Abstract
Background
The choice to give birth at home with a regulated midwife in attendance became available to expectant women in British Columbia in 1998. The purpose of this study was to evaluate the safety of home birth by comparing perinatal outcomes for planned home births attended by regulated midwives with those for planned hospital births.
Methods
We compared the outcomes of 862 planned home births attended by midwives with those of planned hospital births attended by either midwives (n = 571) or physicians (n = 743). Comparison subjects who were similar in their obstetric risk status were selected from hospitals in which the midwives who were conducting the home births had hospital privileges. Our study population included all home births that occurred between Jan. 1, 1998, and Dec. 31, 1999.
Results
Women who gave birth at home attended by a midwife had fewer procedures during labour compared with women who gave birth in hospital attended by a physician. After adjustment for maternal age, lone parent status, income quintile, use of any versus no substances and parity, women in the home birth group were less likely to have epidural analgesia (odds ratio 0.20, 95% confidence interval [CI] 0.14–0.27), be induced, have their labours augmented with oxytocin or prostaglandins, or have an episiotomy. Comparison of home births with hospital births attended by a midwife showed very similar and equally significant differences. The adjusted odds ratio for cesarean section in the home birth group compared with physician-attended hospital births was 0.3 (95% CI 0.22–0.43). Rates of perinatal mortality, 5-minute Apgar scores, meconium aspiration syndrome or need for transfer to a different hospital for specialized newborn care were very similar for the home birth group and for births in hospital attended by a physician. The adjusted odds ratio for Apgar scores lower than 7 at 5 minutes in the home birth group compared with physician-attended hospital births was 0.84 (95% CI 0.32–2.19).
Interpretation
There was no increased maternal or neonatal risk associated with planned home birth under the care of a regulated midwife. The rates of some adverse outcomes were too low for us to draw statistical comparisons, and ongoing evaluation of home birth is warranted.
Studies in the United Kingdom,1 the United States,2 the Netherlands,3 Switzerland4 and New Zealand5 have reported that planned home birth attended by appropriately qualified caregivers appears to be as safe as hospital birth. In Canada, home birth wit h regulated midwifery was introduced in Ontario in 1994. Quebec also sanctioned midwifery in 1994, with the constraint that midwives should practise in birthing centres in the context of a pilot project. In 1998, the option to choose birth at home attended by a regulated midwife became available for residents of British Columbia. The rugged geography and mixed weather conditions in Canada potentially present unique challenges for home birth. In order to address the issue of safety of home birth in BC, we compared selected outcomes for planned home births attended by regulated midwives with those for planned hospital births attended by midwives and by physicians.
Since 1998, midwives have provided a full range of antepartum, intrapartum, postpartum and newborn care for women whose pregnancies are considered to be at sufficiently low risk to fall within the scope of midwifery practice. The choice to deliver at home or in hospital is made by the client and her midwife, based on a policy established by the College of Midwives of British Columbia (CMBC). At the conclusion of our evaluation period in December 1999, there were 58 practising registered midwives in BC. These midwives, who have passed written, oral and practice examinations set by the CMBC, work in individual or group practices and have hospital admitting privileges. Their services are covered through a midwifery plan funded by the Ministry of Health Services.
Methods
We conducted a prospective cohort study in which maternal, fetal and newborn outcomes for women intending to deliver at home with a midwife between Jan. 1, 1998, and Dec. 31, 1999, were compared with those for women of similar obstetric risk status intending to deliver in hospital with a physician or midwife. Approval for the study was obtained from the University of British Columbia Clinical Research Ethics Board.
Home births (study group)
The home birth group consisted of all women enrolled in the Home Birth Demonstration Project (HBDP). Women were registered in the HBDP by their midwife if at 36 weeks' gestation they intended to give birth at home and met eligibility requirements for home birth. Birth at home with a regulated midwife in BC was available only to women who enrolled in the HBDP. Informed written consent to participate in the HBDP was obtained from all participants. Subjects in the HBDP group were included in our study if they still intended to deliver at home and met eligibility requirements for home birth at the onset of labour.
