,051 cases. Oncotargets Ther. 2017;10:3261–76. doi: 10.2147/OTT.S135593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riesco-Eizaguirre G, Gutiérrez-Martínez P, García-Cabezas MA, Nistal M, Santisteban P. The oncogene BRAF V600E is associated with a high risk of recurrence and less differentiated papillary thyroid carcinoma due to the impairment of Na+/I- targeting to the membrane. Endocr Relat Cancer. 2006;13:257–69. doi: 10.1677/erc.1.01119. [DOI] [PubMed] [Google Scholar]
- Ritterhouse LL, Barletta JA. BRAF V600E mutation-specific antibody: A review. Semin Diagn Pathol. 2015;32:400–8. doi: 10.1053/j.semdp.2015.02.010. [DOI] [PubMed] [Google Scholar]
- Sofiadis A, Tani E, Foukakis T. Diagnostic and prognostic potential of MIB-1 proliferation index in thyroid fine needle aspiration biopsy. Int J Oncol. 2009;35:369–74. [PubMed] [Google Scholar]
- Sun J, Zhang J, Lu J. Immunohistochemistry is highly sensitive and specific for detecting the BRAF V600E mutation in papillary thyroid carcinoma. Int J Clin Exp Pathol. 2015;8:15072–8. [PMC free article] [PubMed] [Google Scholar]
- Sung H, Ferlay J, Siegel RL. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- Tang J, Gui C, Qiu S, Wang M. The clinicopathological significance of Ki67 in papillary thyroid carcinoma: a suitable indicator? World J Surg Oncol. 2018;16:100. doi: 10.1186/s12957-018-1384-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tufano RP, Teixeira GV, Bishop J, Carson KA, Xing M. BRAF mutation in papillary thyroid cancer and its value in tailoring initial treatment: a systematic review and meta-analysis. Medicine (Baltimore) 2012;91:274–86. doi: 10.1097/MD.0b013e31826a9c71. [DOI] [PubMed] [Google Scholar]
- Urruticoechea A, Smith IE, Dowsett M. Proliferation marker Ki-67 in early breast cancer. J Clin Oncol. 2005;23:7212–20. doi: 10.1200/JCO.2005.07.501. [DOI] [PubMed] [Google Scholar]
- Yan C, Huang M, Li X, Wang T, Ling R. Relationship between BRAF V600E and clinical features in papillary thyroid carcinoma. Endocr Connect. 2019;8:988–96. doi: 10.1530/EC-19-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Zhang Y, Liu X, Shi B. Prognostic factors for differentiated thyroid carcinoma and review of the literature. Tumori. 2012;98:233–7. doi: 10.1177/030089161209800209. [DOI] [PubMed] [Google Scholar]