Data for HBDP clients were obtained from the British Columbia Reproductive Care Program (BCRCP). Midwives complete standard BCRCP forms that are the same forms as those used by hospitals throughout the province. They include an antenatal record, a birth summary record and a newborn record. Data from BCRCP forms submitted by midwives were abstracted by BCRCP staff into a relational database. In hospital settings, health records staff abstract data from the BCRCP forms in the same manner and submit their databases to the BCRCP. These individual databases are combined to form the British Columbia Perinatal Database Registry. In the event that an HBDP client gave birth in hospital or an HBDP mother or baby was transferred to hospital, the HBDP client was matched to the hospital chart using her Personal Health Number. Data were then extracted from the hospital chart.
In 1998 at the inception of the HBDP, only 65% of hospitals in BC in which births took place were submitting data to the BCRCP. If the hospital in which the HBDP client had delivered was not yet enrolled in the British Columbia Perinatal Data Registry, HBDP forms were reviewed. HBDP forms were designed specifically for the project and were submitted to the HBDP coordinator for every client in addition to the standard BCRCP forms. They contained information about the process of midwifery care, including rates and indications for consultation, referral and transport to hospital.
Household income data in our study were obtained from Statistics Canada. Based on the 1996 census, average household incomes adjusted for household size within a given enumeration area were compared among groups. Enumeration areas for each subject were assigned on the basis of postal codes.
Hospital births with attending physician (physician comparison group)
Subjects in this comparison group had their babies delivered by a physician (family practice, obstetrician, medical resident or medical student) in hospital during the study period. Exclusion criteria were applied to eliminate subjects with any conditions that would render them ineligible for a home birth according to policy set by the HBDP and the CMBC. These conditions included the following:
· Multiple birth
· Heart disease (class I–IV or class unknown)
· Hypertensive chronic renal disease
· Pregnancy-induced hypertension with proteinuria (> 30 mg /dL) diagnosed in the antepartum period
· Insulin-dependent diabetes, either pre-existing or gestational
· Antepartum hemorrhage after 20 weeks' gestation
· Active genital herpes
· Breech or other abnormal presentation
· Gestational age less than 37 weeks or greater than 41 weeks at the onset of labour
· More than one previous cesarean section
· Mother transferred to hospital from another facility
In addition, records were checked to ensure that a midwife was not listed as a caregiver anywhere in the hospital record.
For each study (home birth) subject, a comparison subject was chosen on the basis of matching according to the following criteria:
· Age (< 15 years, 15–19 years, 20–24 years, 25–29 years, 30–34 years, ≥35 years)
· Lone parent status (yes, no)
· Parity (nulliparous v. multiparous)
· Hospital in which the midwife who was caring for study subject had admitting privileges
Subjects were matched according to their sociodemographic and pregnancy characteristics (age, parity and lone parent status), which are known to be associated with particular obstetric outcomes. Matching of hospitals allowed for the selection of comparison groups who came from the same geographic area, with corresponding similarity of climate, transportation, urban versus rural setting, and hospital resources.
Hospital births with attending midwife (midwife comparison group)
Subjects were selected for this comparison group if the baby was delivered in hospital and “midwife” was indicated on the hospital record as any type of caregiver. Intention to deliver at home or hospital was identified through documentation supplied by midwives to the HBDP. The same exclusion criteria were applied to this group as to the physician group. All eligible planned hospital births of midwives' clients in 1998 and 1999 were included.
This comparison group was not matched with the study cohort, because there were insufficient numbers of subjects to accomplish the matching. However, because midwives offer eligible clients the choice of home or hospital births, subjects in this comparison group lived in the same hospital catchment areas as those in the home birth group because the same midwives attended both groups.
Outcomes
Outcomes selected for review included perinatal death and indicators of fetal or newborn and maternal morbidity. These outcomes are included in either the BCRCP database or the Canadian Institute of Health Information (CIHI) database. All hospitals submit abstracted information to the CIHI, and we accessed variables from this database through the BCRCP.
Data analysis
Subjects' data were analyzed according to intended place of birth at the onset of labour. Categorical variables were compared using the χ2 statistic and Fisher's exact test. Continuous variables were analyzed using Student's t-test.
A Bonferroni correction was applied to each table presented, in order to account for multiple comparisons. Multiple comparisons increase the probability of having a statistically significant finding through chance alone. The Bonferroni correction divides the type I (α) error (0.05) by the number of comparisons in the analysis to yield a more conservative p value that is denoted to be statistically significant. For example, in Table 1, a p value that is less than 0.05 divided by 12 (12 comparisons) or 0.004 is considered statistically significant. In Table 2, p values that are less than 0.05 divided by 25 or 0.002 are considered statistically significant. In Tables 3 and 4 this value is 0.05 divided by 15 or 0.003.
Table 1
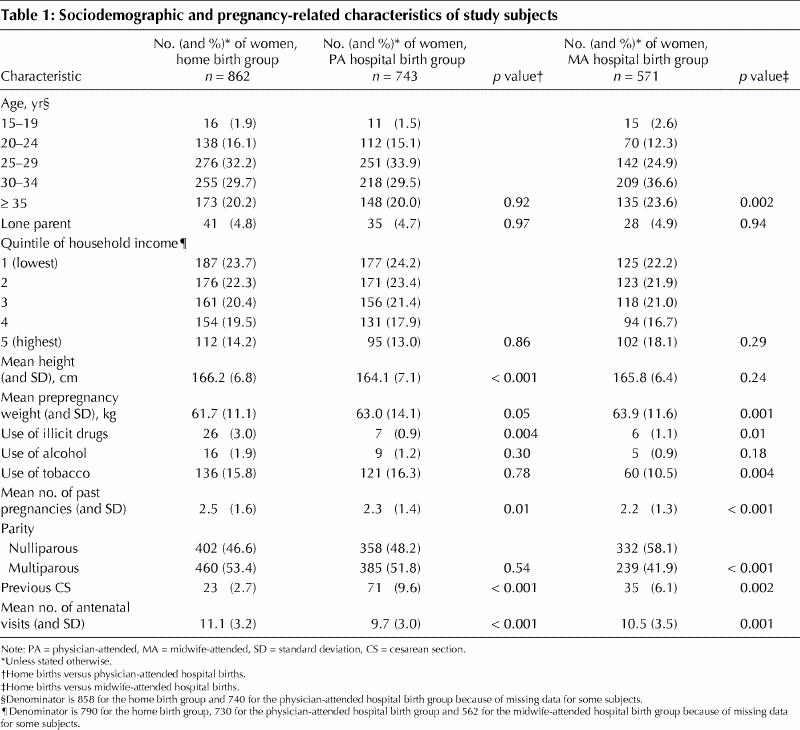
Table 2

Table 3
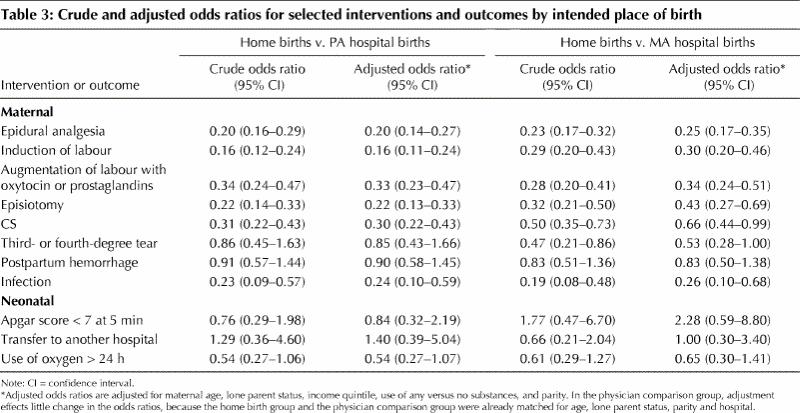
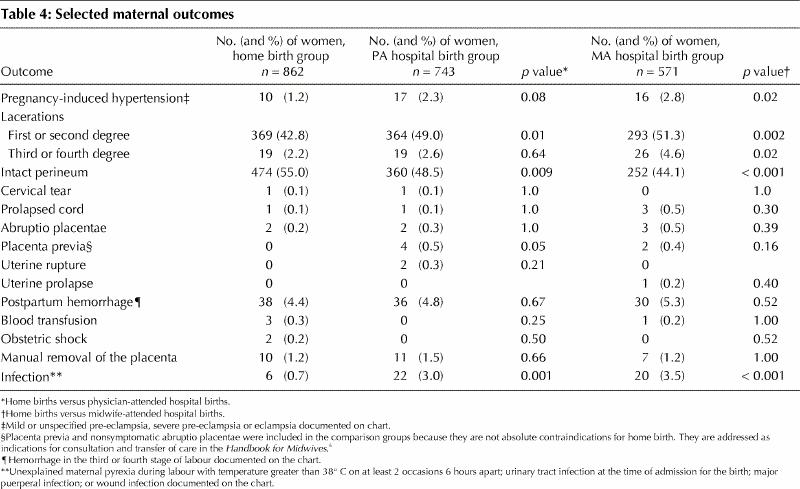
Table 4
Maternal demographic and obstetric variables listed in Table 1 were examined for their role as confounders of associations with the prevalence of selected adverse outcomes using unconditional logistic regression. Adverse outcomes were selected for multivariate analysis on the basis of clinical importance and sufficient numbers of outcomes with which to undertake a multivariate analysis. An estimated odds ratio and 95% confidence intervals were computed for each multivariate analysis.
Results
There were 862 subjects in the home birth cohort. Only 743 physician-attended, in-hospital births could be matched with the home births for age, lone parent status, parity and hospital. There were 571 subjects in the midwife-attended, planned hospital birth cohort in total. Sixty-seven of the home births occurred in areas where the hospital at which the midwife had privileges was not yet enrolled in the BCRCP database and, thus, data were not available from these hospitals. Subjects in our study were situated throughout the province as follows: Lower Mainland, 35.8%; Fraser Valley, 18.8%; Vancouver Island, 33%; and Interior/Northern BC, 12.3%.
Sociodemographic and pregnancy-related characteristics
The home birth group was similar to the group who had a planned hospital birth attended by a physician (physician comparison group) in age, lone parent status, income quintile and parity because of the matching process (Table 1). Clients in the home birth group were taller than those in the physician comparison group. The home birth group was younger than the group who had a planned hospital birth attended by a midwife (midwife comparison group) and weighed slightly less at the beginning of pregnancy. There were fewer nulliparous clients in the home birth group compared with the midwife comparison group. Clients in the home birth group had slightly higher rates of gravidity compared with the midwife comparison group. Clients in the home birth group were more likely to report the use of tobacco during pregnancy than the midwife comparison group and were more likely to report the use of illicit drugs during pregnancy than the physician comparison group. Clients in the home birth group attended more prenatal visits and were less likely to have had a previous cesarean section compared with either comparison group.
Among home births, 110 (12.8%) were conducted by physicians, 8 (0.9%) by “other” persons (qualified second attendants, usually nurses, attended deliveries when back-up midwives were not available) and 6 (0.7%) were unattended. Midwives attended 738 deliveries (85.6%). In the midwife-attended hospital group, 162 (28.4%) clients had their babies delivered by physicians, 4 (0.7%) by nurses and one (0.2%) by “other.” Midwives attended 404 deliveries (70.8%).
Interventions in labour
The overall rate of transport to hospital for the home birth group was 21.7%, with 142 (16.5%) transports occurring during labour. In the home birth group, there was less frequent use of analgesia, electronic fetal monitoring, augmentation or induction of labour, and episiotomy (Table 2). There were fewer cesarean sections among women in the home birth group (6.4%) compared with the physician comparison group (18.2%) or the midwife comparison group (11.9%). Rates of cesarean section for multiparous women, when women with previous cesarean sections were excluded, were not different (p value cut-off for statistical significance after the Bonferroni correction 0.002). There were fewer cesarean sections for dystocia in the home birth group compared with either comparison group.
In a multivariate analysis controlling for maternal age, lone parent status, income quintile, parity or use of any substances (illicit drugs, alcohol or tobacco), women who intended to have home births were significantly less likely to be exposed to induction or augmentation of labour, epidural analgesia, episiotomy or cesarean section (Table 3).
Maternal outcomes
Thirty-one (3.6% of women in the home birth group) emergency transports took place. Reasons for emergency transports were the following: avoidance of unattended home birth (1), no supervisor available for a conditional midwife in the process of completing the requirements for general registration (1), fetal heart rate decelerations (7), breech presentation diagnosed in labour (2), active herpes in labour (1), thick meconium in labour (2), second-stage arrest of labour (1), hemorrhage (3), retained placenta (3), repair of episiotomy (2), newborn with respiratory distress (5), newborn with birth asphyxia (2), newborn with distended abdomen (1). The median total time from a 911 call to arrival at hospital was 37 minutes, with a range of 15–93 minutes.
Women in the home birth group were more likely to have an intact perineum compared with the midwife comparison group (Table 4). The p value cut-off for statistical significance after the Bonferroni correction was 0.003. There were no differences in rates of postpartum hemorrhage among the 3 groups, but the only 2 cases of obstetric shock occurred in the home birth group. Three of 4 subjects who required blood transfusion were in the home birth group. There were fewer infections in the home birth group compared with either comparison group. In a multivariate analysis controlling for maternal age, lone parent status, income quintile, use of substances and parity (Table 3), there were no significant differences among comparison groups with respect to third-degree or fourth-degree tears or postpartum hemorrhage.
Neonatal outcomes
Neonatal outcomes are presented for babies who did not have major congenital anomalies.
There were 3 cases of perinatal death in the home birth group: 2 stillbirths and one neonatal death. There was one stillbirth in the physician comparison group and no deaths in the midwife comparison group. The relative risk of perinatal death comparing midwife-attended births at home with physician-attended, planned hospital births was 2.5 (95% confidence intervals 0.27–24.5). The 95% confidence intervals for the rate of perinatal death for the home birth group were between 0.9 and 9.0 per thousand births, for the physician comparison group between 0.1 and 8.9 per thousand births and for the midwife comparison groups between 0 and 8.1 per thousand births.
Among perinatal deaths in the home birth group (Table 5), the first stillbirth had no obvious explanation and permission to perform an autopsy was refused by the parents. Fetal demise appeared to have occurred before the onset of labour. In the second stillbirth, a specific cause of death could not be identified by autopsy. The pregnancy had been uneventful, but the midwife ceased to be able to hear the fetal heart during early labour and an emergency transport was initiated. The infant was born at home “tangled in the cord” and resuscitative efforts failed both in transit and on arrival at the hospital. Fetal death was thought to have occurred within a few hours prior to delivery. The infant who died at 2 days of age was the subject of a detailed coroner's inquest, which could not determine a final cause of death. There was no evidence that the ischemia took place during labour and delivery; fetal heart rate patterns during labour were essentially normal. The baby was extremely asphyxiated at birth, however, and never breathed spontaneously. There was evidence of severe hypoxic ischemic encephalopathy with extensive hemorrhage and infarction in other major organs, indicative of a pre-labour insult.
Table 5
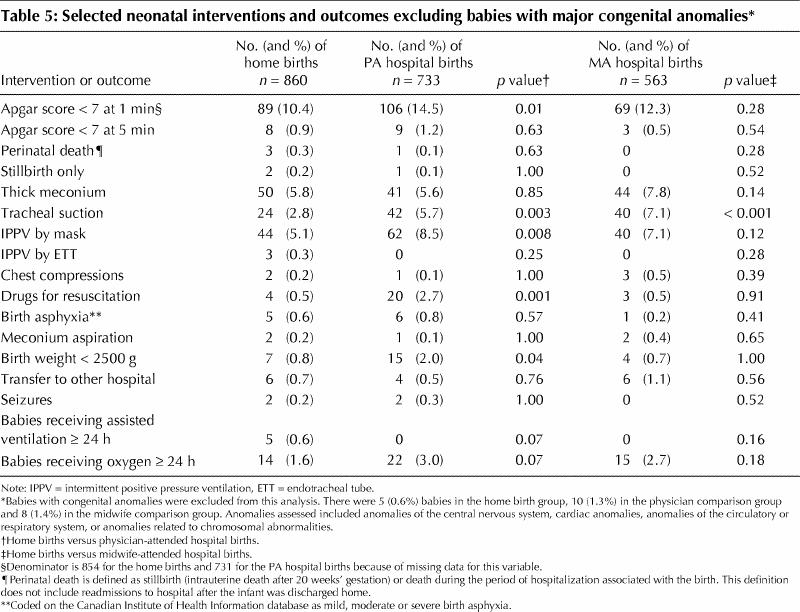
Five babies in the home birth group required assisted ventilation for more than 24 hours, compared with none in either comparison group. Among these babies, one was the baby who died in the neonatal period. Two babies had meconium aspiration syndrome, another was thought to have aspirated clear amniotic fluid, and the fifth had evidence of meconium aspiration although none was seen during labour. We were not able examine the association between need for ventilatory support in a multivariate analysis, because there were no cases in either comparison group.
Rates of low Apgar scores at 5 minutes did not differ among the groups (Table 5) (p value cut-off for statistical significance after Bonferroni correction 0.003). Rates of thick meconium at birth did not differ among the groups. Two babies in the home birth group, one in the physician comparison group and one in the midwife comparison group had meconium aspiration syndrome. Tracheal suction was performed more frequently among babies in the midwife comparison group compared with the home birth group. Drugs for neonatal resuscitation were used more frequently among the physician comparison group. There were 3 sets of twins delivered in the home birth group (data not shown). One set was delivered in hospital; the other 2 were undiagnosed prior to delivery and delivered at home. Apgar scores for twins delivered at home were 7 or more at one minute and 8 or more at 5 minutes. There were no babies delivered at home with breech presentation. Two mothers with cases of breech presentation were transported to hospital as an emergency transport during labour. A controlled multivariate analysis of selected outcomes did not reveal any additional significant associations (Table 3).
Interpretation
Rates of transport to hospital in our study were similar to those reported elsewhere. A recently published evaluation of 961 midwife-attended births in birthing centres in Quebec7 reported a transport rate to hospital during the intrapartum period of 15.8%, which is close to our rate of 16.5%. In a study of 1001 home births in the Toronto area before the regulation of midwifery, the transport rate during labour and post partum was 16.5%.8 In other national, population-based studies of planned home births, rates of intrapartum transport ranged from 14.5% in Australia9 to 20.3% in the Netherlands.3
The rate of emergency transports in our study (3.6%) was slightly higher than in a US study that reported an emergency transport rate of 1%.10 This retrospective survey was limited by a response rate of only 67.6%. The definition of “emergency” is a subjective one arrived at by the midwife in each study.
Rates of interventions during the intrapartum period were predictably lower for the home birth group compared with both groups of women with planned hospital births. These rates are similar to or lower than those reported for women who had given birth in the birthing centres in Quebec.7
Maternal outcomes
Rates of postpartum hemorrhage (≥1000 mL blood loss) were comparable among the groups. In the home birth group there were 2 cases of obstetric shock, and there were none in either comparison group. Three women in the home birth group required a blood transfusion, as did one in the midwife comparison group and none in the physician comparison group. The rate of blood transfusion in our home birth group was 0.3%; in the Quebec study it was 0.2% for births in birthing centres attended by midwives and 0.4% for their physician comparison group.7 The rate of postpartum hemorrhage was 3.8% at the birthing centres in Quebec compared with 4.4% for home births in our study.
An expert review panel reviewed all home births in which there was an emergency transport, an adverse perinatal outcome, unattended birth, or some interagency or interprofessional communications issue. During the course of the project, recommendations arising from each review were forwarded to the Steering Committee of the HBDP, whose membership included representation from the CMBC. A course of action was then decided by the steering committee and implemented by the CMBC. Several clinical issues were identified for inclusion in continuing education initiatives with midwives. These included clinical assessment skills in the antenatal period, documentation of instructions given to clients to ensure that midwives could arrive at the birth in a timely fashion, early transport after identification of thick meconium in the amniotic fluid and active management of the third stage of labour for women at risk for postpartum hemorrhage.11
Neonatal outcomes
A comparison of adverse neonatal outcomes did not identify increased risk for babies born at home as part of the HBDP.
In other studies of planned home birth or birth in a birthing centre, the rate of perinatal death excluding infants with major congenital anomalies ranged from 1.1 per thousand in a British study1 to 10 per 1000 in the Quebec study,7 with reported rates in the United States,2 the Netherlands,3 Switzerland,4 New Zealand5 and Australia9,12 falling in between. Although our perinatal death rate lies well within the rates described in other population-based studies, it deserves ongoing monitoring in view of the small numbers of births it is based on to date. A study large enough to compare perinatal death rates accurately, if the annual rate of home births with regulated midwives in BC were to remain the same as it is today, would require 7–8 years of data collection.
Rates of exposure to thick meconium did not differ among our study groups, nor did the rate of meconium aspiration. Intubation and suction of vigorous infants, even in the presence of thick or particulate meconium, has not been associated with a decrease in meconium aspiration syndrome or other respiratory disorders.13 The question of the efficacy of tracheal suction for the compromised infant, however, remains unanswered.13 Of the babies who were exposed to thick meconium and whose Apgar score at one minute was less than 7, 45% in the home birth group received tracheal suction compared with 75% in each comparison group. Babies exposed to thick meconium who are not vigorous at birth may be disadvantaged in the home birth group, particularly in view of the trend toward increased need for assisted ventilation in this group.
The rate of Apgar scores that were less than 7 at 5 minutes in the home birth group, excluding stillbirths and babies with congenital anomalies, was 0.9%, which was not different from those in the comparison groups. The rate in the Quebec study among newborns whose mothers intended to deliver at birthing centres was 4.1%.7 Rates of seizure did not appear to be different among our 3 groups and are too low to be compared statistically within our study or with the Quebec rate of 0.6%. Rates of birth weight that was less than 2500 g (0.8%) in our home birth group did not differ from the midwife comparison group (0.7%) and were somewhat lower than the rate of 2% among women attended by midwives in the Quebec study.
The outcome analysis was limited by the fact that not all the hospitals from which control subjects should have been drawn were enrolled in the British Columbia Perinatal Data Registry. Furthermore, some hospitals to which infants in the home birth and comparison groups were transferred were also not enrolled in the registry. It is possible that some adverse outcomes for both the home birth babies and the comparison groups were omitted because of a lack of accessibility to all relevant data. However, in the home birth group, additional records were available with information about indications for consultation, transfer of care to a physician and transport to hospital. Among cases with adverse outcomes identified on BCRCP forms, the entire chart was reviewed by the expert review panel. It is likely that any bias associated with the inability to identify all adverse outcomes would be conservative with respect to the home births, because we had additional information for women with planned home births that we did not have for the comparison groups. In addition, 4 of the 5 hospitals that could not submit data were in rural settings. The absence of comparison subjects from these hospitals, which may have had fewer resources for managing complicated clinical situations, may have biased the analysis against the home birth group.
Despite the care taken in this study to match the 3 groups, there may be differences regarding the women who chose home birth that placed them at either lower or higher risk for adverse outcomes that we are unable to measure.
Our study has evaluated outcomes during the first 2 years of implementation of midwifery, including home birth, in BC. During this time, policy and protocols have continued to evolve. It may not be possible to generalize our findings to ensuing years as midwifery communication systems and practice become more integrated within our health care system.
Our findings from BC support those of previous reports that suggest that there are no indications of increased risk associated with planned home birth attended by regulated midwives, compared with those attended by either midwives or physicians in hospital. However, the consequences of some of the expected complications (thick meconium in the amniotic fluid and hemorrhage) may be more serious for women and their babies when women deliver at home than when they deliver in hospital. These comparisons are based on small numbers and warrant ongoing evaluation.
Footnotes
This article has been peer reviewed.
Acknowledgements: This project was supported by a financial contribution from the Health Transition Fund, Health Canada. The views expressed here do not necessarily represent the official policy of federal, territorial or provincial governments.
Competing interests: None declared.
Correspondence to: Dr. Patricia Janssen, Department of Family Practice, University of British Columbia, 5804 Fairview Ave., Vancouver BC V6T 1Z3; fax 604 822-6950; pjanssen@interchange.ubc.ca
References
- 1.Chamberlain G, Wraight A, Crowley P. Birth at home: a report of the national survey of home births in the UK by the National Birthday Trust. Pract Midwife 1999;2:35-39. [PubMed]
- 2.Janssen P, Holt V, Myers S. Licensed midwife-attended, out-of-hospital births in Washington State: Are they safe? Birth 1994;21:141-8. [DOI] [PubMed]
- 3.Wiegers T, Keirse M, van der Zee J, Berghs G. Outcome of planned home and planned hospital births in low risk pregnancies: prospective study in midwifery practices in the Netherlands. BMJ 1996;313:1309-13. [DOI] [PMC free article] [PubMed]
- 4.Ackermann-Liebrich U, Voegeli T, Günter-Witt K, Kunz I, Züllig M, Schindler C, et al. Home vs. hospital deliveries: follow up study of matched pairs for procedures and outcome. BMJ 1996;131:1313-8. [DOI] [PMC free article] [PubMed]
- 5.Gulbransen G, Hilton J, McKay L, Cox A. Home birth in New Zealand 1973–93: incidence and mortality. N Z Med J 1997:110;87-9. [PubMed]
- 6.Handbook for midwives and health care professionals. Victoria (BC): Ministry of Health and Ministry Responsible for Seniors, Home Birth Demonstration Project; 2000.
- 7.Fraser W, Hatem-Asmar M, Krauss I, Maillard F, Bréart G, Blais R. Comparison of midwifery care to medical care in hospitals in the Quebec Pilot Projects Study: clinical indicators. L'Équipe d'Évaluation des Projets-Pilotes Sages-Femmes. Can J Public Health 2000;91(1):I5-11. [DOI] [PMC free article] [PubMed]
- 8.Tyson H. Outcomes of 1001 midwife-attended home births in Toronto, 1983–1988. Birth 1991;18:14-9. [DOI] [PubMed]
- 9.Woodcock H, Read A, Moore D, Stanley F, Bower C. Planned homebirths in Western Australia 1981–1987: a descriptive study. Med J Aust 1990;153:672-8. [PubMed]
- 10.Anderson R, Murphy P. Outcomes of 11,788 planned home births attended by certified nurse-midwives. J Nurse Midwifery 1995;6:483-92. [DOI] [PubMed]
- 11.Janssen P, Lee S. Home Birth Demonstration Project. Final Report to the Health Transition Fund, Appendix C, 2000. Victoria: British Columbia Ministry of Health and Ministry Responsible for Seniors; 2000. Project no BC404.
- 12.Bastian H, Keirse M, Lancaster P. Perinatal death associated with planned home birth in Australia. BMJ 1998;317:384-8. [DOI] [PMC free article] [PubMed]
- 13.Wiswell T, Gannon C, Jacob J, Goldsmith L, Szyld E, Wiess K, et al. Delivery room management of the apparently vigorous meconium-stained neonate: results of the Multicenter International Collaborative Trial. Pediatrics 2000; 1:1-7. [DOI] [PubMed]


